Abstract
Objectives:
The principal aim of our study is to investigate risk factors for lateral trochanteric pain (LTP) after direct anterior approach (DAA) primary total hip arthroplasty (THA).
Methods:
A retrospective case control study was developed from 542 patients who underwent primary THA over a 9-year period to form two patient cohorts. Two hundred and seventy-one patients diagnosed with LTP were matched with 271 controls. Chart review revealed patient demographics, surgical approach, and femoral components utilized. Change in limb length and offset were assessed through preoperative and postoperative radiographic measurements.
Results:
There was a higher proportion of current or former smokers in the LTP group (34.5% vs 21.74%, p=0.003). There was no significant difference in use of high offset stems vs. standard offset stems between groups (15.9% vs. 18.5%, p=0.494). However, the LTP group had significantly higher increase in both femoral offset (+3.55mm vs +1.79mm, p<0.001) and total offset (+0.16mm vs -1.16mm, p=0.031) in comparison to controls.
Conclusion:
An increase in total offset, femoral offset, and smoking history are factors associated with LTP after DAA primary THA.
Key Words: DAA, Direct anterior approach, Femoral offset, Lateral trochanteric pain, THA
Introduction
Total hip arthroplasty (THA) is one of the most successful orthopaedic surgeries and its demand is on the rise.1,2 The goal of performing a THA is to eliminate pain and improve function, however THA surgery is not without risk and some patients have debilitating post-operative complaints.3 One of the most common complaints following THA is lateral trochanteric pain (LTP), with incidence ranging from 1.2 to 23.3%.4-9 LTP can worsen postoperative outcomes, and can be severe enough to cause patients to regress to an overall disability similar their pre-arthroplasty state.8-10
It is believed that LTP pain is initiated from repetitive microtrauma to the soft tissue overlying the greater trochanter and tearing and atrophy of the abductor muscles and tendons.11,12 LTP can be successfully treated with conservative measures such as rest, physical therapy, heat, ultrasound, non-steroidal anti-inflammatories, and corticosteroid injections.6,13,14 In their large retrospective review, Skibicki et al found a greater than 95% success rate in patients with LTP treated with physical therapy and oral medications and found an almost 90% success rate with three or less corticosteroid injections.6
Previous studies had identified several risk factors for the development of LTP. Specifically, multiple studies have indicated that female gender is a risk factor for LTP.6,8,15 Other potential risk factors such as surgical approach and offset are not agreed upon.6,8,13,14 Initially described by Charnley, femoral offset is critical for a stable and functional THA and plays an important role in THA longevity. The abductors of the hip must counteract the force of body weight during the stance phase of gait. Increasing offset optimizes the lever arm and provides a mechanical advantage of the abductors, therefore, decreasing joint reactive forces and polyethylene wear.16-18 Some authors suggest that increased femoral offset and alteration in hip biomechanics lead to LTP after THA.7,19,20 Others found no correlation between high offset components8 or femoral offset21,22 and the development of LTP.
In spite of the speculation of the relationship between offset and LTP, there is a paucity of data in the orthopaedic literature. We hypothesize that increasing total offset will lead to an increase in LTP following THA. The principal aim of our study is to investigate risk factors for LTP after direct anterior approach (DAA) primary THA.
Materials and Methods
Study Design
After approval by the Institutional Review Board, we performed a retrospective review of all primary hip replacements performed at our academic institution between October 31, 2010 and October 31, 2019. Further screening was performed for the diagnosis of ipsilateral trochanteric bursitis using an ICD-10 diagnosis code (International Classification of Diseases, 10th Revision [ICD-10] M70.60, ICD-10 M70.61, ICD-10 M70.62). The clinical diagnosis of LTP was defined as any patient with an ICD-10 diagnosis code for ipsilateral trochanteric bursitis plus subjective complaints of lateral hip pain as well as objective tenderness to palpation over the greater trochanter.
