Abstract
Background:
Physical therapy (PT) has an important role in Integrative Oncology programs, addressing the unique physical health needs of individuals with cancer through exercise counseling. We share our experience with the PT component of our telehealth comprehensive lifestyle modification program including data from our first cohort of patients.
Methods:
The PT component of our lifestyle modification program included 6 one-hour synchronous video sessions (30 minutes exercise education, 30 minutes exercise) over the 12-week program. Participants received handouts electronically that included information regarding each week’s exercise-related topic, as well as weekly exercise assignments. Outcomes included weight, days of aerobic exercise, minutes of aerobic exercise, and days of strengthening exercise. Six patients completed the program and submitted an anonymous exit survey providing qualitative feedback on the program.
Results:
On average, patients reported engaging in aerobic exercise 4 days per week and strength training 2 days per week after the intervention. There were notable increases in days of strength training. Patients lost an average of 4.2% of their body weight over the course of the 12-week program. Qualitative feedback showed that the first cohort of patients described the telehealth program as enjoyable, valuable, and convenient.
Discussion:
Physical therapy exercise programs can be modified and tailored for delivery in a telehealth environment. Increased patient access remains a strength of this model, serving to equip patients with the tools needed for increasing aerobic and strength training activity. Overall, the program was implemented successfully, and the anonymous feedback survey completed after program completion showed high patient satisfaction.
Keywords: physical therapy, telehealth, lifestyle, exercise counseling, patient satisfaction, integrative oncology
Introduction
Cancer can have profound effects on both emotional and physical well-being. While Western biomedical approaches focus on treating cancer as a disease, it is important to also address the patient’s illness experience. 1 The illness experience can be defined as how cancer as a disease affects areas of personal (physical and mental), family, cultural, spiritual, and financial well-being. Cancer centers should focus on addressing both the disease and illness experience to optimize patient quality of life. The Integrative Medicine Center (IMC) at The University of Texas MD Anderson Cancer Center takes a patient-centered, evidence-informed approach based on the biopsychosocial model 2 to encourage mind-body practices and lifestyle modification alongside conventional cancer care and treatment. 3 Interventions include lifestyle modifications such as exercise and diet, non-pharmacologic pain and symptom control through oncology massage and acupuncture, along with mind-body practices and psychological interventions to reduce stress and improve sleep and overall quality of life. The IMC includes clinicians from various fields of medicine: physicians, advance practice providers, health psychologists, physical therapist, acupuncturist, massage therapist, dietician, mind-body specialist, and music therapist.
Physical activity, exercise, and fitness in cancer has an important role. The benefits of exercise during and after cancer treatment are numerous and include increased muscle mass and strength, improved sleep quality, reduction in long-term and late effects of cancer treatment, improved balance and mobility, reduced bone loss from hormonal therapies, radiation, or inactivity, decreases in depression and anxiety, and reduction in cancer recurrence and improvements in overall survival.4 -8 Exercise has the most robust effect on breast cancer outcomes, including risk of recurrence or death, when compared to other lifestyle factors such as weight management, diet, smoking, alcohol intake, or vitamin supplementation.7,9 -13 Additionally, exercise improves chemotherapy completion rates in individuals with breast cancer, contributing to improved outcomes.14,15 While further research is needed, exercise may also enhance the efficacy of various cancer treatments such as chemotherapy, radiation, and immunotherapy through systemic and local responses. 16 Improved immune and metabolic function, reduced inflammation, and improved tumor vascularization and blood flow have all been proposed mechanisms for how exercise may contribute to improved efficacy of cancer treatments. 17 Compared to moderate intensity exercise, vigorous intensity exercise can cause increased inflammation, yet this increase in inflammation is acute and in the long run all forms of exercise are associated with lower levels of inflammation.18 -20 Yet, dose of exercise, such as frequency and intensity, is an important component in developing exercise prescriptions.
As part of the MD Anderson Integrative Medicine Center, a physical therapist addresses the unique physical health needs of individuals with cancer through exercise counseling. The physical therapist with an oncology specialization develops safe, effective, and individually tailored exercise programs. 21 These exercise programs assist patients in improving exercise quantity and quality, while considering factors that may limit exercise such as cancer treatment-related symptoms and side effects such as fatigue, neuropathy, reduced balance, pain, impaired blood counts, nausea, and premorbid musculoskeletal issues.15,22 -24
The American Institute for Cancer Research, the American College of Sports Medicine (ACSM), and the American Cancer Society (ACS) have found exercise during and after cancer treatment to be safe and recommended.25,26 In fact, the ACSM has created a global health initiative called “Exercise is Medicine,” encouraging providers to include physical activity in treatment plans and referring to qualified exercise professionals. 27 With an emphasis on safety and effectiveness, these and other guidelines developed by experts in the field outline specific types, intensity, and frequency of exercise to help with management of cancer-related symptoms.28,29 A key role of the physical therapist in an oncology setting is ensuring appropriate levels of exercise in patients during all stages of their cancer journey.
The physical therapist not only provides individual consultations and follow-ups but is also a key clinician in lifestyle change programs offered in the MD Anderson Integrative Medicine Center. Prior to the COVID-19 pandemic, we developed an intensive multidisciplinary integrative medicine lifestyle modification program, called IM FIT, to help facilitate healthy lifestyle changes in individuals with cancer. IM FIT is a 12-week intensive group lifestyle modification intervention, specifically designed for individuals with cancer, with weekly sessions led by experts in the areas of physical therapy, nutrition, and health psychology. This reimbursable program successfully contributed to weight reduction, improved mental health, and improvements in lifestyle factors such as diet and exercise. 30
IM FIT uses exercise counseling and education as well as prescribed exercise to facilitate recovery from cancer treatment while mitigating cancer treatment related symptoms. Goals of the physical therapy (PT) component of the IM FIT program include: improve functional outcomes, enhance quality of life, improve cardiorespiratory fitness, improve total body strength, reduce fall risk, reduce risk of osteoporosis associated with aging and cancer treatment, and reduce risk of cancer recurrence. ACSM and ACS guidelines are followed, specifically, 150 minutes per week of moderate intensity aerobic exercise or 75 minutes of vigorous intensity aerobic exercise, as well as 2 days per week of muscle strengthening activities of moderate intensity.31,32 The program emphasizes safe and effective exercise while giving the tools needed to implement their own personal exercise program with the goal of meeting guideline recommendations. Physical limitations and various factors that may require exercise modification include fall history, neuropathy, balance deficits, lymphedema, bone health, chemotherapy history, musculoskeletal issues such as arthritis, post-surgical precautions, cognition, and impaired lab values. The PT portion of IM FIT includes education, active exercise participation, and weekly homework prescription.
