Abstract
The purpose of this manuscript is to describe the clinical course of a 66-year-old patient with chronic kidney disease due to focal segmental glomerulosclerosis in whom an access arteriovenous fistula was created in the anatomical snuffbox. At discharge, the fistula thrill was normal. Two months later, a duplex examination revealed previously unrecognized obstruction of the mid-forearm segment of the cephalic vein; flow was maintained by a perforator into the deep venous system, which returned blood to the upper arm cephalic vein above the occlusion. A second, subsequent radiocephalic anastomosis was performed in the wrist to augment flow. The fistula was successfully cannulated after 12 weeks of maturation.
Keywords: Arteriovenous fistula, Deep vein system, Fistula maturation, Hemodialysis, Perforating vein
A crucial aspect in maintaining hemodialysis (HD) therapy is an optimal vascular access in patients with end-stage renal disease. The radiocephalic arteriovenous fistula (RCAVF) in the wrist stands out as preferred vascular access for HD, due to its low risk of infection and dysfunction. Unfortunately, RCAVF has two major disadvantages: a high early failure rate, ranging between different groups from 5% to 46%, and a high maturation failure rate.1 In Jemcov’s prospective study, female sex, older patient age, and poor upper extremity vessels were considered as major risk factors of maturation failure.2 We report the case of a patient with a snuffbox fistula (SBAVF), with late maturation, associated with a mid-cephalic vein (CV) occlusion and maintained fistula flow, through a dilated distal perforating vein (DPV) and deep vein system (DVS). Subsequently, more proximally located anastomosis, in the wrist, was necessary to obtain maturation. To our knowledge, this is the first case demonstrating that DPV and DVS may play a pivotal role in maintaining patency and effective maturation of distal AVF.
Case description
