Abstract
The association of physical activity with renal outcome and mortality in advanced chronic kidney disease (CKD; i.e., estimated glomerular filtration rate [eGFR] < 45 ml/min/1.73m2) is poorly studied. We examined this association in patients with advanced CKD in Japan. We used the Rapid Assessment of Physical Activity to assess baseline physical activity and classify patients as active or inactive. CKD progression was defined as 40% decline in eGFR, eGFR < 10, or requiring dialysis or transplantation. Among the 1,808 eligible patients, after adjusting for possible confounders, hazard ratios (HRs) for poor renal outcome in the active group were 0.68 (95% CI, 0.44–1.04), 1.09 (0.86–1.38), and 1.01 (0.82–1.25) in CKD stage G3b, G4, and G5, respectively, suggesting a renal benefit of exercise in CKD stage G3b. Adjusted HRs for death were 0.79 (0.40–1.57), 0.55 (0.38–0.80), and 0.75 (0.44–1.26) in stage G3b, G4, and G5, respectively. While the adjusted HRs of death were 0.84 (0.52–1.38) and 0.60 (0.43–0.83) in diabetic and non-diabetic patients, suggesting that exercise may reduce mortality in non-diabetic patients. Our study suggests that exercise is associated with better survival in non-diabetic patients with CKD stage G3b-5, and better renal outcome in diabetic and non-diabetic CKD stage G3b.
Keywords: Physical activity, Exercise, eGFR decline, Renal outcomes, Mortality
Subject terms: Health care, Nephrology
Introduction
Frailty and protein-energy wasting are common in older adults with CKD and are associated with impaired physical performance, lower quality of life, and poor survival. Therefore, prevention and treatment of these conditions in older CKD patients are emergent issues that often require a multidisciplinary approach, including physical therapy, medication, nutritional support, nursing, and mental and social support1. The association between physical activity and prognosis in CKD patients started to attract attention in the 20th century. In 2010, Tentori et al. reported that mortality risk was 37% lower in dialysis patients who performed regular exercise2. And in 2014, Chen et al. found in a study in Taiwan that regular walking was associated with lower mortality and risk of renal replacement therapy in patients with CKD stage G3 to G5: The risks of mortality and renal replacement therapy were 33% and 21% lower in the walking group than in the non-walking group, respectively3. In 2012, the KDIGO (Kidney Disease Improving Global Outcomes) clinical practice guidelines recommended that CKD patients aim for at least 30 min of physical activity, five times per week4. However, this recommendation was based on evidence of the link between exercise therapy and cardiovascular health, and it was still unclear whether interventional exercise was effective for renal function. Therefore, in 2018 we performed a systematic review and found that exercise therapy leads to a slight but significant increase in estimated glomerular filtration rate (eGFR) in this population (mean increase, 2.22 ml/min/1.73m2 [95% CI, 0.68, 3.76])5. Thereafter, other studies provided similar evidence suggesting a positive interventional effect of physical activity on short-term eGFR6,7. Thus, in patients with CKD, exercise appears to have beneficial effects on not only cardiovascular disease but also renal function.
In addition, one study reported that exercise may prevent the development of sarcopenia, help maintain muscle mass, and increase plasma myostatin in patients with CKD stage G3 to G5 8. Myostatin is one of the myokines released from muscle, and several studies have suggested that myokine-mediated muscle-kidney crosstalk can improve kidney energy metabolism and fibrogenesis in kidney disease9. These findings imply that exercise may improve renal outcomes and reduce mortality in patients with advanced CKD. On the other hand, to date the evidence is based mostly on findings in obese and relatively young CKD patients, and evidence for the effects of exercise in older, frail patients with CKD, especially those with advanced CKD, is very limited. In addition, though exercise therapy is the first-line therapy for patients with diabetes, there is no clear evidence for those in patients with diabetic kidney disease. Therefore, in this 5-year study in a nationally representative cohort in Japan, the REACH-J study, we aimed to clarify the association between physical activity and renal outcome and mortality in patients with advanced CKD, in particular with respect to the presence of diabetes.
Materials and methods
Study design and patient sample
The REACH-J study is an ongoing 5-year prospective cohort study of non-dialysis patients with CKD stage G3b to G5 (eGFR ≤ 45 ml/min/1.73m2) being treated at 31 nephrology clinics in Japan. To minimize patient selection bias, the clinics were randomly selected from the nationwide nephrology specialist list after stratification by region and facility size, in alignment with the international Chronic Kidney Disease Outcomes and Practice Patterns (CKDopps) project. The study design of the REACH-J study and CKDopps project have been published previously10–12. Briefly, anonymized data were collected annually from patients and physicians, including clinical data and a patient questionnaire. Information on patients’ medical history and complications, including diabetes, hypertension, cardiovascular diseases, and cancers, were collected from medical records. Patients aged younger than 20 years, those with a history of kidney transplantation or dialysis, and those who did not agree to participate in the study were excluded.
