Abstract
Background:
Meniscus root tears comprise 10% to 21% of all meniscal tears. These tears alter knee biomechanics, elevating contact pressure, akin to a meniscectomy. Consequently, they are linked to advanced joint degeneration and cartilage damage in the affected compartment.
Purpose:
To systematically evaluate and relate the current literature describing the diagnosis and treatment strategies for meniscus root tears.
Study Design:
Scoping review; Level of evidence, 4.
Methods:
This review was conducted following the guidelines of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews. Inclusion criteria encompassed English-language clinical and preclinical research, technical notes, and narrative reviews on meniscus root tears. Exclusion criteria were studies on patellar tendon rupture, studies on medial patellofemoral ligament rupture with additional knee joint ligament injuries, studies of patients <16 years old, and studies involving open fractures. The data were summarized using a descriptive analysis and a thematic analysis.
Results:
After 1425 articles were identified, 461 studies were included; 17% (n = 78) were case reports or case series, 15% (n = 71) were technical notes, 9% (n = 41) addressed aspects of diagnosis, 7% (n = 32 ) were narrative reviews, and 5% (n = 21) were systematic reviews or meta-analyses. Studies presenting original data comprised 57% (n = 262) of all included studies, and 97% of the studies were of evidence levels 3 to 5. Contributions were mainly from the United States (n = 123; 27%), Republic of Korea (n = 102; 22%), and Japan (n = 99; 21%). Many studies (n = 216; 47%) focused on the treatment and outcomes of meniscus root tears. A significant chronological surge in the quantity of studies addressing the diagnosis and treatment of meniscus root tears was evident, particularly over the past 3 years. Consensus was found regarding the definition of meniscus root tears, the advantages of early repair, and postoperative rehabilitation protocols. The variations in surgical techniques and operative strategies created the greatest amount of contention, along with clinical assessment and imaging modalities.
Conclusion:
High-level evidence studies for diagnosing and managing meniscus root tears were scarce. A consensus has yet to be reached regarding the role of concomitant osteotomy, comparison of repair techniques, the use of a centralization stitch, patient factors affecting outcomes, and long-term outcomes of nonoperative management.
Keywords: meniscus, meniscus root, osteoarthritis, knee arthroscopy, joint preservation
Recent decades have seen a paradigm shift in the management of meniscal tears, as continued research sheds light on their unique biomechanical implications, treatment nuances, and clinical consequences, paving the way for an emphasis on meniscal preservation. 140 Critical to the function of the menisci, particularly in load distribution, is the integrity of the peripheral circumferential fibers and root attachments.45,151 Meniscus root tears, defined as radial tears up to 1 cm from the meniscus root attachment, 21,22, 132,154,191 have been consistently associated with impaired joint kinematics and contact mechanics and are frequently the underlying cause behind significant conditions such as subchondral insufficiency fractures, rapidly progressing osteoarthritis (OA), or ligament reconstruction failure.6,34,77,198
The significance of meniscus root tears within the scope of all meniscal injuries is 2-fold, because tears of the meniscus root comprise an estimated 10% to 21% of all meniscal tears.35,87,132 From a biomechanical standpoint, the meniscus roots have a crucial role in transforming and dispersing axial tibiofemoral loads as hoop stresses.6,18 These structures are integral to the proper functioning of the menisci and, in turn, knee biomechanics, because the menisci are responsible for absorbing 50% to 70% of loads experienced by the medial and lateral compartments.6,18 Tears of the meniscus root cause extrusion of the meniscus, leading to a disruption in the distribution of forces across the tibial plateau, as a result of the loss of hoop stress.126,154 Resulting abnormal, high-peak tibiofemoral contact pressures and decreased contact areas may lead to degenerative cartilage damage. 6 Loss of the meniscus root attachment, and associated function, has been shown to result in a biomechanical state that mirrors that of a total menisectomy.6,148,171
Efforts in the past decade have raised attention to the importance of meniscal preservation and repair13,14,51,180 because the consensus now acknowledges that meniscectomy consistently results in rapidly progressive OA of the knee.55,116,171 This shift has been driven by a mounting body of evidence demonstrating both the adverse consequences of meniscectomy and the advantageous outcomes achieved through meniscus root repair. 112 Although several techniques for surgical repair of the meniscus root have been described and are used, the most common technique is the transtibial pullout repair. §§
Discussions concerning the most valuable clinical signs, imaging methods, operative versus nonoperative strategies, surgical techniques, and protocols for rehabilitation are numerous across the literature. However, a low level of evidence still characterizes a large contingent of the studies on meniscus root tears, and topics of debate are often addressed in narrative reviews largely expressing expert opinion. To date, a robust overview that assesses the scope, variety, and overall consolidation of literature concerning meniscus root tears is lacking.
The purpose of the present study was to conduct a methodically rigorous scoping review outlining the literature that examines the diagnosis and management of meniscus root tears. The findings of this study will aid in shared and informed decision-making as well as highlight gaps in the literature, paving the way for the establishment of future research priorities.
Methods
Literature Search
This review was conducted following the guidelines outlined in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews. A systematic search of PubMed and EMBASE databases was performed in accordance with the 2020 PRISMA guidelines, 172 with the purpose of identifying studies to answer the broad question of what is currently known about the diagnosis and treatment of meniscus root tears in the literature. This search was performed between date of inception and June 30, 2023, using the search terms “meniscus” OR “meniscal” AND “root” AND “lesion” OR “tear.” The Boolean terms “AND” and “OR” were used to extract relevant studies. The reference lists of all studies that fulfilled the inclusion criteria were subsequently explored until no additional pertinent articles were discerned. Titles and abstracts were evaluated for eligibility by 2 reviewers (J.R.G. and S.G.A.). In cases of unresolved consensus, the study advanced to an examination of the full text, with a third reviewer (M.H.) ultimately determining the study's inclusion or exclusion.
Study Selection
Studies were considered eligible if they met the inclusion criteria, which were created through expert consultation. Experts were defined as physicians who treat a high volume of patients with meniscus root tears and who educate internationally on the subject (J.C., F.F., A.G.G., I.M., G.M., N.N.V., and R.F.L.). The inclusion and exclusion criteria for study selection are shown in Table 1.
Table 1.
Selection Criteria for Studies
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| • Individual case reports, technical notes, opinion pieces, and narrative reviews regarding meniscus root tears • Clinical and preclinical studies related to meniscus root tears • Studies reporting the outcomes of management of meniscus root tears • Studies reporting concomitant meniscus body and meniscus root tears |
• Studies not relevant to meniscus root tears • Conference abstracts, book chapters • Studies not in the English language • Studies reporting on patellar tendon rupture, medial patellofemoral ligament rupture in combination with ≥1 ligaments of the knee joint • Studies including pediatric patients (aged <16 years, skeletally immature) • Studies including open fractures |
Data Extraction
Charting tables were used to record, compile, and assimilate extracted data. A priori categories were charted as well as emerging themes. Demographic information regarding diversity within the population of study participants was noted. Four reviewers (J.R.G., S.G.A., M.H., and F.A.) undertook data extraction. Any discrepancies were discussed by the group of reviewers. A structured assessment of quality was omitted, given that the primary objective of scoping reviews is to chart the landscape of available evidence rather than exclusively seek the best available evidence. The methodological approach adopted within this scoping review facilitated the extraction, aggregation, and synthesis of existing knowledge within this expansive domain, and the information was summarized in the following manner:
A descriptive analysis that includes geographic mapping of studies, chronological analysis by year of publication, study methods, focus of studies, and level of evidence assigned for all clinical articles using the Journal of Bone and Joint Surgery ranking system 202
A thematic analysis that describes how the existing published literature relates to the initial research question and aims of the present study, along with the main findings from the studies, organized by theme
Results
Descriptive Analysis
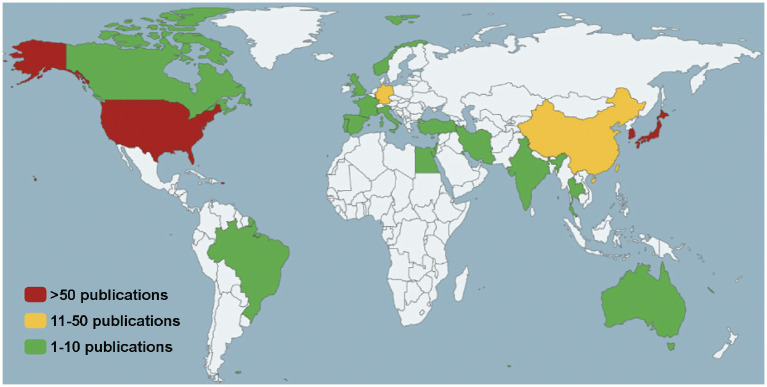
The study selection process and the results of the search are outlined in Figure 1. A total of 461 studies met the inclusion criteria and aligned with the aims and research question of the present review. A significant chronological surge was evident in the quantity of studies addressing the diagnosis and treatment of meniscus root tears (Figure 2). The earliest study was published in 2002, and the largest number of studies was published in 2023. A summary of all included studies is in Supplemental Table S1, available separately.
Figure 1.
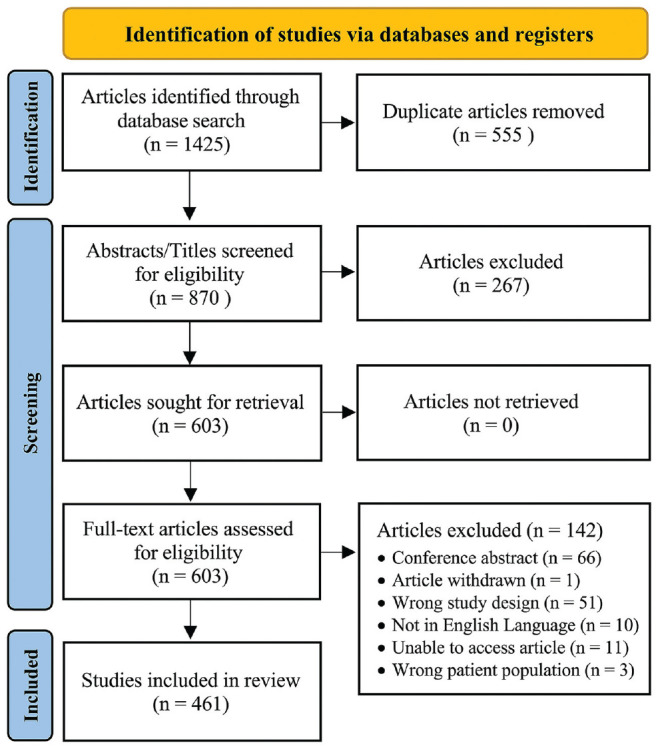
Diagram demonstrating the article selection process conducted according to the 2020 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 172
Figure 2.
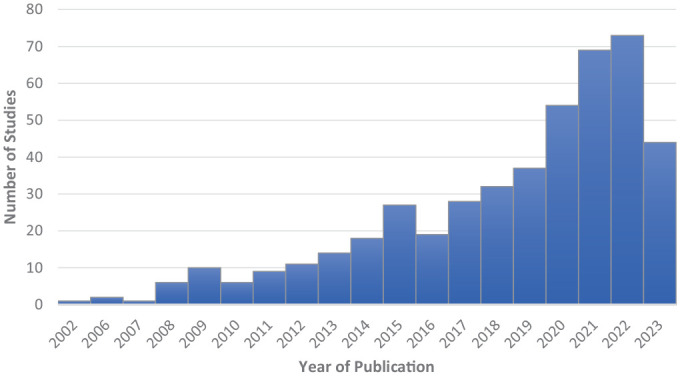
Bar graph demonstrating the number of studies related to meniscus root tear by publication year.
In total, 24 countries produced studies that were included in this review. Contributions were most significant from the United States (123 studies; 27%), the Republic of Korea (102 studies; 22%), and Japan (99 studies; 21%). A heatmap illustrating the nations with the highest publication frequency is shown in Figure 3.
Figure 3.
Heatmap of countries demonstrating geographic concentration of studies related to meniscus root tear.
Considerable heterogeneity was seen in the design and method of the studies (Figure 4). Studies were predominantly of lower order evidence, with levels 3 to 5 accounting for 97% of the total.
Figure 4.
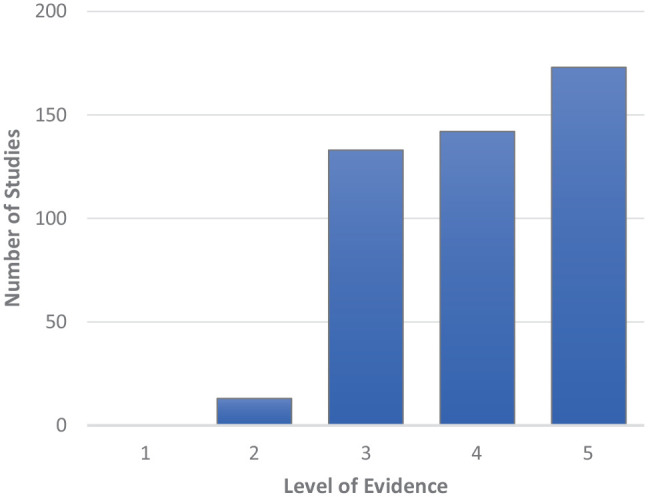
Distribution of included studies according to level of evidence, as determined by the Journal of Bone and Joint Surgery ranking system. 202
A total of 21 systematic reviews ‖‖ were included in this scoping review for the purpose of obtaining demographic information such as age, race and ethnicity, and sex ratio of patients included in studies analyzing various aspects of the diagnosis and management of meniscus root tears. Of these reviews, 12 (57%) reported the sex of the participants. Women comprised 52% of the total patients, and the mean age of included individuals was 50.2 years. No systematic review reported on the race and ethnicity of participants. However, an analysis of all studies included in this scoping review demonstrated that only 10 studies (2.17%) reported on the race and ethnicity of participants, with 10 studies specifying Asian participants and 2 studies specifying White participants. A few studies assessed meniscus root tears in the context of high-level sport (n = 5)14,73, 78,98,152,196 or in a military setting (n = 1), 98 although a large majority of studies did not mention or investigate these special populations.
