Abstract
ABSTRACT
Introduction
ISMiHealth is a clinical decision support system, integrated as a software tool in the electronic health record system of primary care, that aims to improve the screening performance on infectious diseases and female genital mutilation (FGM) in migrants. The aim of this study is to assess the health impact of the tool and to perform a process evaluation of its feasibility and acceptability when implemented in primary care in Catalonia (Spain).
Methods and analysis
This study is a cluster randomised control trial where 35 primary care centres in Catalonia, Spain will be allocated into one of the two groups: intervention and control. The health professionals in the intervention centres will receive prompts, through the ISMiHealth software, with screening recommendations for infectious diseases and FGM targeting the migrant population based on an individualised risk assessment. Health professionals of the control centres will follow the current routine practice.
A difference in differences analysis of the diagnostic rates for all aggregated infections and each individual condition between the intervention and control centres will be performed. Mixed-effects logistic regression models will be carried out to identify associations between the screening coverage and predictor factors. In addition, a process evaluation will be carried out using mixed methodology.
Ethics and dissemination
The study protocol has been approved by the institutional review boards at Hospital Clínic (16 June 2022, HCB/2022/0363), Clinical Research Ethics Committee of the Primary Care Research Institute IDIAPJGol (22 June 2022, 22/113-P) and the Almería Research Ethics Committee (27 July 2022, EMC/apg). The study will follow the tenets of the Declaration of Helsinki and Good Clinical Practice. All researchers and associates signed a collaboration agreement in which they undertake to abide by good clinical practice standards.
Findings will be disseminated in peer-reviewed journals and communications to congresses.
Trial registration number
Keywords: Mass Screening, Clinical Decision-Making, INFECTIOUS DISEASES, Electronic Health Records, Primary Health Care
STRENGTHS AND LIMITATIONS OF THE STUDY.
To the best of our knowledge, this is the first cluster randomised controlled trial with embedded process evaluation (using mixed methods) to assess the effectiveness, health impact, feasibility and acceptability of a systematic multidisease screening decision support system (ISMiHealth) targeting migrants at primary care level.
A strength of this study is that ISMiHealth is integrated into the health information system of 35 primary care centres, with a large targeted population. In addition, the use of the tool will be randomly allocated to the intervention and control centres, minimising the risk of confounding.
An asset of the ISMiHealth tool is the improvement of the surveillance and control of infectious diseases and female genital mutilation cases in the migrant population.
A limitation of this study is that the data for the analysis will be extracted from the routine data collected in the electronic health record systems. These data are collected for reasons other than the study objectives which can lead to inaccuracy or insufficient information of some variables.
The ISMiHealth tool provides recommendations that are up to the healthcare worker to follow and to the patient to accept them, therefore results may vary significantly within centres.
Introduction
In an increasingly interconnected world, enhanced by social inequalities and natural catastrophes, migration has become a growing and crucial phenomenon that affects all countries of the world.1 Unprecedented rises in migration to and within the European Union (EU) in recent years have resulted in numerous challenges for health services,2 including in Spain, where the foreign-born population represented 17.2% of the total Spanish population (2023).3
The migrant populations, including migrant workers, undocumented migrants, asylum seekers, refugees and other groups on the move, may have particular health needs when compared with the autochthonous population.1 4 They may be disproportionately affected by key infections, including tuberculosis (TB), HIV, hepatitis B virus (HBV) and hepatitis C virus (HCV) and this increased risk has been associated with the epidemiology of such infections in the country of birth, with socioeconomic risk factors and other comorbidities on arrival to Europe.5 Similarly, certain imported infections, such as strongyloidiasis, schistosomiasis and Chagas disease, only prevalent in migrant populations,6,9 are of increasing importance in non-endemic areas due to the risk of transmission under special circumstances (transplants, blood-transfusion or congenitally),8 and also because they are potentially severe, particularly if there is a diagnosis delay in immunosuppressed patients.9 Moreover, female genital mutilation (FGM) is a neglected condition with a sociocultural component, mostly practiced in sub-Saharan African countries.10 A study conducted in an European country estimated 38 000 migrant women who suffered this practice.11 A Spanish study reported a profound lack of knowledge of health professionals about FGM, which suggests an underdiagnosis of cases and their sequelae, insufficient implementation of protocols of action, and scarce referral of women who suffered FGM to the appropriate specialised services and professionals to attend their health needs.12
Integrated programmes represent a key step forward to deliver more cost-effective services adapted to the needs of migrants within European countries.13 The European Centre for Disease Control and Prevention (ECDC) guidelines14 call for innovative approaches to multidisease testing in high-risk migrants. As primary care is usually the first contact point of the migrant population with the health system (besides urgent care), these health facilities are key to recognise and meet migrants’ health needs.15 16 In Spain, the public health system provides universal coverage and free access to healthcare to everybody, irrespective of the migration status of an individual.17 Thus, the Spanish primary care system is an ideal setting for interventions targeting the migrant population.18
There has been an outstanding development of clinical decision support systems (CDSS) in the last decade19 aimed to improve patient care by strengthening medical decisions. The decrease in consultation time, wrong diagnosis and test duplication in primary care settings support the cost-effectiveness of implementing CDSS.20 Our research group has already developed an innovative prototype CDSS (ISMiHealth),18 which using precision medicine (based on the variables sex, age and country of origin), facilitates targeted screening recommendations to migrant patients presenting for a routine appointment at primary care in Catalonia, Spain. Preliminary data from the pilot study showed that ISMiHealth improves the diagnosis of targeted conditions and that the tool is feasible to implement,18 acceptable to healthcare professionals and well adapted to the primary care context.21
Objectives
The aim of this study is to implement and evaluate an integrated, primary care-based screening programme for communicable diseases and FGM for migrant populations in Spain to promote their health and integration.
