Abstract
Background
The risk of falls causing periprosthetic fracture has become an issue with the increase in the number of patients undergoing long-term follow-up after total hip arthroplasty (THA) and the aging of patients. The Timed Up and Go test (TUG) is utilized to evaluate fall risk. This study investigated muscle volume around the hip joint based on computed tomography (CT), CT value, and muscle strength to investigate contributing factors to poor TUG 1 year post-THA.
Methods
This study retrospectively investigated 124 patients with unilateral hip osteoarthritis who underwent THA and classified them based on TUG results at 1 year postoperatively into TUG of < 10 s (fast group [103 patients]) and ≥ 10 s (slow group [21 patients]). Body mass index, the volume and CT density of the psoas major and gluteus medius muscles on CT images, pre- and postoperative hip flexion muscle strength, and hip abductor muscle strength were compared in each group.
Results
Age was significantly older and preoperative abductor (fast Group: 1.0 ± 0.3 and slow Group: 0.7 ± 0.3, P = 0.003) and flexion muscle strengths (0.9 ± 0.3 and 0.7 ± 0.3, respectively, P = 0.02) on the healthy side were significantly lower in the slow group. The gluteus medius muscle demonstrated significantly lower CT density in the slow group on both sides. Nominal logistic regression analysis revealed that age and preoperative healthy abductor muscle strength, which are poor factors for TUG 1 year post-THA, were significantly associated with TUG of ≥ 10 s at 1 year post-THA.
Conclusions
The poor factors for TUG 1 year after THA were age and preoperative abductor muscle strength on the healthy side.
Keywords: Timed up and Go test(TUG), Gluteus medius muscle, Total hip arthroplasty(THA), CT density of muscle
Introduction
Total hip arthroplasty (THA) in patients with end-stage hip osteoarthritis is considered one of the most successful surgeries in the orthopedic field, and the number of THA is expected to increase as the population ages [1]. The indication for surgery is expanding because the safety of surgery is relatively guaranteed, and the number of elderly people aged 70–90 who undergo THA will increase in the future [2]. Additionally, the 32-year survival rate of implants is good at 80%, and patients after THA have been predicted to continue to get older in the future [3].
Conversely, falls among the elderly have become a serious social problem in recent years [4], and approximately one-third of patients reported a history of falling at least once within the first year post-THA [5]. Falls are associated with periprosthetic hip fractures post-THA. Reportedly, periprosthetic hip fractures are prevalent in elderly people, and treatment is challenging and the long-term mortality rate is high [6, 7]. To prevent periprosthetic hip fractures, the risk of falling after THA needs to be evaluated. Falls may be associated with a decline in lower limb muscle strength and balance during walking [4].
Timed Up and GO test (TUG) is utilized to evaluate fall risk post-THA. TUG is an effective test to screen for dynamic balance disorders related to increased risk of falls [8]. Older age, female sex, and decreased hip flexion strength are adverse factors for TUG [9, 10]. Decreased abduction muscle strength contributes to unstable walking in patients with hip osteoarthritis [11]. The psoas major muscle, which is a hip flexor, helps maintain posture while walking [12]. Nankaku revealed a decrease in preoperative gluteus medius cross-sectional area as a predictor of limping 6 months post-THA in patients with hip osteoarthritis [11]. However, the muscle shape is widely variable, whereas cross-sectional analysis influences the measurement section area, particularly in patients with severe hip deformity. Muscle volume assessment on computed tomography (CT) has been validated in patients with hip osteoarthritis [13]. Although hip function improves after THA surgery, muscle strength on the operated side has been reported to decrease, sometimes lasting more than two years after surgery [14, 15]. Preoperative sarcopenia, a generalized weakness of the muscles, has been reported to result in poor functional outcomes after THA [16]. We believe that measurement of preoperative muscle volume and muscle strength can be a factor in predicting hip function after THA.
Muscle volume around the hip joint based on CT, CT value, and muscle strength were investigated to elucidate contributing factors to poor TUG 1 year after THA.
