Abstract
Background
Lung cancer remains the primary cause of cancer-related mortality globally, treated using immune checkpoint inhibitors (ICIs), which are introducing new therapeutic potential and complexities, including severe immune-related adverse events (irAEs) and rare fistula formation. The interaction between coronavirus disease 2019 (COVID-19) and ICIs further complicates treatment outcomes, occasionally leading to spontaneous tumor regression, suggesting potential immune response modulation by COVID-19. This report elucidates a unique case of non-small cell lung cancer (NSCLC) managed with these challenges, highlighting the delicate balance required for modern oncological care.
Case Description
A 44-year-old male patient with stage IIIC NSCLC, no driver mutations such as those in epidermal growth-factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genes, and a tumor proportion score of <1% experienced multiple complications after ICI plus chemotherapy. The treatment regimen comprised durvalumab, tremelimumab, carboplatin, and nab-paclitaxel. The patient experienced multiple complications including: (I) esophageal mediastinal fistula; (II) severe irAEs such as grade 3 colitis; (III) COVID-19 and Candida albicans infections; (IV) cytokine release syndrome; and (V) myocarditis. Treatment interventions included high-dose steroids, antifungal therapy, mechanical support in the intensive care unit, and hemodialysis. The patient showed remarkable tumor regression and recovery from acute adverse events with eventual tumor resolution and closure of the esophageal mediastinal fistula. Tumor cells were positive for angiotensin-converting enzyme 2, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may have infected tumor cells and caused an antitumor effect as an oncolytic virus.
Conclusions
Clinicians should be aware that COVID-19 might be associated with the development of severe irAEs and unexpectedly enhanced antitumor effects. The findings also suggest new fields of study regarding the interaction between viral infection and tumor immune response, which may inform future therapeutic approaches.
Keywords: Esophagomediastinal fistula, immune checkpoint inhibitors (ICIs), non-small cell lung cancer (NSCLC), case report
Highlight box.
Key findings
• The key findings of this study highlight the intricate balance required in treating non-small cell lung cancer with immune checkpoint inhibitors (ICIs). The case report describes a 44-year-old patient who developed multiple complications, including severe immune-related adverse events (irAEs), cytokine release syndrome, and an esophagomediastinal fistula, after ICI treatment. Despite these complications, the patient experienced significant tumor regression.
What is known and what is new?
• ICIs have transformed cancer treatment but can cause severe irAEs. Coronavirus disease 2019 (COVID-19) can exacerbate irAEs in patients undergoing ICI therapy.
• The study presents a rare case of an esophagomediastinal fistula in a lung cancer patient, previously unreported in such cases. It suggests a potential link between COVID-19 infection and enhanced antitumor immunity, contributing to rapid tumor regression but also severe complications.
What is the implication, and what should change now?
• The interaction between COVID-19 and ICI therapy might enhance antitumor effects, possibly acting as an oncolytic virus. However, it also raises the risk of severe irAEs and complications like fistula formation. Clinicians should closely monitor lung cancer patients receiving ICIs, especially in the context of COVID-19, for signs of severe irAEs and unusual complications. Further research is necessary to understand the mechanisms by which COVID-19 influences tumor immunity and how this knowledge can be leveraged to improve cancer treatment strategies.
Introduction
Background
Lung cancer is the leading cause of cancer-related mortality worldwide and presents significant challenges in terms of diagnosis, staging, and treatment. Recent statistics indicate that non-small cell lung cancer (NSCLC) remains a leading cause of cancer-related mortality, with the coronavirus disease 2019 (COVID-19) pandemic introducing new challenges in managing patients with NSCLC (1,2). The advent of immune checkpoint inhibitors (ICIs) has revolutionized the treatment landscape, offering new hope for patients with advanced cancer. However, these therapies are not without risk, as they can induce complications, such as serious immune-related adverse events (irAEs) and, although rare, fistula formation.
