ABSTRACT
Background
Mothers of high‐risk neonates experience tremendous stress during neonatal intensive care unit (NICU) admission. This stress has a negative impact on mothers' participation in neonatal care activities, psychological health and coping skills in the NICU.
Objective
To determine the impact of interventional strategies to reduce maternal stress and enhance coping skills during neonatal admission to the NICU.
Design
A scoping review was carried out following the methodological framework outlined by Arksey and O'Malley.
Methods
This scoping review was conducted as per the Joanna Briggs Institute guidelines, including a quality appraisal checklist for randomised and nonrandomised controlled trials. Patterns, advances, gaps, evidence for practice and research recommendations from the review (PAGER framework) were used to report the results. The following international databases were used to search for primary articles: Medline via PubMed, EBSCOhost via CINAHL, Scopus, Web of Science and the ProQuest Medical Library. Original studies published in English between January 2011 and January 2023 from low‐ and middle‐income countries (LMICs) that assessed maternal stress and coping skills during neonatal NICU admission were included in the review.
Results
The review included 15 articles from LMICs, of which 60% were from middle‐income, 25% were from lower‐middle‐income and 15% were from low‐income countries. Interventional strategies were described under five categories. Maternal stress decreased significantly across all three subscales of the PSPS: ‘sight and sound’, ‘baby looks and behavior’ and ‘parental relationship with baby and role alteration’ during neonatal NICU admission. Interventional strategies involving family‐centred care and emotional and psychological supportive care have been reported to have a consistently positive impact on alleviating maternal stress and enhancing coping skills in the NICU.
Conclusion
Healthcare professionals, especially nurses, are pivotal in promptly recognising maternal stress and NICU stressors. The participation of mothers in neonatal care, such as through family‐centred care and emotional support interventions, significantly reduces maternal stress and enhances coping skills.
Keywords: coping skills, low‐ and middle‐income countries, mother, neonatal care, NICU, participation, stress
1. Introduction
High‐risk neonates, that is, premature, low birth weight or neonates with any other medical illness admitted to the neonatal intensive care unit (NICU), have a greater chance of mortality, accounting for approximately 15% of all neonates globally (Ebadi, Attarha, and Nokani 2022; WHO 2020). Most of these mortality rates are reported in low‐ and middle‐income countries (LMICs) across Asia and sub‐Saharan Africa, with many infants dying within the first days of life (Mianda, Todowede, and Schneider 2023). Mitigating mortality among these individuals is crucial for meeting the United Nations Sustainable Development Goals, which aim to reduce neonatal mortality to 12 deaths per 1000 live births by 2030 (WHO 2023). Furthermore, these vulnerable neonates require extended care in neonatal units with prolonged stays (Siva et al. 2024). The average length of stay in the NICU for high‐risk neonates in developed countries is 10.2 (SD = 5.2) days (Toptas et al. 2018) and it is 39 (SD = 25) days in LMICs (Mahovo and Velaphi 2019). In 2014, maternal and child health was designated as a flagship priority in the World Health Organisation's Southeast Asia Region. In countries such as India, the current framework for maternal and neonatal care often involves separating sick neonates from mothers who remain in the posnatal ward and can only visit neonates in the NICU, as advised by healthcare professionals (WHO 2023).
Parents, particularly mothers, are usually overburdened and worried about the separation of babies and the uncertain future of their neonates admitted to the NICU (Kegler et al. 2019). This is largely attributed to preterm birth, low birth weight, birth asphyxia, neonatal sepsis and perinatal depression, which collectively pose significant challenges to global health (Iqbal et al. 2023; Phagdol et al. 2022). Neonatal life‐threatening conditions, alterations to the anticipated parental function, NICU protocols and inability to safeguard neonates all contribute to feelings of grief, loss, distress, frustration, guilt and helplessness among parents (Ebadi, Attarha, and Nokani 2022; Siva, Phagdol, et al. 2023). Additionally, the appearance and behaviour of high‐risk neonates cause severe stress among parents, especially because separation from the mother is a significant stressor during NICU admission (Pichler‐Stachl et al. 2019; Siva et al. 2024). These stressors can negatively impact maternal psychological health, emotional control, interactions with babies, lack of bonding and mothers' milk production (Pichler‐Stachl et al. 2019). Similarly, stress and anxiety among mothers may lead to a decrease in their efficacy and competence, hindering their participation in neonatal care activities in the NICU and their future parenting style (Lomotey et al. 2020; Siva, Nayak, et al. 2023). Parents from LMICs are disproportionately exposed to various risk factors, such as limited healthcare resources, cultural factors and socioeconomic and cumulative financial hardship related to the long duration of neonatal stay in the NICU (Kumar and Mallick 2020).
Encouragement and constant support from healthcare administrators or the public health sector are pivotal for implementing sustainable interventions in neonatal care to achieve long‐term expected maternal and child‐positive outcomes (Khoddam et al. 2023; Mianda, Todowede, and Schneider 2023). It is imperative to involve the mothers and families in the routine care of neonates, not only to enhance short‐ and long‐term health and developmental outcomes but also to improve the overall caregiving experience for parents and family members. This highlights the significance of the ‘zero separation’ concept, advocating for mothers to stay with their small and sick babies after birth, facilitated by the establishment of mother–newborn care units (WHO 2020). However, despite these challenges, nurses play a pivotal role in providing vital supportive care to alleviate maternal stress during neonatal NICU admission (Khoddam et al. 2023). Through empathetic communication, education and emotional support, NICU nurses can help mothers cope with the distress of having hospitalised neonates and separating neonates due to medical conditions (Jagtap et al. 2023). Additionally, they facilitate maternal participation in neonatal caregiving activities in the NICU and encourage mothers to actively participate in infant care decision‐making despite challenging circumstances (Siva, Nayak, et al. 2023). Moreover, by advocating for family‐centred care and navigation models and implementing culturally sensitive approaches, NICU nurses contribute significantly to enhancing maternal well‐being and competencies in neonatal care activities and fostering resilience in LMICs (Siva et al. 2024).
However, there are considerable variations in LMICs' healthcare expenditures and service delivery, as well as maternal and infant health burdens such as low birth weight and prematurity (Burger et al. 2020). As a result of the continuing discrepancies in maternal psychological stress, neonatal clinical outcomes are increasingly being incorporated into global health research in LMICs (Lomotey et al. 2020; Siva, Phagdol, et al. 2023). Globally, several existing interventions are being implemented to reduce maternal stress and stressors, especially LMICs, in which healthcare professionals adopt different interventional strategies with available resources to improve maternal psychological health and coping skills by enhancing health literacy on routine neonatal care activities during NICU admission (Mianda, Todowede, and Schneider 2023; Oyekunle et al. 2021). Based on the latest information, researchers opted for a scoping review methodology to evaluate the effectiveness of intervention strategies in mitigating maternal stress and enhancing coping skills during neonatal NICU admission in LMICs. This scoping review was tailored to address a specific research question and methodology, aiming to comprehensively map out diverse perspectives within the literature regarding intervention strategies for reducing maternal stress across various contexts in LMICs. Additionally, the review sought to elucidate measures of maternal psychosocial health during NICU admission, including coping skills, mother–infant bonding, breastfeeding and levels of empowerment related to health literacy.
2. Methods
We adopted a scoping review methodology to address the complex interplay of maternal stress, stressors and coping skills in accordance with various sociocultural, psychological and environmental factors within the NICU. This approach allows for a comprehensive examination of maternal psychological health, offering more timely insights than traditional systematic reviews. By streamlining components of primary articles, scoping reviews expedite the review process, aiding in policy development and the implementation of tailored interventions for maternal and neonatal well‐being.
