Abstract
Celiac disease (CD) has a significant impact on the quality of life for those affected, particularly in social settings. One major challenge for these individuals is dining out, as they must constantly avoid cross-contact with gluten, contend with a limited range of restaurant options, and often encounter unknowledgeable or misinformed staff. This study aims to evaluate the effectiveness of an educational program designed to enhance the understanding of CD and gluten-free diet (GFD) among future catering staff, thereby improving the social experiences of individuals with CD. A 3-h theoretical and practical session was developed for professional cookery students, focusing on predefined competencies and learning outcomes related to GFD. The study involved a sample of 100 students from Vitoria-Gasteiz, Spain. Following the intervention, students demonstrated increased knowledge regarding gluten content in foods and the application of GFD principles, including cross-contact prevention. However, during the practical activity, the gluten-free dish they prepared was not safe for CD patients to consume. Additionally, the students' perception of the difficulty in providing a GFD remained unchanged. Future sessions should emphasise the importance of interpreting food labels and practising cross-contact prevention. The strong interest in training hospitality students to promote social inclusion of CD patients highlights the need for more programmes to enhance their dining options and safety.
Keywords: Catering, Education, Students, celiac disease, Gluten-free diet, Cross-contact
Highlights
-
•
A training course can enhance students' knowledge about gluten content in foods.
-
•
Catering students find interpreting food labels challenging.
-
•
There should be a greater emphasis on the practical aspects to avoid cross-contact.
-
•
Improving the offer and safety of gluten-free options promotes social inclusion.
1. Introduction
Celiac disease (CD) is an autoimmune disorder that arises in genetically susceptible individuals who develop an immune response against gluten [1,2]. The symptoms of this disease are diverse and heterogeneous, and can be both gastrointestinal and extraintestinal. The most common gastrointestinal symptoms are diarrhoea, abdominal pain, bloating and flatulence. In contrast, extraintestinal symptoms are often related to inadequate micronutrient absorption and autoimmune status [[3], [4], [5]]. The prevalence of the disease is estimated to be around 1–2%, being more common in women than in men. Additionally, it is more frequently diagnosed in children than in adults [6,7].
The only treatment for the disease is a strict, lifelong gluten-free diet (GFD). Gluten is found in several cereals such as wheat, rye and barley, and therefore, in food products derived from those cereals [8,9]. Furthermore, gluten-containing foods are the basis of the diet in many regions, and therefore, the GFD involves a major lifestyle change and poses many challenges [[10], [11], [12], [13]]. Some of the challenges of the GFD include achieving a balanced diet, avoiding cross-contact and eating out [10,11,14,15].
The GFD must be nutritionally balanced, just like other diets. However, several studies have shown that the GFD is often low in carbohydrates and high in protein and saturated fats [11,[16], [17], [18]]. This may be attributed, on the one hand, to the difficulty of eliminating gluten-containingcereals from the diet, since cereals are part of a fundamental food group in a balanced diet. On the other hand, specific gluten-free products are often of poorer nutritional quality than their gluten-containing counterparts, which may contribute to dietary imbalances [[19], [20], [21], [22]]. In addition, if gluten-free cereals or pseudo cereals selection is not wide enough in the diet, it may also contribute to enhance the exposition to some undesirable components present in the most commonly consumed gluten-free cereals [23,24].
At the same time, one of the biggest challenges of the GFD is cross-contact. The term “cross-contact” is used when a gluten-free food comes into contact with gluten and this can be harmful to susceptible consumers. Cross-contact can occur in a number of situations such as: a) in the production of a food, when sharing facilities and equipment with gluten-containing foods, b) during cooking, both at home and in restaurants, and c) during consumption, when food is shared with other people [10,25]. Avoiding cross-contact is really important as such unconscious exposure to gluten has been linked to permanent damage to the intestinal mucosa [26].
In relation to the above, CD has a huge impact on the quality of life of people that suffer from it, especially on a social level. Various studies have shown that people with CD often feel different or excluded. This may be due to the difficulties of eating out, as they have to constantly avoid gluten cross-contact, and the choice of restaurants is often limited and staff is sometimes dismissive or uninformed [14,15,27,28].
In fact, several studies have highlighted the lack of knowledge of people working in the catering industry about CD and GFD [[29], [30], [31], [32], [33]]. Nevertheless, according to the study carried by Aziz et al., the awareness of CD among chefs has increased in recent years [34], and some studies have shown the presence of gluten in restaurants serving food under the gluten-free label [[35], [36], [37], [38]]. Likewise, a strategy to reduce cross-contact in restaurant kitchens could be to educate chefs about the GFD [15,39]. In addition, it would also be interesting to contribute to the availability of gluten-free options on restaurant menus [15,40,41].
Hence, the objective of this work is to present and evaluate the effectiveness of an educational programme that aims to increase the knowledge regarding CD and GFD of future catering staff in order to raise awareness and contribute to improving the social situation of people with CD.
2. Methods
2.1. Trial design
As mentioned, the objective of the study is to evaluate the effectiveness of an educational programme for students of professional cookery training. The programme consists of a 3-h theoretical-practical intervention aimed at improving knowledge of CD and GFD in future catering professionals. The programme was designed by University professors and researchers from the Gluten3s research group, and it was delivered by a research team member. The organization chart of the intervention can be seen in Table 1.
Table 1.
Organisation chart of the intervention.
| ACTIVITY | PARTICIPANTS | DURATION (minutes) |
|---|---|---|
| 1. Complete the PRE-questionnaire | Students, individually | 15 |
| 2. Opening presentation with a video. What is CD? What is gluten? What does a GFD look like? | A nutritionist, interacting with students | 20 |
| 3. Cooking session: cooking and tasting a gluten-free healthy recipe | Students, in groups | 60 |
| 4. Analysis of food handling during the cooking session through a checklist and discussion with peers: gluten cross-contact | Students, with the nutritionists' oral feedback | 20 |
| 5. Final presentation. Keys to the GFD: safe, balanced and socially inclusive | A nutritionist, interacting with students | 20 |
| 6. Resolution and discussion of a case study. How would you act if a person with CD came to your establishment to have lunch? | Students, with the nutritionists' oral feedback | 30 |
| 7. Complete the POST-questionnaire | Students, individually | 15 |
The activities carried out in the session were specifically designed according to previously defined competences and learning outcomes (depicted in Table 2), which, in turn, were classified according to their level of abstraction according to Bloom's taxonomy [42,43]. The students' evaluation was made in a continuous way through feedback during the session, but it was not graded. The intervention was evaluated using specifically designed questionnaires that were administered before (PRE-questionnaire) and immediately after (POST-questionnaire) the intervention (Appendix A). The students' perceptions of the activity was also measured by two questions.