Rationale and knowledge gap
The global COVID-19 epidemic has further complicated cancer treatment with ICIs, with studies indicating an increase in the incidence and severity of irAEs in patients undergoing such treatments. Although severe iAEs increased with COVID-19 (3), there are reports of spontaneous tumor regression after COVID-19 (4-6), suggesting that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may be involved in the tumor immune response.
Objective
This case report details the management of a 44-year-old patient with NSCLC who developed multiple complications after ICI treatment, including an esophageal mediastinal fistula, severe irAEs, and infection. This case exemplifies the complex balance required in cancer treatment, where an aggressive treatment strategy with ICIs can result in both tumor remission and severe irAEs. We present this case in accordance with the CARE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-444/rc).
Case presentation
Initial presentation
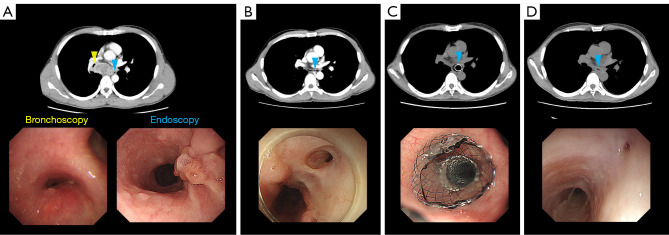
A 44-year-old man with no previous medical history visited the hospital because of an esophageal transit disorder. The patient underwent endobronchial ultrasound-guided transbronchial needle aspiration at station 7 for a mass in the right lower lobe with associated intrathoracic adenopathy. The tumor had metastasized to the mediastinum and compressed the right bronchus, partially exposing itself to the esophagus (Figure 1A). Histological examination revealed NSCLC. Subsequently, imaging confirmed a stage IIIC NSCLC diagnosis. The patient tested negative for driver mutations, such as those in epidermal growth-factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genes, with a tumor proportion score of <1%.
Figure 1.
Chest CT and endoscopy results. (A) Before starting chemotherapy, the tumor in the mediastinum was observed to be compressing the bronchial wall and was partially exposed to the esophagus. (B) After 42 days of chemotherapy, the tumor disappeared; however, an air space extended from the esophagus into the mediastinum. Endoscopy revealed a fistula at the same site. (C) Endoscopic examination showing that the fistula was covered by the stent immediately after placement of the esophageal stent. (D) After removal of the esophageal stent, CT revealed the absence of a tumor. Endoscopy revealed a small dimple at the site of the fistula. Yellow arrowhead represents bronchoscopic observation sites, and blue arrowheads represent gastrointestinal endoscopic observation sites. CT, computed tomography.
Treatment regimen
The patient received durvalumab (1,500 mg/body, day 1) plus tremelimumab (75 mg/body, day 1) and chemotherapy. The chemotherapy regimen comprised carboplatin (an area under the curve of 6) on day 1 and nab-paclitaxel (100 mg/m2) on days 1, 8, and 15.
Complications
On day 8 of treatment, the patient developed grade 2 liver dysfunction with fever that spontaneously resolved. On day 34 of treatment, the patient developed grade 3 colitis. Therefore, 125 mg/day methylprednisolone (mPSL) was administered and the symptoms resolved. However, the patient again developed a fever on day 37. Blood culture findings were negative; however, the patient tested positive for COVID-19, and remdesivir was administered. On day 39, the patient developed diarrhea over 20 times a day, with worsening colitis; therefore, mPSL 1 g was administered during days 39–41. On day 42, the enteritis recovered to grade 2; however, the patient again developed fever on day 43. Blood culture revealed the presence of Candida albicans. Contrast-enhanced computed tomography (CT) revealed a marked reduction in lymph node metastasis at station 7; however, an esophagomediastinal fistula developed (Figure 1B). Fungalemia may have been a hematogenous infection from the esophagomediastinal fistula; therefore, we terminated oral intake and initiated feeding through a tube and central vein. On the night of day 43, the patient went into shock and developed cytokine release syndrome (CRS) and myocarditis.
