Abstract
Introduction
Hernia repair is a common procedure performed by general surgeons. Introduced in 1990s, the use of laparoscopic hernia repair has recently increased and, consequently, rare complications previously unknown have been reported.
Presentation of case
A 43-years-old male patient who underwent a transabdominal preperitoneal patch plasty (TAPP) procedure for symptomatic bilateral inguinal hernia. On the sixth postoperative day, the patient was admitted for small bowel obstruction (SBO) and underwent reoperation; the central portion of the peritoneal suture in the left inguinal region was lacerated and a hole in the peritoneum had performed a hernia orifice, causing small bowel occlusion by preperitoneal herniation. After the hernia was released, the peritoneum was closed again and the surgery was completed.
Discussion
SBO after TAPP procedure is a rare complication and should be considered in patients with abdominal pain and vomiting after TAPP procedure.
Conclusion
This complication can be prevented with appropriate peritoneal closure techniques and treated with early laparoscopic surgery.
Keywords: Transabdominal preperitoneal hernioplasty, Complications, Laparoscopy, Inguinal hernia, Small bowel occlusion
Highlights
-
•
The Transabdominal Preperitoneal Hernia Repair is a safe procedure.
-
•
The small bowel occlusion after TAPP is a rare entity.
-
•
The Preperitoneal hernia after TAPP procedure is a very rare disease.
-
•
This complication can be prevented with appropriate peritoneal closure techniques.
-
•
This complication can be treated with laparoscopic surgery.
1. Introduction
Repair of inguinal hernias is one of the most common procedures performed by general surgeons around the world.
Minimally invasive techniques for groin hernia reapir were first introduced in the early 1980s.
Transabdominal preperitoneal (TAPP) hernioplasty is, today, a commonly used technique for the repair of adult inguinal hernias [1].
Its benefits are fast recovery, less surgical site complications, less postoperative discomfort and a shorter time to return to work [[1], [2], [3]].
Patients have better quality of life scores and degree of satisfaction after laparoscopic inguinal repair, what makes this operation an appropriate treatment for patients with inguinal hernia [4].
Postoperative complications of laparoscopic surgery are rare and minor, including seroma formation, internal organ damage, chronic pain and testicular complications. As increasing numbers of TAPP procedures are being performed worldwide, uncommon complications have become more frequent and need to be considered in perioperative and postoperative management.
The TAPP procedure requires peritoneal opening and suturing, and abdominal adhesion may still occur, leading to serious complications such as intestinal obstruction, strangulation and necrosis.
Small bowel obstruction is a rare complication after TAPP procedure and has been reported to occur in ~0.1–0.23 % of cases [2].
This report presents a case of Small Bowel Occlusion caused by a laceration of the peritoneum after TAPP, resulting in a preperitoneal hernia.
The present work has been reported in line with the SCARE criteria [5].
2. Presentation of case
A 43-years-old male patient who underwent a TAPP procedure for symptomatic bilateral inguinal hernia (direct on the right and indirect to the left). Clinical history of arterial hypertension treated with ACE inhibitors. No alterations in preoperative tests. No previous surgery.
TAPP procedure was performed by an experienced laparoscopic surgeon. The anatomic 3D meshes were fixed with the absorbable Tacks. In this case, peritoneal closure was achieved with continuous absorbable suture (Vicryl 2/0). No tension was present during peritoneal closure. The operative time was 65 min and no intraoperative problems were observed. The patient was discharged on the first day after surgery, however, he was readmitted to the hospital on the third postoperative day because abdominal pain and vomiting.
No pain on palpation of the abdomen or signs of parietal rigidity. Bowel open to feces and gas. Blood tests normal, no alterations on the CT performed urgently in the emergency room (Fig. 1).
Fig. 1.
CT-Scan performed on the third postoperative day which shows no signs of small bowel obstruction.
The symptoms resolved spontaneously after 2 h of fasting and rehydration, therefore, the patient was discharged.
However, he continued to have intermittent abdominal pain, in left side, and he was readmitted again on postoperative day 6.
The new CT showed fluid distention of some loops of the small intestine, with thickened walls, in the lower left abdominal quadrant without signs of caliber alteration (Fig. 2, Fig. 3).
Fig. 2.
CT-Scan performed on the sixth postoperative day, showed fluid distention of some loops of the small intestine.
Fig. 3.
