Abstract
Objectives
Digital technologies in healthcare are rapidly advancing, and have the potential to enhance delivery across outpatient, inpatient, and community settings, thus ultimately improving healthcare practices. These technologies have been demonstrated to be among the safest alternatives to in-person visits for vulnerable or homebound people, thereby avoiding travel and facilitating healthcare-provider communication. This review was aimed at understanding the application of digital technology to promote physical activity and exercise in older adults with type 2 diabetes mellitus.
Methods
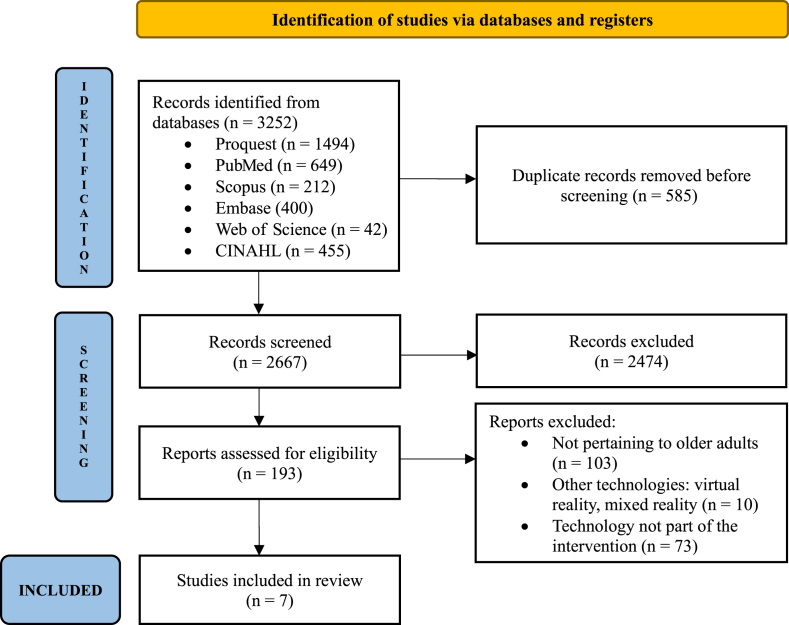
A comprehensive scoping review method was followed, according to the six-step framework developed by Arksey and O'Malley. A search was performed in six databases: Scopus, Embase, PubMed, ProQuest, Web of Science, and the Cumulated Index to Nursing and Allied Health Literature (CINAHL). Seven studies were retrieved.
Results
The search in the six databases returned 3252 records, only seven of which met the final selection criteria and were included in the review. All seven studies were conducted in high-income countries. Only one of the seven studies reported using a detailed exercise protocol.
Conclusion
Digital technology using smartphones provides an effective and a feasible solution to deliver physical activity promotion programs to older adults with type 2 diabetes mellitus, and can improve heath related outcomes.
Keywords: Aged, Digital technology, Exercise, Physical activity, Scoping review, Type 2 diabetes mellitus
الملخص
أهداف البحث
تتطور التقنيات الرقمية بسرعة في مجال الرعاية الصحية، مع إمكانية تعزيز تقديم الخدمات في العيادات الخارجية والداخلية والمجتمعية، مما يؤدي في النهاية إلى تحسين ممارسات الرعاية الصحية. وقد ثبت أنها واحدة من أكثر البدائل أمانا للزيارات الشخصية للأفراد المعرضين للخطر وأولئك المحصورين في منازلهم، وبالتالي تقليل السفر وتسهيل التواصل بين مقدمي الرعاية الصحية. تهدف هذه المراجعة إلى فهم تطبيق التكنولوجيا الرقمية في تعزيز النشاط البدني والتمارين الرياضية لدى كبار السن المصابين بداء السكري من النوع 2.
طريقة البحث
تم اتباع منهجية مراجعة شاملة لتحديد النطاق باستخدام إطار العمل المكون من ست خطوات الذي طوره أركسي وأومالي. تم إجراء بحث في ست قواعد بيانات: سكوبس، وإمباس، وبوب ميد، وبروكويست، وويب أوف ساينس، والفهرس التراكمي لأدبيات التمريض والصحة المتحالفة، وتم استرداد سبع دراسات.
النتائج
شمل البحث من ست قواعد بيانات 3252 سجلا. ولم تستوف سوى سبع وثائق معايير الاختيار النهائية وتم تضمينها في مراجعتنا. وقد نشأت جميع الدراسات السبع في بلدان ذات دخل مرتفع. ولم تذكر سوى دراسة واحدة من الدراسات السبع استخدام بروتوكول مفصل للتمرين.
الاستنتاجات
تعتبر التكنولوجيا الرقمية من حيث الهواتف الذكية حلا فعالا ومجديا لتقديم برامج تعزيز النشاط البدني لكبار السن المصابين بمرض السكري من النوع 2 ويمكنها تحسين النتائج المتعلقة بالصحة.
