Abstract
Background
The social distancing measures associated with the COVID-19 pandemic had far reaching effects on sexual behavior worldwide. However, it remains unclear whether sexual contact with non-steady partners was a contributor to the spread of SARS-CoV-2. The aim of this study was to (i) describe risk factors for SARS-CoV-2 seropositivity after the first pandemic wave among people using HIV Pre-Exposure Prophylaxis (PrEP) in Zurich, Switzerland, including sexual contact with non-steady partners, and (ii) assess whether the SARS-CoV-2 seropositivity among PrEP users in this time period differed from that of a demographic matched population level comparison group.
Methods
The study was conducted between July 2020 and October 2020 as a nested cross-sectional study within two ongoing cohort studies, SwissPrEPared (all eligible PrEP users in Switzerland ≥ 18 years old) and Corona Immunitas (a series of cross-sectional and longitudinal studies measuring the SARS-CoV-2 seroprevalence across Switzerland, beginning in April 2020). All SwissPrEPared participants were recruited from Checkpoint Zurich (the main PrEP clinic in Zurich) and were men having sex with men or transgender women. Data were collected on participants’ SARS-CoV-2 antibody status, social characteristics and behavioral data after the first wave of the pandemic in Switzerland, and seroprevalence was compared with a propensity score-matched sample from the general Zurich population.
Results
Of the 218 participants enrolled, 8.7% (n = 19, 95% CI: 5.5–13.5%) were seropositive for SARS-CoV-2 during the first pandemic wave, higher than that of the general male population in Zurich aged 20–65 (5.5%, 95% CI: 3.8–8.2%). Participants on average reduced their social outings, but the seronegative were more socially active before, during, and after the first lockdown period. In a logistic model, increasing mean sexual partner count was not associated with seropositivity (OR: 1.02, 95% CI: 0.95, 1.07). The estimated risk ratio for seropositivity for the participants compared to the general Zurich population after propensity score matching was 1.46 (95% CI: 0.53, 3.99).
Conclusions
Our study suggests that SARS-CoV-2 seropositivity was slightly elevated among people taking PrEP in Zurich during the first wave of the pandemic, but that socializing and sexual activity were less important than other factors in contributing to risk.
Keywords: COVID-19, PrEP, MSM, Switzerland, SARS-CoV-2 seroprevalence, sexual behavior
Background
Soon after the emergence of SARS-CoV-2, unprecedented restrictions on social contact and mobility were implemented globally to contain the virus, including rules on restricting sexual contacts. These restrictions often had unintended consequences, especially on mental health [1], stress, substance use, and sleep patterns [2–4]. These consequences were not evenly distributed among the population, with the burden of the mental health effects of social distancing falling disproportionately on vulnerable populations such as adolescents, young people, and people with minority sexual orientation or gender identity [4–6]. In Switzerland, social distancing measures were implemented starting in March 2020, and the strongest restrictions occurred over the first waves of the pandemic.
Social distancing measures were particularly difficult for people with non-steady sexual partners to implement [6]. Sexual behavior is complex and cannot be changed easily; previous research has shown that mate-seeking motives (especially among young men) was one of the strongest predictors of lack of compliance with social distancing measures [7]. People who are not in steady sexual relationships are more likely to live alone and thus more likely to suffer from social and mental isolation due to the pandemic and its associated restrictions. A study in Germany showed that loneliness, anxiety and depression during the pandemic were particularly high among people with minority sexual orientation or gender identity, and especially those living alone [5]. Some estimates suggest that over 50% of urban households are solitary in many metropolitan areas [2], and that men having sex with men (MSM) are particularly likely to live alone [6].
A robust scientific evidence base has emerged that the first phases of the COVID-19 pandemic had significant effects on sexual behavior worldwide [6, 8]. However, few studies focused specifically on people with non-steady sexual partners or the result of changes in their sexual behavior on risk of acquiring SARS-CoV-2 [8]. Much of the research in this area has focused on MSM, partly due to pre-existing research on sex behaviors in this population. Most studies on changes in sexual activity among MSM showed reductions in numbers of sexual partners during the first phases of the pandemic [1, 9–12]. However, a few studies showed no change or even increases in the number of sexual partners in this population during the first year of the pandemic [13–15]. It still remains poorly understood how social distancing measures during the pandemic affected the sexual health of people not in a steady relationship. It also remains unclear whether sexual contact with non-steady partners was a contributor to the spread of SARS-CoV-2.
HIV pre-exposure prophylaxis (PrEP), a preventative treatment for HIV, involves the use of antiretroviral medication by individuals who are HIV-negative but at high risk of infection. As PrEP is almost exclusively taken by people with multiple sexual partners, some studies have taken advantage of existing PrEP cohorts to investigate how the pandemic investigated sexual risk taking [1, 16–20]. However, these studies suffered from lack of a comparable population cohort to understand whether risk was elevated in PrEP cohorts compared to other populations with similar demographic characteristics. In our study, we were able to integrate people taking PrEP into an existing population level seroprevalence study (Corona Immunitas) to better examine and compare the influence of sexual behavior on the COVID-19 pandemic on this population.
The aim of this study was to (i) describe risk factors for SARS-CoV-2 seropositivity after the first pandemic wave among people using PrEP in Zurich, Switzerland, including sexual contact with non-steady partners, and (ii) assess whether the SARS-CoV-2 seropositivity among PrEP users in this time period differed from that of a demographic matched population level comparison group.
Methods
Study design, setting and participants
This study is a cross-sectional study nested within two ongoing studies: SwissPrEPared and Corona Immunitas. The study was conducted between July 2020 and October 2020, a period corresponding to the end of the first pandemic wave and the beginning of the second.
