Abstract
Introduction
In Africa, healthcare professionals experienced various mental health problems during COVID-19. However, very little was done on the extensive evidence regarding mental disorders. The purpose of this umbrella review is to provide comprehensive data on the prevalence of anxiety, depression, stress, and insomnia among healthcare professionals during the COVID-19 pandemic in Africa.
Materials and Methods
Systematic searches of databases African Journals Online, MedRxiv, PubMed, and Google Scholar were used to identify studies from the occurrence of COVID-19 from December 2019 to March 2023 were included. To pool the gathered data for results with a 95% confidence interval (CI), DerSimonian-Laird random effects meta-analysis was used. For heterogeneity examination, I2 was used. The quality assessment was evaluated by using the Joanna Briggs Institute (JBI) critical appraisal checklist.
Results
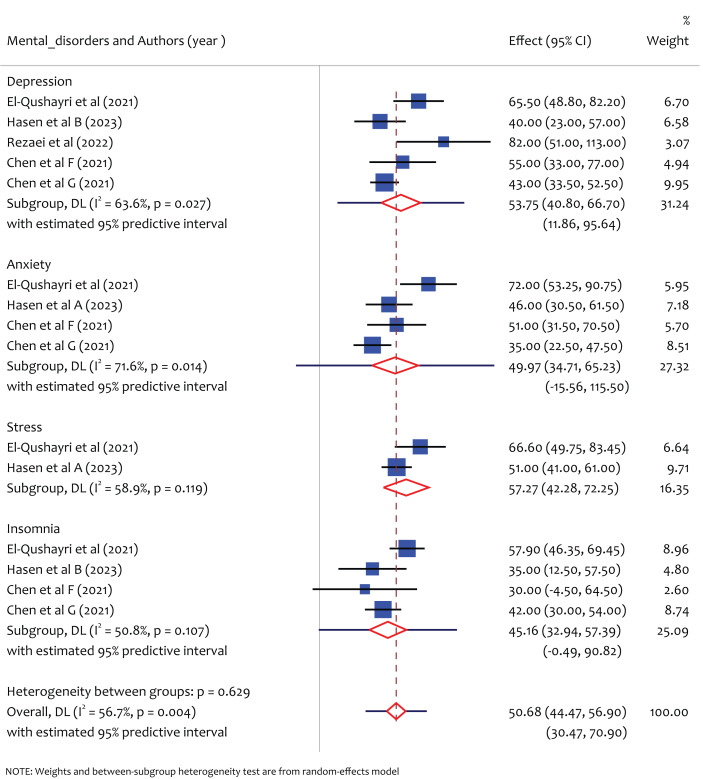
A total of five studies reported the prevalence of depression, the pooled prevalence was 53.75% (95% CI [40.80–66.70], I2 = 63.6%, p = 0.027). In a total of four studies, the pooled prevalence of anxiety was 49.97% (95% CI [34.71–65.23], I2 = 71.26%, p = 0.014). From a total of two studies, the pooled prevalence of stress was 57.27% (95% CI [42.28–72.25], I2 = 58.9%, p = 0.119). From a total of four studies, the pooled prevalence of insomnia was 45.16% (95% CI [32.94–57.39], I2 = 50.8%, p = 0.107).
Conclusions
The COVID-19 pandemic highly affects the mental health of healthcare professionals in Africa. Stress, depression, anxiety, and insomnia symptoms were representing the most common based on evidences from existing meta-analyses. This evidence can help experts when executing specific interventions that address mental health problems among healthcare professionals during future public health crises.
Keywords: COVID-19, Mental health, Mental disorders, Healthcare professionals, Anxiety, Depression, Stress, Insomnia, Umbrella review, Africa
Introduction
The coronavirus was initially reported in Wuhan City, China, in December 2019, which has spread worldwide (World Health Organization, 2020). In terms of COVID-19 protection and management, healthcare professionals are at the forefront. The stressors related to COVID-19 pandemic, coupled with the fear of infection and the emotional toll of witnessing suffering and loss among patients, contribute to detrimental effects on mental health. Due to their duty they are vulnerable to COVID-19, and the high contact rate with COVID-19 patients result in stress and depression during the pandemic (Asnakew, Amha & Kassew, 2021; Shaukat, Mansoor Ali & Razzak, 2020).
The COVID-19 pandemic has had a profound impact on healthcare professionals worldwide, including those in Africa. The healthcare workforce in Africa has long been under-resourced and overburdened, with high levels of burnout and mental health issues already prevalent before the pandemic. The added stress and pressure of the COVID-19 pandemic have likely exacerbated these issues, leading to higher rates of depression, anxiety, stress, and insomnia among healthcare professionals. The ongoing COVID-19 pandemic has affected healthcare systems everywhere, particularly in Africa, with challenges that have never been seen before. The continent has a fragile healthcare infrastructure and limited resources to combat the pandemic’s effects, leading healthcare professionals to face significant physical, emotional, and psychological strains. COVID-19 pandemic and related restrictions can impact mental health (Dragioti et al., 2022). The fear, worry, and uncertainty surrounding such an unknown threat and containment strategies can put a burden on mental health (Chen et al., 2021). A significant number of HCWs manifest various psychological problems in Africa. According to Olashore et al. (2021) reported the psychological impact of COVID-19 on health care workers in African countries and the most common psychological problems were anxiety disorder (with rates ranging from 9.5% to 73.3%) and depression (with rates ranging from 12.5% to 71.9%). The pandemic impacts African healthcare workers through insomnia, depression, and fear of safety in their families (Nchasi et al., 2022).
In Africa until March 2024, about 12,381,551 COVID-19 confirmed cases and 259,261 death were reported by Africa CDC (2024). Africa, as a continent, presents a diverse range of challenges for healthcare professionals. Many countries in Africa struggle with limited resources, inadequate infrastructure, high patient-to-staff ratios, and a lack of mental health support systems. These challenges often place a significant burden on healthcare professionals, leading to increased stress levels, burnout, and ultimately, the development of mental health problems. Likewise, the tension of the pandemic on healthcare professionals cannot be understated. With an unprecedented number of patients, a shortage of necessary medical supplies, and major protocol changes, healthcare workers are being pushed to the brink of their limits. Many are forced to work long hours and take on significantly more patients than they would normally be expected to handle. Moreover, the fact that the threat of COVID-19 lingers has illuminated the higher risk that many healthcare professionals face. To address the mental health crisis amongst healthcare professionals, it is important for employers and healthcare organizations to offer their staff more support. This support can come in the form of offering additional time off, providing counseling services and emotional support, or opening up channels for communication to ensure that healthcare professionals feel heard (Hasen, Seid & Mohammed, 2023c).
