Abstract
Sleep difficulties affect up to 98% of Parkinson’s disease (PD) patients and are often not well treated. How globus pallidus internus (GPi)-DBS could help is less understood. We retrospectively analyzed sleep outcomes in 32 PD patients after GPi-DBS with a two-year follow-up. We observed high heterogeneity in sleep response to pallidal stimulation: 16 patients showed clinically meaningful improvement, 9 had minor changes, and 7 experienced worsened sleep quality, with no overall significant change on the Parkinson’s Disease Sleep Scale-2 (P = 0.19). Further analysis revealed that stimulation of the left sensorimotor GPi was significantly associated with sleep improvement. Fiber tracts from the left sensorimotor GPi to the bilateral sensorimotor cortex, right GPi, brainstem, and bilateral cerebellum were linked to better sleep, while projections to the left hippocampus correlated with worsened sleep. These findings may guide personalized GPi-DBS lead placement to optimize sleep outcomes in PD.
Subject terms: Parkinson's disease, Outcomes research, Circadian rhythms and sleep
Introduction
Sleep disturbances have been observed in 75‒98% of patients with Parkinson’s disease (PD), though no satisfactory treatment is available1,2. PD motor symptoms could interrupt the initiation or maintenance of sleep1. Disruption of basal ganglia function also plays an important role in sleep disturbances3. Deep brain stimulation (DBS) is a well-established treatment for control of motor symptoms in PD. Stimulation of the subthalamic nucleus (STN) has been proven to alleviate sleep symptoms by modulating basal ganglia neuronal activity in patients with PD4.
Globus pallidus internus (GPi) DBS is as effective as STN-DBS for motor symptoms. Although it is preferred for patients with worse non-motor symptoms5–8, its effects on sleep are not well studied. Nevertheless, several studies have shown that GPi-DBS can induce a general increase in sleep quality5,9–11. Dafsari and colleagues reported that GPi-DBS significantly improved patients’ sleep/fatigue subdomain on the Non-Motor Symptoms Scale12,13. Weaver and colleagues showed that GPi-DBS could improve sleep time, sleep quality, and alleviate daytime fatigue8,14. We presume GPi-DBS might have a positive effect on sleep, but to the best of our knowledge, suitably powered research with large sample size and prolonged follow-up has not yet been conducted to comprehensively examine the effects of pallidal stimulation on sleep in patients with PD. Additionally, it is unclear how GPi-DBS can affect basal ganglia function as it relates to sleep. GPi is the outflow of the basal ganglia through the thalamus, which has inhibitory output to sleep-wake circuitry structures such as the basal forebrain and pedunculopontine nucleus15–18. Strong sleep-stage dependency in pallidal electrophysiological signals was found recently in PD by our team’s research19. We hypothesize that pallidal stimulation has a distinct impact on sleep compared to STN-DBS.
In this study, we investigated whether GPi-DBS would ameliorate or deteriorate sleep quality in patients with PD. We first examined clinical information to validate the effects of GPi-DBS on sleep quality and to understand how divergencies in clinical features would lead to differences in sleep quality. Secondly, we analyzed the location of electrode contacts through brain imaging. We reconstructed individual-level electrode positions and volume of tissue activated (VTA), followed by a group-level optimal stimulation site and a structural connectome seeded by an optimal stimulation site, which was then correlated with sleep improvement.
Results
Demographic statistics and clinical results
A total of 32 PD patients after GPi-DBS were reOcruited. The follow-up time for collecting PDSS-2 and RBDSQ were 1.67 ± 1.02 years. The enrollment and exclusion process are shown in Fig. 1. There were 20 males and 12 females included, with an average age of 62 ± 9 years and an average disease duration of 11 ± 4 years. Among them, 14 patients’ predominant symptoms were tremor, 8 were bradykinesia, 3 were rigidity, 5 were mixed symptoms, and 2 were other20. Detailed baseline information can be seen in Table 1.
Fig. 1. Subject screening workflow.
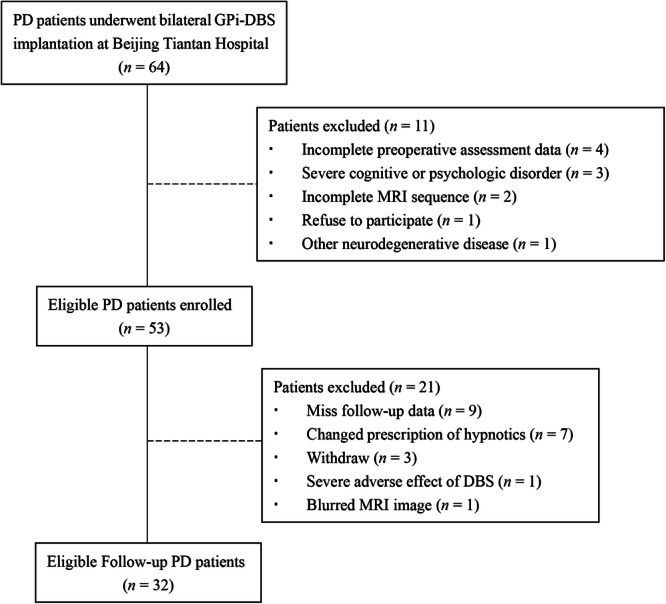
PD: Parkinson’s disease; GPi-DBS: globus pallidus internus deep brain stimulation.
Table 1.
Patient demographics and correlations with PDSS-2 improvement
| Total | Estimates for PDSS-2 improvement (n = 32) | Estimates for RBD improvement (n = 26) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| mean | sd | Estimate | p | p(FDR) | p(FWE) | Estimate | p | p(FDR) | p(FWE) | |
| Numer of Patients (N) | 32 | |||||||||
| Age | 62.03 | 9.39 | 0.45 | 0.07 | 0.24 | 1.00 | 0.08 | 0.59 | 0.94 | 1.00 |
| sex (ratio of male) | 0.38 | 0.48 | −0.55 | 0.91 | 0.91 | 1.00 | −3.35 | 0.18 | 0.92 | 1.00 |
| Disease Duration | 10.74 | 3.76 | 0.97 | 0.06 | 0.24 | 0.88 | 0.59 | 0.07 | 0.92 | 1.00 |
| Education Years | 10.33 | 4.31 | −0.68 | 0.25 | 0.42 | 1.00 | −0.13 | 0.69 | 0.94 | 1.00 |
| Age of Onset | 50.27 | 9.33 | 0.31 | 0.23 | 0.42 | 1.00 | −0.01 | 0.92 | 0.94 | 1.00 |
| Follow-up Years | 1.67 | 1.02 | −1.00 | 0.67 | 0.77 | 1.00 | −0.01 | 0.92 | 0.94 | 1.00 |
| baseline motor and non-motor symptoms | ||||||||||
| MDS-UPDRS III(off) | 47.72 | 20.98 | −0.09 | 0.31 | 0.47 | 1.00 | 0.26 | 0.37 | 0.94 | 1.00 |
| MDS-UPDRS III(on) | 20.75 | 13.47 | 0.11 | 0.42 | 0.52 | 1.00 | −0.02 | 0.94 | 0.94 | 1.00 |
| Hoehn-Yahr Stage | 2.90 | 0.69 | 6.02 | 0.08 | 0.24 | 1.00 | 2.36 | 0.54 | 0.94 | 1.00 |
| IRLS | 9.00 | 9.85 | 0.28 | 0.02 | 0.24 | 0.33 | 0.07 | 0.64 | 0.94 | 1.00 |
| HAMA | 15.84 | 6.34 | 0.50 | 0.16 | 0.34 | 1.00 | 0.25 | 0.25 | 0.92 | 1.00 |
| HAMD | 16.72 | 8.24 | 0.46 | 0.10 | 0.25 | 1.00 | 0.06 | 0.68 | 0.94 | 1.00 |
| PDQ39 | 57.81 | 23.11 | 0.09 | 0.38 | 0.52 | 1.00 | 0.02 | 0.72 | 0.94 | 1.00 |
| ASP_SCOPA_AUT | 23.19 | 9.67 | 0.44 | 0.07 | 0.24 | 1.00 | -0.02 | 0.88 | 0.94 | 1.00 |
MDS-UPDRS movement disorder society-unified Parkinson’s disease rating scale, IRLS index of restless legs syndrome, HAMA Hamilton anxiety scale, HAMD Hamilton depression scale, PDQ-39 Parkinson’s disease quality of life-39 items, SCOPA-AUT scale for outcomes in PD for autonomic symptoms.
*significant result with P < 0.05.