A 66-year-old patient with chronic kidney disease, due to focal segmental glomerulosclerosis and hypertension, was referred to our clinic to prepare for renal replacement therapy. He had an AVF created in the right anatomical snuffbox. At discharge, one day after surgery, the fistula thrill was normal. His duplex examination 2 months later, performed as a routine follow-up, revealed a previously unrecognized obstruction of the mid-forearm segment of the CV and a flow diversion, through a dilated DPV (≥2 mm) to radial artery comitans vein, and back to the upper part of the forearm and CV in the antecubital fossa (AF) (Fig 1). His fistula blood flow was 385 ml/min, and the diameter of CV in AF was 5 mm. This low flow was the main reason for making a second subsequent anastomosis in the wrist, between the radial artery (RA) and the CV, to increase vessel diameters and blood flow. Two weeks later, his brachial artery (BA) blood flow was 1061 ml/min, and the CV diameter in the AF was 8 mm. The RA and BA diameters were 5.3 mm and 6.4 mm, respectively. The first cannulation in the antecubital fossa was performed 12 weeks after the second surgery (Fig 2). We plan to use a second needle to cannulate CV in the arm in the future. There is also a small segment of CV in the upper part of the forearm that is suitable for cannulation.
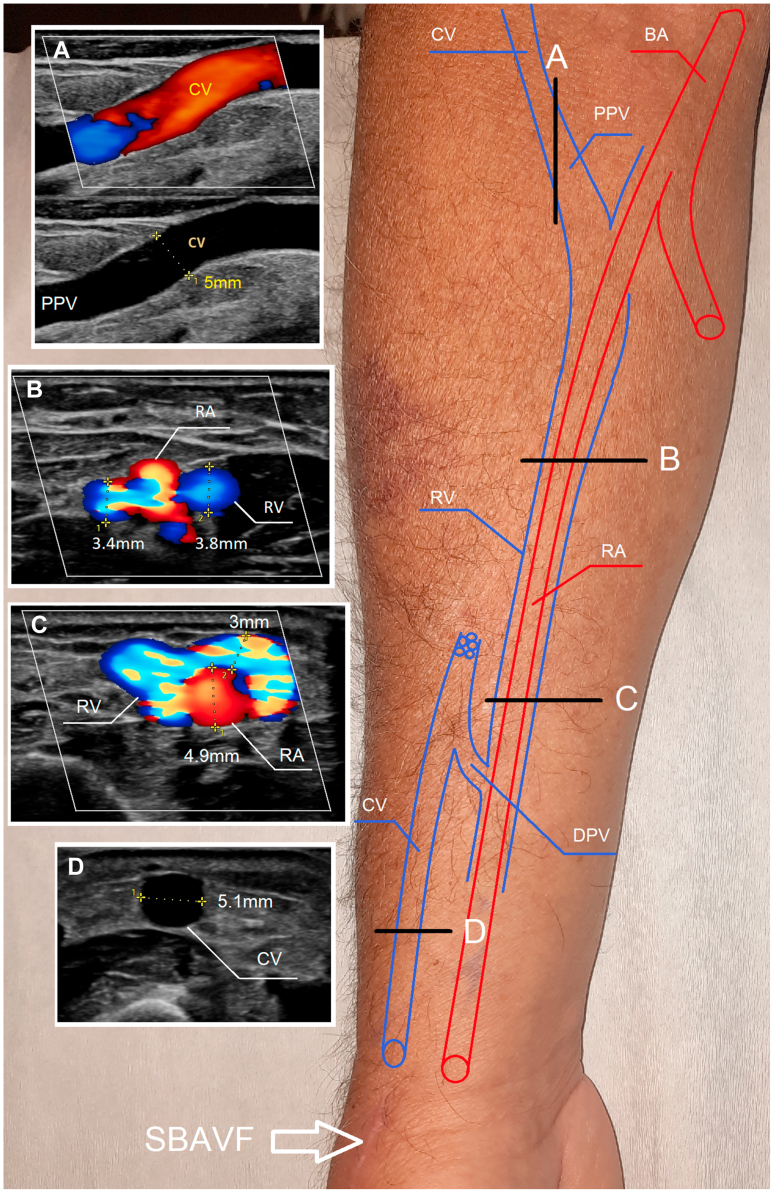
Fig 1.
Doppler ultrasound examination. After snuffbox fistula (SBAVF), the blood in the middle one-third of the forearm flows into the deep vein system, and in the area of the antecubital fossa (AF), it returns through the proximal perforating vein (PPV) back to the superficial system (ie, cephalic vein [CV] on the arm. A, Doppler ultrasound longitudinal view through the CV. B, Ultrasound transverse view through the radial artery (RA) and radial vein (RV). C, Doppler ultrasound transverse view through the RA and RV. D, Doppler ultrasound transverse view through CV in the arm. BA, Brachial artery; DPV, distal perforating vein.
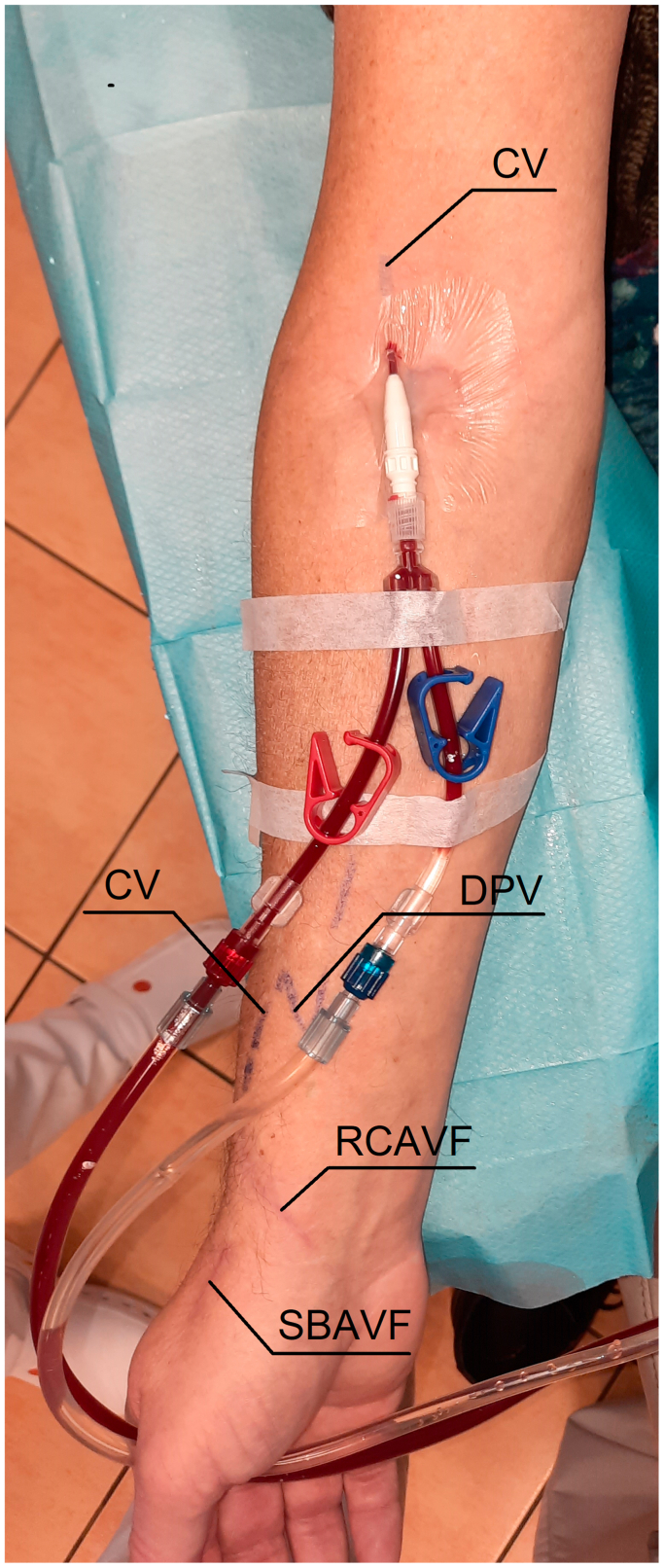
Fig 2.