Exercise is a key strategy in oncology rehabilitation, and disseminating innovative clinical applications continues to be an integral component of advancing the field. During the COVID-19 pandemic, we modified the IM FIT protocol to allow assessments and interventions (including PT) to be delivered through video sessions, thus named IM FIT telehealth. A telehealth IM FIT model increases patient access, reduces infection risk, and reduces travel and scheduling barriers associated with participating in a 12-week in-person program. The current manuscript explores patient feedback and exercise factors to reveal insight into the viability of including telehealth PT as a component of a comprehensive lifestyle program for cancer survivors. Findings from this type of research can help inform next steps in optimizing delivery of telehealth PT to a unique patient population.
Methods
Patients were initially evaluated via telehealth (video) within the IMC by a physician as part of the integrative oncology consultation. The IM FIT telehealth program was introduced to interested and eligible patients who were then referred to the physical therapist, health psychologist, and registered dietician for one-on-one telehealth consultations and further evaluation. Inclusion criteria were: 1) high interest and need for weight loss [body mass index (BMI) ≥25], 2) high interest in transitioning to a plant-based diet (typical plate is filled with at least two-thirds of plant-based foods), 3) high interest in engaging in a regular exercise program. A plant-based diet was recommended based on guidelines from the third World Expert American Institute of Cancer Research report. 33 Due to the added value of healthy eating and exercise to reduce risk of cancer recurrence, we did not exclude normal-weight individuals. 7 Exclusion criteria were severe psychological distress or eating disorders or the inability to exercise at least 3 days per week and engage in resistance training. Patients were asked to commit to the 12-week duration of the program and attend at least 10 out of 12 sessions. Although the program was first created for individuals who completed active cancer treatment, it was adapted to allow patients to be in active treatment due to patient interest. The cohort was capped at 8 patients to ensure that group physical therapy supervision was feasible in the telehealth setting and for addressing limitations associated with third party reimbursement. The duration of recruitment lasted approximately 2 months. Data was collected as part of the University of Texas MD Anderson Cancer Center IRB-approved “Integrative Medicine Center Registry Protocol” (DR11-0149, Rev July 7, 2023).
Intervention
IM FIT telehealth is a 12-week group program consisting of physical therapy, health psychology, and nutrition sessions delivered via hospital-based interactive video. Physical therapy sessions were 60 minutes, every other week, nutrition sessions were 60 minutes, every other week (alternating with physical therapy), and health psychology sessions were 60 minutes, every week. The same physical therapist, dietician, and health psychologist conducted their respective sessions for the entirety of the program. A detailed description of the in-person IM FIT program has been published previously. 30 In contrast to the in-person program, IM FIT telehealth had 6 sessions of PT and nutrition each, rather than 12 sessions each. The telehealth nutrition sessions focused on: benefits of a plant-based diet, understanding sugar, meal planning/smart shopping, healthy snacks on the go/healthy restaurants, flavor up your food, health concerns about dairy. Psychology frequency and content remained the same. Handouts were shared electronically and reviewed together during interactive video via screen sharing. PT sessions are described in detail as follows.
Prior to initiation of the program, patients were encouraged to self-purchase hand weights and resistance bands that would be used for resistance training during the program. Patients were educated on types of equipment and weight size. Patients did not indicate any difficulty with acquiring hand weights and resistance bands, and some patients already had these materials. Yoga was counted as a strength training activity due to a recent meta-analysis on yoga RCTs showing that yoga practice is associated with significant increases in lower limb strength compared to controls. 34 PT sessions generally involved 30 minutes of exercise education followed by 30 minutes of group exercise led by the physical therapist. Participants were provided a PT packet (emailed through the medical records) that included extensive information regarding each week’s exercise-related topic, as well as exercises to be performed and homework assigned each week. See Table 1 for a description of the PT protocol for each session. The physical therapist monitored patients adequately through the group telehealth environment and made any needed suggestions for form correction to ensure appropriate and safe exercise execution. Although PT sessions were every other week, PT homework was completed weekly.
Table 1.
IM FIT Telehealth Physical Therapy Session Overview.
