Abstract
Background
The Coronavirus disease 2019 (COVID-19) pandemic led to healthcare system changes aimed at minimizing disease transmission that impacted experiences with obstetric healthcare.
Objective
To explore experiences of clinicians providing obstetric care during the COVID-19 pandemic.
Study Design
Qualitative, in-depth, semi-structured interviews were conducted with five nurse practitioners and 16 obstetrical physicians providing a mix of outpatient and inpatient obstetric care during the COVID-19 pandemic in a mid-sized, Midwestern city in the United States. Interviews elucidated challenges and facilitators of obstetric care provision and vaccination of pregnant patients against COVID-19 during the pandemic. Transcripts were coded inductively then deductively using the Health Equity Implementation Framework (HEIF), which integrates a disparities framework and implementation framework to highlight multilevel factors that influence obstetric care. Thematic analysis was conducted, and thematic saturation was reached.
Results
We interviewed 21 clinicians. Clinicians recounted personal challenges such as social isolation and burnout that could be countered by social support. Challenges within the clinical encounter included implementation of infection mitigation efforts, vaccine counseling, and limitations of telehealth. However, when successfully implemented, telehealth facilitated care and circumvented barriers. Clinicians cited challenges at the healthcare system level such as rapidly evolving knowledge and recommendations, restrictive visitor policies, personnel shortage, and inadequate institutional resources to support pandemic-related stressors. However, interdisciplinary care and guidelines available for clinicians facilitated care. Clinicians reported that challenges at the societal level included financial strain, lack of childcare, medical mistrust, politicization of medicine, misinformation, and racism. Societal-level facilitators included insurance access, community outreach, positive policy changes, and fostering trust in medicine.
Conclusion
The pandemic produced unique stressors and exacerbated existing challenges for clinicians providing obstetric care. Applying the HEIF to the findings emphasizes the influence of societal factors on all other levels. Identified facilitators can inform interventions to address stressors in obstetric care that have resulted from the changed sociopolitical landscape of the pandemic.
Key words: challenges, COVID-19 vaccination, facilitators, health equity, misinformation, mistrust, obstetric care provision, qualitative methods, social determinants of health, telehealth
AJOG Global Reports at a Glance.
Why was this study conducted?
The Coronavirus disease 2019 (COVID-19) pandemic changed health systems by exacerbating existing barriers and introducing new obstetric care provision challenges. This study aimed to highlight the experiences of obstetric clinicians practicing in the Midwestern United States during the pandemic using semi-structured interviews.
Key findings
Obstetric clinicians named multiple challenges during the pandemic that spanned the clinical encounter, healthcare system, and societal levels but additionally identified multi-level facilitators that addressed stressors and supported their ability to provide higher-quality obstetric care.
What does this add to what is known?
Unique stressors during the COVID-19 pandemic are identified for obstetric care, and facilitators can be used to inform interventions to improve care delivery.
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic drastically changed obstetric care delivery.1 Whereas most nonemergent medical care paused during the pandemic, obstetric care continued without reprieve. To minimize disease transmission, in-person prenatal visits were minimized, telehealth was integrated, and visitor restrictions were enforced.2, 3, 4, 5, 6, 7, 8, 9 While prior studies have assessed pandemic-related barriers and facilitators related to patient experiences in obstetrics, few studies explored obstetric clinicians’ experiences.4,8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 Among studies examining clinician perspectives, most have focused on challenges of telehealth and reduced prenatal care schedules,4,12,18,19 rather than exploring sociopolitical contexts in which clinicians practice. Particularly, little work has been done within the urban American Midwest, which houses its own unique political, social, and historical context. Redlining, a practice employed in the 1930s labeling Black neighborhoods as “hazardous” resulting in these areas receiving minimal federal mortgage assistance, is one example of the long history of structural racism through slavery and segregation in this region that has left behind a legacy of health disparities between neighboring zip codes.20
The present study is guided by the Health Equity Implementation Framework (HEIF), an equity-centered determinant implementation schematic, to examine multilevel domains of challenges and facilitators.21 We sought to explore the experiences of clinicians providing obstetric care in the Midwest during the COVID-19 pandemic to inform future care provision interventions.
Materials and methods
Participants were convenience-sampled from a list of obstetric nurse practitioners and physicians from academic, private, and federally qualified health center (FQHC) practices who deliver at a tertiary care center in a mid-sized, Midwestern city and were clinically active during the pandemic; students and residents were excluded. Those meeting criteria were recruited through email, verbally consented, and compensated with a $25 gift card. Sampling continued until thematic saturation, which was ascertained when no new codes emerged after analysis.22 The Washington University institutional review board approved this study (#202012075).