Antifungal drugs, mPSL 1 g pulse for five days, tocilizumab 8 mg/kg once, immunoglobulin 5 g for 3 days, vasopressor agents, and hemodialysis were administered in the intensive care unit. Intensive therapy was successful, and the patient’s vital signs stabilized within approximately one week. Dialysis was completed after 2 months. After the fungemia diagnosis, the patient developed Candida endophthalmitis; however, it resolved without sequelae. Two months after CRS onset, the patient developed cytomegalovirus infection, which was resolved with ganciclovir treatment. Steroid therapy was tapered over 4 months.
Two months after CRS onset, an esophageal stent was placed for the esophagomediastinal fistula (Figure 1C) and oral intake was restarted. Five months after CRS onset, the esophageal stent was removed and the esophagomediastinal fistula was closed, leaving only a small dimple (Figure 1D). More than 6 months after the beginning of treatment, CT showed tumor remission with no recurrence. Figure 2 illustrates the clinical course of the patient. A brief progress table is presented as Table S1.
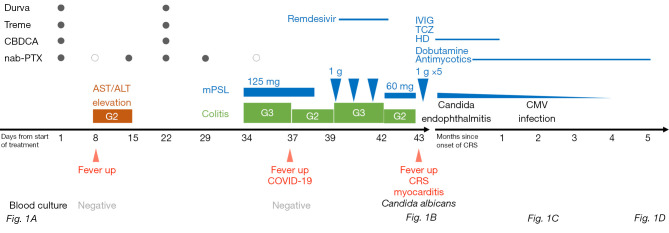
Figure 2.
Clinical course. Durva, durvalumab; Treme, tremelimumab; CBDCA, carboplatin; nab-PTX, nab-paclitaxel; AST, aspartate transaminase; ALT, alanine transaminase; G, grade; mPSL, methylprednisolone; COVID-19, coronavirus disease 2019; CRS, cytokine releasing syndrome; IVIG, intravenous immunoglobulin; TCZ, tocilizumab; HD, hemodialysis; CMV, cytomegalovirus; Fig, figure.
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Esophagomediastinal fistula is a serious and fatal complication of esophageal cancer and cancer therapy; however, it has never been observed in lung cancer. Esophageal fistulas develop in 6–10% of patients with esophageal cancer who receive ICI after chemoradiotherapy (7). Fistula development in esophageal cancer is associated with tumor regression after treatment, presenting risk factors such as advanced cancer, large tumors, upper central esophageal invasion, stenting, and radiotherapy (8,9). In chemoradiotherapy, the median time from the initial diagnosis to fistula development is 7.9 months (10). Furthermore, the time to fistula development in patients receiving ICI treatment after chemoradiotherapy for esophageal and lung cancers is 3–4 months (10,11). Therefore, ICI responses may be associated with mucosal defects. In the present report, the patient developed an esophagomediastinal fistula approximately 6 weeks earlier. Fistula formation was probably due to the esophageal involvement of mediastinal lymph node metastases and a significant response to ICI treatment. Similar complications have been reported in other cases of NSCLC treated with ICIs. For instance, tracheamediastinal and tracheoesophageal fistulas have been reported as rare complications of ICI therapy in advanced lung cancer (10,11). In both previous reports, other factors such as chemoradiotherapy, mechanical irritation with esophageal stents, and delayed wound healing with angiogenesis inhibitors were considered as potential factors for fistula formation; however, the fistula formed 6–10 weeks after ICI administration, and a temporal causal relationship with the other factors could not be established, making the ICI a suspect drug. In the present case, although cytotoxic chemotherapy was administered concurrently, the course of treatment is consistent with previous reports that ICIs are most likely to be involved in fistula formation.
