Abstract
Introduction: Lifestyle is the root cause of most chronic disease, disability, and death. Lifestyle Medicine (LM) is an established, board certifiable field of medicine. Physical Medicine and Rehabilitation (PM&R) is a multidisciplinary field which focuses on function and quality of life. The symbiosis of PM&R and LM is increasingly being recognized. Objective: To gauge the awareness of, use of, and interest in LM of PM&R residents and ask if they think PM&R physicians should be leaders in LM. Methods: Cross sectional survey of PM&R residents across PM&R programs in the USA. Results: Fifty-three percent of PM&R residents were familiar with LM. 85 and 84% of their medical schools and residencies had no LM education. PM&R residents “sometimes” included LM principles in their patient encounters. 88 and 89% of PM&R residents thought that medical schools and residencies should have LM education and 78% thought that PM&R physicians should be leaders of LM. Conclusions: This is the first study assessing the views on LM of PM&R residents. Despite the fact that PM&R residents lacked LM education, over half knew about LM. The vast majority felt that there should be more LM education in medical school and residency, and that PM&R physicians should be leaders of LM.
Keywords: education, lifestyle medicine, PM&R, exercise, nutrition, function, quality of life
“In theory and the residents agree, PM&R physicians should be leaders in LM.”
Main Document
Lifestyle habits are the root cause of >80% of chronic disease, disability, and premature death. Lifestyle Medicine (LM) is an established, board certifiable field of medicine that focuses on the prevention, treatment, and reversal of chronic disease through the evidence-based lifestyle therapeutic interventions of a healthful whole-food, plant-predominant eating pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection. Founded in 2004, the American College of Lifestyle Medicine (ACLM) is the medical professional society for healthcare providers dedicated to the practice of LM. 1 LM is aligned with, but separate from Preventive Medicine, Integrative Medicine, Complimentary/Alternative Medicine, and Functional Medicine. As unhealthy lifestyle behaviors are at the root of >80% of chronic disease, LM should become the foundation of conventional medicine and a critical component of care for all health professionals managing patients with chronic diseases.
The importance of LM education is increasingly being recognized and is therefore more commonly being taught in medical schools and residencies, both formally and informally. 2 The ACLM now has 9000 members, including over 3200 physicians who have passed the American Board of Lifestyle Medicine (ABLM) since its first exam in 2017. Grass-roots medical student and faculty lead Lifestyle Medicine Interest Groups (LMIGs) are growing in medical schools with over 100 groups across the country, the first at Harvard Medical School, 3 all supported by the ACLM. 4 There are over 200 residency programs that are implementing the Lifestyle Medicine Residency Curriculum (LMRCs) across many different medical specialties (including six PM&R programs) and one established LM fellowship. To be certified in LM, physicians must first achieve a primary board certification. LM is not recognized by the American Board of Medical Specialties (ABMS). 1
The inaugural university department of Physical Medicine and Rehabilitation (PM&R) was founded in 1929, first recognizing the intense deconditioning and functional deterioration seen in bedbound patients. 5 PM&R has since developed into a thriving and multidisciplinary field which focuses on function and quality of life with complex and vulnerable populations.