Focus of Studies
In the cohort of included studies that presented original clinical data (n = 262), a subset of 55 studies (21%) were centered on investigating aspects of the diagnosis of meniscus root tears. These studies examined various imaging modalities, clinical examination maneuvers, clinical usefulness of imaging findings, and classification systems. Within this subset, 29 studies were of level 2 or 3 evidence, encompassing 3 cross-sectional, 6 prospective, and 20 retrospective studies.
A substantial portion of the included studies presenting original clinical data addressed elements associated with the treatment and outcomes of meniscus root tears (n = 206; 79%). Within this category, 112 studies were of level 2 or 3 evidence, comprising 17 prospective, 93 retrospective, and 2 cross-sectional studies. The focus of these studies included comparative assessment, evaluation, and descriptive analysis of meniscus root repair techniques, along with analysis of factors affecting postoperative outcomes and the progression of OA and meniscal extrusion and comparison of operative versus nonoperative management.
Of all included studies, 47% (n = 218) addressed treatment and outcomes, 17% were case reports or case series (n = 78), 15% (n = 71) were technical notes, 9% (n = 41) addressed aspects of diagnosis, 7% (n = 32) were narrative reviews, and 5% (n = 21) were systematic reviews or meta-analyses, as seen in Figure 5.
Figure 5.
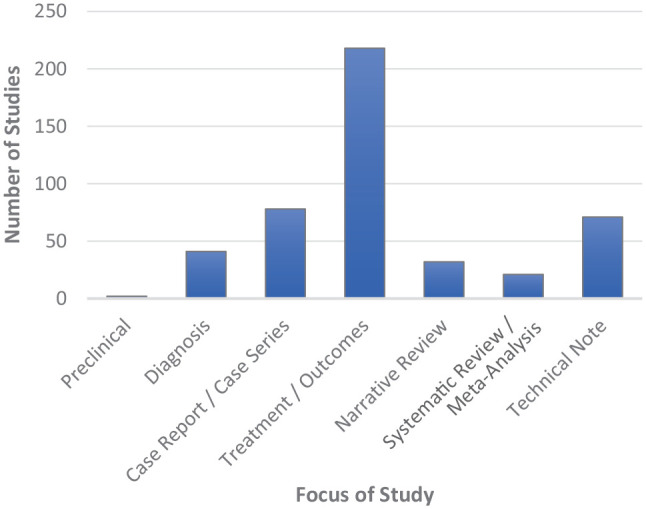
Distribution of studies according to their primary focus.
Thematic Analysis
Nomenclature and Definitions
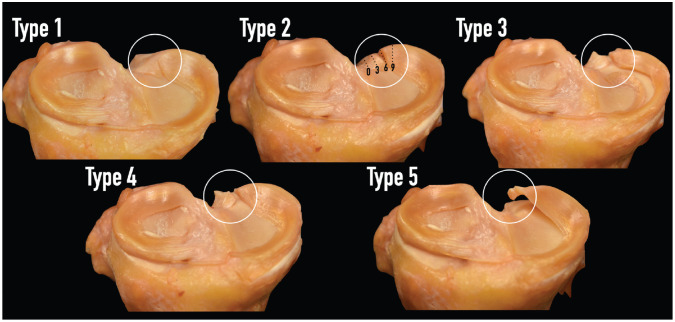
Meniscus root tears are most commonly defined as either an avulsion at the insertion site of the meniscal attachment or a complete radial tear located within 1 cm of the meniscal insertion. 21 In the present study, the earliest definitions of meniscus roots were from 2006. Jones et al 88 defined the posterior root of the medial meniscus as “a strong, thick structure” that is “visible on MRI as a low-signal band of tissue extending from the posterior horn of the meniscus to its attachment on the proximal tibia, immediately anterior to the posterior cruciate ligament.” Also in 2006, Brody et al 19 defined meniscus roots as “the last few millimeters of meniscal tissue angling down to the tibial plateau attachment in the intercondylar notch.” Then, in 2008, Griffith et al 67 were the first to report a meniscus root avulsion fracture while also documenting its repair and reporting outcomes at 3-year follow-up. In 2009, Ahn et al 3 defined a posterior lateral (PL) meniscus root tear as “a tear that occurs less than 1 cm from the posterior insertion.” This was the most common definition found among the literature reviewed. Some studies used a slightly different definition, describing root tears as occurring within 9 mm of the posterior bony attachment as opposed to within 1 cm of the insertion. This is likely based on the definition used by LaPrade et al 124 for a type 2 meniscus root tear, defined as a “complete radial tear within 9 mm from the bony root attachment.” LaPrade et al 124 were the first to create a classification of meniscus root tears by tear morphology, and it has become the primary established classification system. As per this classification system, the remaining types of tear patterns are as follows: “partial stable root tear (type 1), complete radial tear within 9 mm from the bony root attachment (type 2), bucket-handle tear with complete root detachment (type 3), complex oblique or longitudinal tear with complete root detachment (type 4), and bony avulsion fracture of the root attachment (type 5)” 124 (Figure 6).
Figure 6.
The LaPrade classification 124 for meniscus root tears using cadaveric specimens.
Many studies either did not define a root tear or used a nonspecific definition like the one used by Lim et al, 149 which defined a root tear as a “radial tear at its posterior root attachment.” A small group of studies defined a meniscus root tear as a radial tear within 5 mm of the bony attachment. Despite the few discrepancies regarding specific distance from the root attachment site, there appears to be an overall well-accepted definition of meniscus root tears.
Meniscus Root Anatomy and Biomechanics
Various cadaveric studies aimed to establish the root attachments’ anatomy and their relation to anatomic landmarks.86,122,192 A thorough comprehension of the native anatomy is paramount when managing meniscus root tears, as nonanatomic repairs fail to restore meniscal function. 123
In terms of arthroscopically relevant landmarks, the anterior root of the lateral meniscus is located 14.4 mm anteromedial to the apex of the lateral tibial eminence and most notably lies in close relation to the tibial insertion of the anterior cruciate ligament (ACL). 122 The center of the ACL insertion is 5 mm posteromedial to the center of the anterior lateral (AL) root, 122 with studies reporting a 41%-63% overlap of the AL root area with the ACL tibial insertion.122,192 This notable proximity is reflected in biomechanical findings by LaPrade et al 129 demonstrating that ACL tunnel reaming decreases the AL root attachment area and ultimate failure strength, whereas in the clinical setting, Oshima et al 169 characterized lateral deviation during tibial tunnel reaming as an independent risk factor for postoperative lateral meniscal extrusion.
The anterior medial (AM) root is found 18.2 mm anteromedial to the center of the ACL and approximately 32.8 mm anterior to the posterior medial (PM) root. 192 The AM root is at risk during intramedullary nailing of the tibia.44,131
The biomechanical implications of anterior root tears are markedly less studied than those of posterior root tears. The consequences of AL root detachment were highlighted in a study by Espejo-Reina et al, 48 who reported decreased contact areas and increased peak contact pressures at low knee flexion angles, similar to those of a lateral meniscectomy. For the medial meniscus, a similar impairment of contact mechanics may be expected, as Costa et al 36 reported approximately 90% of medial meniscal extrusion (MME) greater than 6 mm after AM root tears—seeing that extrusion itself is associated with the progression of degenerative joint disease.103,148
The anatomy of the posterior root attachments was thoroughly described by Johannsen et al. 86 The PM root attachment is described as located 9.6 mm posterior and 0.7 mm lateral to the apex of the medial tibial eminence. The “shiny white fibers” comprise up to 60% of the overall PM root area and lie in proximity to the fibers of the posterior cruciate ligament (PCL). 86 A laboratory study by LaPrade et al 130 highlighted this relation, reporting the potential for iatrogenic damage to the PM root during tibial tunnel reaming for PCL reconstruction. The PL root is described as located 4.2 mm medial and 1.5 mm posterior to the apex of the lateral tibial eminence. 86 Although infrequent, the PL root may be damaged during ACL tibial tunnel reaming, and we found 1 case report of iatrogenic injury during tunnel reaming for the posterolateral bundle during double-bundle ACL reconstruction. 127
Biomechanically, evidence of the deleterious consequences of tears to the posterior root attachments of the medial and lateral menisci is overwhelming. ¶¶ A landmark study by Allaire et al 6 on PM root tears highlighted not only altered knee kinematics—in the form of significantly increased lateral tibial translation and external rotation—but also massively impaired contact mechanics, with peak contact pressures in the medial compartment akin to those found after a medial meniscectomy. Injury to the peripheral circumferential fibers of the meniscus, characteristic of root tears, ultimately leads to significant meniscal extrusion,49,171 compounding the potential for OA progression. 46 When combined with an injury to the ACL, a PM root tear may potentiate the overloading effect of an increased tibial slope on ACL graft strain.16,185 Aside from causing compromised contact mechanics and the potential for extrusion, tears to the PL root attachments generate significant increases in knee laxity. 188 Smith et al 188 reported a significant increase in anterior laxity during both the anterior-drawer test and the pivot-shift test in a concomitant PL root injury relative to an isolated ACL group. These findings further highlight the role of the lateral meniscus as a secondary stabilizer. 57
Etiology
Meniscus root tears occur in both acute and chronic settings as well as an iatrogenic manner. Acute injuries more commonly occur in the setting of traumatic insult, whereas chronic injuries frequently result as a consequence of degenerative OA. 82 Acute traumatic injuries to the meniscus root often occur in younger patients with knee hyperflexion and rotatory blow or with concomitant ligamentous injury, most commonly injury of the ACL.82,86,154 Older patients tend to present with chronic meniscus root injuries that occur as a consequence of degenerative OA and low-energy mechanisms.139,173
Etiology and mechanism of injury also vary between the 2 locations of meniscus root tears. Tears of the lateral meniscus root are commonly reported with a history of trauma, with Koo et al 109 demonstrating this association in up to 95% of cases. Moreover, a large majority of patients with lateral meniscus root tears (LMRTs) experience concomitant injuries of the ACL.109,127 Koo et al found that 95% of patients with verified tears of the lateral meniscus root also had simultaneous tears of the ACL. Karpinski et al 93 demonstrated that this relationship occurred in 82.4% of patients. The rate with which these 2 injuries are associated varies significantly from the rate at which medial meniscus root tears (MMRTs) and ACL tears are associated. It has been shown that these injuries occur in a concomitant manner in only 5.7% to 13.6% of cases.93,109
Iatrogenic injury to the meniscus roots during surgical procedures of the knee is an underrecognized complication and diagnostic dilemma in patients with residual symptoms after initial surgery. During ACL reconstruction, malpositioning of the tibial tunnel can result in inadvertent damage to the meniscus roots, particularly the AL root. Moreover, cadaveric studies have demonstrated significant reduction in AL root strength and attachment area after anatomic ACL tibial tunnel reaming.129,130 This may occur due to the considerable (41%-63%) overlap between the ACL and AL root footprints.122,192 Clinically, increased risk of lateral meniscal extrusion after ACL reconstruction has been associated with excessive lateralized tunnel trajectory. 169 Iatrogenic tears of the AL root after ACL reconstruction were first noted by LaPrade et al 125 in a series of case reports.
Injury to the posterior meniscus roots may also occur during transtibial drilling for PCL reconstruction.20,96 In a laboratory study, reaming of a tibial tunnel in the center of the PCL footprint resulted in significantly decreased strength and area of the posterolateral root attachment. 129 Clinically, malpositioned PCL tunnels have been reported to cause detachment of the posterior roots.95,96,130
Although key steps in surgical technique may mitigate the risk, it is evident that iatrogenic meniscus root tears represent an underrecognized complication across common knee operations. Awareness and vigilance are needed to avoid meniscus root injury during surgery as well as to detect and address iatrogenic injury postoperatively.
Location of Tears
Of the studies included in the review, 67% specifically discussed medial meniscus posterior root tears (MMPRTs). Given that only 18% of included studies reported on lateral meniscus posterior root tears (LMPRTs), it is evident that research on meniscus root tears has predominantly centered on the most common anatomic location of injury. It is worth noting that 9.5% of studies included in the present review reported on both MMPRTs and LMPRTs. Within the scope of the included studies, the medial meniscus anterior root was discussed in 1% of studies, the lateral meniscus anterior root in 0.7% of studies, and both the medial and lateral meniscus anterior root in 0.4% of studies. A discussion surrounding all possible anatomic locations of meniscus root tear was found in 3.4% of studies.
Although 43 studies included in the present review discussed both MMRTs and LMRTs, only 5 studies1,40,93,109,111 directly compared these 2 locations of meniscus root tears. The study design varied, as 3 studies were retrospective and 2 were prospective. The studies also varied by geographic origin, with 2 studies originating from the United States, 1 study from Norway, 1 study from Germany, and 1 study from the Republic of Korea. All of these studies were published between 2015 and 2023.
Significant differences were seen in patient characteristics and demographics between patients with MMRTs and LMRTs. Studies consistently demonstrated that patients who experienced tears of the medial meniscus root tended to be significantly older than patients with LMRTs, with a mean age of 52 and 30 years, respectively.93,109,111 Furthermore, MMRTs have been found to be associated with a higher body mass index.93,109,111 Interestingly, Krych et al 111 found that tears of the medial meniscus root occurred more frequently in female patients, whereas tears of the lateral meniscus root occurred more often in male patients.
Meniscal extrusion is a significant predictor of OA progression of the knee.31,46 Similar to the degree of meniscal extrusion, differences in OA incidence and severity between MMRTs and LMRTs have been demonstrated, and MMRTs are associated with significantly more severe OA as demonstrated by the rate and degree of concomitant cartilage damage in the affected compartment.93,109,111 Krych et al 111 demonstrated that patients with MMRTs had a higher Kellgren-Lawrence grade at the time of presentation, and Koo et al 109 reported that OA more frequently occurred in patients with MMRT than in patients with LMRT. Karpinski et al 93 studied a cohort of 104 patients, of whom 53 and 51 patients were diagnosed with MMRT and LMRT, respectively. Those authors found that mechanical varus angle was significantly higher in patients with MMRTs (5.6°) than in patients with LMRTs (2.4°) and that patients with MMRTs and a higher varus angle also showed more severe OA.