During the pandemic, healthcare workers are affected by mental disorders (Hill et al., 2022). The higher prevalence rates of depression in the African population compared to elsewhere (Chen et al., 2021). South Africa’s healthcare professionals working in a tertiary hospital were with high levels of mental health problems during the early COVID-19, and the prevalence of mental distress was 57.4% (Lee et al., 2022). During COVID-19, the prevalence of mental distress was 92.7% among Ugandan health workers (Kirabira et al., 2022). Also in Egypt, HCWs had a high prevalence of anxiety, at 49.38%, insomnia at 56.17%, and poor sleep quality at 67.9% (Al-Otaibi et al., 2022). During the pandemic studies in Ethiopia presented that the prevalence of stress on healthcare professionals was 78.3% (Yitayih et al., 2021), 61.8% (Teshome et al., 2020), 63.7% (Asnakew, Amha & Kassew, 2021), 40.2% (Hajure et al., 2021), 42% (Tsehay, Belete & Necho, 2020), 51.6% (Chekole et al., 2020), 31.4% (GebreEyesus et al., 2021), study in Egypt 66.6% (El-qushayri et al., 2021). and 55.1% (Asnakew, Amha & Kassew, 2021).
Likewise studies in Ethiopia reported that the prevalence of insomnia was 15.9% (Jemal et al., 2021), 50.20% (Yitayih et al., 2021) and 40.8% (Habtamu et al., 2021; Zhang et al., 2021) and global study prevalence was 34.4% (Batra et al., 2020), in Egypt 71.8% (El-qushayri et al., 2021) 73.3% (Sagaon-Teyssier et al. 2020), in Kenya 36% (Kwobah et al., 2021). A global meta-analysis result on the prevalence of anxiety among HCWs found that it was 23.2%, depression 22.8%, and insomnia 38.9% (Rezaei-Hachesu et al., 2022). Besides, a review of studies found that the worldwide prevalence of mental disorders among healthcare workers was between 29.9% and 32.7% had anxiety, 28.4% to 31.3% had depression, and about 40% had sleeping problems (Dragioti et al., 2020). The study findings in the prevalence of mental disorders among healthcare workers with wide disparity evident during this pandemic in Africa (Fernandez et al., 2021). Yet, little reviews were done in Africa regarding the prevalence of mental health problems among healthcare professionals during COVID-19.
Hence, a pooled summary of the results of the meta-analyses on the prevalence of mental health problems among African healthcare professionals during COVID-19 is crucial. This research intends to provide thorough data on the impact of the COVID-19 pandemic on the mental health of healthcare professionals in Africa. Studying an umbrella review on these mental health problems among healthcare professionals in Africa during COVID-19 can provide valuable insights into the magnitude of the problem, the risk factors involved, and potential interventions that can help support the mental well-being of healthcare workers in the region. This research can inform policies and practices aimed at mitigating the impact of the pandemic on the mental health of healthcare professionals and ultimately improving their overall well-being and ability to provide quality care to patients.
Objective
The main goal of this study is to present thorough data on the prevalence of mental health problems among healthcare professionals through COVID-19 in Africa.
Materials and Methods
Protocol registration
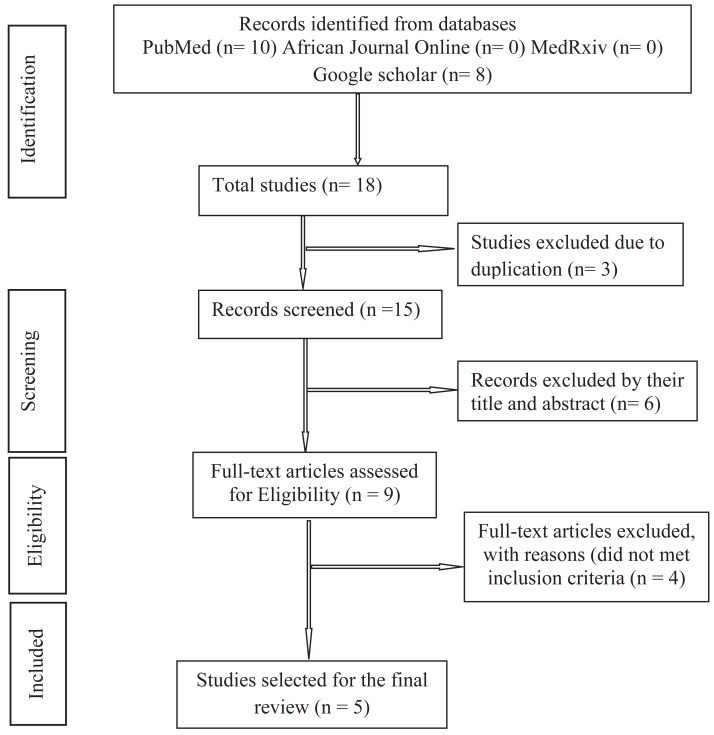
We performed an umbrella review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA 2020) guidelines for reporting of systematic reviews and meta-analyses presented in Fig. 1. The protocol was registered in the International Prospective Register of Systematic Reviews with PROSPERO registration number: CRD42022383939.
Figure 1. Preferred reporting items for systematic reviews and meta-analysis (PRISMA) flow diagram.
Search strategy
PubMed, African Journal Online, MedRxiv and Google Scholar databases were searched and articles published from the occurrence of COVID-19 from December 2019 to March 2023 were included. Studies from systematic reviews and meta-analyses were taken into consideration to measure the pooled prevalence mental health problems among healthcare professionals in Africa. Every possible keyword combinations were included in systematic searches. Mendeley removed duplicates from the search results (Kwon et al., 2015). The following search terms were used: “COVID-19”, “COVID-19 virus”, “2019 novel corona virus disease”, “SARS CoV-2 infection”, “COVID-19 pandemic”, “COVID-19 infection”, “mental disorder”, “mental illness”, “anxiety”, “depression”, “sleep quality”, “insomnia”, “health workers”, “healthcare professionals”, “nurses”, “doctors”, “pharmacists”, “Ethiopia”, “Algeria”, “Angola”, “Benin”, “Botswana”, “Burkina Faso””, Burundi”, “Cabo Verde”, “Cameroon”, “Central African Republic (CAR)”, “Chad”, “Comoros”, “Congo”, “Democratic Republic of the Congo”, ”Republic of the Cote d’Ivoire”, “Djibouti”, “Egypt”, “Equatorial Guinea”, “Eritrea”, “Eswatini”, “Gabon”, “Gambia”, “Ghana”, “Guinea”, “Guinea-Bissau”, “Kenya”, “Lesotho”, “Liberia”, “Libya”, “Madagascar”, “Malawi”, “Mali”, “Mauritania”, “Mauritius”, “Morocco”, “Mozambique”, “Namibia”, “Nigeria”, “Nigeria”, “Rwanda”, “Sao Tome and Principe”, “Senegal”, “Seychelles”, “Sierra Leone”, “Somalia”, “South Africa”, “South Sudan”, “Sudan”, “Tanzania”, “Togo”, “Tunisia”, “Uganda”, “ Zambia”, “Zimbabwe” (Hasen, Seid & Mohammed, 2023c). Two researchers (AAH and AAS) have screened the titles and abstracts of the studies independently, and any differences between the researchers were resolved by consensus or by the third author (AAM). The search strategy of database is presented in Table 1.
