Abstract
Context: Adolescents and young adults (AYA) with spina bifida (SB) are more susceptible to obesity due to impaired mobility. There is limited access to physical activity for this population.
Objective: The primary aim of this study was to evaluate the feasibility of a mobile health app in a weight management program for AYA with SB. This was determined by measuring program adherence, active use of the app (defined as ≥3 uses per week), and user rating of the Pt Pal™ mobile app. Secondary outcomes were changes in BMI, quality of life, and health behavior, and the number of active participants over time.
Methods: Patients from the SB Clinic of a large metropolitan hospital between the ages of 11–21 years and overweight were invited to participate. The program consisted of group nutrition sessions and an individualized exercise plan using a mobile app with coaching. Outcome measures were program adherence, changes in BMI, and validated survey responses. Descriptive statistical analysis was performed.
Results: Fifteen participants enrolled, and ten participants completed the program. Five of the ten participants attended the nutrition sessions. The number of active app users declined after the first week. Seventy percent of participants decreased their BMI. Most participants reported the program improved their ability to exercise regularly, eat a healthier diet and feel more self-confident. Peds QL™ psychosocial health domains increased postintervention. The YRBS showed increased physical activity and less sedentary time postintervention.
Conclusions: This mobile app-based weight management program with coaching implemented may not be feasible for adoption in the general population of AYA with SB; however, it was well received by some, and further testing is needed to determine how to improve feasibility. This study provides useful information to guide future programs utilizing digital health and coaching.
Keywords: Spina bifida, Mobile health app, Weight management, Obesity prevention
Introduction
Spina Bifida (SB) is one of the most common central nervous system birth defects, occurring in 1.9 per 10,000 live births (1, 2, 3). Spina Bifida is a neural tube defect resulting in muscle weakness and paralysis based on the size and location of the lesion (4, 5). Associated impairments include weakness and decreased sensation in the lower extremities (6). Consequently, youth with SB are more susceptible to obesity. The prevalence of obesity is 34–64% in AYA with SB (7). Most children with SB survive well into adulthood; however, aging increases the likelihood of becoming obese (8).
SB is the result of multiple nutritional, environmental, and genetic factors (5). There are certain ethnic groups that are more susceptible (9). Hispanic mothers are most vulnerable compared to non-Hispanic white mothers9 based on recent studies (10). In addition, there is a greater prevalence of obesity among Hispanic children with SB when compared with their non-Hispanic counterparts (7, 11, 12).
Obesity is a significant comorbidity in those with SB given their baseline mobility limitations. Additional bodyweight perpetuates the cycle of sedentary behavior with increased caloric intake, leading to further decline in ambulation (13). Furthermore, obesity increases the risks of pressure ulcers and loss of independence impacting quality of life (14). Thus, it is imperative that patients with SB have access to opportunities to be active. One challenge to pediatric weight management programs is attrition related to the burden of visits, with one study reporting parents expressing frustration with the lack of flexibility (15, 16). Mobile health (mHealth) app-based platforms allow for flexibility and greater autonomy (17). Recent research demonstrates that youth with SB were physically and cognitively capable of using commercially available mobile apps; however, adaptation of existing technologies for persons with SB is recommended (18).
The primary aim of this study was to evaluate the feasibility of using the Pt Pal™ mobile health app in a weight management program for AYA with SB. Feasibility was assessed by measuring program adherence (participation and completion), active use of the app (defined as ≥3 uses per week), and user ratings of the Pt Pal app. The secondary outcome measures were changes in BMI pre- to postintervention, quality of life through the validated Pediatric Quality of Life (PedsQL™) survey, and health behavior based on a modified Youth Risk Behavioral Surveillance (YRBS) survey. We hypothesized that the intervention would support participants in decreasing BMI, improve quality of life and increase health-promoting behaviors.
