Abstract
What is already known about this topic?
The prevalence of COPD in Chinese individuals aged 50 years and above was obviously higher than that in younger adults, but the risk factors for this age group were unclear.
What is added by this report?
The prevalence was estimated at 12.8% and 5.7% for males and females over 50 in 2020–2021, with confirmed risk factors of cigarette smoking, a family history of respiratory diseases, respiratory symptoms, and a history of cough or respiratory diseases during childhood.
What are the implications for public health practice?
The findings may help clinicians and the public identify individuals at high risk of COPD and take targeted measures in a timely manner.
Keywords: Chronic Obstructive Pulmonary Disease, Risk Factor, China
In China, chronic obstructive pulmonary disease (COPD) is characterized by high prevalence, substantial economic burden, and low detection rate (1–4). Previous nationwide studies found that COPD prevalence was significantly higher in adults aged 50 years and older (1–3). However, few studies have explored the risk factors for COPD in this age group, especially lifestyle factors such as alcohol consumption and dietary intake (5). Moreover, sex heterogeneity is a widely validated characteristic of COPD (6). This study utilized data from the latest resurvey of the China Kadoorie Biobank (CKB) to assess the sex-specific risk factors for COPD among participants aged 50 years and older. The results revealed that 12.8% of males and 5.7% of females had COPD. Cigarette smoking, a family history of respiratory diseases, respiratory symptoms, a history of respiratory diseases before 18 years of age, and chronic cough until 14 years of age were positively associated with COPD, whereas being overweight and obese was inversely associated with COPD. Smoking cessation, enhancing screening or treatment for individuals with a history of respiratory symptoms or diseases during childhood or adulthood, and maintaining a healthy weight might help prevent COPD in individuals aged 50 years and older.
The CKB is a population-based prospective cohort study that included over 500,000 participants from 10 PLADs at the baseline survey during 2004–2008. In the third resurvey during 2020–2021, 25,087 participants aged 40–95 years were randomly selected, constituting approximately 5% of the baseline population. The third resurvey followed a procedure similar to the baseline survey (7). Two-stage lung function measurements were performed to screen for potential COPD. First, all participants without contraindications were guided to use handheld Vitalograph Pneumotrac Spirometers (Model 6800) to record at least two valid results. The highest values were used to calculate the FEV1/FVC ratio, and participants with a ratio <0.7 entered the second stage. The difference between the two stages was the inhalation of a bronchodilator before measurement in the second stage. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criterion, an FEV1/FVC ratio <0.7 in the second stage (post-bronchodilator) indicated prevalent COPD (5). The present study included participants aged ≥50 years (n=24,640) and further excluded those with unsuccessful lung function tests (first stage: n=5,933, second stage: n=99) and those with missing values for key covariates (n=49). Finally, 6,707 males and 11,852 females were included.
Analyses were performed separately for males and females. First, COPD prevalence was calculated across sociodemographic groups (age, region, education level, and household income) using logistic regression models, to adjust for age and study area. Second, associations between lifestyle factors and COPD were explored. Based on previous studies (8) and data availability, the following lifestyle factors were included: smoking status, alcohol consumption, fresh fruit and red meat intake, physical activity, BMI, central obesity, passive smoking, and household air pollution. Models for each lifestyle factor were adjusted for the aforementioned sociodemographic factors and other lifestyle factors. Third, associations between respiratory factors and COPD were examined using logistic models, adjusting for all sociodemographic, lifestyle, and respiratory factors. Respiratory factors included respiratory symptoms, chronic cough until 14 years of age, a history of respiratory diseases before 18 years of age, and a family history of respiratory diseases. The multiplicative interaction between sex and each lifestyle and respiratory factor was calculated using likelihood ratio tests. All analyses were performed using Stata (version 17.0, StataCorp, College Station, TX, USA), and two-sided P values <0.05 were considered statistically significant.
The mean age was 65.2±8.6 years in males, of whom 900 (12.8%) had COPD. In females, the mean age was 63.8±8.3 years, and the prevalence of COPD was 648 (5.7%). Males had a higher percentage of individuals with an education level ≥ middle school and income ≥100,000 Chinese Yuan (CNY)/year (P<0.001). Notably, 54.6% of males reported daily smoking and 21.8% reported daily drinking,while only 1.7% and 1.2% of females reported these behaviors,respectively (Table 1).