Table 2.
Competences and learning outcomes of the activity.
| COMPETENCE | LEARNING OUTCOME (LO) | METHODOLOGY (Table 1 activity nº) |
|---|---|---|
| Promote the inclusion of people with CD by raising awareness about the disease among catering students. | LO1. She/He describes the symptoms and trigger of CD Bloom's level of abstraction: 2 (understand) |
-Opening presentation (2) |
| LO2. She/He describes gluten (its use when cooking) and identifies its location. Bloom's level of abstraction: 2 (understand) |
- Opening presentation (2) - Video (2) - Cooking session (3) |
|
| LO3.She/He knows what a GFD looks like: safe, balanced and inclusive. Bloom's level of abstraction: 3 (apply) |
- Opening presentation (2) - Cooking session (3) - Analysis of correct food handling (4) - Final presentation (5) - Case study (6) |
|
| LO4. She/He interprets the label of gluten-free products. Bloom's level of abstraction: 3 (apply) |
- Opening presentation (2) - Cooking session (3) |
|
| LO5. She/He adapts the service for celiac customers Bloom's level of abstraction: 5 (evaluate) |
- Cooking session (3) - Final presentation (5) - Case study (6) |
|
| Analyse the concept of cross-contact and how to prevent it. | LO6. She/He analyses cross-contact: avoidance and proper handling of foodstuffs Bloom's level of abstraction: 4 (analyse) |
- Opening presentation (2) - Cooking session (3) - Analysis of correct food handling (4) - Final presentation (5) - Case study (6) |
|
Analyse the concept of cross-contact and how to prevent it. AND Promote the inclusion of people with CD by raising awareness about the disease among catering students. |
LO7.She/He cooks a 100 % gluten-free menu/dish Bloom's level of abstraction: 3 (apply) |
- Opening presentation (2) - Cooking session (3) - Analysis of correct food handling (4) -Final presentation (5) -Case study (6) |
2.2. Participants
The study involved students from intermediate and higher professional training courses related to cookery, such as: cookery management, cookery and gastronomy, and catering services. The inclusion criteria for the study were to be enrolled in a vocational training course in Vitoria-Gasteiz city (northern Spain) and to be of legal age. All participants agreed to participate in the study by signing an informed consent form.
Based on findings from a preliminary pilot study and bibliography, it was projected that a sample size of 75 participants would be needed to achieve a statistical power of 80 % and a 5 % α error level to detect a small-medium effect size (Cohen's d of 0.30) for knowledge acquisition. Considering potential dropout rates observed in similar studies, the final sample size was increased by 20 % to a total of 90 students.
The research project received ethical approval from the University of the Basque Country, UPV/EHU, Ethics Committee for Human Research (M10/2020/081, July 01, 2020). Participation in the study posed no risks to the participants, except for the time they dedicated to it.
2.3. Statistical analysis
Statistical analysis was conducted using the SPSS software. Descriptive analysis was performed on sample's characteristics and response variables. The data distribution was found to be non-normal. To compare the PRE and POST questionnaires, Wilcoxon tests were used for quantitative responses. For multiple-choice questions (qualitative variables), McNemar test was used for binary variables, and Friedman and Marginal Homogeneity tests were performed for variables with more than two response options. Statistical significance was determined at a p-value of less than 0.05 for differences observed between the PRE and POST questionnaires (95 % confidence).
3. Results
3.1. Sample characteristics
Data was initially collected from 101 students from Gamarra Cooking School and Egibide Cooking School (Vitoria-Gasteiz, Spain) in the years 2022 and 2023. One of them had anomalous values in more than three answers to the questionnaire (Z-value>3) and was therefore eliminated from the study. From the final group of student (n = 100), 50 were female (50 %), 48 (48 %) were male and 2 (2 %) identified themselves otherwise.
None had CD. However, 79 (79 %) participants knew someone with CD, 19 (19 %) did not, and 2 (2 %) did not respond. Among those who knew a person with CD, for 4 (5 %) it was their partner or cohabitant, for 15 (19 %) it was a relative, for 33 (42 %) a friend and for 27 (34 %) an acquaintance without a close relationship.
3.2. Knowledge perception about celiac disease (LO1)
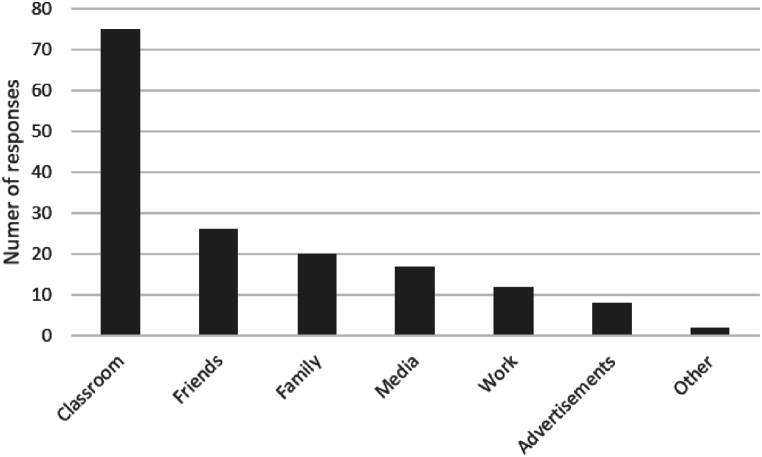
Prior to the intervention, participants reflected their knowledge of CD with 2.3 ± 0.9 points on a 0–4 scale. When asked where they learned about the disease, they reported learning about the disease through various ways: 75 % reported learning in the classroom, 26 % through friends, 20 % through family, 17 % through the media, 12 % at work, 8 % through advertising and 2 % through other means, e.g. the dietician (Fig. 1). After the intervention, their perception of knowledge increased significantly to 3.2 ± 0.6 (p < 0.001).