Specific objectives
To validate the ISMiHealth tool and evaluate its effectiveness in Catalonia, Spain.
To carry out a process evaluation of the ISMiHealth tool at primary care level in Catalonia, Spain.
To test the ISMiHealth tool in selected primary care centres (PCCs) with another health information system (in Andalusia, Spain).
Methods and analysis
Randomised controlled trial in Catalonia, Spain
Study design and setting
A pragmatic cluster randomised controlled trial, with two parallel groups randomly allocated using a 1:1 ratio, will be conducted in 35 PCCs of four areas of Catalonia, Spain.
Catalonia is among the Spanish regions with the highest proportion of foreign residents, with approximately 1.3 million(16.3%) migrants in 2022.22 This study will be conducted in four different areas of Catalonia, where percentages of the foreign population are as follows: 13.2% in ‘Costa de Ponent’, 16.9% in ‘Tarragona’, 17.4% in ‘Terres de l’Ebre’ and 20.1% in ‘Lleida’.23 24 The screening programme will be implemented in a real-life context in the selected PCCs.
In Catalonia, the registration in the municipal residents’ register grants access to the health system and, accordingly, to primary care irrespective of their legal status as long as the registry in any municipality of Catalonia for more than 3 months is accredited and also under special circumstances if this criterion is not fulfilled.25
The study protocol has been registered at http://www.clinicaltrials.gov on May 22, 2023 (identifier: NCT05868005) and http://www.clinicaltrials.govis aligned with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) reporting guidelines (online supplemental annex 1).26 When reporting the trial results, the Consolidated Standards of Reporting Trials (CONSORT) guidelines for randomised trials will be followed.27
Study population
All general practitioners and nurses working at the participating centres will be included in the study as users of the tool.
The tool and the outcomes of the study will be evaluated in migrant patients, the indirect beneficiaries of the tool. The inclusion criteria for the screening programme are as follows: migrants coming from countries in the geographic areas of Africa, Latin-America, Asia and Eastern Europe, following the categorisation of the United Nations Statistical Commission;28 aged ≥15 years old, assigned to a participating PCC and attending the PCCs for any reason. The exclusion criteria are as follows: for the active TB recommendation, migrants residing in the host country for more than 5 years; for FGM recommendation, being a male.
Screening recommendations
A Spanish guidance on migrant screening recommendations was developed based on a consensus of a country-expert transdisciplinary network after a comprehensive review of national and international guidelines on screening of infectious diseases and FGM in migrants. The following screening recommendations were agreed: HIV serological tests to migrants >15 years old born in a country with an HIV prevalence >1%, based on Spain’s national guidelines.29 Following the ECDC recommendations,14 serological tests for HBV (HBsAg and IgG HBc) and HCV (IgG HCV) will be offered to >15 years old migrants coming from countries with a prevalence >2%. Active TB will be screened through chest radiographies in individuals >15 years old that recently arrived to the host country (<5 years) and that were born in countries with a TB incidence >50 cases/100 000 inhabitants, inspired by the National Institute for Health and Care Excellence guidelines.30
Regarding strongyloidiasis, schistosomiasis and Chagas disease, all >15 years old migrants coming from countries where these conditions are endemic will be tested. The countries endemic for strongyloidiasis and schistosomiasis are also defined in the ECDC guidelines,14 while for Chagas disease, the 21 countries listed by the Pan American Health Organisation31 will be considered. The screening of FGM will target >15 years old females born in the 31 countries that follow this practice, using the data of the United Nations International Children’s Emergency Fund (UNICEF).32