الكلمات المفتاحية: كبار السن, التكنولوجيا الرقمية, ممارسة الرياضة, النشاط البدني, مراجعة النطاق, مرض السكري من النوع 2
Introduction
The growing prevalence of non-transmissible diseases, particularly in the aging population, and a shortage in healthcare professionals are jeopardizing the sustainability and standards of healthcare worldwide.1 Diabetes is a rapidly increasing global health concern.2 Over the past 15 years, diabetes-related health costs have escalated by 316%, rising from $232 billion in 2007 to $966 billion in 2021.3 Type 2 diabetes mellitus (T2DM) is the most prevalent form of diabetes worldwide, and physical inactivity and obesity as key risk factors.4,5 Approximately 38% of individuals with T2DM engage in vigorous or moderate physical activity for less than 10 min per week.6 Several factors, including fear of injury, lack of motivation, and lack of enjoyment, contribute to older adults’ unwillingness to use exercise facilities. These individuals may also struggle with limited adherence and persistence in physical activity programs. However, physical activity has been shown to improve overall quality of life among older adults with T2DM, and to help prevent increases in blood glucose, body weight, cholesterol, blood pressure, and cardiovascular disease.7,8
Digital behavior change interventions are a planned series of actions using digital technologies, such as mobile applications (apps), websites, and wearable devices (e.g., activity trackers), to modify specific behavioral patterns (e.g., physical activity) in individuals.9 Improving digital health delivery contributes to good health and well-being, which is an integral part of United Nations Sustainable Development Goal 3, and consequently promotes healthy aging in individuals with T2DM worldwide.10 Recent technological advancements, such as websites and mobile messaging, have been found to positively influence the physical activity levels of individuals with T2DM. Using smartphone apps provides an opportunity to engage a diverse patient population, regardless of socioeconomic status. The wide availability of smartphones and the internet might help close the gap between what people need and what healthcare can provide, thus allowing patients to access exercise or physical activity programs.11 However, a scoping review discussing and summarizing the delivery of physical activity and exercise to older adults through digital technology (mobile and wearable), the type of physical activity delivered, and its effects was lacking. Hence, this study had the following objectives:
-
1.
Assessment of types of digital technology (mobile and wearable) that deliver physical activity and exercise to older adults with T2DM, along with the types of physical activity and exercise delivered
-
2.
Assessment of outcome measures used to assess physical activity and exercise delivered through digital technology
-
3.
Assessment of the effects of these digital technology interventions on health-related outcomes
Methods
The scoping review method was considered the most applicable method for this review, because it enables rapid assessment of emerging evidence and identifies research gaps for further systematic reviews. The key topics were also represented according to the Joanna Briggs Institute (JBI) guidelines for scoping reviews. This scoping review was performed according to the framework outlined by Arksey and O'Malley, including 1) formulating the research question, 2) identifying applicable studies, 3) selecting studies, 4) extracting data, and 5) compiling, summarizing, and presenting findings.12,13 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) checklist and the Cochrane Handbook for Systematic Reviews of Interventions were used to guide the reporting processes.
Identifying and formulating the research question
The study focused on older adults with T2DM and examined the use of digital technologies including mobile devices, tablets, and wireless technologies (such as smartwatches and activity trackers), but excluded accelerometers and pedometers. The study also investigated the physical activity-related outcomes measured. Hence, the review was driven by the following three research questions:
-
1.
What types of digital technology (mobile and wearable) have been used to deliver physical activity and exercise to older adults with T2DM, and what types of physical activity and exercise are delivered?
-
2.
What outcome measures have been evaluated to assess physical activity and exercise delivered through digital technology?
-
3.
What are the effects of these digital technology interventions on health-related outcomes?
Searching and identifying the relevant studies
This scoping review included studies on physical activity and exercise delivered through digital technology as an intervention for older adults with T2DM. The measured outcomes were physical activity and clinical outcomes. Likewise, observational study designs (e.g., case-control, cross-sectional, retrospective cohort, and prospective cohort studies) were excluded (Table 1). Keywords used in this review were “Older Adults” AND “Digital Technology” AND “Physical Activity” OR “Exercise” AND “Type 2 Diabetes Mellitus.” A literature search was conducted from September 2023 to November 2023 in the following six electronic databases: Web of Science, Scopus, Embase, ProQuest, PubMed, and Cumulated Index to Nursing and Allied Health Literature (CINAHL). The PubMed search was as follows: (((“Aged”[Mesh] OR Elderly[tw] OR “60 years and above”[tw] OR “Older Adults”[tw] OR Geriatric [tw] OR Seniors[tw] OR Ageing[tw]) AND (Digital Technology[Mesh] OR Telemedicine[Mesh] OR Internet-Based Intervention[Mesh] OR Mobile Applications[Mesh] OR Digital Health OR Telehealth OR Digital Technolog∗ OR Digital Interventions OR ehealth OR mhealth OR Physical activity monitor OR Physical Activity Sensor)) AND (“Diabetes Mellitus, Type 2”[Mesh] OR “Non-insulin Dependent Diabetes Mellitus” OR T2DM OR “Type 2 Diabetes Mellitus”)) AND (“Exercise”[Mesh] OR “Physical Activity” OR “Exercise Training” OR “Physical Activity Participation” OR “Physical Training” OR “Aerobic Activit∗” OR “Endurance Activit∗” OR “Lifestyle Activit∗” OR “Recreational Activit∗” OR “Stretching” OR “Resistance Training” OR Walking).
Table 1.