SwissPrEPared national program and cohort study
The SwissPrEPared program is a large, ongoing nation-wide Swiss cohort of PrEP users. Individuals are eligible to participate if they are ≥ 18 years old and express interest in PrEP in one of the participating medical centers. While the study is open to anyone interested in PrEP, virtually all participants are, in practice, MSM. The enrollment for the SwissPrEPared study is detailed elsewhere [21], but in brief, all persons interested in PrEP and 18 years of age or older living in Switzerland are eligible for the SwissPrEPared study. Following recommendations in line with those of the European AIDS Clinical Society (EACS) [22], three monthly screenings for counseling and STI screening are recommended for those on daily PrEP and at least six monthly screenings for those on event-based PrEP. Active participants of the SwissPrEPared study who attended Checkpoint Zurich for their routine PrEP appointments between July 15 and October 6, 2020 (before the second wave of the COVID-19 pandemic hit Switzerland), were eligible for participation in the Corona Immunitas substudy. Checkpoint Zurich is the largest PrEP center in Switzerland.
Corona Immunitas national research program
Corona Immunitas is a nation-wide Swiss research program of cross-sectional and longitudinal SARS-CoV-2 seroprevalence studies that investigated the spread and impact of infection with SARS-Cov-2 in Switzerland over six phases (https://www.corona-immunitas.ch/en/) [23–[27. To ensure comparability, a standardized protocol (ISRCTN18181860) [28] including the same baseline questionnaire and serological testing was administered in the Swiss general population and in several subpopulations [29]. For this study, we used data from Corona Immunitas phase 2 of the canton of Zurich, for which randomly selected individuals from the general population were recruited using age stratified sampling (20–64 years, ≥ 65 years) and invited to participate. These data from the general public was used as a comparison for the data from SwissPrEPared.
The SwissPrEPared study (NCT03893188) was approved by the lead ethical committee (EC) in Zurich on 14 May 2019 (BASEC Nr. 2018 − 02015), followed by the approval of all ECs from the other cantons. The Corona Imunitas study was approved by the lead EC in Zurich (BASEC Nr. 2020 − 01247), followed by the approval of all ECs from the other cantons. All participants signed a written informed consent.
Procedures and measurements
A poster with information about the Corona Immunitas study and the study team contact information was placed in the Checkpoint Zurich waiting area. During their routine visits, SwissPrEPared participants were informed about the Corona Immunitas study by their healthcare providers, and given contact information for the study team. Finally, all Checkpoint Zurich SwissPrEPared participants who were not yet enrolled in Corona Immunitas were sent a text message inviting them to enroll. The Corona Immunitas study team contacted all participants by email or telephone, answered questions, arranged an enrollment visit, and sent out an electronic version of the informed consent and Corona Immunitas standardized baseline questionnaire prior to the enrollment visit. The Corona Immunitas standardized baseline questionnaire collects data on demographics and household characteristics, health and COVID-19 related symptoms, test results, potential exposures, and compliance with pandemic measures. At the visit, the informed consent was signed and completeness of the questionnaire was checked and completed if necessary. A 10 mL blood sample was then taken for the seroprevalence testing. Participants that did not show up to their scheduled enrollment visit were contacted again to schedule a new appointment.
Further data on demographic, clinical, and sexual characteristics were collected within the frame of the SwissPrEPared study. These data were collected from all participants digitally via the SwissPrEPared web application, described in detail elsewhere [1, 21]. In brief, the web application collects health (e.g. symptoms) and behavioral (e.g. number of sexual partners) data from participants via a digitally administered survey and integrates it with clinical and lab-based data (e.g. test results) in one comprehensive database that streamlines the continuity of medical care for this population. After participants consented to the Corona Immunitas study and filled out the Corona Immunitas baseline questionnaire, longitudinal data on number of sexual partners, sexual behavior change during the pandemic, PrEP use, dating app use, education, other medical diagnoses, and COVID-19 vaccine status were extracted from the SwissPrEPared database. Participants were asked about the total number of sexual partners since their last visit (usually three months ago) and also whether they had sex with occasional partners in the last three months.
Serological testing
Participants were considered to have a positive test result if they tested positive for either IgG or IgA antibodies. As in all Corona Immunitas studies, the Sensitive Anti-SARS-CoV-2 Spike Trimer Immunoglobulin Serological (SenASTrIS) Luminex binding assay was used [30]. It was developed by the Vaud Central University Hospital (CHUV), the Swiss Federal Institute of Technology in Lausanne (EPFL), and the Swiss Vaccine Center, has a specificity of 99.7% and sensitivity of 96.6% at 15 days after infection, and has been validated in the general population as well as specific subgroups [30].
Statistical analysis
Descriptive statistics for the overall study population and by seropositivity status were calculated using median and interquartile range (IQR) for continuous variables and counts and percentages for categorical variables. To calculate the mean number of sexual partners during the study period, the number of sexual partners reported in the SwissPrEPared followup questionnaire was averaged over all followup questionnaires filled out between March 1, 2020 and October 6, 2020. For questions from the repeated SwissPrEPared followup survey where participants had multiple appointments during that time frame and may have answered differently, we took the most recent answer (e.g. changes in sexual behavior during the pandemic). Confidence intervals (CI) for binomial proportions were produced using the Clopper-Pearson confidence intervals (CI) in base R (binom.test). To calculate the overall prevalence of antibodies in both the study population and the population comparison group, we adjusted for sensitivity and specificity using a Bayesian framework. The posterior distributions for the true prevalence were derived by applying Bayes’ theorem, assuming beta-distributed priors for the parameters, and incorporating the known test sensitivity/specificity of the antibody test. The adjusted prevalence and associated 95% credible intervals were reported.
