Abstract
Purpose of review:
Although many environmental exposures (e.g., air pollution) are geographically patterned and persist as a result of historic economic policies (e.g., redlining), the impact of reproductive and social policies on maternal and child health remains incompletely understood. Reproductive and social policies are increasingly important for maternal and child health equity, particularly following the 2022 US Supreme Court decision in Dobbs v Jackson Women’s Health Organization (‘Dobbs decision’), which restricted access to abortion. Here, we summarize the literature from original research studies examining influences of reproductive and social policy on maternal and child health, focusing on impacts on adverse birth outcomes and policies as sources of stress.
Recent findings:
Several studies suggest that those most impacted by the Dobbs decision are younger, non-white, socioeconomically disadvantaged, and living in states with less access to government safety net programs, all of which are compounded by environmental injustices. Further, studies conducted in the wake of the Dobbs decision find elevated stress levels among women of reproductive age. This may represent one pathway leading to adverse birth outcomes, as epidemiologic studies demonstrate that preterm birth rates increased following the 2016 election, a period of heightened stress.
Summary:
Reproductive and social policies are understudied contributors to adverse outcomes for reproductive aged women and their children. This has important implications for maternal and child health equity, as those who will be the most impacted by reproductive and social policies already experience the highest rates of adverse birth outcomes and environmental toxicant exposure.
Keywords: pregnancy, health equity, stress, policy
Introduction
Adverse maternal and child health outcomes as public health problems
Relative to other developed countries, the United States (US) lags far behind with respect to the rates of adverse health outcomes for persons who give birth and their offspring (hereby referred to as ‘maternal and child health’). For example, the US maternal mortality rate has consistently ranked among the highest of all high-income countries (1). This is further compounded by within country disparities, as non-Hispanic Black women are three times as likely to die during childbirth relative to white women in the US (2). Inequalities in rates of other adverse outcomes, including preterm birth (defined as gestational age less than 37 weeks, the leading cause of infant morbidity and mortality worldwide) (3), follows a similar distribution along racial and ethnic lines in the US (4), and are also markedly higher in the US relative to other high income and developed countries (5). Conventional research on social determinants of health (e.g., low socioeconomic status [SES]) only explain a small amount of the observed Black-white disparities, as Black women with a graduate degree continue to experience preterm birth at rates higher than white women with less education (6). Underappreciated risk factors may include reproductive and social policies, as policies such as paid parental leave, and broad social welfare systems are less prevalent in the US relative to other Western countries (7).
Environmental injustices stem from historic policies
Societies are comprised of complex ecosystems shaped by historical practices and modern-day power dynamics and culture (8). Many historical practices continue to influence present day health and environmental toxicant exposure; for example, individuals living in neighborhoods that were historically redlined, defined using the 1930s federally sponsored Home Owners’ Loan Corporation (HOLC) color-coded map, continued to experience high exposure levels to environmental hazards (e.g., air pollution) in 2010 (9). Relative to HOLC grade A (“best” – green), pregnant persons living a census tract historically rated as HOLC grade D (“hazardous” – red) had a 60% increase in odds of preterm birth in the mid-2010s (10). Examples of legalized discrimination on the basis of race are well-documented and have persisted over time, which has important public health implications, as increasing state-level income inequality is significantly associated with increased odds of preterm birth in the US (11).
Impact of environmental policy on public health
Environmental protections are also directly tied to policies. For example, nearly 100 environmental protections, ranging from reducing greenhouse gas standards to withdrawing from the Paris climate agreement, were officially reversed, revoked or otherwise rolled back during the Trump administration between 2016 and 2020 (12). These rollbacks had direct implications on human health, as the number of environmental and occupational related deaths increased by more than 22,000 annually between 2016 and 2019 (12). On the contrary, environmental policies could also provide the benefit of reducing environmental toxicant levels for pregnant persons. For example, a study using administrative data from California between 2001-2011 observed a significant reduction in preterm births following the closure of coal and power plants among mothers who resided within 0-5 km of the power plant (13). This suggests that policies supporting renewable energy would have a substantial public health benefit.
Implications of the Dobbs decision for maternal and child health equity
The impact of reproductive and social policies on maternal and child health has become even more salient following the June 2022 US Supreme Court decision in Dobbs v Jackson Women’s Health Organization (‘Dobbs decision’) (14). The Dobbs decision overturned Roe v Wade which protected the right to individual privacy, including the right to abortion prior to fetal viability (15). In thirteen states, latent legislation known as “trigger” bans immediately went into effect following the overturning of Roe v Wade, further restricting access to abortion (16). Additional states quickly moved to enact new abortion restrictions, resulting in a state-level patchwork of different policies (16). As of December 2023, half of all states were categorized as having a restrictive abortion policy according to the Guttmacher Institute (17). The Dobbs decision has implications for maternal and child health equity, such as the eradication of access to the full spectrum of medical care and bodily autonomy. Additionally, the fall of Roe v Wade is a salient source of stress for many individuals with gestational capacity. Psychosocial stress is defined as a life event or series of life experiences (either acute or chronic) that exert a significant impact on individual mental, emotional, or physical health and wellbeing (18). The American sociopolitical landscape has been gutted of the last 50 years of reproductive healthcare precedent, and pregnant persons may experience psychosocial stress as a result of this major shift. In this review, we posit that stress related to policy change and political rhetoric that restricts individual healthcare access is an example of sociopolitical stress. Psychosocial stress and sociopolitical stress are distinct, the later contextualizing societal shifts that are informed by relationship between the political environment and social structures or patterning, while the former centers individual experiences. Ultimately, sociopolitical stress can be considered a form of psychosocial stress that accounts for the deeply rooted interrelated nature of politics and society; with individual and societal impacts of these relationships in view.