Health centres randomisation and allocation
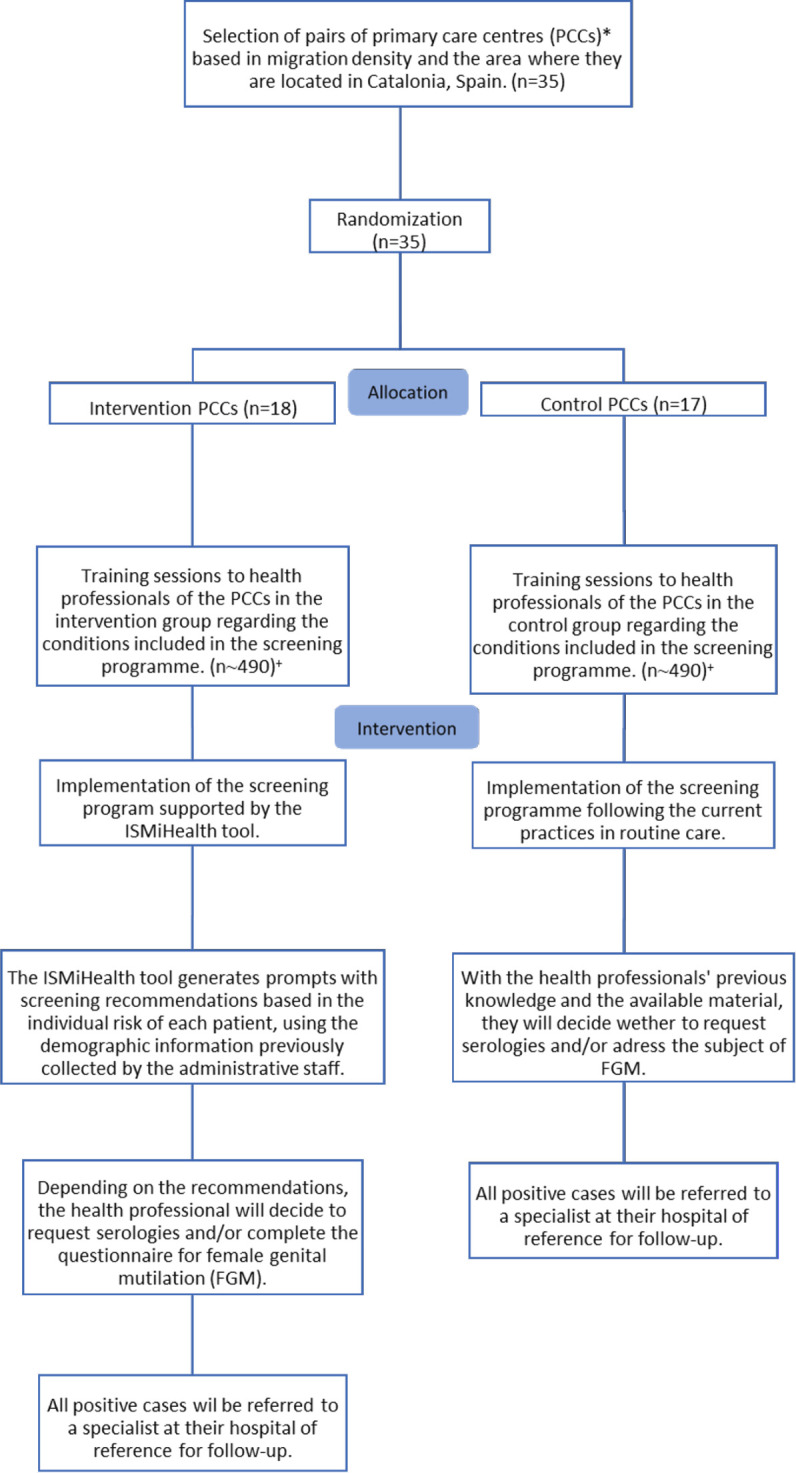
A convenience selection of areas in Catalonia will be performed, based on each primary care management’s interest to participate in the study. Then, the research group will stratify the PCCs by area in Catalonia (Costa de Ponent, Tarragona, Terres de l’Ebre and Lleida) and by density of migrant population in the area (low, medium and high). The PCCs will be paired under these criteria to assure the validity of the results. The randomisation will be performed with the statistical software Stata IC V.16.0 (Stata-16, College Station, TX: StataCorp LLC) for each pair of selected PCC. One PCC will be randomly selected to implement the screening programme supported by the ISMiHealth software (tool-based arm), and it will be compared with the other PCC that will follow the current practices in routine care (non-tool based arm). Therefore, the centres will be randomly allocated to the intervention and control arms using a 1:1 ratio.
Intervention
A multidisease screening programme will be conducted to detect seven infectious diseases (HIV, HBV, HCV, active TB, strongyloidiasis, schistosomiasis and Chagas disease) and FGM cases in the migrant population attended at primary care. First, general practitioners and nurses of all 35 PCCs will receive training sessions on migrant health and the criteria for screening. Then, the intervention will be implemented. Control centres will follow the standard of care supported by the training sessions, whereas in the intervention centres, the screening programme will be facilitated by the ISMiHealth tool.
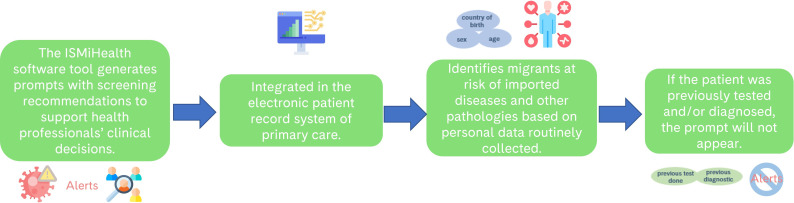
ISMiHealth has already been integrated into the electronic health record (EHR) system of Catalonia, Spain (eCAP)18 and it generates a prompt in the EHR system, as a pending task, with the screening recommendations to be considered by health professionals at the consultation. The software is based on sociodemographic data (country of origin, sex and age) that are routinely registered by the PCC’s administrative staff at the EHR and other parameters, such as, the International Classification Diagnosis (ICD) codes to identify previously diagnosed individuals and laboratory parameters to identify previously tested individuals. Therefore, when an individual attends the PCC for any reason, the health professional will receive real-time prompts with the diseases that should be considered for screening based on an individual risk assessment. ISMiHealth can identify individuals with previous tests and/or diagnosis of any of the conditions included in the screening algorithm and, in such cases, the automated prompt will not show up for that condition (figure 1).
Figure 1. Workflow of the ISMiHealth tool.
All health professionals will be responsible for requesting a screening test and/or the referral to a specialist. Figure 2 shows the flow diagram of the study.
Figure 2. Flow diagram of the ISMiHealth study. *One of the centres was not paired and was allocated in the intervention study arm. +The number of health professionals depends on the human resources of each centre during the study period. PCCs: primary care centres, FGM: female genital mutilation.
Standard care
Control centres (non-tool based arm) will follow the current clinical practice, including the serological tests and the referral pathway of positive cases. When a migrant patient attends the PCC for any reason, health professionals will decide which diseases/conditions should be screened for, according to the existing national/regional guidelines and supported by the aforementioned training programme on the epidemiological background of the conditions.