The study protocol was approved by the Tsukuba institutional review board (approval number: H27-199) and the review board of the Japanese Society of Nephrology (approval number: 29). The study adhered to the Declaration of Helsinki and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement and was registered with the University Hospital Medical Information Network (registration number: UMIN000022145).
Physical activity levels
Patients’ baseline physical activity levels were assessed by the Rapid Assessment of Physical Activity (RAPA) questionnaire, which shows a good correlation with direct measurement of physical activity by accelerometers13,14. The RAPA questionnaire was included in the baseline self-reported patient questionnaire. The RAPA questionnaire consists of nine binary questions (yes/no) with graphical illustrations. In this study, we defined binary levels of physical activity (active or inactive) by applying the approach used in our previous study and by Topolski et al.14. Active was defined as being often or very active according to the responses to the first seven RAPA questions, and inactive, as being never, infrequently, or sometimes active15.
Outcomes
We defined CKD progression as a 40% decline in eGFR from baseline, an eGFR of less than 10 ml/min/1.73m2, or end-stage kidney disease requiring dialysis or transplantation, whichever occurred first, and mortality as fatal events from any cause during follow-up. As additional outcomes, we compared eGFR decline in patients with and without diabetes and between CKD stages in the active and inactive groups.
Statistical analyses
Patient demographics were summarized as mean and standard deviation (SD) or median and interquartile range (IQR). We evaluated incidence rates and hazard ratios (HRs) for renal outcome and death with a modified Poisson regression model and a Cox proportional hazard model, respectively. We also evaluated eGFR decline per year with a linear mixed model with subject and center as random effects. All models were adjusted for age, sex, smoking status, body mass index, eGFR, level of proteinuria, serum albumin, hemoglobin, diabetes, comorbidity score, congestive heart failure, and lung disease and evaluated by activity group, the presence or absence of diabetes, and CKD stage. Multiple imputation was used in all analyses to impute missing covariate values. Twenty complete data sets were imputed, all analyses were performed with each data set, and results were combined using Rubin’s rules.
A comorbidity score was calculated for each patient as the number of comorbidities out of the following 10: coronary heart disease, hypertension, other cardiovascular disease, cerebrovascular disease, peripheral vascular disease, recurrent cellulitis/gangrene, neurologic disease, psychiatric disorder, gastrointestinal bleeding, and cancer15. If separation problems were observed because of the small number of samples, the applicable explanatory variables were excluded from the analyses.
P values of less than 0.05 were considered significant. All analyses were performed with SAS software, version 9.4 (SAS Institute, Cary, NC). Confidence intervals (CIs) were reported as 95% CIs.
Results
From 2,249 patients with advanced CKD, 1,808 eligible patients (407 with diabetes and 1,401 without diabetes) with a baseline assessment of physical activity levels by the RAPA questionnaire were enrolled in the study. We divided patients into active (n = 1,237) and inactive (n = 571) based on the RAPA results. Table 1 shows the characteristics in groups of active and inactive exercises. The mean age of the active group was lower than that of inactive group but the mean eGFR was higher. The proportions of patients with diabetes and/or hypertension and the comorbidity scores were similar in the two groups. Medications were also similar, except for the use of erythropoiesis-stimulating agents (ESA), which were used in significantly fewer patients in the active group than in the inactive group (29% vs. 36%, respectively). Because hemoglobin levels were similar in the two groups, this finding may imply better ESA responsibility in active patients.
Table 1.
Characteristics of patients in groups of active and inactive exercises.