The political landscape defines policy and can shape medical practice. Following the Dobbs decision, 40% of obstetricians/gynecologists (OBGYNs) in states where abortion was banned personally felt constraints on their ability to provide care for miscarriages and other pregnancy-related medical emergencies, relative to 20% nationally according to a Kaiser Family Foundation survey of office-based OBGYNs (19). The ruling also consequently created a culture of fear and confusion among patients, which likely impacts health seeking behaviors among pregnant persons, particularly those with existing barriers to healthcare access (20). Moreover, the impact of the Dobbs decision is unequally distributed across society, as an increase from 0 to 100 miles to the nearest abortion facility is projected to increase the birth rate by 2.2% (21). Further, it is anticipated that that individuals who are socioeconomically disadvantaged and non-white will be most the impacted, perpetuating health inequities. Ultimately, the uptick in abortion restrictions may result in more children being born into poverty (22,23), leading to worsening child health across the next generations.
Purpose of the current review and search strategy
The political landscape also defines environmental policy which, in turn, significantly impacts individual health. There is an urgent need to examine how co-exposure to environmental toxicants and social factors influence maternal and child health (24,25), particularly in populations that experience the highest levels of social stressors, such as poverty and discrimination. Despite this budding field of research, the influence of reproductive and social policy remains under explored. Importantly, individuals who are the most impacted by the Dobbs decision, in terms of healthcare access, are also disproportionately exposed to high levels of environmental toxicants. To illustrate this point, we compared the distribution of the predicted travel time to the nearest abortion facility following the Dobbs decision (26), with the distribution of environmental justice (EJ) indicators using the Environmental Protection Agency’s EJScreen (27). We observe that the southern US has the highest PM2.5 EJ index and longest average travel time to the nearest abortion facility (Figure 1). This highlights that individuals disproportionally impacted by restrictive reproductive policies also experience environmental hazards, leading to a “double jeopardy” of increased susceptibility in marginalized and socioeconomically disadvantaged populations (24).
Figure 1.
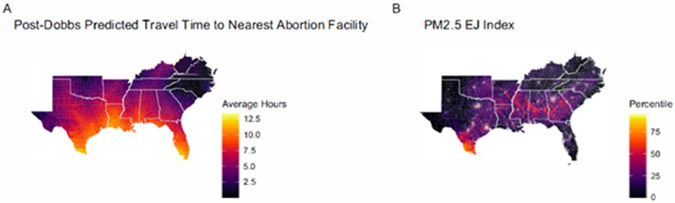
Distribution of (A) predicted travel time to the nearest abortion facility following the 2022 United States Supreme Court Decision in Dobbs v Jackson Women’s Health Organization and (B) environmental justice indicators in the southeastern United States.
Note: In panel A, we use data on the predicted average travel time to the nearest abortion facility post-Dobbs obtained from the Abortion Access Dashboard (https://experience.arcgis.com/experience/6e360741bfd84db79d5db774a1147815) produced by Professor Caitlin Myers at Middlebury College. We use the predicted average hours as of September 2023, which accounts for all abortion bans that have been implemented up until that date.
In panel B, we use the environmental justice indices for PM2.5 for the year 2021. Data were obtained from the United States Environmental Protection Agency’s EJScreen, which calculates indices that combine socioeconomic and demographic characteristics with environmental exposures. Each index combines a demographic index (the percent of people of color and the percent of low-income people) with an environmental indicator that has been converted into a percentile for the given census block group. More details can be found at https://ejscreen.epa.gov/.
Here, we summarize the relevant literature examining influences of reproductive and social policy on maternal and child health, and further explore sociopolitical stress in the context of reproductive and environmental health. We conducted a scoping review, which was guided by an iterative literature search conducted using PubMed, Google Scholar, the National Bureau of Economic Research, and snowball sampling methods. Keywords included in our search were related to politics, stress, reproductive rights, pregnancy, environmental policy, and the Dobbs decision. Papers included in our review were from original research studies. We did not include articles that were narrative pieces or did not include a testable hypothesis, even if these articles supported our hypotheses. Additionally, we developed a conceptual model which was guided by prior conceptual frameworks on multidimensional stress, maternal and child health, and environmental and social determinants of health (28,29).The conceptual model guiding this review posits that the political environment (e.g., divisive rhetoric, polarization) leads to an increase in sociopolitical stress and may result in changes in health seeking behaviors among women of reproductive age. Changes in reproductive and social policies can also impact comprehensive reproductive healthcare through restrictions on comprehensive maternal healthcare and reduced abortion access. Ultimately, we hypothesize that these sociopolitical factors, together, impact maternal and child health and are compounded by existing health disparities, as well as environmental injustice (Figure 2).
Figure 2.