Table 1. Characteristics of participants aged ≥50 in 10 CKB study areas, China, 2020–2021.
| Characteristic | Overall (n=18,559) | Males (n=6,707) | Females (n=11,852) | P for sex difference |
| Note: Baseline characteristics were adjusted for age and study area as appropriate. Values in the table were mean ± standard deviation for continuous variables and percentages for categorical variables. Abbreviation: CKB=China Kadoorie Biobank; MET h/d=metabolic equivalent of task hours per day; BMI=body mass index. | ||||
| Sociodemographic characteristics | ||||
| Age, years | 64.3±8.4 | 65.2±8.6 | 63.8±8.3 | <0.001 |
| Urban area, % | 38.5 | 36.2 | 39.8 | <0.001 |
| Southern area, % | 64.8 | 64.8 | 64.8 | 0.998 |
| Middle school and higher, % | 50.0 | 61.4 | 43.4 | <0.001 |
| Income ≥100,000 Chinese Yuan (CNY)/year, % | 30.3 | 33.2 | 28.7 | <0.001 |
| Lifestyle factors | ||||
| Current daily smoker, % | 20.8 | 54.6 | 1.7 | <0.001 |
| Passive smoker, % | 71.4 | 63.4 | 76.1 | <0.001 |
| Current daily drinker, % | 8.6 | 21.8 | 1.2 | <0.001 |
| Daily intake of fresh fruit, % | 40.7 | 34.4 | 44.1 | <0.001 |
| Daily intake of meat, % | 36.5 | 39.9 | 34.6 | <0.001 |
| Household air pollution, % | 24.0 | 26.1 | 27.2 | 0.023 |
| Physical activity, MET h/d | 16.1±13.8 | 18.8±16.1 | 14.5±12.0 | <0.001 |
| Anthropometric measures | ||||
| BMI, kg/m2 | 24.4±3.4 | 24.4±3.2 | 24.5±3.5 | <0.001 |
| Waist circumference, cm | 85.8±9.4 | 87.6±9.4 | 84.7±9.2 | 0.116 |
COPD prevalence increased with age, with a higher prevalence observed in males than in females across all age groups. Among males, the COPD prevalence for those aged 50–59, 60–69, 70–79, and ≥80 years was 6.4%, 12.7%, 22.1%, and 25.9%, respectively. The corresponding prevalence in females was 2.1%, 5.4%, 10.2%, and 18.6%. In rural regions, the COPD prevalence was 16.1% for males and 6.9% for females, both higher than those in urban regions (9.0% for males and 