| Variable | Inactive (n = 571) | Active (n = 1237) | p-value |
|---|---|---|---|
| Age (years) | 70.8 ± 11.7 | 68.5 ± 12.5 | < 0.001 |
| Male, % | 61 | 66 | 0.057 |
| Current smoker, % | 12 | 10 | 0.151 |
| Body mass index | 23.5 ± 4.3 | 23.5 ± 5.1 | 0.880 |
| eGFR (ml/min/1.73m2) | 22.1 ± 10.4 | 24.1 ± 10.4 | < 0.001 |
| Albumin(g/dl) | 3.9 ± 0.4 | 4.0 ± 0.4 | 0.016 |
| Hemoglobin (g/dl) | 11.6 ± 1.7 | 12.0 ± 1.7 | < 0.001 |
| Calcium (mg/dl) | 8.9 ± 0.6 | 9.0 ± 0.7 | 0.120 |
| Phosphate (mg/dl) | 3.7 ± 0.8 | 3.6 ± 0.8 | 0.026 |
| Intact PTH | 132 [85, 296] | 107 [69, 189] | 0.032 |
| Proteinuria A3, % | 52 | 46 | 0.038 |
| Transferrin saturation < 20%, % | 18 | 19 | 0.907 |
| Ferritin < 100 ng/ml, % | 50 | 54 | 0.420 |
| Complications | |||
| Diabetes, % | 34 | 31 | 0.278 |
| Hypertension, % | 89 | 87 | 0.318 |
| Comorbidity score, out of 10* | 1.7 ± 1.0 | 1.6 ± 1.0 | 0.013 |
| Medications, % | |||
| Renin-angiotensin system inhibitors | 59 | 61 | 0.291 |
| Antihypertensives(other) | 73 | 69 | 0.081 |
| Statins | 38 | 43 | 0.066 |
| SGLT2 inhibitors | 0.7 | 0.8 | 1.000 |
| Erythropoiesis-stimulating agents | 36 | 29 | 0.008 |
| Oral irons | 11 | 10 | 0.545 |
eGFR estimated glomerular filtration rates.
*The comorbidity score was calculated per patient as the number of comorbidities out of the following 10: coronary heart disease, hypertension, other cardiovascular disease, cerebrovascular disease, peripheral vascular disease, recurrent cellulitis/gangrene, neurologic disease, psychiatric disorder, gastrointestinal bleeding, and cancer15.
The crude incidences of CKD progression per 100 person-years in our cohort were 14.3 in total, 13.3 in active group, and 15.3 in inactive group, respectively. Those of death were 3.0 in total, 2.3 in active group, and 4.0 in inactive group, respectively. These data suggests that both CKD progression and death in Japan were lower than those in the previous study in the United States and Brazil15. The adjusted incidence rate of poor renal outcome per 100 person-years was slightly higher in diabetic patients than that of non-diabetic patients (10.4 (8.6, 12.7) vs. 11.9 (9.4, 15.2), p = 0.29). The incidence rate ratio (IRR)s of poor renal outcome in the active group compared with the inactive group were 0.87 (0.66, 1.14) in diabetic and 1.03 (0.88, 1.22) in non-diabetic patients, and the IRRs of death was 0.86 (0.53, 1.38) in the diabetic and 0.57 (0.40, 0.79) in the non-diabetic patients (Table 2). As can be seen in Table 2, incidence rates increased in higher CKD stages. Similarly, the adjusted incidence rate of death per 100 person-years was slightly higher in diabetic patients than that of non-diabetic patients (1.7 (1.1, 2.8) vs. 1.5 (1.0, 2.3), p = 0.57).
Table 2.
Adjusted incidence rates of renal outcomes and death by CKD stages, per 100 person-years.
| CKD Stage |
Renal outcome | Death | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diabetic (n = 407) | Non-diabetic (n = 1,401) | Diabetic (n = 407) | Non-diabetic (n = 1,401) | |||||||||
| Active (n = 269)) | Inactive (n = 138) | IRR | Active (n = 968) | Inactive (n = 433) | IRR | Active (n = 269) | Inactive (n = 138) | IRR | Active (n = 968) | Inactive (n = 433) | IRR | |
| All | 20.0 (14.6, 27.2) | 23.0 (16.1, 32.9) | 0.87 (0.66, 1.14) | 9.1 (7.2, 11.4) | 8.8 (6.9, 11.1) | 1.03 (0.88, 1.22) | 3.6 (1.9, 7.0) | 4.2 (2.2, 8.1) | 0.86 (0.53, 1.38) | 0.8 (0.4, 1.6) | 1.5 (0.8, 2.7) | 0.57 (0.40, 0.79) |
| G3b | 6.3 (2.8, 14.0) | 10.2 (4.4, 23.5) | 0.61 (0.32, 1.19) | 2.5 (1.4, 4.5) | 3.3 (1.8, 6.0) | 0.77 (0.48, 1.21) | 2.2 (0.4, 11.2) | 1.2 (0.1, 13.1) | 1.82 (0.24, 14.11) | 0.5 (0.1, 1.7) | 0.7 (0.2, 2.5) | 0.72 (0.33, 1.56) |
| G4 | 14.2 (9.4, 21.6) | 15.6 (9.6, 25.3) | 0.91 (0.61, 1.36) | 9.8 (7.1, 13.5) | 8.8 (6.2, 12.4) | 1.12 (0.89, 1.41) | 4.4 (2.5, 7.9) | 4.1 (2.2, 7.6) | 1.08 (0.54, 2.19) | 1.0 (0.4, 2.4) | 2.2 (1.0, 5.1) | 0.43 (0.27, 0.68) |
| G5 | 88.1 (53.4, 145.4) | 91.6 (48.7, 172.5) | 0.96 (0.61, 1.51) | 36.4 (26.4, 50.4) | 34.0 (24.4, 47.5) | 1.07 (0.83, 1.39) | 1.7 (0.5, 6.6) | 2.6 (0.8, 8.5) | 0.65 (0.27, 1.57) | 0.6 (0.1, 2.2) | 0.8 (0.2, 2.7) | 0.73 (0.37, 1.44) |
IRR: incidence rate ratio in the active group compared with the inactive group (active/inactive).