Population, Intervention (exposure), Comparison, and Outcomes (PICO) framework.
| Population | Older adults above 60 years with T2DM |
| Intervention (exposure) | Any physical activity or exercise intervention in which technology was a method of delivery∗ (only studies using mobile phones, tablets, computers, or physical activity trackers were included) |
| Comparison | Any physical activity/exercise not delivered through a digital technology or no intervention |
| Outcomes | Health-related outcomes (physical activity-related outcomes and clinical outcomes) |
| Exclusion | |
| Language | Other than English |
| Publications | Observational study design (case-control, prospective cohort, cross-sectional, and retrospective cohort studies) |
Study selection
The first and second authors (TA and UUN) independently searched the literature. Rayyan software (https://www.rayyan.ai/) was used to remove duplicates and screen the exported citations. All authors (TA, UUN, MMK, and GAM) reviewed the titles and abstracts to determine eligibility. The studies were included according to the selection criteria in Table 1. The first and second authors (TA and UUN) screened the included studies, which were then reviewed and discussed by all authors (TA, UUN, MMK, and GAM).
Data extraction
Each author conducted the data extraction process separately by using an Excel spreadsheet. Several components from the studies were extracted and examined. The data chart consisted of the author's name, year, journal, study design, country, objective, sample size, population, type of digital technology device, study setting, duration of the intervention, outcome measures, type of physical activity, outcome of the study, facilitators of digital technology use, and barriers to digital technology use. All authors validated the data extraction components and resolved any discrepancies through discussions, which further improved the extracted information.
Critical appraisal of the articles
The randomized controlled trials (RCTs) were evaluated with the JBI appraisal tool, which assesses the risk of bias in RCTs. For non-randomized controlled studies, the JBI checklist for quasi-experimental designs was used to evaluate the risk of bias. The critical assessment considered the proportion of positive responses. Articles were classified as having a low risk of bias if their score was at least 70%, a moderate risk of bias if their score was 50%–69%, and a high risk of bias if their score was less than 49%.14,15
Collecting, summarizing, and reporting of the results
A flowchart was used to illustrate the flow of this review, showing the total number of articles excluded and the reasons for exclusion throughout the review. The text and tables provide a descriptive summary of the study objectives, sample size, country, study design, author, and publication year (Table 2). To address the research question, several tables were created containing the following data: the type of digital technology device used, study setting, intervention duration, outcome measures, type of physical activity, study outcome, and facilitators of, and barriers to, the use of digital technology (Table 3).
Table 2.
Study characteristics.
| No. | Author name; year | Country | Study design | Objective | Sample size and population |
|---|---|---|---|---|---|
| 1 | Louise Poppe et al., 2019.19 | Belgium | Randomized controlled trial | To test the efficacy of the MyPlan 2.0 app in altering behavioral determinants and behavior in individuals with T2DM | 54; older adults with T2DM |
| 2 | Morwenna Kirwan et al., 2022.18 | Australia | Pre-post evaluation design | To evaluate whether the beat it online program enhances physical fitness and decreases waist size in older adults with T2DM | 171; older adults 60–89 years of age |
| 3 | Michelle Dugas et al., 2018.16 | United States | Randomized controlled trial | To explore mobile health in motivating lifestyle change among older veterans. | 29; older adults 61–86 years of age |
| 4 | Chenglin Sun et al., 2019.21 | China | Randomized controlled trial | To investigate the use of mobile phone health applications for the management of older Chinese adults with T2DM | 91; older adults above 65 years of age with T2DM |
| 5 | Rozmin Jiwani et al., 2022.17 | USA | Single-arm, intervention study | To examine whether a lifestyle intervention combined with mobile health technology for self-monitoring might decrease frailty in older adults who are overweight or obese, and have T2DM | 20; older adults above 65 years of age with T2DM |
| 6 | Kexin Yu et al., 2020.22 | Taiwan | Single arm, feasibility study | To test the efficacy of a mobile health intervention for older adults with T2DM in rural Taiwan | 97; patients with T2DM 55 years of age or above |
| 7 | João Balsa et al., 2020.20 | Portugal | Intervention study | To describe the prototype's features and evaluate its utility | 11; older adults with T2DM and 9 experts |
Table 3.
Effects of digital technology-based physical activity promotion.
| No. | Author name; year | Study setting | Duration | Outcome measures | Type of physical activity/exercise | Outcome of the study |
|---|---|---|---|---|---|---|
| 1. | Louise Poppe et al., 2019.19 | Home | 5 weeks |
Primary outcomes:
|
Physical activity incorporated into activities of daily living | RCT 1: The PA intervention group showed a decrease in self-reported sitting time (p = 0.09) and an improvement in accelerometer-measured moderate (p= 0.05) and moderate-to-vigorous PA (p = 0.049). The sedentary behavior intervention group showed more breaks from sedentary time, as measured by accelerometers, than the control group (p = 0.005). The intervention group showed a marginal improvement in action planning outcome (p = 0.08). |
| 2. | Morwenna Kirwan et al., 2022.16 | Home-based exercise | 8 weeks |
|
Dynamic warm-up and cool-down; aerobic, strength, and flexibility activities | The 8-week program resulted in significant improvements in participants' waist sizes, aerobic fitness, muscular strength, flexibility, and balance, in both men and women (all p < 0.001). |
| 3. | Michelle Dugas et al., 2018.18 | Home | 13 weeks |
|
Not reported | Participants with high adherence experienced an average 1.0-point decrease in glycated hemoglobin from the start to the end of the study, after accounting for age and treatment condition. |
| 4 | Chenglin Sun et al., 2019.21 | Home-based | 6 months |
|
|
|
| 5. | Rozmin Jiwani et al., 2022.17 | Community/home | 6 months |
|
|
|
| 6. | Kexin Yu et al., 2020.22 | Community/home | 12 weeks |
|
General physical exercise and physical activity | A specific diet and exercise program resulted in improved self-care behaviors at 4 months. However, the improvements in exercise, blood glucose monitoring, and diet were not maintained at the 8-month follow-up. |
| 7. | João Balsa et al., 2020.20 | Community/home | 26 days for older adults; 8–10 days for experts |
|
Not reported |
|
Results
We initially identified 3252 articles across six databases. After removal of 585 duplicates, 2667 articles remained. Further screening of titles and abstracts led to the exclusion of 2474 irrelevant articles. Consequently, 193 articles were assessed for eligibility, and 186 were excluded for not meeting the criteria. Ultimately, only seven articles met the selection criteria and were included in the review (Figure 1).