2.1. Research Question
To determine the impact of interventional strategies to reduce maternal stress and enhance coping skills during neonatal admission to the NICU.
2.2. Design
We followed the preferred reporting items for systematic reviews and meta‐analyses extension for scoping reviews (PRISMA‐ScR) guidelines to report the scoping review results. Additionally, we followed patterns, advances, gaps, evidence for practice and research recommendations from the review (PAGER framework) (Table 1).
TABLE 1.
PAGER framework.
| Pattern | Advances | Gaps | Evidence for practice | Research recommendations |
|---|---|---|---|---|
|
Investigating the relation between neonatal NICU admission and maternal stress. What challenges do LMIC mothers encounter while their babies are in the NICU? |
There is evidence of an increased maternal stress with neonatal NICU admission, separation of baby, neonatal medical condition, lack of communication with healthcare members and maternal health literacy. | There is a need for ongoing research to investigate the specific stress and stressors and assess the comprehensive effects of interventions to improve maternal health literacy and reduce maternal stress during neonatal NICU admission in LMICs. | Primary studies have indicated that factors such as neonate separation, severity of the child's illness, limited communication with healthcare professionals and complexity of NICU environment can negatively impact maternal psychological health. | To conduct experimental research to deliver comprehensive healthcare support to parents, communicate with mothers and involve the mothers in neonatal care activities in NICU to minimise the maternal stress and stressors related to neonatal NICU admission in LMICs. |
| Maternal perception and participation in neonatal care activities in the NICU. | There is increasing evidence in LMICs concerning maternal perception of participation in neonatal care at NICU, and communication with healthcare members to alleviate maternal stress. | Limited evidence exists in LMICs regarding the impact of maternal participation in neonatal care activities in NICU to improve the psychological well‐being of mothers and neonates during NICU admission. | Nurses and physicians should recognise importance of maternal participation in neonatal care at NICU, including skin‐to‐skin contact, gentle touch and vocal stimulation, which can reduce maternal stress and enhance neonatal health outcomes. | To improve maternal health literacy and promote maternal participation in neonatal care activities within the NICU, such as KMC, feeding, holding and massaging the baby to decrease maternal stress and enhance maternal psychological well‐being and neonatal clinical outcomes. |
| What intervention can effectively lower maternal stress levels and enhance maternal coping skills in LMICs? | Evidence suggests that early intervention strategies can effectively lower maternal stress and enhance coping ability during complex neonatal NICU admissions. | No scoping reviews have been conducted in LMICs to identify what type of intervention strategies can effectively reduce maternal stress and enhance coping skills in the NICU. | Studies that include effective communication and involving the mothers in neonatal care activities at NICU should be prioritised to improve mother's psychological health including self‐efficacy and competencies in neonatal care activities at NICU. | Appropriate early strategies such as family‐centred care including constant emotional support should be integrated into routine neonatal care at NICU in LMICs to minimise maternal stress and enhance coping skills in neonatal care activities. |
2.3. The Eligibility Criteria
2.3.1. Inclusion Criteria
The studies included in the analysis focused on mothers of neonates admitted to the NICU. The primary objective was to assess the effectiveness of interventions on maternal stress and coping skills within the NICU environment. Studies conducted specifically in LMICs, written in English and published between January 2011 and January 2023 were included.
2.3.2. Exclusion Criteria
Excluded from consideration were articles published in languages other than English; systematic, scoping or narrative reviews; studies that included mothers with pre‐existing mental health conditions or substance use disorders; studies involving mothers with full‐term or stillborn infants; and articles that primarily focused on the stress and coping skills of fathers or other family members without specifically tracking maternal stress and coping skills.
2.4. Search Strategy
Using the population, intervention, comparison and outcome (PICO) model, the search strategy was carried out based on the study's objectives. A comprehensive literature search was carried out using PubMed, CINAHL via EBSCO host, Scopus, Web of Science and ProQuest Medical Library databases, with key search terms including mothers, parents, caregivers, neonates, high‐risk neonates, premature, family‐centred care, family‐based nursing, maternal participation, therapy, education, support, strategies, stress, psychological stress, stressors, experience, coping, coping skills, stress management and neonatal intensive care unit. The data sources and search strategies used for the databases are given in the Supporting Information. Initial records identified from electronic database searches, relevant reviews and retrieved studies were imported into Rayyan software. After removal of duplicates, titles and abstracts were screened, and full‐text articles for potentially relevant studies were retrieved for further assessment by two independent researchers (SN and BV). When there were disagreements, a third independent researcher (BSN) assisted in resolving any disagreements.
2.5. Data Extraction
Following the instructions of the Cochrane Library, data were systematically collected from studies that satisfied all the inclusion criteria. To facilitate this process, a standardised coding sheet was employed, which systematically recorded the following information: (i) study ID, citation details, authors' names, (ii) country, (iii) participant characteristics (including sample size, mothers' age and day of recruitment), (iv) attributes of the experimental group and control group (comprising details about the intervention content, type of contact, duration of intervention and the specific intervention techniques employed) and (v) outcome measures. This data extraction process was carried out by the first author (NS) and subsequently cross‐verified by the second author (BV).
2.6. Quality Appraisal
Two reviewers (SN and BV) investigated all 15 articles utilising the JBI criteria for randomised controlled trials (RCTs) and quasi‐experimental studies to conduct a critical appraisal. The following factors were used to establish the quality of the RCTs: randomisation accuracy, the confidentiality of the treatment group, the baseline homogeneity of the treatment group, the presence of blinding treatment, the reliability of the outcomes measured and the statistical analysis. The following criteria were used to select the quasi‐experimental study articles for the synthesis phase: clear evidence of cause and effect, involvement of control group participants, the presence of multiple outcome measurements (both pre‐ and postintervention), the presence of follow‐up, the reliability of outcome measures and statistical analysis. The critical appraisal results yielded 15 articles for the extraction and analysis phases.
3. Results
3.1. Search Results
The initial search of the five databases yielded 1820 articles (N = 1286). A total of 208 duplicates were spotted. A total of 1612 studies were assessed for eligibility using the inclusion and exclusion criteria based on title and abstract screening, resulting in 34 articles. Subsequently, a full‐text assessment of these 34 papers led to the exclusion of 19 articles. Overall, 15 articles from LMICs were retained for this review. A visual representation of this search process is depicted in Figure 1.
FIGURE 1.
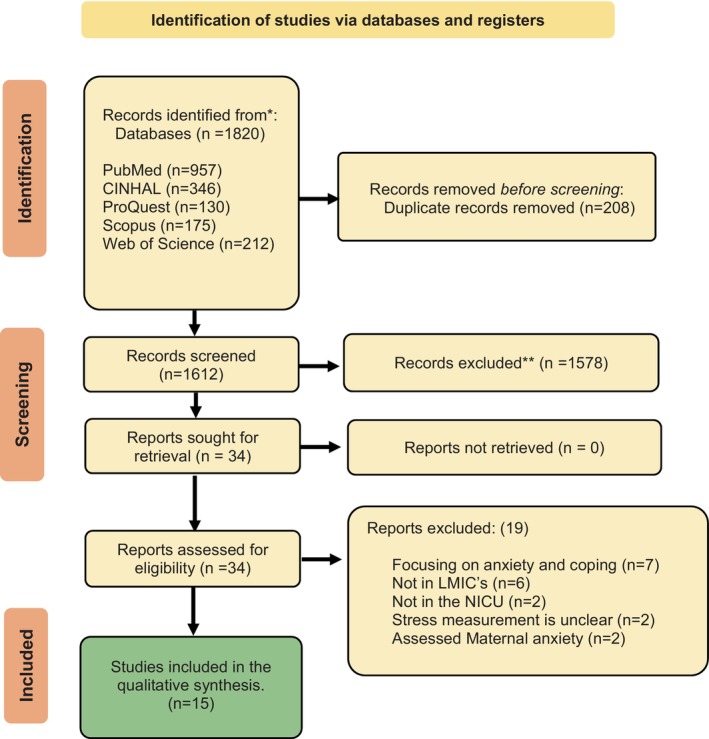
PRISMA flow diagram at each stage of the selection process. PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases and registers.