Materials and methods
This retrospective study included 148 female patients with unilateral hip arthritis who underwent primary THA from April 2019 to October 2022 (Fig. 1). All participants were females to avoid the influence of gender differences in muscle mass and skeletal muscle fatty degeneration [17]. This study excluded 14 patients who did not undergo examination 1 year postoperatively, 2 patients with no appropriate CT imaging range, 3 patients with high hip dislocation (Crowe types III and IV in 2 and 1 patients, respectively), and 5 patients with neurological disease. The final participants included 124 patients. The cut-off value for TUG was set at 10 s based on the previous reports [11, 18]. This value is lower than other TUG values recommended for predicting future fall risk, such as TUG 16 s [19] and 13.5 s [20]. However, Arnold et al. suggest that setting TUG to a high value to predict falls may miss many older people at moderate to high risk of falling [18], and we finally set the TUG cut-off value at 10 s.
Fig. 1.
Patient selection flowchart
The patients were categorized into the fast group (< 10 s of TUG, n = 103) and the slow group (≥ 10 s of TUG, n = 21).
The Ethics Committee and Institutional Review Board of Yamaguchi University Hospital (H2020-068–2) approved the trial protocol.
Methods
This study evaluated age, height, body mass index (BMI), surgical approach (posterolateral [PL], modified Watson-Jones approach [mWJ], and direct anterior approach[DAA]), femoral components (Mainstay; KYOCERA, Accolade II; Stryker, Exceter; Stryker, Corail; Depuy Synthes, Actis; Depuy Synthes), the volume and CT density of the gluteus medius and psoas muscles assessed with preoperative CT examination, abduction and flexion muscle strength pre-operatively and 1 year postoperatively, postoperative global offset (GO), and history of falls postoperatively.
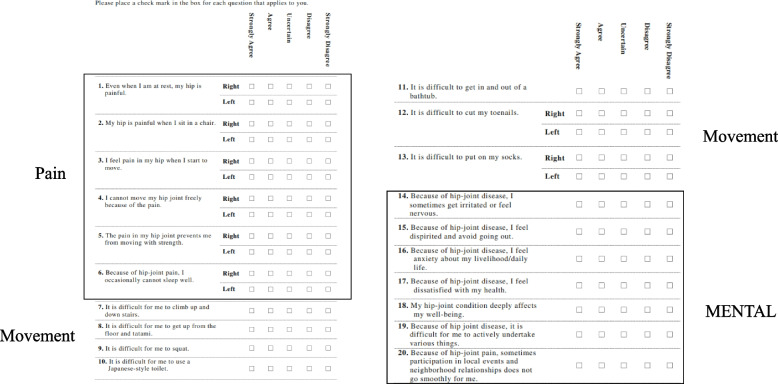
The same team performed the surgery using an intraoperative CT-based navigation system (CT Hip 1.1, Stryker, Mahwah, NJ). Additionally, we use a CT-based 3-dimensional templating system (ZedHip; LEXI, Tokyo, Japan) for preoperative planning. Moreover, the Japanese Orthopedic Association Hip Disease Evaluation Questionnaire (JHEQ) was used preoperatively and 1 year postoperatively for patient-reported outcome measures [21] The JHEQ consists of pain (28 points), movement (28 points), and mental health (28 points), with higher scores indicating better results. Questions are raised for pain, movement, and mental subscales, with possible scores for each item of 0–4, indicating strongly agree, agree, unsure, disagree, and strongly disagree, respectively) (Fig. 2). The maximum total score is 84 points. Some questions can be answered separately for the left and right sides, thereby differentiating and evaluating the affected from the healthy sides.
Fig. 2.
Japanese Orthopedic Association Hip Disease Evaluation Questionnaire (JHEQ). The JHEQ consists of pain (28 points), movement (28 points), and mental (28 points) subscales, with higher scores indicating better outcomes. Questions on the left and right side of the hip joint are to be answered separately, which can be evaluated separately on the affected and healthy side
Muscle volume and CT density
CT was performed preoperatively and 2 weeks postoperatively using a helical-roux CT scanner (Aquilion Precision System, Toshiba Medical System, Tokyo, Japan 120 kv, 300 mA). Patients were assessed in the supine position with their pelvis in the neutral position and the lower limb placed in the patient’s natural rotation, wherein the lower leg position is in a relaxed position. We did not enforce lower legs to patella median position because muscle stretch may affect the muscle volumes.