Fig. 1.
Number of responses of participants' sources of CD knowledge. It was possible to select more than one answer for each participant.
3.3. Knowledge about the GLUTEN content of foods and application to achieve a GFD (LO2 and LO3)
To assess whether the intervention served to increase their knowledge about gluten content in food and how to achieve a GFD, six questions were added to the questionnaire. The intervention increased their perception that they know more about what gluten is and where it is. Moreover, it was objectively measured whether their knowledge of the gluten content of cereals and foods in general had actually increased, and it had. In addition, they improved their knowledge about the position of gluten-containing foods in the food pyramid. They also improved their holistic view of the GFD, the importance of it being safe and nutritionally but also socially balanced. The results are shown in Table 3.
Table 3.
Questions to evaluate participants’ knowledge regarding gluten content of foods.
| Question | Type of response | PRE response Quantity (%) or Mean ± SD |
POST response Quantity (%) or Mean ± SD |
p |
|---|---|---|---|---|
| Do you know what gluten is? | Scale 0 (I do not know) −4 (I know it very well) | 2.67 ± 0.88 | 3.38 ± 0.62 | <0.001 |
| Do you know where gluten is found? | Scale 0 (I do not know) −4 (I know it very well) | 2.83 ± 0.93 | 3.35 ± 0.58 | <0.001 |
| From the following list of cereals, which ones contain gluten? | Number of correct responses (0–8) | 5.52 ± 1.46 | 6.82 ± 1.09 | <0.001 |
| Which of the following list of foods usually contain gluten? | Number of correct responses (0–9) | 8.49 ± 0.90 | 8.83 ± 0.59 | <0.001 |
| Where in the food pyramid are foods that are generally harmful to people with CD found? | Correct response | 45 | 68 | <0.001 |
| Incorrect response | 54 | 26 | ||
| No response | 1 | 6 | ||
| What should a GFD look like? | Number of correct responses (0–3) | 1.16 ± 0.77 | 1.41 ± 0.80 | <0.001 |
∗As n = 100, the number of responses and the percentage are equal, so only the percentages are described.
3.4. Food labels interpretation (LO4)
To evaluate the impact of the intervention on participants' ability to interpret food labelling, six inquiries were added to the questionnaire. The results indicated an improvement in participants' self-awareness of what to look for to determine if a food was gluten-free. However, most participants still believed that all gluten-free foods must be labelled as 'gluten-free,' which is incorrect. Additionally, there was significant uncertainty when participants analysed four specific labels. These findings are detailed in Table 4.
Table 4.
Questions to evaluate participants’ food labels interpretation.
| Question | Type of response | PRE response Quantity (%) or Mean ± SD |
POST response Quantity (%) or Mean ± SD |
p |
|---|---|---|---|---|
| Do you know what to look for on a label to find out if a food contains gluten or not? | Scale 0 (I do not know) −4 (I know it very well) | 3.04 ± 1.02 | 3.56 ± 0.54 | <0.001 |
| Do all gluten-free foods have to be labelled “gluten-free”? | No | 16 | 15 | <0.01 |
| Yes | 70 | 81 | ||
| I do not know | 14 | 2 | ||
| No response | 0 | 2 | ||
| Does this food contain gluten? (popcorn, with marked traces) | No | 28 | 35 | NS |
| Yes | 63 | 59 | ||
| I do not know | 8 | 3 | ||
| No response | 1 | 3 | ||
| Does this food contain gluten? (conventional biscuits) | No | 3 | 1 | NS |
| Yes | 89 | 96 | ||
| I do not know | 6 | 0 | ||
| No response | 2 | 3 | ||
| Does this food contain gluten? (chicken breast) | No | 73 | 83 | NS (0.095) |
| Yes | 10 | 9 | ||
| I do not know | 15 | 6 | ||
| No response | 2 | 2 | ||
| Does this food contain gluten? (specific gluten-free bread) | No | 63 | 69 | NS |
| Yes | 30 | 28 | ||
| I do not know | 6 | 1 | ||
| No response | 1 | 2 |
∗As n = 100, the number of responses and the percentage are equal, so only the percentages are described. NS: non significant.
3.5. Awareness regarding cross-contact (LO6)
In order to assess their awareness of cross-contact, they were presented with five statements with which they had to indicate their level of agreement. The results in Table 5 show how their awareness increased after the intervention, and therefore, they realised the importance of certain aspects, whereas some issues were clear since from the beginning.
Table 5.
Statements and participants’ agreement in avoiding possible cross-contact critical points.
| Statement | Type of response | PRE response Mean ± SD |
POST response Mean ± SD |
p |
|---|---|---|---|---|
| No special measures are required in the storage of raw materials to prepare a safe gluten-free dish | Scale 0 (disagree) – 4 (agree) | 0.75 ± 1.16 | 0.53 ± 0.99 | NS (0.066) |
| I must check, one by one, the labelling of each ingredient to ensure that it is gluten-free | Scale 0 (disagree) – 4 (agree) | 3.32 ± 1.04 | 3.42 ± 0.98 | NS |
| It is advisable to use dedicated pans and utensils | Scale 0 (disagree) – 4 (agree) | 3.02 ± 1.14 | 3.18 ± 1.20 | NS |
| Once plated, the dish should be covered until ready to serve | Scale 0 (disagree) – 4 (agree) | 2.74 ± 1.13 | 3.37 ± 1.04 | <0.001 |
| For cleaning those hard-to-clean kitchen surfaces and utensils it is recommended to use 60 % alcohol | Scale 0 (disagree) – 4 (agree) | 2.13 ± 0.91 | 3.38 ± 0.90 | <0.001 |
NS: non significant.
3.6. Perceived difficulty in providing a GLUTEN-free menu (LO5)
To determine their ability to adapt services for customers with CD, participants were asked to rate the difficulty of three specific situations. The results are shown in Table 6. The intervention did not alter their perception of the difficulty involved in cooking and serving a gluten-free menu, designing a balanced gluten-free menu, or maintaining a permanent gluten-free dish offering. They consistently rated these tasks as not very difficult to very easy, with average scores on the 0–4 scales.
Table 6.