**significant result with P < 0.05 – not significant after FWE correction.
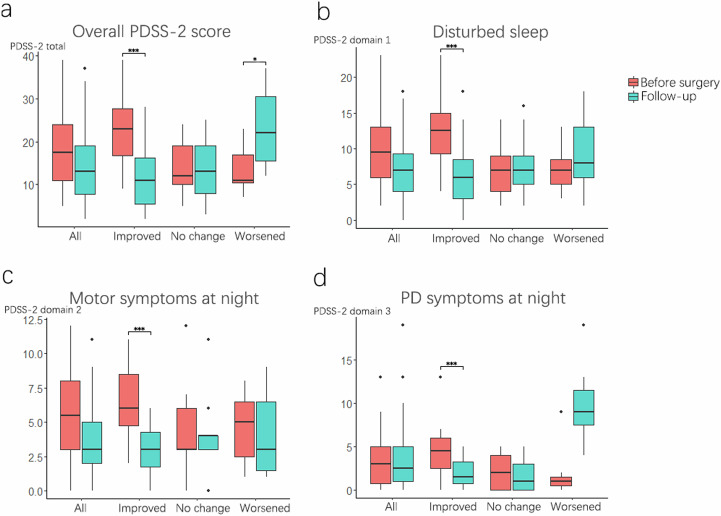
The mean Parkinson’s Disease Sleep Scale 2 (PDSS-2) after GPi-DBS was 14.66 ± 8.73 compared to 18.38 ± 8.18 at pre-surgery, which was not a significant change (P = 0.17). Regression analysis also revealed that no clinical characteristics or pre-surgery Parkinson’s disease assessment scale scores, such as UPDRS, HAMA, HAMD, and IRLS, were associated with sleep improvement. (Table 1). Additionally, according to previous studies, patients with a PDSS-2 score ≥14 are considered poor sleepers21,22. Among the 32 patients, the number of poor sleep patients changed from 21 (65.62%) to 14 (43.75%) at 2-year follow-up (χ2 = 3.27, df = 1, P = 0.07). Furthermore, the clinically minimal important difference (MID) for PDSS-2 was 2.07 for improvement, and 3.44 for deterioration (Table 2). Sixteen patients (50%) had an improved PDSS-2 score (group 1), seven patients (22%) had worsened sleep (group 2), and nine (28%) patients had a minor change (group 3). The change in PDSS-2 score in the three groups is shown in Fig. 2. The three subdomains of the PDSS-2 among the three groups were compared, where we found all three subdomains, i.e., disturbed sleep, motor symptoms at night, and score for PD symptoms at night, were significantly improved in group 1 (PDSS-2 improved patients) (Fig. 2). On the contrary, in group 2 (PDSS-2 worsened patients), only PD symptoms at night were significantly worsened, while motor symptoms at night (P = 0.80) and disturbed sleep (P = 0.55) were not significantly changed.
Table 2.
Demographic data for the three MID-based groups
| Total | PDSS2 improved | PDSS2 not changed | PDSS2 worsened | |||||
|---|---|---|---|---|---|---|---|---|
| mean | sd | mean | sd | mean | sd | mean | Sd | |
| Numer of Patients (N) | 32 | 16 | 9 | 7 | ||||
| Age | 62.03 | 9.39 | 63.08 | 7.85 | 61.78 | 9.51 | 59.97 | 6.81 |
| ratio of male | 0.38 | 0.48 | 0.50 | 0.50 | 0.22 | 0.42 | 0.29 | 0.49 |
| Disease Duration | 10.74 | 3.76 | 10.38 | 3.82 | 13.11 | 3.09 | 8.49 | 2.97 |
| Education Years | 10.33 | 4.31 | 10.21 | 4.00 | 11.00 | 3.92 | 9.71 | 4.50 |
| Age of Onset | 50.27 | 9.33 | 51.72 | 6.71 | 47.89 | 11.05 | 49.67 | 7.07 |
| Follow-up Years | 1.67 | 1.02 | 1.48 | 0.94 | 1.86 | 1.15 | 1.89 | 0.97 |
| MDS-UPDRS III(off) | 47.72 | 21.31 | 44.63 | 17.45 | 48.00 | 30.33 | 53.00 | 21.18 |
| MDS-UPDRS III(on) | 21.42 | 13.37 | 22.25 | 12.43 | 19.86 | 13.74 | 21.13 | 16.39 |
| Hoehn-Yahr Stage | 2.90 | 0.69 | 2.93 | 0.90 | 2.81 | 0.97 | 2.93 | 0.24 |
| LEDD | 810.68 | 406.48 | 756.02 | 413.46 | 789.29 | 458.72 | 924.51 | 375.44 |
| IRLS | 9.00 | 9.85 | 5.40 | 10.80 | 5.83 | 8.25 | 12.08 | 8.67 |
| HAMA | 15.84 | 6.34 | 13.00 | 2.39 | 17.00 | 6.00 | 16.40 | 7.06 |
| HAMD | 16.72 | 8.24 | 17.14 | 7.75 | 14.33 | 5.58 | 17.81 | 9.08 |
| PDQ39 | 57.81 | 23.11 | 57.57 | 21.72 | 56.11 | 17.46 | 58.81 | 25.45 |
| SCOPA_AUT | 23.19 | 9.67 | 21.86 | 10.67 | 23.67 | 12.20 | 23.48 | 7.04 |
| DBS parameters | ||||||||
| Pulse width | 79.69 | 15.29 | 83.75 | 16.68 | 74.44 | 14.88 | 77.14 | 11.13 |
| Frequency | 132.66 | 19.59 | 132.50 | 18.62 | 132.22 | 26.94 | 133.57 | 12.15 |
| Amplitude (Voltage) | 2.62 | 0.78 | 2.79 | 0.95 | 2.37 | 0.56 | 2.56 | 0.55 |
MDS-UPDRS Movement disorder society-unified Parkinson’s disease rating scale, LEDD Levodopa equivalent dose, IRLS index of restless legs syndrome, HAMA Hamilton anxiety scale, HAMD Hamilton depression scale, PDQ-39 Parkinson’s disease quality of life-39 items, SCOPA-AUT scale for outcomes in PD for autonomic symptoms.
Fig. 2. The sleep outcomes following GPi-DBS in three groups.
Boxplots compare PDSS-2 scores before surgery and follow-up in 32 patients. The lower and upper boundaries of a box plot represent the 25th and 75th percentiles, respectively. The median is represented by the centerline. The whisker lines extend to the smallest and largest non-outlier data points (interquartile range multiplied by 1.5). a Change in overall PDSS-2 score in all patients and three MID-divided groups; b change in the score of disturbed sleep; c change in the score of motor symptoms at night; d change in the score of PD symptoms at night. Because the PDSS-2 scores were not normally distributed, a Wilcoxon test was conducted. Significant P-values after Bonferroni correction are indicated. ***P < 0.001, *P < 0.05, signed-rank test.
Patients’ rapid eye movement (REM) behavior disorder (RBD) symptoms were evaluated using the RBD screening questionnaire (RBDSQ), with 26 patients completing this. The change in RBDSQ score was from 5.28 ± 4 to 5.04 ± 4.43, which was not a significant change (P = 0.87). Using 6 as the threshold of RBDSQ score23, 13 (50%) patients had RBD pre-surgery and 11 (42.3%) at follow-up (χ2 = 0.08, df = 1, P = 0.77). The analysis of RBD in the three groups showed that only group 2, patients with worsened PDSS-2 score, (P = 0.03) had a significantly higher RBD score at follow-up compared to the pre-surgery stage, which implied that patients with worsened sleep might have worsened RBD problems. The change in RBDSQ score in the three groups is shown in Supplementary Fig. 1. Patients’ motor symptoms were assessed using the UPDRS-III, though only 11 patients had follow-up results for the UPDRS-III.
The large standard deviations in the PDSS-2 and RBDSQ score changes indicated high heterogeneity in response to pallidal stimulation among patients. Linear regression with family-wise error (few) corrections showed no covariate was significantly correlated to PDSS-2 and RBD change (Table 1).
Comparing the effect of GPi-DBS and STN-DBS on sleep
We compared the change of PDSS-2 score in GPi-DBS patients with 32 age, sex, follow-up time, and sleep symptoms severity-matched STN-DBS patients. There was no demographic level difference between STN-DBS cohort and GPi-DBS cohort. Therefore, we believed the two cohorts were comparable. (detailed demographic data shown in supplementary Table 1). As shown in Table 3, we found STN-DBS significantly reduced the PDSS-2 score from 18.81 ± 5.35 to 14.31 ± 5.20 (p = 0.0003). We also found that STN-DBS did not significantly change the RBDSQ score.
Table 3.
Sleep outcome of GPi-DBS compared with STN-DBS
| Presurgery | Follow-up | p value | ||||
|---|---|---|---|---|---|---|
| mean | sd | mean | sd | |||
| GPi-DBS | ||||||
| PDSS-2 | 18.38 | 8.18 | 14.66 | 8.73 | 0.17 | |
| RBDSQ | 5.28 | 4.00 | 5.04 | 4.43 | 0.87 | |
| STN-DBS | ||||||
| PDSS-2 | 18.81 | 5.35 | 14.31 | 5.20 | 0.00 | ** |
| RBDSQ | 5.55 | 4.01 | 5.40 | 5.30 | 0.51 | |
PDSS-2 Parkinson’s disease sleep scale, RBDSQ rapid eye movement sleep disorder screening questionnaire.
*significant result with P < 0.05.