3.2. Study Characteristics
Of 15 studies, 8 were conducted in Iran, 2 in India, 2 in Turkey, 2 in Malaysia and 1 in Jordan. Among these, eight were RCTs, and seven were non‐RCTs. Notably, 60% of the studies were conducted in middle‐income countries, 25% in lower‐middle‐income countries and the remaining 15% in low‐income countries.
3.3. Sample Characteristics
Of the 15 studies analysed, 11 focused on recruiting mothers of preterm babies admitted to the NICU. The mothers ranged in age from 22 to 34 years, with an average age of 28 years. Six studies provided information on fathers' age, revealing that most fathers were between 28 and 36 years of age, with a mean age of 31 years. All studies were conducted in urban tertiary care hospitals. In total, 11 studies reported parental education levels, showing that the majority of mothers had education levels below graduation. The average age of the neonates in both groups was 3 days, with an average birth weight of 1200 g in the intervention group and 1290 g in the control group. The complete study sample and study characteristics are depicted in Table 2.
TABLE 2.
Characteristics and summary of article findings.
| Author, Year | Country | Objective | Study Design | Study Population | Outcome measures | Intervention | Results |
|---|---|---|---|---|---|---|---|
| Yilmaz and Küçük Alemdar (2022) | Turkey | To determine the effects of supportive interventions on the stress levels of mothers with infants hospitalised in the NICU | Randomised Controlled Trial (RCT) | Mothers of high‐risk neonates admitted to NICU (N = 85)—45 in the intervention and 40 in the control group | Maternal stress, anxiety and salivary cortisol level | Educational and Supportive Nursing Interventions | Supportive nursing intervention significantly reduced maternal stress related to the NICU environment, anxiety levels and saliva cortisol levels compared to the control group |
| Beheshtipour et al. (2014) | Iran | To determine the effect of educational programmes on parental stress during their preterm neonate's admission to NICU | Double‐blind RCT | Parents of high‐risk neonates admitted to NICU (N = 120) | Parental stress | Educational programme | Educational programmes have significant effect on reducing maternal stress during neonatal NICU admission (t = 5.23, p < 0.001) |
| Ebadi, Attarha, and Nokani (2022) | Iran | To investigate the effect of midwife‐based listening visits (MBLV) on stress, anxiety and depression among mothers of premature infants | RCT | Mothers of premature neonates who were admitted to the NICU (N = 60) | Maternal stress, anxiety and depression | Midwife‐based listening visit (MBLV) | The mean scores of anxiety, F(2, 98) = 19.92, p < 0.001), stress, F(2, 98) = 43.94, p < 0.001) and depression, F(2, 98) = 42.95, p < 0.001) significantly reduced after 4 and 8 weeks of intervention in the MBLV group |
| Khazaii et al. (2018) | Iran | To examine the effects of preterm infant care education on stress among the mother's neonates admitted to NICU | RCT | Mothers of premature neonates who were admitted to the NICU (N = 62) | Maternal stress | Preterm Infant Care Education programme | The mean scores of maternal stresses and environmental domains in the experimental group were significantly lower than in the control group (p = 0.05) |
| Mirlashari et al. (2021) | Iran | To determine the effect of group discussion between mothers and the healthcare team on mothers' stress and coping skills | Nonrandomised, prospective intervention study | Mothers with premature infants (N = 40) | Maternal stress and problem‐focused coping skills | Family‐centred care (FCC) with group discussion | Mothers in FCC with group discussion were shown significant reduction of stress compared to the control group (p = 0.002). Problem‐focused coping skills were increased significantly in the intervention group (p < 0.001) |
| Chourasia et al. (2013) | India | To determine the effect of counselling on the stress levels of NICU mothers | Interventional crossover study | Mothers of high‐risk neonates admitted to NICU (N = 100) | Maternal stress | Planned counselling sessions | There was a significant reduction in the postcounselling stress levels among NICU mothers in all three subscales of PSS: NICU, F(1,98) = 5.46, p < 0.001 |
| Al‐Maghaireh et al. (2020) | Jordan | To assess the impact of an emotional support training programme on acute stress disorder among mothers of preterm infants admitted to NICU | RCT | Mothers of preterm neonates admitted to NICU (N = 48) | Maternal stress | Emotional support training programme | There is a statistically significant difference found between the interventional and control groups [t (23) = 6.07, p < 0.001], with the mean scores of 18.53 (SD = 9.3) |
| Mousavi et al. (2021) | Iran | To investigate the impact of maternity support programmes on mothers' stress | Nonrandomised, prospective and experimental study | Mothers of preterm neonates admitted to NICU (N = 143) | Maternal stress | Maternity support programme | In the intervention group, maternal stress levels were significantly reduced compared to the control group mothers (p < 0.001) |
| Goral and Geçkil (2022) | Turkey | To investigate the effect of a comprehensive supportive programme on maternal stress levels in a NICU | Quasi‐experimental study | Mothers whose premature neonates were admitted to NICU (N = 62) | Maternal stress | Comprehensive support programme | Intervention group mothers' stress levels were significantly reduced, 2.95 (SD = 0.72), than the control group, 3.74 (SD = 0.82) (p < 0.001) in the posttest |
| Abdeyazdan et al. (2014) | Iran | To evaluate the effect of a family support intervention on the stress levels among the parents of preterm infants | Quasi‐experimental study | Parents of preterm infants admitted to NICU (N = 50) | Parental stress | Family support intervention | The intervention group's scores showed a significant reduction in maternal stress (p < 0.001) and improved coping ability among mothers (p < 0.001) |
| Jouybari et al. (2020) | Iran | To examine the effect of narrative writing and art therapy on maternal stress in the NICU during infants' hospitalisation | RCT | Mothers of infants admitted to the NICU. (N = 105) | Maternal stress | Narrative writing and art therapy | No significant differences were found between the groups and there is statistically significant difference in pre‐ and postintervention stress levels of mothers in both groups (p = 0.92) |
| Mianaei et al. (2014) | Iran | To evaluate the effect of COPE programme on maternal stress and anxiety levels among mothers of premature babies | RCT | Mothers of premature infants admitted to the NICU (N = 90) | Maternal stress | Creating Opportunities for Parent Empowerment (COPE) | After performing each phase of the COPE programme, mothers' stress levels and anxiety levels were significantly reduced than the control group (p < 0.001) |
| Ong et al. (2019) | Malaysia | To investigate the effectiveness of a structured nursing intervention programme on maternal stress and NICU‐related maternal coping abilities | Quasi‐experimental design | Mothers of premature infants admitted to NICU (N = 216) | Maternal stress | Structured nursing intervention programme | Mean total score of maternal stress and parental role and relationship subscale decreased significantly in intervention group (p = 0.04; p < 0.001). Additionally, maternal coping ability improved substantially in the intervention group (p < 0.001) |
| Dabas et al. (2019) | India | To assess the impact of relaxation techniques on stress, anxiety and milk output among the postpartum mothers of hospitalised neonates in the NICU | Nonblinded RCT | Mothers of high‐risk neonates admitted to the NICU (N = 57) | Stress, anxiety and milk output | Audio‐assisted relaxation technique | A significant reduction was observed in maternal stress (p < 0.001) and anxiety (p < 0.001) and an improvement in milk output in the experimental group compared to the control group |
| Samsudin et al. (2023) | Malaysia | To assess the effectiveness of Kangaroo Care Education Programme on the mother's perception, knowledge, perceived barriers and stress | A quasi‐experimental and longitudinal study | Mother–infant dyads (N = 48) | Maternal stress, perception, knowledge and perceived barriers | Maternal Kangaroo Care Education Program | At 3 months of postintervention, the experimental group reported a significant reduction in stress levels and improved knowledge of KMC. The mothers' perceived barriers towards Kangaroo Care significantly decreased in the intervention group (p < 0.001) |
3.4. Stress Measures Analysed
Thirteen studies used the Parental Stress Scale: Neonatal Intensive Care Unit (PSS: NICU) questionnaire to evaluate maternal stress, while two studies utilised a 5‐point rating scale. The 15 articles included in this scoping review were thoroughly examined, and their content was narratively summarised across five main categories. Table 3 provides a comprehensive description of each intervention.
