Abstract
Introduction and importance
Cholecystectomy is the most common general surgery procedure, necessitating thorough knowledge of bile duct anatomy. Despite the bile duct's anatomical diversity, reports of double cystic ducts are rare. This case presentation aims to emphasize the importance of recognizing this unusual anatomical variant during surgical procedures to prevent complications and ensure patient safety.
Case presentation
This is a 22-year-old woman with a history of lupus. Initial clinical and ultrasound evaluations concluded she had cholangitis, choledocholithiasis, and cholecystitis.
A cholecystectomy was performed, during which a double cystic duct was identified and confirmed with intraoperative cholangiography.
Five days after surgery, the patient exhibited increased bilirubin levels, and a follow-up cholangiography showed dilation of the common bile duct with no passage of contrast medium into the duodenum. She underwent ERCP with endoprosthesis placement and is currently under follow-up with adequate progress.
Clinical discussion
Double cystic ducts are extremely rare anatomical variants. These variations pose significant challenges for surgeons during surgery, emphasizing the need for a universal culture of safety during cholecystectomy.
Although this anatomical variant is rare, surgeons must be aware of it. Given the uncertainty of anatomy, it is advisable to perform intraoperative imaging, such as cholangiography, before sectioning any duct.
Conclusion
Double cystic duct variations are rare, but when bile duct anatomy is unclear, intraoperative cholangiography is essential. This technique improves visualization of biliary structures, aiding informed decisions before duct ligation and reducing the risk of bile duct disruption.
Keywords: Double cystic, Choledocholithiasis, Cholecystitis, Bile duct, Cholecystectomy, Case report
Highlights
-
•
Cholecystectomy is the most common general surgery procedure
-
•
The bile duct is one of the most anatomically diverse structures
-
•
Anatomical variations of double cystic ducts are extremely rare
1. Introduction
Anatomical variations of the extrahepatic bile duct are common, but double cystic ducts are extremely rare [1]. In 1998, Takahisa et al. reported the case of a 78-year-old woman with a double cystic duct. At that time, fewer than 10 cases had been reported worldwide [2]. Only 22 cases have been reported in the literature, the last one in 2022 [3]. Women have 75 % of the cases [4]. The importance of understanding anatomical variants, such as the double cystic duct, lies in their role in preventing complications like disruption of the biliary tract, as these variants increase the risk of biliary duct injury [5]. In this article, we present the case of a young female patient who was admitted with cholangitis and acute cholecystitis. During the transsurgical procedure, the presence of a double cystic duct was detected, which was ligated, and the bile duct was explored, leaving a T-drain. She was referred for endoscopic retrograde cholangiopancreatography (ERCP). This work has been reported according to SCARE criteria [6].
2. Case presentation
2.1. Patient information
A 22-year-old woman with a history of systemic lupus sought medical attention due to a 3-day clinical picture.
2.2. Clinical findings
She first presented with pain in the right upper quadrant, accompanied by nausea and vomiting on three occasions, made up of gastro-biliary content. She presented with a fever of 38.5 degrees, acholia, choluria, and generalized jaundice. Despite self-medicating with paracetamol, she did not improve, so she came to the emergency room.
There the patient was found to have generalized jaundice, a yellowish sclera, dehydrated oral mucosa, a fever of 38.1 degrees, tachycardia, and pain in the right upper quadrant, with a Murphy sign but no signs of peritoneal irritation. Given these clinical manifestations that suggested cholecystitis and cholangitis.
2.3. Lab tests and imaging
She underwent ultrasound of the liver and bile ducts, which revealed dilation of the intrahepatic bile duct of up to 6 mm. There was choledochus of 18 mm, with evidence of echogenicity 18 × 8 mm in the middle third in the interior, which cast an acoustic shadow. The gallbladder measured 13 × 7.4 mm and had multiple stones inside, as well as free perivesicular fluid. The laboratory results were as follows: total bilirubin 8.35 mg/dl, direct bilirubin 6.41 mg/dl, indirect bilirubin 1.94 mg/dl, aspartate transaminase 48 U/l, alanine transaminase 37 U/l, gamma-glutamyl transpeptidase 226 U/l, albumin 1.90 g/dl, hemoglobin 8.3 g/dl, hematocrit 26.5 %, leukocytes 47.46 × 103/μl, neutrophils 92 %, prothrombin time 17.5 s, time to peak 61.6 s, and international normalized ratio 1.65.