| Physical therapy session/topic | Education | Exercise | Homework |
|---|---|---|---|
| Week 1: Program introduction and introduction to exercise | -Introduction to IM FIT telehealth -Review of exercise equipment options for program -Review of program expectations including attendance policy, weekly homework, exercise related goals, and overall purpose of the program -Exercise topics: benefits of exercise, aerobic versus strengthening exercise, monitoring exercise intensity, muscle anatomy, red flags in exercise, FITT (frequency, intensity, time, and type) principle |
-Exercises demonstrated and reviewed with patient: bicep curls, tricep kickback, chest press, rows, upright row, lateral raise, hamstring curl, mini squat, single leg heel raise, and planks -Exercise logs provided, weekly logging recommended |
-Participate in 3, 20-min sessions of moderate aerobic exercise, achieving RPE of 4 to 6 -Perform the strengthening exercises reviewed, 2 sets of 12 repetitions each at patient determined weight (ability to complete 2 sets of 12 with moderate difficulty), 2x/week -Fill out exercise plan/log |
| Week 2: Essential components of fitness | -Reviewed previous week’s homework -Defined the following components of fitness: cardiorespiratory fitness, muscle strength, muscle endurance, flexibility, body composition, balance and coordination, and agility/speed/power -Differences between exercise and activity; reducing sedentary behavior |
-30 min exercise routine, 15 min of aerobic exercise and 15 min of strengthening exercise -Exercises demonstrated: bicep curls with band, tricep pull down with band, wall push ups, seated rows with band, overhead press with dumbbells, shoulder blade squeeze with band, bridging, clam shells with and without band, side lying hip abduction, and side plank with bent knee |
-Participate in 3 to 4, 25 to 30 min sessions of moderate aerobic exercise -Perform the strengthening exercises reviewed, 2 sets of 12 repetitions each at patient determined weight (ability to complete 2 sets of 12 with moderate difficulty), 2x/week -Fill out exercise plan/log |
| Week 3: Safe approach to exercise | -Reviewed previous week’s homework -Reviewed safe exercise: physiological warm-up, cool down, when to stop exercising, and stretching -Various stretches for major muscle groups reviewed |
-30 min strengthening routine, including a 5 min aerobic warm up, new exercises for the week, and a 10 min stretching cool down - Exercises added: squats, forward lunge, lateral lunge, and lunges with resistance. - Stretches added: single knee to chest, laying on back hamstring, seated hamstring, laying on back hip flexor, laying on back glutes, seated glutes, laying on side quadriceps, standing calve stretch, standing chest stretch with wall, standing or sitting tricep behind the head stretch, standing or sitting shoulder stretch, seated trunk stretch, kneeling hip flexor stretch |
- Participate in 5, 30 min sessions of moderate aerobic exercise -Design upper body strengthening exercises, incorporate new lower body exercises -Perform the strengthening exercises, 2 sets of 12 repetitions each at patient determined weight (ability to complete 2 sets of 12 with moderate difficulty), 2x/week -Fill out exercise plan/log |
| Week 4: Progressing your exercise and advancing your fitness | -Reviewed previous week’s homework -Exercise topics: progressing exercise, advancing fitness levels, energy balance equation, and importance of maintaining variety in exercise |
-30 min exercise routine utilizing the principles discussed for how to progress aerobic and strengthening exercise. -Progressed previously given exercises |
- Design your own exercise plan for the week -Create a plan to strengthen every major muscle group, 2 sets of 12 repetitions each at patient determined weight (ability to complete 2 sets of 12 with moderate difficulty), 2x/week -Fill out exercise plan/log |
| Week 5: The role of exercise in maintaining a healthy weight | -Reviewed previous week’s homework -Education: role of exercise in maintaining a healthy weight -Discussed tools to keep energy balance equation balanced |
-30 min circuit workout incorporating aerobic and strengthening exercises -Circuit: High knee marching (or jogging) OR stationary recumbent bike OR row machine, push ups on counter top or wall, standing ceiling and floor taps, bicep curls OR upright rows with free weights, treadmill OR stationary recumbent bike OR row machine OR high knee marching with elbow twist, rows with resistance band OR free weights, sit to stand squats, scapular squeezes with resistance band, air boxing, bridges, side planks |
- Design your own exercise plan for the week. -Create a plan to strengthen every major muscle group, 2 sets of 12 repetitions each at patient determined weight (ability to complete 2 sets of 12 with moderate difficulty), 2x/week -Fill out exercise plan/log -Write exercise plan moving forward |
| Week 6: Transitioning to independent exercise | -Reviewed previous weeks homework -Education: transitioning to independent exercise, community opportunities for exercise, online/virtual opportunities, phone applications, fitness trackers -Group discussion and sharing of individual exercise plans moving forward -Sharing of 3 exercise “motivators” moving forward |
-15 min balance training program -Education provided on varying balance exercises -Balance handout given with exercises |
- Create your own circuit class at home, 8 to 10 stations incorporating aerobic and strengthening exercises -Circuit to be reviewed at follow up 1-on-1 session |
Measures
Weight
Participants were asked to record their weight as measured via a home bathroom scale in the morning after awakening and with minimal clothing. Patients were asked to self-report their weight weekly. BMI was calculated with the formula (lbs × 703)/height inches 2 .
Weekly activity recall
Patients’ exercise minutes were recorded at week 0 (pre-program, via email questionnaire) and weekly starting at week 5, until week 12 (via patient reported recall). There was a gap in weekly exercise data recorded from week 0 to week 5 due to the original plan to take exercise data at week 0 and week 12. However, at week 5 of the program, the decision was made that regular, weekly recording of exercise minutes would allow for better understanding of program effectiveness, as well as allow for greater exercise accountability among participants. Activity recall included: number of days of aerobic exercise, minutes of aerobic exercise, and number of days of strengthening exercise. Weekly exercise numbers (starting at week 5) were gathered via text message and recorded by the physical therapist every week, regardless of whether it was a PT session or a nutrition session. Patients were encouraged to record all exercise into exercise logs provided in program packet for their own tracking purposes.
Program development questionnaire
Due to interest in understanding the telehealth experience of IM FIT, patients were sent an anonymous feedback survey approximately 2 weeks after the 12-week program finished. Questions in the survey included what participants liked and did not like about the program (5-point Likert scale response choices), pros and cons to the telehealth environment as well as program logistics, knowledge gained, large takeaways, suggestions for improvement, and an opportunity for open-ended feedback.
Statistical analyses
Due to data reflecting one cohort of patients, this study is descriptive in nature. Data reported included number of sessions attended, changes in weight and percent body weight, and changes in aerobic/strength training activity. Qualitative data from the anonymous survey was examined descriptively.
Results
Eight patients began the IM FIT telehealth program in September 2022. They were mostly women (n = 7) and the average age was 54 years (range = 30-68). Cancer diagnoses were endometrial (n = 3), breast (n = 3), brain (n = 1), and thyroid (n = 1). BMI varied across the cohort; n = 5 were in the obese category (BMI ≥ 30), n = 2 were in the overweight category (25.0 ≤ BMI < 30), and n = 1 was in the normal weight category. At the start of the program, all patients had completed active treatment. During IM FIT, 1 patient needed to restart treatment but decided to continue with the program.
Six out of the 8 participants completed the program in December 2022, equating to a drop-out rate of 25%. Both participants that dropped out were female and not in active treatment. Reasons for drop out included life stressors or conflicting work schedule commitments. On average, patients attended 11.3 out of 12 total sessions. The average session attendance for PT was 97%, for nutrition 94%, and for health psychology 94% of the available sessions.