The adjusted model includes adjustment for age, sex, smoking status, body mass index, eGFR, level of proteinuria, serum albumin, hemoglobin, diabetes, comorbidity score, cognitive heart failure, and lung disease. Renal outcome was defined as a 40% decline in eGFR from baseline, an eGFR of less than 10 ml/min/1.73m2, or end-stage kidney disease requiring dialysis or transplantation, whichever occurred first.
Significant values are given in italics.
When patients were divided according to CKD stage, in diabetic patients the adjusted IRR indicated a trend towards a lower incidence of poor renal outcomes in the active group than in the inactive group (Table 2). This trend was also observed in all CKD stages in the diabetic group but only in CKD stage G3b in the non-diabetic group. The IRRs of death were significantly lower in non-diabetic patients, with the lowest IRR in CKD stage G4 (0.43 [0.27, 0.68]). The IRRs of death in diabetic patients did not show any trends by CKD stage.
Next, we analyzed the HRs of poor renal outcome and death by Cox proportional hazard models and eGFR declines in active and inactive patients by diabetes status and CKD stage. Models were adjusted for age, sex, smoking status, body mass index, eGFR, level of proteinuria, serum albumin, hemoglobin, diabetes, lung disease, congestive heart failure, and comorbidity score (Table 3; Fig. 1). Overall, the adjusted HRs for poor renal outcome were less than 1 in stage G3b, and those for death were less than 1 in all CKD stages. In diabetic patients, the adjusted HRs for poor renal outcome were less than 1 in the whole group and in stages G3b, G4, and G5 (Table 3), and the adjusted HRs for death were below 1 in the whole group and stage G5 but greater than 1 in stage G3b and G4. Thus, these results suggest that exercise may be beneficial for renal outcome but not for mortality in diabetic patients with better renal function. On the other hand, in non-diabetic patients the adjusted HRs for poor renal outcome were greater than 1 in the whole group, less than 1 in stage G3b, and greater than 1 in stage G4 and G5 and the adjusted HRs for death were less than 1 in the whole group and also in stage G3b, G4, and stage G5. These results suggest that exercise may be beneficial for mortality but not for renal outcome in non-diabetic patients. Regarding eGFR decline in these groups, eGFR declined a similar amount in the active and inactive patients in both the diabetic and non-diabetic subgroups; however, among patients with CKD stage G3b, it declined significantly less in the active group than in the inactive group, suggesting renoprotective effects of activity in early CKD stages.
Table 3.
The adjusted hazard ratios of renal outcome and death, and difference of eGFR declines, divided by physical activity (active vs. inactive).
| CKD | Renal outcome | p | Death | p | eGFR slope difference | p | eGFR slope(active) | eGFR slope(inactive) | |
|---|---|---|---|---|---|---|---|---|---|
| Stage | HR (95% CI) | HR (95% CI) | ml/min/1.73m2, vs. inactive |
ml/min/1.73m2 | ml/min/1.73m2 | ||||
| All | total | 1.00 (0.87, 1.16) | 0.96 | 0.62 (0.48, 0.82) | < 0.001 | 0.01 (-0.12, 0.15) | 0.83 | -1.56 (-1.63, 0.15) | -1.58 (-1.70, -1.45) |
