Abstract
Background
Advance care planning (ACP) is pivotal in mitigating end-of-life suffering and ensuring healthcare congruence with the values of older adults and dignity in death. Despite its paramount importance, the current readiness for ACP among community-dwelling older adults and the intricate influencing factors have yet to be explored.
Objective
To review the literature focusing on ACP readiness among community-dwelling older adults and the influencing factors.
Methods
A scoping review conducted using the Arksey and O’Malley (2005) framework. Electronic databases (PubMed, CINAHL, Cochrane, Web of Science, PsycINFO), as well as grey literature databases (OpenGrey and GreyLit.org) were searched to identify studies published in English between January 2012 and March 2023.
Results
19 studies were selected, comprising 3 qualitative, 13 quantitative, 2 mixed-methods, and 1 review article. The study evaluated the readiness of older adults for ACP by examining their knowledge and attitudes. It categorizes influencing factors into intrinsic and extrinsic levels. This review revealed that the knowledge about ACP among older adults across all settings was limited. However, they had positive attitudes toward it. In addition, intrinsic factors including sociodemographic characteristics, psychological factors, and family relationships, along with extrinsic factors including health care professionals’ attitudes and experience, as well as policies and laws, influenced the ACP readiness among older adults.
Conclusions
This study established the groundwork for future ACP intervention trials, providing a theoretical framework to guide their design and implementation. operationalization.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12904-024-01583-4.
Keywords: Advance care planning, Community, Older adults, Influencing factor, Readiness
Introduction
The aging population is increasing in industrialized countries worldwide. Death is an inevitability, and older adults have a high prevalence of chronic disease, severe comorbidities, low quality of life (QOL), and high death rates from disease [1]. In the absence of a cure for a disease, older people believe that treatment to prolong life is painful and undesirable [2]. In addition, a significant proportion of older people, estimated to be up to 70%, cannot make decisions about their end-of-life (EOL) care [3], which has significant implications, such as psychological and financial burdens on family members, exacerbating intra-family conflicts, and wasting valuable medical resources [4, 5].
Advance care planning (ACP) is the process of making decisions about medical treatment, including future consent to, refusal of, or withdrawal of treatment and substitute decision-making [6]. ACP reduces the decision-making burden on families and mitigates the overuse of healthcare resources [7–9]. ACP readiness is a key determinant for health care professionals (HCPs) to judge the timing of ACP initiation, it is distinct from acceptance and can be seen as a preliminary stage leading to either the adoption or resistance to ACP [10]. HCPs and older adults consider ACP readiness to be a crucial factor when deciding whether to engage in a conversation about ACP [11]. Given the aging population and the increasing awareness of individuals’ rights to make healthcare decisions, it is vital to understand older adults’ ACP readiness to ensure healthcare choices are consistent with their values.
ACP tends to be predominantly applied in clinical settings, primarily for EOL patients [12, 13]. Nonetheless, recognizing the community’s pivotal role in primary healthcare—specifically in disseminating health policy information and elevating public awareness [14], the Institute of Medicine has emphasized that community-dwelling older adults are essential groups for ACP development [15]. Despite this recognition, the existing literature offers limited insight into the readiness of community-dwelling older adults to engage in conversations about ACP [16, 17]. Previous studies have shown that the intricate interplay of factors influences ACP readiness, including cultural background, the timing of discussions, existing medical conditions, and the attitudes and beliefs of HCPs, underscoring the complexity of the ACP process [18, 19]. As a result of these complexities, it is necessary to address the literature gaps and provide a comprehensive overview of the literature on ACP readiness among community-dwelling older adults.
A scoping review aims to comprehensively map and summarize the existing literature on a specific topic or research question. It is beneficial when the research topic is complex, emerging, or multidisciplinary [20]. A scoping review entails an initial assessment of the breadth, extent, and characteristics of the available literature [21]. We employ a scoping review methodology in this study, focusing on the community-dwelling older adults’ ACP readiness and the factors influencing readiness. The objectives of this scoping review were to (1) identify the extent of ACP readiness among community-dwelling older adults and (2) identify factors influencing the ACP readiness of community-dwelling older adults. The results of this scoping review are a valuable resource for disseminating public information, clarifying the current ACP readiness of community-dwelling older adults and the factors influencing that readiness, and guiding future systematic reviews and other studies.
Methods
This scoping review followed the framework initially proposed by Arksey and O’Malley [21], with subsequent modifications introduced by Levac, Colquhoun [22]. The review process adhered to a structured approach consisting of seven key stages: (1) protocol and registration, (2) eligibility criteria, (3) information sources, (4) search strategy, (5) evidence selection, (6) data charting, and (7) result synthesis [23].
Protocol and registration
This scoping review report uses the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guidelines [23]. These protocols have been registered in the Open Science Framework (Registration DOI: 10.17605/OSF.IO/HRJNT) [24].
Eligibility criteria
The researcher (GF) carried out a comprehensive search strategy in consultation with two experienced research librarians (XL & ZQ) to develop the search terms and search strings. Articles were selected for review if they met the following inclusion criteria: (1) focused on ACP readiness of community-dwelling older adults, (2) included adults aged 50 and over (this age was chosen because, at this age, the attention of primary care turns to chronic disease and cancer screening, providing an opportunity for healthy older adults to be introduced to ACP [25]]), (3) conducted within community settings or nursing homes, (4) involved original research, including quantitative, qualitative, and mix-method studies, systematic reviews, and literature reviews, and (5) had full-text available in English. The exclusion criteria for this literature included articles published in other languages, and studies that described ACP readiness of the younger population or did not mention age.