Demographics were surveyed. We created the interview guide based on the HEIF to encompass COVID-19 testing and vaccination and obstetric care provision during the pandemic. The interview guide was iteratively reassessed for further exploration of themes and revised accordingly after team discussion. After conducting seven interviews, we included more questions on clinician burnout, sociopolitical factors influencing care, medical mistrust, and telehealth (Appendix A, Table 1).
Table 1.
Example interview questions and/or probes based on the Health Equity Implementation Framework (HEIF)
| Personal factors | Could you talk about any personal challenges you have experienced when providing care, such as feeling burned out or overwhelmed? |
| Clinical encounter | How do you counsel patients on COVID-19 vaccination during pregnancy? What makes counseling sessions more successful? What have you learned from counseling sessions? |
| Healthcare system factors | Are there are certain systems in place that make it easier or more difficult for you to provide care or for patients to receive care during the pandemic? |
| Societal factors | How has the current social and political environment during the pandemic affected your ability to provide care as well as patients’ ability to access care? |
Sinha. Experiences of Midwestern obstetric clinicians. AJOG Glob Rep 2024.
Data collection occurred from May 2022 to May 2023. Twenty- to 50-minute interviews were conducted virtually or in-person by trained team members (DS, AS), recorded, transcribed, uploaded to NVivo 12 (QRS International, Burlington, MA), and deidentified. A codebook of themes, codes, definitions, and example quotes was constructed. The primary coder (DS) developed granular codes inductively, organized into overarching parent codes based on the HEIF. All transcripts were split between two secondary coders (AB, AN), double-coded, and compared to the primary coding; discrepancies were addressed and resolved through discussion. Coded data were analyzed using thematic analysis.23 We utilized the Consolidated Criteria for Reporting Qualitative Research (Appendix B).24
Our interdisciplinary team engaged in ongoing reflexive discussion on how our political beliefs, privilege, identities, roles in healthcare/academia, and pre-existing relationships with participants shape our biases toward data collection, interpretation, and analysis.
Results
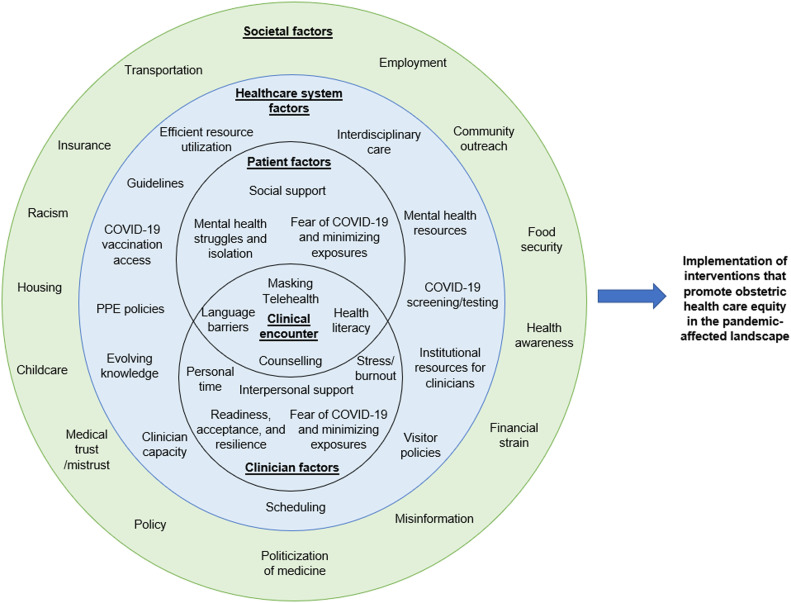
Thirty-three clinicians were eligible and contacted, and we consented and interviewed 21 (Table 2). The majority identified as women (90.5%), White (90.5%), physicians (71.4%), with ≤10 years in post-training practice (76.2%), in an academic setting (76.2%). Personal, clinical encounter, healthcare system, and societal factors derived from the HEIF were organized into challenges and facilitators of obstetric care during the pandemic (Figure).21 Exemplary quotes are presented (Appendixes C and D).
Table 2.