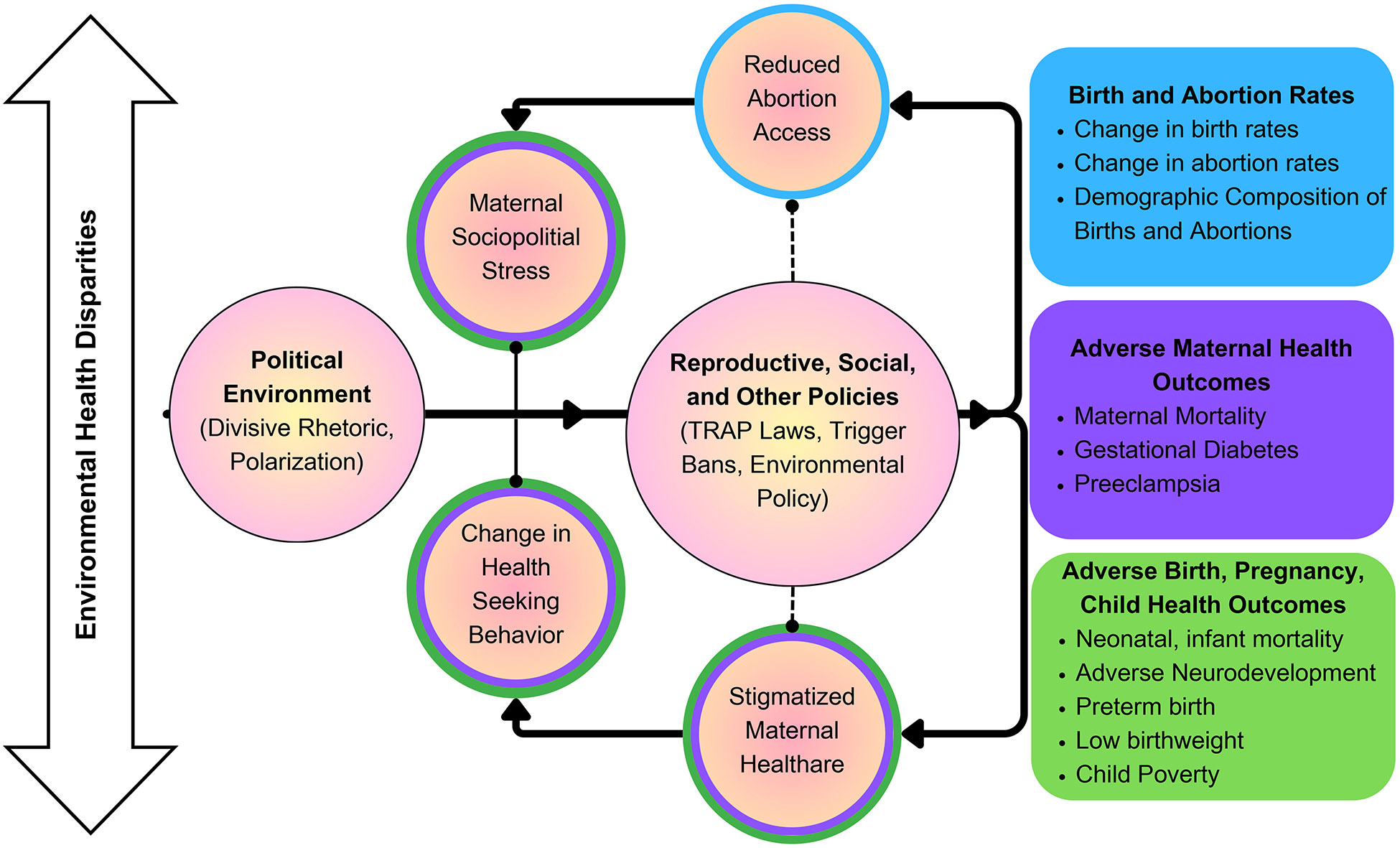
Conceptual model showing hypothesized associations between reproductive and social and policies and maternal and child health equity.
Abbreviations: TRAP: targeted regulation of abortion providers
Impact of political events on adverse birth outcomes and birth rates
Adverse birth outcomes and implications for worsening child health
Several studies leveraging administrative databases have observed a change in the rate of adverse birth outcomes following presidential elections. The majority of these studies have focused on the 2016 election, finding that the overall preterm birth rate in New York City increased from 7.0% to 7.3% in the 8 months following the inauguration of President Trump (30), with some of the highest rate increases observed for women who were Hispanic/Latina and born outside of the US (30). It is hypothesized that one pathway through which Latina women may be disproportionately impacted is via increased stress following anti-immigration policies and rhetoric commonly used during and following the 2016 election. For example, a study defining anti-immigration rhetoric using Google trend analytics, observed that this rhetoric was associated with fewer prenatal care visits among foreign born Latina pregnant persons in Houston, Texas (31). The hypothesis that Latina and Hispanic women may be disproportionately impacted by sociopolitical stress is supported by additional research that used birth certificates and observed an increase in the odds of preterm birth and low birthweight among Latinas in the US between 2017-2019 (the ‘post Trump’ period) relative to 2014 (the ‘pre Trump’ period) (32). Effect sizes were greatest in magnitude among foreign born Latinas (odds ratio [OR]= 1.17, 95% confidence interval [CI]= 1.14, 1.19 for 2019 compared to 2014) relative to US born Latinas (OR= 1.14, 95% CI= 1.11, 1.16 for 2019 compared to 2014), which supports the findings from the New York City study (30). Relatedly, the risk of periviable births, defined as births <26 weeks gestation, also increased for Latina women in the months surrounding the 2016 election (ranging from a 0.392 increase in risk in April 2016 to a 0.095 increase in risk in November 2016 (33). Taken together, these findings underscore the notion that severe sociopolitical stressors are associated with adverse birth outcomes. In this instance of the 2016 election, this was manifested among Latinas and immigrant populations, perhaps due to increases in anti-immigration political rhetoric and policy implementation.
Changes in reproductive and social policies result in more births and have health equity implications
It is anticipated that the Dobbs decision will lead to an increase in adverse birth outcomes, as well as an increase in birth rates, which is supported by preliminary evidence from Texas (34). In Georgia, a study estimating the multiyear effect of House Bill 481 (which prohibits abortions after detection of embryonic cardiac activity, approximately 6 weeks gestation) found that House Bill 481 will limit 90% of elective terminations in the state (35), which could ultimately lead to an increase in the number of births. With respect to the US broadly, the Dobbs decision is expected to result in an additional 12,911 maternal mortalities, 83,911 neonatal intensive care unit admissions, 3,311 more neonatal mortalities, and 904 more cases of profound neurodevelopmental disability according to estimates from a decision and economic analysis model (36).