| G3b | 0.68 (0.44, 1.04) | 0.08 | 0.79 (0.40, 1.57) | 0.51 | 0.58 (0.21, 0.94) | 0.003 | -1.41 (-1.58, -1.24) | -1.98 (-2.28, -1.69) | |
| G4 | 1.09 (0.86, 1.38) | 0.47 | 0.55 (0.38, 0.80) | 0.002 | -0.24(-0.45, -0.03) | 0.02 | -1.86 (-1.98, -1.75) | -1.62 (-1.79, -1.45) | |
| G5 | 1.01 (0.82, 1.25) | 0.92 | 0.75 (0.44, 1.26) | 0.28 | -0.06(-0.18, 0.06) | 0.30 | -0.97 (-1.21, -0.72) | -0.87 (-1.16, -0.58) | |
| Diabetic | total | 0.88 (0.66, 1.17) | 0.37 | 0.84 (0.52, 1.38) | 0.5 | 0.02 (-0.36, 0.40) | 0.91 | -1.72 (-1.92, -1.52) | -1.75 (-2.08, -1.41) |
| G3b | 0.37 (0.15, 0.91) | 0.03 | 1.57 (0.27, 9.23) | 0.62 | 0.68 (-0.47, 1.83) | 0.24 | -1.80 (-2.34, -1.27) | -2.48 (-3.50, -1.47) | |
| G4 | 0.89 (0.53, 1.49) | 0.65 | 1.04 (0.51, 2.15) | 0.91 | -0.26(-0.70, 0.17) | 0.23 | -1.85 (-2.09, -1.60) | -1.58 (-1.97, -1.20) | |
| G5 | 0.93 (0.62, 1.40) | 0.74 | 0.78 (0.29, 2.05) | 0.61 | -0.10(-0.44, 0.24) | 0.56 | -0.97 (-1.21, -0.72) | -0.87 (-1.16, -0.58) | |
| Non-diabetic | total | 1.05 (0.88, 1.25) | 0.58 | 0.60 (0.43, 0.83) | 0.002 | 0.01 (-0.16, 0.17) | 0.94 | -1.52 (-1.60, -1.44) | -1.53 (-1.67, -1.38) |
| G3b | 0.73 (0.43, 1.23) | 0.23 | 0.66 (0.29, 1.49) | 0.32 | 0.42 (0.07, 0.76) | 0.02 | -1.36 (-1.53, -1.20) | -1.78 (-2.08, -1.47) | |
| G4 | 1.10 (0.84, 1.44) | 0.49 | 0.39 (0.24, 0.62) | < 0.001 | -0.17 (-0.38, 0.04) | 0.12 | -1.81 (-1.94, -1.68) | -1.64 (-1.83, -1.45) | |
| G5 | 1.05 80.81, 1.36) | 0.72 | 0.72 (0.37, 1.41) | 0.34 | -0.03 (-0.26, 0.21) | 0.82 | -1.08 (-1.20, -0.96) | -1.05 (-1.28, -0.83) |
HR hazard ratio, CI confidence interval, DKD diabetic kidney disease, CKD chronic kidney disease, p p-value, eGFR estimated glomerular filtration rate. Renal outcome was defined as a 40% decline in eGFR from baseline, an eGFR of less than 10 ml/min/1.73m2, or end-stage kidney disease requiring dialysis or transplantation, whichever occurred first.
The adjusted model includes adjustment for age, sex, smoking status, body mass index, eGFR, level of proteinuria, serum albumin, hemoglobin, diabetes, comorbidity score, cognitive heart failure, and lung disease.
Significant values are given in italics.
Fig. 1.
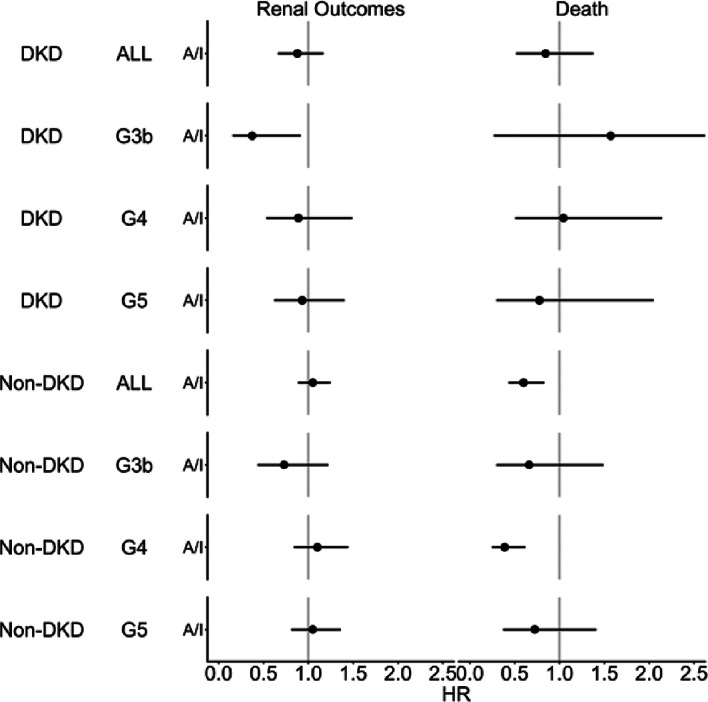
The adjusted hazard ratios of renal outcome and death divided by physical activity (active vs. inactive). DKD diabetic kidney disease, HR hazard ratio, G3b G4, and G5 represents CKD stages. Renal outcome was defined as 40% decline of eGFR from baseline, eGFR < 10 ml/min/1.73m2, or end-stage kidney disease requiring dialysis or transplantation, whichever occurred first. Models were adjusted for age, sex, smoking status, body mass index, eGFR, level of proteinuria, serum albumin, hemoglobin, diabetes, comorbidity score, cognitive heart failure, and lung disease. The comorbidity score was calculated per patient as the number of comorbidities out of the following 10: coronary heart disease, hypertension, other cardiovascular disease, cerebrovascular disease, peripheral vascular disease, recurrent cellulitis/gangrene, neurologic disease, psychiatric disorder, gastrointestinal bleeding, and cancer.
