Abstract
Objective
Thrombophilia screening has been performed in patients with conditions such as previous fetal death, (fetal growth restriction) FGR, preeclampsia, (hemolysis. elevated liver enzyme, low platelet count) HELLP Syndrome, previous abruptio placentae, previous thrombosis in pregnancy, and abnormal placental histology. The actual role of hereditary thrombophilia in recurrent pregnancy loss (RPL) is still debated. This study was intended to determine the incidence of specific gene defects for hereditary thrombophilia and to ascertain their impact on RPL in central Anatolia in Turkey.
Methods
This retrospective cohort study was performed between January 2012 and December 2022. All pregnant women with a complete hereditary screening profile were included. The investigated gene polymorphisms were methylenetetrahydrofolate reductase (MTHFR) C677T, MTHFR A1298C, Factor V Leiden G1691A, and Factor II prothrombin G20210A. Cases of pregnant women at least two or more consecutive pregnancy losses before 22 weeks of gestation were defined as RPL. The rates of genetic screening and their association with RPL were analyzed.
Results
RPL was identified in 224 (27.58%) of the 812 pregnant women with complete genetic screening. Although there was no difference in terms of age, body mass index, numbers of ectopic pregnancies, molar pregnancies, or dilatation & curettage (p > 0.05), gravity (2.0 [2.0–3.0] vs. 4.0 [3.0–5.0]), parity (1.0 [1.0–2.0] vs. 1.0 [0–1.0]), live birth (1.0 [1.0–2.0] vs. 1.0 [0–1.0]), anembryonic pregnancy (0 [0–0] vs. 0 [0–0]), miscarriage (0 [0–1.0] vs. 3.0 [2.0–3.0]), and stillbirth (0 [0–0] vs. 0 [0–0]) numbers differed significantly between the groups (p < 0.05). While no significant differences were determined in MTHFR A1298C, Factor V Leiden, factor II prothrombin G20210A, or homocysteine levels (p > 0.05), the homozygous MTHFR C677T positivity rates differed significantly (6.3% in the non-RPL group vs. 11.6% in the RPL group, p = 0.027) .
Conclusion
The homozygous MTHFR C677T polymorphisms was found to be more frequent in women with RPL. Further studies with larger cohorts are needed to confirm our results.
Keywords: Factor V, Hereditary thrombophilia, Methylenetetrahydrofolate reductase, Pregnancy loss
Introduction
Thrombophilia is a condition potentially predisposing to seriuos pregnanacy complications associated with more than half of thromboembolic events during pregnancy [1]. The obstetric manifestations of thrombophilia include infertility, repeated miscarriages, intrauterine growth restriction, preeclampsia, (hemolysis. elevated liver enzyme, low platelet count) HELLP syndrome, and neonatal fulminant purple [1–4].
Inheritance patterns and risks for individuals diagnosed with inherited thrombophilia have previously been studied. The hereditary form of thrombophilia is usually associated with two or more gene defects [1]. Factor V Leiden (FVL) mutation, prothrombin G20210A mutation, protein C deficiency, protein S deficiency, antithrombin deficiency, hyperhomocysteinemia, and methylenetetrahydrofolate reductase (MTHFR) mutations are the most frequent genetic abnormalities detected in patients with inherited thrombophilia [5–7]. The screening protocol for thrombophilia has been usually recommended in women with a personal history of venous thromboembolism, thrombosis at a young age (< 40 years), more than two family members with a history of thrombosis (> two members), thrombosis at unusual sites, and poor obstetric histories, such as more than three miscarriages, late miscarriage, and fetal death [1, 8].
Recurrent pregnancy loss (RPL) is a well-known clinical entity associated with hereditary thrombophilia. Several medical associations have defined RPL as two or more spontaneous miscarriages before 20 to 24 weeks’ gestation [2, 9–12]. RPL can be seen in 1–5% of women of reproductive age. Although there are various chromosomal, genetic, structural, anatomic, endocrine, and immune causes of RPL, the exact reason cannot be identified in currently nearly half of the cases, and these are classified as idiopathic [6, 10, 13, 14]. Thrombophilic disorders are one of the most frequently suspected etiologies in RPL [6]. However, the relationship between thrombophilia and RPL has not been clearly demonstrated due to the heterogeneity in the inclusion criteria of previously published studies and the different ethnic origins of the patients enrolled [10].