Training sessions
Before the intervention, health professionals (including medical doctors and nurses) from both intervention and control centres will receive online training sessions on the conditions included: epidemiology, diagnostic tools, available treatments, particular aspects in high-risk groups such as immunosuppressed patients, data on cost-effectiveness and screening recommendations for migrants. Health professionals will have access to the training material during the study period. Participants in the intervention arm will receive practical information (compiled in a video) about the usage of the tool.
Study procedures
All screening tests will fulfil the current clinical practice procedures. The serological tests for HIV and viral hepatitis will be performed according to each centre’s referral laboratory, including HIV antibodies, HBV surface (HBs) antigen and IgG core antibodies, and IgG core antibodies for HCV using an ELISA test. Regarding the serologies of the imported infections, an ELISA test (SciMedx-Corporation, Denville, NJ, USA) will be performed for Strongyloides stercoralis infection, an ELISA for IgG against Schistosoma mansoni (Novagnost S. mansoni IgG; Siemens-Diagnostics, Marburg, Germany) for Schistosoma spp. infection, and two different immunoassays will be used for the detection of a Trypanosoma cruzi infection, a chemiluminescent immunoassays test (Architect Chagas (Abbott laboratories, Wiesbaden, Germany)) and an ELISA test (ORTHO T. cruzi ELISA Test System (Ortho-Clinical Diagnostics)).
The assessment of FGM will be conducted through a short ad hoc questionnaire, linked to the EHR system, that will help health professionals to assess whether this practice is common in the patient’s ethnicity/region/family and if the patient has suffered it. The screening could result in the diagnosis of FGM where health professionals should examine possible health consequences in the female patient and the referral to a specialist.
All positive cases will be referred to a specialist at their hospital of reference, where they will receive follow-up care according to the current clinical practice.
Sample size
Preliminary data from the pilot cluster randomised trial showed that there was a 2.1 (95% CI 1.6–2.6, p-value<0.001) increase of the diagnostic yield in intervention centres (tool-based arm) in comparison with control centres (non-tool based arm),.18 Therefore, to achieve a difference-in-difference detection rate of all aggregated infections of two (with 95% precision) between the intervention and control centres, it was estimated that at least 32 centres should be included in the study. The sample size was estimated using PASS V.16 (NCSS, Kaysville, Utah, USA).
There will be 35 PCCs of which 18 PCCs will be intervention centres and 17 control ones, with one unmatched centre. Approximately 980 health professionals that work in these centres will participate in the study.
The technical pilot test will be conducted from October to December 2023, and the intervention will start in January 2024.
Outcome measures
Primary outcome
The primary outcome measure will be the detection rate of the aggregated infections (HIV, HBV, HCV, active TB, T. cruzi, S. stercoralis and Schistosoma spp.). The monthly detection rate between intervention and control PCCs will be compared before and after implementation of the screening programme. All cases will be classified using predefined case definitions, including the number of diagnoses codified through the ICD-10 codes, number of positive laboratory tests and referrals to specialists.
Secondary outcomes
The secondary outcomes will be as follows: (1) the detection rate of each individual condition (infections and FGM); (2) number of early diagnoses of HIV (based on the CD4 cell count), and VHB and VHC (based on laboratory parameters, such as levels of transaminases, platelets, bilirubin and clotting parameters); (3) number of screening tests performed for the aggregated infections and each individual condition; (4) associations between different sociodemographic and epidemiological factors with the screening tests performed for the aggregated infections and all the individual conditions; (5) number of the diagnosed individuals that have had a follow-up visit in the hospital of reference; (6) number of the diagnosed individuals that have received treatment; (7) number of cured individuals (based on the absence of infection, if possible) and (8) prevalence of each individual condition in the migrant population.
Data sources
Data on test results, diagnoses, specialist referrals, comorbidities and sociodemographic information will be extracted from the EHR system of the Catalan Institute of Health and pseudoanonymised by procedures of the System for the Development of Research in Primary Care (SIDIAP) database.33 34 Data on follow-up visits in the hospital of reference and treatment after diagnosis will be retrieved from the minimum basic data set, also from SIDIAP database. The study variables will be pseudoanonymised, with technical and functional separation, by a data manager. Aggregated data will also be obtained during the process of implementation of the tool with the sole objective of technical monitoring.
The migrant population included in the screening programme will be identified among individuals who attend the selected PCCs for any reason during the intervention period. This study involves handling personal data that are routinely collected in healthcare services. The data extraction will be performed according to the principles established by the healthcare services, including the data protection policies. All processing of patients’ personal data collected within the study will be conducted according to conventional confidentiality.
A data processing agreement will be undertaken with the Primary Care Research Institute IDIAPJGol. All data analyses will be conducted on pseudoanonymised data and no data that could potentially identify an individual will be extracted. Pseudoanonymised data will be stored in the Barcelona Institute for Global Health’s (ISGlobal) local server (VPN) and only participating investigators will have access to the database through credentials.
Statistical analysis
A detailed description is included in the statistical analysis plan (online supplemental annex 2).
For the description of the sample in each study site, summary statistics will be presented as frequencies for categorical variables, means with standard deviation for normally distributed continuous variables and medians with interquartile range for non-normally distributed continuous variables.
The effectiveness of the tool will be evaluated and compared between the intervention and control centres. To analyse the effect of the intervention on all aggregated infections and each individual condition, a difference-in-differences approach will be conducted using a generalised linear model. Linear regressions will be performed for the monthly detection rates, comparing the intervention and control centres. Trends of the monthly detection rate prior to the implementation of the screening programme between both groups will also be analysed.