Students’ perception in different activities related to providing a gluten-free menu.
| Perceived degree of difficulty of the following activities | Type of response | PRE response Mean ± SD |
POST response Mean ± SD |
p |
|---|---|---|---|---|
| Cooking and serving 100 % gluten-free in a safe way | Scale 0 (very easy) – 4 (very difficult) | 2.15 ± 0.89 | 2.09 ± 1.01 | NS |
| Designing a nutritionally balanced gluten-free menu | Scale 0 (very easy) – 4 (very difficult) | 2.23 ± 0.99 | 2.08 ± 1.06 | NS |
| Maintain a permanent supply of gluten-free dishes | Scale 0 (very easy) – 4 (very difficult) | 1.97 ± 0.96 | 1.88 ± 1.13 | NS |
NS: non significant.
3.7. Qualitative analysis of the cooking process of the GLUTEN-free recipe
The participants cooked a simple gluten-free recipe in groups. The recipe consisted of buckwheat crepes filled with avocado, quinoa, spiced chickpeas, grapes, cherry tomatoes and two sauces (a yoghurt sauce and one romesco sauce). The different preparations were divided into sub-groups, which was the usual way they cooked, and at the end, one group was in charge of assembling the dishes. The activity was repeated with the different students of the different courses.
All the final dishes of all the groups were not safe for consumption by people with CD for various reasons: a) they did not check the labelling of all ingredients and used spices that contained traces of gluten, b) they began without cleaning the utensils, despite being unaware of who had used them previously or if they had been properly cleaned, c) they used crepe makers that traditionally are not cleaned each time they are used so that the non-stick coating is not lost, d) while they were cooking, students from other grades, such as bakers, entered the kitchen with their clothes stained with flour (containing gluten) and leaving dust in the air, and/or e) most of them did not wash their hands before starting to cook.
As asked in the PRE and POST questionnaires, after the intervention they felt more able to prepare a 100 % gluten-free meal than before the intervention (learning outcome 7). Before the intervention they answered the question "Are you able to cook and serve a 100 % gluten-free meal safely?" with a mean of 2.74 ± 1.30 and after the intervention with a mean of 3.38 ± 0.71 on a scale 0 (I am not able) - 4 (I am very able), p < 0.001.
It is worth noting that although they considered themselves capable, when checking the mistakes that had been made during cooking, several students stated that "it was impossible to take everything into account" and that they would not serve their dish to a person with CD.
3.8. Participants' perception of the activity
Once the intervention was over, the participants were asked how interesting they found the activity, reflecting their interest with a mean of 3.6 ± 0.6 on a scale 0 to 4. They were also given the opportunity to highlight in an open question their opinion regarding the activity, and some of the responses were as follows: "I found it interesting to raise awareness and motivate cooking professionals to propose different varieties of gluten-free dishes and that celiac people can enjoy other options", "I liked the practical part and having experienced the carelessness that we can have even though we were aware that the dish we had to prepare should not have gluten" (referring to the fact that in the cooking there was involuntary cross contact), "What I liked most was learning to better empathize with celiacs", "What interested me most about the activity was learning that certain things I did, I did them wrong, and thus being able to correct them".
4. Discussion
As far as the authors are aware, there have not been many studies on educational programmes aimed at improving the knowledge of catering professionals and thus contributing to improving the social situation of people with CD [44]. In the UK, they developed an educational activity that aimed to improve the allergen knowledge of catering staff, and although knowledge improved, the authors stated that more evaluation of allergen training events should be done [45]. In another study in Spain, restaurant staff at two holiday resorts were trained in allergen awareness, increasing the number of allergen-free options in restaurants (48 % increase in gluten-free options) and also improving customer satisfaction [46]. In a similar, but larger-scale study by the same authors, they were able to increase allergen-free options in several restaurants and improve the handling of gluten-free foods [47].
Although not many studies have been done on the subject, several authors, especially those working on the social and psychological aspects of CD, reiterate the need for such activities [15,39,44]. In a systematic review by Young et al. they found that many restaurants and food service workers were interested in receiving allergen training, but few were actually trained. Therefore, this intervention could serve as a model for the development of training programmes for hospitality workers carried out by dietitian-nutritionists or similarly trained individuals [44].
In the previously mentioned UK study, they noted that the number of restaurant staff who attended the educational session was low, with only 48 % of the invited participating [45]. Interfering with students in the same school where they are being trained would therefore be a way to reach more professionals, also avoiding that the participants are only the most motivated people. Thus, the present study focuses on students from a variety of cookery-related degrees. Furthermore, according to the study by Schultz et al., catering students have a similar awareness of CD to chefs who are already working, although students are more aware of the need to prepare gluten-free food [30]. Emphasizing the importance of providing safe gluten-free options to culinary students from the beginning of their education could help to develop empathy and conscientiousness in their future careers.
The intervention was able to increase the students' perception of their knowledge about CD and gluten. Furthermore, it was observed that they did indeed increase their knowledge about the GFD, correctly identifying gluten-free foods and their position in the food pyramid. Their overall vision of what a GFD should look like (safe, balanced and socially inclusive) also improved, although there is still room for improvement. Eating out usually makes it more difficult to follow a GFD. Thus, it has been observed that having better access to gluten-free food in restaurants helps to follow the GFD properly [[48], [49], [50], [51]]. This highlights the responsibility of the catering industry in the welfare of the celiac community and, therefore, the importance of educational interventions in this sense. Hospitality workers need to be aware of the psychosocial impact of the disease on sufferers, as their knowledge and good practice in designing menu options and when cooking in the kitchen can help a lot to improve the quality of life of these people [29,52]. This awareness could lead to more varied and appetising gluten-free options in restaurants, which could help to improve the social situation of people with CD.
The intervention also increased their perception of their own ability to distinguish whether a food was gluten-free or not. However, it was found that they were not very good at identifying a gluten-free food according to its label. Interpreting labelling is complex, and this has also been expressed by people with CD [53,54], so it is really important to pay attention when reading it. In a study by Lessa et al., they found that 46.35 % of food handlers were not used to checking food labelling for allergens [52]. In another study by Ajala and colleagues, they found that the percentage was between 33 % and 37 % [55]. This highlights the need for future educational activities to be more specific and to place special emphasis on the importance of reading labelling and how to do it. Other studies focusing on food allergies have also pointed to the need for more comprehensive and specialised rather than basic food allergy education for hospitality workers [44,[56], [57], [58]].