Figure 1.
PRISMA 2020 Flowchart.
Characteristics of the studies
Study characteristics included study objectives, sample size, study design, sample techniques, and study country of origin. All seven articles reported studies from high-income economy countries or upper and middle-income countries [USA (n = 2)16, 17; Australia (n = 1)18; Belgium (n = 1)19; Portugal (n = 1) 20; China (n = 1)21; and Taiwan (n = 1)22]. All studies were conducted between 2018 and 2022. The included literature consisted of seven research articles (n = 7), all of which reported receiving funding support.
All studies included were interventional studies: three were RCTs,18,19,21 whereas the others had pre-post evaluation, single-arm interventional, single-arm feasibility, and interventional study designs.17,18,20,22 The number of included participants in all seven studies ranged from 11 to 171.
Features of participants and studies
Participants in the included studies were 50 years of age or older. Two studies in adults over 50 years of age were included, because the studies focused on older adults.19,22 Smartphone apps were the preferred type of digital technology and were used in all studies.17 One study used a Fitbit wrist activity tracker and a smartphone app, whereas another used a website or web platform and an optional mobile app.19 Only one study reported a specific exercise protocol with warm-up, cool-down, and aerobic, resistance, and flexibility components.20 Another study described activities of daily living as the physical activity.19 Two studies did not specify the type of physical activity or exercise.18,20 All other studies included a general physical activity or exercise program.
Findings of the studies
Key concept 1: features of digital technology
One study used a website or mobile app to encourage users to set, maintain, and follow their physical activity and sedentary behavior goals, and to provide daily support.19 Three studies used smartphone apps for physical activity promotion.16,20,21 Another study used a wristband activity tracker and a mobile app for self-monitoring of diet and activity.15 Two studies used mobile apps: one incorporating clinician and peer engagement features and the other providing a diabetes self-management app for tablet use.16,22
Key concept 2: duration of intervention
The intervention durations ranged from 26 days20 to 6 months.17,21 Two RCTs reported an intervention duration of 6 months.17,21 Another RCT reported an intervention duration of 5 weeks.19 Two studies, one of which was an RCT, reported a 13 week intervention duration.16 A single-arm feasibility study reported a 12 week intervention duration, whereas a similar study reported a duration of 8 weeks. Another usability study of a mobile health app had a duration of 26 days.20
Key concept 3: type of physical activity delivered
The studies used digital technology to deliver content, in which physical activity or exercise was a commonly included component. One study used a website and optional mobile app that provided physical activity suggestions in the form of daily activities and tips to promote an active lifestyle.19 Another study used a smartphone app with clinician features to deliver a structured home-based exercise program requiring minimal equipment.16 The program included warm-up, cool-down, aerobic, resistance, balance, and flexibility exercises. Similarly, a mobile app provided daily caloric expenditure information and guidance on resistance and aerobic exercises. Another study used a Fitbit activity tracker and app for diet and activity monitoring, which trained participants to achieve and maintain 175 min of physical activity per week over 6 months.17 A separate study used a diabetes self-management app to provide general exercise and physical activity.20 However, two similar studies did not specify the type of physical activity or exercise delivered through digital technology.16,20
Key concept 4: outcome measures
The studies examined a range of outcome measures, including diabetes-related assessments and physical activity-specific metrics. One study used the long Dutch version of the International Physical Activity Questionnaire (IPAQ) to evaluate physical activity and the Longitudinal Aging Study Amsterdam (LASA) questionnaire to assess sedentary behavior.17 Another study reported using various physical fitness assessments, such as the 30-s seated arm curl test (upper limb muscle strength), 30-s sit-to-stand test (lower limb muscle strength), seated sit-and-reach test (flexibility), one-legged stand test (balance), and 2-min step test (aerobic capacity), along with two questionnaires: the Diabetes Empowerment Scale (DES) and the Patient Activation Measure (PAM).18 The Short Physical Performance Battery (SPPB), including a 4-m walk test, time to complete five repeated chair stands without using the hands, and standing balance tests, was combined with questionnaires measuring quality of life, such as the Patient Reported Outcomes Measurement Information System-57 (PROMIS-57) and the Patient Reported Outcomes Measurement Information System (PROMIS) Global Health and Mental Health, as reported in a similar study.17 Likewise, evaluation of diabetes symptoms with the Self-Completion Patient Outcome Instrument (SCPOI) and self-care behaviors (e.g., blood glucose testing, exercise, and diet) in patients with diabetes with the Summary of Diabetes Self-Care Activities (SDSCA) was reported in another study.22 Measurement of glycated hemoglobin (HbA1c) was reported in three studies.16,17,21 Other outcome measures reported across studies included lipid profile and blood pressure.21