Methods
Participants
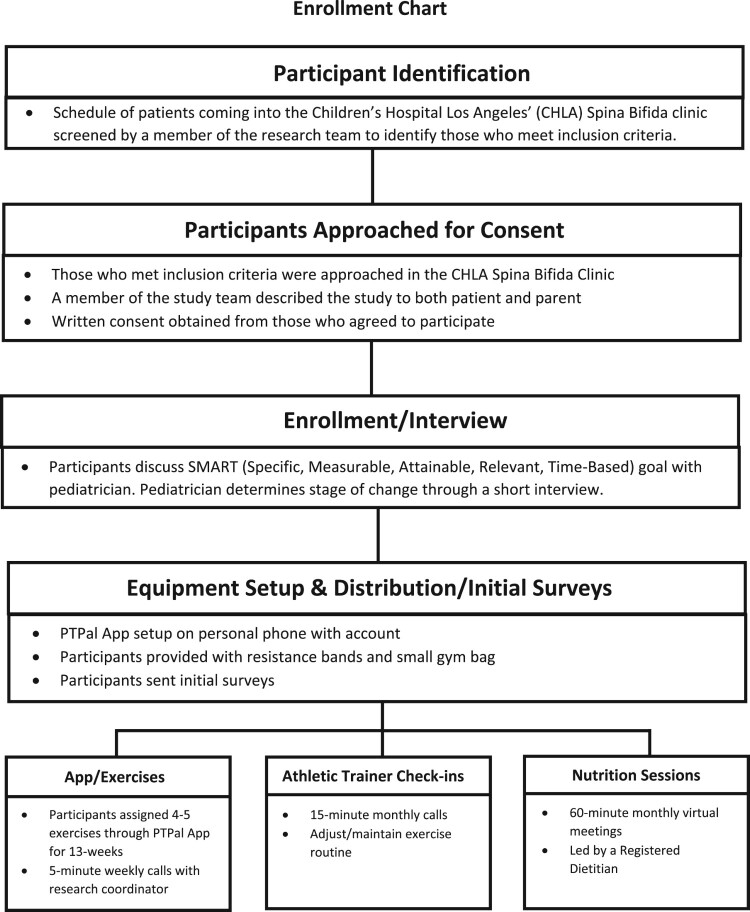
Institutional Review Board approval was obtained for this study. Inclusion criteria were patients between the ages of 11–21 years who had a body mass index (BMI) ≥ 85th percentile who were followed by the Centers for Disease Control and Prevention (CDC) National Spina Bifida Patient Registry (NSBPR) Spina Bifida Program at a large metropolitan hospital. Participants were English or Spanish speaking, with any level of mobility, and had access to a mobile device with smartphone capabilities. Electronic Medical Records (EMRs) were reviewed by the research team prior to the SB clinic to identify patients who met age and BMI criteria. Patients who met the inclusion criteria were approached by the research staff and invited to participate. Written consent and assent were obtained from those who agreed to participate (Fig. 1). Patients with a diagnosis of moderate to severe developmental delay, who underwent a recent surgical procedure or who were being actively treated by the wound care management team for a pressure ulcer, and those who were already enrolled in a weight management program were excluded.
Figure 1.
Recruitment and enrollment procedures
Intervention
Study design
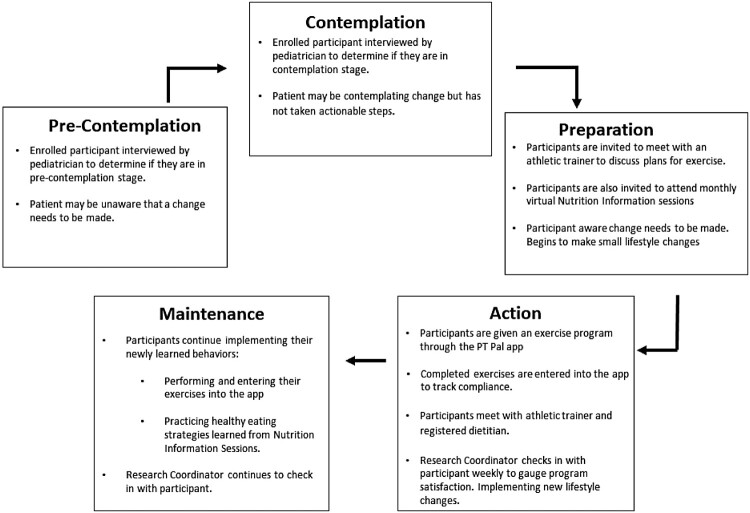
The Transtheoretical Model (TTM) was the conceptual framework that guided program design (Fig. 2). TTM is used to assess readiness for change and consists of 5 phases: (1) pre-contemplation, (2) contemplation, (3) preparation, (4) active change, and (5) maintenance. Pre-contemplation refers to a state where a person has no intention to change and may be unaware of the problem. Moving to the contemplation stage requires acknowledgement that a problem exists, and that change is needed. Preparation involves deliberate intention and small implemented changes; action is applying changed behavior over time, and maintenance is established as a person works to prevent a lapse. As a person continues to adjust their behavior, they move from pre-contemplation to maintenance (19).
Figure 2.
Transtheoretical model (TTM) of health behavior change conceptual framework
The goal of this study was to engage with patients who are in the pre-contemplation and contemplation stages of change and lead them through the cycle of behavioral change. Nutrition and exercise modules were developed with the intention of informing and propelling subjects through these stages.