Many of the states which have moved to restrict access to abortion following the Dobbs decision are clustered in the southeast and are characterized by some of the highest rates of preterm birth, childhood obesity, maternal mortality, and poverty relative to other regions of the US (37-39). In Georgia, House Bill 481 will widen health disparities, as research conducted in the wake of the bill’s passage reveal fewer abortions obtained by patients who are younger, Black, and socioeconomically disadvantaged because these groups are less likely to meet eligibility requirements (35). While more socioeconomically advantaged populations may choose to travel out of state to obtain care, these restrictions may force those with less resources to continue their pregnancy, leading to economic hardship and financial insecurity that can persist for years (40). This anticipated impact is supported by a prior study estimating the impact of targeted regulation of abortion providers (i.e., TRAP laws), which used a stacked difference-in-differences approach and found that the onset of a TRAP law increased the birth rate among Black teens by 3% but had no impact on white teens (41), further underscoring the differential impact across populations.
Prior research has clearly demonstrated that following the birth of a child, women are less likely to return to the labor force; this has led to the motherhood wage gap, in which women fall behind men in earnings after the birth of their first child (42,43). These existing disparities are likely to be compounded by the Dobbs decision, as women living in states that restricted abortion are less likely to have access to government safety net programs to supplement their family’s economic well-being (e.g., child tax credit, expanded Medicaid, universal pre-kindergarten) (44). Families with fewer resources are often faced with difficult decisions regarding their wellbeing, including reliance on low-income housing or highly processed and heavily packaged food options. Long-term, this may result in an increase in toxic chemical exposures via a multitude of pathways. Older building infrastructure, including low-income housing, carry higher risk for inhabitant exposure to environmental neurotoxicants (e.g., lead) relative to newer construction (45). Additionally, children who reported always eating school lunch, which often comes wrapped in large amounts of plastic packaging, had higher levels of certain phthalate metabolites relative to those who ate school lunch less frequently (46).
The Dobbs decision as a reproductive and social policy stressor for women of reproductive age
Researchers have found that psychosocial stress increases following changes in access to comprehensive reproductive healthcare and abortion denial. Using data from the 5-year longitudinal Turnaway Study, women who sought an abortion but were denied one because they were just beyond the facility gestational limit reported higher indicators of stress (e.g., symptoms of anxiety and lower self-esteem) one week after the denial, although stress levels were similar to stress levels observed among those who did not experience a live birth by 6 to 12 months (47). With respect to the Dobbs decision specifically, Dave et al used individual-level data from the Census Bureau Household Pulse Survey and a difference-in-differences model to compare changes in mental distress levels among reproductive age females in the US before and after the Dobbs decision (48). Among women residing in states that immediately restricted abortion, there was a 10% increase in the prevalence of mental distress in the three months following the Dobbs decision, relative to the pre-Dobbs period (48). Cross sectional analyses conducted within the Global Burden of Disease Study similarly observed a modest relationship between access to legal abortion and a lower prevalence of depression among reproductive age women (49). However, these studies are unable to determine if the observed increase in distress is a direct result of policy, underscoring the importance of causal inference and prospective studies in future work. Nonetheless, these findings highlight the loss of abortion rights as a potentially important source of stress for women nationally (48). On a more granular scale, a study conducted in Georgia prior to the passage of House Bill 481 found that 94% of pregnant persons seeking abortion care reported negative emotions (e.g., scared) when asked how they would feel about not being able to have a desired abortion (50). Additionally, consumption of abortion-related media was associated with higher alcohol use intentions and negative affect among women residing in states that immediately restricted abortions following the ruling (51). Taken together, this suggest that restrictions in reproductive autonomy may represent an acute stressor that can subsequently impact health outcomes.
In 2020, the American Psychological Association reported that nearly 70% of Americans were concerned about the future of the nation and cited the 2020 presidential election as a source of stress (52). This suggests that the observed increase in adverse birth outcomes during the 2016 election and subsequent Trump administration may be a contributing factor to sociopolitical stress, stemming from the divisiveness of political rhetoric and election results in the US (30,32,33). Two studies conducted among Latina women in Southern California found that the political climate and sociopolitical stressors related to the Trump presidency were associated with an increase in depression and anxiety in early pregnancy (53,54). Of the specific sociopolitical stressors, nearly 30% reported that potential loss of access to programs and social services such as WIC (Women, Infants, and Children) and that they would be separated from their child as some of their personal fears or concerns regarding the Trump presidency (53). These studies are bolstered by findings from a cross sectional study conducted among college students spanning 10 US universities during the 2020 election, which found that an increase in sociopolitical stress was associated with an increase in depression and less optimism (55).
Biologic plausibility supporting the hypothesis that environmental injustice and sociopolitical stress can lead to adverse maternal and child health outcomes
In the above sections we illustrate that reproductive and social policies are associated with an increased risk of adverse birth outcomes, with preterm birth being the most widely studied. We also highlight the importance of this relationship in the advancement of maternal-child health equity. While the biological mechanisms linking stress to preterm birth are incompletely understood, a leading hypothesis is the activation of biologic stress response pathways (56), leading to an increase in cortisol. Upregulated activation of the autonomic nervous system during times of stress causes the region of the brain responsible for regulation of the body’s internal functions, the hypothalamus, to secrete corticotropin releasing hormone, which activates the pituitary gland (57). Once activated, the pituitary gland releases adrenocorticotropic hormone, which travels via blood circulation to the adrenal glands atop the kidney, triggering the release of cortisol. Studies in animal and human models have described activation of the Hypothalamic-Pituitary-Adrenal axis (HPA Axis) as integral to both psychosocial and physiologic stress responses (58). In other words, HPA Axis activation is the common denominator between physical stress (such as a sore throat or broken bone) and psychosocial (emotional) stress.