3.4% for females). For participants with education levels of illiterate and primary school, middle and high school, and college or university, the respective COPD prevalence was 14.5%, 12.7%, and 4.8% for males and 5.7%, 4.9%, and 4.9% for females. COPD prevalence was also observed to decrease with increasing household income (Figure 1).
Figure 1.
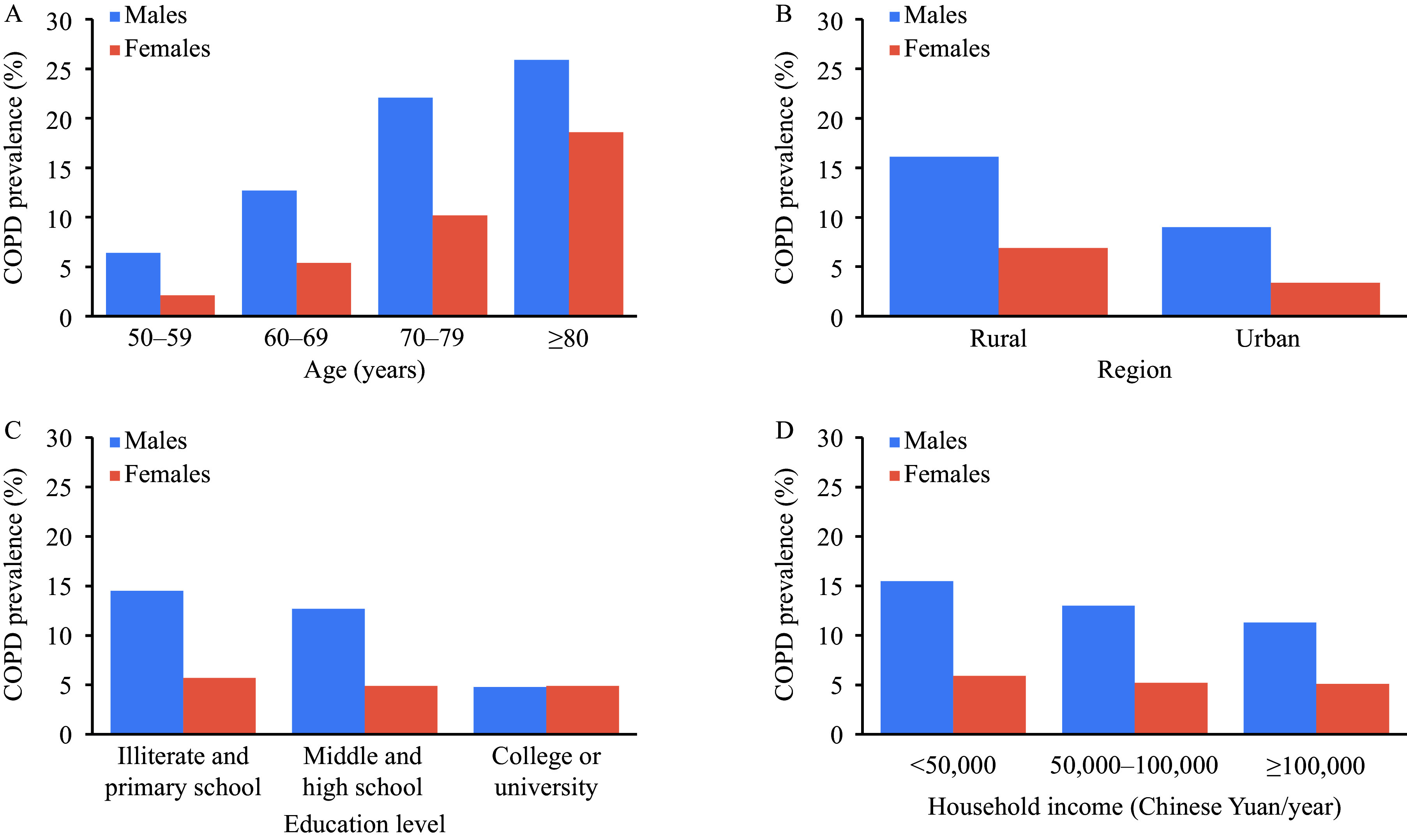
COPD prevalence in adults aged ≥50 with different characteristics in 10 CKB study areas, China, 2020–2021. (A) Age; (B) Region; (C) Education level; (D) Household income.
Abbreviation: COPD=chronic obstructive pulmonary disease; CKB=China Kadoorie Biobank.
After adjusting for sociodemographic and other lifestyle factors, no significant sex difference was observed in the association between lifestyle factors and COPD (P>0.05). Cigarette smoking was positively associated with COPD. Compared with never-smokers, the odds ratios [ORs, 95% confidence interval (CIs)] for current smokers with ≥15 cigarettes/d were 2.14 (1.73, 2.64) for males and 2.72 (1.14, 6.50) for females. Compared with participants with normal BMI (18.5–23.9 kg/m2), being overweight (24.0–27.9 kg/m2) and obese (≥28.0 kg/m2) were negatively associated with COPD, with ORs (95% CIs) of 0.52 (0.42, 0.65) and 0.42 (0.30, 0.59) for males and 0.57 (0.45, 0.71) and 0.49 (0.35, 0.68) for females. The four respiratory factors were significantly associated with COPD. Males who had respiratory symptoms, had been hospitalized for respiratory diseases before 18 years old, had experienced frequent coughs >8 weeks until 14 years old, and had a family history of respiratory diseases were at higher risk of COPD, corresponding to ORs (95% CIs) of 1.65 (1.40, 1.95), 2.22 (1.40, 3.53), 1.96 (1.30, 2.97), and 1.80 (1.46, 2.21), respectively. For females, the ORs (95% CIs) were 1.28 (1.05, 1.56), 2.65 (1.69, 4.16), 2.28 (1.59, 3.28), and 1.42 (1.14, 1.77), respectively (Table 2).