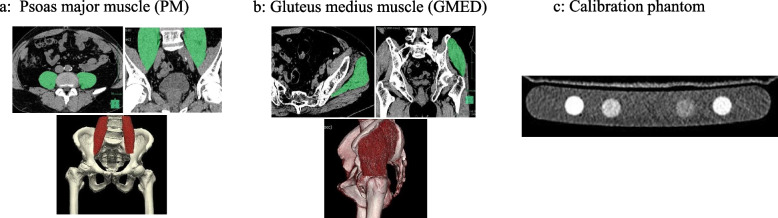
Transverse images were captured from the iliac crest to the foot of each patient with a 1-mm slice thickness. Muscle volume and CT density were measured using dedicated software (Synapse Vincent®: Fujifilm Medical Systems, Tokyo, Japan) referring to previous reports (Fig. 3). A dedicated application within the software was used to automatically measure psoas muscle volume and CT density from the lower border of the L3 vertebral body to the suprapubic bone (Fig. 3a). A free-hand draw method was utilized to measure the gluteus medius muscle by tracing the margin of the gluteus medius muscle, referring to previous reports (Fig. 3b) [22]. The gluteus medius muscle volume and CT density were calculated by masking every three slices from the proximal part where the gluteus medius muscle could be seen to the attachment point of the greater trochanter. Artifacts, such as adjacent bones, were removed, and volumes and CT density were calculated. Volume was divided by height squared to correct for volume effects. CT density was adjusted by calculating the equivalent hydroxyapatite amount in muscle area and a calibration phantom (B-MAS 200; Kyoto-Kagaku, Kyoto, Japan) using dedicated software for adjusted HU calculation of the muscle in the CT image based upon reference values measured in bone mineral reference phantom (Fig. 3c). Muscle volume and CT density were measured on the healthy and affected sides, respectively.
Fig. 3.
The volume and CT density of the psoas major muscle (PM) and gluteus medius muscle (GMED) were measured using dedicated software. a The volume and CT density of the PM were automatically measured using the software application. b The GMED was masked every three slices, and the volume and CT density was calculated. c A calibration phantom (B-MAS 200: Kyoto Scientific, Japan) was placed in the CT scanner and the CT density was corrected using an equal amount of hydroxyapatite in the bone mineral density reference phantom
Timed Up and Go test
TUG was measured preoperatively and 1 year postoperatively. The TUG measures the time required by a patient to stand up from an armless chair, walk a distance of 3 m, turn, walk back to the chair, and sit down. The test was performed by walking at their maximum speed.
Hip abduction and flexion muscle strengths
A handheld dynamometer (ANIMA; uTas F-1) was utilized to measure hip abduction and flexion strength preoperatively and 1 year post-THA. A dynamometer was placed on the outside of the distal thigh to measure hip abduction and flexion muscle strengths in the supine position. The healthy and affected sides were measured thrice times each, and the maximum muscle strength (N) was identified.
Global offset
Measurements were conducted using the CT-based three-dimensional templating system (ZedHip; LEXI, Tokyo, Japan) for preoperative planning. Based on previous reports, we transferred preoperative and 2-week postoperative CT images and constructed independent three-dimensional pelvis and femur models, and acetabular and femoral offsets were measured [23]. Acetabular and femoral offsets were measured by projecting onto the functional pelvic plane (Fig. 4). Acetabular offset is the distance between the pubic symphysis and the center of the femoral head, whereas femoral offset is the distance between the center of the femoral head and shaft. Global offset (GO) was the sum of acetabular offset and femoral [23].
Fig. 4.

Measurement of offset. A Acetabular offset: distance between the cup center and the pubic symphysis. B Femoral offset: distance between the cup center and the femoral axis. Global offset are the sum of A and B
Sample size calculation
Analysis was conducted using G*power (Faul, Erdfelder, Buchner, & Lang, 2009). A power analysis revealed that at least 15 patients in one group and 83 patients in the other were required to compare the groups using a t-test, with an effect size of 0.8, a power of 0.8, and an alpha error of 0.05.