Information sources
Electronic databases (PubMed, CINAHL, Cochrane, Web of Science, PsycINFO), as well as grey literature databases (OpenGrey and GreyLit.org) were thoroughly searched and examined. The search results were limited to articles published from January 2012 to March 2023. The reference lists in the selected articles were screened and manually reviewed to identify additional relevant articles and capture as much information as possible.
Search strategy
Appropriate search terms or combinations of medical subject headings (MeSH) were utilized in each database. Generally, the following terms were included: “(advance care planning), OR (advanced directives), OR (end-of-life planning), AND (readiness), OR (preparedness), OR (awareness), OR (perception), OR (attitudes), OR (willingness), OR (behavioral tendencies), AND (community), OR (nursing homes), AND (older adults), OR (elderly), OR (aged)” (for full search strategies, see Supplementary Table 1).
Selection of sources of evidence
A researcher (GF) uploaded search results to Covidence, an online platform supporting systematic literature review data handling [26]. Following the upload, a thorough review was conducted. Initially, duplicate entries were identified and removed. Subsequently, two researchers (XL & ZQ) independently screened article titles and abstracts. After this initial screening, they comprehensively reviewed the full texts of the selected articles and extracted relevant data from the selected studies. Areas of conflict were resolved through discussions in online meetings (XL & ZQ). Researchers and steering group members were asked to suggest key articles published or in the press by January 2012. The results were checked against these and added if they were missing. A flow diagram of the search process and study selection is presented in Fig. 1.
Fig. 1.
PRISMA inclusion/exclusion flowchart
Data charting process
We employed a simplified form of inductive coding to identify patterns in the data and aid interpretation [27]. After collating article details and content, the researchers (GF & XL) categorized reported themes and subthemes. From these data, we generated domains covering key aspects of the published research on ACP readiness among community-dwelling older adults and factors influencing readiness. Themes and domains were developed by a researcher (GF) and were reviewed by the research team.
Data synthesis
In this stage, we followed the scoping review framework proposed by Levac, Colquhoun [22], incorporating accepted methods for thematic synthesis as recommended by Tricco, Lillie [28]. First, the characteristics of the studies were reported. Second, the study results on ACP readiness among community-dwelling older adults and the influencing factors were summarized. Third, the results were discussed, and the implications for future research, practice, and policy were articulated.
We summarized the studies’ main characteristics, including author names, publication year, country of the study conducted, study method, study aims, sample size, age of participants, and key findings. Table 1 summarizes the outcomes of this synthesis.
Table 1.
Summary of outcomes from 19 articles
| No. | Author(s) (year) Study country of the conducted | Study Method | Study Aim | Sample | Key Findings | |
|---|---|---|---|---|---|---|
| ACP Readiness Status | ACP Readiness Influencing Factors | |||||
| 1 | Xu et al. (2023) Hong Kong, China | Quantitative study | To assess the experience, knowledge, and preferences of EOL care among nursing home residents in Hong Kong and identify factors related to their preferences. |
286 (age ≥ 65) |
• Only 5.9% of participants had knowledge about ACP. • Most participants expressed positive attitudes toward ACP. |
• Age • Education level • Family support. |
| 2 | Tang et al. (2023) Singapore | Meta-synthesis | To synthesize evidence regarding older adults’ perceptions of ACP in preparation for EOL care. | 14 studies |
• Participants expressed a willing to learn about ACP. • Participants expressed positive attitudes toward ACP. |
• Death attitude • Psychological readiness for ACP • Confidence in HCPs • Family support • Self-reliance • Timeliness of ACP |
| 3 |
Demirkapu et al. (2023) Belgium |
Qualitative research | To explore ACP-related knowledge, experience, views, facilitators and barriers among older Moroccan adults in Belgium. |
25 (age ≥ 60) |
• Most participants lacked knowledge about ACP. • Most participants expressed positive attitudes toward ACP. |
• Knowledge about ACP • Health status • Death attitude • Family support |
| 4 |
Wang et al. (2022) USA |
Quantitative study | To examine the association between family relationships and older Chinese Americans’ attitudes toward family involvement in EOL care discussions. |
260 (age ≥ 55) |
NA |
• Family cohesion • Family conflict |
| 5 | Ho et al. (2022) Hong Kong, China | Quantitative study | To examine decision-making preferences for EOL care in Japan, Hong Kong, and South Korea. |
415 (age ≥ 65) |
• Three-quarters of the participants were not willing to participate in a formal ACP. | • Family support |
| 6 | Fleuren et al. (2021) Netherlands | Quantitative study | To describe the prevalence of ACP and the relationship between subjective life expectancy and engagement in ACP among older people in the Netherlands. |
1585 (age ≥ 57) |
• Most participants had knowledge about ACP. • 75% of participants were willing to discuss ACP-related topics with loved ones, but only one-third were willing to participate in a formal ACP. |
• Health status • Subjective life expectancy |
| 7 | Van Dyck et al. (2021) USA | Quantitative study | To examine ACP knowledge and its correlation with engagement in older adults. |
921 (age ≥ 55) |
• More than a quarter of the participants had a low level of knowledge about ACP. | • Knowledge about ACP |
| 8 | Yang et al. (2021) China | Mixed-methods research | To investigate preference and the factors influencing ACP for community-dwelling older patients in China. |
Quantitative phase: 471, Qualitative phase: 14 (age ≥ 60) |
