Abstract
目的
报告近五年某医院从肿瘤患者样本分离的病原菌特征和多重耐药菌检出率,为感染防控提供参考。
方法
回顾性收集四川大学华西医院2019年1月−2023年12月期间6428例肿瘤患者样本的病原学培养及菌株体外敏感性结果,总结数据趋势。
结果
从80386份样本中分离到病原菌16393株,检出率为20.4%;剔除从同一患者分离的重复菌株,7951株(81.1%)细菌菌株中以大肠埃希菌(14.5%)、肺炎克雷伯菌(13.2%)、金黄色葡萄球菌(9.4%)、鲍曼不动杆菌复合群(9.3%)和铜绿假单胞菌(7.7%)为主;1857株(18.9%)真菌菌株中以白色念珠菌(56.5%)、热带念珠菌(9.0%)和近平滑念珠菌(8.0%)最常见。主要菌种的样本来源不同,不同肿瘤来源的菌种分布也不同(P<0.05)。耐碳青霉烯大肠埃希菌和肺炎克雷伯菌的检出率分别为2.5%(29/1152)和12.3%(129/1050);耐甲氧西林金黄色葡萄球菌的检出率为22.0%(165/749),近四年的检出率呈上升趋势(P<0.01);耐碳青霉烯鲍曼不动杆菌和铜绿假单胞菌的检出率分别为40.3%(298/739)和8.8%(54/612)。
结论
肿瘤患者病原菌以革兰阴性菌为主,多重耐药菌的检出率较高,耐甲氧西林金黄色葡萄球菌的检出率呈上升趋势。
Keywords: 肿瘤, 病原, 耐药, 多重耐药菌
Abstract
Objective
To investigate the characteristics of the pathogens isolated from the specimens of tumor patients and detection rates of multidrug-resistant bacteria in a hospital in the past five years, so as to provide references for infection prevention and control.
Methods
The results of pathogenic culture and in vitro susceptibility of the strains isolated from the specimens collected between January 2019 and December 2023 from tumor patients were retrospectively collected, and the trends of the data were analyzed and summarized.
Results
A total of 16393 strains were isolated from 80386 specimens, producing a detection rate of 20.4%. After excluding the duplicate strains isolated from the same patients, Escherichia coli (14.5%), Klebsiella pneumoniae (13.2%), Staphylococcus aureus (9.4%), Acinetobacter baumannii complex (9.3%), and Pseudomonas aeruginosa (7.7%) predominated the 7951 (81.1%) bacterial strains. Among the 1857 (18.9%) fungal strains, Candida albicans (56.5%), Candida tropicalis (9.0%), and Candida parapsilosis (8.0%) were the most common ones. The specimen sources differed among the prevalent species, and the species distribution varied among specimens from different types of tumors (P<0.05). The detection rates of carbapenem-resistant Escherichia coli and Klebsiella pneumoniae were 2.5% (29/1152) and 12.3% (129/1050), respectively. The detection rate of methicillin-resistant Staphylococcus aureus was 22.0% (165/749), maintaining an upward trend in the last four years (P<0.01). The detection rates of carbapenem-resistant Acinetobacter baumannii and Pseudomonas aeruginosa were 40.3% (298/739) and 8.8% (54/612), respectively.
Conclusion
Gram-negative bacteria were the prevalent pathogens of tumor patients. The detection rate of multidrug-resistant bacteria was relatively high, and the detection rate of methicillin-resistant Staphylococcus aureus showed an upward trend.
Keywords: Tumor, Pathogen, Resistance, Multidrug-resistant bacteria
肿瘤患者往往免疫力低下,抗御病原能力下降,容易并发感染,例如肺癌患者并发肺部感染[1],结直肠癌、肝癌和胃癌患者并发腹腔感染[2]。已有研究结果显示,不同肿瘤来源分离株的主要菌种存在差异,多重耐药菌的检出率较高,给感染的防控带来严峻挑战,例如:乳腺癌患者术后感染病原菌中金黄色葡萄球菌占比高,耐甲氧西林菌株占6.0%[3];实体瘤患者血液样本分离株以大肠埃希菌和克雷伯菌属为主,多重耐药菌占15.5%[4];血液系统肿瘤患者血液样本分离株中铜绿假单胞菌较多,耐碳青霉烯类菌株占59.3%[5]。了解本地区肿瘤患者的病原菌特征,关注多重耐药菌检出率变化趋势,对于感染防控具有重要临床意义。因此,本研究回顾性分析近五年肿瘤患者样本的病原学培养及菌株体外敏感性结果,监测多重耐药菌的检出率变化,为该类患者并发感染的防控提供参考,整理报道如下。
1. 资料与方法
1.1. 对象
纳入四川大学华西医院2019年1月−2023年12月期间送检样本进行病原学培养且临床诊断感染性疾病的肿瘤患者6428例。本研究获四川大学华西医院生物医学伦理审查委员会批准(2023年审1461号)。
1.2. 菌种分布及体外药物敏感性
从实验室信息系统回顾性收集患者样本(尿液、血液、分泌物、呼吸道样本及其他体液等)中病原菌分离情况以及主要菌种的体外药物敏感性检测结果,药敏结果判定参照CLSI M100文件 [6]和专家共识[7]。多重耐药菌定义为对3类或3类以上抗菌药物同时耐药的细菌[8]。
1.3. 统计学方法
分类变量以频数(n)和百分比(%)表示,采用WHONET5.6分析菌种分布(构成比)以及菌株对抗菌药物的耐药率(R%)和敏感率(S%);采用SPSS20.0软件进行卡方检验或Fisher确切概率法分析组间多个构成比/率的差异或趋势,α=0.05。
2. 结果
2.1. 菌株检出率
2019年1月−2023年12月,从80386份样本中分离到16393株菌,检出率为20.4%;各年度送检样本的病原菌检出率依次为20.4%(2819/13843)、19.5%(2695/13818)、20.9%(3454/16540)、25.6%(4406/17210)和15.9%(3019/18975),差异有统计学意义(χ2=531.625, P<0.01)。
2.2. 菌种分布和来源
剔除从同一患者分离的重复菌株,合计分离到细菌7951株(81.1%)和真菌1857株(18.9%),各年度的主要菌种分布差异有统计学意义(χ2=132.758, P<0.01),见表1。细菌菌株以大肠埃希菌(14.5%)、肺炎克雷伯菌(13.2%)、金黄色葡萄球菌(9.4%)、鲍曼不动杆菌复合群(9.3%)和铜绿假单胞菌(7.7%)为主;真菌菌株以白色念珠菌(56.5%)、热带念珠菌(9.0%)和近平滑念珠菌(8.0%)常见。
表 1. The distribution of prevalent species of the strains isolated from tumor patients in 2019 to 2023.