Key concept 5: facilitators of, and barriers to, the use of digital technology
Only one study identified technically challenged health professionals as the most common barrier to implementing digital health interventions, whereas the other studies did not report similar barriers.18 Several studies found various factors facilitating the use of mobile health apps, such as a streamlined interface and a goal-oriented approach, which increased adherence. However, other studies did not identify any additional facilitators.16
Key concept 6: study setting and effect of intervention on outcomes
Seven studies were conducted in community or home settings. Participants, regardless of their sex, showed improved aerobic fitness, waist size, muscle strength, balance, and flexibility after an 8-week smartphone-based exercise program (p < 0.001).18 One study used a website or web platform with an optional mobile app (a website encouraging users to set, adhere to, and sustain personal goals for sedentary behavior and physical activity in a group) combined with an optional mobile app providing daily support. The physical activity intervention group showed less time spent sitting (p = 0.09), along with more moderate (p = 0.05) and moderate-to-vigorous (p = 0.049) physical activity, as evaluated with accelerometers. The sedentary behavior intervention group showed a greater increase in accelerometer-assessed breaks compared to the physical activity intervention group (p= 0.005).19 A study among older United States veterans found high adherence to self-reported medication, exercise, diet, and blood glucose monitoring. That study used a mobile app with features for interacting with peers and clinicians. The average HbA1C level decreased by 1.0 points after the intervention. However, the HbA1C level decreased only 0.48 points, for individuals with moderate adherence. Finally, no significant change in HbA1C levels was observed before versus after the intervention among participants with poor adherence.16 Another study used a mobile health app and reported that the HbA1c level was considerably lower in the intervention group than that observed at baseline (mean = 6.84% [SD = 0.765%] vs. mean = 7.84% [SD = 0.73%], p < 0.001) and that observed in the control group at 6 months (mean = 6.84% [SD = 0.765%] vs. mean = 7.22% [SD = 0.87%], p = 0.02). In the intervention group, postprandial blood glucose levels showed improvements over baseline levels after 6 months (mean = 10.62 [SD = 2.07] mmol/L vs. mean = 13.10 [SD = 4.13] mmol/L, p = 0.002).21 The study involved frail older adults with T2DM. Participants were provided with a Fitbit wristband activity tracker and mobile app for self-monitoring. At baseline, 72% of participants were pre-frail, 22% were frail, and 6% were not frail. At the follow-up, the mean body weight increased from 205.66 [SD = 45.52] lb. to = 198.33 [SD = 43.6] lb. (p ≤ 0.001), and the mean frailty scores decreased considerably, from 1.61 [SD = 1.15] to 0.94 [SD = 0.94] (p = 0.01). No changes were seen in the PROMIS-57 questionnaire results after the intervention (p-value >0.05), but slight changes were observed in the mean PROMIS-Global health questionnaire results (42.63 [SD = 6.37] to 44.25 [SD = 6.77]) and (48.87 [SD = 9.03] to 51.69 [SD = 6.46]), respectively.17 A study among older patients with T2DM in rural Taiwan examined the long-term effects of a mobile health program and observed improvements in exercise behaviors (0.68 days/week increase, 95% CI, 0.14 to 1.22, P < 0.05) after 4 months.22
Critical appraisal of the studies
Two RCTs reported a high risk of bias, and one RCT reported a moderate risk of bias21 (Table 4). Meanwhile, among non-RCTs, a high risk of bias was reported in three studies,17,20,22 and a moderate risk of bias was reported in one study18 (Table 5).
Table 4.
JBI Critical Appraisal for risk of bias assessment for randomized controlled trials.14
| No. | Author name; year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Score | Responses of ‘Yes’ | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Louise Poppe et al., 2023.18 | Yes | No | Yes | No | No | Unclear | No | No | Yes | Unclear | Yes | Yes | Yes | 6 | 46 % | High |
| 2. | Michelle Dugas et al., 2018.15 | Yes | No | Yes | No | No | No | No | No | Unclear | Unclear | Yes | Yes | Yes | 5 | 38 % | High |
| 3. | Chenglin Sun et al., 2019.20 | Yes | Yes | Yes | Unclear | Unclear | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | 9 | 69 % | Moderate |
Table 5.
