Abstract
After the outbreak of the novel coronavirus at the end of December 2019 in China, it has become a global pandemic. Clinical manifestation of coronavirus disease 2019 (COVID-19) has a wide range of presentations from asymptomatic to severe multi-organ involvement. Hemoptysis appears to be one of the major manifestations of severe acute respiratory syndrome that is related to COVID-19 infection. The occurrence of hemoptysis is multifactorial. However, massive hemoptysis is usually related to pulmonary aspergillosis or severe bronchiectasis due to corticosteroid pulse therapy that can be life-threatening. This manuscript presents five cases of successful life-saving bronchial artery embolization in patients with COVID-19 infection who were suffering from massive hemoptysis that was mostly related to aspergillosis and bronchiectasis. These cases are followed by a review of the literature.
Keywords: SARS-Cov-2, invasive pulmonary aspergillosis, angioembolization, bronchiectasis, polyvinyl alcohol, embolization, hemoptysis
After the outbreak of the novel coronavirus at the end of December 2019 in Hubei Province, China, it has become a global pandemic. 1 Clinical manifestation of coronavirus disease 2019 (COVID-19) has a wide range of presentations from asymptomatic status to severe multiorgan involvement including acute respiratory distress syndrome (ARDS) in 33% and death in 16% of hospitalized patients. 2 Fever (89.1%), cough (72.2%), myalgia, and fatigue (42.5%) are the common symptoms, and hemoptysis seems to be an atypical manifestation of severe acute respiratory syndrome occurring in the setting of coronavirus-2 (SARS-CoV-2) infection. 3 Hemoptysis is defined as coughing blood or bloody sputum from the respiratory tract including the trachea and bronchi. 4 5 The most common causes of hemoptysis are acute and chronic bronchitis, bronchiectasis, pneumonia, tuberculosis, and lung cancer. However, in patients with COVID-19 infection, diffuse alveolar damage with intra-alveolar hemorrhage and necrosis of parenchymal cells may lead to lung cavitation and hemoptysis. 6 7 Recently, new studies have revealed a 3% hemoptysis rate in a large cohort of confirmed COVID-19 patients. 8
While high-dose corticosteroid pulse therapy (HDCPT) has shown a reducing effect on the mortality rate in severe COVID-19 patients, opportunistic infections such as aspergillosis have emerged as a manifestation of this severe immunosuppression. The overall incidence of COVID-19-associated pulmonary aspergillosis (CAPA) has been reported to be 13.5%, ranging between 2.5 and 35.0%. 9
Aspergillosis is one of the most common causes of massive hemoptysis in developed countries. 10 Clinically, aggressive pulmonary aspergillosis presents as acute non-specific pneumonia with cough, chest pain, and fever and can become life-threatening with the occurrence of massive hemoptysis. 11
In the case of massive hemoptysis, emergency treatment of the underlying cause can be life-saving. After resuscitation and airway protection, bronchial artery embolization (BAE) is a minimally invasive procedure and is the treatment of choice in critically ill patients suffering from life-threatening hemoptysis. 12 13 The safety and effectiveness of BAE for massive hemoptysis have been proven since its first use in 1973. Currently, biocompatible polyvinyl alcohol (PVA) particles and other non-biodegradable materials are commonly used for BAE worldwide. 14 15 In this manuscript, we present five cases of BAE using PVA in post-COVID-19 patients suffering from massive hemoptysis.
Case Presentation
Case 1
A 69-year-old male was admitted to the emergency department (ED) with fever, cough, and hemoptysis (approximately 200cc). He had an oxygen saturation of 89%. He had a history of diabetes, hypertension, and hypothyroidism. Six weeks before his presentation, he had been treated for COVID-19 infection and received remdesivir, corticosteroids, and aspirin therapy. He was admitted to the intensive care unit (ICU). His chest computed tomography (CT) scan revealed cavities in his left lung suggestive of fungus balls with a honeycombing appearance of both lungs ( Fig. 1 ). Laboratory findings revealed a low hemoglobin level of 9 mg/dL and an increase in partial thromboplastin time and INR level. The patient had persistent severe hemoptysis. Therefore, angiography and BAE ( Figs. 2 and 3 ) on his left bronchial artery were successfully performed leading to the resolution of his hemoptysis. The patient remained hemodynamically stable without further hemoptysis.