Table 1. The search strategy of databases.
| Search number | Search detail |
|---|---|
| #1 | “COVID-19”[MeSH Terms] |
| #2 | “mental illness”[Mesh Terms] |
| #3 | “COVID-19”[Title/Abstract] OR COVID-19 infection ”[Title/Abstract] OR “SARS Cov-2 infection Title/Abstract] OR “COVID-19 pandemic”[Title/Abstract] OR “new corona virus” [Title/Abstract] AND “health care professionals”[Title/Abstract] OR “health workers”[Title/Abstract] OR “nurses”[Title/Abstract] OR “doctors”[Title/Abstract] OR “pharmacists”[Title/Abstract] OR “health care workers”[Title/Abstract] AND “Ethiopia” [Title/Abstract] OR “Algeria” [Title/Abstract] OR“Angola” OR “Benin” [Title/Abstract] OR “Botswana” [Title/Abstract]OR“Burkina Faso” [Title/Abstract]OR “Burundi” [Title/Abstract]OR “Cabo Verde” [Title/Abstract] OR“Cameroon” [Title/Abstract] OR “Central African Republic (CAR)” [Title/Abstract] OR“Chad” [Title/Abstract] OR “Comoros” [Title/Abstract] OR “Congo” [Title/Abstract] OR“Democratic Republic of the Congo” [Title/Abstract] OR”Republic of the Cote d’Ivoire” [Title/Abstract] OR “Djibouti” [Title/Abstract] OR“Egypt”[Title/Abstract], OR“East Africa”[Title/Abstract] OR“South Africa”[Title/Abstract]OR“North Africa”[Title/Abstract] OR“East Africa”[Title/Abstract] OR “Centeral Aftica”[Title/Abstract] OR“West Africa”[Title/Abstract] |
| #4 | “mental illness” [Title/Abstract] OR “psychiatric problem” [Title/Abstract] OR “mental disorders” [Title/Abstract] AND “anxiety” [Title/Abstract] OR “depression” [Title/Abstract] OR “insomnia” [Title/Abstract] OR “stress” [Title/Abstract] OR “psychology problem” [Title/Abstract] OR “mental health effect” [Title/Abstract] OR “psychological disturbance” [Title/Abstract] AND “meta-analysis” [Title/Abstract] OR “systematic review” [Title/Abstract] |
| #5 | #1 AND #2 |
| #6 | #3 AND #5 |
| #7 | #4 AND #6 |
| #8 | Limit to systematic review OR meta analysis |
Eligibility criteria
Inclusion criteria
For this umbrella review all systematic review and meta-analysis studies that focused on healthcare professionals and investigations on the impacts of COVID-19 on the mental health of healthcare professionals in Africa were included. This study is employed following the condition, context and population (CoCoPop) framework for the organization of search terms.
Condition: Mental health problems.
Context: Studies conducted in Africa during the COVID-19 pandemic.
Population: This study includes systematic review and meta-analysis studies involving healthcare professionals as a whole.
Study design: Systematic review and meta-analysis studies that report on the prevalence of mental health problems among healthcare professionals during COVID-19 in Africa.
Language: Only studies reported in English.
Publication year: Studies published until March, 2023.
Exclusion criteria
The following studies were excluded: single-level studies i.e., observational studies, studies that included whole population, descriptive reviews, randomized controlled trials, editorials, comments, conference abstracts and expert opinions were excluded.
Outcome measures
The pooled prevalence of mental health problems such as anxiety, depression, stress and insomnia among health care professionals during the COVID-19 pandemic in Africa is the primary outcome in this umbrella review.
Selection of studies
Two researchers (AAH and AAS) measured the studies based on inclusion and exclusion criteria. Firstly, they evaluated both the titles and abstracts of the studies identified from the searched databases. Then full-text screening was done to screen the full texts selected in the previous stage. Besides, we have a justification for the inclusion and exclusion of studies in the PRISMA flow diagram. Finally, the lists of eligible studies for this umbrella review were prepared.
Methodological quality assessment
Two researchers (AAH and AAS) assessed the quality of the included studies by Joanna Briggs Institute’s (JBI) critical appraisal checklist for systematic reviews and research syntheses (Perera et al., 2021). This method assessed the following items: (1) Is the review question clearly and explicitly stated? (2) Were the inclusion criteria appropriate for the review question? (3) Was the search strategy appropriate? (4) Were the sources and resources used to search for studies adequate? (5) Were the criteria for appraising studies appropriate? (6) Was critical appraisal conducted by two or more reviewers independently? (7) Were there methods to minimize errors in data extraction? (8) Were the methods used to combine studies appropriate? (9) Was the likelihood of publication bias assessed? (10) Were recommendations for policy and/or practice supported by the reported data? (11) Were the specific directives for new research appropriate? , and the question in the checklist were answered as “yes”, “no”, “unclear” and Not applicable “NA”(Aromataris et al., 2017). Each entry was evaluated with “yes” or “no”, and the number of “yes” will be counted. Studies score higher than 70% are considered high quality, between 50% and 70% are medium quality and those with a score less than 50% are considered low quality (Hou et al., 2017). Studies with medium and above quality score were considered for analysis.
Data extraction
Two researchers (AAH and AAS) screened the titles and abstracts of all identified articles for eligibility. The required data for this study was extracted by piloted data collection format. After initially screening articles for inclusion based on titles and abstracts, full-text articles were screened. Differences were resolved by deep discussion with a researcher (AAM) to reach an agreement. Data were collected from the selected studies containing, the author’s name, year of publication, country, study design, study population, quality assessment method, searched databases, search restrictions, number of studies, number of reviewers, type of mental illnesses includes depression, anxiety, stress and insomnia, instrument pooled prevalence of mental illness with corresponding 95% confidence interval (CI) were collected.
Data synthesis
Stata version 14.0 (StataCorp, College Station, TX, USA) software was used to conduct this umbrella review. We have calculated pooled prevalence for each mental health problem along with a 95% CI and corresponding p-value. Heterogeneity among eligible study’s findings was assessed using the I2 test, and if I2 >50%, it is considered as a significant heterogeneity (Feilong Zhu et al., 2020). To pool the collected data for each outcome with a 95% CI, DerSimonian-Laird random effects meta-analysis was used.The systematic review characteristics are presented in a tabular form and descriptively. Results of the pooled prevalence of anxiety, depression, stress and insomnia are presented as % with 95% CIs and are graphically presented in the forest plot.