Participant demographics (n=21)
| Demographics | n (%)a |
|---|---|
| Gender | |
| Woman | 19 (90.5%) |
| Man | 1 (4.8%) |
| Nonbinary | 0 (0.0%) |
| Transgender woman | 0 (0.0%) |
| Transgender man | 0 (0.0%) |
| Other | 0 (0.0%) |
| N/A | 1 (4.8%) |
| Race and/or ethnicityb | |
| American Indian or Alaskan Native | 0 (0.0%) |
| Asian or Pacific Islander | 0 (0.0%) |
| Black or African American | 1 (4.8%) |
| Hispanic or Latino/a | 0 (0.0%) |
| Middle Eastern or North African | 0 (0.0%) |
| White | 19 (90.5%) |
| None of the above | 0 (0.0%) |
| More than one race | 0 (0.0%) |
| N/A | 1 (4.8%) |
| Years in practice | |
| 0–10 y | 16 (76.2%) |
| >10 y | 4 (19.0%) |
| N/A | 1 (4.8%) |
| Practice setting | |
| Academic practice | 16 (76.2%) |
| FQHC | 2 (9.5%) |
| Private practice | 2 (9.5%) |
| Other | 0 (0.0%) |
| N/A | 1 (4.8%) |
| Clinician role | |
| NP | 5 (23.8%) |
| OB/GYN physician | 15 (71.4%) |
| Other | 0 (0.0%) |
| N/A | 1 (4.8%) |
FQHC, federally qualified health center; N/A, not available, indicating nonresponse; NP, nurse practitioner.
One participant did not complete the demographic survey
Race and/or ethnicity was surveyed to further contextualize experiences. It was self-reported, and categories were created by the authors.
Sinha. Experiences of Midwestern obstetric clinicians. AJOG Glob Rep 2024.
Figure.
Adaptation of the Health Equity Implementation Framework21
Societal, healthcare system, clinical encounter, and personal factors (composed of patient and clinician factors) affecting obstetric care identified by participants are displayed, and societal factors create the environment in which the other levels exist.
The HEIF can be used for consideration of relevant factors for the future design and implementation of interventions to increase obstetric care equity.
PPE, personal protective equipment.
Sinha. Experiences of Midwestern obstetric clinicians. AJOG Glob Rep 2024.
Personal factors
Major challenges included social isolation and absence of support (Appendix C.1). For example, a participant's nonmedical spouse had difficulty understanding the unique stressors placed upon clinicians. Childcare became an enormous burden after school closures. Clinicians reported increased mental health needs among patients, requiring them to take on roles of a “counselor and a therapist and a friend” (participant 5 [P5]). Constantly changing processes resulted in “decision fatigue” (P17). Many clinicians bore witness to severe COVID-19 morbidity, resulting in worry about their families, while also experiencing “vitriol” (P21) toward healthcare workers. Unsurprisingly, these increased demands resulted in stress and burnout:
“…the sort of mental exhaustion and the mental stress of knowing you…missed two years of your kids’ life…is an exhaustion and a grief…a lot of us still feel some grief over that and missing years with aging family…” (P11)
Despite these challenges, social and mental health support was available. Clinicians perceived that virtual support groups and flexibility working from home improved access to social supports for patients, especially postpartum. For clinicians, covering one another's shifts and family providing childcare allowed time to work longer hours. Clinicians attempted to prioritize their mental health and self-care through exercise, taking personal time, counseling, and distancing themselves from news and social media. Clinicians also expressed an ability to compartmentalize along with resilience and acceptance in the face of uncertainty, allowing them to “be a better provider to…patients” (P4).
The clinical encounter
Challenges included substantial fear of contracting COVID-19 and implementation of protective measures (Appendix C.2). For example, universal masking policies limited nonverbal cues, exacerbated language barriers, and impaired therapeutic relationships with patients declining to mask. Most clinicians reported implementing telehealth to limit exposures. However, challenges included difficult technology, lack of privacy, trouble “establish[ing] a rapport” (P21), blunted nonverbal communication, dependence on remote monitoring, and inadequate infrastructure, particularly for underinsured patients. Yet, many clinicians also recognized telehealth as a facilitator, allowing clinicians to “maintain continuity of care” (P11) through circumventing barriers of transportation, childcare, and employment, and increasing access to postpartum and mental health care. Telehealth uniquely allowed clinicians to gain a “glimpse into [the patient's] home,” contextualizing patients’ lives and support systems (P17). A clinician deemed telehealth to be more “patient-focused” (P14) by avoiding “the discomfort of being in a doctor's office” (P14) with less administrative work, leaving more time for patient interaction. Most clinicians adopted both telehealth and in-person options through the pandemic and emphasized the need for flexibility to maximize access.