Hemodialysis (HD) using maturated fistula. CV, Cephalic vein; DPV, distal perforating vein; RCAVF, radiocephalic arteriovenous fistula; SBAVF, snuff-box fistula.
Discussion
Despite advances in surgical techniques and perioperative care, fistula maturation remains a challenging part of hemodialysis access. This was shown by Bylsma et al, who conducted a meta-analysis that raised doubt on the AVF’s utility in addressing end-stage renal disease.3 They evaluated the outcomes of more than 60,000 AVF access formations and found 1-year primary, primary assisted, and secondary patency rates of 64%, 73%, and 79%, respectively. However, only 26% of created fistulas were reported as mature at 6 months, and 21% of fistulas were abandoned without use.
Clinical fistula maturation is the result of a crucial process in establishing functional vascular access for patients undergoing HD. It refers to the formation of a mature, useable AVF supplying the necessary blood volume for efficient dialysis. Data from a prospective cohort study by Robbin et al, based on 602 patients who received a new single-stage AVF, demonstrated that unassisted maturation can be predicted by three ultrasound parameters: fistula blood flow, diameter, and depth.4 Performing such assessment 6 weeks after surgery provides valuable guidance regarding early intervention to facilitate maturation (eg, percutaneous angioplasty or early planning of a second anastomosis), which may increase utilization of the fistula.
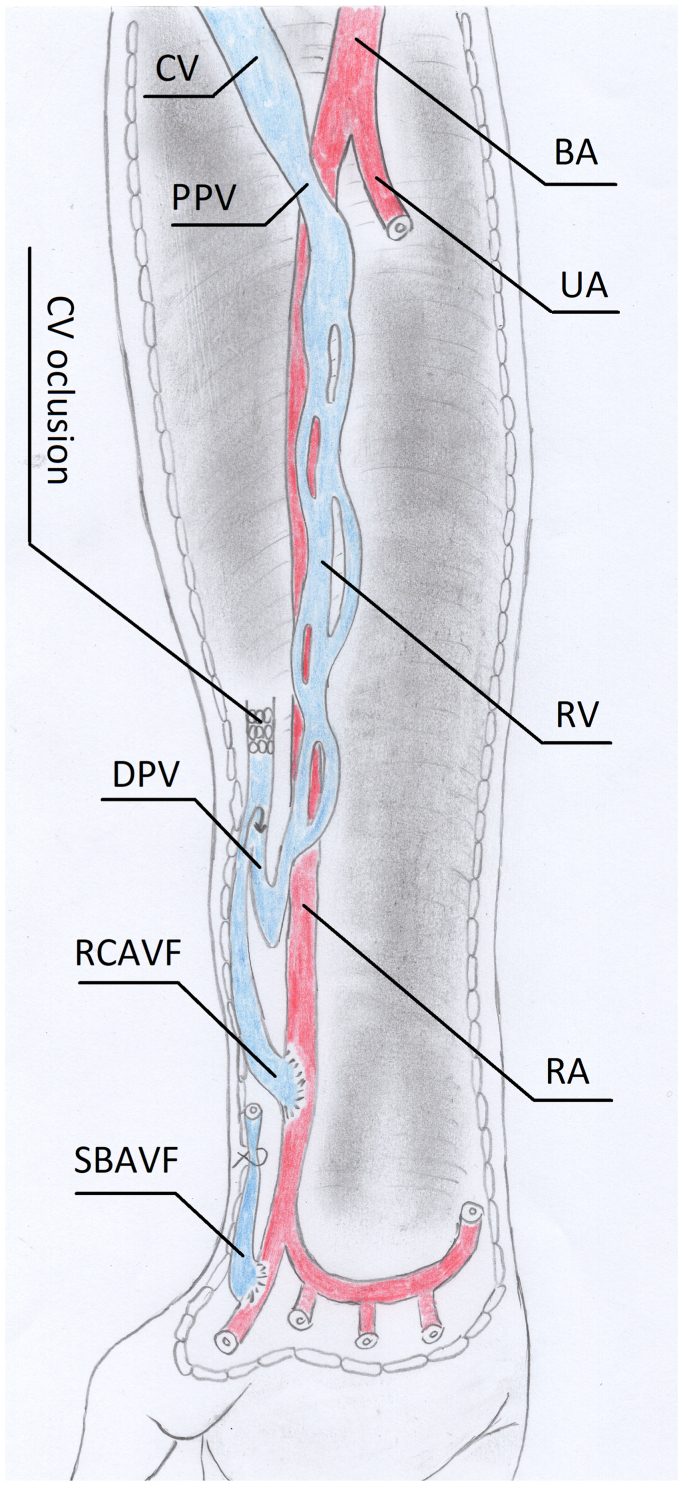
We describe the case of a patient whose primary fistula (SBAVF) did not fulfil all criteria of maturation 8 weeks after its creation, due to unrecognized CV occlusion. The previously created AVF was probably responsible for the dilatation of DPV and DVS, which maintained patency to the AF proximal perforating vein, and the upper arm superficial CV (Fig 3). To improve the flow and diameter of the CV in the upper arm, a new anastomosis between the RA and the CV was created in the wrist as renal failure progressed. Despite the occlusion of the superficial vein system, this approach was effective, and the first dialysis was performed 3 months later. This allowed us to avoid potential consequences associated with a proximal fistula, such as high-output heart failure and hand ischemia.
Fig 3.
Illustration of vascular anatomy following radiocephalic arteriovenous fistula (RCAVF) creation. BA, Brachial artery; CV, cephalic vein; DPV, distal perforating vein; PPV, proximal perforating vein; RA, radial artery; RV, radial vein; SBAVF, snuff-box fistula; UA, ulnar artery.