Table 2. Association between lifestyle and respiratory factors and COPD among adults aged ≥50 in 10 CKB study areas, China, 2020–2021.
| Factors | Males (n=6,707) | Females (n=11,852) | P for sexual difference |
| Note: Values in the table were ORs (95% CIs). For lifestyle factors, models were adjusted for age, study areas, household income, education leve in the table. For respiratory factors, models were further adjusted the respiratory factors in the table. Physical activity was divided by tertiles. Central obesity was defined as waist circumference ≥90 cm for males and ≥85 cm for females. Respiratory symptoms included coughing frequently, coughing up sputum after getting up in the morning, and wheezing or having a whistle in the chest. History of respiratory diseases before 18 years old included pneumonia, bronchitis, or tuberculosis. Family history of respiratory diseases included COPD, chronic bronchitis, emphysema, and cor pulmonale. Abbreviation: COPD=chronic obstructive pulmonary disease; CKB=China Kadoorie Biobank; MET h/d=metabolic equivalent of task hours per day; BMI=body mass index; OR=odds ratio; CI=confidence interval. | |||
| Lifestyle factors | |||
| Smoking status | 0.152 | ||
| Never | 1.00 | 1.00 | |
| Former | 1.48 (1.11, 1.97) | 3.10 (1.48, 6.48) | |
| Current and 1–14 cigarettes/d | 1.97 (1.57, 2.47) | 2.17 (1.42, 3.31) | |
| Current and ≥15 cigarettes/d | 2.14 (1.73, 2.64) | 2.72 (1.14, 6.50) | |
| Alcohol drinking | 0.288 | ||
| Non-current weekly | 1.00 | 1.00 | |
| Former weekly | 1.06 (0.83, 1.35) | 0.81 (0.47, 1.39) | |
| Current weekly | 0.93 (0.67, 1.29) | 0.42 (0.14, 1.20) | |
| Current daily | 0.87 (0.72, 1.06) | 1.11 (0.65, 1.90) | |
| Daily intake of fresh fruit | 0.236 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.03 (0.86, 1.23) | 1.08 (0.89, 1.31) | |
| Daily intake of red meat | 0.726 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.15 (0.94, 1.42) | 0.81 (0.64, 1.02) | |
| Physical activity (MET h/d) | 0.514 | ||
| Tertile 1 | 1.00 | 1.00 | |
| Tertile 2 | 0.89 (0.73, 1.08) | 0.88 (0.70, 1.09) | |
| Tertile 3 | 0.86 (0.71, 1.04) | 0.97 (0.79, 1.19) | |
| BMI (kg/m2) | 0.916 | ||
| <18.5 | 1.44 (0.98, 2.12) | 1.47 (0.97, 2.22) | |
| 18.5–23.9 | 1.00 | 1.00 | |
| 24.0–27.9 | 0.52 (0.42, 0.65) | 0.57 (0.45, 0.71) | |
| ≥28.0 | 0.42 (0.30, 0.59) | 0.49 (0.35, 0.68) | |
| Central obesity | 0.621 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.21 (0.97, 1.52) | 1.18 (0.94, 1.47) | |
| Passive smoking | 0.617 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.02 (0.86, 1.22) | 1.08 (0.88, 1.33) | |
| Household air pollution | 0.591 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.06 (0.76, 1.48) | 1.32 (0.84, 2.08) | |
| Respiratory factors | |||
| Respiratory symptoms | 0.185 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.65 (1.40, 1.95) | 1.28 (1.05, 1.56) | |
| History of respiratory diseases before 18 years old | 0.571 | ||
| No/don't know | 1.00 | 1.00 | |
| Yes | 2.22 (1.40, 3.53) | 2.65 (1.69, 4.16) | |
| Chronic cough until 14 years old | 0.505 | ||
| Rarely/don’t know | 1.00 | 1.00 | |
| Sometimes | 1.32 (0.87, 2.00) | 1.89 (1.30, 2.75) | |
| >8 weeks/year | 1.96 (1.30, 2.97) | 2.28 (1.59, 3.28) | |
| Family history of respiratory diseases | 0.086 | ||
| No | 1.00 | 1.00 | |
| Yes | 1.80 (1.46, 2.21) | 1.42 (1.14, 1.77) | |
DISCUSSION
This cross-sectional study, conducted from 2020 to 2021, explored risk factors for COPD among Chinese adults aged 50 years and older. Findings highlighted the detrimental effect of early-life respiratory injury on COPD risk. Early-life adverse exposures may stunt lung growth and predispose individuals to chronic inflammation and remodeling of the respiratory mucosa (9). This study provided new evidence for identifying the high-risk population for COPD, thereby effectively facilitating prevention strategies.