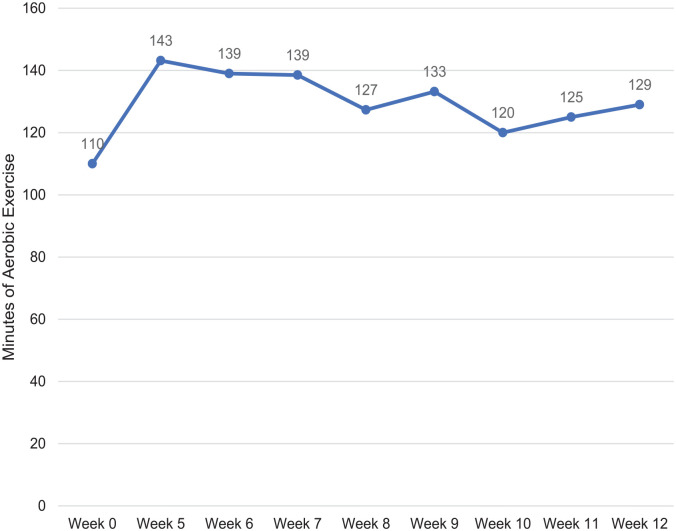
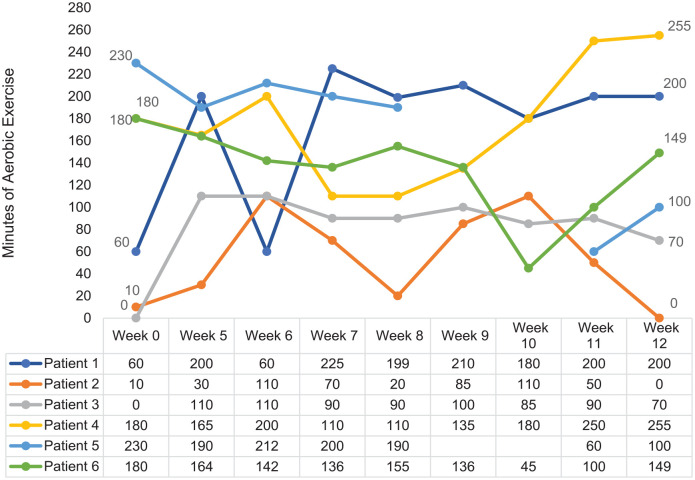
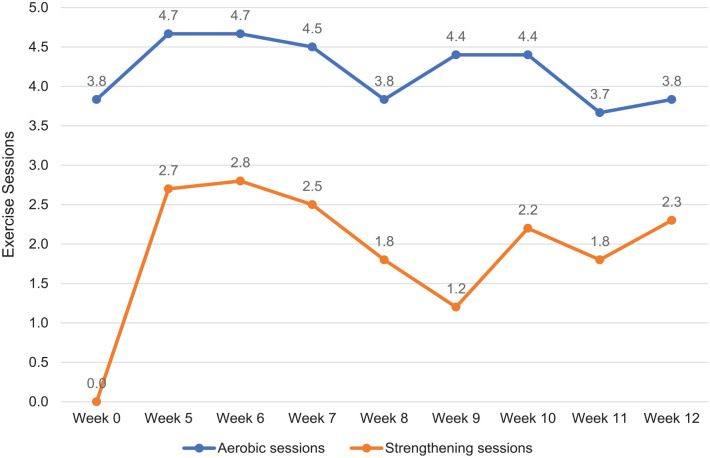
Average minutes of aerobic activity at week 0 (pre-program) and week 5 through week 12 are shown in Figure 1. Figure 2 shows minutes of aerobic exercise per week for individual participants over the course of the intervention. Average minutes of aerobic exercise increased from baseline to session 5 and then remained stable over the 12-weeks. Yet, there was large variability within patients and between patients (Figure 2). Figure 3 shows the weekly activity recall, portrayed in number of exercise sessions per week of aerobic and strengthening activity. Patient 5 had 2 weeks (week 9 and week 10) where no activity recall report was communicated to the therapist; this data was counted as missing and not included in average scores. By the end of the program, the average days of aerobic exercise was 4 days per week, and the average days of strengthening exercise was 2 days per week.
Figure 1.
Average minutes of aerobic exercise per week.
Figure 2.
Individual minutes of aerobic exercise per week.
Figure 3.
Weekly activity recall among IM FIT telehealth participants, average number of exercise sessions per week.
Self-reported weights were recorded for each participant, each week of the program. Average weight loss over the course of the intervention was 5.1 kg (11.3 lbs.), which equates to an average body weight loss of 4.2%.
There was strong social support and accountability within the program, as demonstrated by participants initiating their own texting group on a communication app so they could interact regularly throughout the week. Within the PT sessions, group members discussed how their exercise was going, any issues/questions they had, and would at times share their exercise progress and/or struggles with the group. This allowed the physical therapist to modify exercise instructions/homework as needed, as well as allowed group members to encourage and support each other in the exercise realm. Multiple group members voiced positive feedback regarding exercising in the telehealth environment, reporting they felt more comfortable and were not worried about looking “silly” while exercising with others due to being in their own physical environments. Participants often referred to the group as “family.” Group members even created a team to participate in a cancer-specific 5K fundraiser.
The IM FIT telehealth anonymous feedback survey was completed by 4 out of the 6 participants. See Tables 2 and 3 for close-ended and open-ended item responses, respectively; all 4 participant responses were included. Patients overwhelmingly reported being pleased with the program, and many voiced that the program was only doable for them due to the telehealth nature of the program. Both positive feedback and constructive feedback were received regarding the PT component of IM FIT telehealth. One patient specifically reported wanting PT every week, rather than every other week during the program. Another patient reported feeling comfortable while exercising knowing the physical therapist would be watching and correcting form as needed. Additionally, a patient reported they gained knowledge on how to exercise without belonging to a gym. Exercise accountability was also highlighted as a strength of the program. One participant preferred a hybrid (in-person and telehealth) type of program, in part so that the exercise portion could have in-person demonstration and form correction. Program logistics received high scores, including patients reporting high satisfaction levels with the PT provided handouts.
Table 2.