It has been shown that patients who have MMRTs and LMRTs differ in demographic characteristics and associated injuries.93,109,111 Two studies93,111 included in the present scoping review demonstrated that laterality of meniscus root tears also influences treatment outcomes. Krych et al 111 reported that patients who underwent lateral meniscus posterior root repairs had significantly better International Knee Documentation Committee (IKDC) and Tegner scores compared with patients who underwent repair of medial meniscus posterior root repairs. We posit that this may be due to significant differences in patient characteristics between the 2 cohorts, although no definitive explanation has been determined. Studies have reported that 82.4% to 95% of LMRTs occur with concomitant ACL injuries and are repaired simultaneously, so this may affect recovery and outcomes.93,109 Although a significant correlation between older age and decreasing outcome scores was found, previous literature has demonstrated that patients younger than 50 years had similar outcomes as those older than 50 years after undergoing meniscus root repair. 136 However, in the study by Krych et al, 111 the mean age of patients who underwent repair was 29 years. This contributes to the notion that the use of age as a predictor of surgical success after meniscus root repair must be investigated further.
Diagnosis
Clinical
Although physical examination of the knee is a necessary component of the diagnostic workup and critical to suspecting a meniscus root tear, such examination is only moderately effective in revealing the possibility of a tear. Clinical diagnosis is challenging given that patients with root tears do not always present with the typical signs and symptoms associated with a meniscus body injury. Lee et al 144 reported that patients with MMPRTs experienced sensations of their knees locking and giving way only 14.3% and 9.5% of the time, respectively. This same study reported that the 2 most common clinical manifestations found in patients with MMPRTs were pain on full flexion and joint-line tenderness, with an incidence of 66.7% and 61.9%, respectively. 144 Interestingly, a positive McMurray test was found in only 57.1% of patients with MMPRTs. 144 Overall, 50%-60% of patients with meniscus root tears show a combination of a positive McMurray sign, pain on deep flexion, and evidence of meniscal extrusion on palpation.82,186
In the present review, only 10 of the analyzed studies ## (2.2%) specified the clinical signs and symptoms that guided their diagnosis. Joint-line tenderness and posterior knee pain with deep flexion were among the most frequently reported signs. Having a history of a painful popping event in the knee was commonly mentioned as a positive clinical finding. Bae et al 11 evaluated the accuracy of a single event of painful popping for diagnosing MMPRT and found this to have a sensitivity and specificity of 35.0% and 99.5%, respectively, with a diagnostic accuracy of 77.9%. Additional signs and symptoms described in the literature included load-dependent pain, a positive McMurray test, and the inability to fully squat. Akmese et al 5 described a novel sign, called the “Akmese sign,” which was defined as severe medial joint-line tenderness in near extension and minimal or no tenderness in knee hyperflexion, when the knee has a slight varus position. A sensitivity of 86.1% and specificity of 99.1% were demonstrated for the sign, 5 although no further studies have confirmed or mentioned it.
Imaging
Regarding imaging methods, magnetic resonance imaging (MRI) emerged as the primary diagnostic tool, being noted in 233 studies (50.5%). Although MRI was overall the most commonly used modality for assessing meniscal pathology, literature assessing the sensitivity and specificity of MRI in diagnosing meniscus root tears is still limited. Of the 233 studies, only 22 studies a (9.4%) evaluated MRI diagnostic performance.
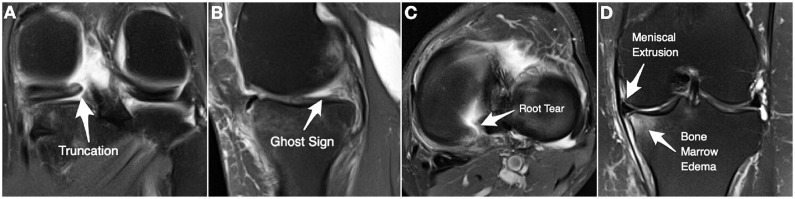
The sensitivity and specificity of MRI for diagnosing MMPRT have been reported as 79%-94% and 80%-100%, respectively, whereas for LMPRT, the figures stand at 60%-94% and 89%-100%, respectively. A 2015 study by LaPrade et al 134 evaluated the diagnostic accuracy of 3.0-T MRI and particularly highlighted the lower sensitivity for diagnosing LMPRT. The authors found that this imaging method had moderate sensitivity and specificity for the detection of posterior meniscus root tears. The negative predictive value and positive predictive value were high and low, respectively. Interestingly, the sensitivity was lower for LMPRT compared with MMPRT. The study concluded that although many root tears may be identified via imaging methods, such as 3.0-T MRI, some tears may be seen only via arthroscopy. 134 When specifically evaluating lateral roots, Minami et al 155 assessed different MRI signs, reporting sensitivity as low as 10.3% when discussing the ghost sign, which is defined as the absence of normal meniscal signal in the sagittal plane (Figure 7), and up to 69.2% when evaluating a vertical line seen in the coronal view, whereas specificity showed more consistent values ranging from 85.5% to 100%. Notably, that study evaluated the diagnostic performance of individual signs. De Smet et al 38 evaluated signs individually, which were then used in combination for diagnosing LMRT. Their study showed that this combination improved diagnostic performance and reached a sensitivity of 84.4% and a specificity of 90.5%.
Figure 7.
Magnetic resonance image of a left knee demonstrating (A) truncation, (B) ghost sign, (C) root tear, and (D) meniscal extrusion and bone marrow edema.
When evaluating diagnostic performance of MRI for MMPRT, the current literature reports higher sensitivity (90% to 96.7%) and specificity (96.7% to 100%) for detecting a radial tear on the axial view, the truncation sign on the coronal view, and the ghost sign on the sagittal view (Figure 7). 29 Several studies have also explored diagnosing MMPRT based on meniscal extrusion (Figure 7), with Park et al 174 demonstrating 79% sensitivity and 86% specificity using an extrusion ratio threshold of 10%. Similar results were reported by Kwak et al, 118 who found a sensitivity of 69% and specificity of 82.9% when using a cutoff value for the meniscal extrusion–medial femoral condyle ratio of 0.08. However, the diagnostic sensitivity was lower in the study by Choi et al 29 (63.3%), with a specificity of 90%. When medial and lateral meniscus roots are examined, there are differences in how often meniscal extrusion occurs and the grade at which it occurs. It has been demonstrated that meniscal extrusion occurs in 81% to 86.8% of patients with MMRT, whereas meniscal extrusion is seen in only 5% to 15.7% of those with LMRT.93,109 Koo et al 109 reported that injuries of the medial meniscus root caused a greater degree of extrusion, with a mean extent of 4.2 mm, compared with a mean of 0.9 mm for LMRT.
Interestingly, Qardash et al 179 demonstrated that performing MRI with the knee in a varus stress position could increase the diagnostic performance for MMPRT based on meniscal extrusion to 95.24% sensitivity and 80.0% specificity.
Among other imaging modalities, computed tomography was reported in 16 studies b (3.5%), although the purpose of these scans extended beyond evaluating meniscus root pathology to encompass factors like limb alignment and tibial rotation preoperatively, OA grade, present cases of root avulsion fractures, and postoperative evaluation of tibial tunnels. Furthermore, 7 studies24,39,43,50,79,92,184 (1.5%) reported using ultrasound, of which 1 study 24 even investigated the diagnostic performance of detecting meniscal extrusion on ultrasound for diagnosing MMPRT and reported a sensitivity of 76% and a specificity of 73.6% in Japanese patients with medial knee pain. Radiographs were reported as being used in 64.1% of the studies included in this review and were primarily indicated for assessing OA level and limb alignment.
Treatment
Operative Versus Nonoperative Management
Five studies2,15,40,113,146 directly compared outcomes of operative versus nonoperative management of meniscus root tears. All 5 of the studies were retrospective in nature, with 2 being cohort studies and the remaining 3 being comparative studies. Three studies were from the United States, and 2 were from the Republic of Korea. All of the studies were completed between 2015 and 2021. The conclusion of whether surgical management or nonoperative management was favored depended on the type of surgical procedure. Krych et al 113 and Lee et al 146 compared partial meniscectomy versus nonoperative management. Although Lee et al found that partial meniscectomy and nonoperative treatment provided symptomatic relief, these investigators also found that partial meniscectomy led to worse progression of OA. Thus, both studies found no advantage to partial meniscectomy over nonoperative management in clinical outcomes or OA progression.113,146
Three studies2,15,40 compared outcomes of root repair versus nonoperative treatment. Bernard et al 15 and Ahn et al 2 compared transtibial pullout root repairs versus nonoperative treatment, and both studies reported better clinical outcomes in the operative groups. Bernard et al 15 also compared root repairs versus partial meniscectomy as well as nonoperative treatment and reported that root repair had the lowest rate of OA progression and total knee arthroplasty, whereas partial meniscectomy had the highest rate. Ahn et al 2 reported similar outcomes between the root repair group and nonoperative group in patients with severe varus alignment or severe cartilage degeneration and recommended other treatment options for this group.
Dragoo et al 40 compared all-inside repair of meniscus root tears versus nonoperative treatment in older patients with moderate OA. These authors found lower rates of OA progression and total knee arthroplasty in the operative group as well as improved patient-reported outcomes. 40
Nonoperative Management Outcomes
Four studies described outcomes of nonoperative treatment of posterior MMRTs without a direct comparison to operative treatment: 1 study 116 was from the United States, 1 study 162 was from India, and 2 studies25,149 were from the Republic of Korea. Three of the studies were retrospective, and 1 was a prospective cohort study. The prospective study, by Neogi et al, 162 found that with supervised physical therapy followed by a home-based program and a short course of analgesics, patients had symptomatic and functional improvement but also had progression of OA over a mean 2-year follow-up. Lim et al 149 had similar findings in a retrospective study, reporting symptomatic relief and improved outcomes in patients with root tears treated nonoperatively, with 2 years of follow-up. However, Lim et al 149 noted that clinical improvement was highest at 12 months before declining to a level that was still above initial scores at final follow-up. Choi et al 25 used a mean follow-up of 46 months and found that nonsurgical treatment for acute MMPRTs did not result in any significant change in clinical outcomes. Choi et al 25 reported a 36% rate of OA progression and a 13% rate of conversion to arthroplasty. Krych et al 116 had the longest mean follow-up time at 5 years and found that nonoperative treatment was associated with poor clinical outcomes, worsening arthritis, and increased rate of arthroplasty. The 2 studies that had the longest follow-up (Choi et al 25 and Krych et al 116 ) were also the most recently published (in 2023 and 2017, respectively). All 4 of these studies appear to show a potential pattern of early improvement followed by a progressive decline in clinical outcomes and worsening of OA. More long-term studies may help to determine whether this is the true course regarding nonoperative management of MMPRTs.
Surgical Technique
Of the 461 full texts reviewed, 346 (75%) discussed surgical technique. Transtibial repairs were evaluated in 221 of the studies, 47 discussed the all-inside repair technique, 35 reviewed suture anchor fixation, 22 made direct comparisons of ≥2 techniques, 14 evaluated either meniscectomy or meniscal debridement, 2 focused on osteotomy alone, and 5 discussed several surgical techniques without comparative analysis.
Transtibial Repair
Of the studies that assessed transtibial repair, 50 were technique notes, 56 were case reports or case series, 35 were cadaveric biomechanical studies, and the remainder were cohort studies, case control studies, and imaging review studies. Of the included studies, 6 studies1,58,61,75,106,166 compared outcomes of different types of transtibial repair.
Three studies75,106,166 noted superior outcomes with the 2-simple-suture technique. Okazaki et al 166 compared outcomes of arthroscopic pullout repair with the 2-simple-suture technique versus the modified Mason-Allen technique and found that although both techniques resulted in improved clinical scores, the 2-simple-suture technique performed superiorly in regard to loading stress on the posterior horn of the medial meniscus. Hiranaka et al 75 assessed medial meniscal extrusion on MRI, comparing the 2-simple-suture pullout repair technique versus the modified Mason-Allen technique. These authors found less postoperative meniscal extrusion and better clinical outcomes with the 2-simple-suture repair compared with the modified Mason-Allen technique. Kintaka et al 106 found that both the 2-simple-suture repair and the modified Mason-Allen suture technique decreased PM meniscal extrusion during knee flexion; however, the modified Mason-Allen technique led to increased extrusion with the knee in extension. Kintaka et al 106 concluded that the 2-simple-suture repair would be more beneficial in terms of distribution forces during weightbearing and ambulation.
Furumatsu et al 61 evaluated clinical outcomes and healing scores after 2-simple-suture repair, 2-simple-suture with additional posteromedial suture, and modified Mason-Allen sutures. The investigators concluded that the additional posteromedial suture did not confer any additional advantage compared with the other 2 techniques. Fujii et al 58 compared load-to-failure rates of 2-simple-suture repair versus the modified Mason-Allen technique in animal models with posterior MMRTs. The investigators reported lower failure load with 2-simple-suture repair compared with the modified Mason-Allen technique.
A 2021 study by Aga et al 1 directly compared outcomes of transtibial meniscus root repair in patients who had injuries to the posterior roots of the meniscus. The authors reported that at 1-year follow-up after repair, 61.1% of patients with LMPRTs were classified as healed via MRI, whereas only 27.7% of patients with MMPRTs were classified as healed. Interestingly, despite surgical intervention, there was a significant increase in meniscal extrusion, from 3.1 ± 1.6 mm to 4.8 ± 1.9 mm at 1-year follow-up. The authors reported no differences between the 2 groups in terms of Knee injury and Osteoarthritis Outcome Score, Lysholm score, or global rating of change (GROC) score for function, although Tegner activity scale was higher and GROC score for pain was lower in the LMPRT versus the MMPRT group. 1
Overall, the studies reviewed found that both 2-simple-suture repair and the modified Mason-Allen technique were successful methods of repairing PM meniscal tears, with the 2-simple-suture being more advantageous in regard to avoiding postoperative meniscal extrusion.