Statistics
This study conducted an analysis using JMP®Pro 15 (SAS Institute Inc). Continuous variables with normal distribution were expressed as mean and standard deviation. The t-test and the chi-square test were used for comparisons between groups for quantitative independent data and categorical data, respectively. We determined preoperative factors with a TUG of 10 s 1 year post-THA using univariate analysis and performed nominal logistic analysis. Intraclass correlation coefficients were calculated to assess the intraobserver and interobserver reliability of muscle volume measurements and CT density of the gluteus medius and psoas major muscles. Hence, the author measured the gluteus medius and psoas major muscle volumes and CT density of 30 randomly selected joints twice at an interval of 6 months, and another orthopedic surgeon (MU) evaluated the same patients, and intraobservation reliability and interobserver reliability were assessed.
Results
The intraobserver and interobserver reliabilities were 0.987 (95% confidence interval [CI]: 0.973–0.994) and 0.893 (95% CI: 0.788–0.948) for the volume measurement (Table 1) and 0.992 (95% CI: 0.983–0.996) and 0.989 (95% CI: 0.976–0.996) for the CT density of the gluteus medius muscle, respectively. The intraobserver and interobserver reliabilities were 0.998 (95% CI: 0.997–0.999) and 0.995 (95% CI: 0.989–0.998) for the volume measurements and 0.951 (95% CI: 0.983–0.996) and 0.978 (95% CI: 0.955–0.990) for the CT density of the psoas major muscle, respectively.
Table 1.
The intraobserver and interobserver reliabilities of the volume measurement of the gluteus medius and psoas major muscles
| Intraobserver reliability ICC (1,1) (95% CI) |
Interobserver reliability ICC (2,1) (95% CI) |
|
|---|---|---|
| Gluteus medius muscle | ||
| Volume | 0.987 (0.973–0.994) | 0.893 (0.788–0.948) |
| CT density | 0.992 (0.983–0.996) | 0.989 (0.976–0.996) |
| Psoas major muscle | ||
| Volume | 0.998 (0.997–0.999) | 0.995 (0.989–0.998) |
| CT density | 0.951 (0.983–0.996) | 0.978 (0.955–0.990) |
ICC Intraclass correlation coefficients, CI Confidence interval, CT Computed tomography
One year post-THA, 103 (83.1%) patients in the fast group reported a TUG of < 10 s, whereas 21 (16.9%) patients in the slow group exhibited a TUG of ≥ 10 s. Age (fast group: 65.3 ± 10.5 and slow group: 74.4 ± 7.8, P < 0.0001) was significantly older in the slow group. Preoperative JHEQ total score on the affected side, preoperative JHEQ movement score and total score on the healthy side, and preoperative JHEQ mental score were significantly lower in the slow group (Table 2). Conversely, there were no significant differences in BMI, femoral components, preoperative JHEQ pain score, preoperative JHEQ movement score on the affected side, as well as pain score on the healthy side.
Table 2.