Regarding cross-contact, the intervention increased their awareness of it, they realised the importance of certain aspects, such as the need to cover dishes if they are not going to be served immediately or the need to clean kitchen surfaces and utensils properly. For other aspects, such as the importance of paying attention to labelling, the special measures to be taken in the storage of raw materials, and the exclusive use of cooking utensils, awareness was already quite high. However, during the cooking process of a gluten-free recipe that took place during the activity, they were not able to avoid cross-contact, although the participants showed that they had a good knowledge of the practices to avoid it. It could be seen that even if the participants theoretically perceived that they had a good ability to distinguish the labelling of gluten-free foods, the vast majority did not put it into practice during the cooking process. Cross-contact is one of the reasons why people with CD still have damaged intestinal mucosa and have symptoms [26] and it is also one of their main concerns when eating out [14,59]. Although it was emphasised in the intervention that the GFD of these people had to be strict and that care had to be taken to ensure its total absence, it was only after they had practised in the kitchen and identified the mistakes made that they realised the true magnitude of the challenge of cooking gluten-free. Future hospitality professionals need to understand the importance of avoiding cross-contact and performing good handling procedures in the kitchen in order to serve secure dishes and avoid contaminating people with CD with gluten, as has been seen to happen in many restaurants [35,37].
It is noteworthy that even though their knowledge of some important aspects of cross-contact avoidance and the importance of checking labels increased, their perception of the difficulty in providing meals for these consumers did not. The students considered that giving a gluten-free menu was neither very difficult nor very easy, both before and after the intervention. Given that after the intervention they know more about the topic but do not perceive preparing a gluten-free menu as complicated, this could contribute to creating more gluten-free options in the restaurants where these students will work in the future. In a cross-sectional study by Khafagy et al. they found that 50.8 % of hospitality workers had the intention to increase gluten-free offerings in their restaurants, which suggests that catering staff recognize the need to provide adequate options for the population with CD. Even if intention is the first step, to execute this intention is also necessary to have the knowledge and the perception that it is achievable [31]. Nevertheless, the perceived difficulty of providing gluten-free food has to be commensurate with their knowledge. In fact, several studies on staffs' knowledge of food allergies have pointed to a worrying discrepancy between knowledge and their comfort level in serving safe food, where their confidence is high or very high and their knowledge is not so high [[60], [61], [62]], which could lead to unsafe situations.
Finally, it is interesting to point out that when participants were able to give their perception of the activity in an open-ended question, they indicated that they realised that they were careless and unconscious when cooking. They thought the activity was motivating to deal with gluten-free cooking. Moreover, it should be noted that they highlighted that the intervention helped them to be more empathetic towards people with CD. Overall, the programme can be considered a firm step towards the inclusion of gluten-avoiding people.
To comment on some of the limitations of the study, it should be highlighted that it was only carried out in the city of Vitoria-Gasteiz. It could be interesting to study its effectiveness in other cities and even countries. In addition, the programme has not been evaluated in the long term, in fact, it was only evaluated immediately after the end of the programme, so it would be enriching to evaluate it in future studies.
5. Conclusion
The educational activity was able to increase the students' knowledge of the gluten content of foods and its application to achieve a GFD. It also increased their awareness of cross-contact. In future activities, special emphasis should be placed on the interpretation of the labelling and its importance, as well as on the practice of avoiding cross-contact. It is important to point out the great interest in training hospitality students to improve the offer and the safety of these diners as well as their inclusion in society. More programs in this direction should be put in place.
CRediT authorship contribution statement
Maialen Vázquez-Polo: Writing – original draft, Investigation, Formal analysis. Virginia Navarro: Writing – original draft, Investigation, Funding acquisition, Formal analysis, Conceptualization. Gesala Perez-Junkera: Writing – review & editing, Investigation. Arrate Lasa: Writing – review & editing, Funding acquisition, Conceptualization. Idoia Larretxi: Writing – review & editing, Conceptualization. Jonatan Miranda: Writing – review & editing, Funding acquisition. Jon Esparta: Writing – review & editing, Investigation. Itziar Churruca: Writing – original draft, Investigation, Funding acquisition, Formal analysis, Conceptualization.
Ethics statement
The intervention was performed in accordance with the Declaration of Helsinki. The study was approved by the University of the Basque Country, UPV/EHU, Ethics Committee for Human Research (M10/2020/081, July 01, 2020). Participation in the study did not involve any risk for the participant; the only associated risk was the use of their time. Informed consent was obtained from all subjects involved in the study prior to the start of the study.
Data availability statement
All data generated or analysed during this study are included in this published article.
Funding
Maialen Vázquez-Polo and Gesala Perez-Junkera are fellows of the University of the Basque Country, UPV/EHU, and the Basque Government, respectively. The GLUTEN3S research group is supported by a grant (GIU18/78, GIU21/053) from the UPV/EHU, and it is recognised by the Basque Government (IT-1419-19). This research was supported by two grants from the University of the Basque Country, UPV/EHU, (University-Society US20/16 and US22/22). Funding sources had no involvement in the study design, collection, analysis nor interpretation of data.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank the teachers of the schools and all the students who participated in the study. We would also like to thank the whole Gluten3S team for their support.