Anonymous Feedback Survey, Close-Ended Item Responses.
| Item | Response choices | Average |
|---|---|---|
| Question 1: How satisfied are you with the IM FIT telehealth program? | 1 (not very) to 5 (very much) | 4.75 |
| Question 2: How relevant and helpful did you find the program for implementing healthy lifestyle choices now and moving forward? | 1 (not very) to 5 (very much) | 4.75 |
| Question 4: How satisfied were you with the logistics and program materials? | 1 (very dissatisfied) to 5 (very satisfied) | Telehealth setting- 4.5 Schedule- 4.5 Program time commitment- 4.75 Provider communication- 4.75 Handouts, Psychology- 5 Handouts, Nutrition- 4.25 Handouts-Physical Therapy- 5 |
| Question 6: Which sessions/topics do you wish you had more of during the program? | Health psychology, nutrition, physical therapy | Each received 2 votes |
| Question 7: How effective do you feel the telehealth environment was for the following? | 1 (not effective) to 5 (very effective) | Learning- 4.75 Group cohesion- 4.5 Fitting your schedule- 4.75 Exercise- 4.5 Accountability- 4.75 |
| Question 8: If you had a choice between doing IM FIT telehealth or doing IM FIT in-person, which would you choose? | Teleheath, in-person, hybrid model, no preference | Telehealth-2 votes Hybrid-2 votes |
Table 3.
Anonymous Feedback Survey, Open-Ended Item Responses.
| IM FIT telehealth anonymous feedback survey * | |||
|---|---|---|---|
| Question 3: What are the top 3 to 5 things you learned (takeaways) from participating in the IM FIT telehealth program? | |||
| Response 1 | Response 2 | Response 3 | Response 4 |
| NR |
“Focus on plan, eating healthy, exercising regularly
Being Consistent, daily. Get back on target if off Keep a Journal, this helps you to progress.” |
“1. The value of using movement to combat fatigue.
2. Even though it feels like I’m starting from zero with my physical abilities, it’s important to still start and trust that small improvements will add up over time. 3. Relaxation techniques to combat anxiety producing situations (eg. medical tests and procedures) 4. New friendships with other cancer patients. Ongoing support and accountability. 5. The importance of catching my thoughts, checking them, and changing them.” |
“Stress reducing techniques
Alternative food choices Different exercises without having to belong to a gym.” |
| Question 8: If you had a choice between doing IM FIT telehealth or doing IM FIT in-person, which would you choose and why? Could you explain why, please? | |||
| “Being virtual made it super easy to connect. But going to the boot walk as a team and being able to meet some people was nice in person. So maybe virtual with a few meet ups?” | “virtual benefits me better because of the travel distance. No way I could travel that many days and the time of day.” | “Although we were somewhat able to overcome it, I miss the human connection with other cohort members and being able to chat before and after our sessions to deepen relationships. Also, I think the exercise portion would’ve been better in person so we could better see movements being demonstrated and our form could be checked. Being able to actually taste recipes that were prepared would be an incentive to prepare them for ourselves.” | “it provided me the opportunity to participate with limited travel time and the added expense of parking. I knew how much time I would be absent from work and it was very negotiable.” |
| Question 9: What could be improved in the next IM FIT telehealth program? | |||
| “Honestly I wish we had more time each week with it.” | “I’d like to see more focus on dietary foods for plant-based diet. How much is allowed to eat, what are not allowed for individual meals.” | “Doing PT every week, rather than bi-weekly. This would allow for check-ins more often, more gradual adjustments to routine, and the opportunity for more variety. Expanded time for group discussion during health psychology. Some of the most beneficial information came from the sharing of others in our group. Lastly, our group ended up being small enough (6) that I feel we could’ve all done PT together and maintained a consistent schedule.” | “Maybe one in person activity like the Boot walk.” |
| Question 10: What did you enjoy about the IM FIT telehealth program and/or what do you believe worked well? | |||
| “Every single aspect. IM Fit changed my life forever. I have never been so in shape and healthy before.” | “I enjoyed meeting people with the same focus on getting and staying healthy. Each doctor was concerned about our wellbeing. The engaging of everyone thoughts and connection with the group.” |
“The accountability within the group to exercise.
The relationships developed within the group and the sharing and support that was offered. Having off-line conversations throughout the week (via WhatsApp) was HUGELY beneficial. I particularly enjoyed the health psychology sessions and addressing all the ways that cancer diagnosis and treatment affects how we deal with stress, diet, exercise, relating to others, etc. Having manageable expectations for exercise that were achievable.” |
“The no judgement zone of the group. the ability to be comfortable while we exercised but the facilitator was watching to correct or form.” |
| Question 11: Feel free to share any other thoughts/comments/feedback you may have. | |||
| “THANK YOU! To everyone who worked on IM Fit from the instructors to those on the backend we never met, you all truly have made the biggest impact on my life that I will forever be grateful for.” | “I really enjoyed the sessions with each of the doctors.” | “Thank you to MDA and the professionals that participate in the IMFIT program. I’m incredibly grateful to have this level of care available to me and am appreciative of how MDA treats the whole patient, and not just the disease. The professionals were personable, encouraging, supportive and caring. They understand the full impact that cancer has had on us physically, emotionally and mentally, and provided specific support to help us overcome some real challenges. Honestly, 12-weeks wasn’t long enough and felt like just the beginning, as this is a lifestyle change to incorporate, and not just a program to participate in.” | “I have thoroughly enjoyed this group and the cohesiveness that we have established. I like the fact that we still meetup through the app WhatsApp. We stay in touch with one another and provide support to each other when needed. We are also a sounding board for each other in times of need and we can’t get to our professional help.” |
Abbreviation: NR, no response recorded.
All responses included from 4 survey completers.
Discussion
Delivering PT interventions as part of a telehealth comprehensive lifestyle modification program was feasible and effective at increasing physical activity. Group members showed increases in strength training days from 0 to 2 days per week. They showed modest increases in minutes of aerobic activity each week that remained stable from week 5 onward. Based on self-reports from patients, we speculate that the intensity of aerobic exercise increased significantly on days exercised over the course of the intervention as patients learned how to identify moderate intensity exercise. Exercise intensity is captured on other measures that will be assessed with additional cohorts of patients in order to present quantitative data with an ample sample size. When examining individual exercise patterns, there was tremendous variability between and within individuals. This in part may be due to the fact that the PT portion of IM FIT emphasized patients tailoring the program based on their needs and starting points.