Fig. 1.
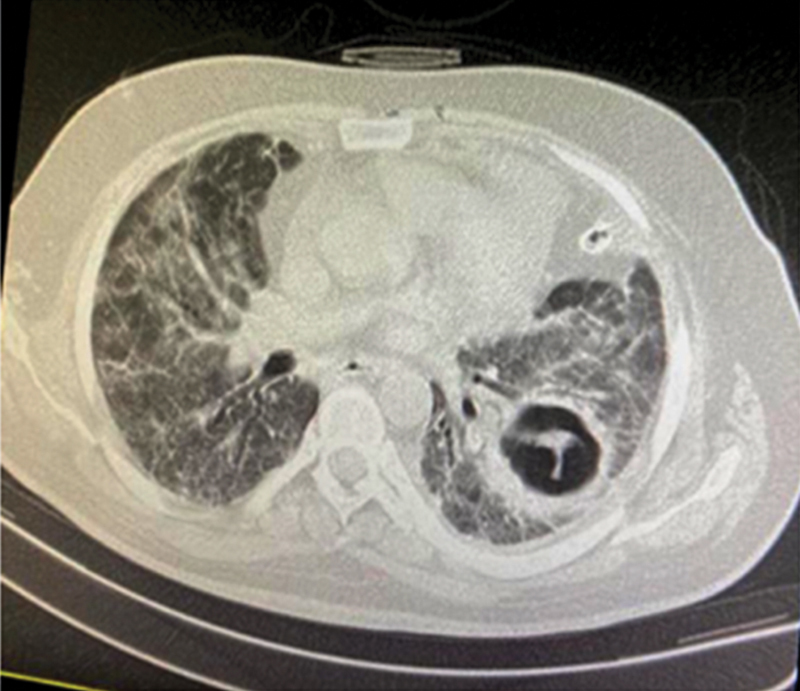
Fungus ball cavity is seen on the CT scan.
Fig. 2.

Angiogram showing arterial supply of the bleeding source.
Fig. 3.

Successful bronchial angioembolization.
Case 2
A 67-year-old male with a history of diabetes, hypertension, chronic kidney disease, ischemic heart disease, and coronary artery bypass graft surgery was admitted to the ICU with cough, dyspnea, and hemoptysis that had started 3 days earlier. Seven weeks prior to admission, he was diagnosed and treated for COVID-19 infection by HDCPT. He had a stable vital sign with an oxygen saturation of 93%. His physical exam revealed a crackling sound in both lungs. His chest CT scan showed a cavity with an air-fluid level in his right lung ( Fig. 4 ). His sputum culture was positive for klebsiella and the polymerase chain reaction (PCR) test for Aspergillus. Three days later, his hemoptysis became massive leading to hemodynamic instability with a drop of his hemoglobin level to 9.1 (mg/dL). Urgent BAE was performed on his right bronchial artery resolving further episodes of hemoptysis. The patient's condition improved and was discharged a few days later.
Fig. 4.
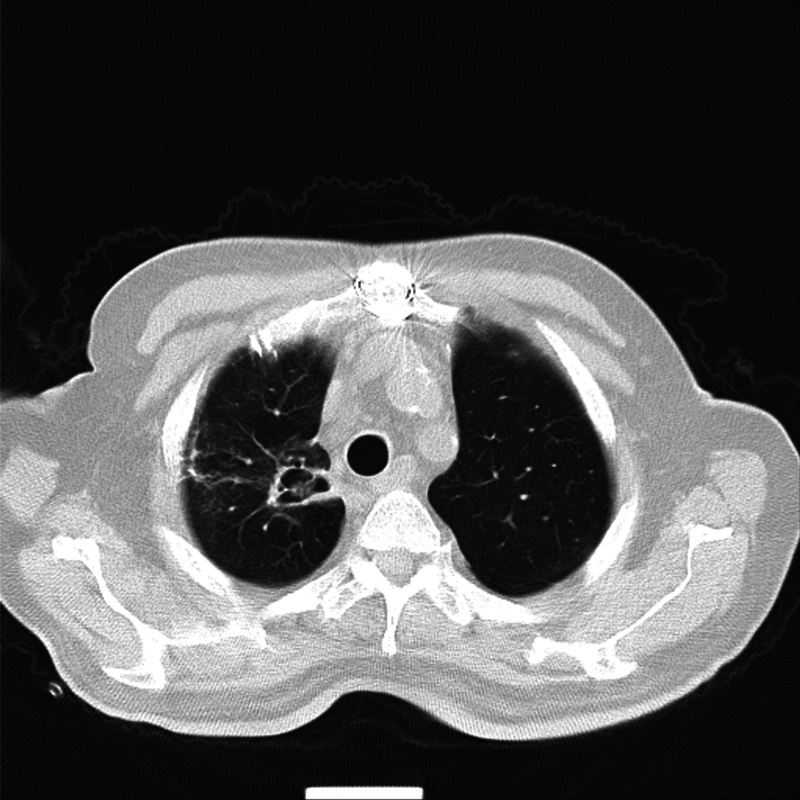
Cavity with an air-fluid level in the right lung.