All patients over the age of 18 who underwent primary THA and were diagnosed with LTP were identified (N=573). The overall incidence of LTP following primary THA in our study population was 1.7% (573/33,761). In order to limit confounding variables, inclusion criteria consisted of surgery performed through the direct anterior approach by 1 of 4 high-volume adult reconstruction surgeons. Patients were excluded if they were less than 18 years old, had surgery performed through the direct lateral or posterior approach, had a history of ipsilateral revision THA, periprosthetic fracture, infection, previous diagnosis of LTP, or dislocation prior to LTP diagnosis. Furthermore, patients were excluded if insufficient radiographs were available or if the operative report was incomplete. A control group was matched in a one-to-one ratio by age, sex, and body mass index (BMI). The final cohort was divided into two groups: LTP group (N=271) and the control group (N=271).
Stem choice was determined by surgeon preference. A sub-analysis was performed to compare high offset stems (N=93) vs. standard stems (N=449). The primary outcome of our study was to identify potential risk factors for LTP after primary THA.
Data Collection
Qualitative data collected for both groups included demographics, laterality, medical comorbidities and smoking history. Operative notes were assessed to record type of femoral stem implanted (high offset vs. standard offset).
Radiographic analysis was performed by a fellowship-trained adult reconstruction surgeon. Radiographs were interpreted using our institution’s viewing software (Sectra Workstation IDS7, Sectra, Linkoping, Sweden) under 2x magnification. Preoperative and postoperative anteroposterior (AP) pelvic radiographs were available for all patients included in the study. Each radiograph was calibrated using a radiopaque sphere of known diameter prior to performing measurements.
Figure 1 demonstrates the measurements that were recorded for each patient preoperatively and postoperatively [Figure 1]. Leg length was measured by first drawing a line tangential and parallel to the most inferior portion of the ischial tuberosity. The most inferior aspect of the ipsilateral lesser trochanter was marked. The perpendicular distance between the ischial tuberosity line and the lesser trochanter line was recorded in millimeters. These measurements were made on the preoperative films and compared to the postoperative films to see if any change in limb length existed, reflecting an overall lengthening or shortening of the operated limb.23,24
Figure 1.
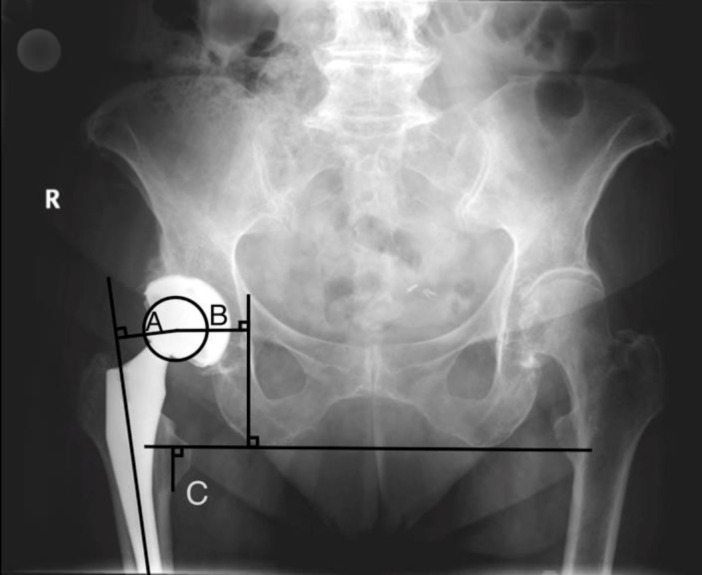
AP Pelvis Measurements: Femoral offset (A) is the distance from the femoral axis to the center of rotation of the femoral head (A), and cup offset (B) is the distance from the medial tear drop to the center of rotation of the femoral head. Total offset equals femoral offset (A) plus cup offset (B). Leg length (C) is the perpendicular distance between the ischial tuberosity line and the lesser trochanter line
When measuring offset on radiographs, we followed the protocol described by Al-Amiry et al. The total offset was measured from the femoral axis, through the center of rotation of the femoral head and ended at the medial aspect of the tear drop. Total offset was divided into femoral offset and cup offset. Femoral offset was recorded as the distance from the femoral axis to the center of rotation of the femoral head and cup offset was measured from the medial tear drop to the center of rotation of the femoral head.25 The difference between postoperative and preoperative measurements from the ipsilateral hip were recorded to obtain an overall change in offset.
Statistical analysis
Statistical analysis was performed using R Studio Software (version 3.6.3, Vienna, Austria). All continuous parametric data is presented as mean (standard deviation) and was analyzed using the Student’s T-tests. Non-parametric continuous data is presented as median and was analyzed by performing the Mann-Whitney tests. All categorical data was compared using the Fisher exact and chi-square tests. All p-values < 0.05 were deemed significant.