Vaccination counseling was difficult prior to safety data; even after formal recommendations were issued, clinicians remained cautious in fear of “ruin[ing] the doctor/patient relationship” (P9) in the charged political climate. Multiple appointments were often required, leading some clinicians to forgo extensive counseling due to competing priorities. Despite difficulty engaging some patients, shared decision-making was an important tool:
“…reminding patients that we're here to support their decisions, even when they aren't the decisions that we've recommended, is…really important…our job is to…give them the information and support that they need so that they can make the right decisions. And then…on a personal level, just actually coming around to feeling really okay with patients making choices that aren't what we recommend, which is a really hard thing.” (P14)
Vaccine counseling often demanded high levels of health literacy. To manage this, a clinician recommended mirroring “our patient population's wording” (P4). Several clinicians chose to share anecdotal experiences of receiving the vaccine while pregnant as an alternative to “sterile” (P15), statistics-based counseling, or “scare tactics” (P21). Including family members was integral for discussions.
Healthcare system factors
Healthcare systems were under stress, constantly adapting to evolving recommendations (Appendix C.3), and these systematic changes were cumbersome. For example, a clinician described the impacts of predelivery COVID-19 testing on the patient experience:
“…we did test everybody who came in…to labor and delivery…if either parent tested positive, the baby would go to the NICU [neonatal intensive care unit] and the parents would be separated from the baby for the first…14 days or something…which was obviously a huge deal.” (P21)
When counseling led to acceptance of COVID-19 vaccination, lack of onsite availability often precluded vaccination. Restrictive visitor policies challenged instances of critical decision-making for families, and milestone experiences excluded support people who “bring a lot of joy around pregnancy” (P19). However, certain policies such as universal adoption of infection precautions, especially masking, were facilitators. Along with deeming masking an effective infection control measure, clinicians perceived that “some patients…felt safer, healthier, more comfortable” (P14).
Staff shortages occurred from an overburdened system and COVID-19 exposures. Thus, clinicians worked longer hours with overbooked schedules. Staff shortages extended to transportation staff, social and case workers, and mental health support, further exacerbating disparities. “Abbreviated” (P19) visits were implemented, but clinicians worried about interrupting “continuity of care” (P19). However, a few clinicians found reduced prenatal schedules unexpectedly efficient and endorsed spacing out visits at the “end of the first and the middle of the second trimester” since “there's not a whole lot going on” (P6). Guidelines from national organizations helped justify reducing prenatal visits and fetal surveillance in select pregnancies, and clinicians felt supported in changing standard of care with the evolving pandemic.6,25
Some clinicians became disheartened when they realized leadership could not safely support their work. Early personal protective equipment shortages resulted in clinicians receiving one set of single-use gear but were instructed “to wear this until it falls apart” (P20). Institutions offered pandemic-related resources that were often inadequate or overwhelmed. Trainees recounted attending physicians hesitating to enter COVID-19-positive rooms while residents did so routinely, and vaccination was offered to them along with other patient-facing staff only after hospital administrators. Overall, a “lack of transparency between the administration and the providers” (P15) fueled a disconnect between institutional decision-making and clinical care, worsening feelings of helplessness and resentment. However, certain institutional resources were well-received. A clinician recalled that a psychiatrist was available just for residents, destigmatizing mental healthcare. Institutional support for out-of-state telehealth licensing and interdisciplinary care models, in which patients had “access to social work,…WIC, dental…their pediatrician, behavioral health, psychiatry” (P6) improved care. A clinician described how resource utilization became more efficient:
“…[the pandemic] improved our utilization of our time and our resources…I never felt patients lacked access…if anything, there was an increased focus on making sure we weren't missing people or losing track of folks…we were offering them anything we could provide in terms of transportation, communication needs.” (P6)
Access to behavioral healthcare was also important to process “trauma and social isolation” (P17) from the pandemic. Support for remote multidisciplinary meetings to discuss high-risk cases “allow[ed] more voices to contribute to the discussion and care of a patient” (P10).
Societal factors
Expected challenges of finances, food, housing, childcare, and transportation resulted from unemployment and closures of shelters, food banks, and daycares, especially for patients at FQHCs (Appendix C.4). Insurance status delayed access to treatment and complicated telehealth billing. When asked how to improve obstetric care during the pandemic, a clinician proposed “giv[ing] everyone healthcare…without any concern about financial ramifications” (P16). Facilitators included policy changes, such as emergency orders for vaccine coverage, updated telehealth billing, and emergency insurance coverage. Additionally, healthcare workers were featured prominently in the press. Clinicians reported patient interactions that were “exceptionally kind” and “sympathetic” (P14) as a result, helping combat burnout. Clinicians perceived that societal focus on healthcare also increased patient health awareness. Patients seemed “more in tune with their body” (P9), able to “protect themselves and their families” (P1), and “able to reach out for help” (P9).