2019−2023年肿瘤患者分离菌株的主要菌种分布
| Organisms | 2019 (n=1652) | 2020 (n=1544) | 2021 (n=2028) | 2022 (n=2614) | 2023 (n=1970) | Total (n=9808) | |||||||||||
| Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | ||||||
| Bacteria | 1277 | 77.3 | 1255 | 81.3 | 1605 | 79.1 | 2102 | 80.4 | 1712 | 86.9 | 7951 | 81.1 | |||||
| Escherichia coli | 211 | 16.5 | 198 | 15.8 | 236 | 14.7 | 271 | 12.9 | 236 | 13.8 | 1152 | 14.5 | |||||
| Klebsiella pneumoniae | 177 | 13.9 | 152 | 12.1 | 201 | 12.5 | 288 | 13.7 | 232 | 13.6 | 1050 | 13.2 | |||||
| Staphylococcus aureus | 125 | 9.8 | 109 | 8.7 | 153 | 9.5 | 196 | 9.3 | 166 | 9.7 | 749 | 9.4 | |||||
| Acinetobacter baumannii complex | 89 | 7.0 | 110 | 8.8 | 158 | 9.8 | 193 | 9.2 | 189 | 11.0 | 739 | 9.3 | |||||
| Pseudomonas aeruginosa | 106 | 8.3 | 103 | 8.2 | 111 | 6.9 | 144 | 6.9 | 148 | 8.6 | 612 | 7.7 | |||||
| Enterobacter cloacae complex | 59 | 4.6 | 56 | 4.5 | 77 | 4.8 | 94 | 4.5 | 77 | 4.5 | 363 | 4.6 | |||||
| Enterococcus faecium | 46 | 3.6 | 39 | 3.1 | 53 | 3.3 | 77 | 3.7 | 63 | 3.7 | 278 | 3.5 | |||||
| Staphylococcus epidermidis | 36 | 2.8 | 38 | 3.0 | 59 | 3.7 | 74 | 3.5 | 49 | 2.9 | 256 | 3.2 | |||||
| Hemophilus influenzae | 57 | 4.5 | 30 | 2.4 | 54 | 3.4 | 64 | 3.0 | 40 | 2.3 | 245 | 3.1 | |||||
| Enterococcus faecalis | 31 | 2.4 | 31 | 2.5 | 34 | 2.1 | 79 | 3.8 | 68 | 4.0 | 243 | 3.1 | |||||
| Fungi | 375 | 22.7 | 289 | 18.7 | 423 | 20.9 | 512 | 19.6 | 258 | 13.1 | 1857 | 18.9 | |||||
| Candida albicans | 194 | 51.7 | 171 | 59.2 | 256 | 60.5 | 289 | 56.4 | 140 | 54.3 | 1050 | 56.5 | |||||
| Candida tropicalis | 35 | 9.3 | 32 | 11.1 | 28 | 6.6 | 51 | 10.0 | 21 | 8.1 | 167 | 9.0 | |||||
| Candida parapsilosis | 28 | 7.5 | 27 | 9.3 | 42 | 9.9 | 36 | 7.0 | 16 | 6.2 | 149 | 8.0 | |||||
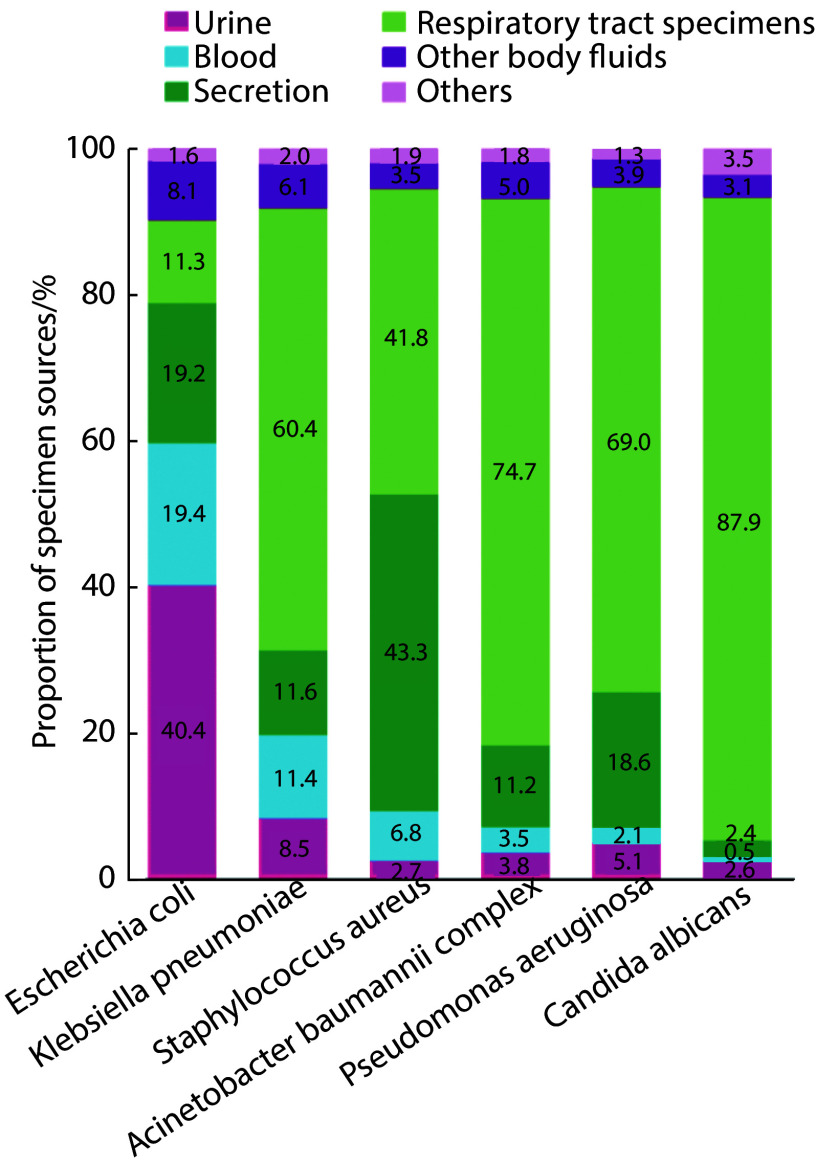
如图1所示,主要菌种的样本来源不同,差异有统计学意义(χ2=2507.564,P<0.001)。不同肿瘤来源分离菌株的菌种分布不同,差异有统计学意义(χ2=1851.041, P<0.01),具体见表2。
图 1.