All-Inside Repair
Of the studies that evaluated all-inside repair, 20 were technical notes, 8 were biomechanical cadaveric or animal studies, and the remainder were cohort studies or case series. Outcomes of all-inside repair were largely favorable among the included studies. Dragoo et al 40 analyzed outcomes of arthroscopic all-inside repair and nonoperative management for both medial and lateral meniscal tears among patients with moderate OA. The investigators found that all-inside repair resulted in better postoperative outcomes compared with nonoperative treatment and had lower risk of arthroplasty. Ahn et al 4 assessed outcomes of all-inside repair of PL meniscus root tears by comparing preoperative and postoperative MRI scans, reporting less lateral meniscal displacement on sagittal MRI scans after all-inside repair. Suh et al 194 concluded that all-inside medial meniscus posterior root repair in addition to high tibial osteotomy (HTO) had better outcomes compared with HTO alone in regard to preservation of joint space. When considering healing of all-inside root repair in patients with normal lower extremity alignment, Jiang et al 84 found that all-inside repair of posterior MMRTs to the PCL had acceptable outcomes. Zhu et al 211 found high rates of meniscal healing after all-inside repair of MMRTs but noted increased extrusion. Jung et al 89 noted incomplete meniscal healing after all-inside repair on postoperative MRI analysis.
Only a minority of the included studies reported adverse outcomes with all-inside repair, including postoperative meniscal extrusion and incomplete meniscal healing. Overall, all-inside repair was shown to be an effective method of addressing meniscus root tears.
Meniscectomy
Of the 14 studies on meniscectomy, c 2 studies were case series, 1 study was a case control study, and the remainder were retrospective cohort studies. The majority of included studies found that meniscectomy as a treatment for meniscal tears did not have superior outcomes compared with nonoperative treatment and in some cases led to progression of arthritis.
For example, Han et al 68 found that 35% of the patients included in their study who underwent partial meniscectomy had progressive arthritis on imaging at a mean follow-up of 6 years. Lee et al 146 found that both nonoperative management and meniscectomy improved preoperative symptoms; however, the investigators noted that meniscectomy resulted in a greater degree of OA progression compared with nonoperative management. When considering lower extremity alignment, a different group, Lee et al, 138 evaluated risk factors for MMPRTs and outcomes of meniscectomy and found that meniscectomy led to better outcomes and was considered a viable salvage option in patients with well-aligned knees compared with patients who had varus knees.
Considering the results of the studies as a whole, meniscectomy has not been shown to have superior outcomes compared with nonoperative management and can actually lead to increased risk of OA progression.
Direct Comparison of Techniques
There were 22 studies d that made direct comparisons between fixation techniques; 8 studies were retrospective cohort or comparative studies, 7 were biomechanical studies, 3 were case-control studies, 2 were case series, and 2 were prospective cohort studies. The most common comparisons were suture anchor repair versus transtibial pullout repair, all-inside repair versus partial meniscectomy, transtibial pullout repair versus partial meniscectomy, and all-inside repair versus transtibial pullout repair.
In a biomechanical study, Chung et al 30 compared transtibial pullout repair with simple sutures, transtibial pullout repair with modified Mason-Allen sutures, and all-inside repair and found that transtibial repair with modified Mason-Allen technique provided the best surface contact area in porcine knees. Yoon et al 207 compared imaging outcomes of transtibial pullout repair and all-inside repair of MMPRTs in a retrospective study. These investigators found that the patients who underwent all-inside repair demonstrated better healing and signal intensity improvement on MRI compared with the transtibial pullout repair group. Additionally, although both repairs were associated with meniscal extrusion 1 year postoperatively, the extrusion ratio was lower in the all-inside repair cohort. Yoon et al noted that there was no significant difference in clinical outcome scores between patients in the transtibial pullout repair group and the all-inside repair group. Dzidzishvili et al 41 compared transtibial pullout repair versus all-inside repair for MMPRTs in a retrospective case-control study and concluded that both techniques led to favorable clinical outcomes. Functional outcomes and radiological progression of arthritis did not differ significantly between the 2 groups postoperatively. 41
Su et al 193 compared nonanatomic trans-PCL all-inside suture repair versus partial meniscectomy for posterior MMRTs in a retrospective imaging study. The investigators observed less advancement of articular cartilage damage and lower rates of meniscal extrusion postoperatively in the all-inside repair group compared with the partial meniscectomy group. When comparing transtibial pullout repair versus partial meniscectomy and nonoperative management of posterior MMRTs in a retrospective study, Bernard et al 15 concluded that repair resulted in less arthritis progression and lower need for conversion to arthroplasty. Considering the results of these studies, it appears that repair in general, whether nonanatomic with all-inside devices or anatomic transtibial pullout, leads to superior postoperative outcomes when compared with meniscectomy.
Feucht et al 52 conducted a biomechanical comparison in a porcine model measuring load to failure and displacement after suture anchor repair and transtibial pullout repair in models with posterior MMRTs, reporting no significant difference in maximum load to failure or displacement after failure between the 2 groups. Suture anchor fixation demonstrated superior stiffness and a lower degree of displacement before failure, but neither fixation technique matched the inherent strength of a native meniscus. When comparing suture anchor repair and transtibial pullout for posterior MMRTs in a prospective study, Kim et al 101 found no significant differences in clinical outcomes between the 2 techniques. Both methods led to improved functional outcomes, and they had similar rates of complete healing and meniscal extrusion postoperatively. 101 In considering these findings, it appears that both transtibial pullout and suture anchor fixation can lead to favorable outcomes.
Centralization
The concept of augmenting meniscus root repairs with a centralization (peripheral stabilization) stitch has emerged in recent years as an adjunctive strategy aimed at correcting residual meniscal extrusion. Extrusion is concerning given its association with inferior outcomes after repair and accelerated cartilage degeneration.19,46,69,76 Anatomic root fixation alone often does not fully correct extrusion,7,28 likely reflecting involvement of additional factors such as medial collateral ligament tightness or plastic deformation of the extruded meniscus.137,150 This issue has prompted interest in techniques that address extrusion through suturing and anchoring the meniscus body to the tibial plateau.
Initial cadaveric and clinical studies on medial meniscal centralization combined with root repair have shown encouraging results. Biomechanical evidence has demonstrated that addition of a centralization stitch helps minimize meniscal extrusion and better restores contact mechanics compared with root repair alone.37,108,115,170 Small clinical series have reported favorable outcomes at short-term follow-up when centralization is performed along with root fixation.156,170 For example, Mochizuki et al 156 reported significantly decreased extrusion ratio and improved clinical scores at 2 years after medial meniscus root repair with centralization. Comparable benefits with lateral meniscal centralization have likewise been shown. 107
Although initial studies support the potential for centralization to provide added protection against persistent extrusion, long-term clinical evidence is still needed. 170 Additionally, concerns exist regarding the technical difficulty of the procedure as well as risks of overconstraining the meniscus,137,150 and the optimal indications and techniques for centralization require further clarification. Some authors advise routine centralization for all root repairs, 137 whereas other guidelines reserve centralization for cases with major preoperative extrusion exceeding 3 to 5 mm.150,170 Nevertheless, the arthroscopic centralization concept represents an encouraging contemporary adjunct that merits continued investigation as a strategy to improve upon standard root repairs.
Operative Treatment With Osteotomy
Of the 461 studies analyzed in the present scoping review, 36 studies (7.8%) reported including an osteotomy as part of the treatment when the patient had varus alignment associated with MMRT. Among this group, 9 studies e (25%) analyzed the postoperative outcomes after osteotomy.
As reported by Jing et al, 85 patients who had MMPRT and concomitant varus alignment achieved promising clinical results at 18-month follow-up when treated with a medial opening-wedge HTO (MOWHTO) combined with all-inside repair of the MMPRT. Similar results were reported by Kim et al, 104 where 17 patients who had MMPRT, varus alignment, and medial Kellgren-Lawrence grade of <3 were treated with HTO and a remodified Mason-Allen suture technique repair of the root tear. The investigators showed significantly better clinical outcomes after surgery, no changes in Kellgren-Lawrence grades after a mean of 66 months, and 64.7% complete healing rates at second-look arthroscopy 2 years after surgery. Rocha de Faria et al 183 also reported improved clinical and functional outcomes when performing MMPRT repair alone or with associated HTO, although their study entailed only 6 months of follow-up and did not include comparisons between the groups.
Ridley et al 181 retrospectively analyzed cases of MMPRT repairs and found that neutral preoperative alignment correlated with better outcomes. Moreover, their study reported that patients with preoperative varus alignment who underwent concomitant HTO presented worse outcomes even when compared with patients without HTO and with >5° of varus alignment. 181
Itou et al 80 evaluated outcomes after MMPRT repair with associated MOWHTO for patients with preoperative varus alignment (>4°) and for patients with what the authors called “moderate varus alignment” (<4°). After surgery, alignment in all patients was taken to −2.7° or −3.7°, achieving good clinical and functional outcomes with no differences between the patient groups. The authors concluded that HTO should be considered for patients who have MMPRT even when their limb alignment is <4° varus.
Lee et al 143 sought to assess the efficacy of MOWHTO in treating patients who presented with MMPRT without actually performing MMPRT repair. The authors reported improved clinical outcomes after surgery, although a second-look arthroscopy revealed a low rate of healing potency of the root tear repair and cartilage in patients who underwent osteotomy alone. Similarly, Jing et al 85 reported that despite having good clinical outcomes after osteotomy and repair, 59% of patients treated with HTO and MMPRT repair presented lax healing at second-look arthroscopy, and the investigators concluded that the healing of the root was not related to an improved clinical outcome.
Some clinical studies found in the literature compared isolated HTO versus HTO and MMPRT repairs as possible treatments for patients with MMPRT.94,141,147 No significant differences in clinical or radiological outcomes at 2 years postoperatively were reported. Higher healing rates of the posterior root tear were reported when MMPRT repair was performed concomitantly. However, the repair of the root was not related to the postoperative radiological and clinical outcomes, and therefore there is no clear evidence of the need to perform the MMPRT repair during an opening-wedge HTO. 147
Early Versus Delayed Surgery
Of the 461 full texts included in this review, 101 (21.9%) mentioned the timing between injury and surgical intervention for meniscus root tears. Only 6 of those studies63,91,118,153,157,165 reported on early versus delayed timing of surgery. Four of the studies were from Japan, and 2 studies were from the Republic of Korea. All were retrospective studies, with level of evidence 3 or 4, and were completed between 2017 and 2022. Each of these studies recommended early surgical repair, but only 2 studies defined a time cutoff that constituted an “early” intervention. Most studies used MME measurements to track the progression of root tears and as a marker for worse outcomes, based on the relationship of MME to the progression of knee OA. 56
In 2017, Furumatsu et al 63 reported that “MME increased progressively within the short period after the onset of symptomatic MMPRT” and recommended early diagnosis and treatment. They also suggested that future studies aim to determine precise timing of treatment. Moon et al 157 used the receiver operating characteristic curve from their data to determine the optimal cutoff point and found 13 weeks to be the most sensitive and specific. Using this cutoff, Moon et al 157 found that patients with early surgical treatment had improved clinical outcomes, which the investigators credited to decreasing MME progression. Using a linear regression model, Kamatsuki et al 91 applied a cutoff value of 112 days and found that early transtibial pullout repair was more effective in reducing MME; the investigators recommended repair as soon as possible unless the patient already had severe OA. Masuda et al 153 looked at patients who had root tear as well as mild OA and a mean time to surgery of 63 days. The investigators found that transtibial pullout repair improved clinical outcomes and recommended that these patients undergo early repair. This study was limited by lack of a direct comparison to a group that underwent delayed repair, thus not being able to define a cutoff time of early versus late. 153
Kwak et al 118 and Okazaki et al 165 also failed to define a cutoff time while recommending that patients with MMPRT receive early repair. Kwak et al made this recommendation for patients with large MME who were treated nonoperatively, after finding that MME was a reliably poor prognostic factor. Okazaki et al made this recommendation after finding that “early diagnosis of MMPRT and pullout repair can prevent severe MME and high-grade [subchondral insufficiency fracture of the knee].” In the group of women they studied, Okazaki et al found that prolonged MMPRT not only could lead to MME but also could lead to subchondral insufficiency fracture of the knee. Interestingly, the investigators also found that posterior shiny corner lesions may be useful in identifying patients with early MMPRT, especially in those who did not have a painful popping event.
Overall, these studies indicated agreement that early surgical management is preferred in most patients with MMPRT; however, a clearly defined cutoff time of early versus late could be useful in clinical decision-making. Additionally, future studies could investigate the timing of surgery in other locations of meniscus root tears, such as LMPRT, since this review only found studies describing MMPRT surgical timing.
Rehabilitation
A total of 169 studies (36.7%) in this review described rehabilitation protocols, and no significant variances were found among them.
Regarding postoperative weightbearing, all protocols agreed that full weightbearing is not recommended until 6 weeks after surgery. However, there were some variations: Some authors indicated nonweightbearing for the entire first 6 weeks, whereas others recommended nonweightbearing for 2 weeks, followed by partial weightbearing from 2 to 6 weeks. Others even indicated partial weightbearing from day 1 until week 6.
With respect to knee braces, the prevailing recommendation was that patients wear a hinged-knee brace for the first 2 weeks, although some authors recommended a brace for the first 6 weeks. Some studies also included using an unloader brace starting 6 weeks after surgery, when full weightbearing would start, in order to protect the repaired meniscus root.
In the context of range of motion, all studies permitted initiation of rehabilitation from postoperative day 1. However, there were slight variations in the projected timelines for patients to attain 30°, 60°, 90°, or 120° of flexion. Nevertheless, a general consensus emerged that patients were anticipated to achieve 90° of flexion by the 4-week mark and to surpass 120° without loading by the 6-week juncture. Concerning squatting, certain studies sanctioned its resumption at the postoperative 3- or 4-month mark, whereas others advised against its practice altogether.