All participants identified medical mistrust as a challenge, often dichotomized as historical mistrust or pandemic-associated mistrust stemming from misinformation. A clinician described how the “racist heritage” (P16) of her hospital fueled historical mistrust in the community, justified as “true mistrust” (P20). Another clinician stated that while some patients may not identify specific events of injustice in American history such as the Tuskegee study,26 trauma from these events still permeated Black communities served by the participant's FQHC. In contrast, pandemic-associated mistrust centered on heavily politicized misinformation, such as the vaccine “contain[ing] some sort of government tracking device” (P15), or that the vaccine was a “political tool…trying to harm them” (P15). A clinician highlighted the interaction of these contrasting forms of mistrust:
“…the historical perspective has always existed, and I think layering the pandemic on top of that…when you have a population that rightly so has suspicions about the ability of their healthcare system to take care of them, and then you are bombarded by propaganda that's not evidence-based, that is highly tailored towards medical mistrust, I think it really exacerbates the problem and makes it very difficult… Sometimes it's hard to really bridge that gap between…this is a system that has failed you as a person, has failed your family for generations, but here I am trying to do what's best for you.” (P15)
Some patients were noted to be more hesitant of vaccines during pregnancy, and this was worsened by lack of COVID-19 vaccine-specific safety data. Clinicians reported that some patients believed the vaccine “increase[s] the risk of stillbirth” (P19), or “attacks the placenta” (P5). Sources of misinformation included friends, family, and other physicians, and combatting misinformation could dismantle hard-earned trust. A few clinicians noted efforts to avoid paternalism to prevent further mistrust. Stances on vaccination and masking were perceived as political, leading to “aggressive and negative” interactions (P17), and political beliefs emerged as a more salient aspect of identity within the patient-clinician relationship. Pandemic-related political rhetoric was deemed “a disservice to the actual medical needs of communities” (P20).
A few clinicians acknowledged how their racial identity influenced patient relationships and recognized how their White race affected relatability of anecdotal healthcare experiences. Clinicians also discussed how systemic racism impacted their community, citing historical practices that impact present-day health outcomes and fuel mistrust of healthcare institutions. Clinicians acknowledged their limitations but still aspired for change, recognizing that a single obstetric encounter cannot dismantle structural racism, but rather must be tackled “piece by piece” (P20) in the healthcare system.
Clinicians attempted methods of trust-building, such as integration into the community to combat historical mistrust. Clinicians at FQHCs held events providing COVID-19 vaccines, tests, baby supplies, and food. Rather than practicing medicine in a “silo” (P17), the importance of community collaboration for academic clinicians was recognized. Trust was built through being “available to [patients]” (P4) to create a “safe place” (P4) for families, “learning about a patient as a whole” (P15), and including support people in difficult conversations. A clinician described the importance of care continuity:
“…fortunately, for our patients who are in our publicly insured clinic, they have continuity of care…they'll have a resident that sees them for the majority of their pregnancy, they'll have a nurse, midwife or a nurse practitioner who sees them for the continuity…there are patients who have benefited extremely from having a single provider that they can then build trust with over the course of a pregnancy.” (P15)
Structured discussion/comment
Principal findings
We qualitatively explored clinician experiences providing obstetric care during the COVID-19 pandemic through thematic analysis of challenges and facilitators within the domains of the HEIF (Figure).
Results
Lack of social support and burnout could be countered with mental healthcare and self-care. Implementation of telehealth in the clinical encounter was challenging4,5,8,10,17, 18, 19 but telehealth was also identified as a facilitator to circumvent barriers to care.3, 4, 5,10, 11, 12 However, inequities in telehealth capabilities between clinics further exacerbated disparities. Healthcare system challenges such as visitor restrictions and delayed care mirror prior studies,8,9 but interdisciplinary care, professional society guidelines, and institutional resources were identified as critical facilitators. While prior literature highlighted societal factors such as financial strain, childcare, and racism, our study delved into clinician perceptions of their sociopolitical landscape.4,9,10,18,27, 28, 29, 30, 31, 32, 33 Many appeared deeply familiar with historical mistrust from racialized medical trauma stemming from disinvestment from disadvantaged neighborhoods in the urban Midwest. However, the stark politicization of medical knowledge and the vast and rapid spread of pandemic-associated misinformation was unprecedented.