**significant result with P < 0.001.
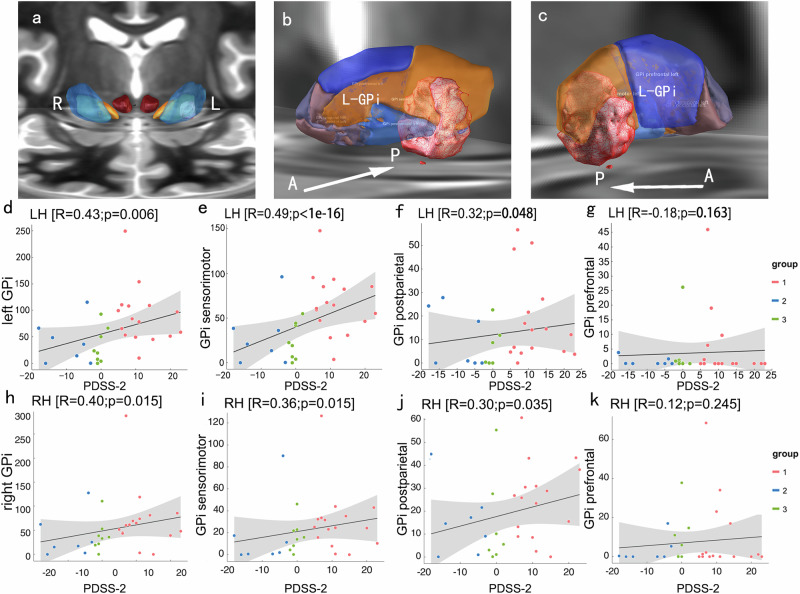
Ideal stimulation region and Sweetspot analysis
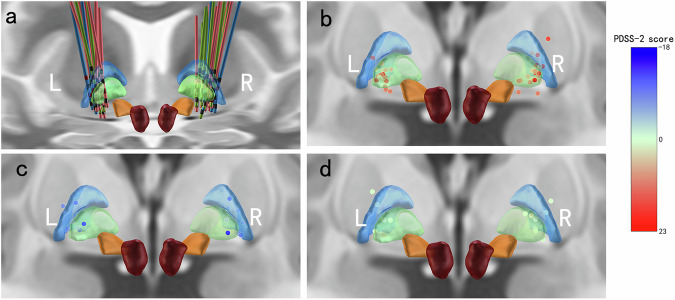
We further investigated the relationship between electrode position and sleep change. Sixty-four electrodes were placed with their active contacts within or close to the GPi shown in the 3D view (Fig. 3). By using lead-DBS sweetspot mapping, individual VTAs were associated with a change in PDSS-2 scores at a group level (Fig. 4). Positively associated voxels are shown in the red area, namely the sweetspot, and negative voxels are shown in blue, the sourspot. Only the sweetspot in the left GPi passed the false discovery rate (FDR) test. The number of voxels in sweetspot overlapped with GPi and GPe were calculated and shown in axial view (Supplementary Fig. 2). In addition, no covariates had an influence on the result. Based on DISTAL minimal atlas, GPi was subdivided into sensorimotor GPi, postparietal GPi, prefrontal GPi, and occipital GPi24. The detailed method could be seen in the early work by Ewert et al24. The sweetspot mostly overlapped with the left sensorimotor GPi, while there were also some voxels in the postparietal GPi, and others did not overlap with the GPi. By regressing the PDSS-2 score to the intersection volume of the sweetspot and the GPi, the left GPi (R = 0.43, P = 0.005), left post-parietal GPi (R = 0.32, P = 0.04), and left sensorimotor GPi (R = 0.49, P = 0.005) were found to be significantly correlated with PDSS-2 score improvement (Fig. 4d‒g). It was similar in the right hemisphere that the right GPi (R = 0.40, P = 0.015), right post-parietal GPi (R = 0.36, P = 0.021), and right sensorimotor GPi (R = 0.30, P = 0.035) were found to be significantly correlated (Fig. 4h‒k). However, no significant sweetspot was found in the right hemisphere, which might could be caused by more widely distributed VTA or relatively small sample size. Sweetspot analysis was conducted on the RBDSQ score. However, no sweetspot or sourspot passed FDR-correction.
Fig. 3. 3D illustration of electrodes and active contacts.
Active contacts are dots colored by the PDSS-2 score change. a 64 electrodes in GPi; b active contacts of patients in group 1; c active contacts of patients in group 2; d active contacts of patients in group 3. Group 1 represents patients with improved PDSS-2 scores, Group 2 represents patients with worsened PDSS-2 scores, Group 3 represents patients with negligible change in PDSS-2 scores.
Fig. 4. 3D illustration of the sweetspot, shown in red indicated voxels correlated to improved PDSS-2.
a Anterior view of sweetspot analysis. Sweetspot voxels were distributed in the left hemisphere only, which were mostly overlapped with the left globus pallidus internus (GPi). b Anterior view of the sweetspot in the left GPi. The GPi was subdivided into sensorimotor (orange), postparietal (blue), prefrontal (dark blue), temporal (pink), and occipital (violet). c lateral and posterior view of the sweetspot. d‒g Individual PDSS-2 scores regressed to the intersection volume of the abovementioned subregions of the left GPi (d left GPi, e left sensorimotor GPi, f left postparietal GPi, g left prefrontal GPi). h‒k Individual PDSS-2 scores regressed to the intersection volume of the abovementioned subregions of the right GPi (h right GPi, e right sensorimotor GPi, f right postparietal GPi, g right prefrontal GPi). Group 1 represents patients with improved PDSS-2 scores, Group 2 represents patients with worsened PDSS-2 scores, Group 3 represents patients with a negligible change in PDSS-2 scores. LH: left hemisphere; RH: right hemisphere.
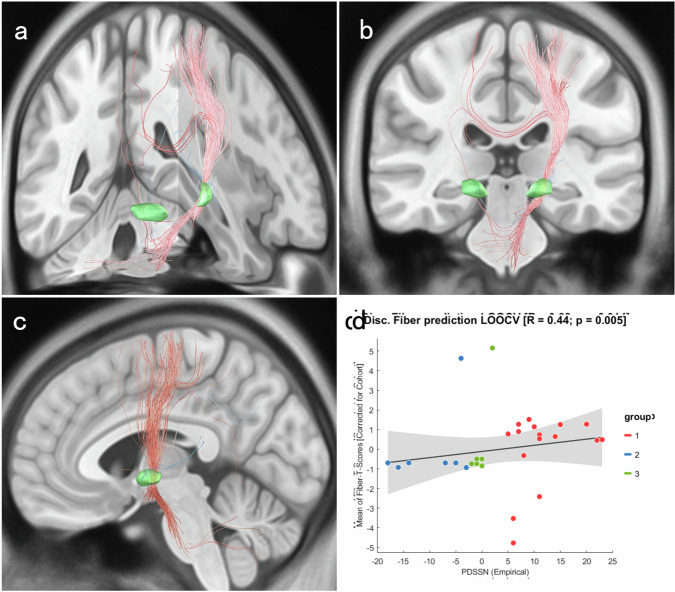
Sleep improvement-related connectome
The structural connectome seeded from the sweetspot and based on the N = 90 PPMI 85 connectome was correlated with the total score and 3 subdomains of the PDSS-2 (Fig. 5)25. In general, the fibers were all rooted from the left GPi, including (1) fibers that connect the left GPi and sensorimotor cortex; (2) fibers that connect the left GPi to the right sensorimotor cortex, right GPi, and right cerebellum through the callosum; and (3) fibers that pass through the brainstem, and some connected to the cerebellar hemispheres. Several negative fibers were also identified, which were connected to the left hippocampus, right sensorimotor cortex through the GPi, left occipital lobe, and brainstem. No covariates influenced the result. Although the activated fibers were calculated based on DISTAL minimal atlas24. Stimulation of GPi-DBS has been confirmed with several diffusion tensor imaging studies to activate those fibers, and also confirmed by fMRI studies to activate the downstream regions, which were also associated with motor and nonmotor symptoms of PD patients26–29. Leave-one-patient-out cross-validation (LOOCV) indicated PDSS-2 improvement was significantly correlated with the weighted mean of fiber T-scores (R = 0.39, P = 0.01). Considering the three subdomains of the PDSS-2, the outcomes for disturbed sleep and motor symptoms at night were similar with fibers of overall PDSS-2 improvement; while for PD symptoms at night, no fibers passed FDR correction (Supplementary Fig. 3). Furthermore, to investigate the impact of motor improvement on sleep, 11 patients with follow-up UPDRS-III scores were selected for correlation analyzes. There was no significant difference in baseline statistics between the sub-cohort and the entire cohort (Supplementary Table 2). We found little change between the structural connectomes before and after introducing UPDRS-III score change as a covariate (Supplementary Fig. 4). Therefore, the PDSS-2 change might not be due to motor symptom improvement. A connectome of RBDSQ score improvement was also constructed (shown in Supplementary Fig. 5). There were no fiber passed FDR-correction.
Fig. 5. Connectome of stimulation-related sleep change.
PDSS2-positively correlated fibers are shown in red and negatively correlated fibers are in blue. All the illustrated fibers were FDR-corrected with P-value < 0.05. 30% fibers were displayed here. There were 119 positive fibers and six negative fibers from the left GPi and no fibers from the right GPi. a 3D view; b Coronal view of fibers; c Sagittal view of fibers; d Leave-One-Out Cross Validation of fiber T-score. Group 1 represents patients with improved PDSS-2 scores, Group 2 represents patients with worsened PDSS-2 scores, Group 3 represents patients with a negligible change in PDSS-2 scores.