CT-Scan performed on the sixth postoperative day, showed fluid distention of some loops of the small intestine with thickened walls, in the lower left abdominal quadrant without signs of caliber alteration.
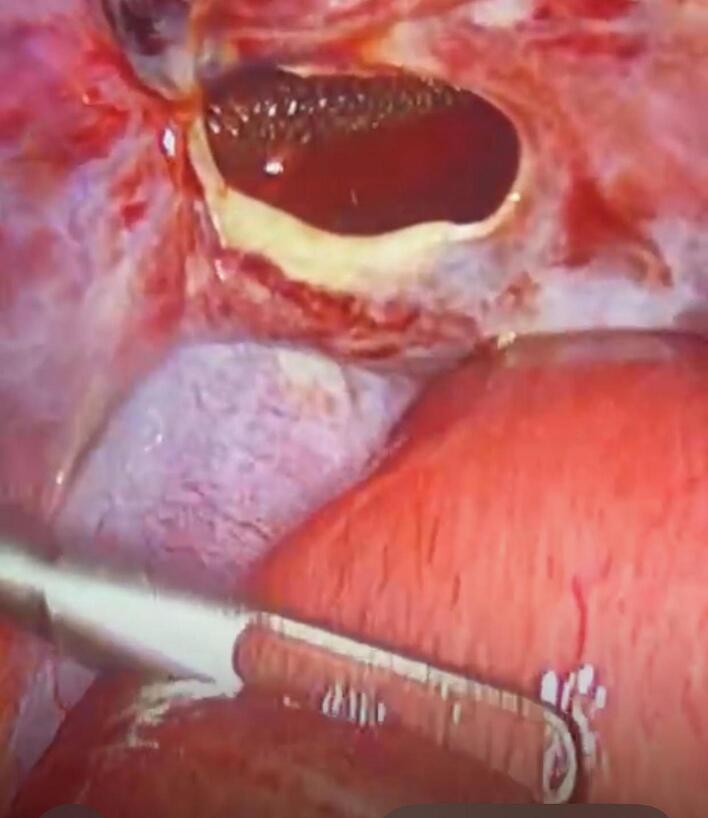
Emergency laparoscopy exploration revealed that the central portion of the peritoneal suture in the left inguinal region was detached and a hole in the peritoneum had performed a hernia orifice, causing small bowel occlusion by preperitoneal herniation (Fig. 4, Fig. 5).
Fig. 4.

Preperitoneal Hernia through partial dehiscence of the central portion of the surgical suture.
Fig. 5.
Peritoneal hernia port through which the prosthesis can be seen on the bottom.
The hernia was released, the peritoneal hole was sutured again with continous 2/0 Vicryl suture and absorbables Tacks and the surgery was completed. The postoperative course was good, and the patient was discharged from the hospital on the third postoperative day.
At the outpatient re-evaluation one month and three months after surgery, he did not present any hernia recurrence or abdominal pain.
3. Discussion
A hernia is a protrusion of a viscus or part of the viscus through the cavity wall in witch it normally resides. Conditions such as coughing, straining, obesity and intra-abdominal malignancy can precipitate hernias. More than 20 million patients worldwide are treated for inguinal hernias annually 2.
Although first described in the 1990s, laparoscopic inguinal hernia repair still finds resistance among surgeons today [6,7]. Main reasons are higher cost, need for general ansthesia and eventual higher rate of major complications associated with laparoscopic repairs [8,9]. Another difficulty related to laparoscopic approach is the greater surgical complexity associated with the need to identify a “new” anatomy of posterior inguinal wall, which is not usual for general surgeons [8,10].
However, there is current evidence for laparoscopic repairs demonstrating significant advantages such as less complications, especially on recurrent cases, faster recovery and less postoperative chronic pain, in addition to recurrence rates at least equivalent to conventional repairs. Patients have better quality of life scores and degree of satisfaction after laparoscopic inguinal repair, what makes this operation an appropriate treatment for patients with inguinal hernia [[11], [12], [13]].
Transabdominal preperitoneal (TAPP) hernioplasty is a commonly used technique for the repair of adult inguinal hernias. It is particularly feasible for bilateral inguinal hernias and recurrent inguinal hernias after open hernia repair [14,15].