To determine whether there was a higher presence of SARS-CoV-2 antibodies in the SwissPrEPared population versus the general Corona Immunitas population-based sample from the same time period, propensity score matching was performed to balance key demographic characteristics (age, household size, trips abroad, education). Because the SwissPrEPared population was predominantly male (99%) and 100% assigned male at birth, analyses with the Corona Immunitas population were restricted to men and those 65 years or below. The data on the general population was accessed directly from the Corona Immunitas study and matched with the SwissPrEPared population. The aim of this analysis was to estimate the average marginal effect of being a member of the cohort taking PrEP during the pandemic while accounting for confounding by the included covariates. The propensity score was estimated using full matching on the propensity score and a probit regression of cohort membership on the covariates, which yielded better balance than did a logistic regression. The relative risk (RR) of being positive for COVID-19 antibodies in the SwissPrEPared population versus the general Corona Immunitas population was estimated along with its associated 95% CI. Matching was performed using the MatchIt package [31], and covariate balance was assessed using cobalt [32], both in R Version 4.2.3 [33].
To determine which predictors were associated with presence of SARS-CoV-2 antibodies in both the SwissPrEPared and general Corona Immunitas population of the same time period, exploratory logistic regression was performed and odds ratios (OR) and their associated 95% CI were reported.
Results
Study Population
A total of 218 participants were enrolled in the Corona Immunitas study from the SwissPrEPared cohort. This represents 31% (218/693) of the participants in the SwissPrEPared study that visited Checkpoint Zurich during the study time period. Participants were all assigned male at birth, and almost all had a male gender identity (99%, 1% female, 1% other), Swiss (73%), German speaking (71%), highly educated (73% completed a higher technical or university degree), and employed or self-employed (85%). The median age was 40.0 (IQR: 34.0, 45.8). Most lived alone (45%) or in a household with one other person (42%). Demographic characteristics were very similar between those who were seropositive and seronegative for SARS-CoV-2 (Table 1; Fig. 1). Of the 218 participants enrolled in the study, 19 (8.7%) tested positive for SARS-CoV-2 antibodies, corresponding to an adjusted prevalence of 8.7% (95% credible interval: 5.7–13.2%).
Table 1.
Demographic and health characteristics of study participants [n (%) or median (IQR)]
| Total | SARS-CoV-2 seropositivity status | ||
|---|---|---|---|
| Positive | Negative | ||
| Participants | 218 | 19 (9%) | 199 (91%) |
| Male gender identity | 216 (99%) | 19 (100%) | 197 (99%) |
| Assigned male at birth | 218 (100%) | 19 (100%) | 199 (100%) |
| Age | 40.0 (34.0, 45.8) | 38.0 (35.0, 45.0) | 40.0 (33.5, 46.0) |
| Swiss nationality | 160 (73%) | 15 (79%) | 145 (73%) |
| Never smoker | 124 (57%) | 13 (68%) | 111 (56%) |
| Additional household members | 1.0 (0, 1.0) | 0 (0, 1.0) | 1.0 (0, 1.0) |
| Number of trips abroad February-October 2020 | 2.0 (0.8,3.0) | 2.0 (1.0, 3.5) | 2.0 (0, 3.0) |
| Ever vaccinated against flu* | 97 (49%) | 6 (35%) | 91 (51%) |
| EuroQoL self-rated health | 88.5 | 82.5 | 89.0 |
| Obligatory schooling | 1 (0.5%) | 0 (0%) | 1 (1%) |
| Vocational | 34 (16%) | 3 (16%) | 31 (16%) |
| Matura | 23 (11%) | 3 (16%) | 20 (10%) |
| Higher technical degree | 61 (28%) | 5 (26%) | 56 (28%) |
| University | 98 (45%) | 8 (42%) | 90 (45%) |
| Missing | 1 | 0 | 1 |
| Employment | |||
| Employed | 167 (77%) | 15 (79%) | 152 (76%) |
| Self-employed | 18 (8%) | 1 (5%) | 17 (9%) |
| Studying | 15 (7%) | 1 (5%) | 14 (7%) |
| Unemployed | 13 (6%) | 1 (5%) | 12 (6%) |
*22 unsure or missing data on previous flu vaccination
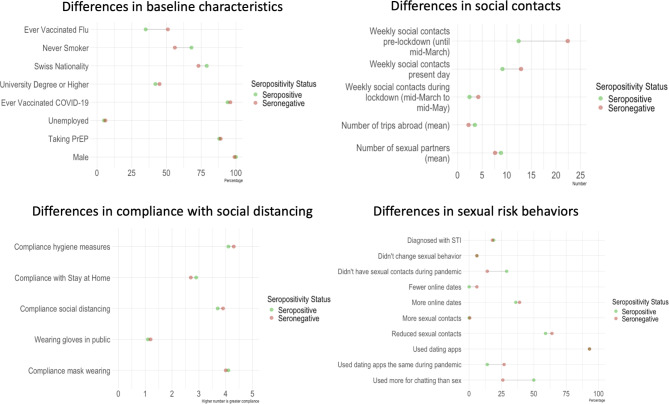
Fig. 1.
Overall comparison of differences between those seropositive and seronegative, ordered from greatest to least except for within the sexual risk taking behavior panel
Health risk behaviors and COVID-19 seropositivity
Those who were seropositive were less likely to have ever been vaccinated against flu (35% vs. 51%). Compliance with recommended social distancing and hygiene measures was similar across those seropositive and seronegative, although the seropositive were slightly less likely to comply with stay-at-home orders (Table 2; Fig. 1). Both groups reduced their social outings during the first lockdown period, but the seronegative were more socially active before, during, and after the first lockdown period, despite the fact that the seropositive were more likely to live alone (Table 1; Fig. 1). Participants also reported during the course of the regular SwissPrEPared study whether they later received a COVID-19 vaccination; vaccine uptake was very high, with at least 96% of both the seropositive and seronegative receiving a COVID-19 vaccination (Fig. 1; n = 198 (91%) of participants reported COVID-19 vaccination status).
Table 2.