For the rest of the secondary outcomes, associations with continuous variables will be evaluated using t-tests, one-way analysis of variance, Wilcoxon Rank-Sum and Kruskal-Wallis tests depending on the distribution of the variables. Pearson’s χ2 test or Fisher’s exact test will be performed to evaluate associations between categorical variables and odds ratios (ORs) will be estimated. Mixed-effects logistic regression models will be carried out to identify associations between the screening performance and sociodemographic and epidemiological characteristics, and adjusted ORs will be estimated using the region of the PCC as a random intercept.
The prevalence of each individual condition will be estimated and reported with its respective 95% confidence interval. The prevalence will be defined as the number of diagnoses identified by the screening tests performed among the people that were tested. Serology tests will be contemplated for HIV, HBV, HCV, T. cruzi, S. stercoralis and Schistosoma spp. infections; for active TB, chest radiographies will be examined; and for FGM, the completed questionnaires will be considered.
Stata IC V.16.0 (Stata-16, College Station, TX: StataCorp LLC) will be used to conduct the data analysis and the precision for the reporting of the results will be 95%, considering statistically significant p-values<0.05. Variables with missing values higher than 10% will not be considered for the analysis of the study.
Process evaluation
The purpose of the process evaluation is to understand the effects of the intervention. These effects can help to inform judgements about its validity by highlighting key screening components (construct validity), by demonstrating connections between the ISMiHealth software tool and primary outcomes (internal validity) and between the actual intervention and other contexts (external validity). Our process evaluation design will be informed by Grant’s theoretical framework for process evaluations in cluster-randomised control trials.35 It will be performed before, during and after the trial period (12 months) using both qualitative and quantitative methods. Table 1 enlists the process domains, research questions per domain and corresponding methods at every study stage. The process domains included in the evaluation are context, recruitment of clusters, delivery and response to clusters, reach to healthcare professionals, response of healthcare professionals to the intervention and unintended consequences.
Table 1. Research questions and corresponding methods at different study stages for the evaluation of each process domain.
| Domain | Research question | Method | Study stage for data collection |
| Context | What is the wider context in which the trial is being conducted?What are the main health needs of migrants visiting primary care centres' (PCCs) facilities? | Focus group discussions (FGDs) with migrants and HC professionals | Preintervention |
| Recruitment of clusters | How are clusters sampled and recruited?Who agrees to participate?Why do clusters agree to participate (or not)? | Documentation of the recruitment process by the research teamQuantitative and qualitative comparisons of recruited and non-recruited clusters | Preintervention |
| Delivery to clusters | How intervention is actually delivered for each cluster? | Real-time technical monitoring by data manager | Early intervention |
| Response of clusters | How is the intervention adopted by clusters? | Observations and field notes by study coordinators about how clusters adopt the interventionReal-time technical monitoring by data manager | During intervention |
| Reach to healthcare (HC) professionals and delivery to migrant patients | To what extent is the software tool used by HC professionals and how is the intervention applied in each setting? | Quantitative comparison of those applying versus not applying the screening toolMeasurement of intervention fidelity across its componentsMini-survey of monitoring | During intervention |
| Response of HC professionals to the intervention | How does the HC professional respond?Can the use of the tool be sustained over time (or not)? | Surveys to HC professionals at intervention arm; interviews with PCC managersFGDs with HC professionalsInterviews with migrants who have been screened with the tool | Postintervention |
| Unintended consequences | Are there unintended changes in processes and outcomes related to the trial intervention? | Surveys, interviews (as above) | During intervention and postintervention |
FGDsfocus group discussionsHChealthcarePCCprimary care centres
In the preintervention stage, the context will be analysed (patients’ health needs, primary care resources, healthcare access barriers and facilitators) through focus group discussions (FGDs)36 with professionals and migrant patients. FGDs will be carried out independently in PCCs selected by convenience, with eight to 10 participants, and will last approximately 60–90 min. Three FGDs with healthcare professionals and three with migrant patients attended at the PCCs will be carried out. General practitioners and nurses, with at least 1 year of contract, will be invited to the FGD through an institutional e-mail from their corresponding manager. The migrant patients will be contacted through general practitioners of the PCCs. Additionally, a pilot test of the ISMiHealth software tool will be conducted with various health professionals to ensure its correct functioning.
During the intervention, real-time technical monitoring of the tool by a data manager will be performed. The technical monitoring will help to identify errors in the implementation of the prompts in the EHR system to be mitigated in real-time. Also, the study coordinators of each study area will report prompt incidents periodically to the research team. After six months of delivery, each study coordinator will send a follow-up survey to the PCCs at the intervention arm in all four health regions. This mini-survey will appraise the reachability of the screening strategy in the health centres.
Finally, at the postintervention stage, the research team will assess the response of healthcare professionals to the screening intervention, that is, to what extent they found it useful, any suggestions for improvement and whether its use can be sustained over time. Towards this aim, FGDs with healthcare professionals at PCCs from the intervention arm will be conducted. Also, an ad-hoc survey of the screening programme acceptance and feasibility, targeting health professionals will be carried out. The survey will include questions about the clinical utility of the tool, the frequency with which it had been possible to do the screening and any related difficulties encountered, as well as recommendations for improvement (if any). Finally, individual interviews with migrants who have been screened with the tool will be conducted.
Qualitative data analysis
Data from the FGDs will be collected through digital audio recordings and field notes. The audio recordings will be stored and secured at ISGlobal’s VPN. All FGDs will be manually transcribed, and a thematic analysis will be performed.37 The analysis will consist of six phases: data familiarisation, code generation, themes’ search, themes’ review, definition of final themes and write-up. The qualitative analysis will be triangulated by two researchers. In the preintervention phase, a rapid qualitative assessment38 will be performed to analyse professionals’ narratives with the purpose to identify elements of the screening programme that require adjustments before the beginning of the intervention.