Irrespective of exact mechanisms underlying physiologic manifestations of stress, chronic activation of stress response pathways is biologically detrimental. The HPA axis, for example, incorporates numerous negative feedback loops to ensure that the release of stress response hormones is meticulously regulated (59). However, in the context of chronic stress, these negative feedback loops can fail to activate, and the stress response can persist in the absence of a trigger. Thus, creating a heightened and continuous state of stress, which can be detrimental to multiple organ systems over time. Importantly, in the context of pregnancy, the release of cortisol targets several major systems of the body, including the placenta (60). It is well-documented that elevated cortisol levels, particularly in early to mid-pregnancy, increase the risk of preterm birth (61). Elevated cortisol levels have been associated with worsening mental health observed during periods of heightened sociopolitical stress, including the 2016 presidential election (62), suggesting that the relationship between sociopolitical stress and preterm birth is biologically plausible. Additionally, a study of 183 adults in Ann Arbor, Michigan and Durham, North Carolina observed that on the night of the 2008 election, salivary cortisol levels were significantly elevated among supporters of the losing presidential candidate relative to supporters of the winning candidate (63). A second study conducted within the week following the 2008 election observed that highly politically partisan individuals had elevated salivary cortisol levels after reading a post-election political essay, relative to when reading a nonpolitical text passage (64). However participants in that study were students recruited from a large, mostly conservative state university which limits the generalizability of these findings to other populations (64).
In pregnancy, timing of estrogen and progesterone fluctuations are tightly regulated throughout each trimester. Environmental stressors, like psychosocial stressors, can cause disturbances to successful activation, timing, and maintenance of hormonal signaling pathways during pregnancy (65). This is supported by findings from prospective birth cohorts showing that exposure to environmental toxicants are associated with perturbations in hormone fluctuation, elevated cortisol levels and HPA axis dysregulation during the prenatal period (66-68). For example, plasticizers, such as phthalates, are known to exert impacts to estrogen signaling through molecular mimicry (69). There is also an established and growing body of research that points to racial disparities in exposure to plasticizers. American socio-cultural and sociopolitical notions of class, beauty, and professionalism are euro-centric and anti-Black. These established norms are rooted in generations of intersectional racism and sexism that were rooted in social policies. Marketing for personal care products, consequently, target Black female consumers, and carry implications for toxic chemical exposure disparities. Black women are six times more likely to use hair care products that contain endocrine disrupting chemicals, such as phthalates, than their white counterparts (70). Compounded sociopolitical stress, therefore, can impact individuals who are minoritized on the basis of their race and gender. A study at Duke University examined circulating cortisol levels among college students who experienced racism and found that cortisol production was significantly elevated following experiences of racial discrimination, and starkly higher among Black women, specifically (71). Together, this underscores the notion that environmental injustice and racial identity politics are two sources of sociopolitical stress with biologic plausibility that have implications for health outcomes, particularly in the context of maternal health.
Summary of existing literature and recommendations for future work
Our review provides evidence that reproductive and social policies are upstream factors that influence maternal and child health equity. We identified several studies which illustrate that women from socioeconomically disadvantaged backgrounds will be the most impacted by the loss of comprehensive reproductive healthcare following the Dobbs decision. Preliminary evidence from the post-Dobbs era finds that births have increased by 2.3% in states which moved to immediately restrict abortion, relative to states that did not restrict abortion access (72). Those who stand to experience the most detrimental impacts of Dobbs already experience the highest levels of environmental toxicant exposures and adverse birth outcomes, both of which occur because of historic environmental injustices. Our review also provides evidence supporting the notion that the Dobbs decision will adversely impact the well-being of children for generations to come. This may occur via the motherhood wage gap and lack of a social safety net to support the positive development of children (e.g., universal pre-kindergarten, Medicaid expansion).
However, we note that most of the existing studies assessing the impact of a policy on a health outcome are limited by residual confounding, and failure to account the multitude of other factors which could be co-occurring with a given policy limits the ability of these studies to assess the policies’ true impact. Additionally, the small number of studies conducted after the Dobbs decision are limited by either cross sectional study design or a short follow up period. As a result, there is an urgent need for longitudinal studies that allow for causal inference to determine the true impact of a reproductive and social and policy. Furthermore, research on environmental exposures and social determinants of health continues to be siloed. While environmental epidemiology studies are beginning to consider co-exposure to environmental and social stressors, these studies are largely not assessing stressors such as sociopolitical stress or the loss of reproductive autonomy, distinct stressors potentially impacting large swaths of women in the US.
Funding:
Stephanie M Eick was supported by the JPB Environmental Health Fellowship and by grants K01ES035082 and P30ES019776 from the National Institutes of Health.
Footnotes
Conflicts of Interest: Stephanie M Eick, Jasmin A Eatman, Madeline Chandler, and Nina R Brooks declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
• Indicates important reference
•• Indicates very important reference
- 1.Douthard RA, Martin IK, Chapple-McGruder T, Langer A, Chang S. U.S. Maternal Mortality Within a Global Context: Historical Trends, Current State, and Future Directions. Journal of Women’s Health. 2021. Feb 1;30(2):168–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen EE, Davis NL, Goodman D, Cox S, Syverson C, Seed K, et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths - United States, 2007-2016. MMWR Morb Mortal Wkly Rep. 2019. Sep 6;68(35):762–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013/November/15 ed. 2013;10 Suppl 1(Suppl 1):S2–S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamilton BE, Martin JA, Osterman M. Births: Provisional Data for 2022. National Center for Health Statistics (U.S.), editor. 2023. Jun 1;(28). Available from: https://stacks.cdc.gov/view/cdc/127052 [PubMed] [Google Scholar]
- 5.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008. Jan 5;371(9606):75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burris Heather H, Lorch Scott A, Kirpalani Haresh, Pursley DeWayne M, Elovitz Michal A, Clougherty Jane E. Racial disparities in preterm birth in USA: a biosensor of physical and social environmental exposures. Arch Dis Child. 2019. Oct 1;104(10):931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bronstein JM, Wingate MS, Brisendine AE. Why Is the U.S. Preterm Birth Rate So Much Higher Than the Rates in Canada, Great Britain, and Western Europe? Int J Health Serv. 2018. Oct 1;48(4):622–40. [DOI] [PubMed] [Google Scholar]
- 8.Tverskoi D, Senthilnathan A, Gavrilets S. The dynamics of cooperation, power, and inequality in a group-structured society. Scientific Reports. 2021. Sep 21;11(1):18670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ••9. Lane HM, Morello-Frosch R, Marshall JD, Apte JS. Historical Redlining Is Associated with Present-Day Air Pollution Disparities in U.S. Cities. Environ Sci Technol Lett. 2022. Apr 12;9(4):345–50. This manuscript found that an economic policy (redlining) was associated with air pollution exposure decades later.