Enrollment visit
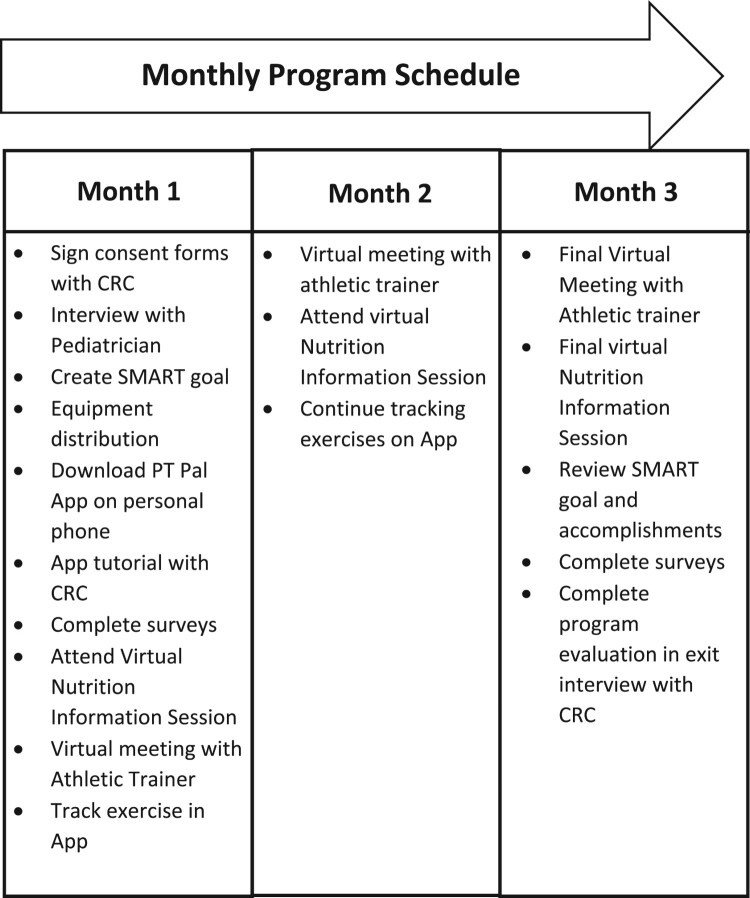
The SB pediatrician conducted a motivational interview to evaluate their stage of change. The pediatrician would assist the participant to create a Specific, Measurable, Achievable, Relevant, and Time Bound (SMART) nutrition and activity goal. The activity goal was discussed with a certified Athletic Trainer, and an individualized exercise program was assigned. Participants were instructed to download the Pt Pal™ app, and instructions were provided. Enrolled participants were provided a packet with resistance bands and health-education handouts. Participants were invited to attend monthly, virtual nutrition education modules and monthly phone follow-ups with the certified athletic trainer (Fig. 3).
Figure 3.
Program outlines
Program components
Pt Pal™ mobile health app
Pt Pal™ (Los Angeles) is an established iOS/Android mobile health application, allowing clients to input data and providers to access the information through the web-based portal. Each participant was assigned a unique, de-identified Pt Pal™ login upon enrollment. Once ambulatory status was determined, the study team assigned an exercise plan to each participant, accessible through the Pt Pal™ app. Each exercise included an instructional video. Pt Pal™ was used to administer all surveys, questionnaires, and handouts throughout the program. Reminders to complete exercises, attend monthly nutrition sessions and schedule monthly athletic trainer meetings were communicated through the app every 2 weeks.
The study team was able track how often each participant logged into the app, how many exercises were performed, and any reported pain or discomfort during any of the assigned exercises. Participants were instructed to do the exercises with a goal of 3 times a week. An active user was defined as an individual who logged exercise into the Pt Pal™ app at least 3 days a week.
Exercise program
An orthopedist and a research coordinator with a physical therapy background developed the exercise modules. A volunteer SB patient and non-affected sibling consented to be recorded for exercise demonstration videos uploaded to the Pt Pal™ exercise library for respective non-ambulatory and ambulatory exercise plans. Each plan consisted of a warmup, stretches, and strengthening exercises. Athletic trainers demonstrated assigned exercises with each participant in person at the time of enrollment with 2 virtual monthly check-in meetings that allowed for modifications and feedback.
Selected exercises for each participant were determined by their International Myelodysplasia Study Group (IMSG) functional spina bifida level and ambulatory status (20). The IMSG functional classification is determined by manual motor testing and classified as thoracic, high lumbar, mid lumbar, low lumbar or sacral. Ambulatory status was defined as being in a standing or seated positioning while performing the exercises. If a participant was able to stand independently with or without braces, they would be considered ambulatory, and those who performed the exercises in their wheelchair were defined as non-ambulatory. The percentage of attempted exercises completed was calculated by tracking the number of attempted exercises and comparing this to the number of exercises that were incomplete due to pain or discomfort.
Nutrition
The nutrition modules were adherent to the current American Academy of Pediatrics obesity guidelines and were developed by a Registered Dietitian (RD) in collaboration with a pediatrician with certification in obesity medicine. Participants were invited to attend a monthly virtual nutrition session on setting nutrition and health goals led by two dietary interns and a senior RD. Each nutrition module was conducted for 45-minutes and covered one of three topics: (1) Introduction/Goals/MyPlate, (2) Nutrition Basics, and (3) Navigating the Grocery Store/Conclusion. These topics were modified from the existing BodyWorks curriculum, a national, empirically validated, Comprehensive Behavioral Family Lifestyle Interventions (CBFLI) program used in our primary care pediatric clinic (Table 1) (21).
Table 1.
Modified bodyworks curriculum.
| Session number | Topic | Related activity |
|---|---|---|
| 1 | Introduction, MyPlate, 5-2-1-0 & SMART Goals | Recipe for a yogurt parfait |
| 2 | Portions & Sugar in Drinks, Food Labels | Recipe for “spa water” – fruit and herb infused water |
| 3 | Grocery Shopping, Fast Food & Family Meal Prep “Instagram” Final | Reading nutrition labels of a favorite food in the house |
Surveys and questionnaires
Each participant was given a 7-question demographic survey upon enrollment. Monolingual Spanish speakers were provided with a Spanish translation and were provided with an interpreter.