NVIVO software will be used for the qualitative analysis.
Quantitative data analysis
Univariate analysis will be conducted against the main variables (sociodemographic, health centre, number of years with experience in migrant health, etc).
Pilot study in Andalusia, Spain
A pilot cluster randomised controlled trial will be conducted in Andalusia, conducting the intervention in seven PCCs, to evaluate the feasibility, acceptability and adaptability of the ISMiHealth tool in another healthcare setting as well as preliminary effectiveness data.
In this case, additional pathologies have been considered for the screening recommendations of the ISMiHealth tool, including syphilis, latent TB infection and intestinal parasites, as decided in the consensus workshop carried out with health professionals of the corresponding site. The functioning of the ISMiHealth software is slightly different. It is based on demographic data stored in the database of users (BDU) of the Andalusia Health Service (SAS). The tool will produce a checklist, where the health professionals will mark the diseases that the patient has been screened for.
The study data will be extracted retrospectively by a specialised information technology (IT) committee of the SAS Institution, which will include the following: (1) the check-list from the tool and (2) the demographic and clinical variables from the BDU. Then, the IT committee will link this information with laboratory and clinical data of the reference hospital (Hospital Universitario Poniente, Almería) and will pseudoanonymise the data.
The limited number of PCCs may prevent the analysis of the health impact of the tool. Therefore, we plan to estimate preliminary effectiveness data. Nevertheless, because the pilot study will be conducted in sevene PCCs of one area (Almería), we would not be able to carry out mixed-effects logistic regression models and logistic regressions will be performed instead.
Patient and public involvement
Recipients of the screening programme (healthcare professionals and the migrant community) are expected to be involved at several stages of the study process, including the design of the software tool, monitoring and evaluation of the intervention.
The design of the software tool will be informed through FGDs with clinicians on the local needs, resources, barriers and facilitators for using a novel screening tool. The pros and cons, as well as key features and preferences for the prompt system, will be taken into consideration to adjust the tool prototype. The relevance of the research aim for the migrant community will be assessed through migrants’ involvement. Their feedback on the screening programme will be collected through FGDs and an ad-hoc survey as part of the feasibility and acceptability analysis.
Ethics and dissemination
Ethical considerations
The study protocol has been approved by the institutional review boards at Hospital Clínic (16 June 2022, HCB/2022/0363), Clinical Research Ethics Committee of the Primary Care Research Institute IDIAPJGol (22 June 2022, 22/113 P) and the Almería Research Ethics Committee (27 July 2022, EMC/apg). The study will follow the tenets of the Declaration of Helsinki and Good Clinical Practice. If any important amendments to the protocol should be made, all parties will be informed immediately.
The screening programme will only provide recommendations to health professionals according to current guideline recommendations, and they will finally decide what tests should be offered to each patient as part of the clinical practice. Accordingly, an explicit written consent form from migrant individuals will not be necessary. However, a letter of commitment will be required from the Director or a responsible of each PCC agreeing to the participation of their respective primary care team (online supplemental annex 3). On the other hand, for the execution of the FGDs, signatures in the individual informed consents will be collected after explaining the study and the participant information sheet. All data will be deidentified and stored in ISGlobal’s VPN, maintaining the integrity and security of data.
This research project is not expected to have any possibly harmful impact on the individuals involved. If an individual is diagnosed, they will be referred and treated as appropriate according to the routine care standard procedures of each centre. All participating researchers and associates signed a collaboration agreement in which they undertake to abide by good clinical practice standards.
Dissemination
The promoter and investigators are committed to publish the results of the study in journal articles, other scientific publications and communications to congresses.
Perspectives
To the best of our knowledge, this is the first cluster randomised controlled trial that evaluates the effectiveness and health impact of a systematic screening programme for multiple conditions in migrants at primary care level. The fact that the software tool is easily integrated in the EHR system, facilitates its implementation in routine clinical care and has the potential to be scaled-up to other health systems. Moreover, it will increase the knowledge of health professionals in assessing the risk of communicable diseases and other conditions in migrants. Another strength of our study is that the software tool will be randomly allocated to the intervention centres, whereas control centres will follow the current clinical practice, which will minimise the risk of confounding. Finally, the feasibility and acceptability assessment of the screening programme will allow for optimisation of the implementation and its integration into clinical practice.
Trial status
Protocol version 7.0, 18 December 2023. The start date of the trial is 1 January 2024 and the expected completion date is 31 December 2024.
supplementary material
Acknowledgements
We are grateful to the patients and the teams of the primary care centres, the general practitioners, nurses and other staff, who will participate in the study. Special thanks to the different institutions that have been part of the design of the study and will collaborate in the development of the intervention, including the Primary Care Research Institute IDIAPJGol, the Catalan Institute of Health, the System for the Development of Research in Primary Care (SIDIAP), the Information System of the Primary Care Service (SISAP) and the Andalusian Health Service (SAS). We are also thankful to the national experts who participated in the workshops carried out in both study sites, Catalonia and Andalusia, contributing their vast knowledge for the development of the screening recommendations.