Discussion
In the present study, we evaluated the effect of GPi-DBS on sleep quality in 32 patients with PD. The results indicated that GPi-DBS did not significantly reduce the PDSS-2 score on a group level. On the contrary, STN-DBS significantly reduced the PDSS-2 score, which is consistent with our hypothesis. Considering the MID, 16 patients had improved sleep, seven deteriorated, and nine had a trivial change. By analyzing demographic data, no covariate was found to be significantly associated with improvement in the PDSS-2, which indicated that clinical traits might have little influence on the effects of GPi-DBS on sleep. The clinical improvement was combined with patients’ brain images to estimate the optimal stimulation point that is associated best with sleep improvement (sweetspot), and whole brain connectome to understand how pallidal stimulation might work on sleep-wake disorders. Sweetspot analysis found electrode contacts placed in regions around the sensorimotor GPi might improve sleep, while no VTA was found to be significantly related to worsened sleep. The structural connectome suggested that sleep-improving fibers connected to extensive brain regions might respond to GPi-DBS stimulation, where sensorimotor regions might play an important role. Moreover, the fibers were probably associated with sleep improvement, but this improvement was not linked to improved motor symptoms.
There have been few studies focused on the sleep-related effects of GPi-DBS. Several cohort studies and cases with polysomnography (PSG), a non-motor symptoms scale, or life quality questionnaire data as the outcome measures suggested that GPi-DBS showed trends in improving sleep quality with regard to sleep latency, sleep efficiency, periodic limb movement, and daytime fatigue10–12. A randomized clinical trial by Weaver and colleagues indicated long-term GPi-DBS could improve sleep time and reduce fatigue5,8,14. However, another study showed that GPi might not influence sleep in any direction27. To the best of our knowledge, this is the first study to use the PDSS-2 to evaluate sleep outcomes for a relatively sizable cohort of PD patients receiving GPi-DBS over an extended period of time. In this study, sleep was improved in 16 patients, worsened in 7 patients, and not changed in 9 patients, which, as a whole, was not significantly improved. Patients with improved sleep had significant improvement of all 3 subdomains of the PDSS-2, while those with worsened sleep had only a significant worsening of PD symptoms at night, which contained nocturnal hallucinations, difficulty in turning around, pain in the extremities, muscle cramp, and snoring or breathing problems30. Specifically, only one patient had hallucinations at night, while others had worsened turning over problems, pain, and muscle cramps. Turning over requires the use of the muscle of the central axis. Worsening axial symptoms has been reported frequently in large DBS trials as an adverse effect after high frequency stimulation5,31. While we applied high frequency stimulation (132.66 ± 19.59) for most of the patients. Although DBS is effective in relieving pain in PD32, some evidence showed a number of patients complained the development of new pain after receiving STN-DBS33. However, there is little evidence indicating whether GPi-DBS could cause newly emerging pain. A recent study suggested that GPi-DBS might decrease beta-endorphin level in PD patients after six months, which might be negatively correlated with pain or bodily discomfort34. However, studies on how would pain affect sleep after GPi-DBS is needed. There was neither evidence showed newly emerging muscle cramps after receiving long-term GPi-DBS. There was also a huge variance in the response to GPi-DBS with regard to individual sleep quality. However, no baseline clinical traits were found to be related to sleep improvement.
The results of the comparation between STN-DBS and GPi-DBS indicated that STN-DBS had a lower mean and smaller variance compared to GPi-DBS. At follow-up, the mean PDSS2 scores for GPi-DBS and STN-DBS were similar (14.66 vs. 14.31), but the variance among GPi-DBS patients was higher (8.37 vs. 5.20). This might suggest a higher uncertainty in the effect of GPi-DBS on sleep compared to STN-DBS. However, this variance was still observed at baseline (8.18 vs. 5.35). Although patients receiving STN-DBS and GPi-DBS were age, sex, symptom severity, and follow-up time matched, there was still a difference in the SD of sleep symptom before surgery. We reckon this was because of factors could not be matched. Among them, a likely one was dyskinesia. Many patients receiving GPi-DBS at our center had severe levodopa-induced dyskinesia compared to STN-DBS. This made it even hard to match UPDRS-IV for GPi-DBS patients and STN-DBS patients. However, dyskinesia may have influence on sleep. For instance, Amato et al. found that slow wave sleep in dyskinesia patients was negatively correlated with disease duration, while non-dyskinesia PD was positively correlated35. They also found that sleep efficiency in patients with dyskinesia was negatively correlated with disease duration, a phenomenon that was not observed in advanced PD. However, although a large proportion of patients with GPi-DBS in this study had dyskinesia, there were still non-dyskinesia PD and chose GPi-DBS for other reasons, which might have introduced a greater variance. We did not, however, investigate the relationship between those patients’ sleep and UPDRS-IV. Future studies on the connection between dyskinesia and sleep are still required. Compared to patients with GPi-DBS, those who selected STN-DBS exhibited less or very mild dyskinesia and were more consistent. As a result, there may be variations in the two patients’ baseline sleep scores.
STN-DBS has been reported to improve sleep by several previous studies36,37. Our team had conducted a meta-analysis of 21 articles involving 541 patients and found that the improvement of sleep by STN-DBS in previous studies was relatively consistent4. In another study on the microlesional effect of STN-DBS on sleep, we found there was a significant relationship between the STN associative area and sleep improvement38. Similarly, indicated by the current results, we found that a region near sensorimotor GPi was significantly related to sleep improvement in GPi-DBS. However, lead reconstruction results showed that activated contacts in GPi did not cover this region for every patient. Therefore, some sleep was improved in some patients while sleep for others was not improved or even worsened. In our results, shown in Fig. 3, the active contacts of improved patients were mostly in left posterior, lateral GPi, while others were more widely distributed, and some were far from sensorimotor GPi, which might lead to less therapeutic effect. Combining with the fiber tracking results, we speculate that the main reason for GPi-DBS not always improving sleep is that sleep improvement effect of pallidal stimulation might depend on targeted connectivity modulation. However, GPi is a relatively large nucleus. During surgical plan-making and electrode implantation, a tiny deviation could lead to a variance in the actual position of the electrode in GPi. Having that said, it is noteworthy that PD patients received pallidotomy surgery, a more thorough way to eliminate GPi function, were reported to have significant improvement in sleep39.
Disturbance of the basal ganglia circuitry might play a role in sleep disorders in patients with PD. The most prominent pathophysiological change in PD is α-synucleinopathy, which leads to deterioration of dopaminergic neurons in the substantia nigra. During this process, extensive brain areas are influenced by reduced dopaminergic input, including the sleep circuitry and sleep regulation center40,41. During this process, the GP is overactivated, which has been linked to reduced sleep quality16,17,42,43. GPi is the outflow region of the basal ganglia and functions as a regulator to initiate muscle movement in REM and behavioral arousal16,44,45. Electrophysiological signals in GPi could reflect the sleep stage during sleep19. Our results demonstrated that most sweetspot voxels were in the sensorimotor GPi, which is also a promising stimulation target to control motor symptoms31. In human, GPi-DBS activates both afferent and efferent fibers around the activated electrode, including subthalamo-pallidal terminals, pallido-pallidal terminals, which cause GPi and STN inhibition46,47. Furthermore, in monkeys treated with 1-methyl-4-phenyl-1,2,3,6-tetrahy dropyridine, it was shown that GPi high frequency stimulation inhibited the M1 region, ventrolateral nucleus of the thalamus, and might cause regular firing of thalamic nuclei48–50. As a result, sleep phase transition is modified, and sleep fragmentation is reduced. To prove this, evidence that utilizes PSG recording is needed.
From the electrode active contacts (Fig. 3), it seemed that most electrode in GPe might not tend to improve sleep. Nevertheless, sweetspot shown in Fig. 4 indicated that the best stimulation site might be lateral to the GPi and GPe border. Overall, we believe that stimulating GPe alone may not improve sleep, but stimulating GPi in combination may improve sleep. Although, there is evidence showing GPe-DBS could improve sleep-wake function both in humans and rats51,52. We assumed that GPe stimulation in rats could not substitute human GPe stimulation because of structural differences. Moreover, the improvement effect of GPe stimulation has only been observed in one subject, which is not representative51. To elucidate the effect of GPe-DBS on sleep, further investigations with larger sample sizes are needed.
As far as we know, there has been abundant literature reporting sleep disorder-related anomalies of cortical and subcortical structures from neuroimaging in patients with PD53–65. However, there were different magnetic resonance imaging (MRI) sequences analyzed with different methodologies. It is difficult to make an exact summary of which structures play more important roles or which structures have more weight over others about the underlying pathophysiology of sleep problems in patients with PD. We hypothesize that interrupting any part of the sleep circuitry could lead to sleep disturbances. In other words, the sleep improvement circuitry modified by DBS could vary among individuals. Therefore, we only discussed regions that were significantly affected in the current study. The fibers with the greatest number associated with sleep improvement were between the GPi and sensorimotor cortex. Furthermore, to rule out the effect of motor symptom improvement on sleep, we introduced UPDRS-III as a covariate in a comparable cohort of 11 patients with motor symptom scale results. The sensorimotor area is the most well-known cortical area to be violated, whether in the early or late stages of PD53–56. This violation contributes to sleep deterioration, as suggested by several studies. Meles and colleagues suggested that sleep fragmentation in early PD may be due to electroencephalography (EEG) microstructural changes in non-REM and REM sleep in the motor cortex57. In addition, RBD patients could have abnormal cortical thickness in motor circuits58, including thinning of the cortices, reduced gray matter in the bilateral medial superior cortices and anterior cingulate cortices, and surface atrophy in the lateral and medial parts of the left GPi58. Furthermore, there was reduced gray matter volume in the left posterior cingulate gyrus and left hippocampus in those with PD comorbid with severe sleep disorder compared with those without59. Rahayel and colleagues found functional connectivity and regional homogeneity in the motor circuitry were significantly reduced in patients with PD with restless legs syndrome (RLS) compared to those without60. Here we found that RLS severity at baseline tended to correlate with sleep improvement (P = 0.02), although this was not significant after we adopted multiple comparison corrections.