Specimen sources of the prevalent species isolated from tumor patients in 2019 to 2023
2019−2023年肿瘤患者主要分离菌种的样本来源
χ2=2507.564, P<0.001. Others: other types of specimens.
表 2. Species distribution of the strains isolated from specimens of different types of tumors in 2019 to 2023.
2019−2023年不同肿瘤来源分离菌株的菌种分布
| Organisms | Lung cancer (n=1806) |
Colorectal cancer (n=1073) |
Liver cancer (n=1071) |
Esophageal cancer (n=924) |
Urinary system cancer (n=873) |
Gastric cancer (n=735) |
Oral cancer (n=546) |
Breast cancer (n=467) |
Pancreatic cancer (n=411) |
Nasopharyngeal cancer (n=307) |
||||||||||||||||||
| Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | Types of isolates |
% | |||||||||
| Escherichia coli | 262 | 14.5 | 147 | 13.7 | 136 | 12.7 | 149 | 16.1 | 112 | 12.8 | 86 | 11.7 | 55 | 10.1 | 23 | 4.9 | 57 | 13.9 | 34 | 11.1 | ||||||||
|
Klebsiella
pneumoniae |
206 | 11.4 | 150 | 14.0 | 160 | 14.9 | 112 | 12.1 | 107 | 12.3 | 76 | 10.3 | 49 | 9.0 | 13 | 2.8 | 52 | 12.7 | 28 | 9.1 | ||||||||
| Candida albicans | 178 | 9.9 | 72 | 6.7 | 105 | 9.8 | 98 | 10.6 | 99 | 11.3 | 48 | 6.5 | 166 | 30.4 | 32 | 6.9 | 24 | 5.8 | 24 | 7.8 | ||||||||
|
Enterobacter
cloacae
complex |
154 | 8.5 | 34 | 3.2 | 41 | 3.8 | 40 | 4.3 | 17 | 1.9 | 18 | 2.4 | 3 | 0.5 | 7 | 1.5 | 17 | 4.1 | 15 | 4.9 | ||||||||
|
Staphylococcus
aureus |
122 | 6.8 | 90 | 8.4 | 68 | 6.3 | 67 | 7.3 | 55 | 6.3 | 46 | 6.3 | 35 | 6.4 | 111 | 23.8 | 28 | 6.8 | 64 | 20.8 | ||||||||
|
Pseudomonas
aeruginosa |
117 | 6.5 | 76 | 7.1 | 81 | 7.6 | 90 | 9.7 | 52 | 6.0 | 46 | 6.3 | 26 | 4.8 | 15 | 3.2 | 31 | 7.5 | 16 | 5.2 | ||||||||
|
Stenotrophomonas maltophilia |
50 | 2.8 | 22 | 2.1 | 20 | 1.9 | 45 | 4.9 | 15 | 1.7 | 14 | 1.9 | 31 | 5.7 | 5 | 1.1 | 7 | 1.7 | 9 | 2.9 | ||||||||
|
Enterococcus faecium |
29 | 1.6 | 64 | 6.0 | 36 | 3.4 | 11 | 1.2 | 51 | 5.8 | 16 | 2.2 | 6 | 1.1 | 4 | 0.9 | 25 | 6.1 | 2 | 0.7 | ||||||||
|
Staphylococcus
epidermidis |
24 | 1.3 | 26 | 2.4 | 40 | 3.7 | 15 | 1.6 | 24 | 2.7 | 13 | 1.8 | 14 | 2.6 | 50 | 10.7 | 10 | 2.4 | 9 | 2.9 | ||||||||
|
Acinetobacter
baumannii complex |
4 | 0.2 | 5 | 0.5 | 10 | 0.9 | 0 | 0 | 11 | 1.3 | 160 | 21.8 | 35 | 6.4 | 29 | 6.2 | 0 | 0 | 4 | 1.3 | ||||||||
2.3. 主要菌种对抗菌药物的体外敏感性
2.3.1. 大肠埃希菌
分离到的1152株大肠埃希菌中产超广谱β内酰胺酶(extended-spectrum β-lactamases, ESBL)菌株占50.1%,耐碳青霉烯菌株占2.5%。各年度分离菌株对头孢唑林、头孢吡肟、头孢哌酮-舒巴坦、氨苄西林-舒巴坦、环丙沙星和左氧氟沙星的耐药率差异有统计学意义(P<0.05), 具体见表3。
表 3. Resistance and susceptibility rates of 1152 Escherichia coli isolates to antimicrobial agents in 2019 to 2023.