• Most participants expressed positive attitudes toward ACP. |
• Death attitudes • Self-reported health status • Family support • Acute medical care experience |
| 9 | Kawakami et al. (2021) Japan | Quantitative study | To examine the knowledge about ACP and their related factors among community-dwelling older people in Japan, Hong Kong, and South Korea. |
404 (age ≥ 50) |
• 30% of participants had knowledge about ACP. • Japanese participants had a higher knowledge rate than South Korea. |
• Education level • Age • Health status |
| 10 | Pei et al. (2021) USA | Quantitative study | To examine how immigrant status and family relationships are associated with ACP among the largest subgroup of Asian Americans. |
430 (age ≥ 55) |
NA |
• Cultural background • Family conflict • Family cohesion |
| 11 | Zhu et al. (2020) China | Mixed-methods research | To measure the knowledge and attitude toward ACP among Chinese people and explore the influencing factors. |
Quantitative phase: 523, Qualitative phase: 16 (age ≥ 60) |
• Participants had a low level of knowledge about ACP. • Participants had a positive attitude toward ACP. |
• Religious beliefs • Health status • LST experience |
| 12 | Cattagniet et al. (2019) Switzerland | Quantitative study | To test the association between increased knowledge of ACP dispositions and positive perceptions of them. |
2125 (aged: 71 ~ 80) |
• 50% participants lacked the knowledge about ACP dispositions. | • Knowledge about ACP |
| 13 | Lee et al. (2018) Korea | Quantitative study | To determine the factors influencing Korean older adults’ attitudes toward ACP, with consideration of an Asian cultural background. |
295 (age ≥ 60) |
• 79.32% participants expressed positive attitudes toward ACP. |
• Education level • Economic status • Cognitive functioning • Physical functioning • Death-related experiences • Family support |
| 14 | Yap et al. (2018) Australia | Qualitative research | To identify factors influencing older Chinese Australians’ willing to participate in ACP. |
30 (age ≥ 55) |
• Participants had a low level of knowledge about ACP. • Participants had a positive attitude toward ACP. |
• Age • Healthcare systems • Support networks • Education level • Health experience |
| 15 | Howard et al. (2018) Canada | Quantitative study | To assess older patients’ willing to participate in ACP and predictors. |
810 (age ≥ 50) |
• Two-thirds of participants had knowledge about ACP-related content. • 52.8% of participants had ACP-related behaviors. |
• Age • Degree of communication with healthcare providers |
| 16 | Ko E et al. (2016) USA | Quantitative study | To explore willingness to complete advance directives and examine the factors impacting willingness among low-income older adults. |
204 (age ≥ 60) |
• 72.1% of participants were willing to complete advance directives. |
• Self-rated health • Social support |
| 17 | Michael et al. (2017) Australia | Qualitative research | To examine the awareness, attitudes, and experiences of ACP among older people and unrelated caregivers of older people residing in the community. | 15 (age ≥ 55) and 27 caregivers | • Participants expressed positive attitudes toward ACP. |
• Cultural background • Knowledge about ACP • Previous medical decision-maker experience |
| 18 | Musa et al. (2015) England | Quantitative study | To assess ACP attitudes of older people in the East Midlands. |
1823 (age ≥ 65) |
• One-third of the participants expressed positive attitudes toward ACP. |
• Age • Gender • Physical function • Family support |
| 19 | Jeong et al. (2015) Australia | Quantitative study | To explore the preparedness for EOL care planning among community-dwelling older persons of culturally and linguistically diverse backgrounds. |
453 (age ≥ 65) |
• Participants expressed a low level of knowledge about ACP. |
• Cultural background • Family support • HCPs’ support |
Results
Study selection and search results
The results of the evidence selection phase are illustrated in a PRISMA 2020 flow diagram [29] as Fig. 1.
Study characteristics
Of the 19 articles conducted in either community or nursing home settings, four articles were from the USA, three articles were from Australia, two articles were from mainland China, two were from Hong Kong SAR, and there was one article each from England, Switzerland, Canada, Singapore, Japan, Netherlands, Belgium, and Korea. Of these, three were qualitative research articles, 13 were quantitative research articles, two were mixed-method articles, and one article was a review. The review of the literature revealed that ACP is more commonly practiced in Western countries, such as the USA, Australia, and European countries. This is consistent with the findings of Martin et al. [30]. However, interest in this topic is increasing in the Asian cultural context, particularly in China, Korea, Singapore and Japan, where they have successfully encouraged people to use or develop ACP in the form of legislation or recommendations [31].
Synthesis of results
The extent of ACP readiness among community-dwelling older adults
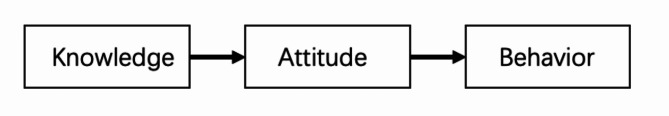
ACP readiness can be defined as an individual’s willingness to actively participate in conversations concerning one’s values and preferences with both family members and HCPs about engaging in ACP [14, 32]. It assesses a person’s behavioral tendency and willingness to participate in the process at the individual level [33]. According to the knowledge-attitude-behavior theory, an individual’s knowledge directly influences their attitudes, consequently impacting their willingness to participate in the behavior (see Fig. 2) [34, 35]. Knowledge serves as an initial step in the process of readiness for action [36, 37], while attitude stands as one of the most significant indicators used to predict and explain intentions and behaviors [38]. Therefore, two subthemes, (1) knowledge about ACP and (2) attitudes toward ACP, were further described to illustrate ACP readiness among community-dwelling older adults.
Fig. 2.