The symbiosis of PM&R and LM is increasingly being recognized. The Institute of Lifestyle Medicine (ILM) was founded within the Department of PM&R at Harvard Medical School in 2007. The ILM is a leader in advocacy and education, training >25 000 clinicians from around the world through 26 live CME programs and a suite of online modules. 6 The first issue of the PM&R Journal in 2009 published two articles supporting the unique qualifications of physiatrists to address the problems of unhealthy lifestyle habits titled “Action on Obesity and Fitness: The Physiatrists Role” 7 and “Maintaining Health, Wellness, and Fitness: A New Niche for Physiatry.” 8 In 2011, experts in PM&R and LM outlined the steps of coaching for behavior change for physiatrists. 9 The PM&R Journal in 2016 published an emerging issue focused on including nutrition on physiatrists’ tables 10 and in 2020 a narrative review on chronic musculoskeletal pain and nutrition. 11 In 2016 and 2017, the American Congress of Rehabilitation Medicine (ACRM) hosted workshops in LM as part of their annual meetings. Since 2018, the ACRM has included a LM Networking Group and LM presentations have been part of their annual meetings. 12 The American Academy of PM&R (AAPM&R) and the Association of Academic Physiatrists (AAP) conferences have also included an increasing number of LM topics over the years. In 2020, it was proposed that physiatrists, are and have the potential to continue to be leaders in the field of LM. 13
PM&R and LM are two compatible fields of medicine that have similar goals for patients including helping patients to thrive at any age or stage of life. A healthful whole-food, plant-predominant eating pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection will all impact brain recovery. 14 The World Cancer Research Fund and the American Institute for Cancer Research annually report on the role of nutrition, physical activity and cancer and recommend a diet rich in whole grains, vegetables, fruit, and beans and physical activity. 15 The ACLM has concluded that remission should be the clinical goal in type 2 diabetes treatment using properly dosed intensive lifestyle interventions, 16 a concept which would greatly affect all patients with diabetes in the rehabilitation field. As published in the PM&R journal, patients with chronic musculoskeletal pain would benefit from evidence-based nutrition. 11 Finally, most chronic conditions including cardiovascular disease, diabetes, obesity, dementia, metabolic syndrome, and arthritis are associated with inflammation, and a healthy lifestyle lowers inflammation. 17 Overall, patients being seen by a physiatrist can greatly benefit from counseling in the six pillars of LM.
Because lifestyle habits are the root cause and play a role in recovery from many prevalent rehab diagnoses, there is a valuable opportunity to prevent, treat, and reverse chronic illness with LM within the established PM&R interdisciplinary team approach to care. Furthermore, as specialists, PM&R physicians often have time and flexibility to address one or two issues and incorporate LM pillars into the clinic visit vs the traditional primary care model that must often address multiple issues in a short amount of time. Although PM&R and LM appear to be compatible in theory, there is often a gap between theory and the practice of medicine. According to the ACLM, there are approximately 40 board ABLM diplomates/PM&R physicians in the United States, with only 10 of them affiliated with an academic PM&R program. 1
This study seeks to gauge PM&R residents’ awareness, current use, and interest in LM. As the future of PM&R, do the current PM&R residents know about LM? Did they receive any formal/informal training in LM in medical school or residency? As PM&R physicians who focus on function and quality of life, do they already naturally incorporate its principles into their encounters? Are they interested in learning more about LM? Do they think PM&R physicians should be leaders of LM?
Methods
An online survey for PM&R residents obtained feedback on their awareness of LM, their current practice of utilizing LM with their patients, (such as discussing eating a healthful diet, exercising 150 minutes per week, sleeping 7–9 hours of per night or good sleep hygiene, using a healthy form of stress management, avoidance or cessation of risky substances and creating or improving positive social connections) as well as gauging their interest in LM. Lastly, we asked if physiatrists should be leaders in LM.
The survey was created on Qualtrics and was estimated to take less than five minutes to complete the 10–12 questions. This study was deemed exempt from the Institutional Review Board (IRB).
Emails were sent out with the survey link to PM&R coordinators of 96 PM&R programs in the United States on two occasions in September 2021. This list was meant to be a comprehensive list of all PM&R programs in the nation. First the coordinators were instructed to send the survey to their residents. Second, about a week later, the coordinators were reminded again. Our goal was to receive at least 100 responses of the approximately 480 PM&R residents across the 96 programs.
All responses were voluntary, anonymous, and confidential.
Results
One hundred and five residents responded. 6.9% PGY1, 30.4% PGY2, 37.3% PGY3, and 25.5% PGY4. The PM&R residents who responded were 44.1% DO and 55.9% MD.
Just over half of the respondents (53.5%) reported being aware of the field of LM and 46.5% reported being unaware of LM. Eighty-five percent of residents did not have any dedicated LM education at their medical school and 84% reported having no dedicated LM education at their PM&R residency.
Residents responded most frequently that they “sometimes” addressed pillars of LM in their patient encounters. The most common LM pillar that residents included in their patient encounters was the avoidance or cessation of risky substances, followed by exercise and sleep hygiene. The least frequently included pillars of LM were eating a healthful diet and creating or improving positive social connections.