Results
Patient Demographics & Surgical Details
In this retrospective case-control study, 542 patients were identified for analysis; 271 in the LTP case group and 271 in the control group. There was no statistically significant difference in age, sex, and body mass index (BMI) between groups, indicating successful matching. The average time between primary THA surgery and LTP diagnosis was 1.5 (SD 1.3) years. There was a higher proportion of current or former smokers in the LTP group in comparison to the controls (34.5% vs 21.74%, p=0.003, [Table 1]. The type of stem used (standard offset or high offset) was not found to be significantly different (15.9% vs 18.5%, p=0.494, [Table 1].
Table 1.
Demographics and Surgical Details
|
Control
(N=271) |
Case (LTP)
(N=271) |
P Value | |
|---|---|---|---|
| Age (years) | 68.2 (9.61) | 67.9 (9.69) | 0.889 |
| Sex | 0.926 | ||
| Female | 190 (70.1%) | 188 (69.4%) | |
| Male | 81 (29.9%) | 83 (30.6%) | |
| Body Mass Index | 29.1 (5.62) | 29.5 (5.15) | 0.388 |
| Smoking History | 0.003 | ||
| Current | 15 (5.54%) | 31 (11.5%) | |
| Former | 44 (16.2%) | 62 (23.0%) | |
| Non-Smoker | 212 (78.2%) | 177 (65.6%) | |
| Laterality | 0.662 | ||
| Left | 108 (39.9%) | 114 (42.1%) | |
| Right | 163 (60.1%) | 157 (57.9%) | |
| Stem Offset | 0.494 | ||
| Standard Offset | 221 (81.5%) | 228 (84.1%) | |
| High Offset | 50 (18.5%) | 43 (15.9%) |
Radiographic Measurements
The LTP group had significantly more increase in femoral offset (average of +3.55mm vs +1.79mm, p=0.004) and total offset (average of +0.16mm vs -1.16mm, p=0.03) compared to controls. There was no difference in leg length change between the LTP group and controls (average of +3.69mm vs +3.41mm, p=0.694) [Table 2].
Table 2.
Radiographic Measurements
| Control (N=271) | Case (N=271) | P Value | |
|---|---|---|---|
| Total Offset change (mm) | -1.16 (8.68) | 0.16 (9.90) | 0.031 |
| Cup offset change (mm) | -2.90 (5.48) | -3.22 (5.71) | 0.854 |
| Fem offset change (mm) | 1.79 (7.47) | 3.55 (8.41) | 0.004 |
| Leg Length Discrepancy (mm) | 3.41 (6.16) | 3.69 (7.38) | 0.694 |
Standard vs. High Offset Femoral Stems
Table 3 displays a sub-analysis of high offset stems vs. standard offset stems. The sub-analysis included 93 high offset stems, with 43 (46.2%) of those patients having LTP. The high offset stem did not demonstrate a statistically significant increase in femoral offset, total offset, or leg length [Table 3].
Table 3.
Comparison of Standard vs. High Offset Femoral Stems
| Standard Offset (N=449) | High Offset (N=93) | P Value | |
|---|---|---|---|
| Control vs Case (LTP) | 0.494 | ||
| Control | 221 (49.2%) | 50 (53.8%) | |
| Case (LTP) | 228 (50.8%) | 43 (46.2%) | |
| Total Offset change (mm) | -0.53 (9.60) | -0.36 (7.93) | 0.636 |
| Cup offset change (mm) | -2.86 (5.46) | -4.04 (6.12) | 0.067 |
| Fem offset change (mm) | 2.46 (8.13) | 3.69 (7.27) | 0.144 |
| Leg Length Discrepancy (mm) | 3.47 (6.68) | 3.91 (7.34) | 0.831 |
Discussion
LTP is a common complaint following THA that can lead to low patient satisfaction and the potential for outcomes similar to patients with end stage osteoarthritis of the hip.8,10 There are many published studies that aim to determine the risk factors and cause of LTP, however, there is no consensus in the literature.7,8,19 In addition, prior studies are limited by assessment of multiple difference approaches and small sample sizes. The primary aim of this study is to more thoroughly evaluate the risk factors for LTP, notably femoral and total offset, in patients who underwent THA through one uniform approach.