In this report, the patient developed severe irAEs, CRS, and myocarditis, in addition to marked tumor shrinkage after COVID-19, particularly colitis that had already developed after the worsening of COVID-19. Recent retrospective studies have revealed that during ICI therapy, COVID-19 increases the frequency of grade 3 or higher irAEs, and the use of anti-programmed cell death protein 1 (PD-1) + anti-cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) antibodies is a risk factor (3). Furthermore, ICI-receiving patients undergoing immunosuppressive therapy are at an increased risk of severe COVID-19 and CRS (12). Therefore, this patient may have experienced exacerbation of COVID-19-triggered irAEs.
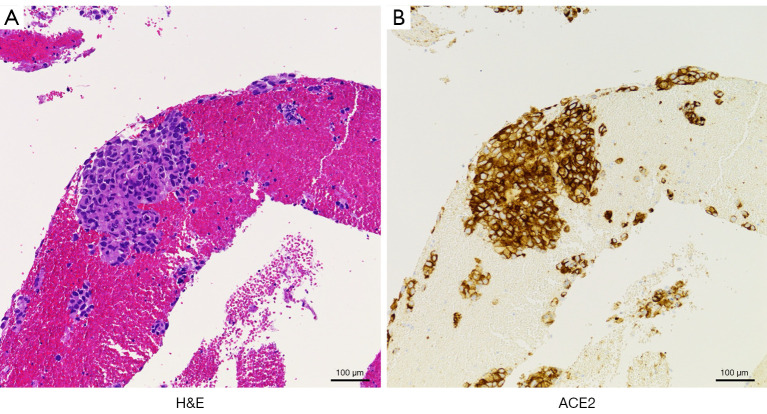
In this case, COVID-19 was also considered a factor contributing to the rapid antitumor effect and esophagomediastinal fistula development. Similar to irAEs, antitumor immunity may be enhanced by COVID-19. Studies have shown spontaneous tumor regression after COVID-19 in lung cancer, other carcinomas, and hematologic tumors (4-6). The mechanisms underlying the enhanced antitumor immunity observed in our case may include viral tumor infection, tumor lysis, and innate immune activity. The hypothesis that SARS-CoV-2 may act as an oncolytic virus, which selectively kills cancer cells and boosts immune response, is supported by several studies. For example, studies have shown that oncolytic viruses can induce cell death and cancer antigen release (13). Additionally, SARS-CoV-2 infection mechanism via angiotensin-converting enzyme 2 (ACE2) expression could further support this hypothesis (14). Recently, a combination therapy involving oncolytic viruses and ICIs has been developed in clinical settings, with excellent therapeutic efficacy (15). In the present case, tumor cells were strongly positive for ACE2 expression (Figure 3), suggesting that SARS-CoV-2 also infected the tumor cells. In this case, we hypothesized that SARS-CoV-2 may have infected the tumor cells during ICI therapy and enhanced the antitumor effect as an oncolytic virus. As similar cases have not yet been reported, continued hypothesis testing is required in the future.
Figure 3.
Pathological findings of endobronchial ultrasound-guided transbronchial needle aspiration at station 7. H&E staining of the biopsy specimen revealed tumor cells (A) expressing ACE2 on the cell membrane (B), which is critical in the infection mechanism of SARS-CoV-2, suggesting that SARS-CoV-2 also infected tumor cells. The scale bars represent 100 µm. H&E, hematoxylin and eosin; ACE2, angiotensin-converting enzyme 2; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Conclusions
Clinicians should carefully monitor the presence of COVID-19 during ICI therapy, as it may be associated with severe irAE development or unexpectedly enhanced antitumor effects. Future research should explore the mechanisms by which viral infections influence tumor immunity and investigate potential therapeutic strategies that leverage these interactions.
Supplementary
The article’s supplementary files as
Acknowledgments
We would like to thank Editage (www.editage.jp) for the English language editing.