The majority of studies permitted patients to commence a gradual return to running within 3 to 4 months postoperatively, followed by a return to sport around the 6-month mark.
Discussion
This methodologically rigorous scoping review describes the current literature on the diagnosis and management of meniscus root tears. In doing so, this review highlights current controversies and identifies areas in the literature that can be explored further with future research. The breadth of this scoping review helped establish the identification of several notable findings related to the occurrence, diagnosis, and treatment of meniscus root tears.
One issue that was evident in the present review was the predominantly low level of evidence on which our knowledge base on meniscus root tears is built. Although the relatively recent focus on root tears may account for this limitation, we must strive to implement higher quality prospective designs in future investigations.
Patient demographic factors such as age and sex were found to have significant relationships to the locations of meniscus root tears, with LMPRTs occurring more frequently in men 111 and younger patients. 139 The younger age of those with LMPRTs may help to explain the findings of decreased meniscal extrusion, decreased OA severity, and better IKDC scores after repair. Further research is needed to investigate the effects of age on success of surgical root repair by looking at these factors. Race and ethnicity are other patient demographic characteristics, along with sex, that have been reported to potentially be associated with disparities in injury, treatment, and outcomes in other types of orthopaedic injuries175,176; however, only 2.17% of the studies reviewed here mentioned race and ethnicity. These disparities can best be identified if the patient data are included in published studies; therefore, improved demographic data collection should be a focus of future meniscus root studies so that these disparities may be elucidated and addressed. Limited data on how race and ethnicity may affect the outcomes of root tears, paired with the lack of studies from regions such as South America, Africa, and Eastern Europe, limit the external validity of the findings reported in the current literature.
The review of studies describing clinical signs and presentation of meniscus root tears shows the broad range of ways these injuries may present, which makes clinical diagnosis challenging.18,34 This is most likely why MRI was found to be the primary diagnostic tool among the studies that were reviewed. Despite being the most widely used imaging method, MRI had a wide range of sensitivity and specificity that were reported depending on the sign, position, or location of root tear that was being examined. Substantial variation exists in several aspects of the use of MRI, such as measurement techniques for meniscal extrusion, particularly as it relates to the coronal cross-sectional reference location, as highlighted by Farivar et al. 49 The limited diagnostic accuracy of both clinical and imaging examination makes it paramount that careful visualization and probing of the meniscus roots be added to the routine diagnostic inventory during knee arthroscopy. Further research into more effective clinical diagnostic and advanced imaging signs will help improve early diagnosis of meniscus root tears, given that preexisting alterations such as mild extrusion likely attributed to meniscotibial ligament attenuation have been reported. 114 This is important so that surgical intervention can be initiated as soon as possible after diagnosis.
Whether to operate on meniscus root tears, as well as when to operate, was largely agreed upon. Of the studies that included direct comparisons, the consensus was that repair of these tears had the best clinical outcomes and the least progression of OA. Although not as effective as repair, meniscectomy and nonoperative management had similar outcomes, but meniscectomy entailed much higher progression of OA.15,113,133,146 Of the studies investigating outcomes of nonoperative treatment, only 1 study 116 with long-term follow-up was included, and it showed poor clinical outcomes. The short-term studies found improved outcomes.149,162 More long-term studies are required to accurately describe the progression and outcomes of nonoperatively managed meniscus root tears. All studies describing the timing of surgery in MMPRTs agreed that early intervention is best, but only 2 of these studies91,157 included cutoff values of early versus late. Apart from establishing cutoff values of early and delayed surgery, future studies could investigate the timing of surgery in other locations of meniscus root tears, since this review found only studies describing MMPRT surgical timing.
Whether or when malalignment should be addressed remains controversial, and we found limited evidence on this topic. The studies describing HTO in MMPRTs found improved clinical outcomes when adding HTO in patients with varus alignment, with 1 study even recommending consideration of HTO in patients with <4° of varus. 80 Conflicting evidence is available on the topic, as Jiang et al 83 suggested that 5° of mechanical malalignment is the threshold for poor clinical outcomes, whereas Moon et al 158 demonstrated similar results after MMPRT repair in patients with mild or moderate varus (0° to 5°) versus patients with severe varus (5°-10°). One interesting finding of the present review was the agreement between several studies that compared HTO with meniscus root repair versus HTO without such repair. These studies demonstrated that despite higher meniscal healing rates in the repair group, there was no difference in radiological or clinical outcomes compared with the nonrepair group.94,141,147 These studies only included data up to 2 years postoperatively. Similar short-term results were seen in the studies of nonoperative management of meniscus root tears. Future studies should investigate long-term outcomes, progression of OA, and conversion to total knee arthroplasty in these patients.
Transtibial repair is the currently accepted gold-standard treatment for meniscus root tears, 150 and the interest in this technique was reflected in 68% of the technique studies included in this review. Many unique approaches and suture techniques for transtibial pullout repair were discussed. Several studies comparing the use of the 2-simple-suture technique versus the modified Mason-Allen technique consistently found them both to be effective but reported that the 2-simple-suture technique provided less meniscal extrusion, with the added benefit of being technically simpler in execution. f
The all-inside technique was also found to be effective in treating meniscus root tears and decreased the progression of OA compared with meniscectomy and nonoperative management. Across retrospective, case-control, and biomechanical study designs, when transtibial pullout and all-inside techniques were directly compared, both techniques appeared to be viable options with favorable postoperative and functional outcomes.30,41 Although biomechanical evidence supported anatomic transtibial repair as the superior technique, 30 surprisingly, Dzidzishvili et al 41 found better healing via MRI and a lower extrusion ratio in the all-inside technique groups. Although additional data and future prospective studies should shed further light on the direct comparison between techniques, we postulate that transtibial pullout repair may be less forgiving in technical execution, as deviations in tunnel placement as little as 5 mm are sufficient to compromise the resulting construct, 123 and knee surgeons as a collective are further along in the learning curve for repair using all-inside devices. This review did not find any randomized controlled trials comparing these techniques, which may provide an opportunity for future research.
Of the studies that presented rehabilitation protocols, a largely similar structure was seen for all protocols. Full weightbearing was not recommended until after 6 weeks in all of the protocols, but timelines for partial weightbearing, values for range of motion, and types of braces used had some slight variations. 160 The different mechanisms and associated injuries between LMRTs and MMRTs may help explain some of the discrepancies in rehabilitation protocols. Of note, the consensual emphasis on early nonweightbearing finds consonance in prior biomechanical evidence suggesting unrecoverable loosening of transtibial pullout MMPRT repair due to simulated early loading during rehabilitation. 190
Limitations
Limitations to scoping reviews like this one include that they are not exhaustive and do not discuss topics in depth. Instead, they provide a broad, contextual overview of the subject matter. Another possible limitation of this study is that 4 researchers conducted data extraction. Although a standardized form was used to collect extracted data and all researchers met to discuss relevant data to be extracted, this number of people increases the chance for variation in the process. Finally, the use of databases to pool relevant studies in this review is a limitation, as it has the potential to leave out older, relevant sources.
Conclusion
High-level evidence studies for diagnosing and managing meniscus root tears were scarce. We found consensus regarding the definition of meniscus root tears, the advantages of early repair, and postoperative rehabilitation protocols. A consensus has yet to be reached regarding the role of concomitant osteotomy, comparison of repair techniques, the use of a centralization stitch, patient factors affecting outcomes, and long-term outcomes of nonoperative management.
Supplemental Material
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241283962 for Diagnosis and Treatment Strategies of Meniscus Root Tears: A Scoping Review by Jose Rafael Garcia, Salvador Gonzalez Ayala, Felicitas Allende, Enzo Mameri, Monique Haynes, Filippo Familiari, Andrew G. Geeslin, Iain Murray, Gilbert Moatshe, Nikhil N. Verma, Robert F. LaPrade and Jorge Chahla in Orthopaedic Journal of Sports Medicine
References 23, 42, 47, 49, 51, 53, 56, 77, 81, 83, 97, 110, 121, 145, 182, 189, 199, 200, 203, 208, 209.
References 9, 10, 17, 24, 26, 27, 29, 43, 59, 60, 64, 71, 92, 115, 117, 134, 142, 155, 161, 167, 178, 179.
Footnotes
Final revision submitted March 18, 2024; accepted March 20, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.G.G. has received education payments from Arthrex and nonconsulting fees from Ossur and Smith+Nephew. I.M. has received consulting fees from Arthrex and Stryker. N.N.V. has received research support from Breg and Ossur, consulting fees from Arthrex and Stryker, royalties from Graymont Professional Products and Smith+Nephew, and hospitality payments from Spinal Simplicity. R.F.L. has received research support from Linvatec and Ossur, education payments from Foundation Medical, consulting fees from Ossur, nonconsulting fees from ConMed and Smith+Nephew, and royalties from Arthrex and Ossur. J.C. has received grant support from Arthrex; education payments from Medwest Associates and Smith+Nephew; consulting fees from DePuy Synthes, RTI Surgical, Ossur, and Vericel; nonconsulting fees from Arthrex and CONMED; and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
ORCID iDs: Jose Rafael Garcia  https://orcid.org/0000-0003-1092-3899
https://orcid.org/0000-0003-1092-3899
Felicitas Allende  https://orcid.org/0000-0001-9319-2571
https://orcid.org/0000-0001-9319-2571
Filippo Familiari  https://orcid.org/0000-0002-3453-2043
https://orcid.org/0000-0002-3453-2043
Supplemental Material: Supplemental Material for this article is available at https://journals.sagepub.com/doi/full/10.1177/23259671241283962#supplementary-materials.
References
- 1. Aga C, Aasen IB, Brocker C, Kise NJ, Heir S. Lateral meniscal posterior root tears experience acceptable healing status after transtibial repair technique. J Exp Orthop. 2021;8(1):114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahn JH, Jeong HJ, Lee YS, et al. Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg. 2015;135(9):1265-1276. [DOI] [PubMed] [Google Scholar]
- 3. Ahn JH, Lee YS, Chang JY, Chang MJ, Eun SS, Kim SM. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16(1):77-80. [DOI] [PubMed] [Google Scholar]
- 4. Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(1):67-75. [DOI] [PubMed] [Google Scholar]
- 5. Akmese R, Malatyalı B, Kocaoglu H, Akkaya Z, Kalem M. A new clinical sign for diagnosing medial meniscus posterior root tear. Orthop J Sports Med. 2021;9(1):2325967120975511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922-1931. [DOI] [PubMed] [Google Scholar]
- 7. Anderson L, Watts M, Shapter O, et al. Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy. 2010;26(12):1625-1632. [DOI] [PubMed] [Google Scholar]
- 8. Anz AW, Branch EA, Saliman JD. Biomechanical comparison of arthroscopic repair constructs for meniscal root tears. Am J Sports Med. 2014;42(11):2699-2706. [DOI] [PubMed] [Google Scholar]
- 9. Argin M, Dastan AE, Kaya Bicer E, Kaya H, Taskiran E. Stress radiography findings in medial meniscus posterior root tears. Knee. 2020;27(5):1542-1550. [DOI] [PubMed] [Google Scholar]
- 10. Asai K, Nakase J, Oshima T, Shimozaki K, Toyooka K, Tsuchiya H. Lateral meniscus posterior root tear in anterior cruciate ligament injury can be detected using MRI-specific signs in combination but not individually. Knee Surg Sports Traumatol Arthrosc. 2020;28(10):3094-3100. [DOI] [PubMed] [Google Scholar]
- 11. Bae JH, Paik NH, Park GW, et al. Predictive value of painful popping for a posterior root tear of the medial meniscus in middle-aged to older Asian patients. Arthroscopy. 2013;29(3):545-549. [DOI] [PubMed] [Google Scholar]
- 12. Banovetz MT, Roethke LC, Rodriguez AN, LaPrade RF. Meniscal root tears: a decade of research on their relevant anatomy, biomechanics, diagnosis, and treatment. Arch Bone Jt Surg. 2022;10(5):366-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bansal S, Floyd ER, Kowalski MA, et al. Meniscal repair: the current state and recent advances in augmentation. J Orthop Res. 2021;39(7):1368-1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Beaufils P, Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions: save the meniscus. Orthop Traumatol Surg Res. 2017;103(8S):S237-S244. [DOI] [PubMed] [Google Scholar]