Discussion
In this study, we examined the association of physical activity with renal outcome and mortality in patients with CKD stage G3b to G5 with and without diabetes. The main findings were that the active group, especially the active non-diabetic patients, had lower mortality than the inactive group (HR 0.60 (0.43, 0.83)), and that poor renal outcomes were less prevalent in the active group than in the inactive group in CKD stage G3b, both in patients with and without diabetes (HR 0.37 (0.15, 0.91) in diabetes, 0.73 (0.43, 1.23) in non-diabetes), even after adjusting for possible confounders. Because we used a random sampling design based on the nationwide nephrology specialist list to minimize patient selection bias, our results may be a good representation of the situation in routine clinical care in Japan.
An association between physical activity and mortality in CKD patients has been reported since the 2010s16. As described in the introduction, Chen et al. found that regular walking was associated with lower mortality and lower risk of renal replacement therapy in patients with CKD stage G3 to G5, however, the authors did not report the effect of regular walking according to diabetes status17. In our study, the IRRs of CKD progression in the active group compared with the inactive group were 13% lower in the diabetic patients, and those of death were 14% and 43% lower in diabetic and non-diabetic patients, respectively. Furthermore, the CKDopps studies in the United States and Brazil reported that the crude incidence of CKD progression and death were 19 and 12 per 100 person-years in never-active patients and 14 and 7 per 100 person-years in low/high active patients, respectively. The incidences found in the above-mentioned study by Chen et al. and the CKDopps studies in patients with advanced CKD, which used the same study design, were higher than those in our Japanese population2,3. Although the definition of activity and the proportion of patients with diabetes were not identical in our study and the study by Chen et al., both studies found a positive association between physical activity and mortality and renal outcome.
In our study, we observed better renal outcome or better eGFR slopes in patients with CKD stage G3b regardless of the presence of diabetes but not in CKD stage G4 and G5. Surprisingly, the level of physical activity was not associated with renal outcome in patients with late stages of advanced CKD regardless of diabetes status, whereas a lower mortality risk was observed in the active non-diabetic patients with CKD stage G4. Recently, several large multidisciplinary interventional studies, including studies on lifestyle management in early stage diabetic and non-diabetic patients, suggested that effects are observed around 10 years after starting an intervention18,19. For example, the Steno-2 study found that the eGFR declines in both intensive and control groups were similar for 4 years but that renoprotective effects were observed thereafter and the yearly eGFR decline in the conventional therapy group was 28% higher than in the intensive therapy group at 21 years19. Therefore, a 5-year observation period may be too short to examine the effects of physical activity on CKD progression and death in CKD patients. The important message from this study is that an active lifestyle is never harmful and may be beneficial in CKD patients with and without diabetes. In addition, recent studies have shown that levels of circulating irisin, an important hormone with anti-inflammatory, anti-oxidative, and anti-apoptotic properties, decrease with increasing CKD stage20. A study in mice found that exercise may increase the amount of irisin released from muscle, which could have an anti-inflammatory effect through nuclear factor kappa B21. Therefore, exercise may have anti-inflammatory or vascular cardioprotective effects in humans that may lead to better renal outcome, especially in early stages of advanced CKD.
This study has several limitations. First, it was not an interventional study in CKD patients with low physical activity. Although our previous systematic review suggested a positive effect of a short-term exercise intervention on renal function5, the effects of long-term lifestyle interventions on renal outcome, especially in patients with advanced CKD and frailty, are still unknown. And as nature of observational study, it is difficult to assess causal relationship between exercise intervention on renal function from our findings. Because frailty is known to be an important factor affecting mortality in CKD patients, future studies should examine the interventional effects of activity in CKD patients with frailty. Second, patients’ physical activity level was obtained from a self-reported questionnaire, not from direct measurement of physical activity by accelerometers. Therefore, we should keep in mind the self-report bias in this study. Nevertheless, the RAPA score is widely known to be useful, and self-report bias usually causes results to approach null, i.e., this self-report bias may not have led to an overestimation our results. Finally, our results may not be generalizable to other countries because patient characteristics, diet, and lifestyles are often different in each country. To overcome this limitation, future international comparison studies need to evaluate the association of physical activity with renal outcomes and mortality.