Baseline characteristics of Fast and Slow groups
| Fast Group N = 103 patients |
Slow Group N = 21 patients |
P-value | |
|---|---|---|---|
| Age (years) | 65.3 ± 10.5 (25–84)a | 74.4 ± 7.8 (55–86)a | < 0.0001 |
| BMI (kg/m2) | 24.0 ± 5.1 (16.3–40.5)a | 25.3 ± 5.6 (18.1–39.3)a | 0.31 |
|
Surgical approach (hips) (PL/OCM/DAA) |
62/9/32 | 9/0/12 | 0.24 |
| Femoral components (hips) | 0.17 | ||
| Mainstay | 43 | 9 | |
| Accolade II | 35 | 4 | |
| Corail | 20 | 5 | |
| Actis | 3 | 1 | |
| Exceter | 2 | 2 | |
| TUG (sec) | |||
| Preoperative | 11.2 ± 4.9 (5.7–26.7)a | 18.3 ± 7.1 (9.2–36.4)a | < 0.0001 |
| Postoperative | 7.1 ± 1.4 (4.7–9.9)a | 13.5 ± 5.1 (10.7–35.0)a | < 0.0001 |
|
Preoperative JHEQ Affect side | |||
| Pain | 6.3 ± 4.9 (0–22)a | 6.2 ± 4.3 (0–12)a | 0.90 |
| movement | 5.1 ± 5.1 (0–20)a | 2.2 ± 3.1 (0–8)a | 0.05 |
| total score | 20.4 ± 13.9 (0–68)a | 13.3 ± 8.3 (0–27)a | 0.03 |
| Preoperative JHEQ Healthy side | |||
| Pain | 25.2 ± 5.4 (0–28)a | 24.3 ± 4.4 (13–28)a | 0.50 |
| Movement | 10.1 ± 4.2 (0–23)a | 6.1 ± 4.0 (1–14)a | 0.0002 |
| Total Score | 43.9 ± 12.0 (10–75)a | 35.3 ± 6.5 (26–50)a | 0.002 |
| Preoperative JHEQ Mental | 8.7 ± 6.3 (0–28)a | 4.6 ± 3.3 (0–9)a | 0.004 |
BMI Body mass index, PL Posterolateral, OCM Orthopadisehe Chirugie Munchen, DAA Direct anterior approach, TUG Timed UP and Go test, JHEQ Japanese Orthopedic Association Hip Disease Evaluation Questionnaire
amean ± SD (range)
History of falls after THA were significantly more frequent in the slow group (fast group: 10 [9.7%] and slow group: 8 [38.1%] patients, P = 0.002).
Preoperative abductor muscle strength (fast group: 1.0 ± 0.3 and slow group: 0.7 ± 0.3, P = 0.003) and flexion muscle strength on the healthy side (fast group: 0.9 ± 0.3 and slow group: 0.7 ± 0.3, P = 0.02) was significantly lower in the slow group (Table 3). Conversely, no significant difference in abductor or flexion muscle strengths on the affected side was found between the two groups. One year post-THA, abductor and flexion muscle strengths were significantly lower in the slow group on both the affected and healthy sides.
Table 3.
Preoperative and postoperative hip abductor and flexion muscle strengths
| Fast Group N = 103 mean ± SD |
Slow Group N = 21 mean ± SD |
P-Value | |
|---|---|---|---|
| Preoperative | |||
| Abductor muscle strength (Nm/kg) | |||
| Affected side | 0.7 ± 0.3 | 0.6 ± 0.3 | 0.05 |
| Healthy side | 1.0 ± 0.3 | 0.7 ± 0.3 | 0.003 |
| Flexion muscle strength (Nm/kg) | |||
| Affected side | 0.6 ± 0.3 | 0.6 ± 0.3 | 0.55 |
| Healthy side | 0.9 ± 0.3 | 0.7 ± 0.3 | 0.02 |
| Postoperative(1year) | |||
| Abductor muscle strength (Nm/kg) | |||
| Affected side | 1.1 ± 0.3 | 0.8 ± 0.2 | < 0.0001 |
| Healthy side | 1.2 ± 0.3 | 0.8 ± 0.3 | < 0.0001 |
| Flexion muscle strength (Nm/kg) | |||
| Affected side | 0.9 ± 0.3 | 0.7 ± 0.3 | 0.001 |
| Healthy side | 1.0 ± 0.3 | 0.7 ± 0.3 | < 0.001 |
CT Computed tomography
The CT density of the gluteus medius was significantly lower in the slow group on both the healthy and affected sides (affected side: fast group: 24.5 ± 13.7 and slow group: 13.4 ± 21.5, P = 0.001, healthy side: fast group: 36.6 ± 7.7 and slow group: 27.1 ± 11.5, P < 0.0001), and the adjusted CT density of the gluteus medius was significantly lower in the slow group (affected side: fast group: 15.6 ± 12.6 and slow group: 6.2 ± 18.1, P = 0.005, healthy side: fast group: 26.3 ± 7.9 and slow group: 19.0 ± 9.7, P = 0.0003) (Table 4). No significant difference in the volume of the gluteus medius was found between the affected and healthy sides. No significant differences in volume, density, or adjusted CT density of the psoas major muscle were observed.