Differences in compliance with social distancing measures; a score of 5 corresponds to the highest compliance levels (“always”)
| Total | SARS-CoV-2 seropositivity status | ||
|---|---|---|---|
| Positive | Negative | ||
| Participants | 218 | 19 (9%) | 199 (91%) |
| How often* have you in the last 7 days… | |||
| Followed social distancing** measures? | 4.0 (4.0, 4.0) | 4.0 (4.0, 4.0) | 4.0 (4.0, 4.0) |
| Stayed home when possible? | 3.0 (2.0, 4.0) | 3.0 (1.5, 4.0) | 3.0 (2.0, 4.0) |
| Worn a mask? | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) |
| Increased hygiene measures*** | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) | 4.0 (4.0, 5.0) |
| Average number of contacts with persons outside the household per week (> 15 min) | |||
| Pre-lockdown (until mid-March 2020) | 15.0 (7.0, 25.0) | 10.0 (5.0, 20.0) | 15.0 (7.2, 30.0) |
| Lockdown (mid-March to mid-May) | 2.0 (1.0, 5.0) | 2.0 (0.5, 4.0) | 2.0 (1.0, 5.0) |
| Present day (time point of survey) | 7.5 (4.0, 15.0) | 5.0 (3.5, 10.0) | 8.0 (4.0, 15.0) |
*Participants answered on a scale from 1 to 5, corresponding to the following frequencies: 1: never, 2: rarely, 3: sometimes, 4: often, 5: always
**No handshakes or hugs, maintain 2 m distance from other people
***Regular handwashing, sneezing into the elbow, using tissue
Sexual behaviors and COVID-19 seropositivity
206 (94%) of participants filled in at least one follow-up questionnaire about sexual behaviors between March 1, 2020 and October 6, 2020. The differences are summarized in Table 3; Fig. 1. The median number of partners reported was higher among those who were seropositive (6.5 vs. 5.0). Most individuals in both groups reported sex with occasional partners during the study period (88% of the seropositive vs. 81% of the seronegative). However, seropositive participants were more likely to report not having had any sexual contacts during the first lockdown (29% vs. 14%). The majority of both groups reported reducing sexual contacts during the first lockdown (59% of seropositive vs. 64% of seronegative). The use of dating apps was almost universal and the same among both groups (93%). Those who were seropositive were more likely to have changed their dating app usage to be more for chatting than for sex in the first lockdown (50% vs. 26%). A similar number of people were diagnosed with an STI during the study period in the seropositive and seronegative groups (18.6% vs. 17.6%).
Table 3.
Differences in sexual behaviors of study participants seropositive and seronegative before, during, and after the first lockdown in March 2020 [n (%) or median (IQR)]
| Total | SARS-CoV-2 seropositivity status | ||
|---|---|---|---|
| Positive | Negative | ||
| Participants who completed at least one survey | 206 (94%) | 17 (89%) | 189 (95%) |
| Number of surveys | 438 | 37 | 401 |
| Currently taking PrEP | 174 (84%) | 14 (82%) | 160 (85%) |
| Partner count* | 5.0 (3.0, 10.0) | 6.5 (2.5, 14.7) | 5.0 (3.0, 10.0) |
| Sex with occasional partners | 168 (82%) | 15 (88%) | 153 (81%) |
| Changes in sexual behavior during the first lockdown | |||
| I only had sex with my steady partner | 23 (11%) | 1 (6%) | 22 (12%) |
| I made an agreement with one of my sexual partners to only have sex with each other (“quarantine buddy”) | 7 (3%) | 0 | 7 (4%) |
| I didn’t have sexual contacts during that time | 31 (15%) | 5 (29%) | 26 (14%) |
| I reduced my sexual contacts | 129 (64%) | 10 (59%) | 119 (64%) |
| I didn’t change my sexual behavior | 12 (6%) | 1 (6%) | 11 (6%) |
| I had more sexual contacts | 1 (0.5%) | 0 | 1 (0.5%) |
| Missing | 3 | 0 | 3 |
| Use dating apps** | 156 (93%) | 14 (93%) | 142 (93%) |
| Changes in dating app behaviors during the first lockdown among those using dating apps (n = 156) | |||
| Use the same | 40 (26%) | 2 (14%) | 38 (27%) |
| Fewer online dates | 8 (5%) | 0 | 8 (6%) |
| Use more for chatting than sex | 44 (28%) | 7 (50%) | 37 (26%) |
| More online dates | 61 (39%) | 5 (36%) | 56 (39%) |
| Other | 3 (2%) | 0 | 3 (2%) |
*If participants filled out more than one follow-up survey, the number of partners they reported was averaged across all their follow-up surveys
**39 participants were missing data on dating app usage; 2 among the seropositive and 37 among the seronegative
In a logistic model including only mean partner count and number of trips abroad during the first pandemic wave in the SwissPrEPared study population only (n = 206), increasing mean partner count (OR: 1.02, 95% CI: 0.95, 1.07) and increasing number of trips abroad (OR: 1.07, 95% CI: 0.92, 1.20) were not significantly associated with seropositivity.
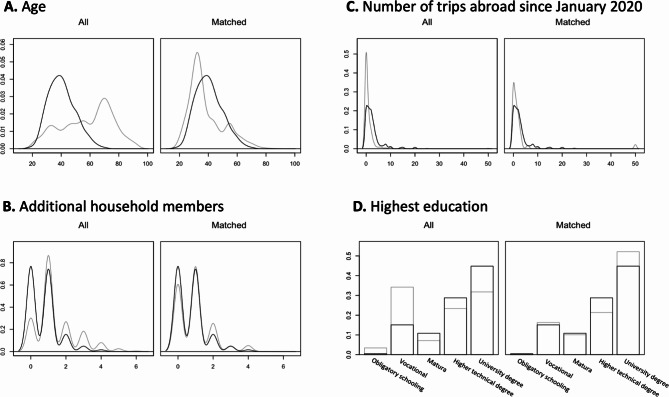
Comparison with general population in Zurich
Of the 218 participants enrolled in the Corona Immunitas study, 19 tested positive for SARS-CoV-2 antibodies, corresponding to an adjusted prevalence of 8.7% (95% credible interval: 5.7–13.2%). When restricted to those with primary residence in Zurich (n = 195, 89%), the prevalence remained 8.7% (95% CI: 5.5–13.5%), which was slightly elevated compared to that of the general population of male 20–65 year old in Zurich during that time period (5.5%, 95% credible interval: 3.8–8.2%). The estimated RR for the SwissPrEPared cohort compared to the general Corona Immunitas population after propensity score matching (Fig. 2) was 1.46 (95% CI: 0.53, 3.99), indicating a 46% increased risk of SARS-CoV-2 positivity for the SwissPrEPared cohort, although not statistically significant.
