Abstract
Introduction
We report a case of troubleshooting against bleeding from an inferior vena cava injury using a gelatin–thrombin matrix.
Case presentation
A 58‐year‐old man underwent robot‐assisted partial adrenalectomy for a right adrenal adenoma causing subclinical Cushing's syndrome. During the surgery, while dissecting between the adrenal gland and the inferior vena cava, bleeding occurred secondary to an inferior vena cava injury. Despite attempts at hemostasis, applying a human fibrinogen–thrombin patch and suturing were both difficult because of poor vision secondary to the bleeding. Hemostasis was ultimately achieved using a gelatin–thrombin matrix, which was accurately placed on the bleeding point using gauze. Open conversion was hence avoided, allowing the completion of the surgery as planned.
Conclusion
Gelatin–thrombin matrix may be effective for managing relatively small inferior vena cava injuries.
Keywords: gelatin–thrombin matrix, inferior vena cava injury, partial adrenalectomy, robotic surgery, troubleshooting
Abbreviations & Acronyms
- GTM
gelatin–thrombin matrix
- IVC
inferior vena cava
Keynote message.
In laparoscopic or robotic surgery, even minor injuries to the inferior vena cava can result in significant bleeding and can be challenging to manage. How can it be dealt with using a minimally invasive approach, avoiding open conversion? One method of dealing with inferior vena cava injuries is presented.
Introduction
In laparoscopic urologic surgery including robotic surgery, severe vascular injury is relatively rare, but can lead to extremely serious consequences when it occurs. Particularly, injuries to the IVC can result in dire situations, sometimes necessitating conversion to open surgery. It is crucial to be well‐versed in various ways of dealing with such injuries. Herein, we report a case of bleeding from an IVC injury during a robot‐assisted right partial adrenalectomy in which hemostasis was achieved using a GTM.
Case presentation
The patient was a 58‐year‐old man who had been receiving treatment for hypertension, diabetes, and hyperlipidemia at a local clinic. A CT scan incidentally revealed a right adrenal adenoma (24 × 14 mm), and further examination led to a diagnosis of subclinical Cushing's syndrome. Due to a history of left adrenalectomy for subclinical Cushing's syndrome, a robot‐assisted partial adrenalectomy was performed for a right adrenal adenoma. The patient was placed in the left lateral decubitus position and the operation was started using a transperitoneal approach. After dissecting between the kidney and the adrenal gland, dissection between the adrenal gland and the IVC was initiated. To reach the psoas muscle on the dorsal side of the adrenal gland, using bipolar forceps to retract the adrenal gland upward and applying contralateral traction to the IVC downward with the assistant's forceps, dissection was performed between the adrenal gland and the IVC. While the IVC was held under contralateral traction, the adrenal gland was retracted upward with a robot arm. This caused the tissue between the adrenal gland and the IVC, which had not been sufficiently dissected, to be pulled, resulting in bleeding from the IVC that appeared to be caused by pulling out of small blood vessel from the IVC (Fig. 1a,b). After increasing the intra‐abdominal pressure to 15 mmHg, we endeavored to achieve hemostasis through gauze compression (total compression time was 54 min), but hemostasis could not be attained. After the bleeding point was identified, we attempted to apply a human fibrinogen–thrombin patch. However, it was difficult to successfully apply the patch to the bleeding point because the field of vision was instantly impaired secondary to bleeding when the pressure was released. Similarly, it was difficult to suture the bleeding point because of poor vision secondary to the hemorrhage. Therefore, hemostasis was attempted using a GTM. Due to severe bleeding and poor visual field, the GTM was placed on the gauze (Fig. 2a) and promptly replaced with gauze pressing on the bleeding point (Fig. 2b,c), and pressure was attempted for 5 min (Fig. 2d). Hemostasis was then achieved (Fig. 3) by the effect of the GTM in contact with the bleeding point. After hemostasis, the GTM was flushed out, and no fillings interfered with the operation. Open conversion was hence avoided, and the operation could be completed as planned.
Fig. 1.
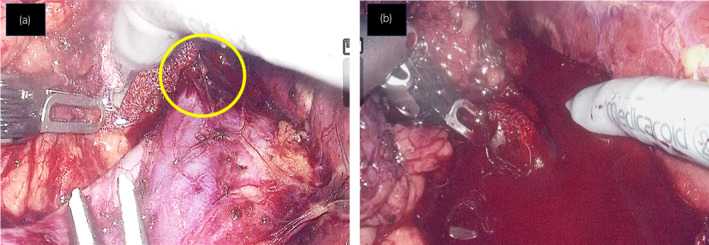
(a) Just before the robot arm pulled the adrenal gland upward and caused bleeding from the IVC. The circle indicates the tissue between the adrenal gland and the IVC that had not been sufficiently dissected. (b) Bleeding from the IVC injury.
Fig. 2.
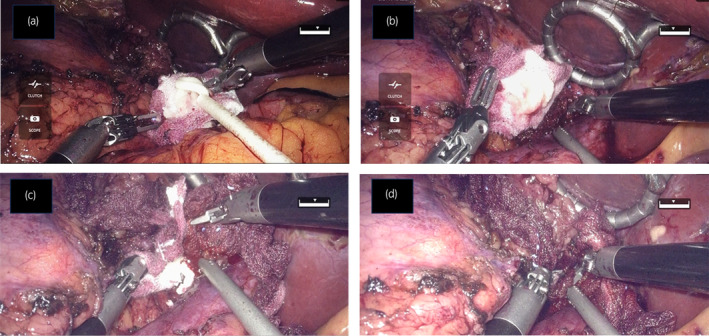
(a) GTM placed on a gauze. (b,c) Gauze pressing on the bleeding point was quickly replaced with a gauze with GTM on it. (d) Applying pressure with gauze containing GTM.