Additionally, eighty-seven percent (87.9%) of residents thought that medical schools should have dedicated LM education, 5.1% thought they should not. Eighty-eight percent (88.8%) of residents thought that PM&R residencies should have dedicated LM education, 4.1% thought they should not.
Most residents reported that they would “probably” sign up for LM education opportunities. The most popular options were for intermittent lunch lectures or intermixed with current lectures.
The vast majority (77.8%) of residents thought PM&R physicians should be leaders of LM while 12.1% thought they should not and 10.1% selected other. All PM&R resident comments are listed in Table 1.
Table 1.
PM&R Resident Comments.
| • YES, this is an area that I have been thinking of pursuing without actually realizing it is already “a thing.” |
| • I think all specialties would benefit, but I think in particular specialties focused on prevention and chronic illness would benefit most. |
| • There is significant cross over and opportunity and physicians trained in function to utilize and prioritize lifestyle medicine in their clinical practice or as their primary specialty. |
| • Perhaps best served by primary care, but definitely high utility for PM&R physicians. |
| • Lifestyle medicine should absolutely be a part of the PM&R physician’s practice, but we should not be the primary leaders in this. That should be the primary care physician’s role. |
| • I feel it is covered well in our curriculum as is, we put heavy emphasis on these modifications of life with our patients. |
| • I think this is very important information to emphasize to patients at each visit. |
| • I have been trying to bring ACLM to [my residency] especially PM&R. |
| • Really appreciate your efforts of incorporating Lifestyle Medicine into Rehab medicine training and practice! |
| • This is super important and should absolutely be a part of our curriculum. |
| • I am very interested in lifestyle medicine and would love a way to connect it into my future practice. |
| • I have great interest in this area and hope to learn how I can incorporate this officially into my future practice. |
| • Would love to learn more about Lifestyle Medicine, unable to do fellowship due to other Fellowship commitments and lunch lectures would interfere with current curriculum, otherwise would be very open to learning more. |
| • I don’t know much about this field, but it seems to dovetail with the goals of Rehab. |
Discussion
LM is a burgeoning area of medicine with ancient wisdom and simple concepts, such as “food is medicine,” and “movement is medicine,” which were words of advice from grandparents and are now evidence-based national guidelines. PM&R focuses on function and quality of life.
Because unhealthy lifestyle habits are the root cause of most chronic disease, it would be beneficial to include LM in the foundation of conventional medicine and create competencies in LM for all health professionals across multiple specialties. Additionally, with the current shift away from the more traditional fee for service models of reimbursement, there may emerge a future direction with more of a public health and a preventive care focus. With this focus, LM will become critical to incorporate into all aspects of medical care. LM education will ideally be incorporated across all medical education, including medical school and residency to complement the existing LM board certification currently available to physicians from all specialties. In addition, there is a specialist track for lifestyle medicine that is in development which will require a fellowship with extensive training and experience in medication deprescribing. According to the results of the study, PM&R residents believe that the specialty of PM&R and the field of LM are compatible.
The field of PM&R has shown increasing interest in LM through history, research, and presentations6-13 and there is significant research now available demonstrating the importance and power of LM, particularly for rehabilitation patients.14-17 Recently, with the COVID pandemic, physiatrists have been stepping forward as leaders of LM, to use LM as a powerful therapy for prevention, control, and even reversal/remission of well-established risk factors for COVID associated morbidity and mortality.18,19 As these risk factors are also the root of many top PM&R diagnoses, there is a clear reason for the overlap of PM&R and LM.
According to our study, over half (53.7%) of PM&R residents were familiar with the field of LM despite the overwhelming lack of LM education in both medical school (85%) and PM&R residency (84%).
The interdisciplinary team physiatric focus on function and quality of life directly benefits by including LM principle into patient encounters including healthful eating, exercising, sleep hygiene, stress reduction, avoiding risky substances, and positive social connection. Despite a lack of LM education in medical school and residency, survey responders most commonly reported that they “sometimes” incorporate LM into their practice, however, more information is needed if we were to compare to other specialties.