The knowledge-attitude-behavior model
Knowledge about ACP
This review revealed that the knowledge about ACP among older adults across all settings was limited. For instance, a study in the USA involving 921 participants aged 55 years and older revealed that only 11.9% answered all ACP-related items correctly [39]. In Australia, among 229 older adults, only 24% of participants were aware of advance directives (ADs) [12]. A survey of 2,125 older residents in Switzerland showed that 50% of participants lacked the knowledge about ACP dispositions [40]. Similarly, in a survey conducted in Japan, Korea, Hong Kong SAR, and China, only 30% of respondents had knowledge about ACP or ADs [17]. The low level of knowledge about ACP was also observed among older Chinese migrants [38, 41]. This is even more evident in mainland China, where a cross-sectional survey in Zhengzhou City showed that 92.7% of older residents in the community had never heard of ACP [42].
Attitude toward ACP
Despite the initial low awareness of ACP, older adults displayed an increased willingness to engage in ACP after being informed about its purpose and benefits. For instance, a study conducted in Korea found that 80% of community-dwelling older adults agreed with the need for an AD after receiving explanations [31]. Similarly, in Switzerland, a notable portion of older adults expressed openness to completing ACP upon becoming aware of its opportunities [40]. In Belgium, interviews with 25 older adults revealed that despite initial lack of knowledge, they showed positive inclination towards ACP following detailed explanations [43]. In Hong Kong, a survey involving 286 older adults demonstrated that, despite their lack of knowledge about ACP, 42.3% of participants expressed a preference for ACP after receiving an explanation [44]. In mainland China, after the investigators explained the related concepts, the attitude toward ACP by older adults in the community was found to be improved [45], aligning with the findings of Zhu et al. [42].
Influencing factors toward ACP readiness among community-dwelling older adults
Implementing ACP among older adults in the community is beneficial in preserving their autonomy, preventing harm, and ensuring equitable treatment [44]. However, various factors can impede individuals’ decision-making processes regarding ACP, including individual demographic characteristics (e.g., age, cultural, and health-related factors), HCP factors, and family support [2]. This review will discuss both intrinsic and extrinsic influencing factors, depending on their origin. Table 2 summarizes the themes concerning the influencing factors on ACP readiness.
Table 2.
A summary of the themes concerning influencing factors on ACP readiness
| Influencing aspects | Influencing factors | |
|---|---|---|
| Intrinsic influencing factors | • Sociodemographic factors |
• Age • Education level • Economic status • Health-related factors • Cultural background |
| • Psychological factors |
• Death anxiety • Mistrust in HCPs |
|
| • Family relationship |
• Family cohesion • Family conflict |
|
| Extrinsic influencing factors | • HCP attitudes and experience toward ACP | |
| • Policies and laws | ||
Intrinsic influencing factors
Three subthemes regarding intrinsic influencing factors were derived from the reviewed studies: (1) sociodemographic characteristics, (2) psychological factors, and (3) family relationships.
Sociodemographic characteristics
In this literature review, we found that age, education level, economic status, health status, acute care experience, and cultural background significantly affect ACP readiness. With age, gradual physiological deterioration, and declining health, older adults tend to think more about issues related to death and are willing to discuss EOL care [17, 46]. However, among older adults, those who are younger are more likely to prefer ACP. Xu et al. [44] found that individuals in age groups 65–74 and 75–84 years may be more receptive to new information and knowledge compared to those aged 85 years and older. This is similar to the findings of Musa et al. [47], who established that younger older adults are more inclined to participate in ACP. Additionally, education level substantially impacts ACP readiness. Studies have shown that older adults with higher levels of education tend to have greater knowledge of and access to health information, which allows them to better understand changes in their condition and prognosis. They are also more aware of the importance of ACP and are, therefore, more willing to participate in it [40, 44]. Furthermore, the level of economic status is found to be inversely related to ACP readiness, with older adults with low economic status being more supportive of ACP [31, 48]. This is possibly due to their uncertainty about the course of their illness, anxiety about their financial ability to afford treatment, and an expectation that ACP will determine their future care.
Health-related factors, including health status and acute care experience, have previously been identified as factors influencing ACP readiness [41, 45]. Older adults with poor health were more willing to participate in ACP [31, 43–45]. This may be related to the fact that older people in poor health, who have long coexisted with a variety of diseases, are characterized by a high mortality rate, a high disability rate, and a poor prognosis. Those who have been enduring significant physical and psychological hardships for an extended period tend to have a lot of doubts about their future physical well-being, as well as a sense of fear and anxiety about what they may experience as they approach the end of their lives. This is why ACP has become even more important for them. Older adults who have been exposed to seriously ill patients and experienced critical first aid are more likely to consider ACP [45], because those who experience these events may develop fear and refuse emergency measures or life-sustaining treatment (LST), influencing their own views on hospice care and the completion of ACP [31, 42, 49].
Awareness levels, attitudes, and the completion of ACP can vary significantly within different cultural contexts [12, 17]. Western countries emphasize patient autonomy, informed decision-making, and truth-telling, which is consistent with the foundation of ACP [44], whereas this idea is contrary to the Confucian culture, where death is considered a taboo topic, and older adults avoid topics related to death. At the same time, Confucian culture emphasizes familism, especially when it comes to EOL care decisions, where family collectivism is valued over patient autonomy [45]. Within this cultural context, children will be motivated by filial piety beliefs and make efforts to prolong the lives of their parents, which may sometimes be in opposition to their parents’ wishes [50]. Even among Western countries, there are differences in the specific ways in which ACP is carried out. For example, individual rights and autonomy are paramount in North America, while in Europe, the focus is more on the balance between the principles of autonomy, beneficence, and justice [46]. Thus, unlike respondents in Canada or the USA who managed to document their ACP, respondents in the Netherlands and the UK preferred to participate in the ACP program informally, such as by discussing it with family members or physicians [46].