Results
This umbrella review summarized the meta-analysis study findings in Africa on the prevalence of mental health problems among healthcare professionals during the COVID-19 pandemic. Figure 1 shows a PRISMA diagram of the steps in the database search and refinement process for the study of healthcare professionals’ mental health issues during the COVID-19 pandemic. Initial results from our database search included 18 studies. Six studies were removed after 15 studies’ titles and abstracts were examined and three duplicates were removed. There were nine full-text studies examined, and four were excluded for reasons that did not meet the inclusion criteria i.e. single-level studies and studies not in Africa. At long last, we perceived five studies proper to this umbrella review.
Study characteristics
In this umbrella review, we included five systematic review and meta-analysis studies (Rezaei et al., 2022; Hasen, Seid & Mohammed, 2023a; Hasen, Seid & Mohammed, 2023b; El-qushayri et al., 2021; Chen et al., 2021) focused on the impact of COVID-19 on the mental health of healthcare professionals in Africa. The selected meta-analyses were published between 2021 and 2023. When we see the regional/country distribution, one study (El-qushayri et al., 2021) was from Egypt, two studies (Hasen, Seid & Mohammed, 2023a; Hasen, Seid & Mohammed, 2023b) were from Ethiopia, two studies (Rezaei et al., 2022; Chen et al., 2021) were from whole Africa. Depending on the types of mental disorders three studies (Hasen, Seid & Mohammed, 2023a; El-qushayri et al., 2021; Chen et al., 2021) were reported anxiety, four studies (Rezaei et al., 2022; Hasen, Seid & Mohammed, 2023b; El-qushayri et al., 2021; Chen et al., 2021) were reported about depression, two studies (Hasen, Seid & Mohammed, 2023a; El-qushayri et al., 2021) were reported about stress and three studies (Hasen, Seid & Mohammed, 2023b; El-qushayri et al., 2021; Chen et al., 2021) were reported about insomnia.
Regarding the quality appraisal instruments used in the included reviews; three studies used the Newcastle–Ottawa Scale (Rezaei et al., 2022; Hasen, Seid & Mohammed, 2023a; Hasen, Seid & Mohammed, 2023b), one study used the National institute of health quality assessment tool (El-qushayri et al., 2021) and one study applied Mixed Methods Appraisal Tool (Chen et al., 2021). Publication bias was reported in three studies (Hasen, Seid & Mohammed, 2023a; Rezaei et al., 2022; Chen et al., 2021) and two studies (El-qushayri et al., 2021; Hasen, Seid & Mohammed, 2023b) do not report it. In addition, Table 2 contains a summary of the key characteristics of the included studies.
Table 2. Key characteristics of included studies for umbrella review of mental health problems among healthcare professionals during COVID-19 in Africa.
| No | Authors | Year | Region/ country | Mental illness | Study Population | Study design | Quality assessment | Searched databases | Search restrictions | # studies | # reviewers | Pooled prevalence % | 95% CI | I2 % | Pubcation bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | El-qushayri1 et al. | 2021 | Egypt | Anxiety | HCWS | SR & MA | National institute of health quality assessment tool | Google Scholar, Scopus, The System For Information on Grey Literature in Europe, Pubmed, The New York Academy of Medicine, and Web of Science | 30 December 2020 to 15 January 2021 | 4 | 7 | 72 | 49.4–86.9 | NR | NR |
| Depression | HCWS | SR & MA | National institute of health quality assessment tool | Google Scholar, Scopus, The System For Information on Grey Literature in Europe, Pubmed, The New York Academy of Medicine, and Web of Science | 30 December 2020 to 15 January 2021 | 5 | 7 | 65.50 | 46.9–80.3 | 98 | NR | ||||
| Stress | HCWS | SR & MA | National institute of health quality assessment tool | Google Scholar, Scopus, The System For Information on Grey Literature in Europe, Pubmed, The New York Academy of Medicine, and Web of Science | 30 December 2020 to 15 January 2021 | 7 | 7 | 66.60 | 47.6–81.3 | NR | NR | ||||
| Insomnia | HCWS | SR & MA | National institute of health quality assessment tool | Google Scholar, Scopus, The System For Information on Grey Literature in Europe, Pubmed, The New York Academy of Medicine, and Web of Science | 30 December 2020 to 15 January 2021 | 2 | 7 | 57.90 | 45.9–69.0 | NR | NR | ||||
| 2 | Hasen et al. A | 2023 | Ethiopia | Anxiety | HCWS | SR & MA | NOS | Pubmed, Cochrane Library, Crossref and Google Scholar | From the occurrence of COVID-19 pademic to June 2022 | 8 | 3 | 46 | 30–61 | 99.07 | No |
| Stress | HCWS | SR & MA | NOS | Pubmed, Cochrane Library, Crossref and Google Scholar | From the occurrence of COVID-19 pademic to June 2022 | 9 | 3 | 51 | 41–62 | 97.85 | No | ||||
| 3 | Hasen et al. B | 2023 | Ethiopia | Depression | HCWS | SR & MA | NOS | Pubmed, Cochrane Library, Crossref, African Journals Online And Google Scholar | From the occurrence of COVID-19 pademic to June 2022 | 7 | 3 | 40 | 23–57 | 99 | NR |
| Insomnia | HCWS | SR & MA | NOS | Pubmed, Cochrane Library, Crossref, African Journals Online And Google Scholar | From the occurrence of COVID-19 pademic to June 2022 | 3 | 3 | 35 | 13–58 | 98.2 | NR | ||||
| 4 | Rezaei et al. | 2022 | Africa | Depression | HCWS | SR & MA | NOS | Pubmed, EMBASE, Scopus, And Web of Science | January 2019 to February 2021 | 24 | 15 | 82 | 35–97 | NR | No |
| 5 | Chen et al. | 2021 | Africa | Anxiety | FLHCWS | SR & MA | MMAT | Pubmed, EMBASE, Web of Science, PsycINFO, and medRxiv | 1 February 2020 to 6 February 2021 | 3 | 12 | 51 | 31-70 | NR | No |
| Depression | FLHCWS | SR & MA | MMAT | Pubmed, EMBASE, Web of Science, PsycINFO, and medRxiv | 1 February 2020 to 6 February 2021 | 3 | 12 | 55 | 32-76 | NR | No | ||||
| Insomnia | FLHCWS | SR & MA | MMAT | Pubmed, EMBASE, Web of Science, PsycINFO, and medRxiv | 1 February 2020 to 6 February 2021 | 3 | 12 | 30 | 2–71 | NR | No | ||||
| Anxiety | GHCWS | SR & MA | MMAT | Pubmed, EMBASE, Web of Science, PsycINFO, and medRxiv | 1 February 2020 to 6 February 2021 | 12 | 12 | 35 | 23–48 | NR | No | ||||
| Depression | GHCWS | SR & MA | MMAT | Pubmed, EMBASE, Web of Science, PsycINFO, and medRxiv | 1 February 2020 to 6 February 2021 | 12 | 12 | 43 | 39–58 | NR | No | ||||
| Insomnia | GHCWS | SR & MA | MMAT | Pubmed, EMBASE, Web of Science, PsycINFO, and medRxiv | 1 February 2020 to 6 February 2021 | 12 | 12 | 42 | 31–55 | NR | No |
Notes.