Three validated questionnaires were used: (1) Pediatric Quality of Life (PedsQL™) (22), (2) Youth Risk Behavioral Surveillance (YRBS) (23) and (3) the Mobile App Rating Scale (MARS) (24). The PedsQL™ survey is a modular instrument comprised of 23 questions used to measure health-related quality of life in healthy children and adolescents and those with acute and chronic conditions.13 The results of the PedsQL™ are based on 4 scales (Physical, Social, Emotional, and School Functioning) and 3 summary scores (Total Scale Score, Physical Health Summary Score, and Psychosocial Health Summary Score). The PedsQL™ scores are calculated by dividing the total score of each section by the number of questions answered, in which the highest possible score is 100. Higher scores indicate greater levels of functioning. The PedsQL™ has been shown to be a reliable measure of quality of life in children and adolescents. Its validity has been demonstrated in children with and without chronic health conditions (22).
The YRBS survey was designed to monitor health-related behaviors that contribute to the death, disability and social problems among youth and young adults (23). For this study, the YRBS was modified to include 16 physical activity and dietary behavior questions. The modified YRBS has been shown to be effective in determining the prevalence of health-related behaviors that contribute to unhealthy dietary habits and physical activity (23).
The 23-question MARS was used to evaluate the quality of the mobile health app. The MARS score is based on 4 characteristics: engagement, functionality, aesthetics, and information (24). Each domain rating is based on a scale from 1 to 5. Engagement measures the ability of the app to engage the user, increasing the likelihood the user will return to use the app. Functionality focused on overall user experience with the app’s features. Aesthetics revealed the user’s opinion on visual appeal, and information reflects the quality and quantity of the information in the app. MARS has been shown to be a reliable measure of the quality of mobile health apps (24).
A Program Evaluation survey was distributed at the final visit to obtain participant feedback. This 40-question survey gathered information regarding the participants’ satisfaction with each aspect of the program. All surveys were distributed before and after the 3-month intervention as described in Table 2.
Table 2.
Assessment time points and key measures.
| Month 1 | Month 2 | Month 3 | |
|---|---|---|---|
| Demographics | x | ||
| Outcome measures | |||
| Participant’s BMI recorded | x | x | |
| Program Adherence | x | x | x |
| YRBS Questionnaire | x | x | |
| PedsQL Inventory | x | x | |
| MARS | x | ||
| Program Evaluation | x | ||
Statistical analysis
Demographic information, program adherence, MARS survey and program evaluation data were descriptively analyzed. Continuous variables are shown as means with standard deviations and categorical or ordinal variables are shown as proportions with percentages. Wilcoxon sign rank tests were used to evaluate the change in BMI, Peds QL™ scores, and YRBS responses from pre- to postintervention. Spearman rank correlation was used to examine the relationship between change in BMI and app usage.
Results
Demographics
Overall, 15 participants were enrolled in the study, and 10 participants completed the program. Those who did not complete the program were lost to follow-up (n = 2 after week 1) or withdrew (n = 3 at weeks 0, 2, and 6) from the study. The mean age of participants who completed the program was 17.5 (standard deviation (SD) 2.2; range 12–21 years old). There were 6 (60%) females and 4 (40%) males. Nine of fifteen enrolled participants (60%) spoke primarily Spanish at home, 1 identified Arabic as their primary language and the remaining spoke English only. All participants were proficient in English, even if they spoke another language at home. Over half (60%, 6/10) of participants were non-ambulatory as previously defined. Demographics of all participants and IMSG functional levels are presented in Table 3.
Table 3.
Participant demographics.
| Measurement | Description | Count | Percentage | Count | Percentage |
|---|---|---|---|---|---|
| Total (N = 15) | Completed (N = 10) | ||||
| Age | 11–14 years | 1 | 6.67% | 1 | 10.0% |
| 15–18 years | 8 | 53.3% | 5 | 50.0% | |
| 19–21 years | 6 | 40.0% | 4 | 40.0% | |
| Average age | 16.1 years | 17.5 years | |||
| Sex | Female | 8 | 53.3% | 6 | 60.0% |
| Male | 7 | 46.7% | 4 | 40.0% | |
| Race/Ethnicity | Latino/Hispanic | 10 | 66.7% | 7 | 70.0% |
| Non-Latino White | 3 | 20.0% | 2 | 20.0% | |
| Non-Latino Black | 1 | 6.7% | 0 | 0 | |
| Multiple Races | 1 | 6.7% | 1 | 10.0% | |
| Insurance type | Medi-Cal | 13 | 86.7% | 9 | 90.0% |
| Private | 1 | 6.7% | 1 | 10.0% | |
| HMO | 0 | 0 | 0 | 0 | |
| PPO | 0 | 0 | 0 | 0 | |