The purpose of this study was to ascertain the rates of specific gene defects for hereditary thrombophilia and possible relations between these gene polymorphisms and RPL in a Turkish population.
Materials and methods
This retrospective cohort analysis of pregnancies between January 2012 and December 2022 was conducted in the Maternal-Fetal Unit of the Hacettepe University, Faculty of Medicine, Obstetrics and Gynecology Department, Ankara, Turkey. The local ethical committee approved the study (Hacettepe University, Ethics Committee, Date 24.09.2009, Number 272079). The researchers agreed to apply the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants prior to hospitalization for future use.
The number of pregnant women attending regular follow-up examinations was 13,728, of whom 1180 were evaluated in the perinatology department. Pregnancies that may pose an increased risk of morbidity or mortality for the mother, fetus, or newborn before or after delivery are evaluated in this clinic. Thrombophilia screening was performed in patients with conditions such as previous fetal death, FGR, preeclampsia, HELLP Syndrome, previous abruptio placentae, previous thrombosis in pregnancy, and abnormal placental histology. Pregnancies with missing hereditary thrombophilia data or that did not conclude with childbirth in our institution were excluded from the study. We also excluded patients with known genetic abnormalities, uterine malformations, and clinically significant uterine fibroids [14]. Eight hundred twelve pregnant women were finally included.
Sociodemographic, obstetric, and clinical data were collected using the patients’ medical files in the hospital information system. Obstetric data included age, body mass index (BMI), gravity, parity, miscarriages, live births, anembryonic pregnancy, ectopic pregnancy, molar pregnancy, stillbirth, and previous dilatation and curettage. The results of the genetic analysis for hereditary thrombophilia were also recorded.
Two or more consecutive pregnancy losses earlier than 22 weeks of gestation, provided that there is at most one surviving child based on the American Society for Reproductive Medicine (ASRM) 2008 criteria, were regarded as RPL [15]. The participants were grouped as RPL-negative (fertile women) (n = 588) and RPL-positive (n = 224).
A real-time polymerase chain reaction test using the fluorescence resonance energy transfer technique was used to analyze the single nucleotide polymorphisms for MTHFR C677T, the MTHFR A1298C, FVLG1691A, and Factor II prothrombin G20210A [2]. Genomic DNA was extracted from venous blood samples. The genetic analyses were performed using commercially available kits. The presence of mutation in these genetic tests was accepted as hereditary thrombophilia-positive [5] and recorded as homozygous or heterozygous. Serum homocysteine levels were measured.
Statistical analysis
The primary outcome was the differences in the prevalance of gene polymorphisms between patients with and without RPL.
For descriptive statistics, mean ± standard deviation was used to present continuous data with normal distribution. Median (25th -75th ) values were used to express continuous variables without normal distribution, while numbers and percentages were used for categorical variables. The Kolmogorov-Smirnov test was applied to assess the normality of distribution of numerical variables. Pearson’s Chi-Square and Fisher’s Exact tests were used to compare differences between categorical variables in 2 × 2 tables. The Independent Samples t-test was applied to compare two independent groups in which numerical variables exhibited normal distribution. The Mann-Whitney U test was applied to compare variables without normal distribution between two independent groups.
Jamovi (Version 2.2.5.0) and JASP (Version 0.16.1) software were used for statistical analysis. Significance (p-value) was set at 0.05 for all statistical analyses.
In the post-hoc power analysis, the power of the study was found to be 99% with an effect size of 0.235 for MTHFR C677T.