- SR & MA
- Systematic review and meta-analysis
- MMAT
- Mixed methods appraisal tool
- NR
- not reported
- NOS
- Newcastle Ottawa Quality Assessment Scale
- HCWS
- healthcare workers
- FHCWS
- frontline healthcare workers
- GHCWS
- General healthcare workers
Quality of included studies
A quality score for the five included studies is shown in Table 3 using the Joanna Briggs Institute (JBI) critical appraisal checklist for systematic reviews and research syntheses. Accordingly, all studies (Rezaei et al., 2022; Hasen, Seid & Mohammed, 2023a; El-qushayri et al., 2021; Chen et al., 2021; Hasen, Seid & Mohammed, 2023b) were considered as high quality based on their JBI quality score higher than 70%, and thus considered for final umbrella review.
Table 3. Joanna Briggs Institute (JBI) critical appraisal checklist for systematic reviews and research syntheses.
| No | Study(year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Total (%) | Overall appraisal |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | El-qushayri et al. (2021) | Y | Y | Y | Y | Y | Y | N | Y | N | Y | Y | 9/11=81.81% | Include |
| 2 | Hasen, Alebachew Seid & Adem Mohammed (2023a) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11/11=100% | Include |
| 3 | Hasen, Alebachew Seid & Adem Mohammed (2023b) | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | 10/11=90.90% | Include |
| 4 | Rezaei et al. (2022) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11/11=100% | Include |
| 5 | Chen et al. (2021) | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | 10/11=90.90% | Include |
Notes.
- Y
- Yes
- N
- No
- U
- Unclear
- NA
- Not applicable
Study overlap assessment
To assess the study overlap we used the calculation of the overall corrected covered area (CCA) approach (Pieper et al., 2014). Accordingly we assessed the study overlap in studies of stress, anxiety, deprssion and insomnia. The CCA is reported as for stress CCA =0%, anxiety CCA =4.5%, depression CCA =3.3% and Insomnia CCA =11.1% a shown in Fig. S1. We found a high levelof overlap in insomia studies.
The pooled prevalence of depression, anxiety, stress, and insomnia
As shown in the forest plot (Fig. 2), the prevalence of common mental health problems (depression, anxiety, stress and insomnia) among healthcare professionals during COVID-19 in Africa was found to be high. Accordingly, a total of five studies reported the prevalence of depression, and the pooled prevalence of depression was found to be 53.75% (95% CI [40.80–66.70], I2 = 63.6%, p = 0.027), and I2 = 63.6%, indicating that there exists significant heterogeneity among study findings on the prevalence of depression among health care professionals through the pandemic in Africa. Similarly, four studies reported the prevalence of anxiety, and the pooled prevalence of anxiety was found to be 49.97% (95% CI [34.71–65.23], I2 = 71.26%, p = 0.014). There exists significant heterogeneity among study findings on the prevalence of anxiety among healthcare professionals in Africa through the pandemic I2 = 71.26%. This study also reported the pooled prevalence of stress, and from a total of 2 studies, the pooled prevalence of stress was 57.27% (95% CI [42.28–72.25], I2 = 58.9%, p = 0.119). No statistically significant heterogeneity of study results has been observed; this might be due to the limited studies included in the meta-analysis. Likewise, from a total of four studies, the pooled prevalence of insomnia was 45.16% (95% CI [32.94–57.39], I2 = 50.8%, p = 0.107), and no statistically significant heterogeneity of study results has been observed.
Figure 2. Forestplot of pooled prevalence of mental disorders among healthcare professionals during COVID-19 in Africa.
Discussion
The current comprehensive umbrella review aimed to determine the pooled prevalence of mental health problems during the COVID-19 pandemic among healthcare professionals in Africa. This review detected five systematic reviews and meta-analyses that evaluated the prevalence of mental health symptoms among healthcare professionals during the COVID-19 pandemic. From the included meta-analysis there is heterogeneity among studies. The variations might be: For example, study populations can greatly impact heterogeneity in research findings. Different demographics, socioeconomic backgrounds, cultural norms, and healthcare access among study participants can all influence how interventions are received and implemented, leading to varying outcomes. Methodologies are another critical factor that can contribute to heterogeneity in research. Variations in study design, data collection methods, sample sizes, and statistical analysis techniques can all affect the reliability and validity of study findings. For instance, using different measurement tools or data collection techniques can produce inconsistent results, making it difficult to compare or generalize findings across studies. However, it is important to consider the implications of heterogeneity on the validity of the study findings. High levels of heterogeneity may indicate that the results are not consistent across studies, which could affect the generalizability of the findings.
The most commonly studied symptoms across all meta-analyses were depression, anxiety, stress and insomnia. The pooled prevalence of depression, anxiety, stress and insomnia is discussed as follows. This umbrella review demonstrates the prevalence rates for depression among healthcare professionals during COVID-19 in Africa, and the pooled prevalence of depression was found to be 53.75% ranging from 40.80% to 66.70%. This is higher than the meta-analysis findings in China, where the pooled prevalence of depression was 39% (Xiong et al., 2022) and also worldwide depression pooled prevalence of 13.4% (Hill et al., 2022), 37% (Saragih et al., 2021), 22.8% (Rezaei-Hachesu et al., 2022). Also the result is higher than globally reported umbrella review prevalence of depression was 28.4% (Dragioti et al., 2020), 17.9% (Fernandez et al., 2021). Compared to a studies in Asia, with pooled prevalence of depression 37.5% (Ching et al., 2021), 34.61% (Norhayati, Che Yusof & Yacob Azman, 2021), the magnitude is high in africa. The cause for the high prevalence and differences of depression in Africa among healthcare professionals during COVID-19 might be due to there were growing concerns over the challenges on the African healthcare workers such as economic insecurity and stressful working conditions, limited access to personal protective equipment and other vital resources such as ventilators. Moreover, the pandemic influences African healthcare workers to social stigma, burnout, insomnia, depression, and fear of safety in their families (Nchasi et al., 2022).