Table 4.
Comparison of volume and adjusted CT density of gluteus medius and psoas major muscles by CT examination
| Fast Group N = 103 mean ± SD |
Slow Group N = 21 mean ± SD |
P-Value | |
|---|---|---|---|
| Gluteus medius muscle | |||
| Volume (ml/m2) | |||
| Affected side | 80.4 ± 16.6 | 75.7 ± 12.9 | 0.22 |
| Healthy side | 94.7 ± 19.5 | 88.0 ± 16.4 | 0.15 |
| CT density (HU) | |||
| Affected side | 24.5 ± 13.7 | 13.4 ± 21.5 | 0.001 |
| Healthy side | 36.6 ± 7.7 | 27.1 ± 11.5 | < 0.0001 |
| Adjusted CT density (mg/cm3) | |||
| Affected side | 15.6 ± 12.6 | 6.2 ± 18.1 | 0.005 |
| Healthy side | 26.3 ± 7.9 | 19.0 ± 9.7 | 0.0003 |
| Psoas major muscle | |||
| Volume (ml/m2) | |||
| Affected side | 21.5 ± 7.0 | 20.9 ± 5.4 | 0.72 |
| Healthy side | 27.5 ± 7.1 | 29.0 ± 7.0 | 0.36 |
| CT density (HU) | |||
| Affected side | 37.8 ± 7.7 | 32.5 ± 7.9 | 0.22 |
| Healthy side | 40.7 ± 6.4 | 37.9 ± 6.9 | 0.07 |
| Adjusted CT density (mg/cm3) | |||
| Affected side | 24.5 ± 7.5 | 23.4 ± 7.6 | 0.51 |
| Healthy side | 29.8 ± 6.2 | 28.1 ± 6.9 | 0.26 |
CT Computed tomography
JHEQ was significantly lower in the slow group in terms of movement and total scores on the affected side and movement, total, and mental scores on the healthy side 1 year post-THA (Table 5). No significant differences in pain items were observed between the two groups on both the affected and healthy sides. No significant difference in GO was found between the two groups on both the affected and healthy sides (Table 6).
Table 5.
The results of postoperative JHEQ between the fast and slow groups
| Fast Group N = 103 mean ± SD |
Slow Group N = 21 mean ± SD |
P-Value | |||
|---|---|---|---|---|---|
|
Postoperative JHEQ |
Affected side | Pain | 25.1 ± 4.3 | 24.7 ± 5.8 | 0.72 |
| Movement | 19.3 ± 6.7 | 15.8 ± 8.0 | 0.04 | ||
| Total Score | 68.2 ± 13.5 | 60.8 ± 17.0 | 0.03 | ||
| Healthy side | Pain | 26.3 ± 3.5 | 26.3 ± 4.6 | 0.98 | |
| Movement | 20.5 ± 5.8 | 16.7 ± 7.8 | 0.01 | ||
| Total Score | 70.6 ± 12.0 | 64.7 ± 15.2 | 0.05 | ||
| Mental | 23.7 ± 5.3 | 20.3 ± 7.0 | 0.01 | ||
JHEQ Japanese Orthopedic Association Hip Disease Evaluation Questionnaire
Table 6.