Clinical implications
While some pandemic-related changes have evolved, others persist and may be implemented again if another pandemic occurred. Therefore, multi-level interventions to improve obstetric care delivery can be designed, assessed, and implemented based on challenges and facilitators identified and can be applied to the persistent charged political climate surrounding reproductive and racial justice in medicine. Shared decision-making for new interventions can decrease decisional conflict and increase uptake.34 Discretionary and flexible use of telehealth could address barriers to care. Transparency and resources from institutions, particularly childcare, mental healthcare, administrative support, and inclusion of clinicians in decision-making could ease burnout and healthcare system stressors. Interdisciplinary coordination between physicians, social work, and nursing, could aid with comprehensive, high-quality care provision.29 Academic centers can partner with community health centers such as FQHCs to promote equity and trust-building.
Research implications
Future work should include design, implementation, and assessment of multilevel, community-based interventions to address identified challenges. An in-depth exploration of stakeholder perspectives, including those of patients, clinicians, social workers, community health workers, and public health officials, on solutions to larger societal issues identified (i.e., mistrust, politicization of medicine, and misinformation) is needed.
Strengths and limitations
Our study identified multi-level facilitators of obstetric care based on the HEIF, beyond telehealth, a major focus of several prior studies.4,5,10,17, 18, 19 Through interviewing clinicians, we centered lived experiences of obstetric clinicians within a stressed healthcare system and society, during unprecedented politicization of medicine and misinformation. While the study's timing, years into the pandemic, did not allow for real-time insight into clinicians’ experiences at its onset, it potentially allowed for more time for reflection on lessons learned while many pandemic-related changes were still persistent. Our findings are particularly pertinent to similar urban Midwestern communities, although lessons learned can be generalized to other settings that face similar challenges of structural racism, insurance barriers, and polarized political environments. However, our results may not be generalizable to nurses, social workers, and midwives given our study sample. The majority of participants identified as White women early in their careers, limiting gendered, racialized, and generational experiences represented. Notably, most participants serve a large proportion of Black patients and thus may have a unique understanding of how discordant racial identities interact within the clinician-patient relationship. Convenience sampling may have precluded us from exploring perspectives of busy clinicians unavailable for interviews, with overrepresentation of academic clinicians. Finally, our data only reflects clinicians’ own perceptions and therefore cannot be extrapolated to represent patients’ actual obstetric experiences.
Conclusions
Through exploring clinicians’ experiences providing obstetric care during the pandemic and navigating sociopolitical challenges, healthcare system stressors, and difficult clinical encounters, we were also able to identify facilitators of care. The presented perspectives may serve to guide obstetric care in the setting of future, inevitable healthcare stressors.
CRediT authorship contribution statement
Drishti D. Sinha: Writing – review & editing, Writing – original draft, Visualization, Investigation, Formal analysis, Data curation, Conceptualization. Megan Foeller: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Funding acquisition, Conceptualization. Abigail S. Bell: Writing – review & editing, Formal analysis. Anthony J. Nixon: Writing – review & editing, Formal analysis. Darrell Hudson: Writing – review & editing, Supervision, Conceptualization. Aimee S. James: Writing – review & editing, Supervision, Conceptualization. Amy R. Scheffer: Writing – review & editing, Methodology, Investigation. Ana A. Baumann: Writing – review & editing, Supervision, Conceptualization. Emily Diveley: Writing – review & editing, Methodology, Data curation. Ebony B. Carter: Writing – review & editing, Supervision, Conceptualization. Nandini Raghuraman: Writing – review & editing, Supervision, Conceptualization. Indira U. Mysorekar: Writing – review & editing, Supervision, Project administration, Funding acquisition, Conceptualization. Jeannie C. Kelly: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Funding acquisition, Conceptualization.
Acknowledgments
Acknowledgments
We would like to thank the clinicians who participated in the study for their insights and time. Financial support for this study was provided by grant # R01HD091218-04S1: The Safety, Testing/Transmission, and Outcomes in Pregnancy with COVID-19 (STOP-COVID) study and the Washington University School of Medicine Dean's Medical Student Research Fellowship for the Yearlong Research Program.
Patient consent statement
Verbal consent obtained.
Clinical trial registration
Not applicable.
Presentation
The findings of this paper have not been presented at any meetings.
Disclaimers
None.
Footnotes
This study was conducted in St. Louis, Missouri, USA.
Condensation: Clinicians identified challenges and facilitators of obstetric care provision related to the clinical encounter, healthcare system, and society during the Coronavirus disease 2019 pandemic.