2019−2023年1152株大肠埃希菌对抗菌药物的耐药率和敏感率
| Antimicrobial agents | 2019 | 2020 | 2021 | 2022 | 2023 | χ2/P | |||||||||
| R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | ||||||
| R: resistant; S: susceptible. | |||||||||||||||
| Amikacin | 2.5 | 97.5 | 1.6 | 98.4 | 3.4 | 96.6 | 2.2 | 97.8 | 0.9 | 99.1 | 3.454/0.485 | ||||
| Gentamicin | 34.5 | 63.5 | 42.9 | 56.6 | 32.9 | 66.7 | 29.8 | 69.8 | 34.7 | 65.3 | 15.144/0.056 | ||||
| Imipenem | 2.5 | 97.5 | 2.2 | 97.8 | 3.4 | 96.6 | 2.2 | 97.8 | 1.4 | 98.6 | 1.951/0.745 | ||||
| Meropenem | 2.5 | 97.5 | 2.2 | 97.8 | 3.4 | 96.6 | 2.2 | 97.3 | 1.4 | 98.6 | 5.466/0.707 | ||||
| Ertapenem | 2.5 | 97.5 | 2.2 | 97.8 | 3.9 | 96.1 | 2.7 | 97.3 | 1.4 | 98.6 | 2.703/0.609 | ||||
| Cefazolin | 55.5 | 44.5 | 57.1 | 42.9 | 54.5 | 45.5 | 61.6 | 38.4 | 79.1 | 20.9 | 30.984/0.000 | ||||
| Cefuroxime | 55.0 | 40.0 | 57.5 | 38.7 | 51.2 | 43.4 | 52.0 | 42.7 | 60.7 | 36.9 | 7.137/0.522 | ||||
| Ceftazidime | 28.5 | 69.0 | 22.1 | 76.8 | 22.7 | 76.3 | 21.8 | 77.3 | 27.6 | 69.7 | 9.133/0.331 | ||||
| Cefotaxime | 51.0 | 47.6 | 55.2 | 43.6 | 51.2 | 48.8 | 49.3 | 49.8 | 57.7 | 41.8 | 6.991/0.538 | ||||
| Cefepime | 27.0 | 71.5 | 26.8 | 72.0 | 26.5 | 72.5 | 28.0 | 70.1 | 33.6 | 63.7 | 15.736/0.046 | ||||
| Piperacillin | 79.0 | 18.0 | 82.3 | 17.7 | 83.4 | 16.1 | 79.9 | 19.2 | 84.4 | 15.1 | 13.154/0.107 | ||||
| Ampicillin | 82.5 | 17.0 | 83.5 | 14.8 | 84.5 | 13.5 | 82.2 | 17.8 | 84.9 | 14.2 | 7.478/0.486 | ||||
| Cefoperazone-Sulbactam | 5.6 | 88.3 | 4.4 | 86.8 | 6.2 | 80.7 | 4.8 | 80.1 | 6.9 | 67.4 | 35.933/0.000 | ||||
| Piperacillin-Tazobactam | 17.7 | 81.8 | 11.2 | 86.6 | 18.4 | 79.6 | 10.8 | 86.5 | 12.5 | 84.0 | 13.108/0.108 | ||||
| Ampicillin-Sulbactam | 57.3 | 42.7 | 47.8 | 52.2 | 48.8 | 51.2 | 42.0 | 57.1 | 45.9 | 51.4 | 25.436/0.001 | ||||
| Ciprofloxacin | 61.5 | 24.5 | 65.4 | 29.1 | 65.2 | 29.5 | 60.4 | 32.4 | 69.2 | 28.0 | 25.100/0.001 | ||||
| Levofloxacin | 56.5 | 17.0 | 64.1 | 16.6 | 58.0 | 30.0 | 54.7 | 36.9 | 63.0 | 32.9 | 76.304/0.000 | ||||
| Trimethoprim-Sulfamethoxazole | 48.7 | 51.3 | 58.8 | 41.2 | 57.0 | 43.0 | 47.3 | 52.7 | 53.2 | 46.8 | 8.119/0.087 | ||||
| Nitrofurantoin | 3.2 | 89.8 | 0 | 91.9 | 0 | 91.7 | 1.1 | 97.7 | 0.8 | 96.1 | 14.505/0.070 | ||||
2.3.2. 肺炎克雷伯菌
分离到的1050株肺炎克雷伯菌中产ESBL菌株占23.4%,耐碳青霉烯菌株占12.3%。各年度分离菌株对头孢唑林、头孢哌酮-舒巴坦和环丙沙星的耐药率差异有统计学意义(P<0.05),具体见表4。
表 4. Resistance and susceptibility rates of 1050 Klebsiella pneumoniae isolates to antimicrobial agents in 2019 to 2023.
2019−2023年1050株肺炎克雷伯菌对抗菌药物的耐药率和敏感率
| Antimicrobial agents | 2019 | 2020 | 2021 | 2022 | 2023 | χ 2 /P | |||||||||
| R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | ||||||
| R: resistant; S: susceptible. | |||||||||||||||
| Amikacin | 6.4 | 93.6 | 8.1 | 91.9 | 12.6 | 87.4 | 8.0 | 92.0 | 12.5 | 87.0 | 10.644/0.223 | ||||
| Gentamicin | 19.8 | 79.1 | 16.2 | 83.8 | 19.7 | 79.2 | 11.9 | 86.4 | 18.5 | 81.5 | 11.857/0.158 | ||||
| Imipenem | 9.9 | 90.1 | 10.8 | 89.2 | 14.2 | 85.8 | 9.2 | 90.8 | 14.9 | 85.1 | 5.140/0.273 | ||||
| Meropenem | 9.9 | 90.1 | 10.8 | 89.2 | 14.2 | 85.8 | 9.2 | 90.8 | 15.4 | 84.6 | 10.011/0.265 | ||||
| Ertapenem | 9.5 | 90.5 | 11.0 | 89.0 | 14.8 | 85.2 | 10.1 | 89.9 | 15.4 | 84.6 | 5.056/0.282 | ||||
| Cefazolin | 90.2 | 9.8 | 29.1 | 70.9 | 31.2 | 68.8 | 43.7 | 56.3 | 81.3 | 18.7 | 118.446/0.000 | ||||
| Cefuroxime | 30.6 | 67.6 | 28.4 | 67.6 | 29.9 | 68.5 | 27.4 | 68.4 | 29.8 | 69.2 | 7.532/0.363 | ||||
| Ceftazidime | 15.1 | 83.1 | 16.2 | 83.1 | 23.1 | 76.9 | 17.4 | 81.7 | 20.1 | 77.5 | 10.800/0.117 | ||||
| Cefotaxime | 22.8 | 74.3 | 23.5 | 75.0 | 27.2 | 72.1 | 21.2 | 78.1 | 25.0 | 72.8 | 4.708/0.788 | ||||
| Cefepime | 22.7 | 76.2 | 19.2 | 80.2 | 23.8 | 74.4 | 19.2 | 79.7 | 21.5 | 77.3 | 2.918/0.939 | ||||
| Piperacillin | 45.0 | 45.0 | 44.6 | 34.5 | 43.5 | 44.0 | 42.6 | 39.7 | 40.7 | 43.1 | 11.561/0.172 | ||||
| Cefoperazone-Sulbactam | 11.2 | 85.3 | 10.6 | 88.2 | 14.7 | 80.0 | 9.4 | 80.6 | 13.6 | 84.0 | 21.691/0.006 | ||||
| Piperacillin-Tazobactam | 18.8 | 74.1 | 16.2 | 79.1 | 23.0 | 73.2 | 17.7 | 77.2 | 20.1 | 78.4 | 10.212/0.250 | ||||
| Ampicillin-Sulbactam | 34.3 | 65.7 | 28.4 | 71.6 | 30.6 | 68.9 | 28.6 | 70.2 | 27.5 | 71.0 | 7.086/0.527 | ||||
| Ciprofloxacin | 25.7 | 62.6 | 25.7 | 69.6 | 29.3 | 68.5 | 23.9 | 72.3 | 28.8 | 68.8 | 25.687/0.001 | ||||
| Levofloxacin | 20.3 | 68.0 | 18.9 | 68.2 | 21.7 | 71.2 | 16.4 | 74.4 | 22.1 | 69.2 | 6.990/0.538 | ||||
| Trimethoprim-Sulfamethoxazole | 19.4 | 80.6 | 15.9 | 84.1 | 25.7 | 74.3 | 19.7 | 80.3 | 23.3 | 76.7 | 5.863/0.210 | ||||
2.3.3. 金黄色葡萄球菌
分离到的749株金黄色葡萄球菌中耐甲氧西林菌株占22.0%,各年度耐甲氧西林菌株的检出率差异有统计学意义(P<0.05),近四年的检出率呈上升趋势,具体见表5。
表 5. Resistance and susceptibility rates of 749 Staphylococcus aureus isolates to antimicrobial agents in 2019 to 2023.