Results
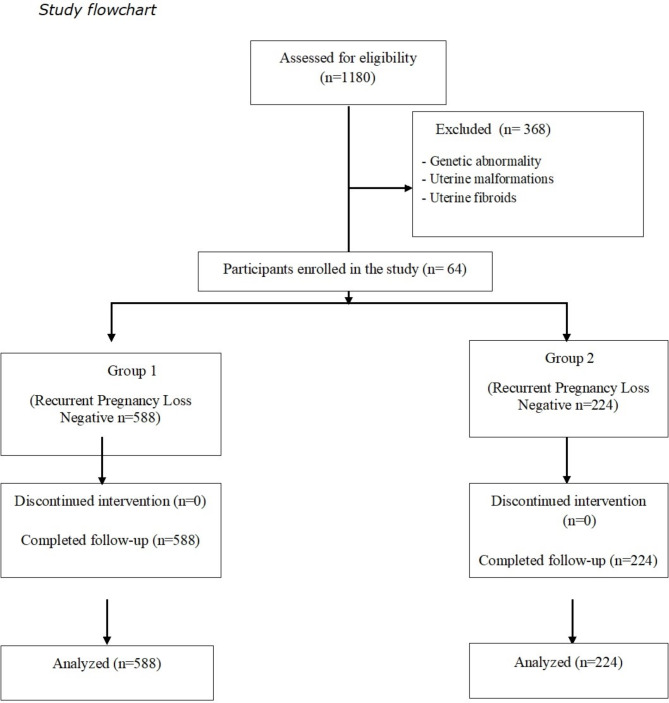
Two hundred twenty-four patients (27.58%) with two or more consecutive pregnancy losses earlier than 22 weeks’ gestation based on the ASRM 2008 criteria were identified. The participants were grouped into two groups: group 1, RPL-negative (n = 588) and group 2, RPL-positive (n = 224) (Fig. 1).
Fig. 1.
Enrollment and follow-up of the study subjects
The participants’ sociodemographic and obstetric characteristics are summarized in Table 1. Although no differences were observed in age, body mass index, numbers of ectopic pregnancies and molar pregnancies, or dilatation & curettage (p > 0.05), gravity and parity numbers, live birth anembryonic pregnancy, miscarriage, and stillbirth differed significantly between the groups (p < 0.05).
Table 1.
Sociodemographic and obstetric characteristics of the participants
| Recurrent Pregnancy Loss Negative (n = 588) |
Recurrent Pregnancy Loss Positive (n = 224) |
P | |
|---|---|---|---|
| Age (years) | 31.05 ± 5.21 | 31.6 ± 5.09 | 0.132 |
| BMI (kg/m 2 ) | 25.23 ± 3.07 | 24.89 ± 3.65 | 0.118 |
| Gravity | 2.0 (2.0–3.0) | 4.0 (3.0–5.0) | < 0.001* |
| Parity | 1.0 (1.0–2.0) | 1.0 (0–1.0) | < 0.001* |
| Live birth | 1.0 (1.0–2.0) | 1.0 (0–1.0) | 0.001* |
| Anembryonic pregnancy | 0 (0–0) | 0 (0–0) | < 0.001* |
| Miscarriage | 0 (0–1.0) | 3.0 (2.0–3.0) | < 0.001* |
| Ectopic pregnancy (n, %) | 11 (1.9%) | 2 (0.9%) | 0.532 |
| Molar pregnancy (n, %) | 6 (1.0%) | 0 (0%) | 0.195 |
| Stillbirth | 0 (0–0) | 0 (0–0) | 0.007* |
| Dilatation & Curettage | 0 (0–0) | 0 (0–0) | 0.766 |
BMI: body mass index
P < 0.05 statistically significant
Table 2 lists the distribution of the hereditary thrombophilia genetic test results between the groups. While no significant differences were observed in the rates of MTHFR A1298C, Factor V Leiden, or factor II prothrombin G20210A, and homocysteine levels (p > 0.05), homozygous MTHFR C677T positivity differed significantly between the groups (6.3% non-RPL vs. 11.6% RPL, p = 0.027) .
Table 2.
Distribution of the genetic test results for hereditary thrombophilia between the groups
| Recurrent Pregnancy Loss Negative (n = 588) |
Recurrent Pregnancy Loss Positive (n = 224) |
p | ||
|---|---|---|---|---|
|
MTHFR C677T n (%) |
Normal | 340 (57.8%) | 113 (50.4%) | 0.027* |
| Heterozygous | 211 (35.9%) | 85 (37.9%) | ||
| Homozygous | 37 (6.3%) | 26 (11.6%) | ||
|
MTHFR A1298C n (%) |
Normal | 433 (73.6%) | 158 (70.5%) | 0.484 |
| Heterozygous | 127 (21.6%) | 57 (25.4%) | ||
| Homozygous | 28 (4.8%) | 9 (4.1%) | ||
|
Factor V Leiden G1691A n (%) |
Normal | 480 (81.6%) | 174 (77.7%) | 0.391 |
| Heterozygous | 100 (17.0%) | 45 (20.1%) | ||
| Homozygous | 8 (1.4%) | 5 (2.2%) | ||
|
Factor II prothrombin G20210A n (%) |
Normal | 568 (96.6%) | 212 (94.6) | 0.226 |
| Heterozygous | 20 (3.4) | 12 (5.4) | ||
| Homocysteine (µmol/L) | 8.57 ± 6.24 | 8.83 ± 5.63 | 0.709 | |
MTHFR: methylenetetrahydrofolate reductase
P < 0.05 statistically significant
Discussion
The study findings show that MTHFR C677T gene polymorphisms are more frequent in the RPL group compared to the control group. However, no significant differences were observed in the rates of the other polymorphisms for hereditary thrombophilia between pregnant women with and without RPL.