In conclusion, our multicenter study suggests that higher physical activity is associated with better renal outcome in CKD stage G3b regardless of diabetes status and with better survival in non-diabetic patients, especially those with CKD stage G4. Therefore, earlier intervention to maintain activity levels may be beneficial in CKD patients. Long-term interventional studies on maintaining physical activity in CKD patients may strengthen the evidence for the effects of an active lifestyle on CKD.
Acknowledgements
We thank all the nephrology specialists in Japan who responded to our REACH-J survey, Dr. Hiroyuki Hoshimoto and all the staff members of the Clinical Trial and Research Center, University of Tsukuba (T-CReDO), Mr. Yoshihiro Ishihara and other staff members of Flexible Inc., and all the staff members of Arbor Research, for their contribution to our work.
Author contributions
J.H. designed the study and wrote the initial draft of the manuscript. T.O. analyzed data. R.Y., Y.I., H.K., C.S., K.Y. collecting and managing the data. J.H., H.O., I.N., T.W., S.M., and K.Y. managing the data and study protocol as steering committee members of the REACH-J. R.P. and R.F. contributed to the design of the study and data interpretation. All authors approved the final version of the manuscript.
Funding
The study was supported by a Grant-in-Aid for Research on Advanced Chronic Kidney Disease, Practical Research Project for Renal Diseases from the Japan Agency for Medical Research and Development, grants from Kyowa-Kirin Co., and Mitsubishi Tanabe Pharm. Preparation of the manuscript was supported in part by JH’s grant from Grants-in-Aid for Scientific Research (JSPS KAKENHI) Grant Number 24K14335.
Data availability
The datasets analyzed during the current study are not publicly available due to data sharing policy of the REACH-J study but are available from the corresponding author after the permission of steering committee of the REACH-J study on reasonable request.
Declarations
Competing interests
The authors declare no competing interests. The REACH-J study is supported by Kyowa Kirin Co. Ltd. and Tanabe-Mitsubishi Pharm Ltd. Dr. Okada is funded by Takeda Pharm., Chugai Pharm., Kyowa-Hakko Kirin, Pfizer, Boehinger Ingelheim, Astellas Pharm., Otsuka Pharm., MSD, Shionogi, Novaltis, Sumitomo Dainippon Pharm., Mitsubishi Tanabe Pharm., and Daiichi Sankyo Co. Dr. Pecoits-Filho and Dr. Pisoni are members of Clinical Research for the non-profit organization Arbor Research Collaborative for health, which has designed and carried out the Dialysis Outcomes and Practice Pattern Study (DOPPS) Program. The DOPPS program is supported by Amgen, Kyowa Kirin, AbbVie Inc., Sanofi Renal, Baxter Healthcare, and Vifor Fresenius Medical Care Renal Pharma Ltd. Additional support for specific projects and countries is also provided in Canada by Amgen, BHC Medical, Janssen, Takeda, Kidney Foundation of Canada (for logistics support); in Germany by Hexal, DGfN, Shire, WiNe Institute; and for the Peritoneal-DOPPS in Japan by the Japanese Society for Peritoneal Dialysis (JSPD). The DOPPS.org website lists the full details. JDOPPS was administered by the Arbor Research Collaborative for Health, Ann Arbor, MI, USA, and supported by Kyowa Kirin Co. Ltd. All support is provided without restrictions on publications. All other authors have no conflict disclosure.
Human and animal rights
The study’s protocol was approved by the Tsukuba institutional review board (IRB) (H27-199) and the review board of the Japanese Society of Nephrology (No. 29), and has been or will be approved by the IRB of each participating facility. The study procedures fully adhered to the Declaration of Helsinki and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement, and was registered with the University Hospital Medical Information Network (UMIN000022145).
Informed consent
Informed consent was and will be obtained from all individual participants included in the study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Junichi Hoshino, Email: hoshino.junichi@twmu.ac.jp.
Kunihiro Yamagata, Email: k-yamaga@md.tsukuba.ac.jp.