The results of Acetabular offset, Femoral offset and Global offset between the fast and slow groups
| Fast Group N = 103 mean ± SD |
Slow Group N = 21 mean ± SD |
P-Value | ||
|---|---|---|---|---|
| Acetabular offset (mm) | Affected side | 86.8 ± 4.7 | 87.5 ± 4.2 | 0.58 |
| Healthy side | 88.3 ± 5.6 | 87.4 ± 4.0 | 0.56 | |
| Femoral offset (mm) | Affected side | 33.4 ± 7.2 | 37.0 ± 6.4 | 0.06 |
| Healthy side | 32.8 ± 6.4 | 35.3 ± 5.9 | 0.14 | |
| Global offset (mm) | Affected side | 120.2 ± 8.1 | 124.5 ± 7.2 | 0.06 |
| Healthy side | 121.1 ± 7.9 | 122.8 ± 7.3 | 0.43 |
Univariate analysis revealed age (P < 0.0001), abductor (P = 0.003) and flexor muscle strengths on the healthy side (P = 0.02), and the CT density of the gluteus medius muscle on the affected (P = 0.001) and healthy sides (P < 0.0001) as preoperative significant factors for TUG of ≥ 10 s. The factors that caused TUG to be ≥ 10 s in 1 year post-THA were investigated using nominal logistic regression analysis, revealing age (odds ratio [OR]: 1.13, 95% CI: 1.0–1.2, P = 0.0002) and preoperative abductor muscle strength on the healthy side (OR: 0.07, 95% CI: 0.0007–0.7, P = 0.02) as significant factors (Table 7). TUG at one year after THA correlated with preoperative abductor muscle strength on the healthy side (R = -0.27 P = 0.002). TUG at one year after THA correlated with age (R = 0.36 P < 0.001).
Table 7.
Factors that caused TUG to be ≥ 10 s in 1 year post-THA investigated using nominal logistic regression analysis
| β | Standardized β | 95%CI | P-value | |
|---|---|---|---|---|
| Age | 0.12 | 0.39 | 0.07–0.17 | < 0.0001 |
| Abductor muscle strength in the healthy side (Nm/kg) | − 2.4 | − 0.25 | 0.004 –4.0 | 0.004 |
Discussion
A most important result of this study was that preoperative abductor muscle strength on the healthy side and age were associated with poor TUG results 1 year post-THA using the nominal logistic regression analysis. The slow group demonstrated significantly lower preoperative abductor muscle strength on the affected and healthy sides, preoperative flexion strength on the healthy side, preoperative CT density of the gluteus medius muscle on the affected and healthy sides, and age than the fast group. The results indicate that strength and muscle quality of the healthy side, but not the affected side, as well as the gluteus medius muscles are important for TUG results 1 year post-THA, contrary to the hypothesis of this study.
The CT density is useful for assessing muscle quality [13]. Goodpaster et al. revealed a high correlation between CT values and skeletal muscle steatosis, which decreases by 1 HU when the lipid concentration increases by 1 g/100 ml [24]. Additionally, increased intramuscular adipose tissue has reduced muscle performance and metabolic status [24]. Reportedly, a large burden is placed on the healthy knee joint in patients with unilateral hip osteoarthritis when walking [25, 26]. Hence, the affected side first experiences muscle weakness and a decreased sense of balance, and the function of the healthy side declines as the affected side worsens [27]. In particular, fatty degeneration of the gluteus medius muscle on the healthy side develops and abductor muscle strength is reduced even with unilateral hip osteoarthritis, as the disease progresses. Ohmori et al. [23] revealed that preoperative one-leg standing time on the healthy side of patients with unilateral hip osteoarthritis was associated with 10-m walking speed 1 year post-THA, confirming the results of the present study. The slow group exhibited lower CT density and preoperative abductor muscle strength in the healthy gluteus medius muscles than the fast group. Adjusted CT densities were obtained, with similar results, as CT density can be biased by the environment. Preoperative abductor muscle strength was a significant factor in the nominal logistic analysis. Therefore, early intervention in patients with unilateral hip osteoarthritis is recommended before the function of the gluteus medius muscle on the healthy side deteriorates.
The results of this study showed that TUG was poor 1 year after THA if there was preoperative reduction in abductor muscle strength on the healthy side. Although pre- and post-operative pain scores were not significantly different between the two groups, the slow group had lower pre-operative and post-operative movement scores and lower mental scores.