TABLE 3.
Description of interventional strategies.
| Educational and supportive nursing interventions | |
| Educational and Supportive Nursing Interventions (Yilmaz and Küçük Alemdar 2022) | Seven interactive sessions were conducted among mothers, including an information booklet on essential neonatal care. The topics focused on the NICU environment, features of neonates born prematurely and at term, care, feeding, diseases, treatment, possible stressors in the NICU, breastfeeding, preparation for discharge and baby care at home |
| Educational Program (Beheshtipour et al. 2014) | Five educational sessions were conducted on the NICU environment, the child's medical condition and treatment and how to interact with the baby, followed by discussion sessions, including a 5th‐day spouse support education session |
| Midwife‐Based Listening Visit (LV) Program (Ebadi, Attarha, and Nokani 2022) | A total of six intensive teaching sessions were delivered, focusing on the child's medical condition treatment and making more effective communication with parents. The consultant LV midwife conducted discussion sessions on recent concerns, helping the mother explain her thoughts, feelings and concerns through active reflexive listening |
| Preterm Infant Care Education Program (Khazaii et al. 2018) | Five sessions were implemented for 3 consecutive days. Sessions were delivered individually and face‐to‐face. After each session, a 45‐min video was shown to the mothers, which contained essential high‐risk neonatal care; also, an educational booklet was provided to the mothers, including information about essential neonatal care and home care |
| Education and Counselling Program (Chourasia et al. 2013) | Mothers were given primary education regarding the NICU structure, set‐up and functions. After adequate discussions with the NICU duty team, the interns would access the baby's medical information and give the mother feedback regarding the baby's progress. Mothers were allowed to look closer at the baby, and their queries, if any, were clarified. The entire process lasted for 30–45 min |
| Creating Opportunities for Parent Empowerment (COPE) (Mianaei et al. 2014) | In the intervention group, the Phase I booklet was given to the mother, and she listened to its audiotape. Immediately following the audiotape, the mother answered the Phase I manipulation check. The first set of activity workbook was then given to the mother with specific instructions on completing them. After 4 to 8 days post‐NICU admission, the mother completed STAI and the Parental Stressor Scale. Next, the booklet was given to the mother in Phase II and she listened to its audiotape. Then, the mother answered the Phase II manipulation check questions, and at the end, she received Phase II of the activity workbook with specific instructions on how to complete it |
| Emotional and psychological support | |
| Maternity Support Program (Mousavi et al. 2021) | Initial stage premature babies’ photo albums were shown to the mother, including spiritual support. The mother was trained to express breast milk, work with a breast pump, store and transport the breast milk and provide emotional support. Mothers were encouraged and empowered to interact comfortably with the infant through the exchange of smell, continuous gentle touch, whispering in the infant's ear, eye contact and KMC as soon as possible |
| Family Support Intervention (Abdeyazdan et al. 2014) | Family support intervention comprises two stages. The first stage was performed 2–4 days after the infant's admission and included informational and observational phases. In the informational phase, parents attended a 60‐min face‐to‐face training, and then the parents were provided with two books and an educational booklet. Two to 4 days later, the second stage (support provision) was started, i.e., the parents received psychological training and obtained the opportunity to share their feelings and experiences with other parents of premature infants during the 2nd‐hour session |
| Emotional Support Training Program (Al‐Maghaireh et al. 2020) | The Emotional Support Program consisted of two phases: informational and supportive. Phase 1, the informational stage, commenced 2–7 days after the infant's admission to NICU and included information and observational phases. During this stage, the mothers attended a 95‐min face‐to‐face training conference. After Phase 1, the researcher gave the mothers educational booklets on essential neonatal care. Two to 4 days later, the supportive second stage commenced, wherein the mothers received psychological training and got the chance to share their experiences and express their feelings with other mothers of premature infants during sessions |
| Comprehensive Support Program (Goral and Geçkil 2022) | The comprehensive programme included introducing the NICU environment, training about the neonates, allowing and encouraging sensual contact with the neonates, providing mothers with the educational booklet, ensuring mothers get acquainted and interacted with parents with similar experiences and group training |
| Family‐Centred care interventions | |
| Maternal Kangaroo Care Education Program (Samsudin et al. 2023) | MKC‐EP complies with KC guidelines and protocols and focuses on the psychological and physical aspects of preparing and implementing Kangaroo Care (KC) (before, during and after). It consists of a PowerPoint presentation, a mannequin‐like simulation and a practical session to equip the mothers with the knowledge and necessary skills to perform KC with their babies. The mothers were guided in performing KC and provided a leaflet on KC techniques. The mothers were reminded to complete KC at least 1 h daily and accumulate to 4 to 5 h weekly |
| Family‐Centred Care Interventions (Mirlashari et al. 2021) | Family‐centred care (FCC) consisted of four discussion sessions on 2 days every week for 2 weeks, and mothers participated in all four group discussion sessions, each lasting 60 min. All mothers in the study received a free booklet about caring for premature infants. The mothers in the intervention group were informed about the topic in advance. The topics were chosen based on the most common area of the mothers' needs and agreed upon by the team members |
| Structured Nursing Intervention Program (Ong et al. 2019) | The structured nursing intervention (SNI) consisted of two meetings. At the first meeting, a simple booklet was given as a guide to mothers, followed by two short message services (SMSs) and telephone calls to update the infant's progress in feeding and body weight. Rapport was developed from the first meeting held within 48 h of admission. Information related to premature infants admitted to the NICU was given to the parents by going through the booklet, and the mother was orientated to the NICU equipment and layout |
| Relaxation techniques | |
| Audio‐Assisted Relaxation Technique (Dabas et al. 2019) | Thirty minutes of audio‐assisted relaxation technique was developed under the guidance of a yoga therapist, including deep breathing, Suksham Vyayam, Anulom‐Vilom, Brahmari, progressive muscle relaxation (PMR) and deep breathing. Relaxation technique was demonstrated and administered to the mothers of neonates admitted to the NICU, the experimental group, by a yoga therapist and researcher on the day of enrolment |
| Art therapy interventions | |
| Narrative Writing and Art Therapy (Jouybari et al. 2020) | There are two interventional groups and one control in the study. In the art therapy group, the mothers completed the Parental Stressor Scale: Neonatal Intensive Care Unit (PSS: NICU) on the 2nd day of admission and drew at least three drawings until the 6th day. On the 6th day of admission, they were again requested to complete the PSS: NICU. In the narrative writing group, the mothers completed the PSS: NICU on the 2nd day of admission and then wrote at least three narratives until the 6th day. On the 6th day of admission, they were again requested to complete the PSS: NICU |
3.5. Maternal Stress
An educational intervention involving the distribution of information booklets demonstrated a significant effect on maternal stress levels, particularly in the ‘sight and sound’ domain of the PSS: NICU (p < 0.001) (Yilmaz and Küçük Alemdar 2022). Another study revealed a significant reduction in NICU environmental stress in the intervention group compared to the control group (p < 0.05), despite no significant differences in mean maternal stress scores after 10 days of the educational intervention (Khazaii et al. 2018). Five days of educational sessions in the NICU environment, the child's medical condition and treatment and participation in neonatal care activities, along with spousal support, resulted in a significant reduction in maternal stress levels within 1 week of intervention (p < 0.001) (Beheshtipour et al. 2014). The midwife‐based listening visit (MBLV) intervention showed a notable difference in mean stress levels at 4 and 8 weeks postintervention in the MBLV group (F(2,98) = 43.94, p < 0.001), with no such difference observed in the control group (Ebadi, Attarha, and Nokani 2022). Similarly, the Creating Opportunities for Parent Empowerment (COPE) programme, involving the completion of an activity booklet, led to significantly lower maternal stress levels (p < 0.001) (Mianaei et al. 2014). According to neonatologists' information, counselling sessions provided by another study significantly reduced stress levels across all three PSS‐NICU subscales, including ‘sight and sound’, ‘baby looks and behavior’ and ‘parental relationship with baby and role alteration’ (p < 0.05) (Chourasia et al. 2013).