Funding: grant # R01HD091218-04S1: The Safety, Testing/Transmission, and Outcomes in Pregnancy with COVID-19 (STOP-COVID) study, Washington University School of Medicine Dean's Medical Student Research Fellowship for the Yearlong Research Program. The funding sources were not involved in the study design, data collection, data analysis and interpretation, manuscript writing, or decision to publish the manuscript.
Conflict of Interest: IUM serves on the scientific advisory board of Luca Biologics. The remaining authors report no conflicts of interest.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xagr.2024.100392.
Appendix. Supplementary materials
References
- 1.American College of Obstetricians and Gynecologists. Addressing health equity during the COVID-19 pandemic: Position statement, 2020. (Accessed 31 July, 2024 athttps://www.acog.org/clinical-information/policy-and-position-statements/position-statements/2020/addressing-health-equity-during-the-covid-19-pandemic).
- 2.Oakes MC, Zhang F, Stevenson L, et al. Changes in the antenatal utilization of high-risk obstetric services and stillbirth rate during the COVID-19 pandemic. Am J Perinatol. 2022;39:830–835. doi: 10.1055/s-0041-1740212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peahl AF, Powell A, Berlin H, et al. Patient and provider perspectives of a new prenatal care model introduced in response to the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. 2021;224:384. doi: 10.1016/j.ajog.2020.10.008. e1–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madden N, Emeruwa UN, Friedman AM, et al. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in New York City: a quantitative and qualitative analysis. Am J Perinatol. 2020;37:1005–1014. doi: 10.1055/s-0040-1712939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Almuslim H, AlDossary S. Models of incorporating telehealth into obstetric care during the COVID-19 pandemic, its benefits and barriers: a scoping review. Telemed e-Health. 2022;28:24–38. doi: 10.1089/tmj.2020.0553. [DOI] [PubMed] [Google Scholar]
- 6.Peahl AF, Smith RD, Moniz MH. Prenatal care redesign: creating flexible maternity care models through virtual care. Am J Obstet Gynecol. 2020;223:389. doi: 10.1016/j.ajog.2020.05.029. e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dosaj A, Thiyagarajan D, ter Haar C, et al. Rapid implementation of telehealth services during the COVID-19 pandemic. Telemed and e-Health. 2020;27:116–120. doi: 10.1089/tmj.2020.0219. [DOI] [PubMed] [Google Scholar]
- 8.Gomez-Roas MV, Davis KDM, Leziak K, et al. Postpartum during a pandemic: challenges of low-income individuals with healthcare interactions during COVID-19. PLoS One. 2022;17 doi: 10.1371/journal.pone.0268698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meaney S, Leitao S, Olander EK, Pope J, Matvienko-Sikar K. The impact of COVID-19 on pregnant womens’ experiences and perceptions of antenatal maternity care, social support, and stress-reduction strategies. Women Birth. 2022;35:307–316. doi: 10.1016/j.wombi.2021.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morgan A, Goodman D, Vinagolu-Baur J, Cass I. Prenatal telemedicine during COVID-19: patterns of use and barriers to access. J Am Med Inform Assoc. 2022;5:ooab116. doi: 10.1093/jamiaopen/ooab116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nelson GA, Holschuh C. Evaluation of telehealth use in prenatal care for patient and provider satisfaction: a step toward reducing barriers to care. J Nurse Pract. 2021;17:481–484. [Google Scholar]
- 12.Ghimire S, Martinez S, Hartvigsen G, Gerdes M. Virtual prenatal care: a systematic review of pregnant women's and healthcare professionals’ experiences, needs, and preferences for quality care. Int J Med Inform. 2023;170 doi: 10.1016/j.ijmedinf.2022.104964. [DOI] [PubMed] [Google Scholar]
- 13.Mirzakhani K, Shoorab NJ, Akbari A, Khadivzadeh T. High-risk pregnant women's experiences of the receiving prenatal care in COVID-19 pandemic: a qualitative study. Biomed Central Pregnancy Childbirth. 2022;22:363. doi: 10.1186/s12884-022-04676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burgess A, Breman RB, Bradley D, Dada S, Burcher P. Pregnant women's reports of the impact of COVID-19 on pregnancy, prenatal care, and infant feeding plans. Am J Matern/Child Nurs. 2021;46:21–29. doi: 10.1097/NMC.0000000000000673. [DOI] [PubMed] [Google Scholar]