Similarly, the pooled prevalence of anxiety was found 49.97% ranged from 34.71% to 65.23%. This is higher than meta-analysis findings in China pooled prevalence of anxiety was 37% (Xiong et al., 2022) and also worldwide anxiety pooled prevalence 16.1% (Hill et al., 2022), 40% (Saragih et al., 2021). The result is higher than global umbrella review results prevalence of anxiety 29.9% (Dragioti et al., 2020), 22.2% to 33.0% (Fernandez et al., 2021). It is higher than the study in Asia reported the pooled prevalence of anxiety 39.7(95%) (Ching et al., 2021), 34.81% (Norhayati, Che Yusof & Yacob Azman, 2021).
The pooled prevalence of stress was 57.27% ranged from 42.28% to 72.25%. This is much higher than meta-analysis findings in worldwide pooled prevalence of stress was 37% (Saragih et al., 2021), Asia 36.4% (Ching et al., 2021), 31.72% (Norhayati, Che Yusof & Yacob Azman, 2021).
Our study also reported the prevalence of insomnia among African healthcare professionals during the COVID-19 pandemic, and the pooled prevalence of insomnia was 45.16% ranged from 32.94% to 57.39%. Compared to the global findings, it is high in magnitude. For instance, a pooled prevalence of insomnia was estimated at 38 9% (Rezaei-Hachesu et al., 2022). The result is higher than the global umbrella review result prevalence of insomnia was 40% (Dragioti et al., 2020), Asia 37.89% (Norhayati, Che Yusof & Yacob Azman, 2021). The high heterogeneity in the pooled prevalence of mental health problems in Africa compared to others could be due to a variety of factors, including: Socioeconomic factors: Africa has a diverse range of socio-economic conditions and disparities, which could contribute to differences in the prevalence of anxiety disorders across different regions within the continent. Access to mental health services: Limited access to mental health services and treatment options in many African countries could result in underreporting of anxiety disorders and higher levels of untreated anxiety. Methodological differences: Variations in study design, methodology, and sampling techniques across different studies could also contribute to the heterogeneity in the pooled prevalence of anxiety in Africa compared to other.
This umbrella review helps primarily to assess the magnitude of mental health problems among healthcare professionals during COVID-19 in Africa. Literatures have indicated Africa as psychologically vulnerable during the pandemic, however such reports are often not summarized, and our umbrella review tried to indicate the mental health problems such as depression, anxiety, stress, and insomnia were highly prevalent in Africa. The study’s findings highlight the need for increased awareness and interventions to address mental health problems among healthcare professionals in Africa during the COVID-19 pandemic. This could include implementing mental health support programs, providing training on coping strategies, and developing policies to support mental health needs. The study’s findings have implications for policy development around mental health support for healthcare professionals in Africa. Policymakers may need to consider implementing guidelines and regulations to support mental health needs, as well as incorporating mental health support into healthcare policies and systems. Also this study involved on the importance of collaboration and partnerships in addressing mental health problems among healthcare professionals in Africa. This could involve collaboration between healthcare providers, government agencies, mental health organizations, and other stakeholders to develop and implement comprehensive mental health support programs. Also our umbrella review highlights the need to improve the quality of systematic reviews and meta analysis in this field of research. Additionally, summarizing existing meta-analyses can help identify gaps and inconsistencies in the existing literature, which can guide future research efforts. By synthesizing the findings of multiple meta-analyses, the researchers can identify common themes and trends in the existing evidence on mental health in Africa, as well as areas where further research is needed.
Whereas, this study has strengths and limitation. To our knowledge, this is the first umbrella review to examine the pooled prevalence of depression, anxiety, stress and insomnia among healthcare professionals during COVID-19 in Africa. One strength of this methodology is that it offers comprehensive evidence on the mental health challenges faced by healthcare professionals during the COVID-19 pandemic in Africa. The screening, data extraction and methodological quality assessment were done by two authors independently. The quality assessment was checked by the Joanna Briggs Institute (JBI) critical appraisal checklist for systematic reviews and research syntheses. Moreover, this study presents the predictive interval in which future studies finding might be in it. However, there are potential limitations to be aware of. Firstly in the absence of sufficient meta-analysis studies on the prevalence of mental health problems among healthcare professionals in Africa, subgroup analyses were not performed due to the limited studies included. Secondly, there is a risk of selection bias as non-English language meta-analyses were not included, potentially skewing the results. Thirdly, there is overlap in primary studies across meta-analyses of insomnia studies might leading to biased estimates. Fourthly, Hetrogeneity in methodologies among primary studies, including sampling methods and assessment tools, could impact the accuracy of prevalence estimates for stress, anxiety, depression, and insomnia. Lastly, it is important to recognize that these mental health problems may vary among different groups of healthcare professionals, highlighting the need for future research to explore prevalence estimates within specific circumstances.
Conclusions
In conclusion, healthcare professionals in Africa were at a high risk of experiencing a variety of mental health problems during the COVID-19 pandemic. The prevalence of anxiety, depression, stress and insomnia among healthcare professionals were significantly higher in Africa compared to other regions. This study’s findings highlight the need to develop appropriate public health interventions to address healthcare professionals’ mental health needs in Africa during COVID-19 and related public health crises.
Supplemental Information
Supplementary figure 1
Abbreviations
- CI
Confidence Interval
- HCWs
Health Care Workers
- JBI
Joanna Briggs Institute
- MeSH
Medical Subject Headings
- PRISMA
Preferred Reporting Items for Systematic Review and Meta-Analysis
Funding Statement
The authors received no funding for this work.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Aragaw Asfaw Hasen conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Ahmed Adem Mohammed conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, and approved the final draft.
Abubeker Alebachew Seid conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Data Availability
The following information was supplied regarding data availability:
All data relevant to the study are included in the article.