Differences in the diagnostic criteria employed for RPL have led to inconsistent outcomes in published studies [2, 3, 9]. Depending on the countries and guidelines involved, different cut-off values have been reported for gestational age and numbers of pregnancy losses. RPL in the present study was diagnosed based on ASRM 2008 criteria [16]. A previous systematic review and meta-analysis revealed no difference in the prevalence of inherited thrombophilia following testing after two versus three pregnancy losses [17]. The findings of several studies have supported this conclusion [18]. Consistent with this approach, we grouped our patients according to a cut-off value of three for the number of pregnancy losses. Under those conditions, we determined no difference in the rates of gene polymorphisms between patients with and without three or more pregnancy losses. It should be remembered that differences in study designs, geographic variations, methods used to select the cases, and definitions and types of RPL may lead to contradictory results.
The frequency and number of these mutations vary depending on patient characteristics, such as ethnicity and geographical differences, and the number of mutations analyzed for inherited thrombophilia. Udumudi et al. [4] proposed that genetic markers for inherited thrombophilia should be increased while evaluating high-risk patients in fertility and obstetric clinics. They recommended the inclusion of genotypes of seven thrombophilia genes (methylenetetrahydrofolate reductase (MTHFR), methionine synthase reductase (MTRR), Methyltransferase (MTR), Annexin A5 (ANXA5), protein Z (PROZ), serine protease inhibitör (SERPINE1), and vascular endothelial growth factor A (VEGFA) in addition to prothrombin, FVL, and MTHFR genes in the risk of inherited thrombophilia for patients with RPL. Several studies have focused on specific nucleotide polymorphisms, such as angiotensin converting enzyme (rs4646994) and β-fibrinogen (rs1800790) [9, 13]. The inclusion of more tests may also lead to the detection of higher rates of thrombophilia.
The frequency of MTHFR C677T in a study from Bosnia was 37.5%, similar to those reported from other countries [18, 19]. Studies from different countries have reported a rate of inherited thrombophilia of almost 33% in patients with RPL [8, 20]. In the present study, FVL mutation (14.3%) was the most frequent type. Mishra et al. [21] detected MTHFRC677T polymorphism (heterozygosity) and FVL heterozygosity in 20.5% and 1.8%, respectively, of Indian patients with RPL. In the present study, the rates of heterozygotes and homozygotes for MTHFR C677T in all pregnant women were 36.5% and 7.8%, respectively, yielding a total of 44.2%. The respective rates for MTHFR A1298C were 22.7% and 4.6%, with a total rate of 27.2%. Similar rates have been reported in other studies from Turkey and from Mexico [12, 22]. The baseline prevalence of MTHFR C677T in the control group is unusually low compared to global data. The reason for this may depend on the ethnicity in the region where the study was conducted. Large-scale studies considering the differences in the patient characteristics and methodologies of these studies are now needed to clarify the inconsistent findings.
The association between inherited thrombophilias and RPL remains controversial [22, 23]. A recent systematic review and meta-analysis concluded that FVL mutation, prothrombin gene, and deficiency of protein S entailed a higher risk of developing RPL [3]. The other mutations (antithrombin and protein C deficiency) were unrelated to RPL. A study from India reported significant associations between hyperhomocysteinemia and MTHFR C677T with early (before 20 gestational weeks) and FVL with both early and late (after 20 gestational weeks) losses [21]. Ahangari et al. [2] showed higher prevalence rates of MTHFR C677T and A1298C mutant alleles in Iranian women with two or more pregnancy losses. Although several authors have speculated that the MTHFR variants are associated with fetal viability, and these configurations result in a selection disadvantage leading to spontaneous abortion, we observed no significant association between gene polymorphisms and RPL [24]. In agreement with the present study, Stamou et al. [20] and López-Jiménez et al. [13] found no impact of prothrombotic and hypofibrinolytic genotypes, including MTHFR C677T and A1298C, FVL, prothrombin gene, antithrombin III, activated protein S, protein C, and protein S on pregnancy loss. Another study from Turkey revealed no significant impact of prothrombin G20210A, FVL G1691A, MTHFR C677T, or MTHFRA1298C on RPL [22]. We think that ethnic and geographic variances may be more critical than expected in yielding such different findings.