Out of the surveyed PM&R residents, 88% thought that medical schools should have dedicated LM education reflecting that all physicians should have access to LM education. Specific for PM&R, 89% thought PM&R residencies should have dedicated LM education. Lastly, 78% thought that PM&R physicians should be leaders of LM. Most comments were positive for the combination of PM&R and LM as seen in Table 1.
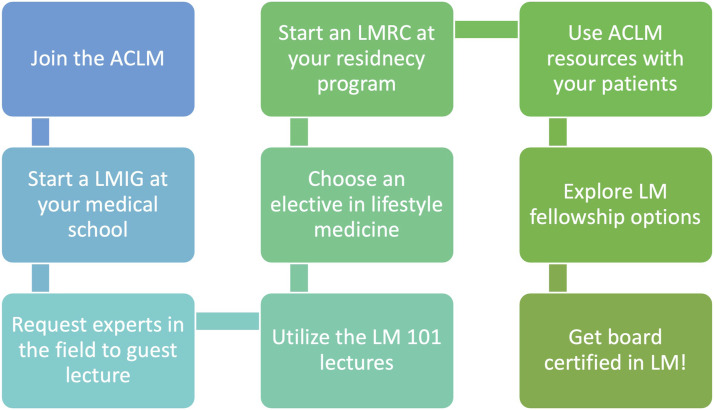
This paper can be a call to action for all health professionals. For those in their training process, they may refer to the steps listed in Figure 1 to incorporate LM education into their training and eventual toolbox. For practicing physicians, LM education is available through ACLM with online CME courses, webinars, as well as patient resources, and LM can be incorporated as single visits, groups visits, hospital consults or included in intensive rehabilitation programs. 1
Figure 1.
Steps to incorporate LM.
From medical school through practicing as a physician there are various ways to get involved with LM. Throughout this journey, the ACLM provides education and resources as well as community and guidance for LM. At medical school, students are encouraged to join the >100 LMIGS to help educate their classmates (and faculty) about LM. Further support can be found in the references 3 and 4. Additionally there are evidence-based, guideline driven, fully vetted resources ready for use such as the LM 101 curriculum PowerPoints and syllabus that accompany the Lifestyle Medicine Handbook co-authored by a physiatrist and co-created by a team at ACLM. Any faculty member or physician in training interested in learning about or teaching LM can download this resource for free from the ACLM website. In residency, there are LM elective opportunities such as Loma Linda University. There is an established LMRC which can be implemented at any interested residency program that is connected to a faculty member with a board certification in LM. As of 2022, there are six PM&R residency programs which incorporate the LMRC. During residency it is encouraged to use ACLM resources for patient education. For a graduating resident or practicing physiatrists, there are options of LM fellowship and board certification.
This paper highlights that PM&R is a unique field of medicine, well equipped for LM with its team focus on function and quality of life while working with complex and vulnerable populations. In theory and the residents agree, PM&R physicians should be leaders in LM. The founder and director of the ILM (EMP, study author) and the current president of the ACLM (EPF, study author) are both faculty of the Harvard PM&R department who have successfully merged the fields of PM&R and LM. Study author EPF has run group lifestyle medicine intervention for stroke patients at Spaulding Rehabilitation Hospital since 2012 and is currently the first PM&R trained physician to serve as president of the ACLM. Continuing this momentum of combining PM&R and LM will serve both patients and providers in both fields of medicine.
Study Limitations
Limitations include the confounding effect of only those interested in LM replying to the surveys. This would potentially inflate the perceived PM&R resident interest in LM.
Conclusion
Despite an overwhelming lack of LM education currently in both medical school and PM&R residency, over half of PM&R resident survey respondents were familiar with LM and the vast majority feels that there should be more dedicated LM education in medical school as well as in PM&R residency. PM&R residents, on average, sometimes naturally include LM principles into their encounters but it is unclear how this compares to other specialties. Both in theory and reported by current PM&R residents, PM&R physicians should be leaders of LM.