References
- Africa CDC (2024).Africa CDC Africa CDC Epidemic Intelligence Weekly Report, August 2024. 2024. https://africacdc.org/download/africa-cdc-weekly-event-based-surveillance-report-august-2024/ https://africacdc.org/download/africa-cdc-weekly-event-based-surveillance-report-august-2024/
- Al-Otaibi et al. (2022).Al-Otaibi T, Abbas A, Nagib AM, Gheith OA, Nair P, Farid MM, Albader MA. COVID-Somnia: anxiety, insomnia, and poor sleep among second-line healthcare workers during COVID-19 Pandemic. The Egyptian Journal of Bronchology. 2022;16(1):47. doi: 10.1186/s43168-022-00143-9. [DOI] [Google Scholar]
- Aromataris et al. (2017).Aromataris E, Godfrey C, Holly C, Kahlil H, Tungpunkom P, Fernandez R. Checklist for Systematic Reviews and Research Syntheses. The Joanna Briggs Institute. 2017. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Systematic_Reviews2017_0.pdf https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Systematic_Reviews2017_0.pdf
- Asnakew, Amha & Kassew (2021).Asnakew S, Amha H, Kassew T. Mental health adverse effects of COVID-19 pandemic on health care workers in North West Ethiopia: a multicenter cross-sectional study. Neuropsychiatric Disease and Treatment. 2021;17:1375–1384. doi: 10.2147/NDT.S306300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra et al. (2020).Batra K, Pal Singh T, Sharma M, Batra R, Schvaneveldt N. Investigating the psychological impact of COVID-19 among healthcare workers: a meta-analysis. International Journal of Environmental Research and Public Health. 2020;17(23):1–33. doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chekole et al. (2020).Chekole YA, Yimer Minaye S, Mekonnen Abate S, Mekuriaw B. Perceived stress and its associated factors during COVID-19 among healthcare providers in ethiopia: a cross-sectional study. Advances in Public Health. 2020;2020:1–7. doi: 10.1155/2020/5036861. [DOI] [Google Scholar]
- Chen et al. (2021).Chen J, Farah N, Kechen Dong R, Chen RZ, Xu W, Yin J, Chen BZ, Delios AY, Miller S, Wan X, Ye W, Zhang SX. Mental health during the COVID-19 crisis in Africa: a systematic review and meta-analysis. International Journal of Environmental Research and Public Health. 2021;18:10604. doi: 10.3390/ijerph182010604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching et al. (2021).Ching SM, Yean Ng K, Wei Lee K, Yee A, Ying Lim P, Ranita H, Kumar Devaraj N, BoonOoi P, Theng Cheong A. Psychological distress among healthcare providers during COVID-19 in Asia: systematic review and meta-analysis. PLOS ONE. 2021;16(10):e0257983. doi: 10.1371/journal.pone.0257983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragioti et al. (2022).Dragioti E, Li H, Tsitsas G, Hwa Lee K, Choi J, Kim J, Jo Choi Y, Tsamakis K, Estradé A, Agorastos A, Vancampfort D, Tsiptsios D, Thompson T, Mosina A, Vakadaris G, Fusar-Poli P, Carvalho AF, Correll CU, Han YJoo, Park S, Shin JIl, Solmi M. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. Journal of Medical Virology. 2022;94(5):1935–1949. doi: 10.1002/jmv.27549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragioti et al. (2020).Dragioti E, Tsartsalis D, Mentis M, Mantzoukas S, Gouva M. Impact of the COVID-19 pandemic on the mental health ofhospital staff: an umbrella review of 44 meta-analyses. International Journal of Nursing Studies. 2020;131:104272. doi: 10.1016/j.ijnurstu.2022.104272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-qushayri et al. (2021).El-qushayri AE, Dahy A, Reda A, Abdelmageed Mahmoud M, Abdel Mageed S, Mostafa A, Kamel A, Ghozy S. A closer look at the high burden of psychiatric disorders among healthcare workers in Egypt during the COVID-19 pandemic. Epidemiolgy and Health. 2021;43:1–8. doi: 10.4178/epih.e2021045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feilong Zhu et al. (2020).Feilong Zhu MZ, Gao M, Zeng C, Wang D, Hong Q, Chen W. Effects of respiratory rehabilitation on patients with novel coronavirus (COVID-19) pneumonia in the rehabilitation phase: protocol for a systematic review and meta-analysis. BMJ Open. 2020;10:e039771. doi: 10.1136/bmjopen-2020-039771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez et al. (2021).Fernandez R, Sikhosana N, Green H, Halcomb EJ, Middleton R, Alananzeh I, Trakis S, Moxham L. Anxiety and depression among healthcare workers during the COVID-19 pandemic: a systematic umbrella review of the global evidence. BMJ Open. 2021;11(9):1–9. doi: 10.1136/bmjopen-2021-054528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GebreEyesus et al. (2021).GebreEyesus FA, Tsehay Tarekegn T, Tsegaye Amlak B, Zeleke Shiferaw B, Solomon Emeria M, Tolessa Geleta O, Fetene Terefe T, Mammo Tadereregew M, Senbeta Jimma M, Seid Degu F, Nigusu Abdisa E, Amare Eshetu M, Moges Misganaw N, Sisay Chanie E. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage Zonal Public Hospitals, Southwest Ethiopia, 2020: a multicenter cross-sectional study. PLOS ONE. 2021;16(11):1–24. doi: 10.1371/journal.pone.0259906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habtamu et al. (2021).Habtamu Y, Admasu K, Tullu M, Damene W, Birhanu A, Beyero T, Birhanu Tekeda A. Mental health outcomes among frontline health-care workers at Eka Kotebe national COVID-19 Treatment Center, Addis Ababa, Ethiopia, 2020: a cross-sectional study. Neuropsychiatric Disease and Treatment Volume. 2021;17(August):2831–2840. doi: 10.2147/ndt.s311949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajure et al. (2021).Hajure M, Dibaba B, Shemsu S, Desalegn D, Reshad M, Mohammedhussein M. Psychological distress among health care workers in health facilities of mettu town during COVID-19 outbreak, South West Ethiopia, 2020. Frontiers in Psychiatry. 2021;12(June):1–8. doi: 10.3389/fpsyt.2021.574671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasen, Seid & Mohammed (2023a).Hasen AA, Seid AA, Mohammed AA. Anxiety and stress among healthcare professionals during COVID-19 in Ethiopia: systematic review and meta-analysis. BMJ Open. 2023a;13:1–11. doi: 10.1136/bmjopen-2022-070367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasen, Seid & Mohammed (2023b).Hasen AA, Seid AA, Mohammed AA. Depression and insomnia among healthcare professionals during COVID-19 pandemic in Ethiopia: a systematic review and meta-analysis. PeerJ. 2023b;11:1–18. doi: 10.7717/peerj.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasen, Seid & Mohammed (2023c).Hasen AA, Seid AA, Mohammed AA. Mental health problems among healthcare professionals during 19 in Africa: a protocol for umbrella review. BMJ Open. 2023c;13:1–5. doi: 10.1136/bmjopen-2023-072337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill et al. (2022).Hill JE, Harris C, Danielle LC, Boland P, Doherty AJ, Benedetto V, Gita BE, Clegg AJ. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. Journal of Advanced Nursing. 