Psychological factors
Psychological factors, such as death anxiety or mistrust in HCPs, exert considerable influence on ACP readiness. Death anxiety may lead older adults to avoid discussions about EOL matters, hindering their participation in ACP [43, 51]. Paradoxically, engagement in ACP has been linked to a reduction in death anxiety and an enhancement of QOL for older adults [45, 51]. Research indicates that older adults completing ACP report lower death anxiety levels and a greater sense of peace compared to those who abstain from ACP [52]. However, initiating ACP discussions abruptly at an older adult’s EOL, without adequate preparation, may trigger negative emotions associated with death, contributing to heightened death anxiety [10]. This underscores the critical importance of timing in initiating ACP discussions, directly impacting the success of ACP [53]. Studies reveal that older adults are more likely to discuss ACP with family members rather than HCPs, citing a lack of trust in HCPs [25, 38, 47]. This distrust stemmed from a belief that engaging in ACP might prompt HCPs to prematurely cease treatment or make medical decisions contrary to their preferences, leading to a reluctance to participate [39, 47]. Additionally, older adults perceived ACP-related issues as sensitive and expressed discomfort discussing them with HCPs due to a perceived lack of sensitivity from them [54]. Further, doubts arose about healthcare aligning with older adults’ ACP due to a lack of follow-ups as well as HCPs’ limited knowledge about ACP [51].
Family relationships
Family relationships can be assessed through two key dimensions: family cohesion and family conflict [38, 50]. Family cohesion is a crucial positive aspect of older adults’ relations with their families [55]. On the other hand, family conflict represents as a risk factor that negatively affects family relationships [56]. Previous studies have shown that high family cohesion is associated with a more positive attitude toward family involvement in discussing EOL care planning and encouraging older adults to participate in ACP [38, 43, 44]. There was also a study that showed that family cohesion had no significant relationship with the contemplation or discussion of ACP, while family conflict can serve as an indicator of a heightened necessity for engaging in ACP [50]. This might be attributed to older adults weighing the potential benefits and burdens of participating in ACP. Despite their positive attitudes toward ACP, they may hesitate to discuss it with their families because of the emotional burden the discussions put upon them. Similarly, systematic reviews have found that older adults may not engage in ACP if they are highly dependent on their families for decision-making [47]. Given the diversity in the research findings, further exploration is needed to clarify the relationship between family relationships and participation in ACP.
Extrinsic influencing factors regarding ACP readiness
Extrinsic factors were explored in many studies that impacted older adults’ decision to discuss their care management, as explained by the two subthemes: (1) HCP attitudes and experience; and (2) policies and laws.
HCP attitudes and experience with ACP
HCPs with negative attitude toward and lack experience in ACP may diminish the willingness of older adults to engage in ACP [51]. Surveys conducted among both HCPs and patients in primary care settings have indicated that discussions should be initiated by HCPs and should involve repetitive interactions with patients [25, 40]. However, in both primary care and hospital settings, HCPs tend to avoid the topic of EOL care and exhibit reluctance in engaging in ACP conversations [25]. This reluctance may stem from fears of legal repercussions for discontinuing LST [31] and concerns about potentially exacerbating negative emotions in patients, which could impede older adults’ access to ACP [46, 57]. Moreover, HCPs often lack experience with ACP. Only 5.9% of individuals aged 65 and older have had an ACP discussion with their HCPs [40]. In Korea, only about one-fifth of doctors had experience in helping patients who had completed an AD [31]. The deficiency in knowledge and experience regarding ACP further contributes to negative attitudes among HCPs toward ACP [2].
Policy and law
Legislative support is crucial for ensuring effective implementation of ACP [58, 59]. Research indicates that the introduction of relevant policies and laws positively influences older adults’ attitudes toward ACP. The earlier these policies and laws are enacted, the sooner ACP prevalence increases [44]. For instance, in the USA, the Patient Self-Determination Act (PDSA) came into effect in 1990, affirming patients’ rights to accept or refuse medical or surgical treatment [31]. In Switzerland, several states passed ACP laws in the late 1990s [40], and since 2002, ACP has been implemented in various settings in Victoria, Australia [12]. The Japanese Ministry of Health, Labor, and Welfare revised guidelines for EOL decision-making in 2018 [59]. South Korea recognized the legal validity of ACP and ADs through legislation in 2016 [60], and Hong Kong developed ACP guidelines in 2010 [17]. The slow development of ACP in mainland China also has a lot to do with the fact that China has not yet enacted specific national legislation that comprehensively defines ACP [42]. ACP management has not been fully integrated into the healthcare system, resulting in inadequate coverage for the community population [42].
Discussion
This review synthesized the current state of ACP readiness and the influencing factors in older adults. The diversity in knowledge, preferences, and arrangements related to EOL issues among older adults underscores the inconsistency in ACP readiness [61]. Despite expanding global research on the topic, the level of knowledge about ACP among older adults remains disconcertingly low across various settings and regions [51]. However, once they receive adequate information about the objectives and benefits of ACP, they become increasingly willing to engage in the process, and willingness becomes stronger with an increased level of knowledge [40]. Effective public knowledge campaigns emerge as a critical intervention to bridge this knowledge gap and foster ACP readiness.
This literature review indicates that ACP motivation is notably higher among younger older adults, those with advanced educational backgrounds, individuals with lower economic status, and those experiencing poorer health and acute care within the community. Given the community’s pivotal role in the primary healthcare system, serving as a vital avenue for disseminating health policies and enhancing public awareness [14], it stands as the optimal platform for conducting ACP activities. Policymakers can strategically leverage this potential by initiating ACP knowledge and promotion efforts targeted at the specific older age groups mentioned earlier. Following this, enabling these older individuals to share their experiences within the community can serve as a powerful means to inspire and motivate other older people to actively participate in ACP.