The TAPP procedure requires peritoneal opening and suturing. As the peritoneal integrity is destroyed, intestinal occlusion occurs occasionally, usually because of adhesion between the bowel and the mesh, herniation at the trocar site, barbed sutures adhesion, or due to an internal hernia through the peritoneal closure defect [16,17].
Statistics show that the incidence of Small Bowel Occlusion after TAPP repair is ~0.1–0.23 % [18].
Therefore, the exact closure of the peritoneum is an indispensable step of TAPP surgery.
Peritoneal closure can be performed with running sutures, tacks, barbed sutures, staples and glue, according to the surgeon's preferences.
Although the running sutures reduced the incidence of intestinal obstruction from herniation through the peritoneal closure, the intra-abdominal suturing is time-consuming and technically demanding [19].
Otherwise, peritoneal closure using tacks, albeit much faster, increased short-term pain compared with suture closure which remain the preferred method [20].
Kapiris et al. observed seven cases (0.23 %) of small bowel occlusion because of peritoneal herniation in a 7-year study of 3017 patients undergoing TAPP hernia repair. They found that peritoneal closure with sutures, compared with other closures, decreased the incidence of this complication; this is probably the result of less tension on the peritoneal flap and a reduced risk of laceration. However, suture closure cannot completely eliminate this complication [19].
As noted in our experience, intestinal obstruction occurred despite continuous suturing.
A preperitoneal herniation is an extremely rare condition that could be avoided. Adequate and skillfull peritoneal closure, performed using a strictly standardized procedure, can achieve good results. Complete closure of the peritoneum during TAPP procedure is essential for preventing preperitoneal herniation and small bowel occlusion.
The dissection of the peritoneal flap from any adhesion and the reduction of the pressure of the pneumoperitoneum to 8 during its suturing are fundamental measures to avoid subsequent peritoneal lacerations.
Although a preritoneal hernia is rare, in the presence of a patient who has recently undergone a TAPP procedure, with vomiting, abdominal pain, constipation and other symptoms of intestinal obstruction, the suspicion of a possible internal hernia must be taken into consideration.
Contrast-enhanced CT Scan can help in the diagnosis of intestinal obstruction and represents a valid means for evaluating the vitality of the intestinal loops.
Laparoscopic surgery is recommended for treating intestinal obstruction after TAPP surgery. Although great care must be taken during insertion of trocars because dilation of the bowel, we believe that laparoscopy is feasible.
Therefor, it is imperative to examine the activity of the entrapped boewl, and it should be performed with caution. If intestinal necrosis or perforation develops, bowel resection and mesh removal shold be considered. Early diagnosis and appropriate treatment are crucial for successful outcomes in patients with small bowel obstruction after TAPP.
4. Conclusion
Although laproscopic TAPP is widely used and accepted as a treatment for inguinal hernia, it is important to remember that rare complications can occur. Appropriate peritoneal closure is recommended to reduce the risk of intestinal hernias and bowel obstruction. The possibility of preperitoneal hernia should be considered in patients with abdominal pain and vomiting after TAPP procedure. We consider laparoscopy the procedure of choise to diagnose and treat this complications.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Ethical approval
Ethic approval has been exempted by our institution because this is a case report and no new studies or new techniques were carried out. The Ethics Committee to which the ASP of Catania refers is the Catania Ethics Committee.
Guarantor
Giovambattista Caruso.
Research registration number
This case report does not require registration as a research study.
Funding
All the authors declare that this research didn't receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Giovambattista Caruso: conceptualization, writing original draft, review and editing, data curation.
Roberto Cantella: Methodology.
Eleonora Di Guardo, data curation.
Alberto Torrisi: Visualization.
Martina Reina: Data curation.
Giuseppe Angelo Reina: Supervision.
Conflict of interest statement
All the authors certify that there is no conflict of interest regarding the material discussed in the manuscript.