References
- 1.Hoshino, J. R. & Rehabilitation Exercise intervention and nutritional support in Dialysis patients. Nutrients. 13. 10.3390/nu13051444 (2021). [DOI] [PMC free article] [PubMed]
- 2.Tentori, F. et al. Physical exercise among participants in the Dialysis outcomes and practice patterns study (DOPPS): correlates and associated outcomes. Nephrol. Dial Transpl.25, 3050–3062. 10.1093/ndt/gfq138 (2010). [DOI] [PubMed] [Google Scholar]
- 3.Chen, I. R. et al. Association of walking with survival and RRT among patients with CKD stages 3–5. Clin. J. Am. Soc. Nephrol.10.2215/cjn.09810913 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eknoyan, G., Lameire, N. & Eckardt, K. U. KDIGO 2012 Clinical Practice Guideline for the evaluation and management of chronic kidney disease. Kidney Int. Supplements. 3, 136–150 (2013). [DOI] [PubMed] [Google Scholar]
- 5.Yamagata, K. et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Ren. Replace. Therapy. 5, 28. 10.1186/s41100-019-0209-8 (2019). [Google Scholar]
- 6.Vanden Wyngaert, K. et al. The effects of aerobic exercise on eGFR, blood pressure and VO2peak in patients with chronic kidney disease stages 3–4: a systematic review and meta-analysis. PLOS ONE. 13, e0203662. 10.1371/journal.pone.0203662 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang, L. et al. Exercise therapy improves eGFR, and reduces blood pressure and BMI in non-dialysis CKD patients: evidence from a meta-analysis. BMC Nephrol.20, 398. 10.1186/s12882-019-1586-5 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou, Y., Hellberg, M., Hellmark, T., Hoglund, P. & Clyne, N. Muscle mass and plasma myostatin after exercise training: a substudy of Renal Exercise (RENEXC)-a randomized controlled trial. Nephrol. Dial Transpl.10.1093/ndt/gfz210 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng, H. et al. Myokine mediated muscle-kidney crosstalk suppresses metabolic reprogramming and fibrosis in damaged kidneys. Nat. Commun.8, 1493. 10.1038/s41467-017-01646-6 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoshino, J. et al. A nationwide prospective cohort study of patients with advanced chronic kidney disease in Japan: the Reach-J CKD cohort study. Clin. Exp. Nephrol.22, 309–317. 10.1007/s10157-017-1453-2 (2018). [DOI] [PubMed] [Google Scholar]
- 11.Mariani, L. et al. The chronic kidney Disease outcomes and practice patterns study (CKDopps): rationale and methods. Am. J. Kidney Dis.68, 402–413 (2016). [DOI] [PubMed] [Google Scholar]
- 12.Hoshino, J. et al. Comparison of annual eGFR decline among primary kidney diseases in patients with CKD G3b-5: results from a REACH-J CKD cohort study. Clin. Exp. Nephrol.25, 902–910. 10.1007/s10157-021-02059-y (2021). [DOI] [PubMed] [Google Scholar]
- 13.Vega-López, S., Chavez, A., Farr, K. J. & Ainsworth, B. E. Validity and reliability of two brief physical activity questionnaires among spanish-speaking individuals of Mexican descent. BMC Res. Notes. 7, 29. 10.1186/1756-0500-7-29 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Topolski, T. D. et al. The rapid assessment of physical activity (RAPA) among older adults. Prev. Chronic Dis.3, A118 (2006). [PMC free article] [PubMed] [Google Scholar]
- 15.Hoshino, J. et al. Associations of Hemoglobin levels with health-related quality of life, physical activity, and clinical outcomes in persons with stage 3–5 nondialysis CKD. J. Ren. Nutr.10.1053/j.jrn.2019.11.003 (2020). [DOI] [PubMed] [Google Scholar]
- 16.Hirai, K., Ookawara, S. & Morishita, Y. Sarcopenia and physical inactivity in patients with chronic kidney disease. Nephro-urology Monthly. 8, e37443. 10.5812/numonthly.37443 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen, I. R. et al. Association of walking with survival and RRT among patients with CKD stages 3–5. Clin. J. Am. Soc. Nephrol.9, 1183–1189. 10.2215/cjn.09810913 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Imasawa, T. et al. Long-term effectiveness of a primary care practice facilitation program for chronic kidney disease management: an extended follow-up of a cluster-randomized FROM-J study. Nephrol. Dial Transpl.38, 158–166. 10.1093/ndt/gfac041 (2023). [DOI] [PubMed] [Google Scholar]
- 19.Oellgaard, J. et al. Intensified multifactorial intervention in type 2 diabetics with microalbuminuria leads to long-term renal benefits. Kidney Int.91, 982–988. 10.1016/j.kint.2016.11.023 (2017). [DOI] [PubMed] [Google Scholar]
- 20.Li, X. & Lindholm, B. The role of irisin in kidney diseases. Clin. Chim. Acta. 554, 117756. 10.1016/j.cca.2023.117756 (2024). [DOI] [PubMed] [Google Scholar]
- 21.Formigari, G. P. et al. Renal protection induced by physical exercise may be mediated by the irisin/AMPK axis in diabetic nephropathy. Sci. Rep.12, 9062. 10.1038/s41598-022-13054-y (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are not publicly available due to data sharing policy of the REACH-J study but are available from the corresponding author after the permission of steering committee of the REACH-J study on reasonable request.