Two quasi‐experimental studies employed two‐phase interventions (informational and observational). NICU‐related stress regarding sights, sounds and neonatal behaviour significantly decreased (p < 0.001), as did overall stress scores (p < 0.001) (Abdeyazdan et al. 2014; Goral and Geçkil 2022). Similarly, two experimental studies implemented emotional and supportive nursing care, including the distribution of a pictorial booklet about high‐risk neonatal care at the NICU. The intervention group experienced reductions in NICU environment‐related stress, infant behaviour and appearance, parental role alteration and overall stress (p < 0.001) (Al‐Maghaireh et al. 2020; Mousavi et al. 2021). Relaxation technique interventions, implemented by a yoga therapist for 10 days, lasted 30 min each. Mothers in the intervention group reported that the relaxation approach helped them manage NICU environmental stresses by reducing stress and anxiety. Compared to the control group, there was a significant reduction in maternal stress (p < 0.001) (Dabas et al. 2019). Mothers in both groups participated in either daily art therapy or narrative writing until the 6th day of NICU admission, resulting in a reduction in maternal stress compared to that in the control group (p < 0.003). However, the mean maternal stress scores did not significantly differ between the art therapy group and the narrative writing group. (p = 0.28) (Jouybari et al. 2020).
3.6. Coping Skills
Emotional and psychological supportive interventions significantly enhanced mothers' coping and active participation in neonatal care activities at the NICU compared to the control group (Goral and Geçkil 2022). In another study, nurses' regular communication with mothers, clarification of doubts and ability to participate in neonatal care activities significantly reduced maternal stress in the NICU (p < 0.001) and enhanced maternal participation in routine neonatal care activities in the NICU (Abdeyazdan et al. 2014). Seven days of information and supportive intervention during high‐risk neonatal NICU admission reduces maternal stress related to neonatal NICU admission and improves psychological resilience to cope with the situation through daily supportive care. Regular staff communication sessions with mothers helped them understand their roles and responsibilities in neonatal care in the NICU through coping skills (Al‐Maghaireh et al. 2020). Additionally, relaxation techniques, supervised by a yoga therapist for 10 days, lasting 30 min each, were reported to be helpful in coping with NICU environmental stresses by reducing maternal stress and anxiety (Dabas et al. 2019).
A structured nursing intervention programme was implemented among mothers at the NICU to enhance their health literacy on high‐risk neonatal care activities and coping skills during NICU admission. In the intervention group, mothers' stress levels were significantly lower on the ‘communication with NICU staff’ and ‘parental role and relationship with baby’ subscales (p < 0.001). After 2 weeks of intervention, mothers' ability to provide care at the NICU and cope with stress and anxiety notably improved (p < 0.001) (Ong et al. 2019). Family‐centred care (FCC) was facilitated through discussion sessions. Continuous room‐in significantly enhanced maternal coping skills with stressors related to neonatal hospitalisation and ‘parental role and relationship with baby’ (p < 0.001). The participation of mothers in neonatal care activities plays a significant role in enhancing maternal competencies in neonatal care activities and coping skills (Mirlashari et al. 2021).
3.7. Breastfeeding Frequency, Milk Output and Bonding
The Maternal Kangaroo Care Education Program (MKC‐EP) follows Kangaroo Care (KC) guidelines and protocols. Mothers receive guidance on challenging KC techniques through demonstrations and are encouraged to practice KC for at least 1 h daily, aiming for 4–5 h per week. This results in improved maternal understanding of KC, leading to reduced stress levels upon initiating skin‐to‐skin care. Moreover, perceived barriers to KC significantly decrease, facilitating successful implementation (p < 0.001) (Samsudin et al. 2023).
Relaxation technique interventions, supervised by a yoga therapist, consisted of 30‐min sessions over 10 days. Mothers in the intervention group reported that these techniques help reduce stress and anxiety levels, subsequently increasing breastfeeding frequency and milk production (p = 0.05) (Dabas et al. 2019).
Each intervention strategy has distinct effects on reducing maternal stress and anxiety, improving coping mechanisms during NICU admission and enhancing early mother–child interactions, bonding and long‐term well‐being (Figure 2).
FIGURE 2.
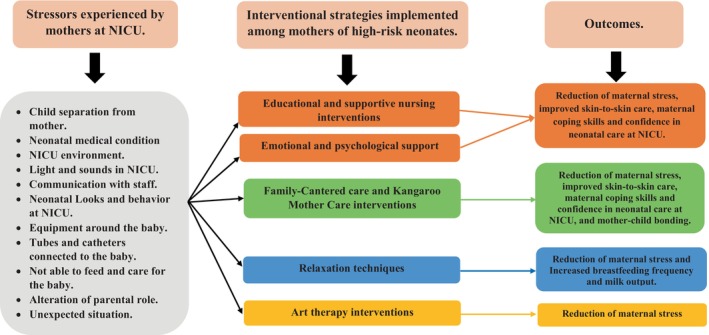
Stressors experienced by the mothers of high‐risk neonates and interventional strategies impact maternal stress in the NICU.
4. Discussion
The scoping review included 15 studies conducted in LMICs (Iran, India, Malaysia, Jordan and Turkey) examining various early interventions to reduce maternal stress and enhance coping skills in the NICU. Health workers, particularly nurses, implemented early interventions among mothers, either individually or in groups, with support from family and peers. Most of the interventions reduce maternal stress (Al‐Maghaireh et al. 2020; Beheshtipour et al. 2014; Chourasia et al. 2013; Dabas et al. 2019; Ebadi, Attarha, and Nokani 2022; Goral and Geçkil 2022; Mianaei et al. 2014; Yilmaz and Küçük Alemdar 2022). However, variability exists in the literature. For instance, some interventions were effective in reducing maternal stress related to ‘sights and sounds’, ‘infant appearance and behavior’, (Khazaii et al. 2018), ‘parental role alteration and relationship with baby’ (Abdeyazdan et al. 2014; Mousavi et al. 2021; Samsudin et al. 2023) and overall stress level (Ong et al. 2019). Certain therapies notably enhance maternal coping skills during neonatal hospitalisation (Abdeyazdan et al. 2014; Al‐Maghaireh et al. 2020; Dabas et al. 2019; Goral and Geçkil 2022; Mirlashari et al. 2021; Ong et al. 2019). Conversely, one study revealed no significant difference between narrative writing and art therapy in reducing maternal stress.