2.4. Treatment and surgical intervention
Treatment included broad-spectrum antimicrobial therapy, fluid resuscitation, stabilization, maintenance in reserve blood products, and fresh-frozen plasma preparation for surgical procedures were performed. During the intervention, an open approach was taken through a Kocher-type incision. A gallbladder with a thickened wall and under tension, as well as perivesicular serous fluid and fibrin creams, was evident.
2.5. Intraoperative findings and procedure
We proceed to the dissection of the hepatocystic triangle, where the cystic artery is identified and a double duct is observed that connects the common bile duct with the gallbladder. These ducts and the artery were ligated using 3–0 silk (Fig. 1, Fig. 2, Fig. 3). Then we performed intraoperative cholangiography at the opening of the common bile duct with abundant discharge of purulent fluid, dilation of the intra- and extrahepatic bile duct, and 20 mm of the bile duct (Fig. 4). Next we explored the bile ducts and obtained multiple 2–8-mm stones. Saline washes were performed, and a T-tube was placed, followed by the insertion of a Penrose drain. Finally, the cavity was closed by planes.
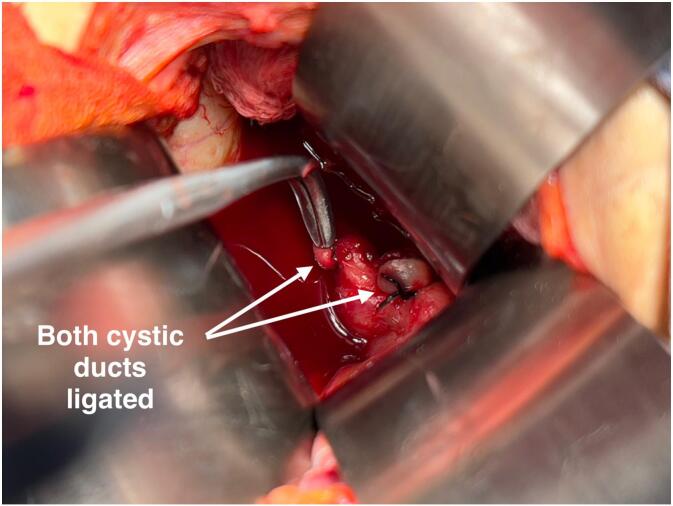
Fig. 1.
Both ligated cysts Both cystic ducts ligated intraoperatively.
Fig. 2.
Gallbladder with a 2nd cyst cannulated with a feeding tube.
Fig. 3.
Postoperative gallbladder with both cysts ligated (2nd cystic cannula with a feeding tube).
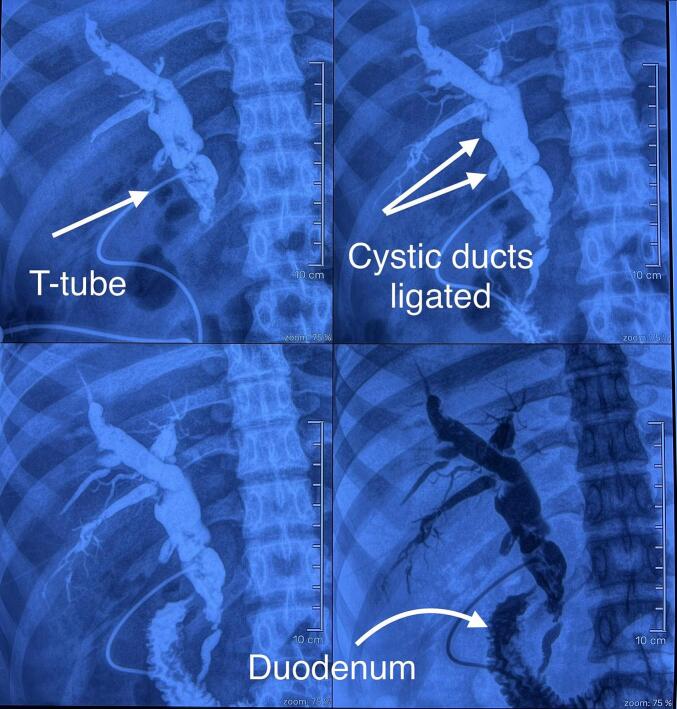
Fig. 4.
Intraoperative cholangiography. Dilation of the intra- and extrahepatic bile duct was observed, with a 20-mm common bile duct and passage of the contrast medium to the duodenum.