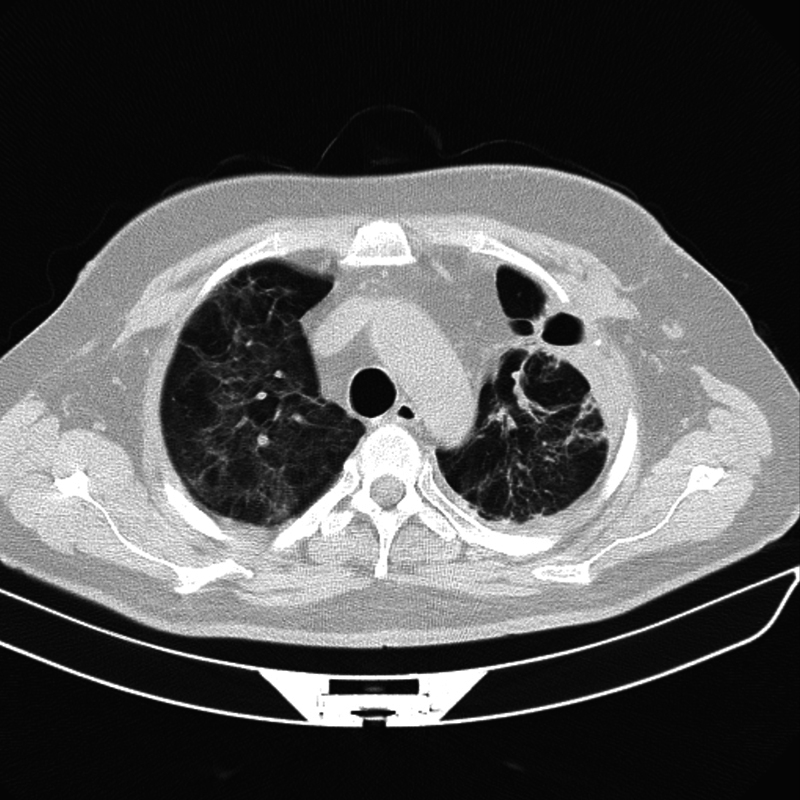
Case 3
A 66-year-old female with a history of diabetes, hypertension, and ischemic heart disease was referred for BAE due to massive hemoptysis (approximately 1 L) with an oxygen saturation of 83% and crackles sound in her both lungs. Four weeks earlier, she was treated by HDCPT because of a COVID-19 infection. Her thoracic CT scan revealed diffuse bilateral ground-glass opacities with consolidations and fungus balls ( Fig. 5 ). The patient underwent successful emergent BAE of a bifurcating bronchial artery with a complete resolution of her hemoptysis.
Fig. 5.

Diffuse bilateral ground-glass opacities with consolidations and fungus ball.
Case 4
A 44-year-old male presented to the ED with dyspnea and chest pain. He had been treated for COVID-19 infection 6 weeks earlier using remdesivir and tocilizumab. His oxygen saturation was 86% at rest. His physical examination revealed decreased sounds in his left lung. Subcutaneous emphysema was detected suggestive of pneumothorax ( Fig. 6 ). Therefore, a chest tube was inserted immediately and he was transferred to the ICU. A week later, massive hemoptysis abruptly developed and his hemoglobin level decreased dramatically from 13.8 to 8 (mg/dL) within 2 days. The patient underwent successful BAE on his right and left and bifurcated bronchial arteries with the resolution of his hemoptysis.