With prior cohorts of in-person IM FIT, the intervention team only assessed exercise levels pre and post intervention. Upon initiating this first telehealth cohort, the physical therapist recognized the need for a more accurate week-to-week reporting of exercise activity. The weekly activity recall involved the physical therapist reaching out to participants each week, asking for a report of exercise activity for the week. Tracking week-to-week exercise numbers helped to improve understanding of each participant’s exercise habits, compliance, and consistency across 12 weeks. Additionally, asking participants each week for their exercise numbers allowed for improved instructor-to-participant accountability and thus likely improved exercise compliance and adherence. Some patients did verbalize that this weekly exercise reporting kept them accountable and was a large motivator to exercise weekly. Preliminary data from this study suggests that IM FIT telehealth, a multidisciplinary healthy lifestyle and weight loss program delivered via video, appears to be effective in increasing weekly exercise numbers across strengthening exercise domains.
It is possible that the telehealth setting may be effective for facilitating weight loss. Average body weight loss was −4.2%, which compares similarly to IM FIT delivered in-person, which had an average body weight loss of −3.9%. 30 However, more data are needed as this study only included 6 patients and used self-reported weight measurements that are subject to biases.
IM FIT telehealth was well-attended and demonstrated feasibility of a telehealth implemented program. The average attendance for the PT sessions was 97% over the course of the program, with 4 out of 6 patients having perfect attendance with the PT portion of the program. Neither screen-fatigue nor the physical distance created by video sessions appeared to make IM FIT less valuable. PT specifically continued to have strong attendance even with the challenges in a virtual environment. Furthermore, telehealth interactions did not appear to prevent appropriate, safe, and effective exercise interventions and instruction.
The first cohort of patients suggests that a telehealth environment does not impede group cohesion. In fact, the group created opportunities for additional support of each other, specifically group text messaging and group fitness activities. Participants expressed the importance of feeling understood by others on multiple levels, both with being a cancer survivor and prioritizing healthy lifestyle changes. Opened-ended comments from the anonymous survey highlighted the connectedness of the group.
The aim of the IM FIT telehealth anonymous feedback survey was to assess and record patients’ thoughts, feedback, and perspectives on IM FIT telehealth. The anonymous feedback survey showed great support and appreciation by the participants for the IM FIT telehealth program. Mixed feedback on preferences for program length and duration might suggest that our clinic could develop 2 types of programs that run simultaneously: a full-length program (1 hour PT, 1 hour nutrition, 1.5 hour health psychology per week) and an abbreviated program (2 hours per week). Patients can choose the program that fits their life and work obligations and preferences. Due to patient feedback on the importance of the group text messaging app, we will likely strongly encourage participation in group messaging for future cohorts. Finally, the anonymous survey noted the value of a hybrid approach for some patients, specifically encouraging in-person meet-ups or opportunities for group exercise. Perhaps creating a future IM FIT program that has a telehealth foundation (for convenience and accessibility) with in-person events and occasions (for social support and group cohesion) will further increase patient satisfaction and program effectiveness.
Recent publications showed similar positive outcomes regarding telehealth delivery of intensive exercise programs, as well as the need for telehealth physical therapist-led exercise programs for individuals with cancer. For example, one study examined whether exercise intensity goals could be achieved in a supervised exercise program delivered via telehealth, in women taking endocrine therapy for breast cancer treatment. 35 The 8-week telehealth program offered supervised strength and aerobic exercise as well as education on topics related to physical activity and behavior change, delivered twice weekly via Zoom by an exercise physiologist. Results showed that individuals surviving breast cancer can successfully be instructed in meeting target rate of perceived exertion goals in the telehealth setting and are more likely to reach goals in the latter half of the program. A recent review assessing exercise programs for individuals surviving cancer found that there is a lack of accessible exercise programs in remote and rural areas, and that most interventions offered were phone-based walking programs for survivors of breast cancer. 36 The review concluded that online options greatly increase accessibility for otherwise non-exercising individuals surviving cancer. IM FIT telehealth was not designed to target rural-based individuals surviving cancer; however, many patients voiced that their ability to participate in the program was heavily dependent on the telehealth component. These patients likely would not have received intensive PT interventions and instruction without telehealth PT services within the IM FIT telehealth program. These recent studies, as well as this preliminary report of the PT component of IM FIT telehealth, suggest that an extensive exercise program led by a physical therapist can be effective and improve patient access.
This study described the implementation of the PT component of a telehealth intensive multi-disciplinary lifestyle change program. Strengths included an intervention program that was previously used in-person and found to have positive outcomes. 30 Meaningful qualitative feedback was gathered and described here to elucidate pros and cons related to the telehealth environment. The program remained a billable service, as telehealth PT services were considered billable services per the Public Health Emergency. Billing for PT services contributes to the sustainability of offering an intensive lifestyle program within a hospital system. The telehealth setting allowed for reduced patient expenses, such as travel and parking costs. Conducting the program in the telehealth setting allowed for increased access to patients who otherwise may not have attended such a program due to logistical constraints. Furthermore, having patients engage in physical activity in their home and work settings demonstrated ways to maintain lifestyle changes beyond the 12-week program.
One limitation of this report is that it only describes a cohort of 8 patients, with a drop-out rate of 25%. Treatment status did not appear to be a limiting factor in this program, as both drop-outs were due to work or personal stressors not related to active treatment. We prioritized sharing this PT telehealth model as early as possible due to changing medical reimbursement rates. Telehealth PT is an evolving practice both for providers and patients. An additional limitation is that patients reported exercise data to the therapist based on their own personal monitoring, rather than a more objective measure such as a fitness watch or app, which may have biased recall. Research suggests that self-reported exercise may be both higher and lower than direct measures of activity.37,38 Self-reported weight is also a study limitation because of concerns about validity relative to objectively measured weight 39 ; however, some studies have also shown that self-reported weight is valid and reliable.40,41 We aim for future cohorts to include staff-measured weight and body composition, which will enable us to consider the validity and reliability of IM FIT self-reported measures.
Continuing research is needed to further evaluate additional outcome measures related to pre- and post-program PT measures. Furthermore, examining the long-term effects of this program over months and years would be beneficial. In the future, we would like to compare IM FIT telehealth to IM FIT in-person groups on exercise, diet, weight loss, and group cohesion outcomes. Adding a waitlist control group will help better evaluate the effectiveness of this program.