Fig. 2.
Comparison of the differences in demographic characteristics among SwissPrEPared participants (black line) and the Corona Immunitas general male population aged 20–65 in Zurich (grey line) before and after matching
To see which of these factors were most strongly associated with SARS-CoV-2 infections in the pooled sample of SwissPrEPared and Corona Immunitas participants, we conducted a separate logistic regression model (Table 4). The odds of SARS-CoV-2 infection increased by 1% for every additional year of age, 5% for every additional household member, 9% for every additional trip abroad, 97% for being a member of SwissPrEPared, and 450% for those who completed only obligatory schooling (vs. having completed a university degree or higher), after adjusting for the covariates in Table 4. Only the number of trips abroad was statistically significantly associated with risk of COVID-19 seropositivity.
Table 4.
Predictors of seropositivity in a pooled logistic regression analysis of SwissPrEPared and general male population participants
| OR | 95% CI | |
|---|---|---|
| Age | 1.01 | 0.99, 1.04 |
| Number of additional household members | 1.05 | 0.75, 1.43 |
| Number of trips abroad February-October 2020 | 1.09 | 1.02, 1.17 |
| SwissPrEPared | 1.97 | 0.84, 4.79 |
| Education* | ||
| Obligatory schooling | 4.50 | 0.91, 17.39 |
| Vocational | 1.15 | 0.48, 2.68 |
| Matura | 1.23 | 0.33, 3.66 |
| Higher technical degree | 0.93 | 0.38, 2.15 |
The odds ratios in bold are those significantly associated with the odds of having a health event that day (95% confidence interval does not cross the null value of 1). As there was no data on sexual behavior from the general male population, these variables were omitted from the model
*Comparison group: those who completed a university degree or higher
Discussion
Our study provides evidence that the risk of SARS-CoV-2 seropositivity among those taking PrEP was higher than in the general population in Zurich in the first wave of the COVID-19 pandemic in Switzerland. The average number of sexual partners during the study period was slightly higher among the seropositive (median 6.5 vs. 5.0). However, seropositive participants were more likely to report not having any sexual contacts at all during the first lockdown (28% vs. 14%) and using dating apps more for chatting than for sex (50% vs. 26%). Only one seronegative participant reported increasing the number of sexual contacts during the first lockdown. This, linked with the finding that social contacts during the first wave of the pandemic were counterintuitively lower among those who were seropositive, suggests that sexual behaviors were not strongly linked with SARS-CoV-2 seropositivity during this time period. Those who were seropositive were more likely to be living alone and less likely to have ever received a flu vaccination, but the risk factor investigated in this study that was most robustly linked with SARS-CoV-2 seropositivity in both the general population and the SwissPrEPared population was the number of trips abroad during the pandemic.
While sexual behavior did not appear to be linked with increased risk of SARS-CoV-2 seropositivity within the SwissPrEPared population during the first pandemic wave, there was still a 46% increased risk of infection with SARS-CoV-2 compared with the general male Corona Immunitas population in Zurich after propensity score matching for age, travel, household size, and education. The population of SwissPrEPared participants differs in important ways with that of the general male population from Corona Immunitas (younger, more highly educated, more often living alone, travel more frequently). It may be that other, unmeasured factors account for this increased risk. It is well known that cluster infections (e.g. within family or friend groups) played an important role in the early transmission of COVID-19 [34], meaning that the risk is not particularly linked to individual characteristics, but instead social group membership.
Differences in SARS-COV-2 seropositivity between the cohort taking PrEP and the general population
The study shows that the prevalence of SARS-CoV-2 infection among participants taking PrEP in Zurich was higher than that of the general Zurich male population from the Corona Immunitas study (prevalence 8.7% vs. 5.5%) during the first pandemic wave. This increased risk persists even after propensity score matching the two populations on some key characteristics, such as age, education, household size, and international travel, although the difference in absolute terms is not large. As is true in other cohorts of people taking PrEP [35], there are key demographic differences between this group and the general population. Although we were able to match the two populations based on these five key characteristics, we were not able to match on other key demographic characteristics that may also have been related to risk of COVID-19 transmission (e.g. profession and occupational exposures, pre-existing health conditions) [36–38].
Health and sexual behaviors and seropositivity in the cohort taking PrEP
Participants taking PrEP who were seropositive for SARS-CoV-2 differed in some key health behaviors and attitudes. Lifetime flu vaccine uptake was higher in the seronegative group (51% vs. 35%), which may translate to their risk attitude and other health behaviors regarding infectious disease in general, known as the healthy vaccine effect [39]. Other studies have also found that those who were previously vaccinated against the flu had decreased risk of SARS-CoV-2 infection [40]. These participants may also have been more likely to take protective measures against other infectious diseases, resulting in lower levels of exposure to SARS-CoV-2. Seropositive participants were more likely to be living alone. While it is well established that the pandemic had adverse effects on the mental health of those living alone [41], there is less evidence on how living alone affected COVID-19 transmission and choices around protective behavior. However, a meta-analysis on household transmission found that counterintuitively those living in households with only one contact had higher secondary attack rates than those living in households with three or more contacts [42]. More studies are needed. The behavioral finding most robustly associated with increased risk of SARS-CoV-2 seropositivity is travel abroad. The important role of travel abroad in infection and transmission of COVID-19 in the early stages of the pandemic has been established in other studies [43, 44].