Fig. 6.
Post-COVID-19 pneumothorax.
Case 5
A 55-year-old male with a history of pulmonary thromboembolism presented to the ED with dyspnea, reduced oxygen saturation, and a positive COVID-19 PCR test. His thoracic CT scan revealed bilateral patchy areas of ground-glass infiltrates without any sign of fungal infection. He was admitted to the ICU and received treatment with tocilizumab and methylprednisolone. On the 10th day of admission, he suffered from massive hemoptysis (approximately 300cc) related to bronchiectasis ( Fig. 7 ) due to COVID-19 infection. The patient underwent successful urgent BAE of his large right bronchial artery with the resolution of his symptoms.
Fig. 7.
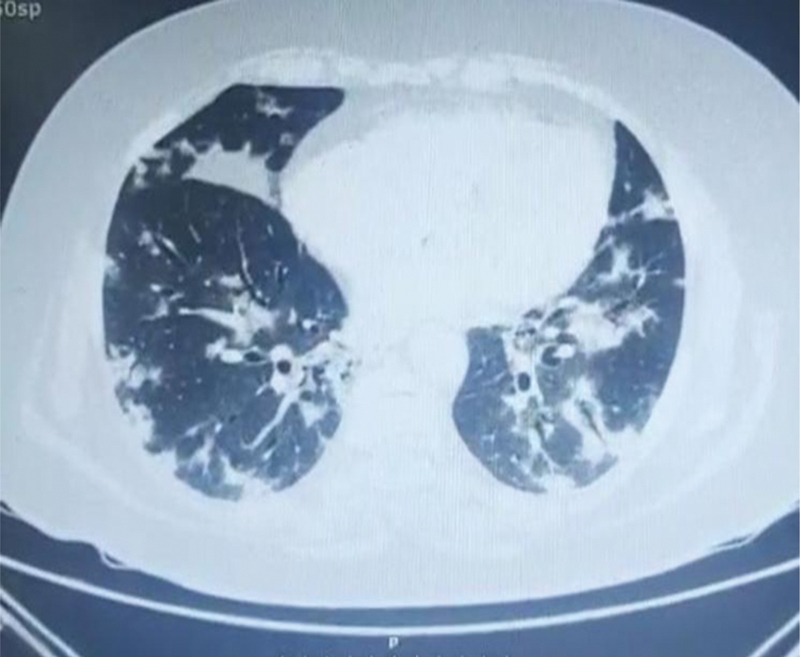
Bronchiectasis in a COVID-19 patient is seen on the CT scan.
Discussion
Our manuscript presented five cases of successfully treated angioembolization for massive hemoptysis in patients with a post-COVID-19 infection that has led to aspergillosis and bronchiectasis ( Table 1 ). All patients had successful resolution of their hemoptysis after the procedure and were symptom-free thereafter for at least 4 months (four out of five patients). One patient passed away because of severe post-COVID-19 complications and multi-organ failure.
Table 1. Patient's characteristics.
| Cases | Age | Sex | Past medical history | Underlying causes of hemoptysis | Time from COVID 19 diagnoses to hemoptysis | Chest CT imaging characteristics | Side of BAE | The number of pathologic vessels | Admission setting |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 69 | Male | Diabetes Hypertension Hypothyroidism |
Aspergillosis | 6 wk | The honeycombing appearance of both lungs | Left bronchial artery | One | ICU |
| Case 2 | 67 | Male | Diabetes Hypertension Chronic kidney disease Ischemic heart disease |
Aspergillosis | 7 wk | Cavity with an air-fluid level in the right lung | Right bronchial artery | One | ICU |
| Case 3 | 66 | Female | Diabetes Hypertension Ischemic Heart disease |
Aspergillosis | 4 wk | Diffuse bilateral ground-glass opacities with limited consolidations | Bifurcated bronchial artery | Two | ICU |
| Case 4 | 44 | Male | Negative | Negative | 6 wk | Subcutaneous emphysema suggestive of pneumothorax | Both right and left and bifurcated bronchial artery | Four | ICU |
| Case 5 | 55 | Male | Pulmonary thromboembolism | Bronchiectasis | 10 d | Bilateral patchy areas of ground-glass infiltration | Right bronchial artery | One | ICU |
Abbreviations: BAE, bronchial artery embolization; Chest CT, chest computed tomography; COVID-19, coronavirus disease 2019; ICU, intensive care unit.