Increasing femoral offset has many biomechanical benefits in THA.22,26-34Although increased offset maximizes strength and range of motion, there are potential risks from increased tension on lateral tissues which can cause lateral trochanteric pain as demonstrated by Leibs et al.35 We hypothesized that increased offset would be associated with LTP. To our knowledge, no prior high-volume study has examined the relationship between change in femoral offset after DAA THA and the presence of LTP. We found that an increase in femoral offset (average +3.55mm vs +1.79mm, p=0.004) from preoperative measurements to be associated with LTP. We also found increased total offset (average +0.16mm vs -1.16mm, p=0.031) to be associated with LTP. While the clinical difference in average total offset change was small, though statistically significant, it represents an increase in offset for patients with LTP compared to an offset decrease for patients without LTP.
A retrospective cohort study by Iorio et al found that femoral offset and LLD did not correlate with postoperative LTP. Furthermore, they included patients with both the direct lateral and posterior approach, making it difficult to compare to our current study.8 Abdulkarim et al. and Sayed-Noor et al. echoed these findings by demonstrating that there was no relation between femoral offset and LTP. They used the direct lateral and posterior approach, respectively and did not include any patients with the direct anterior approach in their analysis.4,7 Wolicek et al. utilized CT scans to examined leg length and offset and its relation to LTP following THA through the anterolateral approach. They also found no significant relationship between leg length and offset and LTP.9 The volume of patients with LTP available for analysis was low in these prior studies, ranging from twenty-one to twenty-nine patients. Our much larger study included 271 patients with LTP and demonstrated that patients with LTP had significantly greater change in femoral and total offset. We provided a high volume of patients utilizing the direct anterior approach to eliminate an approach bias.
Our study demonstrated that a history of smoking was associated with LTP. Shemesh et al. also found that former smokers were more likely to have LTP in their large retrospective cohort study.14 Bishop el al. found that smoking is directly related to rotator cuff tears, which may represent a similar pathology seen in the current study. In a review of the negative effects smoking has on the musculoskeletal system, Lee et al. concluded that smoking is detrimental to the soft tissues and may have a large impact on tendon injury and tendon healing.36 our findings are consistent with this hypothesis.
Potential study limitations include its retrospective design and the use of plain radiographs for the measurement of the femoral offset and LLD. It is recognized that plain radiographs are inferior to CT scans for measurement of femoral offset.37 we mitigated this limitation by calibrating all radiographs to maintain consistent measurements and optimize accuracy and including preoperative and postoperative measurements from the ipsilateral hip, giving our measurements a true representation of the actual change in total offset. Additionally, plain radiographs do not differentiate confounding generators of lateral trochanteric pain (ie: abductor tears or subgluteal pathologies). Given the retrospective nature of the study, advanced imaging is not available for our review. We did not specifically screen all THA patients for LTP but instead relied on patients who presented with complaints of LTP. However, it is important to note that our study is the largest to date analyzing the relationship between offset and LTP. Furthermore, our cohort of LTP patients was matched in a one-to-one ratio with a control group to minimize confounding variables.
Conclusion
An increase in total offset, femoral offset, and smoking history are factors associated with LTP after DAA primary THA. Orthopaedic surgeons should aim to restore hip biomechanics while avoiding excessive offset if possible. Patients should be educated on the potential for postoperative LTP.
Acknowledgment
N/A
Authors Contribution:
All authors have made substantial contributions to this work including, but not limited to study design, data collection, data analysis, writing, and editing. All authors are responsible for the content of this manuscript.
Declaration of Conflict of Interest:
The authors declare that they have no conflict of interest.
Declaration of Funding:
authors have not received grant support or research funding or have any proprietary interests in the materials described in this article. The author(s) received NO financial support for the study
Declaration of Ethical Approval for Study:
This study was evaluated and approved by Rothman Orthopaedic Institute’s IRB- AtlantiCare Medical Regional Center- on 07/26/2023.
The study approval number is #2021-1081.
Declaration of Informed Consent:
There is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.