Furthermore, it is crucial to acknowledge that cultural background plays a significant role in shaping how individuals approach illness, death, and ACP [17]. ACP cannot be universally applied in a one-size-fits-all manner across all countries. Similarly, experiences and practices from one country may not directly translate to another. Therefore, understanding the social and cultural context of each country, as well as the educational backgrounds of older adults, becomes essential in grasping perspectives regarding ACP [17]. Incorporating more discussions about life and death into the current education system could have a profound impact on shifting the mindset of older adults for the future. This factor parallels another. Death anxiety often leads to an avoidance of ACP due to a misunderstanding of death. Research has shown that changing values and increased levels of education can potentially outweigh the influence of cultural taboos, making individuals more open to discussing sensitive topics related to death [41]. It is crucial to increase knowledge about ACP and encourage proactive efforts to promote it among older adults through various communication channels and formats. To ensure that more people understand ACP, including death education, it is important to provide easily understandable information through verbal communication, pamphlets, posters, informative videos, and EOL first aid measures. These efforts can be introduced within community settings to achieve maximum impact. These initiatives aim to encourage a scientific, rational, and open-minded perspective on death, facilitating meaningful conversations about ACP and enhancing its readiness while reducing death anxiety. It’s important to note that initiating ACP discussions abruptly may contribute to additional death anxiety among older adults [10]. Therefore, it is important to choose the right time to start an ACP discussion. Recent research indicates that older adults prefer earlier ACP discussions [51], as their cognitive abilities during this stage enable them to make ACP decisions aligning with their preferences.
Psychological factors often influence medical behaviors, so improving knowledge alone is not enough to increase participation [39, 62]. A previous review has identified that poor communication between older individuals, their families, and healthcare providers serves as a significant barrier to ACP completion [12]. Consequently, external factors such as family support, HCP attitudes and experience regarding ACP, as well as policy and legal considerations, have the potential to influence the ACP readiness among older adults.
EOL decision-making has long been a family affair, transcending individual preferences [38]. Family members play pivotal roles in supporting ACP, especially in community settings [63]. It is imperative to involve both older adults and their family members in the ACP conversation [38, 44]. While family cohesion is important, overreliance and underutilization can result in older adults’ ACP preferences being overlooked, ultimately impeding their participation [38, 44, 47]. Therefore, family members should comprehend the significance of ACP and actively engage in open communication with the patient. Throughout this communication process, family members should demonstrate implicit responsibility by trusting and respecting the older adults’ wishes, creating a harmonious and relaxed atmosphere for the execution of ACP.
The involvement of HCPs is crucial for successful ACP, as it ensures that future medical treatment aligns with the goals and preferences of older adults [46]. Older adults typically hold a deep respect for physicians’ authority, and utilizing these authority figures to attract key support networks, including family members and community groups, has been identified as key to the promotion of ACP [41]. Given the sensitivity the topic, ACP conversations should be initiated by trained HCPs [54] and maintain consistently to ensure that the process accurately reflects the changing preferences and circumstances of older adults.
As demonstrated by Detering et al. [64], the development of policies aimed at guaranteeing patient autonomy in treatment decision-making is essential to promote patient compliance with EOL care preferences. Merely relying on ACP values to guide clinical practice is insufficient to drive change in the absence of formal integration of ACP into the healthcare system. As the number of older adults living in the community increases, the policy and legal issue concerning the incompetent older person becomes more relevant [63]. Therefore, policy and legal adjustments are necessary to promote the use of ACP in routine medical practice. This might include mandating ACP discussions for older adults and encouraging healthcare facilities to implement ACP protocols. Through the formalization of ACP within the healthcare system, a greater number of older adults will have the opportunity to engage in these essential conversations and make informed EOL decisions. This approach can foster a greater appreciation of ACP as an essential element of their healthcare planning, thereby increasing their willingness to engage in ACP.
Limitation
There are some limitations to this work. As this was a scoping review, the quality of the selected studies was not rated, but the methods and variables studied did vary. Additionally, because the articles focused on community-dwelling older adults, our findings may not have implications for the general population. Our scoping review was limited to English language studies only. As such, studies in non-English journals, perhaps more relevant to non-Western populations, were not included.
Conclusion
Since humanistic values continue to gain global prominence and individuals’ sense of autonomy continues to strengthen, ensuring the EOL comfort for community-dwelling older adults has emerged as a societal concern of utmost importance [65]. Understanding the readiness of community-dwelling older adults for ACP, and the factors that influence them, is the pivotal backdrop for addressing the swift aging of the population. It is imperative to craft comprehensive EOL care measures, facilitating community-dwelling older adults’ journey toward a dignified culmination. This research is fundamental to creating ACP policies that prioritize autonomy and dignified EOL experiences in healthcare environments. To conclude, this study lays the bedrock for subsequent ACP intervention trials, offering a robust theoretical framework for their formulation and operationalization.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Table 1. Database search strategy
Acknowledgements
The authors are especially grateful to our colleagues at fellow students at the Universiti Malaya who have provided insight and expertise that greatly assisted this study.
Author contributions
FG analyzed and included the articles, in case of doubt LX and QZ adjudicated. FG was the major contributor in writing the article. CPL and CCC designed the research. All authors read and approved the final manuscript.
Data availability
The full search strategies is provided within the Supplementary Table 1.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Fang Gao, Email: 21gaofang.1127@gmail.com.
Ping Lei Chui, Email: chuipinglei@um.edu.my.