SwissPrEPared participants showed high compliance with social distancing measures. This high level of compliance was similar among both the seropositive and the seronegative. The overwhelming majority of study participants (at least 96%) also later received the COVID-19 vaccination. The results of this study also indicate that SwissPrEPared participants reduced their sexual contacts during the pandemic, similar to what was reported in the United States, Israel, Brazil, and Australia [5–8]. This contrasts with what was found in a 2021 German study of PrEP users, which found no change in sexual behavior compared to pre-pandemic, but a similar rate of seroconversion as that of the general population [17]. Other studies from the United States that recruited through dating applications suggested that MSM did not change their sexual behavior or even increased the number of sexual partners during the pandemic, but that may reflect that these populations were recruited from those actively on dating applications during the pandemic [9, 10]. Another study from the US found age related differences in sexual behavior during the pandemic, with younger MSM having large decreases in testing and PrEP use, but only small reductions in numbers of sexual partners [45].
It is surprising that reported levels of social contacts were lower among the seropositive compared with the seronegative before, during, and after the pandemic. It may have been that these participants were able to safely create opportunities to socialize and/or engage in sexual activities while only minimally increasing transmission risk (e.g. through creating “pods”). It is also possible that these data reflect a reporting bias; i.e., that participants that were aware that they had had COVID-19 underreported their social contacts during the pandemic. This would be supported by the fact that seropositive participants reported more sexual partners during the study period (median 6.5 vs. 5.0). Since these numbers were reported in real time during the pandemic and most likely prior to knowledge of COVID-19 status, it is unlikely that they were affected by reporting bias. Finally, it may be that those who were symptomatic may have been more likely to isolate after their symptomatic episode, or during specific time periods during the pandemic. Future studies on these behavioral aspects of sexual health could incorporate qualitative research to better understand these findings.
The lack of association of education and other sociodemographic characteristics with seropositivity is similar to what was found in the overall Swiss population in the first wave of the pandemic, where only younger age was associated with increased seropositivity [25]. This may reflect high compliance with overall social distancing measures during the initial phases of the pandemic in Switzerland.
Strengths and limitations
This study adds new evidence to the limited research on how sexual contact with non-steady partners was associated with SARS-CoV-2 seropositivity during the first lockdown in Zurich, Switzerland. The data on sexual behavior was collected prospectively as part of routine PrEP visits and was integrated into their clinical care, meaning that recall bias is likely minimized compared to other retrospective studies of behavior change during the pandemic. The availability of matched population level comparison data from the representative Corona Immunitas study provides a robust comparison group that has been missing from previous studies.
This study is subject to some limitations. Participants in this study were those that did not discontinue use of PrEP during the initial pandemic lockdown, meaning that they are likely less risk averse than participants that did stop attending their PrEP visits during this time. The number of people who were seropositive in this cohort was small (n = 19), meaning that the data on behavioral and demographic patterns in seropositivity need to be interpreted with caution. SwissPrEPared participants that did not participate in the Corona Immunitas substudy may have differed from those that did in their attitude towards the pandemic, compliance with social distancing measures, and therefore risk of SARS-CoV-2 infection; however, data are not available on compliance with social distancing or seropositivity in the other SwissPrEPared participants. In addition, similar information on sexual behaviors during the lockdown was not available for sexually active individuals not on PrEP or those on PrEP but not part of the SwissPrEPared program during this time period, so it is not possible to compare this group with other sexually active groups (e.g. heterosexuals). As mentioned above, there is a possibility of reporting bias, with those who had symptoms of COVID-19 remembering being more cautious than they really were. However, data on sexual behavior was reported as part of routine PrEP follow-up visits, making it unlikely that underreporting is linked to COVID-19 status. In addition, data was only collected on the number of sexual partners, not the total number of sexual contacts, which may represent a more important measure of exposure to infection. Finally, there was likely residual confounding in the comparison between the cohort of people taking PrEP and the general male population in Zurich.
Conclusions
Overall, SARS-CoV-2 seropositivity during the first pandemic wave was slightly elevated in a cohort of people taking PrEP compared to the general male population in Zurich, Switzerland. Our study suggests that at least in the first wave of lockdown, socializing and sexual activity were less important than other factors in SARS-CoV-2 seropositivity among those taking PrEP. While we cannot retrospectively identify precisely what those factors were, the association of seropositivity with international travel and deprioritization of health protection measures such as vaccination suggest that these factors may have played a role. Those who were less likely to prioritize precautionary measures such as vaccines may also have been less likely to prioritize complying with social distancing measures.
Acknowledgements
We would like to thank the participants in the study for their time and and contributions to the study, as well as the study administrative staff for their dedicated support of the study.
Author contributions
Conceptualization: B.H., A.Fr., A.Fa.; Methodology: B.H., A.Fa., A.Fr., M.Re., M.A.P., J.S.R., ; Formal analysis and investigation: A.Fa.; Writing - original draft preparation: A.Fa.; Writing - review and editing: B.H., J.K., L.J.S., O.J.K., M.Re., M.Ra., M.A.P., J.S.R.; Funding acquisition: B.H., M.A.P., J.S.R.; Supervision: B.H., A.Fr., J.S.R., M.A.P.
Funding
This study is part of Corona Immunitas research network, coordinated by the Swiss School of Public Health (SSPH+), and funded by fundraising of SSPH + including funds of the Swiss Federal Office of Public Health and private funders (ethical guidelines for funding stated by SSPH + were respected). Financial support from the Swiss Federal Office of Public Health (FOPH) was received by the SwissPrEPared program and study. The funding bodies had no influence on the design, conduct, analysis or interpretation of the study, nor on the decision to publish, the preparation or revisions of the manuscript.
Data availability
De-identified individual participant data underlying the findings and the codes used for this study will be available for researchers. Requests can be made to the Executive Committee of Corona Immunitas [https://zenodo.org/record/7520125] or to the corresponding author.
Declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The SwissPrEPared study (NCT03893188) was approved by the lead ethical committee (EC) in Zurich on 14 May 2019 (BASEC Nr. 2018 − 02015), followed by the approval of all ECs from the other cantons. The Corona Immunitas study was approved by the lead EC in Zurich (BASEC Nr. 2020 − 01247), followed by the approval of all ECs from the other cantons. Informed consent was obtained from all individual participants included in the study.
Consent for publication
not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Winter BL, Hovaguimian F, Kouyos RD, et al. <ArticleTitle Language="En">Changes in mental and sexual health among MSM using HIV pre-exposure prophylaxis during the SARS-CoV-2 pandemic: longitudinal analysis of the SwissPrEPared cohort study. Swiss Med Wkly. 2022;152:w30192. [DOI] [PubMed] [Google Scholar]
- 2.Bzdok D, Dunbar RIM. Social isolation and the brain in the pandemic era. Nat Hum Behav. 2022;6:1333–43. [DOI] [PubMed] [Google Scholar]
- 3.Di Fazio N, Morena D, Delogu G, et al. Mental Health Consequences of COVID-19 Pandemic Period in the European Population: An Institutional Challenge. Int J Environ Res Public Health. 2022;19. 10.3390/ijerph19159347. [DOI] [PMC free article] [PubMed]
- 4.Penninx BWJH, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022;28:2027–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herrmann WJ, Oeser P, Buspavanich P, Lech S, Berger M, Gellert P. Loneliness and depressive symptoms differ by sexual orientation and gender identity during physical distancing measures in response to COVID-19 pandemic in Germany. Appl Psychol Health Well-Being. 2023;15:80–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eleuteri S, Alessi F, Petruccelli F, Saladino V. The Global Impact of the COVID-19 Pandemic on Individuals’ and Couples’ Sexuality. Front Psychol. 2022;12. 10.3389/fpsyg.2021.798260. https://www.frontiersin.org/articles/. [DOI] [PMC free article] [PubMed]
- 7.Gul P, Keesmekers N, Elmas P, et al. Disease Avoidance Motives Trade-Off Against Social Motives, Especially Mate-Seeking, to Predict Social Distancing: Evidence From the COVID-19 Pandemic. Soc Psychol Personal Sci. 2022;13:1281–93. [Google Scholar]
- 8.Amerio A, Lugo A, Bosetti C, et al. Italians Do It … Less. COVID-19 Lockdown Impact on Sexual Activity: Evidence From a Large Representative Sample of Italian Adults. J Epidemiol. 2021;31:648–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McKay T, Henne J, Gonzales G, Quarles R, Gavulic K, Gallegos SG. The COVID-19 Pandemic and Sexual Behavior among Gay and Bisexual Men in the United States. 2020. 10.2139/ssrn.3614113 [DOI] [PMC free article] [PubMed]
- 10.Holloway IW, Garner A, Tan D, Ochoa AM, Santos GM, Howell S. Associations Between Physical Distancing and Mental Health, Sexual Health and Technology Use Among Gay, Bisexual and Other Men Who Have Sex With Men During the COVID-19 Pandemic. J Homosex. 2021;68:692–708. [DOI] [PubMed] [Google Scholar]
- 11.Hammoud MA, Maher L, Holt M et al. Physical Distancing Due to COVID-19 Disrupts Sexual Behaviors Among Gay and Bisexual Men in Australia: Implications for Trends in HIV and Other Sexually Transmissible Infections. JAIDS J Acquir Immune Defic Syndr 2020; 85. https://journals.lww.com/jaids/fulltext/2020/11010/physical_distancing_due_to_covid_19_disrupts.9.aspx [DOI] [PubMed]
- 12.Stephenson R, Sullivan SP, Pitter RA, Hunter AS, Chavanduka TMD. Are We Still Having Sex? Results of Round Two of the Love and Sex in the Time of COVID Survey with Gay, Bisexual and Other Men Who Have Sex with Men. AIDS Behav. 2022;26:2338–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanchez TH, Zlotorzynska M, Rai M, Baral SD. Characterizing the Impact of COVID-19 on Men Who Have Sex with Men Across the United States in April, 2020. AIDS Behav. 2020;24:2024–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Starks TJ, Jones SS, Sauermilch D, et al. Evaluating the impact of COVID-19: A cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug Alcohol Depend. 2020;216:108260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jack RG, Brown D, Reid AR, Howarth et al. Sexual behaviour, STI and HIV testing and testing need among gay, bisexual and other men who have sex with men recruited for online surveys pre/post-COVID-19 restrictions in the UK. Sex Transm Infect 2023;sextrans-2022-055689. [DOI] [PMC free article] [PubMed]
- 16.Uhrmacher M, Skaletz-Rorowski A, Nambiar S, et al. HIV pre-exposure prophylaxis during the SARS-CoV-2 pandemic: Results from a prospective observational study in Germany. Front Public Health. 2022;10. 10.3389/fpubh.2022.930208. https://www.frontiersin.org/articles/. [DOI] [PMC free article] [PubMed]
- 17.Weidlich S, Schneider J, Lee M, et al. Seroconversion rate of SARS-CoV-2 IgG antibodies and dating behaviour in HIV-PrEP users in a German metropolis during the COVID-19 pandemic. Int J STD AIDS. 2023. 09564624231190419. [DOI] [PMC free article] [PubMed]
- 18.Ringshall M, Cooper R, Rawdah W, et al. Chemsex, sexual behaviour and STI-PrEP use among HIV-PrEP users during the COVID-19 pandemic in Brighton, UK. Sex Transm Infect. 2022;98:312–312. [DOI] [PubMed] [Google Scholar]
- 19.van Bilsen WPH, Zimmermann HML, Boyd A et al. Sexual Behavior and Its Determinants During COVID-19 Restrictions Among Men Who Have Sex With Men in Amsterdam. JAIDS J Acquir Immune Defic Syndr 2021; 86. https://journals.lww.com/jaids/fulltext/2021/03010/sexual_behavior_and_its_determinants_during.4.aspx [DOI] [PMC free article] [PubMed]