In addition to the sensorimotor area, the connectome also contained some subcortical and cerebellar regions. Although the underlying mechanism is not clear, some previous evidence suggested that damage to the subcortical and cerebellar circuits might result in sleep change, especially causing RBD in patients with PD. From the literature, increased gray matter volume61,62 and reduced regional homogeneity63 were reported in patients with PD-RBD. Moreover, RBD patients were reported to have reduced gray matter volume in the anterior lobes of the cerebellar hemisphere64 and substantia nigra, and the thalamus, retrosplenial cortex, and angular cortex were also found to have glucose hypometabolism65.
Interestingly, the sweetspot and connectome demonstrated an asymmetric pattern. Although the size of overlapped VTA in both GPi was associated with sleep improvement, we found all fibers were from the left sensorimotor GPi. This might be due to too dispersedly distributed VTA in GPe or relatively small sample size. Nevertheless, some previous evidence suggested that the left hemisphere might play a more important role in sleep. Moreover, the side of initial onset tends to remain more affected as the disease progresses66 and the basal ganglia and substantia nigra show considerable neuropathologic asymmetry67. The responsible brain regions for non-motor symptoms in PD have also been proposed to have an asymmetric pattern. Those with left-side PD (LPD), with more severe right hemisphere nigrostriatal system degeneration, have visuospatial and vigilance deficits68–73. In contrast, in patients with right-side PD (RPD) with more severe left hemisphere degeneration, symptoms of verbal memory performance occur more often68,74. Similar to other non-motor symptoms, sleep-wake function in PD might also be asymmetrically affected by different onset sides. Stavitsky and colleagues studied sleep architecture in LPD and RPD and revealed that although the two groups had no significant difference in sleep architecture, those with LPD showed more daytime sleepiness, nocturnal hallucination, and more vivid dreams75. However, Cubo and colleagues evaluated non-motor symptoms in LPD and RPD and found no significant difference in the sleep quality subdomain76. Considering sleep quality, patients with LPD and RPD might all benefit from DBS, as suggested by increased accumulated slow-wave activity77. Respectively, for LPD with DBS, PSG showed enhanced sleep quality; while for RPD with DBS, PSG showed increased overnight sleep time77. We hypothesize that the cortical regions involved in the sleep-wake circuitry prefer an asymmetrical pattern. The effects of DBS on PD might also depend on laterality. By studying sleep architecture in patients with PD with STN-DBS, Baumann-Vogel and colleagues demonstrated that the location of left electrode contacts was significantly correlated with better sleep efficiency, which is not found on the other side78. However, there have also been studies with contrasting results. Amara and colleagues evaluated unilaterally implanted STN-DBS and suggested that there is no significant improvement after STN-DBS, irrespective of whether the electrode contacts were placed in the right or left hemisphere79. From our results, 14 subjects’ symptoms were initiated in the right side of the body and 18 were initiated in the left side, and thus there was no preference of larger stimulation parameters in the left hemispheres. Further investigation in this area is still needed.
There are several limitations to our study. First, use of antiparkinsonian drugs like Sinemet or Amantadine might influence sleep. Therefore, the prescriptions of the patients included in this study were kept the same as they were preoperative. However, a few patients had their dosage increased due to disease progression. Second, patients who chose to have DBS surgery mostly had severe symptoms. However, disease duration might not fully represent the severity of their symptoms. It would be better to pair matched PD patients with no DBS with the patients included in this study in order to verify the effects of DBS. Third, some patients were lost to follow-up, which might have introduced bias into the results. Loss to follow-up rate is hard to control in a retrospective study. This lack of longitudinal data hampers our ability to accurately assess the deterioration or improvement of sleep after DBS over time. Nonetheless, considering the relatively small number of GPi-DBS surgeries, our sample size is still considerable. Despite these efforts, the loss to follow-up rate remains a potential limitation of this study. Fourth, due to the retrospective nature of the study, many data were hard or even failed to collect at follow-up, including UPDRS-III, IRLS, etc. The high loss of follow-up rate for motor symptoms is a notable limitation. This gap in data affects the robustness of our conclusions. And the very small cohort who finished motor assessment might not be representative for the entire cohort. This limitation is common in retrospective studies, and it is important to consider when interpreting the results.
Methods
Patients
This retrospective study was performed in accordance with the Declaration of Helsinki and approved by the ethical committee of Capital Medical University Affiliated Beijing Tiantan Hospital (KY2022-006-02). The patients involved were anonymous and approved to the informed consent. Between October 2016 and September 2021, a total of 63 patients diagnosed with PD who had undergone GPi-DBS at our center were screened for inclusion in this retrospective study. They were implanted with two DBS electrodes (the detailed surgical procedure is described later). To test our hypothesis, we further enrolled STN-DBS patients who matched with GPi-DBS patients in number, age, sex, follow-up time, and motor and nonmotor symptoms severity. T-test between the two groups was conducted to ensure that no significant difference exists. The reason for matching is to avoid potential difference between GPi-DBS cohort and STN-DBS cohort, which would be mentioned below. All patients received preoperative MRI and postoperative computed tomography (CT) and had undergone careful visual evaluation during stereotactic planning by a multidisciplinary team of experienced neuroradiologists, neurologists, and neurosurgeons.
There were no set criteria for GPi-DBS; however, in our center, patients with antiparkinsonian-drug-induced dyskinesia or cognitive impairment were preferred to have GPi-DBS. This is why patients received GPi-DBS might have difference between STN-DBS. Patients were excluded if: (1) they had electrodes removed due to complications; (2) we were unable to follow up; (3) although psychiatric and cognitive disorders were not in exclusion criteria, patients had comorbid very severe psychiatric or cognitive disorder might prevent us from collecting data at follow-up, were therefore excluded. Sleep disruption was not considered as an inclusion criterion in the design.
Two quadripolar electrodes (PINS-L302 or Medtronic-3387) were implanted in the bilateral GPi for each patient according to the surgical procedure described in previous studies19,80. In short, the patients would have a 3 T high-resolution MRI head scan one day before surgery and an anatomical CT scan after fixing with a Leksell stereotactic frame. T1 and T2 MRI images were registered to CT and the GPi was set as the target. Microelectrode recording was conducted to determine the best trajectory for DBS in the GPi. Once the target was verified, the DBS quadripolar electrode was implanted along the microelectrode trajectory. After being implanted in the subclavicular region while under general anesthesia, the electrodes were subsequently attached to an implantable pulse generator (IPG).
Motor score and subjective sleep quality
All patients received the assessment of PD motor and non-motor symptoms, psychometric assessment, and cognitive evaluation before surgery. Patients undergone GPi-DBS surgery between October 2016 and September 2021 we retrospectively enrolled in this study. They were intended to be regularly followed up for the same assessment as pre-surgery at 3 months, 6 months, 1 year, 2 years, 3 years, 4 years after surgery. Self-rating scales including PDQ39, Autonomic nervous system symptoms, PDSS-2, RBDSQ, etc., could be collected online or through phone calls. Others including motor symptoms (UPDRS-III), HAMA, HAMD were collected when the patients come to visit our hospital. For better comparing the effect of STN-DBS and GPi-DBS on sleep, a cohort of 32 age, sex, disease duration, and motor symptom severity matched patients undergone STN-DBS were enrolled. They had undergone the same assessment procedure as abovementioned GPi-DBS patients had. The patients’ predominant motor symptoms were decided based on UPDRS-III sub items: (1) tremor-dominant: one of items 3.17–3.18 ≥ 2 while item 3.3–3.14 < 2 and the onset symptom was resting tremor; (2) rigidity dominant: one of items 3.3 ≥ 2 while items 3.14, 3.17–3.18 < 2 and the onset symptom was rigidity; (3) bradykinesia: item 3.4 ≥ 2 while items 3.3, 3.17–18 < 2 and the onset symptom was bradykinesia ; (4) mixed symptoms: the predominant and onset symptoms were more than one of abovementioned symptoms; (5) other: other predominant or onset symptoms like pain or dyskinesia. Demographic data and UPDRS-I, -II, and -III, H-Y stage scores, and other scales were reserved as covariates for further analysis. The main outcome here was subjective sleep quality, which was evaluated using the PDSS-2 including three subdomains that respectively assess motor symptoms at night, PD symptoms at night, and disturbed sleep30,81. RBD was evaluated using the RBDSQ82. Motor symptoms at night evaluated sleep-related motor symptoms that might influence sleep, including restless legs, urge of moving, RBD, and tremor, PD symptoms at night evaluates nonmotor symptoms, including hallucination, immobility, pain, muscle cramps, and trouble with breathing. Disturbed sleep describes more basic sleep conditions, including subjective feelings on sleep, prolonged sleep onset latency, sleep maintenance, night urination, and daytime sleepiness.
Because some patients showed very little improvement in PDSS-2 score at follow-up compared to pre-surgery, MID was utilized as the grouping basis to gain more clinical relevance. According to the previously mentioned method for PDSS-2, the value of MID was calculated83,84. As a result, patients were divided into three groups depending on whether the sleep symptoms had improved or worsened to the MID: group 1 for patients with improvement of sleep, group 2 for patients with deterioration, and group 3 for patients with minor change. An inter-group t-test of the covariates was performed to validate the difference between the three groups.