2019−2023年749株金黄色葡萄球菌对抗菌药物的耐药率和敏感率
| Antimicrobial agents | 2019 | 2020 | 2021 | 2022 | 2023 | χ 2 /P | |||||||||
| R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | ||||||
| −: not applicable; R: resistant; S: susceptible. | |||||||||||||||
| Penicillin G | 91.7 | 8.3 | 91.3 | 8.7 | 93.0 | 7.0 | 93.2 | 6.8 | 96.1 | 3.9 | 3.187/0.527 | ||||
| Oxacillin | 21.5 | 78.5 | 17.5 | 82.5 | 20.2 | 79.8 | 24.9 | 75.1 | 32.7 | 67.3 | 10.385/0.034 | ||||
| Gentamicin | 6.6 | 90.1 | 10.7 | 86.4 | 9.4 | 84.4 | 7.3 | 88.1 | 3.8 | 93.6 | 8.811/0.359 | ||||
| Clindamycin | 30.6 | 69.4 | 27.2 | 71.8 | 33.9 | 65.4 | 25.6 | 73.3 | 25.2 | 74.8 | 6.604/0.580 | ||||
| Erythromycin | 52.9 | 45.5 | 48.5 | 49.5 | 53.1 | 46.1 | 52.5 | 45.2 | 43.9 | 56.1 | 8.471/0.389 | ||||
| Vancomycin | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | − | ||||
| Linezolid | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | − | ||||
| Tigecycline | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | − | ||||
| Rifampin | 0 | 100 | 0 | 100 | 0 | 99.2 | 0 | 98.9 | 0.6 | 99.4 | 7.348/0.500 | ||||
| Levofloxacin | 11.6 | 88.4 | 10.7 | 88.3 | 20.2 | 78.3 | 12.4 | 87.6 | 16.7 | 82.7 | 11.020/0.201 | ||||
| Trimethoprim-Sulfamethoxazole | 10.7 | 89.3 | 15.5 | 84.5 | 16.3 | 83.7 | 16.3 | 83.7 | 12.2 | 87.8 | 2.943/0.567 | ||||
2.3.4. 鲍曼不动杆菌复合群
分离到的739株鲍曼不动杆菌复合群中耐碳青霉烯菌株占40.3%。各年度分离菌株对阿米卡星、头孢吡肟、哌拉西林、头孢哌酮-舒巴坦和替加环素的耐药率差异有统计学意义(P<0.05),具体见表6。
表 6. Resistance and susceptibility rates of 739 Acinetobacter baumannii complex isolates to antimicrobial agents in 2019 to 2023.
2019−2023年739株鲍曼不动杆菌复合群对抗菌药物的耐药率和敏感率
| Antimicrobial agents | 2019 | 2020 | 2021 | 2022 | 2023 | χ 2 /P | |||||||||
| R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | ||||||
| R: resistant; S: susceptible. | |||||||||||||||
| Amikacin | 34.5 | 61.9 | 38.1 | 61.9 | 37.7 | 62.3 | 32.5 | 67.5 | 34.7 | 65.3 | 22.287/0.004 | ||||
| Gentamicin | 39.3 | 60.7 | 41.5 | 58.5 | 43.5 | 55.8 | 33.1 | 66.9 | 37.3 | 62.7 | 8.037/0.430 | ||||
| Imipenem | 41.2 | 58.8 | 43.4 | 56.6 | 43.5 | 55.8 | 36.1 | 63.9 | 38.5 | 61.5 | 6.486/0.593 | ||||
| Meropenem | 41.2 | 58.8 | 43.4 | 56.6 | 43.9 | 56.1 | 36.1 | 63.9 | 38.5 | 61.5 | 2.662/0.616 | ||||
| Ceftazidime | 40.5 | 53.6 | 41.5 | 50.0 | 42.8 | 50.7 | 36.7 | 60.9 | 38.7 | 58.9 | 11.748/0.163 | ||||
| Cefepime | 42.4 | 57.6 | 44.3 | 54.7 | 44.2 | 52.9 | 36.7 | 63.3 | 37.9 | 62.1 | 15.589/0.049 | ||||
| Piperacillin | 41.2 | 56.5 | 43.4 | 43.4 | 43.2 | 50.4 | 36.7 | 58.6 | 42.0 | 55.6 | 20.796/0.008 | ||||
| Cefoperazone-Sulbactam | 11.6 | 48.7 | 21.7 | 50.0 | 25.2 | 57.0 | 28.6 | 61.3 | 39.2 | 59.6 | 92.788/0.000 | ||||
| Piperacillin-Tazobactam | 41.2 | 57.6 | 46.2 | 51.0 | 45.2 | 51.1 | 38.1 | 58.9 | 44.0 | 56.0 | 9.031/0.340 | ||||
| Ampicillin-Sulbactam | 42.4 | 54.1 | 48.1 | 48.1 | 45.9 | 50.4 | 40.5 | 52.4 | 44.8 | 51.6 | 6.380/0.605 | ||||
| Ciprofloxacin | 42.4 | 57.6 | 43.4 | 55.7 | 43.5 | 55.8 | 36.7 | 63.3 | 39.5 | 59.9 | 4.282/0.831 | ||||
| Levofloxacin | 41.2 | 57.6 | 44.3 | 55.7 | 43.5 | 55.8 | 35.7 | 63.7 | 37.9 | 61.5 | 4.300/0.829 | ||||
| Minocycline | 18.9 | 56.6 | 20.0 | 51.4 | 19.0 | 42.9 | 9.0 | 51.7 | 16.1 | 43.7 | 9.705/0.286 | ||||
| Trimethoprim-Sulfamethoxazole | 28.2 | 71.8 | 33.7 | 66.3 | 29.1 | 70.9 | 27.5 | 72.5 | 28.1 | 71.9 | 1.253/0.869 | ||||
| Polymyxin B | 0 | 100 | 1.5 | 88.5 | 0 | 100 | 0 | 100 | 0 | 100 | 3.614/0.461 | ||||
| Tigecycline | 1.2 | 91.8 | 1.9 | 95.2 | 1.4 | 97.1 | 0.6 | 98.8 | 0 | 99.4 | 19.194/0.014 | ||||
2.3.5. 铜绿假单胞菌
分离到的612株铜绿假单胞菌中耐碳青霉烯菌株占8.8%。各年度分离菌株对头孢他啶、头孢吡肟和多粘菌素B的耐药率差异有统计学意义(P<0.05),具体见表7。
表 7. Resistance and susceptibility rates of 612 Pseudomonas aeruginosa isolates to antimicrobial agents in 2019 to 2023.