4.1. Implications of Education Programmes
Studies have consistently shown that maternal stress levels and coping skills are influenced by maternal demographic factors such as education level and occupation status in LMICs (Ebadi, Attarha, and Nokani 2022; Mirlashari et al. 2021). Prematurity, low birth weight, neonatal medical conditions and the NICU environment are significant stressors during neonatal NICU admission, exacerbating parental stress and depressive symptoms (Abdeyazdan et al. 2014; Yilmaz and Küçük Alemdar 2022; Siva, Phagdol, et al. 2023; Forde, Fang, and Miaskowski 2022; Buffa et al. 2018). Additionally, the NICU environment, including sensory stimuli and the appearance of the baby, can exacerbate parental stress and depression (Buffa et al. 2018; Siva, Phagdol, et al. 2023). Due to limited healthcare access and resources, the healthcare system of LMICs should prioritise interventions that empower mothers through effective communication and education sessions in NICUs (Nurlaila et al. 2022; Siva, Phagdol, et al. 2023). Providing clear information through education sessions and booklets enhances parental participation both in the NICU and at home after discharge (Khazaii et al. 2018; Siva et al. 2024). Bedside educational sessions, along with daily neonatal updates through telephone calls and SMS messages, are effective at mitigating stress levels among mothers in the intervention group (Ong et al. 2019). Moreover, verbal information about the child's condition, treatment plan and NICU environment adjustment during neonatal visits at NICU, along with counselling sessions, can minimise maternal stress (Beheshtipour et al. 2014; Chourasia et al. 2013).
4.2. Implications for Family‐Centred Care Interventions
In LMICs such as Iran, parental participation in neonatal care in the NICU often has less of a priority (Mirlashari et al. 2021). FCC in NICUs, which emphasises improved communication, maternal participation in neonatal care activities and emotional support, has been proven to be beneficial for mothers to reduce stress levels and enhance neonates' clinical outcomes (Mirlashari et al. 2021; Ong et al. 2019; Samsudin et al. 2023). FCC is likely to alleviate maternal stress by enabling mothers to visit, hold, provide KC and participate in primary care activities, thereby enhancing their responsiveness to infants and fostering mother–infant bonding (Soni and Tscherning 2021). Research by Mirlashari et al. (2021) and Ong et al. (2019) suggested that FCC, along with structured nursing interventions, positively influences overall developmental care, consequently reducing maternal stress during neonatal admissions. Furthermore, feedback from these mothers underscores various coping skills, including active participation in care, seeking information, relying on family and friends and connecting with other parents (Mirlashari et al. 2021). Moreover, healthcare providers in LMICs, given their resources, can enable mothers to visit their infants at their convenience, openly express their emotions, close communication gaps and address concerns during subsequent visits to the NICU (Ebadi, Attarha, and Nokani 2022).
4.3. Implications for Emotional and Psychological Support Interventions
Four studies (Abdeyazdan et al. 2014; Al‐Maghaireh et al. 2020; Goral and Geçkil 2022; Mousavi et al. 2021) focused on providing emotional and psychological support to mothers to reduce maternal stress, but their approaches varied significantly. Cultural and economic factors may account for the observed differences in the effectiveness of maternity support programmes (Hirtz et al. 2023). Training and offering higher levels of psychological and emotional support yield more flexible and rapid reductions in maternal stress where there are fewer literacy levels, such as LMICs (Akbarian et al. 2018; Kruk et al. 2022; Mousavi et al. 2021). Emotional support training programmes can alleviate maternal stress by providing continuous training and emotional support, empowering mothers about their neonates' medical status and teaching coping skills throughout the neonatal NICU stay (Al‐Maghaireh et al. 2020). Although relaxation techniques have rarely been studied in LMICs (1 of 15 studies, 6.6%), they have significant potential to reduce maternal stress. The stress and anxiety experienced by mothers of hospitalised neonates can hinder the oxytocin and prolactin reflexes necessary for lactation (UvnäsMoberg et al. 2020; Walter, Abele, and Plappert 2021), especially in preterm mothers (Levene et al. 2022). Relaxation methods can lower stress levels, including auditory, cognitive and muscle relaxation. Dabas et al. (2019) reported that audio‐assisted relaxation techniques successfully reduced maternal stress and improved milk production. It is advisable to include maternal relaxation as a standard part of NICU care, as it is straightforward, practical, cost‐effective and resource efficient (Nurlaila et al. 2022). Mothers have reported that relaxation interventions are beneficial, soothing and easy to follow (Dabas et al. 2019).
4.4. Implications for Research
The synthesis also highlights substantial variability already observed in the literature from the NICU. For example, some of the interventions had immediate effects on maternal stress and coping skills, and few reported that maternal stress was reduced after a couple of weeks when the baby's condition improved, including regular encouragement from healthcare professionals. LMICs often face resource constraints and disparities in healthcare access (Burger et al. 2020). NICU experience is emotionally challenging, and maternal stress can have significant implications for mental health, bonding, breastfeeding, parental empowerment and long‐term outcomes in LMICs with limited healthcare resources (Kruk et al. 2022; Siva, Phagdol, et al. 2023). Moreover, there is a lack of comprehensive, in‐depth reviews and navigation intervention strategies in clinical settings to reduce maternal stress levels in the NICU even after discharge to improve long‐term health outcomes in LMICs. Therefore, implementing effective healthcare interventions can contribute to addressing health inequities by ensuring that all mothers, regardless of education and socioeconomic status, receive appropriate support and care. This can help families and healthcare systems improve expected health outcomes for vulnerable populations. However, this review emphasises that prioritising unique needs, implementing early healthcare interventions and incorporating them into standard neonatal care at NICUs in LMICs are essential for the psychological well‐being of mothers and high‐risk neonatal clinical outcomes in the future.
4.5. Conclusion
Healthcare professionals, especially nurses, play a crucial role in promptly identifying maternal stress and stressors in NICU settings. Involving mothers in neonatal care activities, such as family‐centred care and emotional support interventions coupled with educational sessions, effectively reduces maternal stress and improves coping skills. It is necessary for healthcare systems in LMICs to integrate these interventions into standard NICU policies to enhance maternal psychological health and improve maternal competencies in neonatal care activities during neonatal NICU admission within existing resources.
4.6. Limitations
In this scoping review, several limitations pose challenges to effectively implementing interventions across LMICs. Resource constraints, including limited access to specialised healthcare facilities, trained personnel and essential medical equipment, hinder the implementation of complex interventions. Additionally, the cultural and societal factors prevalent in LMICs may impact the acceptance and efficacy of interventions, necessitating understanding and addressing cultural practices and preferences for successful implementation. Moreover, the ongoing support, training and resources required by many interventions could be strained by limited healthcare systems.
Due to access limitations, we did not search the PsycINFO database, and this scoping review focused solely on articles published in English and conducted within LMICs, resulting in a few methodological constraints.
Author Contributions
N.S. and B.V. conceived the topic. B.S.N. and L.E.S.L. conceptualised the research project, its goals and hypotheses. N.S. and B.V. designed the search strategies and conducted the search process. B.S.N. and J.A.N. has provided the inputs in methodology. N.S. and B.V. independently screened and extracted the data. N.S. wrote the manuscript with the support of B.V., J.A.N. and B.S.N. The primary and independent authors received valid input from all authors. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Supporting information
Data S1.
Acknowledgements
Authors appreciate the technical assistance and resources the Manipal Academy of Higher Education (MAHE), Manipal and ICMR SRF provided for supporting this research work.
Funding: This work was supported by the Indian Council of Medical Research, IRIS Number—2021‐8364.
Contributor Information
N. Siva, Email: siva.n@learner.manipal.edu.
Binil Velayudhan, Email: vp.binil@manipal.edu.
Baby S. Nayak, Email: baby.s@manipal.edu.