References
- 1.Ge Y, et al. The challenge and strategy selection of healthy aging in China. Manage World. 2020;36:86–96. [Google Scholar]
- 2.Ho LYW, et al. Decision-making preferences on end-of-life care for older people: exploration and comparison of Japan, the Hong Kong SAR and South Korea in East Asia. J Clin Nurs. 2022;31(23–24):3498–509. [DOI] [PubMed] [Google Scholar]
- 3.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deng R, Chen L, Shi B. Research progress of advanced care planning under Chinese culture. Chin J Nurs. 2015;50(9):1117–21. [Google Scholar]
- 5.Michael N, et al. Cancer caregivers advocate a patient-and family-centered approach to advance care planning. J Pain Symptom Manag. 2014;47(6):1064–77. [DOI] [PubMed] [Google Scholar]
- 6.Sudore RL, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manag. 2017;53(5):821–32. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitchell S, Plunkett A, Dale J. Use of formal advance care planning documents: a national survey of UK Paediatric Intensive Care Units. Arch Dis Child. 2014;99(4):327–30. [DOI] [PubMed] [Google Scholar]
- 8.Chan CW, et al. The evaluation of a palliative care programme for people suffering from life-limiting diseases. J Clin Nurs. 2014;23(1–2):113–23. [DOI] [PubMed] [Google Scholar]
- 9.Lum HD, Sudore RL, Bekelman DB. Advance care planning in the elderly. Med Clin. 2015;99(2):391–403. [DOI] [PubMed] [Google Scholar]
- 10.Hutchison LA, et al. Readiness to participate in advance care planning: a qualitative study of renal failure patients, families and healthcare providers. Chronic Illn. 2017;13(3):171–87. [DOI] [PubMed] [Google Scholar]
- 11.Zwakman M, et al. Unraveling patients’ readiness in advance care planning conversations: a qualitative study as part of the ACTION Study. Support Care Cancer. 2021;29(6):2917–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeong S, et al. Planning ahead’ among community-dwelling older people from culturally and linguistically diverse background: a cross-sectional survey. J Clin Nurs. 2015;24(1–2):244–55. [DOI] [PubMed] [Google Scholar]
- 13.Biondo PD, et al. Understanding advance care planning within the south Asian community. Health Expect. 2017;20(5):911–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rietjens JA, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–51. [DOI] [PubMed] [Google Scholar]
- 15.Care FO, Planning AC. Dying in America: improving quality and honoring individual preferences near the end of life. Mil Med. 2015;180:365–7. [DOI] [PubMed] [Google Scholar]
- 16.Zwakman M, et al. Unraveling patients’ readiness in advance care planning conversations: a qualitative study as part of the ACTION Study. Support Care Cancer. 2021;29:2917–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawakami A, et al. Advance care planning and advance directive awareness among east Asian older adults: Japan, Hong Kong and South Korea. Geriatr Gerontol Int. 2021;21(1):71–6. [DOI] [PubMed] [Google Scholar]
- 18.Master JF, et al. The compliance of end-of-Life Care preferences among older adults and its facilitators and barriers: a scoping review. J Am Med Dir Assoc. 2021;22(11):2273–e22802. [DOI] [PubMed] [Google Scholar]
- 19.Spelten ER, et al. Factors influencing the engagement of cancer patients with advance care planning: a scoping review. Eur J Cancer Care. 2019;28(3):e13091. [DOI] [PubMed] [Google Scholar]
- 20.Munn Z, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 22.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tricco AC, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 24.Cuykx I. pre-registration of the scoping review protocol. 2022; https://osf.io/7undg/
- 25.Howard M, et al. Older patient engagement in advance care planning in Canadian primary care practices: results of a multisite survey. Can Fam Physician. 2018;64(5):371–7. [PMC free article] [PubMed] [Google Scholar]
- 26.Innovation VH. Covidence systematic review software. Melbourne, Victoria, Australia: Veritas Health Innovation. 2023; https://www.covidence.org/
- 27.Braun V, Clarke V. What can thematic analysis offer health and wellbeing researchers? Taylor & Francis; 2014. p. 26152. [DOI] [PMC free article] [PubMed]
- 28.Tricco AC, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 30.Martina D, et al. Advance care planning in Asia: a systematic narrative review of healthcare professionals’ knowledge, attitude, and experience. J Am Med Dir Assoc. 2021;22(2):e3491–34928. [DOI] [PubMed] [Google Scholar]
- 31.Lee JE, et al. Factors influencing attitudes toward advance directives in Korean older adults. Arch Gerontol Geriatr. 2018;74:155–61. [DOI] [PubMed] [Google Scholar]
- 32.Shaw M, et al. Characterizing readiness for advance care planning from the perspective of residents, families, and clinicians: an interpretive descriptive study in supportive living. Gerontologist. 2018;58(4):739–48. [DOI] [PubMed] [Google Scholar]
- 33.Walczak A, et al. Patient perspectives regarding communication about prognosis and end-of-life issues: how can it be optimised? Patient Educ Couns. 2013;90(3):307–14. [DOI] [PubMed] [Google Scholar]
- 34.Yi Q, Hohashi N. Comparison of perceptions of domestic elder abuse among healthcare workers based on the knowledge-attitude-behavior (KAB) model. PLoS ONE. 2018;13(11):e0206640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu L, et al. Use of a knowledge-attitude-behaviour education programme for Chinese adults undergoing maintenance haemodialysis: Randomized controlled trial. J Int Med Res. 2016;44(3):557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promotion. 1997;12(1):38–48. [DOI] [PubMed] [Google Scholar]
- 37.Levoy K, Salani DA, Buck H. A systematic review and gap analysis of advance care planning intervention components and outcomes among cancer patients using the transtheoretical model of health behavior change. J Pain Symptom Manag. 2019;57(1):118–39. e6. [DOI] [PubMed] [Google Scholar]