The impact of other thrombophilia mutations, FVL G1691A and factor II prothrombin G20210A, on RPL has also been studied [2, 10, 25–27]. Although most of these studies have reported odds ratios from 0.5 to 18 [2, 9, 27], there were no significant differences in the rates of these polymorphisms between patients with and without RPL in the current study. Consistent with our findings, Ahangari et al. [2] and Wingeyer [26] both reported that mutations of prothrombin G20210A and FVL G1691A were not associated with RPL. Padda et al. [25] concluded that the effect of FVL G1619A and prothrombin gene G20210A mutations on various obstetric outcomes are inconclusive and insubstantial. We believe that ethnic and geographic differences may result in inconsistent outcomes.
In the light of the higher rates of these mutations, authors usually recommend genetic testing for hereditary thrombophilia in patients with RPL in order to provide proper management and genetic counseling to high‑risk couples [2, 9]. However, the ESHRE guidelines are opposed to routine screening for all cases of RPL, unless in the presence of a combination of inherited and other thromboembolism risk factors [28]. Patient-based management therefore seems to be a more appropriate way to handle such patients. Although our findings do not support the application of routine screening for hereditary thrombophilia, we do recommend these programs in selected patient groups.
Hyperhomocysteinemia is another hematological abnormality that adversely impacts fertility outcomes. Previous studies have reported various rates, up to 30.4% [21]. Mutations in the MTHFR lead to increased levels of homocysteine. MTHFR mutations and hyperhomocysteinemia are considered risk factors for the pathogenesis of RPL [13]. Hyperhomocysteinemia was detected in 10.6% of all patients and in 14.7% of women with RPL in the present study. This controversial association may be related to the variable frequencies of MTHFR compound heterozygous or homozygous genotypes.
The impact of hereditary thrombophilia on outcomes such as intrauterine growth restriction and hypertensive disorders of pregnancy has been studied previously [1, 6]. Voicu et al. [1] showed that the prothrombin G20210A mutation and antithrombin deficiency were significantly correlated with the development of intrauterine growth restriction. Others found that homozygous variants of MTHFR play a significant role in the development of pregnancy complications [29]. Pregnancy outcomes in patients with and without hereditary thrombophilia were not evaluated in the present research.
The principal limitations of this study were its retrospective design and inclusion of only screened pregnant women. The absence of data concerning other congenital thrombophilic defects and the pregnancy outcomes was another limitation. Nevertheless, the high number of patients in this study was one of its major strengths.
In conclusion, there is a higher frequency of the MTHFR C677T mutation in the group of women with poor perinatal outcomes, without a history of thromboembolism, who were screened for hereditary thrombophilias. Although no significant differences were determined in the rates of the other genetic tests in pregnancies with and without RPL, the genetic testing of these variants is not an absolute necessity for Turkish pregnant women. Nevertheless, screening programs for hereditary thrombophilia (especially MTHFR C677T and family members with hereditary thrombophilia) might be beneficial for detecting the risk of pregnancy losses in selected populations.
Acknowledgements
None.
Author contributions
H.B.S. wrote the main manuscript tex.H.B.S. and M.S.B. collected the data. H.B.S. performed the statistical analysis.All authors reviewed and approved the manuscript.
Funding
None.
Data availability
Data are available with the permission of the corresponding author. E-mail: drberkansayal@yahoo.com.