Compared with nationwide studies using the same definition of COPD (GOLD), the prevalence among adults aged 50 years and older in 10 CKB study areas was lower, which might be attributed to differences in survey areas and sampling methods (1–3). However, this study also revealed the high burden of COPD among Chinese adults aged 50 years and older, especially among males. Unlike other common chronic diseases, such as diabetes and cardiovascular diseases, this study and previous studies consistently indicated that being overweight and obese seems to be a protective factor for COPD (1,10). Existing literature indicates that being underweight increases COPD risk (1,10). Therefore, a healthy weight should be the primary target for general health. Regarding respiratory factors, the China Pulmonary Health study revealed that the COPD risk for participants with frequent coughs before 14 years of age increased by 1.57 times, consistent with the present study (1). A meta-analysis indicated that serious childhood respiratory infections, pneumonia, or bronchitis increased COPD risk, with an OR (95% CI) of 2.23 (1.63, 3.07) (9). Our results suggest that the critical period of COPD prevention should be shifted earlier to childhood. An integrated intervention strategy could be considered, including systematic health education for parents and targeted screening and treatment for children with respiratory symptoms or diseases.
This study has several limitations. First, the 5% survival sample of the CKB cohort is not nationally representative. Second, participants were required to have spirometry data, excluding a large proportion with unsuccessful lung function tests or missing covariates, which may have introduced selection bias. Third, the GOLD criterion may have led to overdiagnosis in older adults. Fourth, recall bias and reverse causality may be present due to the cross-sectional study design.
Our findings elucidated the risk factors of COPD for Chinese individuals aged 50 years and older. Screening for COPD using spirometry is paramount in individuals with smoking habits and a history of respiratory symptoms or diseases. Smoking cessation should be a public health priority. Our results underscore the necessity of early-life lung protection.
Conflicts of interest
No conflicts of interests.
Funding Statement
Supported by the National Natural Science Foundation of China (82388102, 82192900, 82192901, 82192904). The CKB baseline survey and the first re-survey were supported by a grant from the Kadoorie Charitable Foundation in Hong Kong. The long-term follow-up is supported by grants from the UK Wellcome Trust (212946/Z/18/Z, 202922/Z/16/Z, 104085/Z/14/Z, 088158/Z/09/Z), grants (2016YFC0900500) from the National Key R&D Program of China, National Natural Science Foundation of China (81390540, 91846303, 81941018), and Chinese Ministry of Science and Technology (2011BAI09B01)
References
- 1.Wang C, Xu JY, Yang L, Xu YJ, Zhang XY, Bai CX, et al Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–17. doi: 10.1016/S0140-6736(18)30841-9. [DOI] [PubMed] [Google Scholar]
- 2.Fang LW, Gao P, Bao HL, Tang X, Wang BH, Feng YJ, et al Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. 2018;6(6):421–30. doi: 10.1016/S2213-2600(18)30103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhong NS, Wang C, Yao WZ, Chen P, Kang J, Huang SG, et al Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–60. doi: 10.1164/rccm.200612-1749OC. [DOI] [PubMed] [Google Scholar]
- 4.Chen SM, Kuhn M, Prettner K, Yu FY, Yang T, Bärnighausen T, et al The global economic burden of chronic obstructive pulmonary disease for 204 countries and territories in 2020-50: a health-augmented macroeconomic modelling study. Lancet Glob Health. 2023;11(8):e1183–93. doi: 10.1016/S2214-109X(23)00217-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agusti A, Celli BR, Criner GJ, Halpin D, Anzueto A, Barnes P, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Eur Respir 2023;61(4):2300239. https://doi.org/10.1183/13993003.00239-2023.
- 6.Milne KM, Mitchell RA, Ferguson ON, Hind AS, Guenette JA Sex-differences in COPD: from biological mechanisms to therapeutic considerations. Front Med. 2024;11:1289259. doi: 10.3389/fmed.2024.1289259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen ZM, Chen JS, Collins R, Guo Y, Peto R, Wu F, et al China Kadoorie Biobank of 0. 5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40(6):1652–66. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang IA, Jenkins CR, Salvi SS Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. 2022;10(5):497–511. doi: 10.1016/S2213-2600(21)00506-3. [DOI] [PubMed] [Google Scholar]
- 9.Duan PF, Wang Y, Lin RQ, Zeng YM, Chen CS, Yang L, et al Impact of early life exposures on COPD in adulthood: a systematic review and meta-analysis. Respirology. 2021;26(12):1131–51. doi: 10.1111/resp.14144. [DOI] [PubMed] [Google Scholar]
- 10.Li JC, Zhu L, Wei YX, Lv J, Guo Y, Bian Z, et al Association between adiposity measures and COPD risk in Chinese adults. Eur Respir J. 2020;55(4):1901899. doi: 10.1183/13993003.01899-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]