References
- 1.Man Yi, et al. Recurrent abdominal pain due to small bowel volvulus after transabdominal preperitoneal hernioplasty: a case report and review of literature. World J. Clin. Cases. May 26 2021;9(15):3696–3703. doi: 10.12998/wjcc.v9.i15.3696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shirakabe Katsudai, et al. Preperitoneal herniation after transabdominal preperitoneal patch plasty: a case report. J. Surg. Case Rep. 2023;3:1–3. doi: 10.1093/jscr/rjad099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caruso G., et al. Gangrenous appendicitis in Amyand’s hernia: surgical approach under local anesthesia. Case report and review of the literature. Int. J. Surg. Case Rep. Feb 2021;79:215–218. doi: 10.1016/j.ijscr.2021.01.048. (Epub 2021 Jan 16) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Furtado Marcelo, et al. Systemization of laparoscopic inguinal hernia repair (TAPP) based on a new anatomical concept; Inverted Y and Five Triangles. ABCD Arq. Bras. Cir. Dig. 2019;32(1) doi: 10.1590/0102-672020180001e1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: aggiornamento delle linee guida consensus Surgical CAse REport (SCARE) Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Askarpour S., et al. Comparison between inguinal herniotomies with and without incising external oblique aponeurosis: a randomized clinical trial. Arq. Bras. Cir. Dig. Jul-Sep 2017;30(3):187–189. doi: 10.1590/0102-6720201700030006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosi H.R., et al. Robotic assisted single site for bilateral inguinal hernia repair. Arq. Bars. Cir. Dig. Apr-Jun 2016;29(2):109–111. doi: 10.1590/0102-6720201600020011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neumayer L., et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N. Engl. J. Med. 2004;350(18):1819–1827. doi: 10.1056/NEJMoa040093. [DOI] [PubMed] [Google Scholar]
- 9.Simons M.P., et al. European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Claus C.M., et al. Prospective, randomized, and controlled study of mesh displacement after laparoscopic inguinal repair: fixation versus no fixation of mesh. Surg. Endosc. Mar 2013;30(3):1134–1140. doi: 10.1007/s00464-015-4314-7. [DOI] [PubMed] [Google Scholar]
- 11.Abbas A.E., et al. Patient-perspective quality of life after laparoscopic and open hernia repair: a controlled randomized trial. Surg. Endosc. 2012;26(9):2465–2470. doi: 10.1007/s00464-012-2212-9. [DOI] [PubMed] [Google Scholar]
- 12.Mc Cormac K., et al. Transabdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia. 2005;9(2):109–114. doi: 10.1007/s10029-004-0309-3. [DOI] [PubMed] [Google Scholar]
- 13.Pedroso L.M., et al. Comparative study of postoperative pain between the Lichtenstein and laparoscopy surgical techniques for the treatment of unilateral primary inguinal hernia. Arq. Bras. Cir. Dig. Jul-Sep 2017;30(3):173–176. doi: 10.1590/0102-6720201700030003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahon D., et al. Prospective randomized trial of laparoscopic (transabdominal preperitoneal) vs open (mesh) repair for bilateral and recurrent inguinal hernia. Surg. Endosc. 2003;17:1386–1390. doi: 10.1007/s00464-002-9223-x. [DOI] [PubMed] [Google Scholar]
- 15.HerniaSurge Group Internationl guidelines for groin hernia management. Hernia. 2018;22:1–165. doi: 10.1007/s10029-017-1668-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lovisetto F., et al. Laparoscopic transabdominal preperitoneal (TAPP) hernia repair: surgical phases and complications. Surg. Endosc. 2007;21:646–652. doi: 10.1007/s00464-006-9031-9. [DOI] [PubMed] [Google Scholar]
- 17.Bringman S., et al. Intestinal obstruction after inguinal and femoral hernia repair: a study of 33,275 operations during 1992-2000 in Sweden. Hernia. 2005;9:178–183. doi: 10.1007/s10029-004-0305-7. [DOI] [PubMed] [Google Scholar]
- 18.Sartori A., et al. Rare intraoperative and postoperative complications after transabdominal laparoscopic hernia repair: results from the Multicenter Wall Hernia Group Registry. J. Laparoendosc. Adv. Surg. Tech. A. 2021;31:290–295. doi: 10.1089/lap.2020.0459. [DOI] [PubMed] [Google Scholar]
- 19.Kapiris S.A., et al. Laparoscopic transabdominal preperitoneal (TAPP) hernia repair. A 7-year two-center experience in 3017 patients. Surg. Endosc. 2001;15:972–975. doi: 10.1007/s004640080090. [DOI] [PubMed] [Google Scholar]
- 20.Moldovanu R., et al. Laparoscopic transabdominal pre-peritoneal (TAPP) procedure – step – by – step tips and tricks. Chirurgia (Bucur) 2014;109:407–415. [PubMed] [Google Scholar]