DBS lead localization
Detailed elucidation of the method for DBS localization has been mentioned before by Horn and Kühn85. Briefly, using SPM12 (http://www.fil.ion.ucl.ac.uk/spm/software/spm12/; postoperative MRI) or BRAINSFit software (https://www.nitrc.org/projects/multimodereg/; postoperative computed tomography), postoperative images were linearly coregistered to preoperative MRI. Each patient’s images registrations were carefully reviewed and adjusted as necessary. Using the SyN technique implemented in advanced normalization tools (http://stnava.github.io/ANTs/), images were then normalized into the ICBM 2009b NLIN asymmetric space based on the preoperative MRI. Using Lead-DBS software (www.lead-dbs.org;85), DBS electrode connections were located inside the Montreal Neurological Institute and Hospital (MNI) space.
Volume of tissue activated (VTA) analysis
VTA for each patient was generated by using Lead-DBS (www.lead-dbs.org;85). A Finite Element Method (FEM)-based model using the Simbio/FieldTrip pipeline as implemented was used to predict the volumes of tissue activated (VTA) based on the long-term DBS settings86. Voltage or amplitude of stimulation and the spatial coordinate of the active contact were input for further computation. The E-field was computed using this model on a tetrahedral four-compartment mesh that takes account of the gray matter (σ = 0.33 S/m) and white matter (σ = 0.14 S/m), electrode contacts, and insulating components. The E-field is the gradient distribution of the electrical charge in space, measured in Volts per millimeter. To determine the size and form of the VTA, the E-Field gradient was thresholded for magnitudes greater than the conventional value of 0.2 V/mm. The red nucleus, internal and external pallidum, and STN were the parts of the DISTAL atlas that were used to characterize the gray matter24. The subregions of GPi were also divided according to DISTAL minimal atlas24.
Voxel-wise sweetspot analysis
Voxel-wise sweetspot analysis was conducted by using sweetspot analysis imbedded in Lead-DBS (www.lead-dbs.org;85). In this analysis, a N-image was firstly created by counting the number of VTAs that intersected in each voxel, where voxels covered less than 20% VTAs were excluded. Each voxel in the relevant VTA was assigned a change in PDSS-2 score to create a mean effect map. To generate a mean-image, the mean change score for every voxel was then computed. Each voxel of the matched mean-image was subjected to voxel-wise statistical test to produce the p-image. To find significant (P < 0.05) differences in the mean change score of each voxel from zero, two-sided Wilcoxon signed-rank tests were employed. Positive voxels (sweet) were defined as having a mean change score that was significantly less than zero, while negative voxels (sour) were defined as having a mean change score that was greater than zero. We added covariates including age, sex, disease duration, education years, age of onset, follow-up years, off-stage MDS-UPDRS III (before surgery), off-stage H-Y stage (before surgery), IRLS, HAMA, HAMD, PDQ-39 to control for their influence on the model. Each voxel’s P-values were corrected using FDR correction at an α-level of 0.05. The sweetspot was exported as neural image mask file and the number of voxels overlapped with GPi and GPe was calculated using RESTplus toolbox in matlab (v1.30, www.restfmri.net)87.
Connectivity analysis
A PD connectome based on the Parkinson’s Progression Markers Initiative (www.ppmi-info.org) was used to estimate the structural connection between each VTA and all other brain voxels25. This PD patient’s PPMI dataset was previously estimated and has been used in the context of DBS multiple times25,88–90. The lead-DBS fiber-filtering method was used to identify white matte fiber tracts overlapped by VTAs. A total of 20,000 fibers were sampled in each subject using DSI Studio’s generalized q-sampling approach. Each voxel’s number of fibers that traveled through it was counted, creating the traditional fiber-density map. A minimum of 20% of the included patients’ VTAs were set as the threshold for fibers used for further analysis. By connecting the connection of the fiber tract to VTAs across patients with clinical outcomes, a “Fiber T-score” was created. For each tract, (mass-univariate) two-sample t-tests were done to compare clinical outcomes in linked and disconnected VTAs. The clinical outcomes in this study included change in PDSS-2 and RBDSQ. A high absolute t-value suggested that the fiber was highly selective between VTAs that were responding well for patients’ improvement (positive t-score) or deterioration (negative t-score), or that it was a sign of a successful treatment or significant adverse effect, respectively. The t-values of the fibers were tested using FDR-correction and an α-level of 0.05 was the threshold. Fibers with top 30% T-score were illustrated. We added covariates including age, sex, disease duration, education years, age of onset, follow-up years, off-stage MDS-UPDRS III (before surgery), off-stage H-Y stage (before surgery), IRLS, HAMA, HAMD, PDQ-39 to control for their influence on the model. To assess the accuracy of individual patient results, leave-one-patient-out cross-validation was performed over the whole dataset based on the structural connections. All the fibers in thirty-one (out of 32) patients were employed in the leave-one-patient-out approach to forecast the remaining patients.
Statistical analysis
We first evaluated the association between clinical/demographic characteristics and PDSS-2/RBDSQ change using univariate and multivariate linear models by R version 4.0.5. Differences with P < 0.05 were considered statistically significant. Presurgery and follow-up PDSS-2 scores, subdomains scores, and RBDSQ scores were non-Gaussian distributed tested using a Shapiro-Wilk test and therefore were compared by two-tailed Wilcoxon tests. All the P values were adjusted for FDR multiple testing. Graphs were generated with Rpackage ggplot2 version 3.3.591. Detailed calculations for PDSS-2 correlated sweetspot and structural connectivity have been mentioned above.
Supplementary information
Acknowledgements
JGZ is supported by the National Nature Science Foundation of China (81830033). ACY receives funding from the National Nature Science Foundation of China (81870888). The funders played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript.
Author contributions
Z.Z.T. and Y.Z.X. designed the study and wrote the article. L.D.F. refined the research design, conducted additional analysis of the data, as well as rewrote and revised the manuscript during revisions. Y.Z.X. collected clinical and brain imaging data. Z.Z.T. and X.H.T. conducted data analysis. F.H.Y., Q.G.F., Z.Q. and J.Y. supported with data analysis. Z.Z.T., Q.G.F. and Z.Q. performed sleep, UPDRS-III evaluations. Z.J.G., Y.A.C., and M.F.G. are surgeons for the patients and gave necessary technical support.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon request. The underlying code for this study is available in lead-dbs86 and can be accessed via this link [http://lead-dbs.org].
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Zhaoting Zheng, Defeng Liu.
Contributor Information
Zixiao Yin, Email: zixiao_yin@ccmu.edu.cn.
Anchao Yang, Email: yang.anchao@163.com.
Jianguo Zhang, Email: zjguo73@126.com.
Supplementary information
The online version contains supplementary material available at 10.1038/s41531-024-00800-4.