Abbreviations
- celiac disease
(CD)
- gluten-free diet
(GFD)
- learning outcome
(LO)
Appendix A. Questionnaire to evaluate the intervention
| Competence | Learning Outcome (LO) | Question to evaluate the intervention | When completed | Response |
|---|---|---|---|---|
| Promote the inclusion of people with CD by raising awareness about the disease among catering students | LO1 | How much do you know about CD? | PRE/POST | Scale 0 (nothing) – 4 (much) |
| LO2 | Do you know what gluten is? | PRE/POST | Scale 0 (nothing) – 4 (much) | |
| Do you know where gluten is found? | PRE/POST | Scale 0 (nothing) – 4 (much) | ||
| From the following list of cereals, which ones contain gluten? | PRE/POST | Multiple choice: Rice, wheat, maize, barley, rye, buckwheat, spelt, quinoa |
||
| Which of the following list of foods usually contain gluten? | PRE/POST | Multiple choice: Potato, milk, pasta, cake, fresh fish and meat, sugar, olive oil, banana, bread |
||
| LO3 | Where in the food pyramid are foods that are generally harmful to people with CD found? | PRE/POST | Multiple choice: - At the base of the food pyramid - At the top of the food pyramid - In the middle of the food pyramid - I do not know |
|
| What should a GFD look like? | PRE/POST | Multiple choice: - Grain free - Nutritionally balanced - Safe, gluten free - Socially inclusive - Safe, lactose free - I do not know |
||
| LO4 | Do you know what to look for on a label to find out if a food contains gluten or not? | PRE/POST | Scale 0 (nothing) – 4 (much) | |
| Do all gluten-free foods have to be labelled "gluten-free"? | PRE/POST | Yes/No/I do not know | ||
| Does this food contain gluten? (4 pictures) | PRE/POST | Yes/No/I do not know | ||
| LO5 | Indicate the degree of difficulty of these activities: | PRE/POST | Scale 0 (very difficult) – 4 (very easy) | |
| - Cooking and serving 100 % gluten-free in a safe way | ||||
| - Designing a nutritionally balanced gluten-free menu | ||||
| - Maintain a permanent supply of gluten-free dishes | ||||
| Analyse the concept of cross-contact and how to prevent it. | LO6 | Indicate your degree of agreement with the following statements: | PRE/POST | Scale 0 (strongly disagree) – 4 (strongly agree) |
| - No special measures are required in the storage of raw materials to prepare a safe gluten-free dish. | ||||
| - I must check, one by one, the labelling of each ingredient to ensure that it is gluten-free. | ||||
| - It is advisable to use dedicated pans and utensils. | ||||
| - Once plated, the dish should be covered until ready to serve. | ||||
| -For cleaning those hard-to-clean kitchen surfaces and utensils it is recommended to use 60 % alcohol. | ||||
| Analyse the concept of cross-contact and how to prevent it. AND Promote the inclusion of people with CD by raising awareness about the disease among catering students |
LO7 | Are you able to cook and serve a 100 % gluten-free meal safely? | PRE/POST | Scale 0 (not able to) – 4 (very able to) |
References
- 1.Lebwohl B., Sanders D.S., Green P.H.R. Coeliac disease. Lancet. 2018;391:70–81. doi: 10.1016/S0140-6736(17)31796-8. [DOI] [PubMed] [Google Scholar]
- 2.Husby S., Koletzko S., Korponay-Szabó I.R., Mearin M.L., Phillips A., Shamir R., et al. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2012;54:136–160. doi: 10.1097/MPG.0b013e31821a23d0. [DOI] [PubMed] [Google Scholar]
- 3.Ludvigsson J.F., Leffler D.A., Bai J.C., Biagi F., Fasano A., Green P.H., et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62:43–52. doi: 10.1136/gutjnl-2011-301346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sainsbury A., Sanders D.S., Ford A.C. Prevalence of irritable bowel syndrome-type symptoms in patients with celiac disease: a meta-analysis. Clin. Gastroenterol. Hepatol. 2013;11 doi: 10.1016/j.cgh.2012.11.033. 359-65, e1. [DOI] [PubMed] [Google Scholar]
- 5.Jericho H., Sansotta N., Guandalini S. Extraintestinal manifestations of celiac disease: effectiveness of the gluten-free diet. J. Pediatr. Gastroenterol. Nutr. 2017;65:75–79. doi: 10.1097/MPG.0000000000001420. [DOI] [PubMed] [Google Scholar]
- 6.Gujral N., Freeman H.J., Thomson A.B.R. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J. Gastroenterol. 2012;18:6036–6059. doi: 10.3748/wjg.v18.i42.6036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh P., Arora A., Strand T.A., Leffler D.A., Catassi C., Green P.H., et al. Global prevalence of celiac disease: systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2018;16 doi: 10.1016/j.cgh.2017.06.037. 823-836, e2. [DOI] [PubMed] [Google Scholar]
- 8.Mulder C.J., van Wanrooij R.L., Bakker S.F., Wierdsma N., Bouma G. Gluten-free diet in gluten-related disorders. Dig. Dis. 2013;31:57–62. doi: 10.1159/000347180. [DOI] [PubMed] [Google Scholar]
- 9.Francavilla R., Cristofori F., Stella M., Borrelli G., Naspi G., Castellaneta S. Treatment of celiac disease: from gluten-free diet to novel therapies. Minerva Pediatr. 2014;66:501–516. [PubMed] [Google Scholar]
- 10.Aljada B., Zohni A., El-Matary W. The gluten-free diet for celiac disease and beyond. Nutrients. 2021;13 doi: 10.3390/nu13113993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cardo A., Churruca I., Lasa A., Navarro V., Vázquez-Polo M., Perez-Junkera G G., et al. Nutritional imbalances in adult celiac patients following a gluten-free diet. Nutrients. 2021;13:2877. doi: 10.3390/nu13082877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valitutti F., Trovato C.M., Montuori M., Cucchiara S. Pediatric celiac disease: follow-up in the spotlight. Adv. Nutr. 2017;8:356–361. doi: 10.3945/an.116.013292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacCulloch K., Rashid M. Factors affecting adherence to a gluten-free diet in children with celiac disease. Paediatr. Child Health. 2014;19:305–309. doi: 10.1093/pch/19.6.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vázquez-Polo M., Navarro V., Larretxi I., Perez-Junkera G., Lasa A., Matias S., et al. Uncovering the concerns and needs of individuals with celiac disease: a cross-sectional study. Nutrients. 2023;15:3681. doi: 10.3390/nu15173681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh P., Dennis M. Eliminating dietary gluten: don't Be a "glutton for punishment". Dig. Dis. Sci. 2018;63:1374–1375. doi: 10.1007/s10620-018-5010-y. [DOI] [PubMed] [Google Scholar]