- 15. Bernard CD, Kennedy NI, Tagliero AJ, et al. Medial meniscus posterior root tear treatment: a matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med. 2020;48(1):128-132. [DOI] [PubMed] [Google Scholar]
- 16. Bernholt D, DePhillipo NN, Aman ZS, Samuelsen BT, Kennedy MI, LaPrade RF. Increased posterior tibial slope results in increased incidence of posterior lateral meniscal root tears in ACL reconstruction patients. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3883-3891. [DOI] [PubMed] [Google Scholar]
- 17. Berthold DP, Muench LN, Herbst E, et al. High prevalence of a deep lateral femoral notch sign in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1018-1024. [DOI] [PubMed] [Google Scholar]
- 18. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016-3030. [DOI] [PubMed] [Google Scholar]
- 19. Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805-810. [DOI] [PubMed] [Google Scholar]
- 20. Cerminara AJ, LaPrade CM, Smith SD, Ellman MB, Wijdicks CA, LaPrade RF. Biomechanical evaluation of a transtibial pull-out meniscal root repair: challenging the bungee effect. Am J Sports Med. 2014;42(12):2988-2995. [DOI] [PubMed] [Google Scholar]
- 21. Chahla J, LaPrade RF. Meniscal root tears. Arthroscopy. 2019;35(5):1304-1305. [DOI] [PubMed] [Google Scholar]
- 22. Chahla J, LaPrade RF, Krych AJ, Verma NN, Cole BJ, Yanke AB. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees: letter to the editor. Am J Sports Med. 2019;47(10):NP53-NP54. [DOI] [PubMed] [Google Scholar]
- 23. Chang PS, Radtke L, Ward P, Brophy RH. Midterm outcomes of posterior medial meniscus root tear repair: a systematic review. Am J Sports Med. 2022;50(2):545-553. [DOI] [PubMed] [Google Scholar]
- 24. Chiba D, Sasaki T, Ishibashi Y. Greater medial meniscus extrusion seen on ultrasonography indicates the risk of MRI-detected complete medial meniscus posterior root tear in a Japanese population with knee pain. Sci Rep. 2022;12(1):4756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Choi BS, Chung J, Kwak J, Han HS. Subchondral insufficiency fracture is a predictive factor of osteoarthritis progression and conversion to arthroplasty in non-surgically treated medial meniscus root tear. Knee Surg Sports Traumatol Arthrosc. 2023;31(10):4492-4500. [DOI] [PubMed] [Google Scholar]
- 26. Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602-1606. [DOI] [PubMed] [Google Scholar]
- 27. Choi JY, Chang EY, Cunha GM, Tafur M, Statum S, Chung CB. Posterior medial meniscus root ligament lesions: MRI classification and associated findings. AJR Am J Roentgenol. 2014;203(6):1286-1292. [DOI] [PubMed] [Google Scholar]
- 28. Choi NH. Radial displacement of lateral meniscus after partial meniscectomy. Arthroscopy. 2006;22(5):575.e1-4. [DOI] [PubMed] [Google Scholar]
- 29. Choi SH, Bae S, Ji SK, Chang MJ. The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2098-2103. [DOI] [PubMed] [Google Scholar]
- 30. Chung KS, Choi CH, Bae TS, et al. Comparison of tibiofemoral contact mechanics after various transtibial and all-inside fixation techniques for medial meniscus posterior root radial tears in a porcine model. Arthroscopy. 2018;34(4):1060-1068. [DOI] [PubMed] [Google Scholar]
- 31. Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42-49. [DOI] [PubMed] [Google Scholar]
- 32. Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG. Root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of long-term survivorship and clinical outcomes at minimum 10-year follow-up. Am J Sports Med. 2020;48(8):1937-1944. [DOI] [PubMed] [Google Scholar]
- 33. Chung KS, Ha JK, Yeom CH, et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941-1950. [DOI] [PubMed] [Google Scholar]
- 34. Cinque ME, Chahla J, Moatshe G, Faucett SC, Krych AJ, LaPrade RF. Meniscal root tears: a silent epidemic. Br J Sports Med. 2018;52(13):872-876. [DOI] [PubMed] [Google Scholar]
- 35. Cinque ME, DePhillipo NN, Moatshe G, et al. Clinical outcomes of inside-out meniscal repair according to anatomic zone of the meniscal tear. Orthop J Sports Med. 2019;7(7):2325967119860806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17-23. [DOI] [PubMed] [Google Scholar]
- 37. Daney BT, Aman ZS, Krob JJ, et al. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47(7):1591-1600. [DOI] [PubMed] [Google Scholar]
- 38. De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480-486. [DOI] [PubMed] [Google Scholar]
- 39. Diermeier T, Tisherman RE, Wilson K, et al. The lateral meniscus extrudes with and without root tear evaluated using ultrasound. J ISAKOS. 2022;7(6):195-200. [DOI] [PubMed] [Google Scholar]
- 40. Dragoo JL, Konopka JA, Guzman RA, Segovia N, Kandil A, Pappas GP. Outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. Am J Sports Med. 2020;48(5):1127-1133. [DOI] [PubMed] [Google Scholar]
- 41. Dzidzishvili L, López-Torres II, Sáez D, Arguello JM, Calvo E. A comparison of the transtibial pullout technique and all-inside meniscal repair in medial meniscus posterior root tear: prognostic factors and midterm clinical outcomes. J Orthop. 2021;26:130-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Edwards C, Goldman BH, Turley J, Richey B, Deal MJ, Kalbac D. Outcomes after surgical repair of medial meniscal root tears: a review. J Knee Surg. 2021;34(14):1599-1602. [DOI] [PubMed] [Google Scholar]
- 43. Elkwesny GMM, Ali KAM, Sakr HMES, Ismael MGH. Role of musculoskeletal ultrasound in assessment of extrusion of the medial meniscus of the knee joint compared to MRI as a reference standard. Systematic Rev Pharm. 2020;11(12):534-540. [Google Scholar]
- 44. Ellman MB, James EW, LaPrade CM, LaPrade RF. Anterior meniscus root avulsion following intramedullary nailing for a tibial shaft fracture. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1188-1191. [DOI] [PubMed] [Google Scholar]
- 45. Ellman MB, LaPrade CM, Smith SD, et al. Structural properties of the meniscal roots. Am J Sports Med. 2014;42(8):1881-1887. [DOI] [PubMed] [Google Scholar]
- 46. Emmanuel K, Quinn E, Niu J, et al. Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis—data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24(2):262-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Eseonu KC, Neale J, Lyons A, Kluzek S. Are outcomes of acute meniscus root tear repair better than debridement or nonoperative management? A systematic review. Am J Sports Med. 2022;50(11):3130-3139. [DOI] [PubMed] [Google Scholar]
- 48. Espejo-Reina A, Prado-Novoa M, Espejo-Baena A, Peña-Trabalon A, Perez-Blanca A. Biomechanical consequences of anterior root detachment of the lateral meniscus and its reinsertion. Sci Rep. 2022;12(1):6182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Farivar D, Hevesi M, Fortier LM, Azua E, LaPrade RF, Chahla J. Meniscal extrusion measurements after posterior medial meniscus root tears: a systematic review and meta-analysis. Am J Sports Med. 2023;51(12):3325-3334. [DOI] [PubMed] [Google Scholar]
- 50. Farivar D, Knapik DM, Vadhera AS, et al. Medial meniscal extrusion of greater than 3 mm on ultrasound suggests combined medial meniscotibial ligament and posterior medial meniscal root tears: a cadaveric analysis. Arthroscopy. 2023;39(8):1815-1826. [DOI] [PubMed] [Google Scholar]
- 51. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762-769. [DOI] [PubMed] [Google Scholar]
- 52. Feucht MJ, Grande E, Brunhuber J, et al. Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am J Sports Med. 2014;42(1):187-193. [DOI] [PubMed] [Google Scholar]
- 53. Feucht MJ, Kühle J, Bode G, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808-1816. [DOI] [PubMed] [Google Scholar]
- 54. Feucht MJ, Salzmann GM, Pestka JM, Südkamp NP, Niemeyer P. Simultaneous avulsion fracture of the posterior medial and posterior lateral meniscus root: a case report and review of the literature. Arch Orthop Trauma Surg. 2014;134(4):509-514. [DOI] [PubMed] [Google Scholar]
- 55. Floyd ER, Rodriguez AN, Falaas KL, et al. The natural history of medial meniscal root tears: a biomechanical and clinical case perspective. Front Bioeng Biotechnol. 2021;9:744065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fong FJY, Ong BWL, Lee YHD. Medial meniscal extrusion in patients with medial meniscus root tears: a systematic review and meta-analysis. Orthop J Sports Med. 2023;11(3):23259671231151698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Frank JM, Moatshe G, Brady AW, et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med. 2017;5(6):2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Fujii M, Furumatsu T, Kodama Y, et al. A novel suture technique using the FasT-Fix combined with Ultrabraid for pullout repair of the medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2017;27(4):559-562. [DOI] [PubMed] [Google Scholar]
- 59. Furumatsu T, Fujii M, Kodama Y, Ozaki T. A giraffe neck sign of the medial meniscus: a characteristic finding of the medial meniscus posterior root tear on magnetic resonance imaging. J Orthop Sci. 2017;22(4):731-736. [DOI] [PubMed] [Google Scholar]
- 60. Furumatsu T, Hiranaka T, Kintaka K, et al. A characteristic MRI finding to diagnose a partial tear of the medial meniscus posterior root: an ocarina sign. Knee Surg Relat Res. 2021;33(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Furumatsu T, Hiranaka T, Okazaki Y, et al. Medial meniscus posterior root repairs: a comparison among three surgical techniques in short-term clinical outcomes and arthroscopic meniscal healing scores. J Orthop Sci. 2022;27(1):181-189. [DOI] [PubMed] [Google Scholar]
- 62. Furumatsu T, Kodama Y, Fujii M, et al. A new aiming guide can create the tibial tunnel at favorable position in transtibial pullout repair for the medial meniscus posterior root tear. Orthop Traumatol Surg Res. 2017;103(3):367-371. [DOI] [PubMed] [Google Scholar]
- 63. Furumatsu T, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29(4):295-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Furumatsu T, Okazaki Y, Hiranaka T, et al. An MRI-based suspension bridge sign can predict an arthroscopically favorable meniscal healing following the medial meniscus posterior root repair. J Orthop Sci. 2021;26(2):237-242. [DOI] [PubMed] [Google Scholar]
- 65. Furumatsu T, Okazaki Y, Okazaki Y, et al. Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res. 2019;105(1):107-111. [DOI] [PubMed] [Google Scholar]
- 66. Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1469-1477. [DOI] [PubMed] [Google Scholar]
- 67. Griffith CJ, LaPrade RF, Fritts HM, Morgan PM. Posterior root avulsion fracture of the medial meniscus in an adolescent female patient with surgical reattachment. Am J Sports Med. 2008;36(4):789-792. [DOI] [PubMed] [Google Scholar]
- 68. Han SB, Shetty GM, Lee DH, et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26(10):1326-1332. [DOI] [PubMed] [Google Scholar]
- 69. Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18(3):189-192. [DOI] [PubMed] [Google Scholar]
- 70. Hiranaka T, Furumatsu T, Kamatsuki Y, et al. The distance between the tibial tunnel aperture and meniscal root attachment is correlated with meniscal healing status following transtibial pullout repair for medial meniscus posterior root tear. Knee. 2020;27(3):899-905. [DOI] [PubMed] [Google Scholar]
- 71. Hiranaka T, Furumatsu T, Miyazawa S, et al. Increased cleft width during knee flexion is useful for the diagnosis of medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2022;30(11):3726-3732. [DOI] [PubMed] [Google Scholar]
- 72. Hiranaka T, Furumatsu T, Okazaki Y, et al. Accuracy of the newly developed Zimmer Biomet root aiming guide in tibial tunnel creation compared with that of conventional guides. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2023;32:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hiranaka T, Furumatsu T, Okazaki Y, et al. Postoperative external tibial rotation is correlated with inferior meniscal healing following pullout repair of a medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2022;30(4):1491-1498. [DOI] [PubMed] [Google Scholar]
- 74. Hiranaka T, Furumatsu T, Okazaki Y, Kintaka K, Yamawaki T, Ozaki T. A newly-developed guide can create tibial tunnel at an optimal position during medial meniscus posterior root repairs. J Orthop Sci. 2022;27(4):815-820. [DOI] [PubMed] [Google Scholar]
- 75. Hiranaka T, Furumatsu T, Okazaki Y, Kodama Y, Kamatsuki Y, Ozaki T. Preoperative morphologic changes of the medial meniscus correlate with suture translations during knee flexion in pullout repair of medial meniscus posterior root tear. Knee. 2021;28:346-353. [DOI] [PubMed] [Google Scholar]
- 76. Homan M, Braaten J, Banovetz M, Kennedy N, LaPrade R. Meniscal root tears: repair and salvage techniques. J Cartilage Joint Preservation. 2022;3:100098. [Google Scholar]
- 77. Hussain ZB, Chahla J, Mandelbaum BR, Gomoll AH, LaPrade RF. The role of meniscal tears in spontaneous osteonecrosis of the knee: a systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47(2):501-507. [DOI] [PubMed] [Google Scholar]
- 78. Hwang BY, Kim SJ, Lee SW, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606-1610. [DOI] [PubMed] [Google Scholar]
- 79. Ikuta F, Takahashi K, Hashimoto S, et al. Effect of physical therapy on early knee osteoarthritis with medial meniscal posterior tear assessed by MRI T2 mapping and 3D-to-2D registration technique: a prospective intervention study. Mod Rheumatol. 2020;30(4):738-747. [DOI] [PubMed] [Google Scholar]
- 80. Itou J, Kuwashima U, Itoh M, Okazaki K. High tibial osteotomy for medial meniscus posterior root tears in knees with moderate varus alignment can achieve favorable clinical outcomes. J Exp Orthop. 2022;9(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Jackson GR, Warrier AA, Wessels M, et al. A systematic review of adverse events and complications after isolated posterior medial meniscus root repairs. Am J Sports Med. 2024;52(4):1109-1115. [DOI] [PubMed] [Google Scholar]
- 82. James E, Cinque M, Chahla J, LaPrade R. An evidence-based approach to the diagnosis and treatment of meniscal root tears. Minerva Ortopedica e Traumatologica. 2017;68:81-90. [Google Scholar]
- 83. Jiang EX, Abouljoud MM, Everhart JS, et al. Clinical factors associated with successful meniscal root repairs: a systematic review. Knee. 2019;26(2):285-291. [DOI] [PubMed] [Google Scholar]