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Footnotes
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-444/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-444/coif). The authors have no conflicts of interest to declare.
References
- 1.Reyes R, López-Castro R, Auclin E, et al. MA03.08 Impact of COVID-19 Pandemic in the Diagnosis and Prognosis of Lung Cancer. J Thorac Oncol 2021;16:S141. [Google Scholar]
- 2.Kumar S, Chmura S, Robinson C, et al. Alternative Multidisciplinary Management Options for Locally Advanced NSCLC During the Coronavirus Disease 2019 Global Pandemic. J Thorac Oncol 2020;15:1137-46. 10.1016/j.jtho.2020.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo M, Liu J, Miao R, et al. A Single Center Retrospective Study of the Impact of COVID-19 Infection on Immune-related Adverse Events in Cancer Patients Receiving Immune Checkpoint Inhibitors. J Immunother 2022;45:389-95. 10.1097/CJI.0000000000000440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang X, Chen J, Sun J, et al. Tumor reduction after SARS CoV 2 infection in a patient with lung cancer: A case report. Oncol Lett 2024;27:169. 10.3892/ol.2024.14302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pasin F, Mascalchi Calveri M, Calabrese A, et al. Oncolytic effect of SARS-CoV2 in a patient with NK lymphoma. Acta Biomed 2020. doi: . 10.23750/abm.v91i3.10141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ottaiano A, Scala S, D'Alterio C, et al. Unexpected tumor reduction in metastatic colorectal cancer patients during SARS-Cov-2 infection. Ther Adv Med Oncol 2021;13:17588359211011455. 10.1177/17588359211011455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu J, Deng R, Ni T, et al. Efficacy and safety of radiotherapy/chemoradiotherapy combined with immune checkpoint inhibitors for locally advanced stages of esophageal cancer: A systematic review and meta-analysis. Front Oncol 2022;12:887525. 10.3389/fonc.2022.887525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goh KJ, Lee P, Foo AZX, et al. Characteristics and Outcomes of Airway Involvement in Esophageal Cancer. Ann Thorac Surg 2021;112:912-20. 10.1016/j.athoracsur.2020.10.015 [DOI] [PubMed] [Google Scholar]
- 9.Choi MK, Park YH, Hong JY, et al. Clinical implications of esophagorespiratory fistulae in patients with esophageal squamous cell carcinoma (SCCA). Med Oncol 2010;27:1234-8. 10.1007/s12032-009-9364-z [DOI] [PubMed] [Google Scholar]
- 10.Sumi T, Ikeda T, Kure K, et al. Bronchomediastinal Fistula During Durvalumab Therapy After Chemoradiotherapy in Stage III NSCLC. J Thorac Oncol 2019;14:1860-1. 10.1016/j.jtho.2019.06.003 [DOI] [PubMed] [Google Scholar]
- 11.Yao Y, Liu Z, Li Q, et al. Successful immune checkpoint inhibitor-based rechallenge in a patient with advanced esophageal squamous cell cancer: A case report. Thorac Cancer 2022;13:497-501. 10.1111/1759-7714.14279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bakouny Z, Labaki C, Grover P, et al. Interplay of Immunosuppression and Immunotherapy Among Patients With Cancer and COVID-19. JAMA Oncol 2023;9:128-34. 10.1001/jamaoncol.2022.5357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melcher A, Harrington K, Vile R. Oncolytic virotherapy as immunotherapy. Science 2021;374:1325-6. 10.1126/science.abk3436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020;181:271-280.e8. 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahalingam D, Wilkinson GA, Eng KH, et al. Pembrolizumab in Combination with the Oncolytic Virus Pelareorep and Chemotherapy in Patients with Advanced Pancreatic Adenocarcinoma: A Phase Ib Study. Clin Cancer Res 2020;26:71-81. 10.1158/1078-0432.CCR-19-2078 [DOI] [PMC free article] [PubMed] [Google Scholar]