| None | 0 | 0 | 0 | 0 | |
| Not disclosed | 1 | 6.7% | 0 | 0 | |
| Parent’s highest education level | Less than high school | 4 | 26.7% | 3 | 30.0% |
| Some high school | 2 | 13.3% | 2 | 20.0% | |
| High school graduate or equivalent | 3 | 20.0% | 1 | 10.0% | |
| Vocational or technical school | 1 | 6.7% | 0 | 0 | |
| Some college or associate degree | 1 | 6.7% | 1 | 10.0% | |
| Completed college (bachelor’s degree) | 3 | 20.0% | 1 | 10.0% | |
| Graduate school | 0 | 0 | 0 | 0 | |
| Not disclosed | 1 | 6.7% | 0 | 0 | |
| Household income | Less than $10,000 | 4 | 26.7% | 4 | 40.0% |
| $10,000–$19,999 | 2 | 13.3% | 1 | 10.0% | |
| $20,000–$29,999 | 0 | 0 | 0 | 0 | |
| $30,000–$39,999 | 2 | 13.3% | 1 | 10.0% | |
| $40,000–$49,999 | 1 | 6.7% | 1 | 10.0% | |
| $50,000–$59,999 | 1 | 6.7% | 1 | 10.0% | |
| $60,000–$69,999 | 1 | 6.7% | 1 | 10.0% | |
| $70,000–$79,999 | 1 | 6.7% | 0 | 0 | |
| Not disclosed | 2 | 13.3% | 1 | 10.0% | |
| Spina bifida level | High Lumbar | 4 | 26.7% | 3 | 30.0% |
| Mid Lumbar | 2 | 13.3% | 1 | 10.0% | |
| Low Lumbar | 3 | 20.0% | 2 | 20.0% | |
| Sacral | 2 | 13.3% | 2 | 20.0% | |
| Thoracic | 4 | 26.7% | 2 | 20.0% | |
| Ambulatory status | Ambulatory | 7 | 46.7% | 6 | 60.0% |
| Non-Ambulatory | 8 | 53.3% | 4 | 40.0% |
Program adherence
The program was implemented over a 3-month (13-week) period for each participant. At the onset, about half of the participants were using the mobile app. However, the number of participants declined from 8/15 (53%) people in week 1–3/15 (20%) in week 2. Temporary increases in app use occurred at both the 4- and 8-week period, which correlated to the time of their virtual check-in with the athletic trainer (Fig. 4). Out of the fifteen enrolled participants, two were lost to follow-up and 3 withdrew. Out of the ten participants who completed the program, two attended all 3 monthly check-ins, three attended 2 check-ins and the remaining five completed the initial meeting only.
Figure 4.
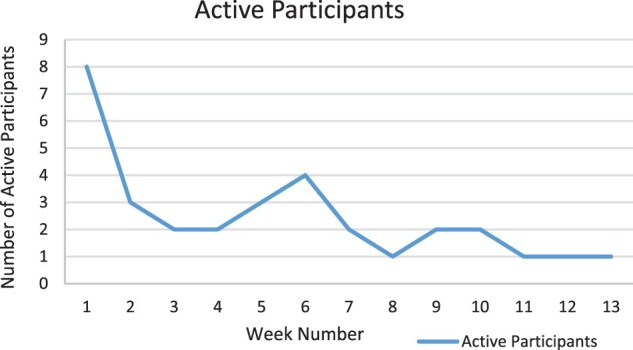
Number of active participants* during 13-week intervention. *Active participant was defined as using the app three or more days per week
Fifty percent (5/10) of the participants who completed the program attended at least one of the Nutrition Sessions. Of those who attended, they found the information presented was helpful. Eight four percent of attempted exercises were completed. Exercises that were incomplete were secondary to pain or difficulty.
Body composition measurements
Both pre- and postintervention height and weight were recorded for nine of ten participants who completed the program. Of these, seven reduced their overall BMI, two increased their BMI and one was not seen back in clinic for measurements (Table 4). Collectively, participants saw a 1 kg/m2 drop in average BMI from pre- (31.6 ± 8.2) to postintervention (30.5 ± 6.9) although the difference was not statistically significant (P = 0.11). Spearman’s rank correlation found no significant relationship between app usage and change in BMI (ρ = 0.23, P = 0.55).
Table 4.
Changes in BMI from pre- to post-intervention.
| Subject | BMI Pre-Intervention (kg/m2) | BMI Post-Intervention (kg/m2) | Change in BMI (kg/m2) | Percent (%) change in BMI |
|---|---|---|---|---|
| 1 | 25.4 | 24.3 | −1.1 | −4.5% |
| 2 | 25.8 | 28.4 | +2.4 | +9.3% |
| 3 | 28.1 | 25.7 | −2.4 | −8.5% |
| 4 | 43.0 | 40.8 | −2.2 | −5.1% |
| 5 | 21.7 | 20.6 | −1.1 | −5.1% |
| 6 | 49.4 | 42.3 | −7.1 | −14.3% |
| 7 | 32.0 | 32.3 | +0.3 | +0.9% |
| 8 | 28.4 | 27.3 | −1.1 | −3.9% |
| 9 | 34.3 | 32.9 | −1.4 | −4.1% |
| 10 | 25.8 | ND* | ND* | ND |
*Patient completed post-intervention surveys but did not come into the Spina Bifida clinic for post-intervention BMI measurements. ND = no data.
Survey outcome measures
In the program evaluation, 9/10 (90%) participants who completed the survey liked the program overall, and all (10/10) would recommend this program to a friend interested in weight management. However, only 3/10 (33%) participants would recommend the Pt PalTM app alone. Participants rated the app through the MARS as a Quality Mean Score of 3.57/5. App users rated Pt PalTM highest in functionality (3.9/5) and lowest (3.2/5) in engagement.
PedsQL™ and the modified YRBS were completed pre- and postintervention. The results of the modified YRBS revealed that 5/10 (50%) of those who finished the program reported being active at least one more day per week than they were before the program. This increase in activity was also reflected in 4/10 (40%) participants reporting less time spent watching TV, and 6/10 (60%) reporting less time playing computer or phone games. Three out of 10 (30%) participants reported eating at least one more serving of fruit and vegetables per day. Again, due to the small sample size, these numbers did not reach statistical significance but are worth noting.