- 84. Jiang J, Xing D, Ni L, Chen J. Non-anatomical arthroscopic all-inside repair of medial meniscus posterior root tear to posterior cruciate ligament for patients with normal lower limb alignment. Orthop Surg. 2022;14(2):397-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Jing L, Liu K, Wang X, et al. Second-look arthroscopic findings after medial open-wedge high tibial osteotomy combined with all-inside repair of medial meniscus posterior root tears. J Orthop Surg (Hong Kong). 2020;28(1):2309499019888836. [DOI] [PubMed] [Google Scholar]
- 86. Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40(10):2342-2347. [DOI] [PubMed] [Google Scholar]
- 87. Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy. 1995;11(4):386-394. [DOI] [PubMed] [Google Scholar]
- 88. Jones AO, Houang MTW, Low RS, Wood DG. Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol. 2006;50(4):306-313. [DOI] [PubMed] [Google Scholar]
- 89. Jung YH, Choi NH, Oh JS, Victoroff BN. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40(6):1406-1411. [DOI] [PubMed] [Google Scholar]
- 90. Kamatsuki Y, Furumatsu T, Hiranaka T, et al. Accurate placement of a tibial tunnel significantly improves meniscal healing and clinical outcomes at 1 year after medial meniscus posterior root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3715-3723. [DOI] [PubMed] [Google Scholar]
- 91. Kamatsuki Y, Furumatsu T, Miyazawa S, et al. The early arthroscopic pullout repair of medial meniscus posterior root tear is more effective for reducing medial meniscus extrusion. Acta Med Okayama. 2019;73(6):503-510. [DOI] [PubMed] [Google Scholar]
- 92. Karpinski K, Diermeier T, Willinger L, Imhoff AB, Achtnich A, Petersen W. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3311-3317. [DOI] [PubMed] [Google Scholar]
- 93. Karpinski K, Forkel P, Häner M, Bierke S, Petersen W. Etiology of posterior meniscus root tears: medial vs. lateral. Arch Orthop Trauma Surg. 2023;143(1):429-437. [DOI] [PubMed] [Google Scholar]
- 94. Ke X, Qiu J, Chen S, et al. Concurrent arthroscopic meniscal repair during open-wedge high tibial osteotomy is not clinically beneficial for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):955-965. [DOI] [PubMed] [Google Scholar]
- 95. Kennedy MI, Strauss M, LaPrade RF. Injury of the meniscus root. Clin Sports Med. 2020;39(1):57-68. [DOI] [PubMed] [Google Scholar]
- 96. Kennedy NI, Michalski MP, Engebretsen L, LaPrade RF. Iatrogenic meniscus posterior root injury following reconstruction of the posterior cruciate ligament: a report of three cases. JBJS Case Connect. 2014;4(1)(suppl 6):e20. [DOI] [PubMed] [Google Scholar]
- 97. Khoo JR, Yau WP. Repair of meniscus root tear—is there a difference between medial meniscus root repair and lateral meniscus root repair? A systematic review and meta-analysis. J Orthop Surg (Hong Kong). 2023;31(2):10225536231175233. [DOI] [PubMed] [Google Scholar]
- 98. Kidron A, Thein R. Radial tears associated with cleavage tears of the medial meniscus in athletes. Arthroscopy. 2002;18(3):254-256. [DOI] [PubMed] [Google Scholar]
- 99. Kim C, Bin SI, Kim JM, Lee BS, Kim TH. Progression of radiographic osteoarthritis after partial meniscectomy in degenerative medial meniscal posterior root tears was greater in varus- than in neutral-aligned knees: a minimum 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3443-3449. [DOI] [PubMed] [Google Scholar]
- 100. Kim CW, Lee CR, Gwak HC, et al. Clinical and radiologic outcomes of patients with lax healing after medial meniscal root repair: comparison with subtotal meniscectomy. Arthroscopy. 2019;35(11):3079-3086. [DOI] [PubMed] [Google Scholar]
- 101. Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644-1653. [DOI] [PubMed] [Google Scholar]
- 102. Kim SB, Ha JK, Lee SW, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346-354. [DOI] [PubMed] [Google Scholar]
- 103. Kim YM, Joo YB, An BK, Song JH. Age and meniscal extrusion are determining factors of osteoarthritis progression after conservative treatments for medial meniscus posterior root tear. J Pers Med. 2022;12(12):2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Kim YM, Joo YB, Lee WY, Kim YK. Remodified Mason-Allen suture technique concomitant with high tibial osteotomy for medial meniscus posterior root tears improved the healing of the repaired root and suppressed osteoarthritis progression. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1258-1268. [DOI] [PubMed] [Google Scholar]
- 105. Kim YM, Joo YB, Noh CK, Park IY. The optimal suture site for the repair of posterior horn root tears: biomechanical evaluation of pullout strength in porcine menisci. Knee Surg Relat Res. 2016;28(2):147-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Kintaka K, Furumatsu T, Okazaki Y, et al. Comparison of two simple stitches and modified Mason-Allen suture for medial meniscus posterior root tear based on the progression of meniscal posterior extrusion: a retrospective cohort study. J Orthop Surg (Hong Kong). 2021;29(3):23094990211049569. [DOI] [PubMed] [Google Scholar]
- 107. Koga H, Muneta T, Watanabe T, et al. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32(10):2000-2008. [DOI] [PubMed] [Google Scholar]
- 108. Koga H, Watanabe T, Horie M, et al. Augmentation of the pullout repair of a medial meniscus posterior root tear by arthroscopic centralization. Arthrosc Tech. 2017;6(4):e1335-e1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Koo JH, Choi SH, Lee SA, Wang JH. Comparison of medial and lateral meniscus root tears. PLoS One. 2015;10(10):e0141021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Krivicich LM, Kunze KN, Parvaresh KC, et al. Comparison of long-term radiographic outcomes and rate and time for conversion to total knee arthroplasty between repair and meniscectomy for medial meniscus posterior root tears: a systematic review and meta-analysis. Am J Sports Med. 2022;50(7):2023-2031. [DOI] [PubMed] [Google Scholar]
- 111. Krych AJ, Bernard CD, Kennedy NI, et al. Medial versus lateral meniscus root tears: is there a difference in injury presentation, treatment decisions, and surgical repair outcomes? Arthroscopy. 2020;36(4):1135-1141. [DOI] [PubMed] [Google Scholar]
- 112. Krych AJ, Hevesi M, Leland DP, Stuart MJ. Meniscal root injuries. J Am Acad Orthop Surg. 2020;28(12):491-499. [DOI] [PubMed] [Google Scholar]
- 113. Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1117-1122. [DOI] [PubMed] [Google Scholar]
- 114. Krych AJ, LaPrade MD, Hevesi M, et al. Investigating the chronology of meniscus root tears: do medial meniscus posterior root tears cause extrusion or the other way around? Orthop J Sports Med. 2020;8(11):2325967120961368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Krych AJ, Nauert RF, Song BM, et al. Association between transtibial meniscus root repair and rate of meniscal healing and extrusion on postoperative magnetic resonance imaging: a prospective multicenter study. Orthop J Sports Med. 2021;9(8):23259671211023774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Krych AJ, Reardon PJ, Johnson NR, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383-389. [DOI] [PubMed] [Google Scholar]
- 117. Krych AJ, Wu IT, Desai VS, et al. High rate of missed lateral meniscus posterior root tears on preoperative magnetic resonance imaging. Orthop J Sports Med. 2018;6(4):2325967118765722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Kwak YH, Lee S, Lee MC, Han HS. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):781-786. [DOI] [PubMed] [Google Scholar]
- 119. Kwon OJ, Bin SI, Kim JM, et al. There is no difference in radiographic outcomes after average 9 years after arthroscopic partial medial meniscectomy for both posterior horn tears and posterior horn root tears. Arthroscopy. 2020;36(2):524-532. [DOI] [PubMed] [Google Scholar]
- 120. Kwon SW, Kim JB, Kim CH, Hong SJ, Hong YC, Jang BW. Comparison of medial and lateral tibial tunnel in pullout repair of posterior root tear of medial meniscus: radiologic, clinical, and arthroscopic outcomes. J Orthop Surg (Hong Kong). 2020;28(2):2309499020918759. [DOI] [PubMed] [Google Scholar]
- 121. Kyun-Ho S, Hyun-Jae R, Ki-Mo J, Seung-Beom H. Effect of concurrent repair of medial meniscal posterior root tears during high tibial osteotomy for medial osteoarthritis during short-term follow-up: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22(1):623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. LaPrade CM, Ellman MB, Rasmussen MT, et al. Anatomy of the anterior root attachments of the medial and lateral menisci: a quantitative analysis. Am J Sports Med. 2014;42(10):2386-2392. [DOI] [PubMed] [Google Scholar]
- 123. LaPrade CM, Foad A, Smith SD, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912-920. [DOI] [PubMed] [Google Scholar]
- 124. LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363-369. [DOI] [PubMed] [Google Scholar]
- 125. Laprade CM, James EW, Engebretsen L, Laprade RF. Anterior medial meniscal root avulsions due to malposition of the tibial tunnel during anterior cruciate ligament reconstruction: two case reports. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1119-1123. [DOI] [PubMed] [Google Scholar]
- 126. LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471-479. [DOI] [PubMed] [Google Scholar]
- 127. LaPrade CM, Jisa KA, Cram TR, LaPrade RF. Posterior lateral meniscal root tear due to a malpositioned double-bundle anterior cruciate ligament reconstruction tibial tunnel. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3670-3673. [DOI] [PubMed] [Google Scholar]
- 128. LaPrade CM, LaPrade MD, Turnbull TL, Wijdicks CA, LaPrade RF. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43(4):899-904. [DOI] [PubMed] [Google Scholar]
- 129. LaPrade CM, Smith SD, Rasmussen MT, et al. Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadaveric model, part 1: the anterior cruciate ligament. Am J Sports Med. 2015;43(1):200-206. [DOI] [PubMed] [Google Scholar]
- 130. LaPrade CM, Smith SD, Rasmussen MT, et al. Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadaveric model, part 2: the posterior cruciate ligament. Am J Sports Med. 2015;43(1):207-212. [DOI] [PubMed] [Google Scholar]
- 131. LaPrade MD, LaPrade CM, Hamming MG, et al. Intramedullary tibial nailing reduces the attachment area and ultimate load of the anterior medial meniscal root: a potential explanation for anterior knee pain in female patients and smaller patients. Am J Sports Med. 2015;43(7):1670-1675. [DOI] [PubMed] [Google Scholar]
- 132. LaPrade R, Floyd E, Carlson G, Moatshe G, Chahla J, Monson J. Meniscal root tears: solving the silent epidemic. J Arthrosc Surg Sports Med. 2021;2:47-57. [Google Scholar]
- 133. LaPrade RF, Geeslin AG, Chahla J, et al. Posterior lateral meniscal root and oblique radial tears: the biomechanical evidence supports repair of these tears, although long-term clinical studies are necessary. Arthroscopy. 2022;38(12):3095-3101. [DOI] [PubMed] [Google Scholar]
- 134. LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):152-157. [DOI] [PubMed] [Google Scholar]
- 135. LaPrade RF, LaPrade CM, James EW. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23(2):71-76. [DOI] [PubMed] [Google Scholar]
- 136. LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884-891. [DOI] [PubMed] [Google Scholar]
- 137. Leafblad ND, Smith PA, Stuart MJ, Krych AJ. Arthroscopic centralization of the extruded medial meniscus. Arthrosc Tech. 2021;10(1):e43-e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Lee BS, Bin SI, Kim JM, Park MH, Lee SM, Bae KH. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees. Am J Sports Med. 2019;47(3):606-611. [DOI] [PubMed] [Google Scholar]
- 139. Lee DH, Lee BS, Kim JM, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222-229. [DOI] [PubMed] [Google Scholar]
- 140. Lee DR, Reinholz AK, Till SE, et al. Current reviews in musculoskeletal medicine: current controversies for treatment of meniscus root tears. Curr Rev Musculoskelet Med. 2022;15(4):231-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Lee DW, Lee SH, Kim JG. Outcomes of medial meniscal posterior root repair during proximal tibial osteotomy: is root repair beneficial? Arthroscopy. 2020;36(9):2466-2475. [DOI] [PubMed] [Google Scholar]
- 142. Lee DW, Moon SG, Kim NR, Chang MS, Kim JG. Medial knee osteoarthritis precedes medial meniscal posterior root tear with an event of painful popping. Orthop Traumatol Surg Res. 2018;104(7):1009-1015. [DOI] [PubMed] [Google Scholar]
- 143. Lee HI, Park D, Cho J. Clinical and radiological results with second-look arthroscopic findings after open wedge high tibial osteotomy without arthroscopic procedures for medial meniscal root tears. Knee Surg Relat Res. 2018;30(1):34-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951-958. [DOI] [PubMed] [Google Scholar]
- 145. Lee JK, Jung M, Yang JH, et al. Repair versus nonrepair of medial meniscus posterior root tear: a systematic review of patients’ selection criteria, including clinical and radiographic outcomes. Medicine (Baltimore). 2020;99(10):e19499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Lee NH, Seo HY, Sung MJ, Na BR, Song EK, Seon JK. Does meniscectomy have any advantage over conservative treatment in middle-aged patients with degenerative medial meniscus posterior root tear? BMC Musculoskelet Disord. 2021;22(1):742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Lee OS, Lee SH, Lee YS. Comparison of the radiologic, arthroscopic, and clinical outcomes between repaired versus unrepaired medial meniscus posterior horn root tear during open wedge high tibial osteotomy. J Knee Surg. 2021;34(1):57-66. [DOI] [PubMed] [Google Scholar]
- 148. Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569-574. [DOI] [PubMed] [Google Scholar]
- 149. Lim HC, Bae JH, Wang JH, Seok CW, Kim MK. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2010;18(4):535-539. [DOI] [PubMed] [Google Scholar]
- 150. Mameri ES, Kerzner B, Jackson GR, et al. Top ten pearls for a successful transtibial pull-out repair of medial meniscal posterior root tears with a concomitant centralization stitch. Arthrosc Tech. 2023;12(7):e1039-e1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Mameri M, Dasari SP, Fortier M, et al. Review of meniscus anatomy and biomechanics. Curr Rev Musculoskelet Med. 2022;15(5):323-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Mariani PP, Iannella G, Cerullo G, Giacobbe M. Avulsion of both posterior meniscal roots associated with acute rupture of the anterior cruciate ligament. J Orthop Traumatol. 2015;16(3):259-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Masuda S, Furumatsu T, Okazaki Y, et al. Transtibial pullout repair reduces posterior extrusion of the medial meniscus. Acta Med Okayama. 2019;73(6):495-501. [DOI] [PubMed] [Google Scholar]