Acknowledgments
We would like to acknowledge the support of Dr Jared Placeway, DO, the program director of the Case Western, MetroHealth PM&R Department as well as the critique of Dr Richard Wilson, MD of Case Western, MetroHealth PM&R Department.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Kelsea J. Sandefur https://orcid.org/0000-0002-5382-8456
Elizabeth P. Frates https://orcid.org/0000-0002-1156-7745
References
- 1.American College of Lifestyle Medicine . About. https://www.lifestylemedicine.org/ACLM/About/What_is_Lifestyle_Medicine/ACLM/About/What_is_Lifestyle_Medicine_/Lifestyle_Medicine.aspx?hkey=26f3eb6b-8294-4a63-83de-35d429c3bb88. Published 2021. Accessed December 14, 2022. [Google Scholar]
- 2.Trilk J, Nelson L, Briggs A, Muscato D. Including lifestyle medicine in medical education: Rationale for American college of preventive medicine/American medical association resolution 959. Am J Prev Med. 2019;56(5):e169-e175. [DOI] [PubMed] [Google Scholar]
- 3.Pojednic R, Frates E. A parallel curriculum in lifestyle medicine. Clin Teach. 2017;14(1):27-31. [DOI] [PubMed] [Google Scholar]
- 4.Stiegmann RA, Abreu A, Gardner JE, Hipple JM, Poling PE, Frates EP. Planting the seeds of change: Growing lifestyle medicine interest groups with the Donald A. Pegg award. Am J Lifestyle Med. 2017;11(6):443-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atanelov L, Stiens SA, Young MA. History of physical medicine and rehabilitation and its ethical dimensions. AMA J Ethics. 2015;17(6):568-574. [DOI] [PubMed] [Google Scholar]
- 6.The Institute of Lifestyle Medicine . About. InstituteofLifestyleMedicine.org. Published 2014. Accessed 2022. [Google Scholar]
- 7.Laskowski ER. Action on obesity and fitness: The physiatrist’s role. PM&R. 2009;1(1):795-797. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein SM. Maintaining health, wellness, and fitness: A new niche for physiatry. PM&R. 2009;1(1):793-794. [DOI] [PubMed] [Google Scholar]
- 9.Frates EP, Moore MA, Lopez CN, McMahon GT. Coaching for behavior change in physiatry. Am J Phys Med Rehabil. 2011;90(12):1074-1082. [DOI] [PubMed] [Google Scholar]
- 10.Polak R, Dacey ML, Phillips EM. Time for food – including nutrition on physiatrists’ tables. PMR J. 2016;8(4):388-390. [DOI] [PubMed] [Google Scholar]
- 11.Elma O, Yilmaz ST, Deliens T, et al. Chronic musculoskeletal pain and nutrition: Where are we and where are we heading? PMR J. 2020;12(12):1268-1278. [DOI] [PubMed] [Google Scholar]
- 12.American Congress of Rehabilitation Medicine . Lifestyle Medicine Networking Group. https://acrm.org/acrm-communities/lifestyle-medicine/. Published 2021. Accessed December 14, 2022. [Google Scholar]
- 13.Phillips EM, Frates EP, Park DJ. Lifestyle medicine. Phys Med Rehabil Clin N Am. 2020;31(4):515-526. [DOI] [PubMed] [Google Scholar]
- 14.Driver S, Juengst S, Reynolds M, et al. Healthy lifestyle after traumatic brain injury: A brief narrative. Brain Inj. 2019;33(10):1299-1307. [DOI] [PubMed] [Google Scholar]
- 15.Clinton SK, Giovannucci EL, Hursting SD. The world cancer research fund/American institute for cancer research third expert report on diet, nutrition, physical activity, and cancer: impact and future directions. J Nutr. 2020;150(4):663-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly J, Karlsen M, Steinke G. Type 2 diabetes remission and lifestyle medicine: A position statement from the American college of lifestyle medicine. Am J Lifestyle Med. 2020;14(4):406-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bodai BI, Nakata TE, Wong WT, et al. Lifestyle medicine: A brief review of its dramatic impact on health and survival. Perm J. 2018;22:17-025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frates EP, Rifai T. Making the case for “COVID-19 prophylaxis” with lifestyle medicine. Am J Health Promot. 2020;34(6):689-691. [DOI] [PubMed] [Google Scholar]
- 19.Hart J, Katz DL, Kushner RF, Frates B, Hensrud DD. Roundtable discussion: COVID-19 and obesity-implications and integrative management. Alternative Compl Ther. 2021;27(2):57-63. [Google Scholar]