References
- 1.Gómez-Esteban, J. C. et al. Impact of psychiatric symptoms and sleep disorders on the quality of life of patients with Parkinson’s disease. J. Neurol.258, 494–499 (2011). [DOI] [PubMed] [Google Scholar]
- 2.Martinez-Martin, P., Rodriguez-Blazquez, C., Kurtis, M. M. & Chaudhuri, K. R. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov. Disord. : Off. J. Mov. Disord. Soc.26, 399–406 (2011). [DOI] [PubMed] [Google Scholar]
- 3.Mizrahi-Kliger, A. D., Kaplan, A., Israel, Z., Deffains, M. & Bergman, H. Basal ganglia beta oscillations during sleep underlie Parkinsonian insomnia. Proc. Natl Acad. Sci. USA117, 17359–17368 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yin, Z. et al. A quantitative analysis of the effect of bilateral subthalamic nucleus-deep brain stimulation on subjective and objective sleep parameters in Parkinson’s disease. Sleep. Med79, 195–204 (2021). [DOI] [PubMed] [Google Scholar]
- 5.Follett, K. A. et al. Pallidal versus subthalamic deep-brain stimulation for Parkinson’s disease. N. Engl. J. Med.362, 2077–2091 (2010). [DOI] [PubMed] [Google Scholar]
- 6.Okun, M. S. et al. Cognition and mood in Parkinson’s disease in subthalamic nucleus versus globus pallidus interna deep brain stimulation: the COMPARE trial. Ann. Neurol.65, 586–595 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rothlind, J. C. et al. Neuropsychological changes following deep brain stimulation surgery for Parkinson’s disease: comparisons of treatment at pallidal and subthalamic targets versus best medical therapy. J. Neurol., Neurosurg., psychiatry86, 622–629 (2015). [DOI] [PubMed] [Google Scholar]
- 8.Weaver, F. M. et al. Randomized trial of deep brain stimulation for Parkinson disease: thirty-six-month outcomes. Neurology79, 55–65 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eugster, L., Bargiotas, P., Bassetti, C. L. & Michael Schuepbach, W. M. Deep brain stimulation and sleep-wake functions in Parkinson’s disease: a systematic review. Parkinsonism Relat. Disord.32, 12–19 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Tolleson, C. M., Bagai, K., Walters, A. S. & Davis, T. L. A pilot study assessing the effects of pallidal deep brain stimulation on sleep quality and polysomnography in Parkinson’s patients. Neuromodulation19, 724–730 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volkmann, J. et al. Long-term effects of pallidal or subthalamic deep brain stimulation on quality of life in Parkinson’s disease. Mov. Disord. : Off. J. Mov. Disord. Soc.24, 1154–1161 (2009). [DOI] [PubMed] [Google Scholar]
- 12.Dafsari, H. S. et al. Beneficial nonmotor effects of subthalamic and pallidal neurostimulation in Parkinson’s disease. Brain Stimul.13, 1697–1705 (2020). [DOI] [PubMed] [Google Scholar]
- 13.Dafsari, H. S. et al. Beneficial effect of 24-month bilateral subthalamic stimulation on quality of sleep in Parkinson’s disease. J. Neurol.267, 1830–1841 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weaver, F. M. et al. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. Jama301, 63–73, (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kita, T. & Kita, H. Cholinergic and non-cholinergic mesopontine tegmental neurons projecting to the subthalamic nucleus in the rat. Eur. J. Neurosci.33, 433–443 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qiu, M. H., Vetrivelan, R., Fuller, P. M. & Lu, J. Basal ganglia control of sleep-wake behavior and cortical activation. Eur. J. Neurosci.31, 499–507 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu, M. H., Yao, Q. L., Vetrivelan, R., Chen, M. C. & Lu, J. Nigrostriatal dopamine acting on globus pallidus regulates sleep. Cereb. Cortex26, 1430–1439 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang, J., Wang, Z. I., Baker, K. B. & Vitek, J. L. Effect of globus pallidus internus stimulation on neuronal activity in the pedunculopontine tegmental nucleus in the primate model of Parkinson’s disease. Exp. Neurol.233, 575–580 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yin, Z. et al. Pallidal activities during sleep and sleep decoding in dystonia, Huntington’s, and Parkinson’s disease. Neurobiol. Dis.182, 106143 (2023). [DOI] [PubMed] [Google Scholar]
- 20.Stebbins, G. T. et al. How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson’s disease rating scale: comparison with the unified Parkinson’s disease rating scale. Mov. Disord.28, 668–670 (2013). [DOI] [PubMed] [Google Scholar]
- 21.Muntean, M. L. et al. Clinically relevant cut-off values for the Parkinson’s disease sleep scale-2 (PDSS-2): a validation study. Sleep. Med24, 87–92 (2016). [DOI] [PubMed] [Google Scholar]
- 22.Suzuki, K. et al. Evaluation of cutoff scores for the Parkinson’s disease sleep scale-2. Acta neurologica Scandinavica131, 426–430 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Halsband, C., Zapf, A., Sixel-Döring, F., Trenkwalder, C. & Mollenhauer, B. The REM sleep behavior disorder screening questionnaire is not valid in de novo Parkinson’s disease. Mov. Disord. Clin. Pr.5, 171–176 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ewert, S. et al. Toward defining deep brain stimulation targets in MNI space: a subcortical atlas based on multimodal MRI, histology and structural connectivity. NeuroImage170, 271–282 (2018). [DOI] [PubMed] [Google Scholar]
- 25.The Parkinson Progression Marker Initiative (PPMI). Progress in neurobiology95, 629-635, (2011). [DOI] [PMC free article] [PubMed]
- 26.Rozanski, V. E. et al. Connectivity patterns of pallidal DBS electrodes in focal dystonia: a diffusion tensor tractography study. NeuroImage84, 435–442 (2014). [DOI] [PubMed] [Google Scholar]
- 27.Zheng, Z. S. & Monti, M. M. Cortical and thalamic connections of the human globus pallidus: Implications for disorders of consciousness. Front Neuroanat.16, 960439 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sobesky, L. et al. Subthalamic and pallidal deep brain stimulation: are we modulating the same network? Brain : a J. Neurol.145, 251–262 (2022). [DOI] [PubMed] [Google Scholar]
- 29.Miyawaki, E., Perlmutter, J. S., Tröster, A. I., Videen, T. O. & Koller, W. C. The behavioral complications of pallidal stimulation: a case report. Brain cognition42, 417–434 (2000). [DOI] [PubMed] [Google Scholar]
- 30.Trenkwalder, C. et al. Parkinson’s disease sleep scale-validation of the revised version PDSS-2. Mov. Disord. : Off. J. Mov. Disord. Soc.26, 644–652 (2011). [DOI] [PubMed] [Google Scholar]
- 31.Odekerken, V. J. et al. Subthalamic nucleus versus globus pallidus bilateral deep brain stimulation for advanced Parkinson’s disease (NSTAPS study): a randomised controlled trial. Lancet Neurol.12, 37–44 (2013). [DOI] [PubMed] [Google Scholar]
- 32.Flouty, O. et al. Idiopathic Parkinson’s disease and chronic pain in the era of deep brain stimulation: a systematic review and meta-analysis. J. Neurosurg.137, 1821–1830 (2022). [DOI] [PubMed] [Google Scholar]
- 33.Broetz, D., Eichner, M., Gasser, T., Weller, M. & Steinbach, J. P. Radicular and nonradicular back pain in Parkinson’s disease: a controlled study. Mov. Disord. : Off. J. Mov. Disord. Soc.22, 853–856 (2007). [DOI] [PubMed] [Google Scholar]
- 34.Ghilardi, M. G. S. et al. Efficacy of deep brain stimulation of the subthalamic nucleus versus globus pallidus internus on sensory complaints. NPJ Parkinsons Dis.10, 73 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Amato, N. et al. Levodopa-induced dyskinesia in Parkinson disease: Sleep matters. Ann. Neurol.84, 905–917 (2018). [DOI] [PubMed] [Google Scholar]
- 36.Georgiev, D. et al. Long-term effect of bilateral STN-DBS on non-motor symptoms in Parkinson’s disease: a four-year observational, prospective study. Parkinsonism Relat. Disord.89, 13–16 (2021). [DOI] [PubMed] [Google Scholar]
- 37.Ricciardi, L., Sorbera, C., Barbuto, M. & Morgante, F. Sleep disturbances are mainly improved by deep brain stimulation of the subthalamic nucleus. Mov. Disord. : Off. J. Mov. Disord. Soc.34, 154–155 (2019). [DOI] [PubMed] [Google Scholar]
- 38.Ma, R. et al. Sleep outcomes and related factors in Parkinson’s disease after subthalamic deep brain electrode implantation: a retrospective cohort study. Therapeutic Adv. neurological Disord.16, 17562864231161163 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Favre, J., Burchiel, K. J., Taha, J. M. & Hammerstad, J. Outcome of unilateral and bilateral pallidotomy for Parkinson’s disease: patient assessment. Neurosurgery46, 344–353 (2000). discussion 353-345. [DOI] [PubMed] [Google Scholar]
- 40.Gerashchenko, D., Blanco-Centurion, C. A., Miller, J. D. & Shiromani, P. J. Insomnia following hypocretin2-saporin lesions of the substantia nigra. Neuroscience137, 29–36 (2006). [DOI] [PubMed] [Google Scholar]
- 41.Adler, C. H. & Thorpy, M. J. Sleep issues in Parkinson’s disease. Neurology64, S12–S20 (2005). [DOI] [PubMed] [Google Scholar]
- 42.Filion, M. & Tremblay, L. Abnormal spontaneous activity of globus pallidus neurons in monkeys with MPTP-induced parkinsonism. Brain Res.547, 142–151 (1991). [PubMed] [Google Scholar]
- 43.Filion, M., Tremblay, L. & Bédard, P. J. Effects of dopamine agonists on the spontaneous activity of globus pallidus neurons in monkeys with MPTP-induced parkinsonism. Brain Res.547, 152–161 (1991). [PubMed] [Google Scholar]
- 44.Vetrivelan, R., Qiu, M. H., Chang, C. & Lu, J. Role of basal ganglia in sleep-wake regulation: neural circuitry and clinical significance. Front Neuroanat.4, 145 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yuan, X. S. et al. Striatal adenosine A(2A) receptor neurons control active-period sleep via parvalbumin neurons in external globus pallidus. Elife6, 10.7554/eLife.29055 (2017). [DOI] [PMC free article] [PubMed]