2.6. Postoperative outcome and follow-up
After surgery, the patient had an adequate evolution: a decrease in leukocytosis and bilirubin levels, permeable T-drainage, no fever, and tolerated feeding. On the fifth postsurgical day, her bilirubin increased. T-probe control cholangiography revealed dilation of the bile duct with a filling defect at the distal level without passage of the contrast medium to the duodenum (Fig. 5). She was referred for an ERCP with endoprosthesis placement. During the ERCP, a type 1 papilla was observed. During the sphincterotomy, multiple stones measuring 5 mm were identified, and the common bile duct was dilated up to its retropancreatic portion, reaching a diameter of 25 mm. The choledocholithiasis was successfully resolved, and an Amsterdam-type stent was placed. She continued to be followed by outpatient consultations and was also followed up by the rheumatology service for her lupus.
Fig. 5.
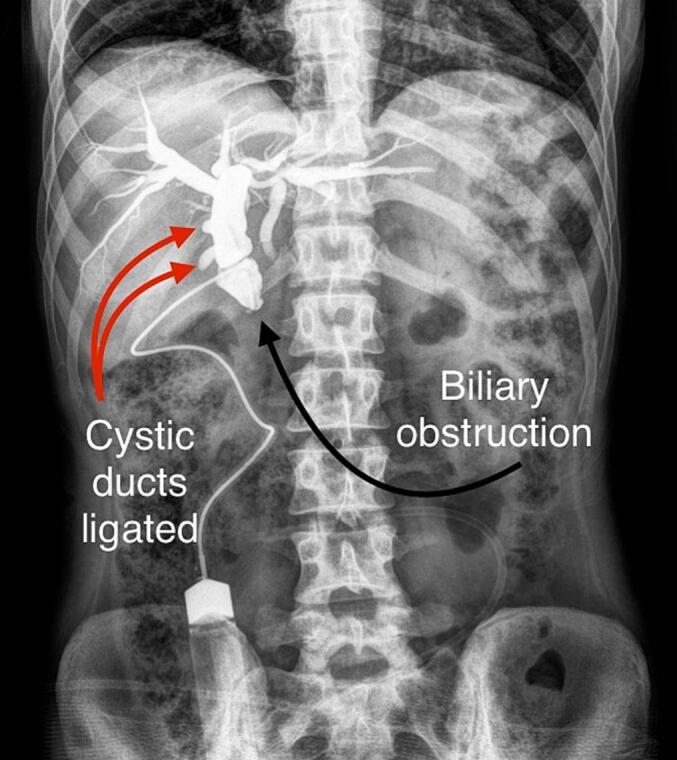
Control cholangiography. The Red arrows: Both cysts ducts ligated. Note that the contrast medium did not pass to the duodenum. The patient was sent for ERCP. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
Anatomical variants of the bile duct are common, with a reported prevalence of between 52.9 % and 58 % in the general population, underscoring its clinical relevance [1]. However, even more remarkable is the rarity of double cystic duct variants. According to a review of the literature, only 22 cases have been reported, as detailed in Table 1. It is reported more frequently in the female population, with an incidence of 78 % [4,7]. The age of presentation in 65 % of the patients is older than 50 years, And it has never been reported in anyone under 30 years old. In our case, the patient was a 22-year-old woman. Flannery and Caster classified the cystic doubles into three groups according to the configuration of the ducts, type Y, H and trabecular, type H being the most common, where the ducts drain separately to the right, left, or common liver [8]. Much like our case, however, a new case has recently been reported where a new configuration called inverse Y is described: a cystic duct of a single gallbladder diverges to form two cystic ducts that drain into the CBD separately [9].
Table 1.