References
- 1.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–19. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Kelmer G, Stone AH, Turcotte J, King PJ. Reasons for Revision: Primary Total Hip Arthroplasty Mechanisms of Failure. J Am Acad Orthop Surg. 2021;29:78–87. doi: 10.5435/JAAOS-D-19-00860. [DOI] [PubMed] [Google Scholar]
- 4.Sayed-Noor AS, Sjoden GO. Greater trochanteric pain after total hip arthroplasty: the incidence, clinical outcome and associated factors. Hip Int. 2006;16:202–6. doi: 10.1177/112070000601600304. [DOI] [PubMed] [Google Scholar]
- 5.Moerenhout K, Benoit B, Gaspard HS, Rouleau DM, Laflamme GY. Greater trochanteric pain after primary total hip replacement, comparing the anterior and posterior approach: A secondary analysis of a randomized trial. Orthop Traumatol Surg Res. 2021;107:102709. doi: 10.1016/j.otsr.2020.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Skibicki HE, Brustein JA, Orozco FR, Ponzio DY, Post ZD, Ong AC. Lateral Trochanteric Pain Following Primary Total Hip Arthroplasty: Incidence and Success of Nonoperative Treatment. J Arthroplasty. 2021;36:193–9. doi: 10.1016/j.arth.2020.07.043. [DOI] [PubMed] [Google Scholar]
- 7.Abdulkarim A, Keegan C, Bajwa R, Sheehan E. Lateral trochanteric pain following total hip arthroplasty: radiographic assessment of altered biomechanics as a potential aetiology. Ir J Med Sci. 2018;187:663–8. doi: 10.1007/s11845-017-1701-1. [DOI] [PubMed] [Google Scholar]
- 8.Iorio R, Healy WL, Warren PD, Appleby D. Lateral trochanteric pain following primary total hip arthroplasty. J Arthroplasty. 2006;21:233–6. doi: 10.1016/j.arth.2005.03.041. [DOI] [PubMed] [Google Scholar]
- 9.Worlicek M, Messmer B, Grifka J, Renkawitz T, Weber M. Restoration of leg length and offset correlates with trochanteric pain syndrome in total hip arthroplasty. Sci Rep. 2020;10:7107. doi: 10.1038/s41598-020-62531-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fearon AM, Cook JL, Scarvell JM, Neeman T, Cormick W, Smith PN. Greater trochanteric pain syndrome negatively affects work, physical activity and quality of life: a case control study. J Arthroplasty. 2014;29:383–6. doi: 10.1016/j.arth.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Kagan A. Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999:135–40. [PubMed] [Google Scholar]
- 12.Pfirrmann CWA, Notzli HP, Dora C, Hodler J, Zanetti M. Abductor Tendons and Muscles Assessed at MR Imaging after Total Hip Arthroplasty in Asymptomatic and Symptomatic Patients. Radiology. 2005;235:969–76. doi: 10.1148/radiol.2353040403. [DOI] [PubMed] [Google Scholar]
- 13.Farmer KW, Jones LC, Brownson KE, Khanuja HS, Hungerford MW. Trochanteric Bursitis after Total Hip Arthroplasty: Incidence and Evaluation of Response to Treatment. J Arthroplasty. 2010;25:208–12. doi: 10.1016/j.arth.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Shemesh SS, Moucha CS, Keswani A, Maher NA, Chen D, Bronson MJ. Trochanteric Bursitis Following Primary Total Hip Arthroplasty: Incidence, Predictors, and Treatment. J Arthroplasty . 2018;33:1205–9. doi: 10.1016/j.arth.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 15.Schwartsmann CR, Loss F, de Freitas Spinelli L, et al. Association between trochanteric bursitis, osteoarthrosis and total hip arthroplasty. Rev Bras Ortop. 2014;49:267–70. doi: 10.1016/j.rboe.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970;72:7–21. [PubMed] [Google Scholar]
- 17.Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131–41. [PubMed] [Google Scholar]
- 18.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. . 2001:125–34. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Incavo SJ, Havener T, Benson E, McGrory BJ, Coughlin KM, Beynnon BD. Efforts to improve cementless femoral stems in THR: 2- to 5-year follow-up of a high-offset femoral stem with distal stem modification (Secur-Fit Plus) J Arthroplasty. 2004;19:61–7. doi: 10.1016/j.arth.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Liebs TR, Nasser L, Herzberg W, Rüther W, Hassenpflug J. The influence of femoral offset on health-related quality of life after total hip replacement. Bone Joint J. 2014;96-B:36–42. doi: 10.1302/0301-620X.96B1.31530. [DOI] [PubMed] [Google Scholar]