Note: The number of pathologic vessels = the number of involved vessels.
According to previous studies, the most important causes of hemoptysis are bronchiectasis, lung cancer, bronchitis, and pneumonia. In our case series, we are reporting the largest case series of successful BAE performed in COVID 19 patients presenting with massive hemoptysis due to complications of high-dose corticosteroids or immune-suppressive therapy that had led to aspergillosis infection-related bronchiectasis. 6 7
Several isolated case reports have been described successfully treated COVID-19 associated hemoptysis in the acute or convalescent phase with BAE. Murgo et al describe a case of COVID-9-related pneumonia with severe hemoptysis successfully treated with BAE. Their experience suggests that the treatment of severe hemoptysis by BAE is feasible and effective. 16 In another report, a 58-year-old man presented at the ED with acute onset of massive hemoptysis with prominent alveolar hemorrhage in his left lung. Bronchial arteriography from the left upper lobe revealed the source of bleeding that was successfully embolized. Surprisingly, nasopharyngeal swabs tested for SARS-CoV-2 using real-time PCR were repeatedly negative. However, eventually, SARS-CoV-2 was detected in bronchoalveolar lavage (BAL). This case emphasizes the added value of bronchoscopy with BAL in the diagnostic work-up of COVID-19 infection in cases with high clinical suspicion despite negative nasal swap testing. 17
Koehler et al 18 performed a retrospective chart review of patients with COVID-19 and ARDS admitted to the medical and surgical ICU. They found that COVID-19-associated invasive pulmonary aspergillosis (IPA) was present in 4 of 19 consecutive critically ill patients with moderate-to-severe ARDS. All of them were treated with intravenous antifungal medications. Their observations suggested a higher increased risk for critically ill COVID-19 patients suffering from co-infection with lung aspergillosis that was associated with higher mortality rates. Therefore, testing for the presence of aspergillus in the lower respiratory tract of critically ill COVID-19 patients should be considered. Spontaneous intrapulmonary bleeding and hemoptysis are typical complications of IPA. 18 Pasula and Chandrasekar 19 reported one critically ill patient with COVID-19 suffering from spontaneous hemoptysis, elevated serum levels of galactomannan, β-D glucan, positive Asp ergillus niger fungal culture, and radiologic evidence of cavitary. Therapy with IV voriconazole was started and continued for a total of 6 weeks with the resolution of hemoptysis without BAE. 19
Sato et al 20 had two interesting observations. First, the fact that COVID-19 pneumonia can lead to lung bulla even without mechanical ventilation or a history of pulmonary disease. Furthermore, hemoptysis as a rare clinical presentation of COVID-19 can occur in the convalescent phase of COVID-19 pneumonia. 20 In one report from Japan, an endotracheal tube obstruction occurred secondary to hemoptysis in an intubated patient with COVID-19 infection. 21 Massive hemoptysis without any other symptoms as the first manifestation of COVID-19 infection has also been reported. 22 The detrimental role of high-dose corticosteroids therapy in COVID-19 patients that can lead to IPA and subsequent hemoptysis has been recognized. 23
Conclusion
In conclusion, COVID-19 infection and HDCPT can lead to massive hemoptysis not only in the acute phase but also during the convalescent phase. Based on our case series and isolated reported cases discussed above, BAE performed in post-COVID-19 patients with massive hemoptysis is a useful procedure and can be life-saving.
Limitations
The study was derived from a single center, and there were little data about previous COVID-19 hospitalization in two patients.
Footnotes
Conflict of Interest None declared.