JBI Critical Appraisal for risk of bias assessment for non-randomized experimental studies.15
| No. | Author name; year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total | Responses of ‘Yes’ | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Rozmin Jiwani et al., 202116 | Yes | No | No | No | Yes | Yes | No | Unclear | Yes | 4 | 44 % | High |
| 2. | Morwenna Kirwan et al., 2022.17 | Yes | No | No | No | Yes | Yes | No | Yes | Yes | 5 | 56 % | Moderate |
| 3. | Yu et al., 2020.21 | Yes | No | No | No | Yes | Yes | No | Unclear | Yes | 4 | 44 % | High |
| 4. | João Balsa et al., 2020.20 | Yes | No | No | No | Yes | No | No | Unclear | Yes | 3 | 33 % | High |
Discussion
This review examined digital technology interventions for older adults. We used broad inclusion criteria to identify both quasi-experimental and experimental studies measuring objective or self-reported outcomes in older populations. We found that most interventions used a standalone mobile app, sometimes with an activity tracker or website, and reported improved outcomes. The studies were conducted in high-income countries, whereas no low- or middle-income countries were represented—an interesting but expected finding. The use of mobile health apps in developing nations has been poorly studied, thus leading to limited effects of these apps. Key challenges in using mobile phone apps for diabetes care in low- and middle-income countries include a lack of funding, difficulty in engaging patients, educating healthcare providers, lack of infrastructure, and adherence to the interventions.20,23
Many studies have shown the effectiveness of mobile technologies in glycemic control and improvement in diabetes management, with high acceptance rates among patients and general practitioners. A mobile app for older diabetic patients has been developed to facilitate self-care, including easy entry of blood glucose levels and reminder alarms for medication administration.24 A study in the United Kingdom has examined digital technology approaches to engage older adults in strength and balance exercises. The study's detailed and thorough evaluation suggested that high-quality mobile apps and websites might potentially replace in-person interventions. However, whether the same results might apply to low- and middle-income countries remains unclear. Features such as in-app discussion forums and video consultations appear to support the level of interaction quality in digital technology interventions.25
The intervention duration of the seven studies varied from 26 days to 6 months. Digital physical activity interventions are most effective when implemented for more than 1 month or 8 weeks. The benefits of the intervention tend to be greatest in the initial few months and subsequently diminish over time.26,27, 28 To better understand how older individuals with T2DM use digital health technologies, including their motivations, use patterns, and the technologies’ effects, long-term studies focusing on barriers to technology use would be beneficial.29
In this review, most studies (five of seven) reported using physical activity promotion strategies, and only two studies incorporated a structured exercise program into a mobile phone app. The studies indicated improvements in the measured outcomes. The research effectively analyzed the use of smartphones for remote patient monitoring, thus demonstrating the viability of this technology in routine healthcare. This technology might decrease healthcare costs by enabling remote monitoring and early detection of worsening conditions.30 Mobile phone apps have the potential to provide customized feedback and integrate lifestyle behavioral change techniques.31
The review examined various metrics, including those associated with physical activity and diabetes. However, no studies collected data through mobile apps. Using mobile apps to gather patient data could help healthcare providers T2DM more systematically and effectively. Continuous data collection might benefit patients, and contribute to progress in healthcare and public health.32
The studies explored using smartphones for remote patient monitoring. The results showed this technology is suitable for routine healthcare, and may potentially lower costs by enabling remote monitoring and early detection of worsening conditions. Clinicians using this technology could identify functional decline and prompt early interventions, thus decreasing the time to before receipt of care and increasing patient involvement in managing their health.33,34 Digital technologies are therefore helpful for older adults with T2DM. One study has found no difference between remote care and in-person care after 3 months, but has indicated improvements in blood glucose levels after 6 months, particularly among women over 40 years of age.35 Further research has indicated that technology-based programs can successfully boost physical activity levels.36 Mobile apps, internet tools, and wearable devices have been demonstrated to be effective in increasing physical activity and decreasing sedentary time.37
The strengths of this study include the comprehensive search of six databases, thus supporting identification of a wide range of relevant articles. Additionally, the lack of timeframe restrictions strengthened the literature review. Furthermore, this study is, to our knowledge, the first scoping review of the literature on the use of digital technology for physical activity and exercise in older adults with T2DM.
This study has several limitations. First, it considered only articles published in electronic databases. Second, it included only articles with full text available, and excluded abstracts and conference proceedings. Third, it included only studies and search terms in English, and consequently might have missed relevant research in other languages. Fourth, it focused solely on digital technologies, such as mobile apps, websites, and activity trackers, without evaluating virtual reality or artificial intelligence. Fifth, although the inclusion criteria targeted older adults over 60 years of age, two relevant studies with adults over 50 and 55 years of age were included, because the target population in both studies was older adults with T2DM who used a mobile app for a physical activity intervention.
Future recommendations
Future research may explore the effects of mobile apps, and help clinicians choose more effective techniques or combinations. Further investigation is needed to develop strategies to achieve long-term, sustained improvements in older adults’ physical activity levels and determine the most effective follow-up to maximize adherence to digital physical activity interventions. Additional research is necessary to understand the health needs or barriers related to using digital health technology in low-income countries and to improve the use of digital initiatives to promote physical activity in older adults in these communities.
Conclusion
In conclusion, this review highlights the major role of digital technology in promoting physical activity among older adults with T2DM. Specifically, smartphones have emerged as a frequently used and effective tool for delivering physical activity interventions to this demographic.
Source of funding
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This scoping review did not require ethics committee approval.
Consent
Not applicable.
Author contributions
TA and GAM conceived and designed this scoping review. TA and UUN performed searches and collated the articles. TA, UUN, MMK, and GAM analyzed and interpreted the data. TA and UUN wrote the initial manuscript draft, and GAM and MMK provided critical input and shaped the manuscript in its current form. All authors (TA, UUN, MMK, and GAM) critically reviewed and approved the final draft, and are responsible for the content and similarity index of the manuscript.