- ••10. Krieger N, Van Wye G, Huynh M, Waterman PD, Maduro G, Li W, et al. Structural Racism, Historical Redlining, and Risk of Preterm Birth in New York City, 2013–2017. Am J Public Health. 2020. Jul 1;110(7):1046–53. This manuscript found that an economic policy (redlining) was associated with preterm birth decades later
- 11.Wallace ME, Mendola P, Chen Z, Hwang BS, Grantz KL. Preterm Birth in the Context of Increasing Income Inequality. Maternal and Child Health Journal. 2016. Jan 1;20(1):164–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ••12. Woolhandler S, Himmelstein DU, Ahmed S, Bailey Z, Bassett MT, Bird M, et al. Public policy and health in the Trump era. The Lancet. 2021. Feb 20;397(10275):705–53. This review article highlights how environmental policy changed during the Trump administration.
- 13.Casey JA, Karasek D, Ogburn EL, Goin DE, Dang K, Braveman PA, et al. Retirements of Coal and Oil Power Plants in California: Association With Reduced Preterm Birth Among Populations Nearby. American Journal of Epidemiology. 2018. Aug 1;187(8):1586–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lazzarini Z. The End of Roe v. Wade — States’ Power over Health and Well-Being. N Engl J Med. 2022. Aug 4;387(5):390–3. [DOI] [PubMed] [Google Scholar]
- 15.Byron JJ, Avalos M, Xiao K (Amy), Klein AA, Leheste JR. Health Equity in a Post ‘Roe Versus Wade’ America. Cureus. 2022. Dec 1;14(12):e32100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Felix M, Sobel L, Salganicoff A. KFF Women’s Health Policy. 2023. [cited 2023 Dec 13]. Legal Challenges to State Abortion Bans Since the Dobbs Decision. Available from: https://www.kff.org/womens-health-policy/issue-brief/legal-challenges-to-state-abortion-bans-since-the-dobbs-decision/ [Google Scholar]
- 17.Guttmacher Institute. Interactive Map: US Abortion Policies and Access After Roe [Internet]. 2023. [cited 2023 Dec 14]. Available from: https://states.guttmacher.org/policies/ [Google Scholar]
- 18.Wheaton B, Young M, Montazer S, Stuart-Lahman K. Social stress in the twenty-first century. In: Handbook of the sociology of mental health, 2nd ed. New York, NY, US: Springer Science + Business Media; 2013. p. 299–323. (Handbooks of sociology and social research.). [Google Scholar]
- 19.Frederiksen B, Ranji U, Gomez I, Salganicoff A. KFF Women’s Health Policy. 2023. [cited 2023 Dec 14]. A National Survey of OBGYNs’ Experiences After Dobbs. Available from: https://www.kff.org/womens-health-policy/report/a-national-survey-of-obgyns-experiences-after-dobbs/ [Google Scholar]
- 20.Gupta S, Perry B, Simon K. Trends in Abortion- and Contraception-Related Internet Searches After the US Supreme Court Overturned Constitutional Abortion Rights: How Much Do State Laws Matter? JAMA Health Forum. 2023. Apr 28;4(4):e230518–e230518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myers C. Forecasts for a post-Roe America: The effects of increased travel distance on abortions and births. Journal of Policy Analysis and Management [Internet]. 2023. Sep 13 [cited 2023 Nov 28];n/a(n/a). Available from: 10.1002/pam.22524 [DOI] [Google Scholar]
- 22.Gruber J, Levine P, Staiger D. Abortion Legalization and Child Living Circumstances: Who is the “Marginal Child”? The Quarterly Journal of Economics. 1999;114(1):263–91. [Google Scholar]
- 23.Miller S, Wherry LR, Foster DG. The Economic Consequences of Being Denied an Abortion. American Economic Journal: Economic Policy. 2023;15(1):394–437. [Google Scholar]
- •24. Padula AM, Monk C, Brennan PA, Borders A, Barrett ES, McEvoy CT, et al. A review of maternal prenatal exposures to environmental chemicals and psychosocial stressors-implications for research on perinatal outcomes in the ECHO program. J Perinatol. 2019/10/17 ed. 2020. Jan;40(1):10–24. This review article highlights the importance of consider both chemical and non-chemical exposures in maternal and child health research.
- •25. Barrett ES, Padula AM. Joint Impact of Synthetic Chemical and Non-chemical Stressors on Children’s Health. Curr Environ Health Rep. 2019/10/23 ed. 2019. Dec;6(4):225–35. This review article highlights the importance of consider both chemical and non-chemical exposures in maternal and child health research.