A few approaches are utilized to improve AVF maturation. Endovascular or open repair may be performed, depending on the underlying cause; however, no substantial differences have been observed between the two methods in general.5 Reanastomosis is a widely acknowledged and efficacious technique utilized to accelerate the process of maturation.6 Despite the patient’s unique fistula outflow circuit anatomy following SBAVF surgery, this technique proved to be highly successful.
Conclusion
Even in patients with extensive superficial vein damage, reanastomosis of fistulas may be an effective method for accelerating fistula maturation and preventing “high” fistulas involving the brachial artery or catheter implantation.
Funding
The study was supported by the Wroclaw Medical University statutory funds (SUBZ.C160.24.090). It was investigator-initiated research. The funding body had no role in the study design, data collection, analyses, and interpretation, or in writing the manuscript.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
The patient provided written consent to publish their case details and images.
References
- 1.Schmidli J., Widmer M.K., Basile C., et al. Editor's Choice - vascular access: 2018 clinical Practice Guidelines of the European Society for vascular surgery (ESVS) Eur J Vasc Endovasc Surg. 2018;55:757–818. doi: 10.1016/j.ejvs.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Jemcov T.K. Morphologic and functional vessels characteristics assessed by ultrasonography for prediction of radiocephalic fistula maturation. J Vasc Access. 2013;14:356–363. doi: 10.5301/jva.5000163. [DOI] [PubMed] [Google Scholar]
- 3.Bylsma L.C., Gage S.M., Reichert H., Dahl S.L.M., Lawson J.H. Arteriovenous Fistulae for Haemodialysis: a Systematic Review and meta-analysis of efficacy and Safety outcomes. Eur J Vasc Endovasc Surg. 2017;54:513–522. doi: 10.1016/j.ejvs.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 4.Robbin M.L., Greene T., Allon M., et al. Prediction of arteriovenous fistula clinical maturation from Postoperative ultrasound Measurements: Findings from the hemodialysis fistula maturation study. J Am Soc Nephrol. 2018;29:2735–2744. doi: 10.1681/ASN.2017111225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McLafferty R., Pryor R.W., Johnson C.M., Ramsey D.E., Hodgson K.J. Outcome of a comprehensive follow-up program to enhance maturation of autogenous arteriovenous hemodialysis access. J Vasc Surg. 2007;45:981–985. doi: 10.1016/j.jvs.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 6.Nassar G.M. Endovascular management of the "failing to mature" arteriovenous fistula. Tech Vasc Interv Radiol. 2008;11:175–180. doi: 10.1053/j.tvir.2008.09.004. [DOI] [PubMed] [Google Scholar]