- 15.Tadesse E. Antenatal care service utilization of pregnant women attending antenatal care in public hospitals during the COVID-19 pandemic period. Int J Women's Health. 2020;12:1181–1188. doi: 10.2147/IJWH.S287534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin MM, Knobel R, Nandi V, Pereira JG, Trapani Junior A, Andreucci CB. Adequacy of antenatal care during the COVID-19 pandemic: observational study with postpartum women. Revista Bras Ginecol Obstet. 2022;44:398–408. doi: 10.1055/s-0041-1741450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craighead CG, Collart C, Frankel R, et al. Impact of telehealth on the delivery of prenatal care during the COVID-19 pandemic: mixed methods study of the barriers and opportunities to improve health care communication in discussions about pregnancy and prenatal genetic testing. JMIR Form Res. 2022;6:e38821. doi: 10.2196/38821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson DH, Henebury MJE, Arentsen CM, Sriram U, Metallinos-Katsaras E. Facilitators, barriers, and best practices for in-person and telehealth lactation support during the COVID-19 pandemic. Nurs Women's Health. 2022;26:420–428. doi: 10.1016/j.nwh.2022.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konnyu KJ, Danilack VA, Adam GP, Friedman Peahl A, Cao W, Balk EM. Changes to prenatal care visit frequency and telehealth: a systematic review of qualitative evidence. Obstet Gynecol. 2023;141:299–323. doi: 10.1097/AOG.0000000000005046. [DOI] [PubMed] [Google Scholar]
- 20.Cambria N, Fehler P, Purnell JQ, Schmidt B. Washington University in St. Louis; St. Louis: 2018. Segregation in St. Louis: dismantling the divide.https://bpb-us-w2.wpmucdn.com/sites.wustl.edu/dist/3/1454/files/2018/06/Segregation-in-St.-Louis-Dismantling-the-Divide-22ih4vw.pdf (Accessed 31 July, 2024, at. [Google Scholar]
- 21.Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement Sci. 2019;14:1–18. doi: 10.1186/s13012-019-0861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ando H, Cousins R, Young C. Achieving saturation in thematic analysis: development and refinement of a codebook. Compr Psychol. 2014;3:03.CP.3.4. [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 24.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J for Qual in Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 25.Boelig RC, Saccone G, Bellussi F, Berghella V. MFM guidance for COVID-19. Am J Obstet Gynecol Matern Fetal Med. 2020;2 doi: 10.1016/j.ajogmf.2020.100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The syphilis study at Tuskegee timeline. 2022. (Accessed 11 June, 2023, at https://www.cdc.gov/tuskegee/timeline.htm.)
- 27.Sword W. A socio-ecological approach to understanding barriers to prenatal care for women of low income. J Adv Nurs. 1999;29:1170–1177. doi: 10.1046/j.1365-2648.1999.00986.x. [DOI] [PubMed] [Google Scholar]
- 28.Ruderman RS, Dahl EC, Williams BR, et al. Provider perspectives on barriers and facilitators to postpartum care for low-income individuals. Women's Health Rep. 2021;2:254–262. doi: 10.1089/whr.2021.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heaman MI, Sword W, Elliott L, et al. Barriers and facilitators related to use of prenatal care by inner-city women: perceptions of health care providers. Biomed Central Pregnancy Childbirth. 2015;15:2. doi: 10.1186/s12884-015-0431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Downe S, Finlayson K, Tunçalp Ö, Gülmezoglu AM. Provision and uptake of routine antenatal services: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;6 doi: 10.1002/14651858.CD012392.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mazul MC, Salm Ward TC, Ngui EM. Anatomy of good prenatal care: perspectives of low income African-American women on barriers and facilitators to prenatal care. J Racial Ethn Health Disparities. 2017;4:79–86. doi: 10.1007/s40615-015-0204-x. [DOI] [PubMed] [Google Scholar]
- 32.Anderson MR, Hardy EJ, Battle CL. COVID-19 vaccine hesitancy during the perinatal period: understanding psychological and cultural factors to improve care and address racial/ethnic health inequities. Women's Health Issues. 2022;32:317–321. doi: 10.1016/j.whi.2022.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thomson G, Cook J, Crossland N, et al. Minoritised ethnic women's experiences of inequities and discrimination in maternity services in North-West England: a mixed-methods study. Biomed Central Pregnancy Childbirth. 2022;22:1–14. doi: 10.1186/s12884-022-05279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scalia P, Durand MA, Elwyn G. Shared decision-making interventions: an overview and a meta-analysis of their impact on vaccine uptake. J Intern Med. 2022;291:408–425. doi: 10.1111/joim.13405. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.