- 21.Sayed-Noor AS, Pedersen E, Wretenberg P, Sjödén GO. Distal lengthening of ilio-tibial band by Z-plasty for treating refractory greater trochanteric pain after total hip arthroplasty (Pedersen-Noor operation) Arch Orthop Trauma Surg. 2009;129:597–602. doi: 10.1007/s00402-008-0693-8. [DOI] [PubMed] [Google Scholar]
- 22.Cassidy KA, Noticewala MS, Macaulay W, Lee JH, Geller JA. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012;27:1863–9. doi: 10.1016/j.arth.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Austin MS, Hozack WJ, Sharkey PF, Rothman RH. Stability and leg length equality in total hip arthroplasty. J Arthroplasty. 2003;18:88–90. doi: 10.1054/arth.2003.50073. [DOI] [PubMed] [Google Scholar]
- 24.Williamson JA, Reckling FW. Limb Length Discrepancy and Related Problems Following Total Hip Joint Replacement. Clin Orthop Relat Res. 1978;134:135–8. [PubMed] [Google Scholar]
- 25.Al-Amiry B, Mahmood S, Krupic F, Sayed-Noor A. Leg lengthening and femoral-offset reduction after total hip arthroplasty: where is the problem - stem or cup positioning? Acta Radiol. 2017;58:1125–31. doi: 10.1177/0284185116684676. [DOI] [PubMed] [Google Scholar]
- 26.Husby VS, Bjørgen S, Hoff J, Helgerud J, Benum P, Husby OS. Unilateral vs bilateral total hip arthroplasty - the influence of medial femoral head offset and effects on strength and aerobic endurance capacity. Hip Int. 2010;20:204–14. doi: 10.1177/112070001002000211. [DOI] [PubMed] [Google Scholar]
- 27.Yamaguchi T, Naito M, Asayama I, Ishiko T. Total hip arthroplasty: the relationship between posterolateral reconstruction, abductor muscle strength, and femoral offset. J Orthop Surg. 2004;12:164–7. doi: 10.1177/230949900401200205. [DOI] [PubMed] [Google Scholar]
- 28.Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20:414–20. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 29.Kiyama T, Naito M, Shinoda T, Maeyama A. Hip Abductor Strengths After Total Hip Arthroplasty Via the Lateral and Posterolateral Approaches. J Arthroplasty. 2010;25:76–80. doi: 10.1016/j.arth.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 30.McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:865–9. [PubMed] [Google Scholar]
- 31.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–42. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 32.Matsushita A, Nakashima Y, Jingushi S, Yamamoto T, Kuraoka A, Iwamoto Y. Effects of the femoral offset and the head size on the safe range of motion in total hip arthroplasty. J Arthroplasty. 2009;24:646–51. doi: 10.1016/j.arth.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 33.Patel AB, Wagle RR, Usrey MM, Thompson MT, Incavo SJ, Noble PC. Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty. 2010;25 doi: 10.1016/j.arth.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 34.Kurtz WB, Ecker TM, Reichmann WM, Murphy SB. Factors affecting bony impingement in hip arthroplasty. J Arthroplasty. 2010;25:624–34. doi: 10.1016/j.arth.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 35.Liebs TR, Nasser L, Herzberg W, Ruther W, Hassenpflug J. The influence of femoral offset on health-related quality of life after total hip replacement. Bone Joint J. 2014;96-B:36–42. doi: 10.1302/0301-620X.96B1.31530. [DOI] [PubMed] [Google Scholar]
- 36.Lee JJ, Patel R, Biermann JS, Dougherty PJ. The musculoskeletal effects of cigarette smoking. J Bone Joint Surg Am. 2013;95:850–9. doi: 10.2106/JBJS.L.00375. [DOI] [PubMed] [Google Scholar]
- 37.Weber M, Woerner ML, Springorum H-R, Hapfelmeier A, Grifka J, Renkawitz TF. Plain radiographs fail to reflect femoral offset in total hip arthroplasty. J Arthroplasty. 2014;29:1661–5. doi: 10.1016/j.arth.2014.03.023. [DOI] [PubMed] [Google Scholar]