- 20.Rogers BG, Tao J, Darveau SC, et al. The Impact of COVID-19 on Sexual Behavior and Psychosocial Functioning in a Clinical Sample of Men who have Sex with Men Using HIV Pre-exposure Prophylaxis. AIDS Behav. 2022;26:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hovaguimian F, Martin E, Reinacher M, et al. Participation, retention and uptake in a multicentre pre-exposure prophylaxis cohort using online, smartphone-compatible data collection. HIV Med. 2022;23:146–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.EACS Guidelines 10.0. 2019. https://www.eacsociety.org/guidelines/eacs-guidelines/
- 23.Amati R, Frei A, Kaufmann M et al. Functional immunity against SARS-CoV-2 in the general population after a booster campaign and the Delta and Omicron waves, Switzerland, March 2022. Eurosurveillance 2022; 27. 10.2807/1560-7917.ES.2022.27.31.2200561 [DOI] [PMC free article] [PubMed]
- 24.Frei A, Kaufmann M, Amati R, et al. Development of hybrid immunity during a period of high incidence of Omicron infections. Int J Epidemiol. 2023;52:1696–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tancredi S, Chiolero A, Wagner C, et al. Seroprevalence trends of anti-SARS-CoV-2 antibodies and associated risk factors: a population-based study. Infection. 2023;51:1453–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amati R, Piumatti G, Franscella G, et al. Trajectories of Seroprevalence and Neutralizing Activity of Antibodies against SARS-CoV-2 in Southern Switzerland between July 2020 and July 2021: An Ongoing, Prospective Population-Based Cohort Study. Int J Environ Res Public Health. 2023;20. 10.3390/ijerph20043703. [DOI] [PMC free article] [PubMed]
- 27.West EA, Kotoun OJ, Schori LJ, et al. Seroprevalence of SARS-CoV-2 antibodies, associated factors, experiences and attitudes of nursing home and home healthcare employees in Switzerland. BMC Infect Dis. 2022;22:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.West EA, Anker D, Amati R, et al. Corona Immunitas: study protocol of a nationwide program of SARS-CoV-2 seroprevalence and seroepidemiologic studies in Switzerland. Int J Public Health. 2020;65:1529–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bruggmann P, Senn O, Frei A, Puhan MA, Fehr J, Falcato L. High SARS-CoV-2 seroprevalence but no severe course of COVID-19 disease among people on opioid agonist treatment in Zurich: a cross-sectional study. Swiss Med Wkly. 2022;152:w30122. [DOI] [PubMed] [Google Scholar]
- 30.Fenwick Craig C, Antony C, Alix T, et al. Changes in SARS-CoV-2 Spike versus Nucleoprotein Antibody Responses Impact the Estimates of Infections in Population-Based Seroprevalence Studies. J Virol. 2021;95. 10.1128/jvi.01828-20. [DOI] [PMC free article] [PubMed]
- 31.Ho D, Imai K, King G, Stuart EA. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J Stat Softw. 2011;42:1–28. [Google Scholar]
- 32.Greifer N. cobalt: Covariate Balance Tables and Plots. 2023 https://ngreifer.github.io/cobalt/
- 33.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. 2023 https://www.R-project.org/
- 34.Liu T, Gong D, Xiao J, et al. Cluster infections play important roles in the rapid evolution of COVID-19 transmission: A systematic review. Int J Infect Dis. 2020;99:374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Westmoreland DA, Pantalone DW, Patel VV, Hoover D, Nash D, Grov C, Demographic. Behavioral, and Geographic Differences Between Men, Transmen, and Transwomen Currently on PrEP, Former PrEP Users, and Those Having Never Used PrEP. AIDS Behav. 2020;24:1304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Charlett A, Hiironen I, Hughes GJ, et al. Workplace exposures associated with COVID-19: evidence from a case-control study with multiple sampling periods in England, August–October 2020. Epidemiol Infect. 2022;150:e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murti M, Achonu C, Smith BT et al. COVID-19 Workplace Outbreaks by Industry Sector and Their Associated Household Transmission, Ontario, Canada, January to June, 2020. J Occup Environ Med 2021; 63. https://journals.lww.com/joem/fulltext/2021/07000/covid_19_workplace_outbreaks_by_industry_sector.5.aspx [DOI] [PMC free article] [PubMed]
- 39.Fine PEM, Chen RT. Confounding in Studies of Adverse Reactions to Vaccines. Am J Epidemiol. 1992;136:121–35. [DOI] [PubMed] [Google Scholar]
- 40.Huang K, Lin S-W, Sheng W-H, Wang C-C. Influenza vaccination and the risk of COVID-19 infection and severe illness in older adults in the United States. Sci Rep. 2021;11:11025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eoin McElroy E, Herrett K, Patel, et al. Living alone and mental health: parallel analyses in UK longitudinal population surveys and electronic health records prior to and during the COVID-19 pandemic. BMJ Ment Health. 2023;26:e300842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Madewell ZJ, Yang Y, Longini IM Jr, Halloran ME, Dean NE. Household Transmission of SARS-CoV-2: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020;3:e2031756–2031756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Böhm S, Böhmer MM, Chen D, et al. Epidemiology and transmission characteristics of early COVID-19 cases, 20 January–19 March 2020, in Bavaria, Germany. Epidemiol Infect. 2021;149:e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Menkir TF, Chin T, Hay JA, et al. Estimating internationally imported cases during the early COVID-19 pandemic. Nat Commun. 2021;12:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goodreau SM, Delaney KP, Zhu W, et al. Impacts of COVID-19 on sexual behaviors, HIV prevention and care among men who have sex with men: A comparison of New York City and Metropolitan Atlanta. PLoS ONE. 2023;18:e0282503. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified individual participant data underlying the findings and the codes used for this study will be available for researchers. Requests can be made to the Executive Committee of Corona Immunitas [https://zenodo.org/record/7520125] or to the corresponding author.