- 26.Myers C, Bennett L, Vale F, Nieto A. Abortion Access Dashboard [Internet]. 2023. [cited 2023 Dec 13]. Available from: https://experience.arcgis.com/experience/6e360741bfd84db79d5db774a1147815 [Google Scholar]
- 27.United States Environmental Protection Agency. EJ Screen: Environmental Justice Screening and Mapping Tool [Internet]. 2023. [cited 2023 Dec 13]. Available from: https://www.epa.gov/ejscreen [Google Scholar]
- 28.Olvera-Alvarez H, Appleton A, Fuller C, Belcourt A, Kubzansky L. An Integrated Socio-Environmental Model of Health and Well-Being: a Conceptual Framework Exploring the Joint Contribution of Environmental and Social Exposures to Health and Disease Over the Life Span. Current Environmental Health Reports. 2018. Jun 1;5. [DOI] [PubMed] [Google Scholar]
- 29.Brenner AB, Zimmerman MA, Bauermeister JA, Caldwell CH. Neighborhood Context and Perceptions of Stress Over Time: An Ecological Model of Neighborhood Stressors and Intrapersonal and Interpersonal Resources. American Journal of Community Psychology. 2013. Jun 1;51(3–4):544–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krieger Nancy, Huynh Mary, Li Wenhui, Waterman Pamela D, Van Wye Gretchen. Severe sociopolitical stressors and preterm births in New York City: 1 September 2015 to 31 August 2017. J Epidemiol Community Health. 2018. Dec 1;72(12):1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chu DM, Aagaard J, Levitt R, Whitham M, Mastrobattista J, Rac M, et al. Cohort Analysis of Immigrant Rhetoric on Timely and Regular Access of Prenatal Care. Obstetrics & Gynecology [Internet]. 2019;133(1). Available from: https://journals.lww.com/greenjournal/fulltext/2019/01000/cohort_analysis_of_immigrant_rhetoric_on_timely.17.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gutierrez C, Dollar NT. Birth and prenatal care outcomes of Latina mothers in the Trump era: Analysis by nativity and country/region of origin. PLOS ONE. 2023. Mar 1;18(3):e0281803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gemmill A, Catalano R, Alcalá H, Karasek D, Casey JA, Bruckner TA. The 2016. presidential election and periviable births among Latina women. Early Human Development. 2020 Dec 1;151:105203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bell SO, Stuart EA, Gemmill A. Texas’ 2021 Ban on Abortion in Early Pregnancy and Changes in Live Births. JAMA. 2023. Jul 18;330(3):281–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Redd SK, Mosley EA, Narasimhan S, Newton-Levinson A, AbiSamra R, Cwiak C, et al. Estimation of Multiyear Consequences for Abortion Access in Georgia Under a Law Limiting Abortion to Early Pregnancy. JAMA Network Open. 2023. Mar 6;6(3):e231598–e231598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nehme L, Ye P, Huang JC, Kawakita T. Decision and economic analysis of hostile abortion laws compared with supportive abortion laws. American Journal of Obstetrics & Gynecology MFM. 2023. Aug 1;5(8):101019. [DOI] [PubMed] [Google Scholar]
- 37.McCarty AT. Child Poverty in the United States: A Tale of Devastation and the Promise of Hope. Sociol Compass. 2016. Jul;10(7):623–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Maternal deaths and mortality rates: Each state, the District of Columbia, United States 2018-2021 [Internet]. 2022. [cited 2023 Dec 14]. Available from: https://www.cdc.gov/nchs/maternal-mortality/MMR-2018-2021-State-Data.pdf [Google Scholar]
- 39.Robert Wood Johnson Foundation. State of Childhood Obesity [Internet]. 2023. [cited 2023 Dec 14]. Available from: https://stateofchildhoodobesity.org/demographic-data/ages-10-17/ [Google Scholar]
- 40.Foster DG, Biggs MA, Ralph L, Gerdts C, Roberts S, Glymour MM. Socioeconomic Outcomes of Women Who Receive and Women Who Are Denied Wanted Abortions in the United States. Am J Public Health. 2022. Sep 1;112(9):1290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •41. Jones K, Pineda-Torres M. Trap’d Teens: Impacts of Abortion Provider Regulations on Fertility & Education. SSRN. 2022. May 19;IZA Discussion Paper No. 14837. This article shows how a social and reproductive policy can impact population health.
- 42.Kleven H, Landais C, Posch J, Steinhauer A, Zweimüller J. Child Penalties across Countries. AEA Papers and Proceedings. 2019;109:122–6. [Google Scholar]
- 43.Kleven H, Landais C, Søgaard JE. Children and Gender Inequality: Evidence from Denmark. American Economic Journal: Applied Economics. 2019;11(4):181–209. [Google Scholar]
- 44.Hanauer A. Institute on Taxation and Economic Policy. 2022. [cited 2023 Dec 14]. Abortion-Restricting States Do Least for Children. Available from: https://itep.org/abortion-restricting-states-do-least-for-children/ [Google Scholar]
- 45.Jacobs David E, Clickner Robert P, Zhou Joey Y, Viet Susan M, Marker David A, Rogers John W, et al. The prevalence of lead-based paint hazards in U.S. housing. Environmental Health Perspectives. 2002. Oct 1;110(10):A599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muñoz I, Colacino JA, Lewis RC, Arthur AE, Meeker JD, Ferguson KK. Associations between school lunch consumption and urinary phthalate metabolite concentrations in US children and adolescents: Results from NHANES 2003–2014. Environment International. 2018. Dec 1;121:287–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biggs MA, Upadhyay UD, McCulloch CE, Foster DG. Women’s Mental Health and Well-being 5 Years After Receiving or Being Denied an Abortion: A Prospective, Longitudinal Cohort Study. JAMA Psychiatry. 2017. Feb 1;74(2):169–78. [DOI] [PubMed] [Google Scholar]
- ••48. Dave D, Fu W, Yang M. Mental Distress Among Female Individuals of Reproductive Age and Reported Barriers to Legal Abortion Following the US Supreme Court Decision to Overturn Roe v Wade. JAMA Network Open. 2023. Mar 23;6(3):e234509–e234509. This article shows that stress levels increased among women in the US following the Dobbs decision.