Leslie Edward S. Lewis, Email: leslie.lewis@manipal.edu.
Faiza Iqbal, Email: faiza.iqbal@learner.manipal.edu.
Judith Angelitta Noronha, Email: judit.n@manipal.edu.
Data Availability Statement
This review used secondary data freely available within the publications reviewed. For more information, please contact the authors.
References
- Abdeyazdan, Z. , Shahkolahi Z., Mehrabi T., and Hajiheidari M.. 2014. “A Family Support Intervention to Reduce Stress Among Parents of Preterm Infants in Neonatal Intensive Care Unit.” Iranian Journal of Nursing and Midwifery Research 19, no. 4: 349–353. [PMC free article] [PubMed] [Google Scholar]
- Akbarian, Z. , Kohan S., Nasiri H., and Ehsanpour S.. 2018. “The Effects of Mental Health Training Program on Stress, Anxiety, and Depression During Pregnancy.” Iranian Journal of Nursing and Midwifery Research 23, no. 2: 93–97. 10.4103/ijnmr.IJNMR_207_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Maghaireh, D. F. , Khalaf I. A., Abdullah K. L., Chan C. M., Basyoun N. R., and Kawafha M. M.. 2020. “The Effect of an Emotional Support Training Program on Acute Stress Disorder Among Mothers of Preterm Infants Hospitalized in Neonatal Intensive Care Units.” Journal of Neonatal Nursing 26, no. 5: 273–277. 10.1016/j.jnn.2020.06.003. [DOI] [Google Scholar]
- Beheshtipour, N. , Baharlu S. M., Montaseri S., and Razavinezhad Ardakani S. M.. 2014. “The Effect of the Educational Program on Iranian Premature Infants' Parental Stress in a Neonatal Intensive Care Unit: A Double‐Blind Randomized Controlled Trial.” International Journal of Community Based Nursing and Midwifery 2, no. 4: 240–250. [PMC free article] [PubMed] [Google Scholar]
- Buffa, G. , Dahan S., Sinclair I., et al. 2018. “Prenatal Stress and Child Development: A Scoping Review of Research in Low‐ and Middle‐Income Countries.” PLoS One 13, no. 12: e0207235. 10.1371/journal.pone.0207235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger, M. , Hoosain M., Einspieler C., Unger M., and Niehaus D.. 2020. “Maternal Perinatal Mental Health and Infant and Toddler Neurodevelopment—Evidence From Low and Middle‐Income Countries. A Systematic Review.” Journal of Affective Disorders 268: 158–172. 10.1016/j.jad.2020.03.023. [DOI] [PubMed] [Google Scholar]
- Chourasia, N. , Surianarayanan P., Bethou A., and Bhat V.. 2013. “Stressors of NICU Mothers and the Effect of Counseling‐Experience From a Tertiary Care Teaching Hospital, India.” Journal of Maternal‐Fetal & Neonatal Medicine: The Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians 26, no. 6: 616–618. 10.3109/14767058.2012.743522. [DOI] [PubMed] [Google Scholar]
- Dabas, S. , Joshi P., Agarwal R., Yadav R. K., and Kachhawa G.. 2019. “Impact of Audio Assisted Relaxation Technique on Stress, Anxiety and Milk Output Among Postpartum Mothers of Hospitalized Neonates: A Randomized Controlled Trial.” Journal of Neonatal Nursing 25, no. 4: 200–204. 10.1016/j.jnn.2019.03.004. [DOI] [Google Scholar]
- Ebadi, N. , Attarha M., and Nokani M.. 2022. “The Effect of Midwife‐Based Listening Visit on Stress, Anxiety, and Depression Among Mothers of Premature Infants in the Neonatal Intensive Care Unit: Randomized Clinical Trial Study.” Iranian Journal of Nursing and Midwifery Research 27, no. 6: 581–586. 10.4103/ijnmr.ijnmr_344_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forde, D. , Fang M. L., and Miaskowski C.. 2022. “A Systematic Review of the Effects of Skin‐To‐Skin Contact on Biomarkers of Stress in Preterm Infants and Parents.” Advances in Neonatal Care 22, no. 3: 223–230. 10.1097/ANC.0000000000000905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goral, E. , and Geçkil E.. 2022. “The Effect of a Comprehensive Support Program on the Stress Level of Mothers in a Neonatal Intensive Care Unit.” Nursing Practice Today 9, no. 1: 54–61. 10.18502/npt.v9i1.7331. [DOI] [Google Scholar]
- Hirtz, K. , Lau M., Hall A., and Fucile S.. 2023. “Interventions Aimed at Reducing the Stress of Mother's Whose Infant Is Born Premature: A Scoping Review.” Journal of Neonatal Nursing 29: 602–611. 10.1016/j.jnn.2022.12.003. [DOI] [Google Scholar]
- Iqbal, F. , Lewis L. E. S., Siva N., Vandana K. E., Purkayastha J., and Shenoy P. A.. 2023. “Modulation of Gut Microbiota: An Emerging Consequence in Neonatal Sepsis.” Clinical Epidemiology and Global Health 20: 101245. 10.1016/j.cegh.2023.101245. [DOI] [Google Scholar]
- Jagtap, A. , Jagtap B., Jagtap R., Lamture Y., and Gomase K.. 2023. “Effects of Prenatal Stress on Behavior, Cognition, and Psychopathology: A Comprehensive Review.” Cureus 15, no. 10: e47044. 10.7759/cureus.47044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jouybari, L. , Abbariki E., Jebeli M., et al. 2020. “Comparison of the Effect of Narrative Writing and Art Therapy on Maternal Stress in Neonatal Intensive Care Settings.” Journal of Maternal‐Fetal & Neonatal Medicine: The Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians 33, no. 4: 664–670. 10.1080/14767058.2018.1499719. [DOI] [PubMed] [Google Scholar]
- Kegler, J. J. , Neves E. T., Silva A. M. d., Jantsch L. B., Bertoldo C. d. S., and Silva J. H. d.. 2019. “Stress in Parents of Newborns in a Neonatal Intensive Care Unit.” Escola Anna Nery 23: e20180178. 10.1590/2177-9465-EAN-2018-0178. [DOI] [Google Scholar]
- Khazaii, T. , Taheri F., Hosseini S., Parhiz Z., and Namdari S.. 2018. “The Effects of Preterm Infant Care Education on Stress Among the Mothers of Preterm Infants Hospitalized in Neonatal Intensive Care Units.” Modern Care Journal in Press. 15, no. 1: 1–6. 10.5812/modernc.69476. [DOI] [Google Scholar]
- Khoddam, H. , Modanloo M., Mehrdad N., Heydari F., and Talebi R.. 2023. “Nurses' Experience of Integrating Evidence‐Based Changes Into Their Practice: A Qualitative Study.” Nursing Open 10, no. 9: 6465–6478. 10.1002/nop2.1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk, M. E. , Lewis T. P., Arsenault C., et al. 2022. “Improving Health and Social Systems for all Children in LMICs: Structural Innovations to Deliver High‐Quality Services.” Lancet (London, England) 399, no. 10337: 1830–1844. 10.1016/S0140-6736(21)02532-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, N. , and Mallick A. K.. 2020. “Maternal Stress in Neonatal Intensive Care Unit Very Often Overlooked by Health Professionals.” Industrial Psychiatry Journal 29, no. 1: 130–133. 10.4103/ipj.ipj_88_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levene, I. , Bell J. L., Cole C., et al. 2022. “Comparing the Effect of a Lactation‐Specific Relaxation and Visualization Intervention Versus Standard Care on Lactation and Mental Health Outcomes in Mothers of Very Premature Infants (The EXPRESS Trial): Study Protocol for a Multicenter, Unmasked, Randomized, Parallel‐Group Trial.” Trials 23, no. 1: 611. 10.1186/s13063-022-06570-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lomotey, A. Y. , Bam V., Diji A. K.‐A., Asante E., Asante H. B., and Osei J.. 2020. “Experiences of Mothers With Preterm Babies at a Mother and Baby Unit of a Tertiary Hospital: A Descriptive Phenomenological Study.” Nursing Open 7, no. 1: 150–159. 10.1002/nop2.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahovo, R. , and Velaphi S.. 2019. “Duration of Hospital Stay and Factors Associated With Prolonged Hospital Stay in Very Low Birth Weight Infants Surviving to Hospital Discharge.” Journal of Pediatrics, Perinatology and Child Health 3, no. 4: 208–220. [Google Scholar]