Literature review of reported cases of double cysts [4].
| Case | Author | Age/gender | Country | Duplication type | Preoperative CPRE | Diagnosis | Operative approach | IOC |
|---|---|---|---|---|---|---|---|---|
| 1 | Perelman 1961 | 56/Female | USA | “H” type | No | Intraoperative | Not reported | Not reported |
| 2 | Senapati and Wolf 1984 | 56/Male | UK | Trabecular type | No | Intraoperative | Open | Yes |
| 3 | 55/Female | “H” type | No | Intraoperative | Open | Yes | ||
| 4 | Nakasugi et al. 1995 | 50/Female | Japan | “Y” type | Yes | Preoperative ERCP | Laparoscopic | Yes |
| 5 | Ng et al. 1996 | 60/Male | Hong Kong | “H” type | Yes | Intraoperative | Laparoscopic converted to open | No |
| 6 | Momiyama et al. 1996 | 66/Female | Japan | “H” type | Yes | Postoperative | Laparoscopic | Yes |
| 7 | Hirono et al. 1997 | 74/Female | Japan | “H” type | Yes | Intraoperative | Laparoscopic | Yes |
| 8 | Fujikawa et al. 1998 | 70/Female | Japan | “H” type | Yes | Intraoperative | Open | Yes |
| 9 | Lobo et al. 2000 | 49/Female | Brazil | “Y” type | No | Intraoperative | Laparoscopic | Yes |
| 10 | Tsutsumi et al. 2000 | 74/Female | Japan | “H” type | Yes | Preoperative ERCP | Laparoscopic | Yes |
| 11 | Shivhare et al. 2002 | 46/Female | India | “H” type | No | Intraoperative | Laparoscopic converted to open | Yes |
| 12 | Huston et al. 2008 | 43/Female | USA | “H” type | No | Intraoperative | Laparoscopic | Yes |
| 13 | Aristotle et al. 2011 | 50/Male | India | “Y” type | NA | Postmortem | NA | NA |
| 14 | Shih et al. 2011 | 37/Male | Taiwan | “Y” type | No | Intraoperative | Laparoscopic | No |
| 15 | Shabanali et al. 2014 | 50/Female | Iran | “H” type | No | Intraoperative | Laparoscopic | No |
| 16 | Otaibi et al. 2015 | 54/Male | USA | “H” type | No | Intraoperative | Laparoscopic | Yes |
| 17 | Samnani et al. 2015 | 34/Female | Pakistan | “Y” type | No | Intraoperative | Laparoscopic | No |
| 18 | Fujii et al. 2017 | 57/Female | Japan | Trabecular type | Yes | Preoperative ERCP | Laparoscopic | Yes |
| 19 | Salih et al. 2017 | 33/Female | Iraq | “Y” type | No | Intraoperative | Laparoscopic | No |
| 20 | Semere et al. 2019 | 34/Female | USA | Trabecular type | No | Intraoperative | Laparoscopic converted to open | Yes |
| 21 | Suhyun Lim et al. [9] | 82/Female | Japan | “H” type | No | Intraoperative | Laparoscopic | Yes |
| 22 | Zhi Liang et al. 2022 [3] | 66/Female | China | “Reverse Y" | Yes | Intraoperative | Laparoscopic | Yes |
| 23 | Carlos J. 2024 Present Case | 22/ Female | México | “H” type | No | Intraoperative | Open | Yes |
Abbreviations: ERCP, endoscopic retrograde cholangiopancreatography.
IOC, intraoperative cholangiogram.
These variations are a significant challenge for surgeons during surgical intervention since 86 % of patients are diagnosed intraoperatively, making it harder to dissect the hepatocystic triangle, thus highlighting the importance of maintaining a universal culture of safety during cholecystectomy [10]. In this way, the likelihood of intraoperative complications, such as disruption of the biliary tract, can be reduced, which undoubtedly contributes to a high rate of postoperative morbidity and mortality.
Although a tomographic study or magnetic resonance cholangiography would have been of great utility before the cholecystectomy [11]. They were not available in our unit during the intervention due to technical failures that were beyond our control.
As we have mentioned, it is rare to find this anatomical variant, but surgeons must keep it in mind, and given the uncertainty of the anatomy, before sectioning a canal, it is worth doing intraoperative imaging such as cholangiography, which is helpful and is used in 75 % of reported cases [12].
4. Conclusions
Although cystic duct variations are extremely rare, when the anatomical configuration of the bile duct is in doubt, it is valuable to resort to tools such as intraoperative cholangiography. This technique allows the biliary anatomy to be visualized more clearly and to make informed decisions before proceeding with the ligation of the ducts, avoiding any disruption of the bile duct.
Consent
Informed consent was taken from the patient for the publication of this report.
Ethical approval
Ethical review and approval were not required for the study the case report participants in accordance with the local legislation and institutional requirements.
The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
REGISTRATION WITH THE NATIONAL BIOETHICS COMMISSION.