Footnotes
Funding: The ISMiHealth project is supported by a grant from Instituto de Salud Carlos III (ISCIII), cofinanced by the European Regional Development Fund (FEDER) from the European Union, through the 'Fondo de Investigación para la Salud (FIS)', grant number PI21/00651. ISGlobal acknowledges support from the grant CEX2018-000806-S funded by MCIN/AEI/ 10.13039/501100011033, and support from the Generalitat de Catalunya through the CERCA programme. ACz is funded by ISCIII cofinanced by FEDER from the European Union through the 'Contratos predoctorales de formación en investigación (PFIS)', grant number FI22/00156. AR-M receives funding from the Strategic Research Programme in Epidemiology at Karolinska Institute. The funders of the study had no role in the study design nor the development of the protocol.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-078337).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
Angeline Cruz, Email: angeline.cruz@isglobal.org.
Alba Cuxart-Graell, Email: alba.cuxart@isglobal.org.
Alessandra Queiroga Gonçalves, Email: aqueiroga@idiapjgol.info.
José Vázquez-Villegas, Email: joseb.vazquez.sspa@juntadeandalucia.es.
Silvia Vallejo-Godoy, Email: silvia.vallejo.sspa@juntadeandalucia.es.
Joaquín Salas-Coronas, Email: joaquin.salas.sspa@juntadeandalucia.es.
Nicolás Piqueras, Email: nicolasm.piqueras.sspa@juntadeandalucia.es.
Sara Martínez-Torres, Email: smartinez@idiapjgol.info.
Eva Artigues-Barberà, Email: eartigues.lleida.ics@gencat.cat.
Yolanda Rando-Matos, Email: yrando.apms.ics@gencat.cat.
Ana Aguilar Margalejo, Email: aaguilar.apms.ics@gencat.cat.
Jesús Vizcaíno, Email: jvizcaino.tgn.ics@gencat.cat.
Pilar Requena, Email: prequena@ugr.es.
Ángela Martínez-Pérez, Email: angela.martinez@isglobal.org.
Elisabet Ferrer, Email: elisabet.ferrer@vhir.org.
Leonardo Méndez-Boo, Email: lmendezboo@gencat.cat.
Ermengol Coma, Email: ecomaredon@gencat.cat.
María Pilar Luzón-García, Email: mp.luzon.sspa@juntadeandalucia.es.
Ethel Sequeira-Aymar, Email: ethel.sequeira@isglobal.org.
Aina Casellas, Email: aina.casellas@isglobal.org.
Marta Vázquez-Montiel, Email: marta.vazquez.montiel.sspa@juntadeandalucia.es.
Constanza Jacques-Aviñó, Email: cjacques@idiapjgol.info.
Laura Medina-Perucha, Email: lmedina@idiapjgol.org.
Elisa Sicuri, Email: elisa.sicuri@isglobal.org.
Stella Evangelidou, Email: stella.evangelidou@isglobal.org.
Carina Aguilar Martín, Email: caguilar.ebre.ics@gencat.cat.
Ana Requena-Mendez, Email: requena.mendez@ki.se.
References
- 1.McAuliffe M, Triandafyllidou A. Geneva: 2021. World migration report 2022. [DOI] [Google Scholar]
- 2.Rome:: Ministero dell’Interno; 2015. Study group on the reception system. Report on the reception of migrants and refugees in Italy. Aspects, procedures, problems. [Google Scholar]
- 3.Instituto Nacional de Estadística Series detalladas desde 2002. Resultados nacionales. población residente por fecha, sexo, grupo de edad y país de nacimiento. 2023. [30-May-2023]. https://www.ine.es/jaxiT3/Datos.htm?t=56937 Available. Accessed.
- 4.World Health Organization Refugee and migrant health. 2022. [30-May-2023]. https://www.who.int/news-room/fact-sheets/detail/refugee-and-migrant-health Available. Accessed. [PubMed]
- 5.European Centre for Disease Prevention and Control . Stockholm: 2014. Assessing the burden of key infectious diseases affecting migrant populations in the EU/EEA. [Google Scholar]
- 6.Asundi A, Beliavsky A, Liu XJ, et al. Prevalence of strongyloidiasis and schistosomiasis among migrants: a systematic review and meta-analysis. Lancet Glob Health. 2019;7:e236–48. doi: 10.1016/S2214-109X(18)30490-X. [DOI] [PubMed] [Google Scholar]
- 7.Requena-Méndez A, Aldasoro E, de Lazzari E, et al. Prevalence of Chagas Disease in Latin-American Migrants Living in Europe: A Systematic Review and Meta-analysis. PLoS Negl Trop Dis. 2015;9:e0003540. doi: 10.1371/journal.pntd.0003540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Requena-Méndez A, Albajar-Viñas P, Angheben A, et al. Health Policies to Control Chagas Disease Transmission in European Countries. PLoS Negl Trop Dis. 2014;8:e3245. doi: 10.1371/journal.pntd.0003245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Requena-Méndez A, Buonfrate D, Gomez-Junyent J, et al. Evidence-Based Guidelines for Screening and Management of Strongyloidiasis in Non-Endemic Countries. Am J Trop Med Hyg. 2017;97:645–52. doi: 10.4269/ajtmh.16-0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization Female genital mutilation. Fact sheet. 2023. [11-Jul-2023]. https://www.who.int/news-room/fact-sheets/detail/female-genital-mutilation Available. Accessed.