- 154. Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127-3131. [DOI] [PubMed] [Google Scholar]
- 155. Minami T, Muneta T, Sekiya I, et al. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1174-1181. [DOI] [PubMed] [Google Scholar]
- 156. Mochizuki Y, Kawahara K, Samejima Y, Kaneko T, Ikegami H, Musha Y. Short-term results and surgical technique of arthroscopic centralization as an augmentation for medial meniscus extrusion caused by medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2021;31(6):1235-1241. [DOI] [PubMed] [Google Scholar]
- 157. Moon HS, Choi CH, Jung M, Lee DY, Hong SP, Kim SH. Early surgical repair of medial meniscus posterior root tear minimizes the progression of meniscal extrusion: 2-year follow-up of clinical and radiographic parameters after arthroscopic transtibial pull-out repair. Am J Sports Med. 2020;48(11):2692-2702. [DOI] [PubMed] [Google Scholar]
- 158. Moon M, Choi CH, Yoo JH, et al. Mild to moderate varus alignment in relation to surgical repair of a medial meniscus root tear: a matched-cohort controlled study with 2 years of follow-up. Am J Sports Med. 2021;49(4):1005-1016. [DOI] [PubMed] [Google Scholar]
- 159. Moran J, Homan MD, LaPrade CM, Kennedy NI, LaPrade RF. Combined repair of medial meniscal ramp lesions and posterior root tears of the lateral meniscus during anterior cruciate ligament reconstruction: a case report. JBJS Case Connect. 2023;13(1). [DOI] [PubMed] [Google Scholar]
- 160. Mueller BT, Moulton SG, O’Brien L, LaPrade RF. Rehabilitation following meniscal root repair: a clinical commentary. J Orthop Sports Phys Ther. 2016;46(2):104-113. [DOI] [PubMed] [Google Scholar]
- 161. Nakamura R, Okano A, Yoshida I, Shimakawa T. A spreading roots sign: characteristic sign of the preliminary stage of medial meniscus posterior root tear on magnetic resonance imaging. J Orthop Sci. 2022;27(5):1107-1113. [DOI] [PubMed] [Google Scholar]
- 162. Neogi DS, Kumar A, Rijal L, Yadav CS, Jaiman A, Nag HL. Role of nonoperative treatment in managing degenerative tears of the medial meniscus posterior root. J Orthop Traumatol. 2013;14(3):193-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Nicholas SJ, Golant A, Schachter AK, Lee SJ. A new surgical technique for arthroscopic repair of the meniscus root tear. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1433-1436. [DOI] [PubMed] [Google Scholar]
- 164. Okazaki Y, Furumatsu T, Hiranaka T, et al. Arthroscopic meniscal healing following medial meniscus posterior root repair: a comparison between two suture materials. J Knee Surg. 2023;36(11):1200-1208. [DOI] [PubMed] [Google Scholar]
- 165. Okazaki Y, Furumatsu T, Hiranaka T, et al. Grade of subchondral insufficiency fracture of the knee and the presence of a posterior shiny-corner lesion are correlated with duration of medial meniscus posterior root tear in women. Acta Med Okayama. 2022;76(2):121-127. [DOI] [PubMed] [Google Scholar]
- 166. Okazaki Y, Furumatsu T, Hiranaka T, et al. Medial meniscus posterior root repair prevents the progression of subchondral insufficiency fracture of the knee. J Orthop Sci. 2021;26(6):1051-1055. [DOI] [PubMed] [Google Scholar]
- 167. Okazaki Y, Furumatsu T, Yamaguchi T, et al. Medial meniscus posterior root tear causes swelling of the medial meniscus and expansion of the extruded meniscus: a comparative analysis between 2D and 3D MRI. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3405-3415. [DOI] [PubMed] [Google Scholar]
- 168. Okimura S, Mae T, Tachibana Y, et al. Biomechanical comparison of meniscus-suture constructs for pullout repair of medial meniscus posterior root tears. J Exp Orthop. 2019;6(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Oshima T, Grasso S, Beach A, Fritsch B, Parker DA. Lateral location of the tibial tunnel increases lateral meniscal extrusion after anatomical single-bundle anterior cruciate ligament reconstruction. J ISAKOS. 2019;4(6):285-289. [Google Scholar]
- 170. Ozeki N, Seil R, Krych AJ, Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS. 2021;6(1):35-45. [DOI] [PubMed] [Google Scholar]
- 171. Padalecki JR, Jansson KS, Smith SD, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699-707. [DOI] [PubMed] [Google Scholar]
- 172. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Papalia R, Vasta S, Franceschi F, D’Adamio S, Maffulli N, Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106:91-115. [DOI] [PubMed] [Google Scholar]
- 174. Park HJ, Kim SS, Lee SY, et al. Medial meniscal root tears and meniscal extrusion transverse length ratios on MRI. Br J Radiol. 2012;85(1019):e1032-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Paul RW, Lee D, Brutico J, Tjoumakaris FP, Ciccotti MG, Freedman KB. Reporting and analyzing race and ethnicity in orthopaedic clinical trials: a systematic review. J Am Acad Orthop Surg Glob Res Rev. 2021;5(5):e21.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Perez BA, Slover J, Edusei E, et al. Impact of gender and race on expectations and outcomes in total knee arthroplasty. World J Orthop. 2020;11(5):265-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Perez-Blanca A, Espejo-Baena A, Amat Trujillo D, et al. Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy. 2016;32(4):624-633. [DOI] [PubMed] [Google Scholar]
- 178. Pula DA, Femia RE, Marzo JM, Bisson LJ. Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury? A case control study. Am J Sports Med. 2014;42(1):173-176. [DOI] [PubMed] [Google Scholar]
- 179. Qardash AAA, Hassan AA, El kady HA, Mohammed HEDG, Abdel-Tawab M, Mohammed NAA. Varus stress MRI in diagnosis of medial meniscal posterior root tear. Egyptian J Radiol Nucl Med. 2022;53(1):39. [Google Scholar]
- 180. Razi M, Mortazavi SMJ. Save the meniscus, a good strategy to preserve the knee. Arch Bone Jt Surg. 2020;8(1):1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Ridley TJ, Ruzbarsky JJ, Dornan GJ, et al. Minimum 2-year clinical outcomes of medial meniscus root tears in relation to coronal alignment. Am J Sports Med. 2022;50(5):1254-1260. [DOI] [PubMed] [Google Scholar]
- 182. Ro KH, Kim JH, Heo JW, Lee DH. Clinical and radiological outcomes of meniscal repair versus partial meniscectomy for medial meniscus root tears: a systematic review and meta-analysis. Orthop J Sports Med. 2020;8(11):2325967120962078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Rocha de Faria JL, Serra Cruz R, Campos ALS, Souza GGA, Di Cavalcanti YS, Goes RA. Meniscal root repair alone or combined with different procedures after at least 6 months of follow-up: a series of cases. Open Access J Sports Med. 2022;13:25-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Rowland G, Mar D, McIff T, Nelson J. Evaluation of meniscal extrusion with posterior root disruption and repair using ultrasound. Knee. 2016;23(4):627-630. [DOI] [PubMed] [Google Scholar]
- 185. Samuelsen BT, Aman ZS, Kennedy MI, et al. Posterior medial meniscus root tears potentiate the effect of increased tibial slope on anterior cruciate ligament graft forces. Am J Sports Med. 2020;48(2):334-340. [DOI] [PubMed] [Google Scholar]
- 186. Seil R, Dück K, Pape D. A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2072-2075. [DOI] [PubMed] [Google Scholar]
- 187. Shimozaki K, Nakase J, Oshima T, Asai K, Toyooka K, Tsuchiya H. Partial lateral meniscus anterior root injuries during anatomical single-bundle anterior cruciate ligament reconstruction are likely to occur in women with small skeletons. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3517-3523. [DOI] [PubMed] [Google Scholar]
- 188. Smith PA, Bezold WA, Cook CR, et al. Kinematic analysis of lateral meniscal oblique radial tears in the anterior cruciate ligament-deficient knee. Am J Sports Med. 2021;49(14):3898-3905. [DOI] [PubMed] [Google Scholar]
- 189. Stein JM, Yayac M, Conte EJ, Hornstein J. Treatment outcomes of meniscal root tears: a systematic review. Arthrosc Sports Med Rehabil. 2020;2(3):e251-e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Steineman BD, LaPrade RF, Haut Donahue TL. Loosening of transtibial pullout meniscal root repairs due to simulated rehabilitation is unrecoverable: a biomechanical study. Arthroscopy. 2019;35(4):1232-1239. [DOI] [PubMed] [Google Scholar]
- 191. Steineman BD, LaPrade RF, Santangelo KS, Warner BT, Goodrich LR, Haut Donahue TL. Early osteoarthritis after untreated anterior meniscal root tears: an in vivo animal study. Orthop J Sports Med. 2017;5(4):2325967117702452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Steineman BD, Moulton SG, Haut Donahue TL, et al. Overlap between anterior cruciate ligament and anterolateral meniscal root insertions: a scanning electron microscopy study. Am J Sports Med. 2017;45(2):362-368. [DOI] [PubMed] [Google Scholar]
- 193. Su J, Wan H, Pang Y, et al. Trans-posterior cruciate ligament all-inside root repair versus partial meniscectomy for medial meniscus posterior root tears: comparison of semiquantitative and quantitative MRI outcomes in cartilage degeneration and osteoarthritic progression. Cartilage. 2022;13(3):19476035221114242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Suh DW, Yeo WJ, Han SB, So SY, Kyung BS. Simple medial meniscus posterior horn root repair using an all-inside meniscal repair device combined with high tibial osteotomy to maintain joint-space width in a patient with a repairable tear. Indian J Orthop. 2021;55(2):397-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Tamura M, Furumatsu T, Hiranaka T, et al. Transtibial pullout repair of lateral meniscus posterior root tear with tissue loss: a case with anterior cruciate ligament injury and medial meniscus tear. Case Rep Orthop. 2022;2022:9776388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Thomas B, de Villeneuve Florent B, Alexandre F, et al. Patients with meniscus posterolateral root tears repair during ACL reconstruction achieve comparable post-operative outcome than patients with isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2023;31(8):3405-3411. [DOI] [PubMed] [Google Scholar]
- 197. Umans H, Morrison W, DiFelice GS, Vaidya N, Winalski CS. Posterior horn medial meniscal root tear: the prequel. Skeletal Radiol. 2014;43(6):775-780. [DOI] [PubMed] [Google Scholar]
- 198. van der Wal WA, Meijer DT, Hoogeslag RAG, LaPrade RF. Meniscal tears, posterolateral and posteromedial corner injuries, increased coronal plane, and increased sagittal plane tibial slope all influence anterior cruciate ligament-related knee kinematics and increase forces on the native and reconstructed anterior cruciate ligament: a systematic review of cadaveric studies. Arthroscopy. 2022;38(5):1664-1688. [DOI] [PubMed] [Google Scholar]
- 199. Wang H, Man Q, Gao Y, et al. The efficacy of medial meniscal posterior root tear repair with or without high tibial osteotomy: a systematic review. BMC Musculoskelet Disord. 2023;24(1):464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Wang L, Zhang K, Liu X, et al. The efficacy of meniscus posterior root tears repair: a systematic review and meta-analysis. J Orthop Surg (Hong Kong). 2021;29(1):23094990211003350. [DOI] [PubMed] [Google Scholar]
- 201. Whi W, Park JY, Choi H, et al. Predicting outcome of repair of medial meniscus posterior root tear with early osteoarthritis using bone single-photon emission computed tomography/computed tomography. Medicine (Baltimore). 2020;99(27):e21047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1-3. [PubMed] [Google Scholar]
- 203. Wu M, Jiang J, Liu Z, Dai X, Dong Y, Xia Y. Age, male sex, higher posterior tibial slope, deep sulcus sign, bone bruises on the lateral femoral condyle, and concomitant medial meniscal tears are risk factors for lateral meniscal posterior root tears: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(12):4144-4155. [DOI] [PubMed] [Google Scholar]
- 204. Wu SH, Yeh TT, Hsu WC, et al. Biomechanical comparison of four tibial fixation techniques for meniscal root sutures in posterior medial meniscus root repair: a porcine study. J Orthop Translat. 2020;24:144-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Xu Z, Li Y, Rao J, et al. Biomechanical assessment of disease outcome in surgical interventions for medial meniscal posterior root tears: a finite element analysis. BMC Musculoskelet Disord. 2022;23(1):1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Yang Q, Zhu XY, Bao JY, et al. Medial meniscus posterior root tears and partial meniscectomy significantly increase stress in the knee joint during dynamic gait. Knee Surg Sports Traumatol Arthrosc. 2023;31(6):2289-2298. [DOI] [PubMed] [Google Scholar]
- 207. Yoon KH, Lee W, Park JY. Outcomes of arthroscopic all-inside repair are improved compared to transtibial pull-out repair of medial meniscus posterior root tears. Arthroscopy. 2023;39(5):1254-1261. [DOI] [PubMed] [Google Scholar]
- 208. Zhan H, Liu Z, Wang Y, et al. Radiographic OA, bone marrow lesions, higher body mass index and medial meniscal root tears are significantly associated with medial meniscus extrusion with OA or medial meniscal tears: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2023;31(8):3420-3433. [DOI] [PubMed] [Google Scholar]
- 209. Zheng T, Song G, Li Y, et al. Clinical, radiographic, and arthroscopic outcomes of surgical repair for radial and avulsed lesions on the lateral meniscus posterior root during ACL reconstruction: a systematic review. Orthop J Sports Med. 2021;9(3):2325967121989678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Zheng T, Song GY, Feng H, et al. Lateral meniscus posterior root lesion influences anterior tibial subluxation of the lateral compartment in extension after anterior cruciate ligament injury. Am J Sports Med. 2020;48(4):838-846. [DOI] [PubMed] [Google Scholar]
- 211. Zhu S, Li X, Wu JL, et al. Non-anatomic repair of medial meniscus posterior root tears to the posterior capsule provided favourable outcomes in middle-aged and older patients. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4261-4269. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241283962 for Diagnosis and Treatment Strategies of Meniscus Root Tears: A Scoping Review by Jose Rafael Garcia, Salvador Gonzalez Ayala, Felicitas Allende, Enzo Mameri, Monique Haynes, Filippo Familiari, Andrew G. Geeslin, Iain Murray, Gilbert Moatshe, Nikhil N. Verma, Robert F. LaPrade and Jorge Chahla in Orthopaedic Journal of Sports Medicine