- 16.Churruca I., Miranda J., Lasa A., Bustamante M., Larretxi I., Simon E. Analysis of body composition and food habits of Spanish celiac women. Nutrients. 2015;7:5515–5531. doi: 10.3390/nu7075234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.González T., Larretxi I., Vitoria J.C., Castaño L., Simón E., Churruca I., et al. Celiac male's gluten-free diet profile: comparison to that of the control population and celiac women. Nutrients. 2018;10:1713. doi: 10.3390/nu10111713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jamieson J.A., Neufeld A. Food sources of energy and nutrients among Canadian adults following a gluten-free diet. PeerJ. 2020;8 doi: 10.7717/peerj.9590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miranda J., Lasa A., Bustamante M.A., Churruca I., Simon E. Nutritional differences between a gluten-free diet and a diet containing equivalent products with gluten. Plant Foods Hum. Nutr. 2014;69:182–187. doi: 10.1007/s11130-014-0410-4. [DOI] [PubMed] [Google Scholar]
- 20.Larretxi I., Simon E., Benjumea L., Miranda J., Bustamante M.A., Lasa A., et al. Gluten-free-rendered products contribute to imbalanced diets in children and adolescents with celiac disease. Eur. J. Nutr. 2019;58:775–783. doi: 10.1007/s00394-018-1685-2. [DOI] [PubMed] [Google Scholar]
- 21.Fry L., Madden A.M., Fallaize R. An investigation into the nutritional composition and cost of gluten-free versus regular food products in the UK. J. Hum. Nutr. Diet. 2018;31:108–120. doi: 10.1111/jhn.12502. [DOI] [PubMed] [Google Scholar]
- 22.Melini V., Melini F. Gluten-free diet: gaps and needs for a healthier diet. Nutrients. 2019;11 doi: 10.3390/nu11010170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brera C., Debegnach F., De Santis B., Di Ianni S., Gregori E., Neuhold S., et al. Exposure assessment to mycotoxins in gluten-free diet for celiac patients. Food Chem. Toxicol. 2014;69:13–17. doi: 10.1016/j.fct.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 24.Raehsler S.L., Choung R.S., Marietta E.V., Murray J.A. Accumulation of heavy metals in people on a gluten-free diet. Clin. Gastroenterol. Hepatol. 2018;16:244–251. doi: 10.1016/j.cgh.2017.01.034. [DOI] [PubMed] [Google Scholar]
- 25.Bascuñán K.A., Vespa M.C., Araya M. Celiac disease: understanding the gluten-free diet. Eur. J. Nutr. 2017;56:449–459. doi: 10.1007/s00394-016-1238-5. [DOI] [PubMed] [Google Scholar]
- 26.Rubio-Tapia A., Rahim M.W., See J.A., Lahr B.D., Wu T.T., Murray J.A. Mucosal recovery and mortality in adults with celiac disease after treatment with a gluten-free diet. Am. J. Gastroenterol. 2010;105:1412–1420. doi: 10.1038/ajg.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolf R.L., Lebwohl B., Lee A.R., Zybert P., Reilly N.R., Cadenhead J., et al. Hypervigilance to a gluten-free diet and decreased quality of life in teenagers and adults with celiac disease. Dig. Dis. Sci. 2018;63:1438–1448. doi: 10.1007/s10620-018-4936-4. [DOI] [PubMed] [Google Scholar]
- 28.See J.A., Kaukinen K., Makharia G.K., Gibson P.R., Murray J.A. Practical insights into gluten-free diets. Nat. Rev. Gastroenterol. Hepatol. 2015;12:580–591. doi: 10.1038/nrgastro.2015.156. [DOI] [PubMed] [Google Scholar]
- 29.Karajeh M.A., Hurlstone D.P., Patel T.M., Sanders D.S. Chefs' knowledge of coeliac disease (compared to the public): a questionnaire survey from the United Kingdom. Clin Nutr. 2005;24:206–210. doi: 10.1016/j.clnu.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Schultz M., Shin S., Coppell K.J. Awareness of coeliac disease among chefs and cooks depends on the level and place of training. Asia Pac. J. Clin. Nutr. 2017;26:719–724. doi: 10.6133/apjcn.072016.03. [DOI] [PubMed] [Google Scholar]
- 31.Khafagy A.A., Qari W.K., Filimban S.S., Bahalaq A.M., Bulkhi A.A. A cross-sectional study of celiac disease awareness in the food industry in the western region of Saudi arabia. Cureus. 2022;14 doi: 10.7759/cureus.25613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simpson S., Lebwohl B., Lewis S.K., Tennyson C.A., Sanders D.S., Green P.H. vol. 6. e-SPEN; 2011. pp. e227–e231. (Awareness of Gluten-Related Disorders: A Survey of the General Public, Chefs and Patients). [Google Scholar]
- 33.Dupuis R., Meisel Z., Grande D., Strupp E., Kounaves S., Graves A., et al. Food allergy management among restaurant workers in a large U.S. city. Food Control. 2016;63:147–157. [Google Scholar]
- 34.Aziz I., Karajeh M.A., Zilkha J., Tubman E., Fowles C., Sanders D.S. Change in awareness of gluten-related disorders among chefs and the general public in the UK: a 10-year follow-up study. Eur. J. Gastroenterol. Hepatol. 2014;26:1228–1233. doi: 10.1097/MEG.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 35.Lerner B.A., Phan Vo L.T., Yates S., Rundle A.G., Green P.H.R., Lebwohl B. Detection of gluten in gluten-free labeled restaurant food: analysis of crowd-sourced data. Am. J. Gastroenterol. 2019;114:792–797. doi: 10.14309/ajg.0000000000000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McIntosh J., Flanagan A., Madden N., Mulcahy M., Dargan L., Walker M., et al. vol. 46. 2011. pp. 1569–1574. (Awareness of Coeliac Disease and the Gluten Status of ‘gluten-free’ Food Obtained on Request in Catering Outlets in Ireland). [Google Scholar]
- 37.Falcomer A.L., Santos Araújo L., Farage P., Santos Monteiro J., Yoshio Nakano E., Puppin Zandonadi R. Gluten contamination in food services and industry: a systematic review. Crit. Rev. Food Sci. Nutr. 2020;60:479–493. doi: 10.1080/10408398.2018.1541864. [DOI] [PubMed] [Google Scholar]
- 38.Oliveira O.M.V., Zandonadi R.P., Gandolfi L., de Almeida R.C., Almeida L.M., Pratesi R. Evaluation of the presence of gluten in beans served at self-service restaurants: a problem for celiac disease carriers. J. Culin. Sci. Technol. 2014;12:22–33. [Google Scholar]