Availability of the data
All available data are presented in the study. The main data will be made available on reasonable request to the corresponding author.
Acknowledgments
We thank the Centre for Podiatry & Diabetic Foot Care and Research, Department of Physiotherapy, Manipal College of Health Professions (MCHP), Manipal Academy of Higher Education (MAHE), India, for knowledge sharing and research support enabling the completion of this review.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Gyasi R.M., Phillips D.R. Aging and the rising burden of noncommunicable diseases in sub-saharan Africa and other low- and middle-income countries: a call for holistic action. Gerontol. 2020 Jul 15;60(5):806–811. doi: 10.1093/geront/gnz102. [DOI] [PubMed] [Google Scholar]
- 2.Sun H., Saeedi P., Karuranga S., Pinkepank M., Ogurtsova K., Duncan B.B., et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022 Jan;183 doi: 10.1016/j.diabres.2021.109119. Epub 2021 Dec 6. Erratum in: Diabetes Res Clin Pract. 2023 Oct;204:110945. https://doi.org/10.1016/j.diabres.2023.110945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holt R.I.G., Speight J. The language of diabetes: the good, the bad and the ugly. Diabet Med. 2017 Nov;34(11):1495–1497. doi: 10.1111/dme.13520. [DOI] [PubMed] [Google Scholar]
- 4.Michie S., Yardley L., West R., Patrick K., Greaves F. Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. J Med Internet Res. 2017 Jun 29;19(6) doi: 10.2196/jmir.7126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korkiakangas E.E., Alahuhta M.A., Laitinen J.H. Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: a systematic review. Health Promot Int. 2009 Dec 1;24(4):416–427. doi: 10.1093/heapro/dap031. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention . CDC; 2022. National diabetes statistics report [Internet]https://www.cdc.gov/diabetes/data/statistics-report/index.html Available from: [Google Scholar]
- 7.Tee E.S., Yap R.W.K. Type 2 diabetes mellitus in Malaysia: current trends and risk factors. Eur J Clin Nutr. 2017 Jul;71(7):844–849. doi: 10.1038/ejcn.2017.44. [DOI] [PubMed] [Google Scholar]
- 8.Collado-Mateo D., Lavín-Pérez A.M., Peñacoba C., Del Coso J., Leyton-Román M., Luque-Casado A. Key factors associated with adherence to physical exercise in patients with chronic diseases and older adults: an umbrella review. Int J Environ Res Publ Health. 2021 Feb 19;18(4):2023. doi: 10.3390/ijerph18042023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stanford K.I., Goodyear L.J. Exercise and type 2 diabetes: molecular mechanisms regulating glucose uptake in skeletal muscle. Adv Physiol Educ. 2014 Dec;38(4):308–314. doi: 10.1152/advan.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United Nations . United Nations Sustainable Development Goals; United Nations: 2023. Goal 3: ensure healthy lives and promote well-being for all at all ages [Internet]https://www.un.org/sustainabledevelopment/health/ Available from: [Google Scholar]
- 11.Bonn S.E., Alexandrou C., Hjörleifsdottir Steiner K., Wiklander K., Östenson C.G., Löf M., et al. App-technology to increase physical activity among patients with diabetes type 2 - the DiaCert-study, a randomized controlled trial. BMC Publ Health. 2018 Jan 10;18(1):119. doi: 10.1186/s12889-018-5026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scoping Reviews Resources | Joanna Briggs Institute [Internet]. jbi.global. Available from: https://jbi.global/scoping-review-network/resources [accessed 19 March 2024].
- 13.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005 Feb 1;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 14.Hariton E., Locascio J.J. Randomised controlled trials - the gold standard for effectiveness research: study design: randomised controlled trials. BJOG. 2018 Dec;125(13):1716. doi: 10.1111/1471-0528.15199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barker T.H., Stone J.C., Sears K., Klugar M., Tufanaru C., Leonardi-Bee J., et al. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evid Synth. 2023 Mar 1;21(3):494–506. doi: 10.11124/JBIES-22-00430. [DOI] [PubMed] [Google Scholar]
- 16.Dugas M., Crowley K., Gao G.G., Xu T., Agarwal R., Kruglanski A.W., et al. Individual differences in regulatory mode moderate the effectiveness of a pilot mHealth trial for diabetes management among older veterans. PLoS One. 2018 Mar 7;13(3) doi: 10.1371/journal.pone.0192807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiwani R., Wang J., Li C., Dennis B., Patel D., Gelfond J., et al. A behavioral lifestyle intervention to improve frailty in overweight or obese older adults with type 2 diabetes: a feasibility study. J Frailty Aging. 2022;11(1):74–82. doi: 10.14283/jfa.2021.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirwan M., Chiu C.L., Laing T., Chowdhury N., Gwynne K. A web-delivered, clinician-led group exercise intervention for older adults with type 2 diabetes: single-arm pre-post intervention. J Med Internet Res. 2022 Sep 23;24(9) doi: 10.2196/39800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poppe L., De Bourdeaudhuij I., Verloigne M., Shadid S., Van Cauwenberg J., Compernolle S., et al. Efficacy of a self-regulation-based electronic and mobile health intervention targeting an active lifestyle in adults having type 2 diabetes and in adults aged 50 Years or older: two randomized controlled trials. J Med Internet Res. 2019 Aug 2;21(8) doi: 10.2196/13363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Balsa J., Félix I., Cláudio A.P., Carmo M.B., Silva I.C.E., Guerreiro A., et al. Usability of an intelligent virtual assistant for promoting behavior change and self-care in older people with type 2 diabetes. J Med Syst. 2020 Jun 13;44(7):130. doi: 10.1007/s10916-020-01583-w. [DOI] [PubMed] [Google Scholar]