The results of the PedsQL™ survey exhibited slight increases in emotional functioning scores (59.5 ± 24.1 pre-intervention, 64.5 ± 17.2 post-intervention, P = 0.500) and social functioning scores (60 ± 25.7 pre-intervention, 67 ± 20.2 post intervention, P = 0.411). However, a slight decrease was seen in physical functioning scores (57.5 ± 19.1 pre-intervention, 53.1 ± 19.0 post-intervention, P = 0.305), and a significant reduction was observed in school functioning scores (52.5 ± 17.6 pre-intervention, 44.4 ± 21.9 post-intervention, P = 0.045). As for the summary scores, Physical Health experienced a slight decrease (57.5 ± 19.1 pre-intervention, 53.1 ± 19.0 post-intervention, P = 0.305) and Psychosocial Health Summary scores experienced a slight increase (57.3 ± 20.6 pre-intervention, 58.7 ± 15.8 postintervention, P = 0.718). Overall, the Total Scale Score remained the same (57.4 ± 18.6 preintervention and 57.3 ± 14.2 post-intervention, P = 0.881).
As part of the program evaluation, participants were asked if they had any suggestions for improving the program. Most conveyed that they would benefit from greater individualization and support and more variety in the exercises provided. Participants also expressed interest in more in-person resources and virtual or in-app group exercise classes.
Discussion
The purpose of this study was to assess the feasibility of using the Pt Pal™ mobile app with coaching to engage AYA with SB in a weight management program. While many studies report similar challenges with adherence, the use of the mobile app with tracking allowed us to observe the specific time points at which attrition occurred and how actively participants were engaged in the program as evident in Fig. 4. Half of our participants used the app during the first week, with an increase in app use at weeks 4 and 8 virtual check-ins with their coach. Based on feedback, there was a preference for pairing the app with coaching and allowing both in-person and virtual opportunities. This underscores the importance of a multimodal approach. A recent systematic review by Schoeppe et al. demonstrated there is evidence supporting the effectiveness of app-based interventions in improving diet, physical activity, and sedentary behaviors; however, they concluded that multi-component interventions appear to be more effective than stand-alone app interventions, consistent with our findings (25). Another study looked at text messaging in upper extremity exercise programs in adults with SB (26) and found low overall participation rates with no significant differences in participation between the message reminder groups. The authors concluded that barriers to exercise participation may outweigh the ability to motivate adults with SB to exercise with electronic reminders, underscoring the need for interaction with the care team. Motivational interviewing and more stringently assessing participants’ readiness to change may impact attrition levels which was a significant issue in this cohort.
While our program duration was brief, based on YRBS survey responses, participants did report improvements with an increase in physical activity and a decrease in sedentary activities postintervention. At baseline, our cohort reported a PedsQL™ score typical among this population compared to non-SB scores (26). Our most active user was an ambulatory 20-year-old female with a high lumbar level of function. She used the app 6–7 times a week or 91% of days during the 3-month period. Her overall Peds QL™ score was the highest among those who completed the program (81.4 pre-intervention, 74.1 post-intervention). Although the most active participant had the highest Peds QL score, greater participation levels did not statistically correlate with higher post-intervention PedsQL™ scores or change in scores. The PedsQL™ allowed us to gain insight into how this population functions in physical, social, emotional, and school domains. School and physical scores were the lowest among the four domains, though this may have been partially due to the COVID-19 pandemic. Social and emotional scores showed slight improvements, but these differences were not statistically significant and did not correlate with the levels of interaction with the app.
BMI was utilized to determine changes in weight over the duration of the program. Although BMI has been a controversial method of identifying obesity within the SB population, the goal of collecting this measurement was to track changes from pre- to post-intervention. The subject with the highest recorded compliance remained the same weight, with a gain of 0.5 kg and a change in BMI of 0.32 kg/m2. The greatest reduction in BMI was a decrease of 7.1 kg/m2 by a subject who used the app 1–2 days per week. Because BMI does not account for body composition, weight changes could be due to changes of fat or muscle mass. Thus, BMI cannot be an entirely reliable measurement of progress for an exercise and strength training program. In the future, we can more accurately assess baseline and post-intervention fitness using aerobic capacity at pre- and postintervention.
The exercise program included strength and stretching exercises. The most painful exercise was the seated crunch, and the most difficult was the seated scapular squeeze. We believe this may be unique to the SB population based on the location of their post-surgical scar, their shorter lower body segments and trunk, and baseline weakness in core strength related to their underlying paralysis. Future modifications should include additional aerobic routines to allow for improvements in flexibility and cardiovascular fitness.
Access to physical activity among youth with SB is limited for children without disabilities. One major challenge was engagement. The lowest MARS sub-score was app engagement which has been shown in other studies (27). Edney et al. reported that inclusion of gamified features enhanced engagement and led to greater increases in physical activity in those who were the most engaged (28). Another study by Lai et al. demonstrated that two wheelchair dependent youth with SB enjoyed the use of a virtual reality system to achieve home exercise guidelines (29). Stiles-Shields et al. conducted a survey of adolescents with SB on their technology usage and found them to be selective users (30). Young adults have higher usage than their younger counterparts, which is similar to our findings where the age range of active users was 15–21 years. Top concerns focused on usability, accessibility, safety, personal barriers, and efficacy. Our cohort reported favorability related to the app functioning but felt it could use improvements in engagement. Within the engagement category, customization and interest received the lowest scores. Although the app was found to be less engaging, the functionality scores revealed that users did find the design to be intuitive and easy to navigate. With this feedback in mind, it is plausible to consider minor adjustments to the mHealth platform to improve overall engagement and adherence to an app-based weight management program.