Declarations
Ethics approval and consent to participate
The local ethical committee approved the study (Hacettepe University, Ethics Committee, Date 24.09.2009, Number 272079). Written informed consent was obtained from all participants prior to hospitalization for future use.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Voicu DI, Munteanu O, Gherghiceanu F, Arsene LV, Bohiltea RE, Gradinaru DM, et al. Maternal inherited thrombophilia and pregnancy outcomes. Exp Ther Med. 2020;20:2411–4. 10.3892/etm.2020.8747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahangari N, Doosti M, Mousavifar N, Attaran M, Shahrokhzadeh S, Memarpour S, et al. Hereditary thrombophilia genetic variants in recurrent pregnancy loss. Arch Gynecol Obstet. 2019;300:777–82. 10.1007/s00404-019-05224-7. [DOI] [PubMed] [Google Scholar]
- 3.Liu X, Chen Y, Ye C, Xing D, Wu R, Li F, et al. Hereditary thrombophilia and recurrent pregnancy loss: a systematic review and meta-analysis. Hum Reprod. 2021;36:1213–29. 10.1093/humrep/deab010. [DOI] [PubMed] [Google Scholar]
- 4.Inal ZO, Inal HA, Kucukkendirci H, Oruc AS. Investigation of cesarean sections at Konya Training and Research Hospital Obstetrics and Gynecology Department between 2010 and 2015. Ginekol Pol. 2017;88:185 – 90. 10.5603/GP.a2017.0036. PMID: 28509319. [DOI] [PubMed]
- 5.Udumudi A, Lava C. Genetic markers for inherited thrombophilia related pregnancy loss and implantation failure in Indian population - implications for diagnosis and clinical management. J Matern Fetal Neonatal Med. 2022;1–9. 10.1080/14767058.2022.2038560. [DOI] [PubMed]
- 6.Karadağ C, Yoldemir T, Karadağ SD, İnan C, Dolgun ZN, Aslanova L. Obstetric outcomes of recurrent pregnancy loss patients diagnosed wıth inherited thrombophilia. Ir J Med Sci. 2017;186:707–13. 10.1007/s11845-017-1569-0. [DOI] [PubMed] [Google Scholar]
- 7.Günebak Şahin T, Sayal B, Coşgun E, Besler T, Beksaç S. Methylenetetrahydrofolate Reductase Enzyme Mutations and Relationship of Homocysteine Vitamin B12 and Folate Blood Levels. Gynecol Obstet Reprod Med. 2013;19:1–6. [Google Scholar]
- 8.Dasari P, Suganya G. Outcome of Index Pregnancy in Women with Recurrent Pregnancy Loss (RPL). J Obstet Gynaecol India. 2022;72(Suppl 1):152–8. 10.1007/s13224-021-01598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Issa NM, El-Neily DAM, El Tawab SS, El-Attar LM. The Prevalence Of Specific Gene Polymorphisms Related To Thrombophilia In Egyptian Women With Recurrent Pregnancy Loss. J Hum Reprod Sci. 2021;14(1):73–80. 10.4103/jhrs.JHRS_24_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khalife S, Geitani R. Association of Inherited Thrombophilia with Recurrent Pregnancy Loss in A Population of Lebanese Women: A Case Control Study. Int J Fertil Steril. 2022;16:247–51. 10.22074/ijfs.2022.540950.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grandone E, Tiscia GL, Mastroianno M, Larciprete G, Kovac M, Tamborini Permunian E, et al. Findings from a multicentre, observational study on reproductive outcomes in women with unexplained recurrent pregnancy loss: the OTTILIA registry. Hum Reprod. 2021;36:2083–90. 10.1093/humrep/deab153. [DOI] [PubMed] [Google Scholar]
- 12.Youssef A, Lashley L, Dieben S, Verburg H, van der Hoorn ML. Defining recurrent pregnancy loss: associated factors and prognosis in couples with two versus three or more pregnancy losses. Reprod Biomed Online. 2020;41:679–85. 10.1016/j.rbmo.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 13.López-Jiménez JJ, Porras-Dorantes Á, Juárez-Vázquez CI, García-Ortiz JE, Fuentes-Chávez CA, Lara-Navarro IJ, et al. Molecular thrombophilic profile in Mexican patients with idiopathic recurrent pregnancy loss. Genet Mol Res. 2016;15(4). 10.4238/gmr.15048728. [DOI] [PubMed]