- 49.Rajkumar RP. The Relationship Between Access to Abortion and Mental Health in Women of Childbearing Age: Analyses of Data From the Global Burden of Disease Studies. Cureus. 2022. Nov 13;14(11):e31433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clark EA, Cordes S, Lathrop E, Haddad LB. Abortion restrictions in the state of Georgia: Anticipated impact on people seeking abortion. Contraception. 2021. Feb 1;103(2):121–6. [DOI] [PubMed] [Google Scholar]
- 51.Post SM, Jobe MC, Malekzadeh AN, AuBuchon KE, Hoffman RK, Stock ML, et al. Watching the fall of Roe v. Wade: Media exposure relates to U.S. women’s alcohol use intentions. Psychol Addict Behav. 2023. Sep 7; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.American Psychological Association. Stress in America™. 2020. (A National Mental Health Crisis.). [Google Scholar]
- 53.Wiley KS, Knorr DA, Chua KJ, Garcia S, Fox MM. Sociopolitical stressors are associated with psychological distress in a cohort of Latina women during early pregnancy. Journal of Community Psychology. 2023. Sep 1;51(7):3044–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramos IF, Campos B, Schetter CD. Pregnancy Anxiety and Beliefs Surrounding Motherhood in Latinas: A Qualitative Study. J Lat Psychol. 2022. Nov;10(4):277–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ballard PJ, Hoyt LT, Yazdani N, Kornbluh M, Cohen AK, Davis AL, et al. Election-related sociopolitical stress and coping among college students in the United States. Journal of American College Health. 2022. Sep 9;1–11. [DOI] [PubMed] [Google Scholar]
- 56.Latendresse G. The interaction between chronic stress and pregnancy: preterm birth from a biobehavioral perspective. J Midwifery Womens Health. 2008/12/31 ed. 2009. Jan;54(1):8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shahid Z, Asuka E, Singh G. Physiology, Hypothalamus. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 58.Kogler L, Müller VI, Chang A, Eickhoff SB, Fox PT, Gur RC, et al. Psychosocial versus physiological stress — Meta-analyses on deactivations and activations of the neural correlates of stress reactions. NeuroImage. 2015. Oct 1;119:235–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thau L, Gandhi J, Sharma S. Physiology, Cortisol. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 60.Dahlerup BR, Egsmose EL, Siersma V, Mortensen EL, Hedegaard M, Knudsen LE, et al. Maternal stress and placental function, a study using questionnaires and biomarkers at birth. PLOS ONE. 2018. Nov 15;13(11):e0207184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Giurgescu C. Are maternal cortisol levels related to preterm birth? J Obstet Gynecol Neonatal Nurs. 2009. Aug;38(4):377–90. [DOI] [PubMed] [Google Scholar]
- 62.Hoyt LT, Zeiders KH, Chaku N, Niu L, Cook SH. Identifying diurnal cortisol profiles among young adults: Physiological signatures of mental health trajectories. Psychoneuroendocrinology. 2021. Jun 1;128:105204. [DOI] [PubMed] [Google Scholar]
- 63.Stanton SJ, LaBar KS, Saini EK, Kuhn CM, Beehner JC. Stressful politics: Voters’ cortisol responses to the outcome of the 2008 United States Presidential election. Psychoneuroendocrinology. 2010. Jun 1;35(5):768–74. [DOI] [PubMed] [Google Scholar]
- 64.Blanton H, Strauts E, Perez M. Partisan Identification as a Predictor of Cortisol Response to Election News. Political Communication. 2012. Oct 1;29(4):447–60. [Google Scholar]
- 65.Filardi T, Panimolle F, Lenzi A, Morano S. Bisphenol A and Phthalates in Diet: An Emerging Link with Pregnancy Complications. Nutrients. 2020;12(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eick SM, Goin DE, Cushing L, DeMicco E, Smith S, Park JS, et al. Joint effects of prenatal exposure to per- and poly-fluoroalkyl substances and psychosocial stressors on corticotropin-releasing hormone during pregnancy. Journal of Exposure Science & Environmental Epidemiology [Internet]. 2021. Apr 6; Available from: 10.1038/s41370-021-00322-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barrett ES, Corsetti M, Day D, Thurston SW, Loftus CT, Karr CJ, et al. Prenatal phthalate exposure in relation to placental corticotropin releasing hormone (pCRH) in the CANDLE cohort. Environment International. 2022. Feb 1;160:107078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Appleton AA, Jackson BP, Karagas M, Marsit CJ. Prenatal exposure to neurotoxic metals is associated with increased placental glucocorticoid receptor DNA methylation. Epigenetics. 2017. Aug 3;12(8):607–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen X, Xu S, Tan T, Lee ST, Cheng SH, Lee FW, et al. Toxicity and Estrogenic Endocrine Disrupting Activity of Phthalates and Their Mixtures. International Journal of Environmental Research and Public Health. 2014;11(3):3156–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.James-Todd T, Senie R, Terry MB. Racial/Ethnic Differences in Hormonally-Active Hair Product Use: A Plausible Risk Factor for Health Disparities. Journal of Immigrant and Minority Health. 2012. Jun 1;14(3):506–11. [DOI] [PubMed] [Google Scholar]
- 71.Richman LS, Jonassaint C. The Effects of Race-related Stress on Cortisol Reactivity in the Laboratory: Implications of the Duke Lacrosse Scandal. Annals of Behavioral Medicine. 2008. Feb 1;35(1):105–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •72. Dench D, Pineda-Torres M, Myers C. The Effects of the Dobbs Decision on Fertility. SSRN. 2023. Nov 27;IZA Discussion Paper No. 16608,. This article shows the preliminary impact of the Dobbs decision on the birth rate.