Conclusions
Prior to our pivot to telehealth delivery of a comprehensive lifestyle modification program, our experience with offering exercise counseling was limited to the in-person setting. Our effort in this exploratory analysis was to better understand the effects of a telehealth PT intervention through qualitative data (open-ended program feedback) and quantitative data (exercise numbers). Through our own experience and that of others,42 -44 we have learned that PT exercise programs can be modified and tailored to be administered in the telehealth environment. Increased patient access remains a strength of this model, serving to equip patients with the tools needed for increasing aerobic and strength training activity. Overall, the program was implemented successfully, and the anonymous feedback survey completed after program completion showed high patient satisfaction with the program. When considering increases in physical activity, weight loss outcomes, positive patient feedback, strong attendance, and an insurance reimbursable model, we conclude that the PT component of IM FIT telehealth is a valuable and effective program to implement in the oncology setting.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Lorenzo Cohen is the co-author of the book Anticancer Living: Transform Your Life and Health with the Mix of Six for which he receives royalties. All other authors have nothing to disclose.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Partial funding for L.C. provided by the Richard E. Haynes Distinguished Professorship for Clinical Cancer Prevention at The University of Texas MD Anderson Cancer Center. This work also received grant support from The University of Texas MD Anderson Cancer Center Duncan Family Institute for Cancer Prevention and Risk Assessment.
Consent to Participate: Data was collected as part of the University of Texas MD Anderson Cancer Center IRB-approved “Integrative Medicine Center Registry Protocol” (DR11-0149, Rev July 7, 2023).
ORCID iD: Gabriel Lopez  https://orcid.org/0000-0002-3685-0280
https://orcid.org/0000-0002-3685-0280
References
- 1. Hahn RA, Kleinman A. Biomedical practice and anthropological theory: frameworks and directions. Annu Rev Anthropol. 1983;12:305-333. Accessed May 6, 2023. http://www.jstor.org/stable/2155650 [Google Scholar]
- 2. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129-136. doi: 10.1126/science.847460 [DOI] [PubMed] [Google Scholar]
- 3. Witt CM, Balneaves LG, Cardoso MJ, et al. A Comprehensive Definition for Integrative Oncology. Natl Cancer Inst Monogr. 2017:3-8. doi: 10.1093/jncimonographs/lgx012 [DOI] [PubMed] [Google Scholar]
- 4. Physical Activity Guidelines Advisory Committee report, 2008. Part A: executive summary. Nutr Rev. 2009;67:114-120. doi: 10.1111/j.1753-4887.2008.00136.x [DOI] [PubMed] [Google Scholar]
- 5. Chekroud SR, Gueorguieva R, Zheutlin AB, et al. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. 2018;5:739-746. doi: 10.1016/S2215-0366(18)30227-X [DOI] [PubMed] [Google Scholar]
- 6. Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36:698-703. doi: 10.1016/s0091-7435(03)00042-2 [DOI] [PubMed] [Google Scholar]
- 7. Hamer J, Warner E. Lifestyle modifications for patients with breast cancer to improve prognosis and optimize overall health. CMAJ. 2017;189:E268-e274. doi: 10.1503/cmaj.160464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schwartz AL, Winters-Stone K, Gallucci B. Exercise effects on bone mineral density in women with breast cancer receiving adjuvant chemotherapy. Oncol Nurs Forum. 2007;34:627-633. doi: 10.1188/07.Onf.627-633 [DOI] [PubMed] [Google Scholar]
- 9. Chlebowski RT. Nutrition and physical activity influence on breast cancer incidence and outcome. Breast. 2013;22 Suppl 2:S30-S37. doi: 10.1016/j.breast.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 10. Dieli-Conwright C, Orozco B. Exercise after breast cancer treatment: current perspectives. Breast Cancer Target Ther. 2015;7:353-362. doi: 10.2147/bctt.S82039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Irwin ML, McTiernan A, Manson JE, et al. Physical activity and survival in postmenopausal women with breast cancer: results from the women’s health initiative. Cancer Prev Res. 2011;4:522-529. doi: 10.1158/1940-6207.CAPR-10-0295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity, risk of death and recurrence in breast cancer survivors: a systematic review and meta-analysis of epidemiological studies. Acta Oncol. 2015;54:635-654. doi: 10.3109/0284186X.2014.998275 [DOI] [PubMed] [Google Scholar]
- 13. Pierce JP, Stefanick ML, Flatt SW, et al. Greater survival after breast cancer in physically active women with high vegetable-fruit intake regardless of obesity. J Clin Oncol. 2007;25:2345-2351. doi: 10.1200/jco.2006.08.6819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bland KA, Zadravec K, Landry T, et al. Impact of exercise on chemotherapy completion rate: a systematic review of the evidence and recommendations for future exercise oncology research. Crit Rev Oncol Hematol. 2019;136:79-85. doi: 10.1016/j.critrevonc.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 15. Courneya KS. Physical activity and cancer survivorship: a simple framework for a complex field. Exerc Sport Sci Rev. 2014;42:102-109. doi: 10.1249/JES.0000000000000011 [DOI] [PubMed] [Google Scholar]
- 16. Morielli A, Courneya K. Effects of exercise on cancer treatment completion and efficacy. In: Schmitz K. (ed.) Exercise Oncology: Prescribing Physical Activity Before and After a Cancer Diagnosis. Springer International Publishing; 2020:209-227. [Google Scholar]