This study had several limitations including small sample size, short time interval to identify lasting behavior adoption and change, and attrition. Moreover, this study occurred during the COVID-19 pandemic where many stressors impacted the participants, families, and staff. Additionally, we did not look at the impact of the app alone compared to the app with coaching.
Conclusion
Obesity in young people affected by SB or other mobility issues warrants further evaluation, including innovative approaches to address this multifactorial issue. The results of this pilot study suggest that there are challenges to implementing an app-based weight management program, impacting widespread feasibility, though the program was well received by some participants. With appropriate modifications, this type of intervention may provide an innovative and cost-effective mHealth option for activity promotion and weight loss. The feasibility will further be improved with additional barrier evaluation and coaching support. Future directions should address the barriers identified in this study and incorporate feedback to develop a multicenter clinical trial.
Disclaimer statements
Acknowledgements We gratefully thank our certified athletic trainers, dietary interns, and SB clinical team for their partnership in this program.
Author contributions Jacquelyn Valenzuela-Moss, BS: Enrollment, Data collection, Manuscript Preparation and Review. Melissa A. Bent, MD: Study Idea and Design, Recruitment, Manuscript Preparation and Review. Kathryn A. Smith, RN, MN, MS, DrPH: Grant mentor, Manuscript Review. Patricia Castillo, MD: Study Design, Recruitment, Manuscript Review. Alexander Van Speybroeck, MD: Grant mentor, Recruitment, Manuscript Review. Hanna Omar, BS: Enrollment, Data Collection, Manuscript Review. Katherine Antoniak, MPH: Study Design, Manuscript Review. Adrian Lin, BS: Data Collection, Manuscript Review. Tishya A.L. Wren, PhD: Statistical Data Analysis, Manuscript Review.
Funding This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)-supported Academic Pediatric Association (APA) Research in Academic Pediatrics Initiative on Diversity (RAPID) program (NIH R25DK096944). This study has been carried out with approval from the Institutional Review Board at Children’s Hospital Los Angeles.
Conflicts of interest Authors have no conflict of interests
References
- 1.National institute of neurological disorders and stroke-national institutes of health: spina bifida fact sheet . Spina bifida fact sheet. NINDS, Publication date June 2013. NIH Publication No. 13-309. [cited 2019 Nov 21]. Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Spina-Bifida-Fact-Sheet.
- 2.Sandler AD. Children with spina bifida: key clinical issues. Pediatr Clin N Am. 2010;57(4):879–892. [DOI] [PubMed] [Google Scholar]
- 3.Azdick S. Spina bifida causes, symptoms and treatment. The Children's Hospital of Philadelphia, 31 Mar. 2014. Available from: https://www.chop.edu/conditions-diseases/spina-bifida.
- 4.Wilson PE, Mukherjee S.. Mobility guidelines for the care of people with spina bifida. J Pediatr Rehabil Med. 2020;13(4):621–627. doi: 10.3233/PRM-200744. PMID: 33325411; PMCID: PMC7838952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gober J, Thomas SP, Gater DR.. Pediatric spina bifida and spinal cord injury. J Pers Med. 2022;12(6):985. doi: 10.3390/jpm12060985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sawin KJ, Bellin MH.. Quality of life in individuals with spina bifida: a research update. Dev Disabil Res Rev. 2010;16(1):47–59. [DOI] [PubMed] [Google Scholar]
- 7.Dosa NP, Foley JT, Eckrich M, Woodall-Ruff D, Liptak GS.. Obesity across the lifespan among persons with spina bifida. Disabil Rehabil. 2009;31(11):914–920. [DOI] [PubMed] [Google Scholar]
- 8.Starowicz J, Cassidy C, Brunton L.. Health concerns of adolescents and adults with spina bifida. Front Neurol. 2021;12:745814. doi: 10.3389/fneur.2021.745814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castillo J, Gandy K, Bradko V, Castillo H.. Language and Latino immigrants living with spina bifida: social determinants of health – the missing dimension in quality-of-life research. J Pediatr Rehabil Med. 2019;12(4):345–359. doi: 10.3233/PRM-180586. PMID: 31744031. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) . Racial/ethnic differences in the birth prevalence of spina bifida – United States, 1995–2005. Mor Mortal Wkly Rep. 2009; 57(53):1409–1413. PMID: 19129744. [PubMed] [Google Scholar]