- 38.Wang KP, et al. Attitude toward family involvement in end-of-Life Care among older Chinese americans: how do Family relationships Matter? J Appl Gerontol. 2022;41(2):380–90. [DOI] [PubMed] [Google Scholar]
- 39.Van Dyck LI, et al. Understanding the role of knowledge in advance care planning engagement. J Pain Symptom Manag. 2021;62(4):778–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cattagni Kleiner A, et al. Advance care planning dispositions: the relationship between knowledge and perception. BMC Geriatr. 2019;19(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yap SS, et al. Exploring the knowledge, attitudes and needs of advance care planning in older Chinese australians. J Clin Nurs. 2018;27(17–18):3298–306. [DOI] [PubMed] [Google Scholar]
- 42.Zhu, et al. Awareness and attitudes toward Advance Care Planning among Community-Dwelling older adults in China: a mixed-methods study. Am J Hosp Palliat Care. 2020;37(9):743–9. [DOI] [PubMed] [Google Scholar]
- 43.Demirkapu H, et al. Advance care planning among older adults of Moroccan origin: an interview-based study. Patient Educ Couns. 2023;113:107794. [DOI] [PubMed] [Google Scholar]
- 44.Xu X, et al. Preferences for end-of-life care: a cross-sectional survey of Chinese frail nursing home residents. J Clin Nurs. 2023;32(7–8):1455–65. [DOI] [PubMed] [Google Scholar]
- 45.Yang Z, et al. Preference and influencing factors of Advance Care Planning for Chinese Elderly patients with Chronic diseases: a mixed-methods Approach. J Hospice Palliat Nurs. 2021;23(2):178–86. [DOI] [PubMed] [Google Scholar]
- 46.Fleuren N, et al. Association between subjective remaining life expectancy and advance care planning in older adults: a cross-sectional study. J Pain Symptom Manag. 2021;62(4):757–67. [DOI] [PubMed] [Google Scholar]
- 47.Musa I, et al. A survey of older peoples’ attitudes towards advance care planning. Age Ageing. 2015;44(3):371–6. [DOI] [PubMed] [Google Scholar]
- 48.Ko E, Lee J, Hong Y. Willingness to complete advance directives among low-income older adults living in the USA. Health Soc Care Commun. 2016;24(6):708–16. [DOI] [PubMed] [Google Scholar]
- 49.Li J, et al. Investigation on Advance Care Planning behaviors in Elderly Chronic Disease patients in the community. Chin Gen Pract. 2022;25(01):94. [Google Scholar]
- 50.Pei Y, Zhang W, Wu B. Advance Care Planning Engagement and End-of-life preference among older Chinese americans: do Family relationships and immigrant Status Matter? J Am Med Dir Assoc. 2021;22(2):340–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tang JMS, et al. A meta-synthesis on the older adults’ perspective of advance care planning. Journal of clinical nursing; 2023. [DOI] [PubMed]
- 52.Kubi B, et al. Theory-based development of an implementation intervention using community health workers to increase palliative care use. J Pain Symptom Manag. 2020;60(1):10–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sudore RL, et al. Outcomes that define successful advance care planning: a Delphi panel consensus. J Pain Symptom Manag. 2018;55(2):245–55. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hudson PL, et al. Benefits and resource implications of family meetings for hospitalized palliative care patients: research protocol. BMC Palliat care. 2015;14(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Perosa LM, Perosa SL. Adolescent perceptions of cohesion, adaptability, and communication: revisiting the circumplex model. Family J. 2001;9(4):407–19. [Google Scholar]
- 56.Fosco GM, Lydon-Staley DM. Implications of family cohesion and conflict for adolescent mood and well‐being: examining within‐and between‐family processes on a daily timescale. Fam Process. 2020;59(4):1672–89. [DOI] [PubMed] [Google Scholar]
- 57.Fukue N, et al. Readiness of Advance Care Planning among patients with Cardiovascular Disease. Front Cardiovasc Med. 2022;9:838240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Prince-Paul M, DiFranco E. Upstreaming and normalizing advance care planning conversations—a public health approach. Behav Sci. 2017;7(2):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Senda K et al. There is something about advance care planning: Report on Dr Karen Detering’s lecture on advance care planning at the Annual Meeting of the Japan Geriatrics Society, 2018. Geriatrics & Gerontology International, 2018. 18(12): pp. 1651–1652. [DOI] [PubMed]
- 60.Kim HS, Yeom GJ. Influence of Advance directives’ self-efficacy of community-dwelling older adults on the completion of Advance directives: mediating the Effect of Intention for Advance directives: a cross-sectional study. J Korean Gerontological Nurs. 2022;24(2):133–41. [Google Scholar]
- 61.Nakao-Hayashizaka KC. End-of-life preparedness among Japanese americans: A Community Survey. J Soc Work End Life Palliat Care. 2022;18(3):216–34. [DOI] [PubMed] [Google Scholar]
- 62.Rice T. The behavioral economics of health and health care. Annu Rev Public Health. 2013;34:431–47. [DOI] [PubMed] [Google Scholar]
- 63.Michael N, O’Callaghan C, Sayers E. Managing ‘shades of grey’: a focus group study exploring community-dwellers’ views on advance care planning in older people. BMC Palliat care. 2017;16(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Detering KM et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ, 2010. 340. [DOI] [PMC free article] [PubMed]
- 65.Jin S et al. Stumbling and growing: a bibliometric study of academic publications of Palliative Care in Mainland China for 2010–2020. J Palliat Care, 2022: p. 08258597211039056. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Table 1. Database search strategy
Data Availability Statement
The full search strategies is provided within the Supplementary Table 1.