2022;78(6):1551–1573. doi: 10.1111/jan.15175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou et al. (2017).Hou Y, Tian J, Zhang J, Yun R, Zhang Z, Chen KH, Zhang C, Wang B. Quality of meta-analysis in nursing fields: an exploration based on the JBI guidelines. PLOS ONE. 2017;12(5):1–12. doi: 10.1371/journal.pone.0177648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal et al. (2021).Jemal K, Senbeta Deriba B, Abeya Geleta T, Tesema M, Awol M, Mengistu E, Annous Y. Self-reported symptoms of depression, anxiety, and stress among healthcare workers in Ethiopia during the Covid-19 pandemic: a cross-sectional study. Neuropsychiatric Disease and Treatment. 2021;17:1363–1373. doi: 10.2147/NDT.S306240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirabira et al. (2022).Kirabira J, Forry JB, Ssebuufu R, Akimana B, Nakawuki M, Anyayo L, Mpamizo E, Chan Onen B, Ingabire J, Gumisiriza N, Waiswa A, Mawanda A, Ashaba S, Kyamanywa P. Psychological distress and associated factors among hospital workers in Uganda during the COVID-19 lockdown—a multicentre study. Heliyon. 2022;8(2021):e08807. doi: 10.1016/j.heliyon.2022.e08807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwobah et al. (2021).Kwobah EK, Mwangi A, Patel K, Mwogi T, Kiptoo R. Mental disorders among health care workers at the early phase of COVID-19 pandemic in Kenya; findings of an online descriptive survey. Frontiers in Psychiatry. 2021;12(July):1–11. doi: 10.3389/fpsyt.2021.665611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon et al. (2015).Kwon Y, Lemieux M, McTavish J, Wathen N. Identifying and removing duplicate records from systematic review searches. Journal of the Medical Library Association. 2015;103(4):184–188. doi: 10.3163/1536-5050.103.4.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2022).Lee H-L, Wilson KS, Bernstein C, Naicker N, Yassi A, Spiegel JM. Psychological distress in South African healthcare workers early in the COVID-19 pandemic: an analysis of associations and mitigating factors. International Journal of Environmental Research and Public Health. 2022;19(15):9722. doi: 10.3390/ijerph19159722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nchasi et al. (2022).Nchasi G, Christabel O, Rahul O, Ahmad S, Soomro U, Nawaz FA. Challenges faced by African healthcare workers during the third wave of the pandemic. Health Science Reports. 2022;5(September):1–5. doi: 10.1002/hsr2.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norhayati, Che Yusof & Yacob Azman (2021).Norhayati MN, Che Yusof R, Yacob Azman M. Prevalence of psychological impacts on healthcare providers during COVID-19 pandemic in Asia. International Journal of Environmental Research and Public Health. 2021;18(17):9157. doi: 10.3390/ijerph18179157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olashore et al. (2021).Olashore AA, Akanni OO, Fela-Thomas AL, Khutsafalo K. The psychological impact of COVID-19 on health-care workers in African countries: a systematic review. Asian Journal of Social Health and Behavior. 2021;4(3):85–97. doi: 10.4103/shb.shb_32_21. [DOI] [Google Scholar]
- Perera et al. (2021).Perera C, Bakrania S, Ipince A, Nesbitt-Ahmed Z, Obasola O, Richardson D. PROTOCOL: impact of social protection on gender equality in low- and middle-income countries: a systematic review of reviews. Campbell Systematic Reviews. 2021;17(2):e1161. doi: 10.1002/cl2.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieper et al. (2014).Pieper D, Antoine S-L, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. Journal of Clinical Epidemiology. 2014;67(4):368–375. doi: 10.1016/j.jclinepi.2013.11.007. [DOI] [PubMed] [Google Scholar]
- Rezaei et al. (2022).Rezaei S, Hoseinipalangi Z, Rafiei S, Dolati Y, Hosseinifard H, Asl MT, Mejareh ZN, Deylami S, Abdollahi B, Ardakani MF, Ghadimi N The global prevalence of depression among health workers during the COVID-19 pandemic: a systematic review and meta-analysis. Journal of Affective Disorders Reports. 2022;8:100326. doi: 10.1016/j.jadr.2022.100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezaei-Hachesu et al. (2022).Rezaei-Hachesu V, Naderyan Fe’li S, Maajani K, Hokmabadi R, Golbabaei F. The global prevalence of anxiety, depression, and insomnia among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Journal of Occupational Health and Epidemiology. 2022;11(1):48–66. doi: 10.52547/johe.11.1.48. [DOI] [Google Scholar]
- Sagaon-Teyssier et al. (2020).Sagaon-Teyssier L, Kamissoko A, Yattassaye A, Diallo F, Rojas Castro D, Delabre R, Pouradier F, Maradan G, Bourrelly M, Cissé M, Vidal L, Keïta BD, Spire B. Assessment of mental health outcomes and associated factors among workers in community-based HIV care centers in the early stage of the COVID-19 outbreak in Mali. Health Policy OPEN Journal. 2020;1:100017. doi: 10.1016/j.hpopen.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saragih et al. (2021).Saragih ID, Tonapa SI, Saragih IS, Advanie S, Batubara SO, Suarilah I, Lin C-J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. International Journal of Nursing Studies. 2021;121:104002. doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaukat, Mansoor Ali & Razzak (2020).Shaukat N, Mansoor Ali D, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. International Journal of Emergency Medicine. 2020;5:1–8. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teshome et al. (2020).Teshome A, Glagn M, Shegaze M, Tekabe B, Getie A, Assefa G, Getahun D, Yenesew N, Temtmie Z, Tolosie K. Generalized anxiety disorder and its associated factors among health care workers fighting COVID-19 in Southern Ethiopia. Psychology Research and Behavior Management. 2020;13:907–917. doi: 10.2147/PRBM.S282822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsehay, Belete & Necho (2020).Tsehay M, Belete A, Necho M. Factors associated with psychological distress and brief resilient coping level during the Covid-19 pandemic among health-care professionals in Dessie, Ethiopia. Psychology Research and Behavior Management. 2020;13:1213–1221. doi: 10.2147/PRBM.S288562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020).World Health Organization COVID-19 situation report. 2020;31(2):61–66. [Google Scholar]
- Xiong et al. (2022).Xiong N, Fritzsche K, Pan Y, Löhlein J, Leonhart R. The psychological impact of COVID-19 on Chinese healthcare workers: a systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology. 2022;57(8):1515–1529. doi: 10.1007/s00127-022-02264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yitayih et al. (2021).Yitayih Y, Mekonen S, Zeynudin A, Mengistie E, Ambelu A. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open. 2021;7(1):1–6. doi: 10.1192/bjo.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2021).Zhang H, Li W, Li H, Zhang C, Luo J, Zhu Y, Wu H, Zhu Z, Xu Y, Wang J, Li C. Prevalence and dynamic features of psychological issues among Chinese healthcare workers during the COVID-19 pandemic: a systematic review and cumulative meta-analysis. General Psychiatry. 2021;34(3):e100344. doi: 10.1136/gpsych-2020-100344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figure 1
Data Availability Statement
The following information was supplied regarding data availability:
All data relevant to the study are included in the article.