- Mianaei, S. J. , Karahroudy F. A., Rassouli M., and Tafreshi M. Z.. 2014. “The Effect of Creating Opportunities for Parent Empowerment Program on Maternal Stress, Anxiety, and Participation in NICU Wards in Iran.” Iranian Journal of Nursing and Midwifery Research 19, no. 1: 94–100. [PMC free article] [PubMed] [Google Scholar]
- Mianda, S. , Todowede O., and Schneider H.. 2023. “Service Delivery Interventions to Improve Maternal and Newborn Health in Low‐ and Middle‐Income Countries: Scoping Review of Quality Improvement, Implementation Research and Health System Strengthening Approaches.” BMC Health Services Research 23, no. 1: 1223. 10.1186/s12913-023-10202-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirlashari, J. , Holsti L., Pooraboli B., et al. 2021. “The Effect of a Group Discussion About Premature Newborns Between Mothers and Healthcare Team on Mother’ Stress and Coping in Neonatal Intensive Care Unit.” Journal of Neonatal Nursing 27, no. 4: 263–268. 10.1016/j.jnn.2020.11.001. [DOI] [Google Scholar]
- Mousavi, S. S. , Keramat A., Chaman R., Mohagheghi P., Mousavi S. A., and Khosravi A.. 2021. “Impact of Maternity Support Program on the Stress of Mothers in the First Encounter With the Preterm Infants.” International Journal of Preventive Medicine 12: 68. 10.4103/ijpvm.IJPVM_314_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurlaila, Herini E. S., Hartini S., and Kusuma M. T. P. L.. 2022. “Interventions to Reduce Parental Stress and Increase Readiness of Parents With Preterm Infants in the Neonatal Intensive Care Unit: A Scoping Review.” Journal of Neonatal Nursing 29: 595–601. 10.1016/j.jnn.2022.12.002. [DOI] [Google Scholar]
- Ong, S. L. , Abdullah K. L., Danaee M., et al. 2019. “The Effectiveness of a Structured Nursing Intervention Program on Maternal Stress and Ability Among Mothers of Premature Infants in a Neonatal Intensive Care Unit.” Journal of Clinical Nursing 28, no. 3–4: 641–649. 10.1111/jocn.14659. [DOI] [PubMed] [Google Scholar]
- Oyekunle, O. O. , Bella‐Awusah T., Ayede A. I., Omigbodun O. O., and Ani C. C.. 2021. “Effect of a Brief Supportive and Educational Intervention on the Psychological Well‐Being of Mothers With Babies in Neonatal Wards of a Tertiary Hospital in Ibadan, Nigeria.” Journal of Tropical Pediatrics 67, no. 2: fmab038. 10.1093/tropej/fmab038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phagdol, T. , Nayak B. S., Lewis L. E., Margaret B., and George A.. 2022. “Designing a Mobile Health Intervention for Preterm Home Care: Application of Conceptual Framework.” Public Health Nursing (Boston, Mass.) 39, no. 1: 296–302. 10.1111/phn.13020. [DOI] [PubMed] [Google Scholar]
- Pichler‐Stachl, E. , Urlesberger P., Mattersberger C., et al. 2019. “Parental Stress Experience and Age of Mothers and Fathers After Preterm Birth and Admission of Their Neonate to Neonatal Intensive Care Unit; A Prospective Observational Pilot Study.” Frontiers in Pediatrics 7, 439: 1–4. 10.3389/fped.2019.00439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samsudin, S. , Chui P. L., Kamar A. B. A., and Abdullah K. L.. 2023. “Maternal Kangaroo Care Education Program in the Neonatal Intensive Care Unit Improved Mothers' Perceptions, Knowledge, Perceived Barriers and Stress Relates to Premature Infant.” Nursing Open 10, no. 1: 349–357. 10.1002/nop2.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siva, N. , Nayak B. S., Lewis L. E. S., et al. 2023. “Involvement of Mothers in High‐Risk Neonatal Care: A Capacity Building Program for Neonatal Nurses.” Journal of Neonatal Nursing 29, no. 1: 91–96. 10.1016/j.jnn.2022.03.001. [DOI] [Google Scholar]
- Siva, N. , Nayak B. S., Lewis L. E. S., et al. 2024. “Randomized Controlled Trial on the Effect of the Neonatal Nurse Navigator Program on Maternal Stress and Neonatal Cortisol Levels.” Journal of Obstetric, Gynecologic & Neonatal Nursing 53, no. 2: 185–196. 10.1016/j.jogn.2023.11.009. [DOI] [PubMed] [Google Scholar]
- Siva, N. , Phagdol T., Nayak B. S., et al. 2023. “Stress and Stressors Experienced by the Parents of High‐Risk Neonates Admitted in Neonatal Intensive Care Unit: Systematic Review and Meta‐Analysis Evidence Available From India.” Stress and Health: Journal of the International Society for the Investigation of Stress 40, no. 2: 1–16. 10.1002/smi.3301. [DOI] [PubMed] [Google Scholar]
- Soni, R. , and Tscherning C.. 2021. “Family‐Centered and Developmental Care on the Neonatal Unit.” Pediatrics and Child Health 31, no. 1: 18–23. 10.1016/j.paed.2020.10.003. [DOI] [Google Scholar]
- Toptas, M. , Sengul Samanci N., Akkoc İ., et al. 2018. “Factors Affecting the Length of Stay in the Intensive Care Unit: Our Clinical Experience.” BioMed Research International 2018: e9438046. 10.1155/2018/9438046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UvnäsMoberg, K. , Ekström‐Bergström A., Buckley S., et al. 2020. “Maternal Plasma Levels of Oxytocin During Breastfeeding—A Systematic Review.” PLoS One 15, no. 8: e0235806. 10.1371/journal.pone.0235806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter, M. H. , Abele H., and Plappert C. F.. 2021. “The Role of Oxytocin and the Effect of Stress During Childbirth: Neurobiological Basics and Implications for Mother and Child.” Frontiers in Endocrinology 12: 742236. 10.3389/fendo.2021.742236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2023. Mother Newborn Care Unit: An Innovation in Care of Small and Sick Newborns. https://www.who.int/southeastasia/news/feature‐stories/detail/mother‐newborn‐care‐unit.
- World Health Organization (WHO). Global Health Observatory (GHO) Data . 2020. Child Mortality and Causes of Death 2020. Geneva, Switzerland: World Health Organization. https://www.who.int/data/gho/data/themes/topics/topic‐details/GHO/child‐mortality‐and‐causes‐of‐death. [Google Scholar]
- Yilmaz, G. , and Küçük Alemdar D.. 2022. “The Effect of Supportive Nursing Interventions on Reducing Stress Levels of Mothers of Infants in the Neonatal Intensive Care Unit: A Randomized Controlled Trial.” Clinical Nursing Research 31, no. 5: 941–951. 10.1177/10547738211047359. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1.
Data Availability Statement
This review used secondary data freely available within the publications reviewed. For more information, please contact the authors.