2019−2023年612株铜绿假单胞菌对抗菌药物的耐药率和敏感率
| Antimicrobial agents | 2019 | 2020 | 2021 | 2022 | 2023 | χ 2 /P | |||||||||
| R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | R/% | S/% | ||||||
| R: resistant; S: susceptible. | |||||||||||||||
| Amikacin | 1.0 | 98.0 | 1.1 | 98.9 | 1.1 | 97.8 | 0 | 100 | 0.8 | 99.2 | 4.754/0.784 | ||||
| Gentamicin | 1.0 | 98.0 | 1.1 | 96.7 | 1.1 | 96.7 | 0 | 98.3 | 0.8 | 98.4 | 2.410/0.966 | ||||
| Imipenem | 7.8 | 90.2 | 7.7 | 91.2 | 10.0 | 88.9 | 11.0 | 87.3 | 7.6 | 92.4 | 3.497/0.899 | ||||
| Meropenem | 7.0 | 89.0 | 3.2 | 93.5 | 8.9 | 91.1 | 9.3 | 87.3 | 7.0 | 93.0 | 10.905/0.207 | ||||
| Ceftazidime | 11.9 | 80.2 | 4.4 | 94.4 | 11.0 | 87.9 | 8.5 | 89.8 | 6.7 | 91.7 | 18.407/0.018 | ||||
| Cefepime | 12.9 | 87.1 | 7.6 | 89.1 | 12.1 | 79.1 | 8.5 | 89.8 | 7.3 | 90.2 | 17.675/0.024 | ||||
| Piperacillin | 13.9 | 80.2 | 12.1 | 82.4 | 15.4 | 79.1 | 14.4 | 79.7 | 9.8 | 88.6 | 5.928/0.655 | ||||
| Cefoperazone-Sulbactam | 14.9 | 70.3 | 15.2 | 73.9 | 13.3 | 75.6 | 13.4 | 71.4 | 11.6 | 67.9 | 5.425/0.711 | ||||
| Piperacillin-Tazobactam | 5.1 | 88.9 | 8.8 | 87.9 | 10.0 | 85.6 | 10.3 | 87.1 | 8.8 | 91.2 | 9.110/0.333 | ||||
| Ciprofloxacin | 8.0 | 89.0 | 7.6 | 88.0 | 8.8 | 87.9 | 5.9 | 88.1 | 1.7 | 90.8 | 9.039/0.339 | ||||
| Levofloxacin | 13.1 | 81.8 | 11.2 | 83.1 | 13.2 | 80.2 | 16.7 | 78.9 | 13.8 | 81.3 | 1.828/0.986 | ||||
| Polymyxin B | 0 | 100 | 0 | 100 | 0 | 100 | 0 | 100 | 14.3 | 85.7 | 18.422/0.001 | ||||
2.4. 多重耐药菌的检出情况
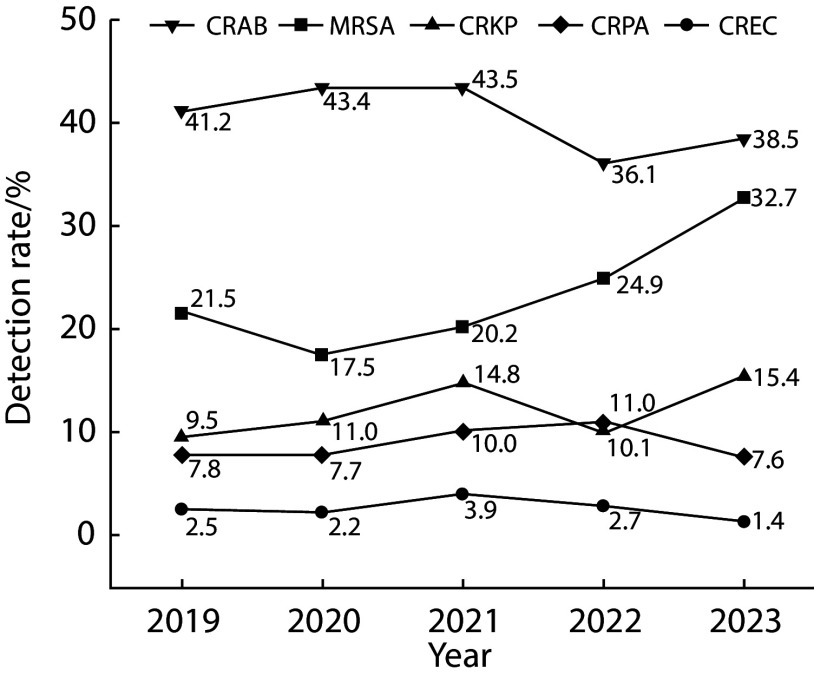
5种主要细菌菌株中耐甲氧西林金黄色葡萄球菌(methicillin-resistant Staphylococcus aureus, MRSA)、耐碳青霉烯大肠埃希菌(carbapenem-resistant Escherichia coli, CREC)、耐碳青霉烯肺炎克雷伯菌(carbapenem-resistant Klebsiella pneumoniae, CRKP)、耐碳青霉烯鲍曼不动杆菌(carbapenem-resistant Acinetobacter baumannii, CRAB)和耐碳青霉烯铜绿假单胞菌(carbapenem-resistant Pseudomonas aeruginosa, CRPA)的总检出率依次为22.0%(165/749)、2.5%(29/1152)、12.3%(129/1050)、40.3%(298/739)和8.8%(54/612),这些多重耐药菌的年度检出率变化如图2所示,MRSA的检出率差异有统计学意义(P=0.034),近四年的检出率呈上升趋势;CREC、CRKP、CRAB和CRPA的检出率差异无统计学意义。
图 2.