Fig. 3.
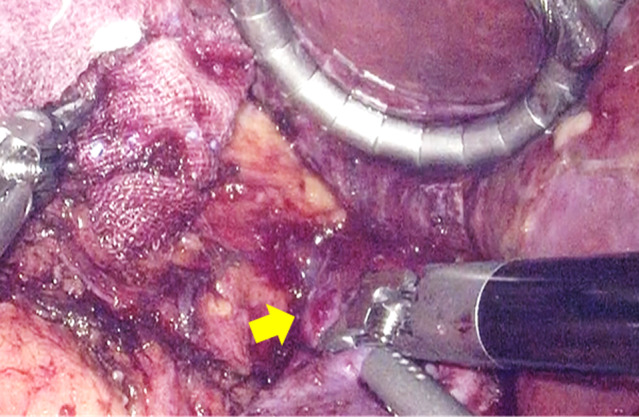
Achievement of hemostasis. The arrow indicates the bleeding point.
Discussion
The incidence of major vascular injuries during laparoscopic urologic procedures is reported to be 1.7%, with 1.4% of cases involving the IVC. 1 Robotic surgery has many advantages, but also carries the potential for catastrophic vascular complications. In case of bleeding from the IVC, the first step in management is direct pressure with gauze to control the bleeding. If a hole is visible, suturing may be attempted to control the bleeding. 2 , 3 Despite the widespread use of robotic surgery and increasing experience with laparoscopic suturing, depending on the site and severity of the bleeding, suturing can be extremely difficult, leading to the consideration of open conversion. GTM is an absorbable homeostatic agent containing porcine gelatin and human thrombin. 4 , 5 Upon contact with blood, the gelatin matrix provides an environment for platelets to adhere and aggregate, thereby promoting the activity of the patient's coagulation cascade to achieve hemostasis. Thrombin assists in hemostasis by promoting the formation of fibrin clots. One of the features of GTM is that it is flowable hemostats and adapts to the irregular shape of the wound surface, allowing surgeons to apply it flexibly and achieve effective tissue contact. Additionally, since the excess can be washed away, it helps maintain a clear view, avoiding the visual obstruction that can occur when overlapping sheet‐type hemostats. GTM is widely used in various surgical fields globally and can be used in both open and laparoscopic surgeries. For the hemostatic effect of a GTM to be achieved, the GTM must have contact with the bleeding point. In case of bleeding from the IVC, it is difficult to apply a GTM to the bleeding site using an endoscopic applicator because of immediate loss of visibility secondary to bleeding. Our method of placing a GTM on a gauze and promptly replacing it with gauze pressing on the bleeding point allows effective contact of the GTM with the bleeding point. Even if hemostasis is not achieved immediately, repeating the process may gradually diminish the intensity of the bleeding. To the best of our knowledge, this is the first report to mention the hemostatic effectiveness of GTM for bleeding from an IVC injury. Although GTM is considered effective for relatively small IVC injuries, it is worth trying because of the potential to avoid open conversion.
Conclusion
Here, a successful case of troubleshooting against bleeding from an IVC injury is reported using a GTM. Because of the variety of situations that may arise in case of an IVC injury, surgeons should be prepared to be flexible.
Author contributions
Tadamasa Shibuya: Writing – original draft. Toru Inoue: Writing – review and editing. Tadasuke Ando: Writing – review and editing. Toshitaka Shin: Writing – review and editing.
Conflict of interest
The authors declare no conflict of interest.
Approval of the research protocol by an Institutional Reviewer Board
Not applicable.
Informed consent
Written informed consent was obtained from the patient for publication in this paper.
Registry and the Registration No. of the study/trial
Not applicable.
Acknowledgments
We appreciate the cooperation of the staff in our institution.
References
- 1. Theil R, Adams JB, Schulam PG, Moore RG, Kavoussi LR. Venous dissection injuries during laparoscopic urological surgery. J. Urol. 1996; 155: 1874–1876. [PubMed] [Google Scholar]
- 2. Moreira DM, Kavoussi LR. Laparoscopic and robotic surgery of the kidney. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA (eds). Campbell‐Walsh‐Wein Urology, 12th edn. Elsevier, Philadelphia, 2020; 2279–2308. [Google Scholar]
- 3. Lim SK, Rha KH. Surgery of the adrenal glands. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA (eds). Campbell‐Walsh‐Wein Urology, 12th edn. Elsevier, Philadelphia, 2020; 2405–2426. [Google Scholar]
- 4. Obermair H, Janda M, Obermair A. Real‐world surgical outcomes of a gelatin‐hemostatic matrix in women requiring a hysterectomy: a matched case‐control study. Acrata Obstet. Gynecol. Scand. 2016; 95: 1008–1014. [DOI] [PubMed] [Google Scholar]
- 5. Woodworth BA, Chandra RK, LeBenger JD, Ilie B, Schlosser RJ. A gelatin‐thrombin matrix for hemostasis after endoscopic sinus surgery. Am. J. Otolaryngol. 2009; 30: 49–53. [DOI] [PubMed] [Google Scholar]