- 46.Johnson, M. D. & McIntyre, C. C. Quantifying the neural elements activated and inhibited by globus pallidus deep brain stimulation. J. Neurophysiol.100, 2549–2563 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Noor, M. S., Steina, A. K. & McIntyre, C. C. Dissecting deep brain stimulation evoked neural activity in the basal ganglia. Neurotherapeutics21, e00356 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnson, M. D., Vitek, J. L. & McIntyre, C. C. Pallidal stimulation that improves parkinsonian motor symptoms also modulates neuronal firing patterns in primary motor cortex in the MPTP-treated monkey. Exp. Neurol.219, 359–362 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anderson, M. E., Postupna, N. & Ruffo, M. Effects of high-frequency stimulation in the internal globus pallidus on the activity of thalamic neurons in the awake monkey. J. Neurophysiol.89, 1150–1160 (2003). [DOI] [PubMed] [Google Scholar]
- 50.Bar-Gad, I., Elias, S., Vaadia, E. & Bergman, H. Complex locking rather than complete cessation of neuronal activity in the globus pallidus of a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated primate in response to pallidal microstimulation. J. Neurosci. : Off. J. Soc. Neurosci.24, 7410–7419 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Castillo, P. R. et al. Globus pallidus externus deep brain stimulation treats insomnia in a patient with Parkinson disease. Mayo Clin. Proc.95, 419–422 (2020). [DOI] [PubMed] [Google Scholar]
- 52.Qiu, M. H., Chen, M. C., Wu, J., Nelson, D. & Lu, J. Deep brain stimulation in the globus pallidus externa promotes sleep. Neuroscience322, 115–120 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goelman, G., Dan, R., Růžička, F., Bezdicek, O. & Jech, R. Altered sensorimotor fMRI directed connectivity in Parkinson’s disease patients. Eur. J. Neurosci.53, 1976–1987 (2021). [DOI] [PubMed] [Google Scholar]
- 54.Berardelli, A., Rothwell, J. C., Thompson, P. D. & Hallett, M. Pathophysiology of bradykinesia in Parkinson’s disease. Brain : a J. Neurol.124, 2131–2146 (2001). [DOI] [PubMed] [Google Scholar]
- 55.Biondetti, E. et al. The spatiotemporal changes in dopamine, neuromelanin and iron characterizing Parkinson’s disease. Brain : a J. Neurol.144, 3114–3125 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fu, Y. et al. Adaptive structural changes in the motor cortex and white matter in Parkinson’s disease. Acta neuropathologica144, 861–879 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Meles, S. K. et al. The metabolic pattern of idiopathic REM sleep behavior disorder reflects early-stage Parkinson disease. J. Nucl. Med. : Off. Publ., Soc. Nucl. Med.59, 1437–1444 (2018). [DOI] [PubMed] [Google Scholar]
- 58.Rahayel, S. et al. Abnormal gray matter shape, thickness, and volume in the motor cortico-subcortical loop in idiopathic rapid eye movement sleep behavior disorder: association with clinical and motor features. Cereb. Cortex28, 658–671 (2018). [DOI] [PubMed] [Google Scholar]
- 59.Lim, J. S. et al. Neural substrates of rapid eye movement sleep behavior disorder in Parkinson’s disease. Parkinsonism Relat. Disord.23, 31–36 (2016). [DOI] [PubMed] [Google Scholar]
- 60.Li, Z. et al. Reduced regional activity and functional connectivity within sensorimotor network in Parkinson’s patients with restless legs syndrome. Mol. pain.15, 1744806919882272 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu, J. et al. Altered regional homogeneity and connectivity in cerebellum and visual-motor relevant cortex in Parkinson’s disease with rapid eye movement sleep behavior disorder. Sleep. Med82, 125–133 (2021). [DOI] [PubMed] [Google Scholar]
- 62.Jiang, X. et al. Abnormal gray matter volume and functional connectivity in Parkinson’s disease with rapid eye movement sleep behavior disorder. Parkinson’s Dis.2021, 8851027 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wen, M. C. et al. Neural substrates of excessive daytime sleepiness in early drug naïve Parkinson’s disease: A resting state functional MRI study. Parkinsonism Relat. Disord.24, 63–68 (2016). [DOI] [PubMed] [Google Scholar]
- 64.Hanyu, H. et al. Voxel-based magnetic resonance imaging study of structural brain changes in patients with idiopathic REM sleep behavior disorder. Parkinsonism Relat. Disord.18, 136–139 (2012). [DOI] [PubMed] [Google Scholar]
- 65.Diaz-Galvan, P. et al. Brain glucose metabolism and nigrostriatal degeneration in isolated rapid eye movement sleep behaviour disorder. Brain Commun.5, fcad021 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Peppe, A. et al. Deep brain stimulation of pedunculopontine tegmental nucleus: role in sleep modulation in advanced Parkinson disease patients: one-year follow-up. Sleep35, 1637–1642 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kempster, P. A., Gibb, W. R., Stern, G. M. & Lees, A. J. Asymmetry of substantia nigra neuronal loss in Parkinson’s disease and its relevance to the mechanism of levodopa related motor fluctuations. J. Neurol., Neurosurg., psychiatry52, 72–76 (1989). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Amick, M. M., Grace, J. & Chou, K. L. Body side of motor symptom onset in Parkinson’s disease is associated with memory performance. J. Int. Neuropsychological Soc. : JINS12, 736–740 (2006). [DOI] [PubMed] [Google Scholar]
- 69.Amick, M. M., Schendan, H. E., Ganis, G. & Cronin-Golomb, A. Frontostriatal circuits are necessary for visuomotor transformation: mental rotation in Parkinson’s disease. Neuropsychologia44, 339–349 (2006). [DOI] [PubMed] [Google Scholar]
- 70.Blonder, L. X., Gur, R. E., Gur, R. C., Saykin, A. J. & Hurtig, H. I. Neuropsychological functioning in hemiparkinsonism. Brain cognition9, 244–257 (1989). [DOI] [PubMed] [Google Scholar]
- 71.Djaldetti, R., Ziv, I. & Melamed, E. The mystery of motor asymmetry in Parkinson’s disease. Lancet Neurol.5, 796–802 (2006). [DOI] [PubMed] [Google Scholar]
- 72.Harris, J. P., Atkinson, E. A., Lee, A. C., Nithi, K. & Fowler, M. S. Hemispace differences in the visual perception of size in left hemiParkinson’s disease. Neuropsychologia41, 795–807 (2003). [DOI] [PubMed] [Google Scholar]
- 73.Lee, A. C., Harris, J. P., Atkinson, E. A. & Fowler, M. S. Evidence from a line bisection task for visuospatial neglect in left hemiparkinson’s disease. Vis. Res.41, 2677–2686 (2001). [DOI] [PubMed] [Google Scholar]
- 74.Starkstein, S., Leiguarda, R., Gershanik, O. & Berthier, M. Neuropsychological disturbances in hemiparkinson’s disease. Neurology37, 1762–1764, (1987). [DOI] [PubMed] [Google Scholar]
- 75.Stavitsky, K. et al. Hallucinations, dreaming, and frequent dozing in Parkinson disease: impact of right-hemisphere neural networks. Cogn. Behav. Neurol. : Off. J. Soc. Behav. Cogn. Neurol.21, 143–149 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cubo, E., Martín, P. M., Martin-Gonzalez, J. A., Rodríguez-Blázquez, C. & Kulisevsky, J. Motor laterality asymmetry and nonmotor symptoms in Parkinson’s disease. Mov. Disord. : Off. J. Mov. Disord. Soc.25, 70–75 (2010). [DOI] [PubMed] [Google Scholar]
- 77.Sousouri, G., Baumann, C. R., Imbach, L. L., Huber, R. & Werth, E. Sleep electroencephalographic asymmetry in Parkinson’s disease patients before and after deep brain stimulation. Clin. Neurophysiol.132, 857–863 (2021). [DOI] [PubMed] [Google Scholar]
- 78.Baumann-Vogel, H. et al. The Impact of Subthalamic Deep Brain Stimulation on Sleep-Wake Behavior: A Prospective Electrophysiological Study in 50 Parkinson Patients. Sleep40, 10.1093/sleep/zsx033 (2017). [DOI] [PubMed]
- 79.Amara, A. W. et al. Effects of subthalamic nucleus deep brain stimulation on objective sleep outcomes in Parkinson’s disease. Mov. Disord. Clin. Pract.4, 183–190 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fan, S. Y. et al. Pallidal versus subthalamic nucleus deep brain stimulation for levodopa-induced dyskinesia. Ann. Clin. Transl. Neurol.7, 59–68 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chaudhuri, K. R. et al. The Parkinson’s disease sleep scale: a new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J. Neurol., Neurosurg., psychiatry73, 629–635 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Stiasny-Kolster, K. et al. The REM sleep behavior disorder screening questionnaire-a new diagnostic instrument. Mov. Disord. : Off. J. Mov. Disord. Soc.22, 2386–2393 (2007). [DOI] [PubMed] [Google Scholar]
- 83.Horváth, K. et al. Minimal clinically important difference on Parkinson’s disease sleep scale 2nd version. Parkinson’s Dis.2015, 970534 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Norman, G. R., Sloan, J. A. & Wyrwich, K. W. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med. care41, 582–592 (2003). [DOI] [PubMed] [Google Scholar]
- 85.Horn, A. & Kühn, A. A. Lead-DBS: a toolbox for deep brain stimulation electrode localizations and visualizations. NeuroImage107, 127–135 (2015). [DOI] [PubMed] [Google Scholar]
- 86.Horn, A. et al. Lead-DBS v2: Towards a comprehensive pipeline for deep brain stimulation imaging. NeuroImage184, 293–316 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jia, X. Z. et al. RESTplus: an improved toolkit for resting-state functional magnetic resonance imaging data processing. Sci. Bull. (Beijing)64, 953–954 (2019). [DOI] [PubMed] [Google Scholar]
- 88.Horn, A. et al. Connectivity Predicts deep brain stimulation outcome in Parkinson disease. Ann. Neurol.82, 67–78 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Horn, A. et al. Deep brain stimulation induced normalization of the human functional connectome in Parkinson’s disease. Brain : a J. Neurol.142, 3129–3143 (2019). [DOI] [PubMed] [Google Scholar]
- 90.Irmen, F. et al. Left prefrontal connectivity links subthalamic stimulation with depressive symptoms. Ann. Neurol.87, 962–975 (2020). [DOI] [PubMed] [Google Scholar]
- 91.Villanueva, R. A. M. & Chen, Z. J. (Taylor & Francis, 2019).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon request. The underlying code for this study is available in lead-dbs86 and can be accessed via this link [http://lead-dbs.org].