Detection rates of multidrug-resistant bacteria isolated from the specimens of tumor patients in 2019 to 2023
2019−2023年肿瘤患者样本中多重耐药菌的检出率
CRAB: carbapenem-resistant Acinetobacter baumannii (χ2=2.613, P=0.625); MRSA: methicillin-resistant Staphylococcus aureus (χ2=10.385, P=0.034); CRKP: carbapenem-resistant Klebsiella pneumoniae (χ2=5.056, P=0.282); CRPA: carbapenem-resistant Pseudomonas aeruginosa (χ2=1.467, P=0.832); CREC: carbapenem-resistant Escherichia coli (χ2=2.703, P=0.609).
3. 讨论
细菌耐药性监测结果是感染性疾病防控的重要依据。世界卫生组织发布的最新报告指出:全球细菌分离株的耐药性增加,各国家及地区应长期开展耐药性监测工作,提供高质量数据用于制定干预措施[9]。研究显示,不同地域及患者人群的主要检出菌种及耐药性存在差异[10-11]。肿瘤患者往往免疫力低下,对病原的抵抗力下降,并发感染的风险高。因此,本研究回顾性分析我院近五年肿瘤患者病原菌特征,关注多重耐药菌检出趋势,为该类患者并发感染的防控提供依据。
本研究纳入2019年1月−2023年12月期间我院收治的6428例肿瘤患者80386份样本中分离的病原菌16393株(检出率为20.4%);剔除同一患者的重复菌株后进一步分析发现:细菌菌株以大肠埃希菌(14.5%)、肺炎克雷伯菌(13.2%)、金黄色葡萄球菌(9.4%)、鲍曼不动杆菌复合群(9.3%)和铜绿假单胞菌(7.7%)为主;真菌菌株以白色念珠菌(56.5%)、热带念珠菌(9.0%)和近平滑念珠菌(8.0%)为主。2020年10月−2021年9月全国肿瘤患者样本分离菌株以大肠埃希菌(22.8%)、肺炎克雷伯菌(16.2%)和金黄色葡萄球菌(9.2%)为主[12]。提示肿瘤人群病原菌特征可能与地区流行病学、人群分布和疾病严重程度等相关,有待进一步研究证实。
本研究纳入的肿瘤患者主要分离菌种的样本来源存在差异,例如:大肠埃希菌主要分离于尿液(40.4%)、血液(19.4%)和分泌物(19.2%),肺炎克雷伯菌主要分离于呼吸道样本(60.4%)、分泌物(11.6%)和血液(11.4%)。2015−2021年中国细菌耐药监测网CHINET监测报告显示:儿童患者样本中大肠埃希菌主要分离自尿液(39.6%)、脓液(21.0%)和呼吸道样本(19.2%),克雷伯菌属细菌主要分离自呼吸道样本(50.1%)、尿液(23.2%)和血液(10.5%)[13]。提示肿瘤患者与非肿瘤患者的主要分离菌种可能相同,但分离来源存在差异,可能与人群的疾病特征相关。
并且,本研究发现不同肿瘤患者样本分离株的主要菌种分布不同,肺癌、食管癌、泌尿系统肿瘤和胰腺癌分离菌株中大肠埃希菌占比高,结直肠癌和肝癌分离菌株中肺炎克雷伯菌最多,乳腺癌和鼻咽癌分离菌株中金黄色葡萄球菌最常见,提示可进一步研究不同肿瘤人群主要病原的感染危险因素、制定策略、评估感染防控干预效果等。
多重耐药菌引起的感染可能导致患者住院时间延长、治疗成本增加和死亡率增高等,是世界关注的公共卫生问题。本研究关注了从纳入肿瘤患者分离的5种常见菌种中多重耐药菌的检出率变化趋势,结果显示:近五年,MRSA、CREC、CRKP、CRAB和CRPA的总检出率依次为22.0%(165/749)、2.5%(29/1152)、12.3%(129/1050)、40.3%(298/739)和8.8%(54/612),CREC、CRKP、CRAB和CRPA各年度检出率差异无统计学意义,但特别值得关注的是MRSA的检出率近四年从17.5%快速上升到32.7%。2014–2019年全国细菌耐药监测网报告显示:MRSA检出率从36.0%下降至30.2%;CREC检出率为1.4%~1.9%;CRKP检出率从6.4%上升至10.9%;CRAB检出率从57.0%下降至56.0%;CRPA检出率从25.6%下降至19.1%[14]。针对目标病原菌,可实施手卫生、接触隔离和合理选用抗菌药物等[15]进行预防干预,针对分离菌株进行遗传学分析可利于干预措施的精准实施和调整[16]。
综上所述,肿瘤患者病原菌以革兰阴性菌为主,主要菌种的样本来源不同,不同肿瘤来源的主要分离菌种也存在差异;多重耐药菌株的检出率较高,耐甲氧西林金黄色葡萄球菌的检出率呈上升趋势。
* * *
作者贡献声明 唐秋萍负责正式分析和初稿写作,王远芳、袁余、舒玲和邓劲负责调查研究和数据审编,何超负责研究项目管理、论文构思和审读与编辑写作。所有作者已经同意将文章提交给本刊,且对将要发表的版本进行最终定稿,并同意对工作的所有方面负责。
Author Contribution TANG Qiuping is responsible for formal analysis and writing--original draft. WANG Yuanfang, YUAN Yu, SHU Ling, and DENG Jin are responsible for investigation and data curation. HE Chao is responsible for project administration, conceptualization, and writing--review and editing. All authors consented to the submission of the article to the Journal. All authors approved the final version to be published and agreed to take responsibility for all aspects of the work.