- 11.McDonald ML, Huang A, Proudfoot JA, Le JT, Chiang GJ, Bush RA.. Association of obesity, BMI, and Hispanic ethnicity on ambulatory status in children with spinal dysraphism followed near the California-Mexico border. J Health Care Poor Underserved. 2016;27(4):1956–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howell CR, Juarez L, Agne AA, Nassel AF, Scarinci IC, Ayala GX, Cherrington AL. Assessing Hispanic/Latino and non-Hispanic white social determinants of obesity among a community sample of residents in the rural southeast US. J Immigr Minor Health. 2022;24(6):1469–1479. doi: 10.1007/s10903-022-01334-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu JS, Dong C, Vo AX, Dickmeyer LJ, Leung CL, Huang RA, Kielb SJ, Mukherjee S. Obesity and anthropometry in spina bifida: what is the best measure. J Spinal Cord Med. 2018;41(1):55–62. doi: 10.1080/10790268.2016.1195071. Epub 2016 Aug 23. PMID: 27551923; PMCID: PMC5810807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hyun S, Li X, Vermillion B, Newton C, Fall M, Kaewprag P, Moffatt-Bruce S, Lenz ER. Body mass index and pressure ulcers: improved predictability of pressure ulcers in intensive care patients. Am J Crit Care. 2014;23(6):494–501; quiz 501. doi: 10.4037/ajcc2014535. PMID: 25362673; PMCID: PMC4385001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sallinen Gaffka BJ, Frank M, Hampl S, Santos M, Rhodes ET.. Parents and pediatric weight management attrition: experiences and recommendations. Child Obes. 2013;9(5):409–417. [DOI] [PubMed] [Google Scholar]
- 16.McPherson AC, Swift JA, Peters M, Lyons J, Joy Knibbe T, Church P, Chen L, Farrell RM, Gorter JW. Communicating about obesity and weight-related topics with children with a physical disability and their families: spina bifida as an example. Disabil Rehabil. 2017;39(8):791–797. [DOI] [PubMed] [Google Scholar]
- 17.Carter MC, Burley VJ, Nykjaer C, Cade JE.. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res. 2013;15(4):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stiles-Shields C, Garcia B, Villota K, Wartman E, Winning AM, Holmbeck GN.. Exploring an existing weight management app for use with adolescents and young adults with spina bifida: usability study. JMIR Pediatr Parent. 2019;2(2):e15153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrés A, Saldaña C, Gómez-Benito J.. The transtheoretical model in weight management: validation of the processes of change questionnaire. Obes Facts. 2011;4(6):433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C.. Functional ambulation in patients with myelomeningocele. J Bone Joint Surg. 1973;55(1):137–148. doi: 10.2106/00004623-197355010-00014. PMID: 4570891. [DOI] [PubMed] [Google Scholar]
- 21.Espinoza J, Chen A, Orozco J, Deavenport-Saman A, Yin L.. Effect of personal activity trackers on weight loss in families enrolled in a comprehensive behavioral family-lifestyle intervention program in the Federally Qualified Health Center setting: a randomized controlled trial. Contem Clin Tri Comm. 2017;7:86–94. doi: 10.1016/j.conctc.2017.06.004. Epub 2017 Jun 15. PMID: 29308436; PMCID: PMC5753795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Varni J. PedsQL TM (Pediatric Quality of Life Inventory TM). Pedsql.org, 2020. Available from: www.pedsql.org/about_pedsql.html.
- 23.Centers for Disease Control and Prevention (CDC) . 1991-2019 High School Youth Risk Behavior Survey Data. Available from: http://yrbs-explorer.services.cdc.gov/.
- 24.Stoyanov SR, Hides L, Kavanagh DJ, Zelenko O, Tjondronegoro D, Mani M.. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3(1):e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoeppe S, Alley S, Van Lippevelde W, Bray NA, Williams SL, Duncan MJ, Vandelanotte C.. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nut Phys Act. 2016;13(1):127. doi: 10.1186/s12966-016-0454-y. PMID: 27927218; PMCID: PMC5142356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crytzer TM, Dicianno BE, Fairman AD.. Effectiveness of an upper extremity exercise device and text message reminders to exercise in adults with spina bifida: a pilot study. Assist Technol. 2013;25(4):181–193. doi: 10.1080/10400435.2012.747572. PMID: 24620701; PMCID: PMC3955014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray CB, Holmbeck GN, Ros AM, Flores DM, Mir SA, Varni JW.. A longitudinal examination of health-related quality of life in children and adolescents with spina bifida. J Pediatr Psychol. 2015;40(4):419–430. doi: 10.1093/jpepsy/jsu098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edney S, Ryan JC, Olds T, Monroe C, Fraysse F, Vandelanotte C, Plotnikoff R, Curtis R, Maher C. User engagement and attrition in an app-based physical activity intervention: secondary analysis of a randomized controlled trial. J Med Internet Res. 2019;21(11):e14645. doi: 10.2196/14645. PMID: 31774402; PMCID: PMC6906621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lai B, Davis D, Narasaki-Jara M, Hopson B, Powell D, Gowey M, Rocque BG, Rimmer JH. Feasibility of a commercially available virtual reality system to achieve exercise guidelines in youth with spina bifida: mixed methods case study. JMIR Serious Games. 2020;8(3):e20667. doi: 10.2196/20667. PMID: 32880577; PMCID: PMC7499165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stiles-Shields C, Anderson L, Driscoll CFB, Ohanian DM, Starnes M, Stern A, Yunez A, Holmbeck GN. Technology usage and barriers to the use of behavioral intervention technologies in adolescents and young adults with spina bifida. J Pediatr Rehabil Med. 2020;13(4):675–683. doi: 10.3233/PRM-190652. PMID: 32986627. [DOI] [PubMed] [Google Scholar]