- 17. Yang L, Morielli AR, Heer E, et al. Effects of exercise on cancer treatment efficacy: a systematic review of preclinical and clinical studies. Cancer Res. 2021;81:4889-4895. doi: 10.1158/0008-5472.CAN-21-1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bower JE. The role of neuro-immune interactions in cancer-related fatigue: biobehavioral risk factors and mechanisms. Cancer. 2019;125:353-364. doi: 10.1002/cncr.31790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cerqueira Marinho DA, Neiva HP, Lourenço O. Inflammatory effects of high and moderate intensity exercise-a systematic review. Front Physiol. 2019;10:1550. doi: 10.3389/fphys.2019.01550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zheng G, Qiu P, Xia R, et al. Effect of aerobic exercise on inflammatory markers in healthy middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials. Front Aging Neurosci. 2019;11:98. doi: 10.3389/fnagi.2019.00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lopez G, Eddy C, Liu W, et al. Physical therapist–led exercise assessment and counseling in integrative cancer care: effects on patient self-reported symptoms and quality of life. Integr Cancer Ther. 2019;18:1534735419832360. doi: 10.1177/1534735419832360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. American Physical Therapy Association. Guide to physical therapist practice 3.0. Published 2014. Accessed January 25, 2019. http://guidetoptpractice.apta.org
- 23. Schmitz KH, Ahmed RL, Troxel AB, et al. Weight lifting for women at risk for breast cancer-related lymphedema: a randomized trial. JAMA. 2010;304:2699-2705. doi: 10.1001/jama.2010.1837 [DOI] [PubMed] [Google Scholar]
- 24. Schmitz KH, Courneya KS, Matthews C, et al. American College of Sports Medicine. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42:1409-1426. doi: 10.1249/MSS.0b013e3181e0c112 [DOI] [PubMed] [Google Scholar]
- 25. American Institute for Cancer Research. Treatment tips: planning and preparing. Published 2020. Accessed May 30, 2023. https://www.aicr.org/cancer-survival/treatment-tips/during-treatment/
- 26. McTiernan A. Physical activity for the prevention and treatment of cancer. Physical activity guidelines for Americans, 2nd Edition Web site. Published 2019. Accessed May 30, 2023. https://www.acsm.org/all-blog-posts/acsm-blog/acsm-blog/2019/11/18/physical-activity-prevention-treatment-cancer-guidelines [Google Scholar]
- 27. American College of Sports Medicine. Exercise is medicine: a global health initiative. Published 2021. Accessed June 14, 2023. https://www.exerciseismedicine.org/#
- 28. Campbell KL, Winters-Stone KM, Wiskemann J, et al. Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc. 2019;51:2375-2390. doi: 10.1249/MSS.0000000000002116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hayes SC, Newton RU, Spence RR, Galvão DA. The exercise and sports science australia position statement: exercise medicine in cancer management. J Sci Med Sport. 2019;22:1175-1199. doi: 10.1016/j.jsams.2019.05.003 [DOI] [PubMed] [Google Scholar]
- 30. Christie AJ, Powers-James C, Narayanan S, et al. Multidisciplinary lifestyle modification program (IM-FIT) for cancer survivors: implementation of a reimbursable model in a cancer hospital. Support Care Cancer. 2021;29:7365-7375. doi: 10.1007/s00520-021-06305-7 [DOI] [PubMed] [Google Scholar]
- 31. American Cancer Society. Physical activity and the person with cancer. Living Well After Cancer Web site. Published 2022. Accessed May 30, 2023. https://www.cancer.org/cancer/survivorship/be-healthy-after-treatment/physical-activity-and-the-cancer-patient.html
- 32. Wolin KY, Schwartz AL, Matthews CE, Courneya KS, Schmitz KH. Implementing the exercise guidelines for cancer survivors. J Support Oncol. 2012;10:171-177. doi: 10.1016/j.suponc.2012.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. World Cancer Research Fund/American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective; Continuous update project expert report. Published 2018. Accessed February 1, 2024. http://dietandcancerreport.org
- 34. Sivaramakrishnan D, Fitzsimons C, Kelly P, et al. The effects of yoga compared to active and inactive controls on physical function and health related quality of life in older adults- systematic review and meta-analysis of randomised controlled trials. Int J Behav Nutr Phys Act. 2019;16:33. doi: 10.1186/s12966-019-0789-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Myers SA, Mackenzie KA, LeVasseur N, Faulkner G, Campbell KL. Can breast cancer survivors achieve exercise intensity goals in a virtual supervised exercise program?: 346. Med Sci Sports Exerc. 2022;54:80-80. doi: 10.1249/01.mss.0000876040.86680.b0 [DOI] [Google Scholar]
- 36. Smith-Turchyn J, Gravesande J, Sabiston CM. Exercise interventions for survivors of cancer living in rural or remote settings: a scoping review. Rehabil Oncol. 2020;38:61-80. doi: 10.1097/01.reo.0000000000000208 [DOI] [Google Scholar]
- 37. Nicolson PJA, Hinman RS, Wrigley TV, Stratford PW, Bennell KL. Self-reported home exercise adherence: a validity and reliability study using concealed accelerometers. J Orthop Sports Phys Ther. 2018;48:943-950. doi: 10.2519/jospt.2018.8275 [DOI] [PubMed] [Google Scholar]
- 38. Prince SA, Adamo KB, Hamel ME, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001-2006. Prev Chronic Dis. 2009;6:A121. Published September 17, 2009. [PMC free article] [PubMed] [Google Scholar]
- 40. Wright FL, Green J, Reeves G, Beral V, Cairns BJ. Million Women Study collaborators. Validity over time of self-reported anthropometric variables during follow-up of a large cohort of UK women. BMC Med Res Methodol. 2015;15:81. doi: 10.1186/s12874-015-0075-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yoong SL, Carey ML, D’Este C, Sanson-Fisher RW. Agreement between self-reported and measured weight and height collected in general practice patients: a prospective study. BMC Med Res Methodol. 2013;13:38. doi: 10.1186/1471-2288-13-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Grundstein MJ, Fisher C, Titmuss M, Cioppa-Mosca J. The role of virtual physical therapy in a post–Pandemic World: pearls, pitfalls, challenges, and adaptations. Phys Ther. 2021;101:1-7. doi: 10.1093/ptj/pzab145 [DOI] [PubMed] [Google Scholar]
- 43. Miller MJ, Pak SS, Keller DR, Barnes DE. Evaluation of pragmatic telehealth physical therapy implementation during the COVID-19 pandemic. Phys Ther. 2021;101:1-10. doi: 10.1093/ptj/pzaa193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Weber S, Manzino A, Wilson C. The benefit of nontraditional rehabilitation settings and care delivery models for people living with and beyond cancer. Rehabil Oncol. 2023;41:62-64. doi: 10.1097/01.reo.0000000000000328 [DOI] [Google Scholar]