利益冲突 所有作者均声明不存在利益冲突
Declaration of Conflicting Interests All authors declare no competing interests.
Funding Statement
四川省科学技术厅重点项目 (No. 2024YFFK0225)资助
Contributor Information
秋萍 唐 (Qiuping TANG), Email: tangqiuping@stu.scu.edu.cn.
超 何 (Chao HE), Email: hc_wsw@126.com.
References
- 1.BERTAGLIA V, MORELLI A M, SOLINAS C, et al Infections in lung cancer patients undergoing immunotherapy and targeted therapy: An overview on the current scenario. Crit Rev Oncol Hematol. 2023;184:103954. doi: 10.1016/j.critrevonc.2023.103954. [DOI] [PubMed] [Google Scholar]
- 2.CAI X, YAN H, ZHANG W, et al Intra-abdominal infection after tumor surgery: tigecycline combined with β-lactam antibiotics versus tigecycline alone. BMC Cancer. 2023;23:682. doi: 10.1186/s12885-023-11169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'CONNOR R, KIELY P A, DUNNE C P The relationship between post-surgery infection and breast cancer recurrence. J Hosp Infect. 2020;106(3):522–535. doi: 10.1016/j.jhin.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 4.RABAYAH R, ALSAYED R B, TAHA A A, et al Microbial spectrum and drug resistance profile in solid malignancies in a large tertiary hospital from Palestine. BMC Infect Dis. 2022;22(1):385. doi: 10.1186/s12879-022-07375-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ARMAN G, ZEYAD M, QINDAH B, et al Frequency of microbial isolates and pattern of antimicrobial resistance in patients with hematological malignancies: a cross-sectional study from Palestine. BMC Infect Dis. 2022;22(1):146. doi: 10.1186/s12879-022-07114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 34th ed. CLSI supplement M100. Clinical and Laboratory Standards Institute, 2024.
- 7.中国医疗保健国际交流促进会临床微生物与感染分会, 中华医学会检验医学分会临床微生物学组, 中华医学会微生物学与免疫学分会临床微生物学组 多黏菌素类与替加环素及头孢他啶/阿维巴坦药敏方法和报告专家共识. 中华检验医学杂志. 2020;43(10):964–972. doi: 10.3760/cma.j.cn114452-20200719-00619. [DOI] [Google Scholar]; Society of Clinical Microbiology and Infection of China International Exchange and Promotion Association for Medical and Healthcare, Clinical Microbiology Group of the Laboratory Medicine Society of the Chinese Medical Association, Clinical Microbiology Group of the Microbiology and Immunology Society of the Chinese Medical Association Expert consensus on polymyxins, tigecycline and ceftazidime/avibactam susceptibility testing. Chin J Lab Med. 2020;43(10):964–972. doi: 10.3760/cma.j.cn114452-20200719-00619. [DOI] [Google Scholar]
- 8.CDC. Multidrug-resistant Organisms (MDRO) Management Guidelines. Centers for Disease Control and Prevention, 2024.
- 9.BERTAGNOLIO S, DOBREVA Z, CENTNER C M, et al. WHO global research priorities for antimicrobial resistance in human health. Lancet Microbe, 2024, 100902.
- 10.Van LETH F, SCHULTSZ C Unbiased antimicrobial resistance prevalence estimates through population-based surveillance. Clin Microbiol Infect. 2023;29:429–433. doi: 10.1016/j.cmi.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 11.IKHIMIUKOR O O, ODIH E E, DONADO-GODOY P, et al A bottom-up view of antimicrobial resistance transmission in developing countries. Nat Microbiol. 2022;7:757–765. doi: 10.1038/s41564-022-01124-w. [DOI] [PubMed] [Google Scholar]
- 12.全国细菌耐药监测网 2021年肿瘤科患者分离细菌耐药监测报告. 中国感染控制杂志. 2023;22(10):1159–1167. doi: 10.12138/j.issn.1671-9638.20233802. [DOI] [Google Scholar]; China Antimicrobial Resistance Surveillance System Antimicrobial resistance of bacteria isolated from patients in department of oncology: surveillance report from China Antimicrobial Resistance Surveillance System, 2021. Chin J Infect Control. 2023;22(10):1159–1167. doi: 10.12138/j.issn.1671-9638.20233802. [DOI] [Google Scholar]
- 13.潘芬, 王春, 张泓, 等 2015~2021年CHINET儿童患者分离的肠杆菌目细菌耐药性变迁. 中国感染与化疗杂志. 2024;24(1):53–63. doi: 10.16718/j.1009-7708.2024.01.008. [DOI] [Google Scholar]; PAN F, WANG C, ZHANG H, et al Changing antibiotic resistance profiles of Enterobacterales strains isolated from children: data from CHINET Antimicrobial Resistance Surveillance Program, 2015-2021. Chin J Infect Chemother. 2024;24(1):53–63. doi: 10.16718/j.1009-7708.2024.01.008. [DOI] [Google Scholar]
- 14.全国细菌耐药监测网. 2014~2019年细菌耐药性监测报告. 中国感染控制杂志, 2021, 20(1): 15-31.; China Antimicrobial Resistance Surveillance System. Antimicrobial resistance of bacteria: surveillance report from China Antimicrobial Resistance Surveillance System in 2014-2019. Chin J Infect Control, 2021, 20(1): 15-31.
- 15.MILLS J P, MARCHAIM D Multidrug-resistant gram-negative bacteria: infection prevention and control update. Infect Dis Clin North Am. 2021;35(4):969–994. doi: 10.1016/j.idc.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 16.JAUNEIKAITE E, BAKER K S, NUNN J G, et al Genomics for antimicrobial resistance surveillance to support infection prevention and control in health-care facilities. Lancet Microbe. 2023;4:e1040–e1046. doi: 10.1016/s2666-5247(23)00282-3. [DOI] [PubMed] [Google Scholar]