- 11.Jordal M, Wahlberg A. Challenges in providing quality care for women with female genital cutting in Sweden - A literature review. Sex Reprod Healthc. 2018;17:91–6. doi: 10.1016/j.srhc.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 12.González-Timoneda A, Ruiz Ros V, González-Timoneda M, et al. Knowledge, attitudes and practices of primary healthcare professionals to female genital mutilation in Valencia, Spain: are we ready for this challenge? BMC Health Serv Res . 2018;18:579. doi: 10.1186/s12913-018-3396-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seedat F, Hargreaves S, Nellums LB, et al. How effective are approaches to migrant screening for infectious diseases in Europe? A systematic review. Lancet Infect Dis. 2018;18:e259–71. doi: 10.1016/S1473-3099(18)30117-8. [DOI] [PubMed] [Google Scholar]
- 14.European Centre for Disease Prevention and Control . Stockholm: 2018. Public health guidance on screening and vaccination for infectious diseases in newly arrived migrants within the EU/EEA. [Google Scholar]
- 15.World Health Organization Declaration of Alma-Ata International Conference on primary health care, Alma-Ata, USSR, 6-12 September 1978. 1978
- 16.O’Donnell CA, Burns N, Mair FS, et al. Reducing the health care burden for marginalised migrants: The potential role for primary care in Europe. Health Policy. 2016;120:495–508. doi: 10.1016/j.healthpol.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Boletín Oficial del Estado . Spain: BOE núm; 2018. Real Decreto-ley 7/2018, de 27 de julio, sobre el acceso universal al Sistema Nacional de Salud; pp. 76258–64. [Google Scholar]
- 18.Sequeira-Aymar E, Cruz A, Serra-Burriel M, et al. Improving the detection of infectious diseases in at-risk migrants with an innovative integrated multi-infection screening digital decision support tool (IS-MiHealth) in primary care: a pilot cluster-randomized-controlled trial. J Travel Med. 2022;29:taab100. doi: 10.1093/jtm/taab100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Dort BA, Zheng WY, Sundar V, et al. Optimizing clinical decision support alerts in electronic medical records: a systematic review of reported strategies adopted by hospitals. J Am Med Inform Assoc. 2021;28:177–83. doi: 10.1093/jamia/ocaa279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutton RT, Pincock D, Baumgart DC, et al. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17. doi: 10.1038/s41746-020-0221-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonçalves AQ, Sequeira-Aymar E, Aguilar Martín C, et al. Usefulness and practicality of a multidisease screening programme targeting migrant patients in primary care in Spain: a qualitative study of general practitioners. BMJ Open. 2022;12:e065645. doi: 10.1136/bmjopen-2022-065645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Instituto Nacional de Estadística Principales series de población desde 1998. Comunidades autónomas. Población extranjera por Nacionalidad, comunidades, Sexo y Año. 2022. [30-May-2023]. https://www.ine.es/jaxi/Datos.htm?path=/t20/e245/p08/l0/&file=02005.px Available. Accessed.
- 23.Institut d’Estadística de Catalunya Població estrangera a 1 de gener. Per àmbits del pla territorial. Catalunya. 2022. [30-May-2023]. https://www.idescat.cat/poblacioestrangera/?b=3 Available. Accessed.
- 24.Generalitat de Catalunya Pla de salut 2021-2025 de la Regió Sanitària Barcelona Àmbit Metropolità Sud. 2022
- 25.Generalitat de Catalunya Què són i com s’assignen els nivells de cobertura? Canal Salut. 2022. [04-Sep-2024]. https://catsalut.gencat.cat/ca/coneix-catsalut/acces-sistema-salut/nivells-cobertura/que-son-i-com-sassignen/index.html Available. Accessed.
- 26.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:1–9. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.United Nations Statistics Division Methodology. Standard country or area codes for statistical use (M49) [30-May-2023]. https://unstats.un.org/unsd/methodology/m49/ Available. Accessed.
- 29.Ministerio de Sanidad Servicios Sociales e Igualdad Plan Nacional sobre Sida, Guía de Recomendaciones para el diagnóstico Precoz del VIH en el ámbito sanitario. 2014. [01-Jun-2023]. https://www.sanidad.gob.es/ciudadanos/enfLesiones/enfTransmisibles/sida/docs/GuiaRecomendacionesDiagnosticoPrecozVIH.pdf Available. Accessed.
- 30.Office for Health Improvement and Disparities Guidance. Tuberculosis (TB): migrant health guide. GOV.UK. 2014. [31-May-2023]. https://www.gov.uk/guidance/tuberculosis-tb-migrant-health-guide Available. Accessed.
- 31.Pan American Health Organization Chagas disease. [30-May-2023]. https://www.paho.org/en/topics/chagas-disease Available. Accessed.
- 32.UNICEF Female genital mutilation (FGM) statistics - UNICEF data. 2023. [30-May-2023]. https://data.unicef.org/topic/child-protection/female-genital-mutilation/ Available. Accessed.
- 33.Bolíbar B, Fina Avilés F, Morros R, et al. SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research. Med Clin (Barc) 2012;138:617–21. doi: 10.1016/j.medcli.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 34.Recalde M, Rodríguez C, Burn E, et al. Data Resource Profile: The Information System for Research in Primary Care (SIDIAP) Int J Epidemiol. 2022;51:e324–36. doi: 10.1093/ije/dyac068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grant A, Treweek S, Dreischulte T, et al. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials. 2013;14:1–10. doi: 10.1186/1745-6215-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilkinson S. Qualitative Research Theory, Method and Practice, 2. 2004. Focus group research; pp. 177–99. [Google Scholar]
- 37.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 38.Nevedal AL, Reardon CM, Opra Widerquist MA, et al. Rapid versus traditional qualitative analysis using the Consolidated Framework for Implementation Research (CFIR) Impl Sci. 2021;16:67. doi: 10.1186/s13012-021-01111-5. [DOI] [PMC free article] [PubMed] [Google Scholar]