- 14.Kiykac Altinbas S, Bayoglu Tekin Y, Dilbaz B, Kilic S, Khalil SS, Kandemir O. Impact of having a high-risk pregnancy on future postpartum contraceptive method choice. Women Birth. 2014;27:254–8. 10.1016/j.wombi.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Karlsen K, Schiøler Kesmodel U, Mogensen O, Humaidan P, Ravn P. Relationship between a uterine fibroid diagnosis and the risk of adverse obstetrical outcomes: a cohort study. BMJ Open. 2020;10(2):e032104. 10.1136/bmjopen-2019-032104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2013;99:63. 10.1016/j.fertnstert.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 17.van Dijk MM, Kolte AM, Limpens J, Kirk E, Quenby S, van Wely M, Goddijn M. Recurrent pregnancy loss: diagnostic workup after two or three pregnancy losses? A systematic review of the literature and meta-analysis. Hum Reprod Update. 2020;26:356–67. 10.1093/humupd/dmz048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee GS, Park JC, Rhee JH, Kim JI. Etiologic characteristics and index pregnancy outcomes of recurrent pregnancy losses in Korean women. ObstetGynecol Sci. 2016;59:379–87. 10.5468/ogs.2016.59.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Practice. bulletin no. 124: inherited thrombophilias in pregnancy. Obstet Gynecol. 2011;118:730 – 40. 10.1097/AOG.0b013e3182310c6f [DOI] [PubMed]
- 20.Stamou M, Intzes S, Symeonidou M, Bazntiara I, Bezirgiannidou Z, Pentidou A, et al. Reproductive Failure and Thrombophilia: Not Enough Evidence for a Tight Bond. Acta Haematol. 2022;145:170–5. 10.1159/000520439. [DOI] [PubMed] [Google Scholar]
- 21.Mishra P, Singh K, Tyagi S, Juneja R, Mahapatra M. Inherited and acquired thrombophilia in women of Indian ethnicity with recurrent pregnancy loss: An observational study from North India. Indian J PatholMicrobiol. 2021;64:741–5. 10.4103/IJPM.IJPM_1317_20. [DOI] [PubMed] [Google Scholar]
- 22.Yengel I, Yorulmaz T, Api M. Association between FVL G1691A, FII G20210A, and MTHFR C677T and A1298C polymorphisms and Turkish women with recurrent pregnancy loss. Med Glas (Zenica). 2020;17:129–35. 10.17392/1062-20. [DOI] [PubMed] [Google Scholar]
- 23.El Hachem H, Crepaux V, May-Panloup P, Descamps P, Legendre G, Bouet PE. Recurrent pregnancy loss: current perspectives. Int J Womens Health. 2017;9:331–45. 10.2147/IJWH.S100817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Isotalo PA, Wells GA, Donnelly JG. Neonatal and fetal methylenetetrahydrofolate reductase genetic polymorphisms: an examination of C677T and A1298C mutations. Am J Hum Genet. 2000;67(4):986–90. 10.1086/303082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Padda J, Khalid K, Mohan A, Pokhriyal S, Batra N, Hitawala G, Cooper AC, Jean-Charles G. Factor V Leiden G1691A and Prothrombin Gene G20210A Mutations on Pregnancy Outcome. Cureus. 2021;13(8):e17185. 10.7759/cureus.17185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.PerésWingeyer S, Aranda F, Udry S, Latino J, de Larrañaga G. Inherited thrombophilia and pregnancy loss. Study of an Argentinian cohort. Med Clin (Barc). 2019;152(7):249–54. 10.1016/j.medcli.2017.12.019. English, Spanish. [DOI] [PubMed] [Google Scholar]
- 27.Turki RF, Assidi M, Banni HA, Zahed HA, Karim S, Schulten HJ, et al. Associations of recurrent miscarriages with chromosomal abnormalities, thrombophilia allelic polymorphisms and/or consanguinity in Saudi Arabia. BMC Med Genet. 2016;10(Suppl 1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.ESHRE Guideline Group on RPL, Bender Atik R, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S, et al. ESHRE guideline: recurrent pregnancy loss. Hum Reprod Open. 2018;2018(2):hoy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jeddi-Tehrani M, Torabi R, Zarnani AH, Mohammadzadeh A, Arefi S, Zeraati H, et al. Analysis of plasminogen activator inhibitor-1, integrin beta3, beta fibrinogen, and methylenetetrahydrofolate reductase polymorphisms in Iranian women with recurrent pregnancy loss. Am J Reprod Immunol. 2011;66:149–56. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available with the permission of the corresponding author. E-mail: drberkansayal@yahoo.com.