References
- 1.Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5:6. doi: 10.1186/s41256-020-00135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzotzos S J, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020;24(01):516. doi: 10.1186/s13054-020-03240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun P, Ren J, Li K, Qie S, Liu Z, Xi J. Response to: sore throat in COVID-19: comment on “Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: A single arm meta-analysis”. J Med Virol. 2020;92(07):716–718. doi: 10.1002/jmv.25818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corey R. 3rd ed. Boston: Butterworths; 1990. Hemoptysis; pp. 211–213. [PubMed] [Google Scholar]
- 5.Sokouti M, Montazeri V. Massive life-threatening hemoptysis from pulmonary hydatid cysts: a 13 - Year experience from an endemic area. Tanaffos. 2008;7:41–46. [Google Scholar]
- 6.Selvaraj V, Dapaah-Afriyie K. Lung cavitation due to COVID-19 pneumonia. BMJ Case Rep. 2020;13(07):e237245. doi: 10.1136/bcr-2020-237245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bidwell J L, Pachner R W. Hemoptysis: diagnosis and management. Am Fam Physician. 2005;72(07):1253–1260. [PubMed] [Google Scholar]
- 8.Lapostolle F, Schneider E, Vianu I et al. Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: the COVID-call study. Intern Emerg Med. 2020;15(05):813–817. doi: 10.1007/s11739-020-02379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chong W H, Neu K P. Incidence, diagnosis and outcomes of COVID-19-associated pulmonary aspergillosis (CAPA): a systematic review. J Hosp Infect. 2021;113:115–129. doi: 10.1016/j.jhin.2021.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keshmiri M S, Shafaghi S, Sharif-Kashani B et al. Preemptive non-selective bronchial artery angioembolization to reduce recurrence rate of hemoptysis. Multidiscip Respir Med. 2020;15(01):723. doi: 10.4081/mrm.2020.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dohen-Bécue F, Salez F, Ramon Pet al. [Management of hemoptysis in invasive pulmonary aspergillosis] Rev Mal Respir 19981506791–796.(French) [PubMed] [Google Scholar]
- 12.Gupta A, Sands M, Chauhan N R. Massive hemoptysis in pulmonary infections: bronchial artery embolization. J Thorac Dis. 2018;10 28:S3458–S3464. doi: 10.21037/jtd.2018.06.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seyyedi S R, Sadeghipour P, Sadr M et al. Outcomes and complications of bronchial angioembolization in patients with massive hemoptysis. Tanaffos. 2019;18(04):310–314. [PMC free article] [PubMed] [Google Scholar]
- 14.Yoon W. Embolic agents used for bronchial artery embolisation in massive haemoptysis. Expert Opin Pharmacother. 2004;5(02):361–367. doi: 10.1517/14656566.5.2.361. [DOI] [PubMed] [Google Scholar]
- 15.Keshmiri M S, Sharifkashani B, Serati A et al. Superselective angioembolisation: a report of two rare cases of hemoptysis. Int J Cardiovasc Pract. 2019;4:19–21. [Google Scholar]
- 16.Murgo S, Lheureux O, Taccone F, Vouche M, Golzarian J. Haemoptysis treated by bronchial artery embolisation in severe acute respiratory syndrome coronavirus 2: case report. CVIR Endovasc. 2020;3(01):61. doi: 10.1186/s42155-020-00154-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peys E, Stevens D, Weygaerde Y V et al. Haemoptysis as the first presentation of COVID-19: a case report. BMC Pulm Med. 2020;20(01):275. doi: 10.1186/s12890-020-01312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koehler P, Cornely O A, Böttiger B W et al. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020;63(06):528–534. doi: 10.1111/myc.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pasula S, Chandrasekar P. Spontaneous hemoptysis in a patient with COVID-19. Chest. 2021;160(01):e39–e44. doi: 10.1016/j.chest.2021.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sato L, Kinoshita N, Nakamoto T, Ohmagari N. Hemoptysis and a newly formed lung bulla in a case of convalescent COVID-19 pneumonia. Intern Med. 2021;60(05):803–805. doi: 10.2169/internalmedicine.5684-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maruhashi T, Wada T, Masuda T, Yamaoka K, Asari Y. Tracheal tube obstruction due to hemoptysis associated with pulmonary infarction in a patient with severe COVID-19 pneumonia. Cureus. 2021;13(02):e13599. doi: 10.7759/cureus.13599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Argun Barış S, Coşkun İS, Selvi G, Boyacı H, Başyiğit İ. Case series of COVID-19 presenting with massive hemoptysis. Turk Thorac J. 2020;21(06):454–456. doi: 10.5152/TurkThoracJ.2020.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seyyedi S R, Sadr M, Chitsazan M, Abedini A, Sharif-Kashani B. Angioembolization in massive hemoptysis for a patient with acute coronary syndrome and history of hydatid cyst. J Cardiol Cases. 2020;23(05):231–233. doi: 10.1016/j.jccase.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]