CNBCEI-11-CEI004-20170731
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Author contribution
Substantial contributions to concept or design: Salvador Carlos Jiménez
Acquisition, analysis, or interpretation of data: Salvador Carlos Jiménez
Drafting of the manuscript:
Salvador Carlos Jiménez
Miriam Natividad Jiménez Velázquez
Juan Carlos Rivera Nava
Raúl Alejandro Núñez Torres
Edgard Efrén Lozada Hernández
Jose Alaniz Ruiz
Critical review of the manuscript for important intellectual content
Salvador Carlos Jiménez
Supervised the work
Edgard Efrén Lozada Hernández
Guarantor
Salvador Carlos Jiménez
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.Chaib E., Kanas A.F., Galvão F.H.F., D'Albuquerque L.A.C. Bile duct confluence: anatomic variations and its classification. Surg. Radiol. Anat. 2014 Mar 2;36(2):105–109. doi: 10.1007/s00276-013-1157-6. Available from. [DOI] [PubMed] [Google Scholar]
- 2.Fujikawa T., Takeda H., Matsusue S., Nakamura Y., Nishimura S. Anomalous duplicated cystic duct as a surgical hazard: report of a case. Surg. Today. 1998;28(3):313–315. doi: 10.1007/s005950050129. Available from: [DOI] [PubMed] [Google Scholar]
- 3.Liang Z., Chen J., Liang Y., Wang J., Song X. Double cystic duct: preoperative use of MRCP without being aware of the anatomic anomaly: a case report. Front. Surg. 2022;9 doi: 10.3389/fsurg.2022.892927. (Available from: /pmc/articles/PMC9271822/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munie S., Nasser H., Go P.H., Rosso K., Woodward A. Case report of a duplicated cystic duct: a unique challenge for the laparoscopic surgeon. Int. J. Surg. Case Rep. 2019;56:78. doi: 10.1016/j.ijscr.2019.02.030. (Available from: /pmc/articles/PMC6407078/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suhocki P.V., Meyers W.C. Injury to aberrant bile ducts during cholecystectomy: a common cause of diagnostic error and treatment delay. AJR Am. J. Roentgenol. 1999;172(4):955–959. doi: 10.2214/ajr.172.4.10587128. (Available from: https://pubmed.ncbi.nlm.nih.gov/10587128/) [DOI] [PubMed] [Google Scholar]
- 6.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. (Available from: https://pubmed.ncbi.nlm.nih.gov/37013953/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salih A.M., Kakamad F.H., Mohammed S.H., Salih R.Q., Habibullah I.J., Muhialdeen A.S., et al. Double cystic duct, a review of literature with report of a new case. Int. J. Surg. Case Rep. 2017;38:146. doi: 10.1016/j.ijscr.2017.07.027. (Available from: /pmc/articles/PMC5537449/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caster M.P.F.M. Anomalías congénitas de la vesícula biliar; 101 casos. Surg. Gynecol. Obstet. 1956;103:439–457. [PubMed] [Google Scholar]
- 9.Lim S., Kim C.H., Paik K.Y., Kim W. Double cystic duct without being aware of the anatomic anomaly during laparoscopic cholecystectomy: the first case of reverse Y type anomaly. Hepatobiliary Pancreat. Dis. Int. 2021;20(2):201–202. doi: 10.1016/j.hbpd.2020.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Gupta V., Jain G. Safe laparoscopic cholecystectomy: adoption of universal culture of safety in cholecystectomy. World J Gastrointest Surg. 2019 Feb 2;11(2):62. doi: 10.4240/wjgs.v11.i2.62. (Available from: /pmc/articles/PMC6397793/) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirao K., Miyazaki A., Fujimoto T., Isomoto I., Hayashi K. Evaluation of aberrant bile ducts before laparoscopic cholecystectomy: helical CT cholangiography versus MR cholangiography. Am. J. Roentgenol. 2000;175(3):713–720. doi: 10.2214/ajr.175.3.1750713. Available from: [DOI] [PubMed] [Google Scholar]
- 12.Michael Brunt L., Deziel D.J., Telem D.A., Strasberg S.M., Aggarwal R., Asbun H., et al. Safe cholecystectomy multi-society practice guideline and state-of-the-art consensus conference on prevention of bile duct injury during cholecystectomy. Surg. Endosc. 2020;34(7):2827–2855. doi: 10.1007/s00464-020-07568-7. Available from: [DOI] [PubMed] [Google Scholar]