- 21.Sun C., Sun L., Xi S., Zhang H., Wang H., Feng Y., et al. Mobile phone-based telemedicine practice in older Chinese patients with type 2 diabetes mellitus: randomized controlled trial. JMIR Mhealth Uhealth. 2019 Jan 4;7(1) doi: 10.2196/10664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu K., Wu S., Lee P.J., Wu D.A., Hsiao H.Y., Tseng Y.C., et al. Longitudinal effects of an intergenerational mHealth program for older type 2 diabetes patients in rural taiwan. Diabetes Educat. 2020 Apr;46(2):206–216. doi: 10.1177/0145721720907301. [DOI] [PubMed] [Google Scholar]
- 23.Bahendeka S. Implementing digital systems in diabetes care in low-income and middle-income countries: successes and challenges. Lancet Diabetes Endocrinol. 2023 Jun;11(6):387–388. doi: 10.1016/S2213-8587(23)00117-1. [DOI] [PubMed] [Google Scholar]
- 24.Hester J., Zabala Z., Winskell K., Pasquel F.J. Diabetes digital health and Telehealth. Academic Press; 2022. Digital health apps for people with diabetes; pp. 101–118. [Google Scholar]
- 25.McGarrigle L., Boulton E., Todd C. Map the apps: a rapid review of digital approaches to support the engagement of older adults in strength and balance exercises. BMC Geriatr. 2020 Nov 18;20(1):483. doi: 10.1186/s12877-020-01880-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Q., Egelandsdal B., Amdam G.V., Almli V.L., Oostindjer M. Diet and physical activity apps: perceived effectiveness by app users. JMIR Mhealth Uhealth. 2016 Apr 7;4(2):e33. doi: 10.2196/mhealth.5114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schoeppe S., Alley S., Van Lippevelde W., Bray N.A., Williams S.L., Duncan M.J., et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Activ. 2016 Dec 7;13(1):127. doi: 10.1186/s12966-016-0454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Romeo A., Edney S., Plotnikoff R., Curtis R., Ryan J., Sanders I., et al. Can smartphone apps increase physical activity? Systematic review and meta-analysis. J Med Internet Res. 2019 Mar 19;21(3) doi: 10.2196/12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wegener E.K., Kayser L. Smart health technologies used to support physical activity and nutritional intake in fall prevention among older adults: a scoping review. Exp Gerontol. 2023 Oct 1;181 doi: 10.1016/j.exger.2023.112282. [DOI] [PubMed] [Google Scholar]
- 30.Ashton L.M., Hutchesson M.J., Rollo M.E., Morgan P.J., Collins C.E. Motivators and barriers to engaging in healthy eating and physical activity. Am J Men's Health. 2017 Mar;11(2):330–343. doi: 10.1177/1557988316680936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Middelweerd A., Mollee J.S., van der Wal C.N., Brug J., Te Velde S.J. Apps to promote physical activity among adults: a review and content analysis. Int J Behav Nutr Phys Activ. 2014 Jul 25;11:97. doi: 10.1186/s12966-014-0097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Epis O.M., Casu C., Belloli L., Schito E., Filippini D., Muscarà M., et al. Pixel or paper? Validation of a mobile technology for collecting patient-reported outcomes in rheumatoid arthritis. JMIR Res Protoc. 2016 Nov 16;5(4) doi: 10.2196/resprot.5631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arora S., Venkataraman V., Zhan A., Donohue S., Biglan K.M., Dorsey E.R., et al. Detecting and monitoring the symptoms of Parkinson's disease using smartphones: a pilot study. Parkinsonism Relat Disorders. 2015 Jun;21(6):650–653. doi: 10.1016/j.parkreldis.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 34.Lein DH Jr, Willig J.H., Smith C.R., Curtis J.R., Westfall A.O., Hurt C.P. Assessing a novel way to measure three common rehabilitation outcome measures using a custom mobile phone application. Gait Posture. 2019 Sep;73:246–250. doi: 10.1016/j.gaitpost.2019.07.251. [DOI] [PubMed] [Google Scholar]
- 35.Cho J.H., Kim H.S., Yoo S.H., Jung C.H., Lee W.J., Park C.Y., et al. An Internet-based health gateway device for interactive communication and automatic data uploading: clinical efficacy for type 2 diabetes in a multi-centre trial. J Telemed Telecare. 2017 Jul;23(6):595–604. doi: 10.1177/1357633X16657500. [DOI] [PubMed] [Google Scholar]
- 36.Fanning J., Mullen S.P., McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012 Nov 21;14(6):e161. doi: 10.2196/jmir.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stephenson A., McDonough S.M., Murphy M.H., Nugent C.D., Mair J.L. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Activ. 2017 Aug 11;14(1):105. doi: 10.1186/s12966-017-0561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]