- 39.Bianchi D.M., Maurella C., Gallina S., Gorrasi I.S.R., Caramelli M., Decastelli L. Analysis of gluten content in gluten-free pizza from certified take-away pizza restaurants. Foods. 2018;7 doi: 10.3390/foods7110180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mandracchia F., Llauradó E., Valls R.M., Tarro L., Solà R. Evaluating mediterranean diet-adherent, healthy and allergen-free meals offered in tarragona province restaurants (Catalonia, Spain): a cross-sectional study. Nutrients. 2021;13 doi: 10.3390/nu13072464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sálcová D., Aleš H. Gluten-free food – the influence of selected qualitative characteristics on consumer decision making of coeliacs in hospitality establishments. Czech J. Food Sci. 2015:513–517. [Google Scholar]
- 42.Bloom B., Krathwohl D.R. 1956. Taxonomy of Educational Objetives: the Classification of Educational Goals, by a Committee of College and University Examiners. Handbook I: Cognitive Domain, NY, Longmans, Green. [Google Scholar]
- 43.Anderson L. SAGE publications; Washington: 2014. Taxonomy of Educational Objetives. [Google Scholar]
- 44.Young I., Thaivalappil A. A systematic review and meta-regression of the knowledge, practices, and training of restaurant and food service personnel toward food allergies and Celiac disease. PLoS One. 2018;13 doi: 10.1371/journal.pone.0203496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bailey S., Billmeier Kindratt T., Smith H., Reading D. Food allergy training event for restaurant staff; a pilot evaluation. Clin. Transl. Allergy. 2014;4:26. doi: 10.1186/2045-7022-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tarro L., Aceves-Martins M., Tiñena Y., Parisi J.L., Blasi X., Giralt M., et al. Restaurant-based intervention to facilitate healthy eating choices and the identification of allergenic foods at a family-oriented resort and a campground. BMC Publ. Health. 2017;17:393. doi: 10.1186/s12889-017-4333-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tarro L., Mandracchia F., Queral J., Besora-Moreno M., Vilanova N., Valls R.M., et al. Impact of an intervention on healthy offerings and allergenic food management in restaurants: a parallel randomized controlled study. Nutrients. 2013;15:4869. doi: 10.3390/nu15234869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abu-Janb N., Jaana M. Facilitators and barriers to adherence to gluten-free diet among adults with celiac disease: a systematic review. J. Hum. Nutr. Diet. 2020;33:786–810. doi: 10.1111/jhn.12754. [DOI] [PubMed] [Google Scholar]
- 49.Zarkadas M., Cranney A., Case S., Molloy M., Switzer C., Graham I.D., et al. The impact of a gluten-free diet on adults with coeliac disease: results of a national survey. J. Hum. Nutr. Diet. 2006;19:41–49. doi: 10.1111/j.1365-277X.2006.00659.x. [DOI] [PubMed] [Google Scholar]
- 50.Barratt S.M., Leeds J.S., Sanders D.S. Quality of life in Coeliac Disease is determined by perceived degree of difficulty adhering to a gluten-free diet, not the level of dietary adherence ultimately achieved. J Gastrointestin Liver Dis. 2011;20:241–245. [PubMed] [Google Scholar]
- 51.Lee A.R., Ng D.L., Diamond B., Ciaccio E.J., Green P.H.R. Living with coeliac disease: survey results from the USA. J. Hum. Nutr. Diet. 2012;25:233–238. doi: 10.1111/j.1365-277X.2012.01236.x. [DOI] [PubMed] [Google Scholar]
- 52.Lessa K., Lozano M., Esteve Más M.J., Frígola Cánoves A. Food allergy knowledge, attitudes and practices: a pilot study of the general public and food handlers. European Journal of Nutrition & Food Safety. 2016;6:58–64. [Google Scholar]
- 53.Gutowski E.D., Weiten D., Green K.H., Rigaux L.N., Bernstein C.N., Graff L.A., et al. Can individuals with celiac disease identify gluten-free foods correctly? Clin Nutr ESPEN. 2020;36:82–90. doi: 10.1016/j.clnesp.2020.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Muhammad H., Reeves S., Ishaq S., Mayberry J., Jeanes Y.M. Adherence to a gluten free diet is associated with receiving gluten free foods on prescription and understanding food labelling. Nutrients. 2017;9:705. doi: 10.3390/nu9070705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ajala A.R., Cruz A.G., Faria J.a.F., Walter E.H.M., Granato D., Ana A.S.S. Food allergens: knowledge and practices of food handlers in restaurants. Food Control. 2010;21:1318–1321. [Google Scholar]
- 56.Radke T.J., Brown L.G., Faw B., Hedeen N., Matis B., Perez P., et al. Restaurant food allergy practices — six selected sites, United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2017;66:404–407. doi: 10.15585/mmwr.mm6615a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee Y.M., Xu H. Food allergy knowledge, attitudes, and preparedness among restaurant managerial staff. J. Foodserv. Bus. Res. 2015;18:454–469. [Google Scholar]
- 58.Shafie A.A., Azman A.W. Assessment of knowledge, attitude and practice of food allergies among food handlers in the state of Penang, Malaysia. Publ. Health. 2015;129:1278–1284. doi: 10.1016/j.puhe.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 59.Wieser H., Segura V., Ruiz-Carnicer A., Sousa C., Comino I. Food safety and cross-contamination of gluten-free products: a narrative review. Nutrients. 2021;13 doi: 10.3390/nu13072244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bailey S., Albardiaz R., Frew A.J., Smith H. Restaurant staff's knowledge of anaphylaxis and dietary care of people with allergies. Clin. Exp. Allergy. 2011;41:713–717. doi: 10.1111/j.1365-2222.2011.03748.x. [DOI] [PubMed] [Google Scholar]
- 61.Ahuja R., Sicherer S.H. Food-allergy management from the perspective of restaurant and food establishment personnel. Ann. Allergy Asthma Immunol. 2007;98:344–348. doi: 10.1016/S1081-1206(10)60880-0. [DOI] [PubMed] [Google Scholar]
- 62.Wham C.A., Sharma K.M. Knowledge of café and restaurant managers to provide a safe meal to food allergic consumers. Nutr. Diet. 2014;71:265. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.