TUG can be conducted in a short time and is considered useful for evaluating fall risk [28]. Additionally, the Centers for Disease Control and Prevention recommends TUG as a screening test for fall risk in older adults [29]. The history of falls post-THA was significantly frequent in the slow group. Additionally, TUG is useful for predicting postoperative functional outcomes in patients with hip prostheses and is a predominant preoperative and postoperative evaluation [29–32]. Conversely, literature investigating factors that cause poor TUG after THA is limited, and this study is the first to report that preoperative abductor muscle strength on the healthy side is a factor that causes poor TUG 1 year post-THA. Previous studies have revealed that a decrease in GO on the operated side reduces abductor muscle strength and declines walking ability [33]. This study revealed no significant difference between the two groups because a CT-based three-dimensional templating system was used for preoperative planning. The offset was planned to be no > 10 mm compared to the healthy side; thus, the effect of the offset was considered minor.
This study has limitations. This study did not evaluate CT 1 year postoperatively due to radiation exposure. However, previous reports indicate that the gluteus medius muscle muscle persists even 2 years post-THA on the affected and healthy sides [15]. Additionally, this study only evaluated the psoas major and gluteus medius muscles. Evaluation of other muscles is desirable for a practical understanding of functional impairment in hip osteoarthritis because hip movements require complex coordination of multiple muscles. In the future, our volumetric/qualitative CT analysis will be useful for assessing other muscles and providing better information compared to traditional analyses based on muscle cross-sectional area.
Conclusion
We measured preoperative muscle volume and CT density of the psoas major muscle and gluteus medius muscle, evaluated the longitudinal change of these muscle strengths, and investigated whether they were factors for poor TUG 1 year post-THA. The unfavorable factors for TUG 1 year post-THA include preoperative abduction strength in the healthy side and age. Surgical treatment is recommended before fatty degeneration and weakness of gluteus medius muscles develop in patients with unilateral hip arthritis.
Acknowledgements
This work was supported by JSPS KAKENHI [grant number JP23K10426].
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TK, TI, YM, TO, TK, KY, UM and TS. The first draft of the manuscript was written by Takehiro Kawakami and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other supports were received for the conduct of the study or the preparation of this manuscript.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This retrospective, case-control study was approved by the Institutional Review Board of Yamaguchi University Graduate School of Medicine (the ethics committee of Yamaguchi University Graduate School of Medicine, reference number: H2020-068-2). The ethical standards from the 1964 Helsinki declaration and its later amendments were upheld. Informed consent was obtained from all participants for this study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 3 and 4.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Rupp M, Lau E, Kurtz SM, Alt V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res. 2020;478:1622–33. 10.1097/CORR.0000000000001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLaughlin JR, Johnson MA, Lee KR. Uncemented total hip arthroplasty with a tapered titanium femoral component: a minimum 30-year follow-up. Bone Jt Open. 2023;4:79–86. 10.1302/2633-1462.42.BJO-2022-0142.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganz DA, Latham NK. Prevention of falls in community-dwelling older adults. N Engl J Med. 2020;382:734–43. 10.1056/NEJMcp1903252. [DOI] [PubMed] [Google Scholar]
- 5.Levinger P, Wee E, Margelis S, et al. Pre-operative predictors of post-operative falls in people undergoing total hip and knee replacement surgery: a prospective study. Arch Orthop Trauma Surg. 2017;137:1025–33. 10.1007/s00402-017-2727-6. [DOI] [PubMed] [Google Scholar]
- 6.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–65. 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Lindahl H, Oden A, Garellick G, Malchau H. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007;40:1294–8. 10.1016/j.bone.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Nightingale CJ, Mitchell SN, Butterfield SA. Validation of the timed up and go test for assessing balance variables in adults aged 65 and older. J Aging Phys Act. 2019;27:230–3. 10.1123/japa.2018-0049. [DOI] [PubMed] [Google Scholar]
- 9.Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29:64–8. 10.1519/00139143-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Beauchet O, Fantino B, Allali G, et al. Timed Up and Go test and risk of falls in older adults: a systematic review. J Nutr Health Aging. 2011;15:933–8. 10.1007/s12603-011-0062-0. [DOI] [PubMed] [Google Scholar]
- 11.Nankaku M, Tsuboyama T, Aoyama T, et al. Preoperative gluteus medius muscle atrophy as a predictor of walking ability after total hip arthroplasty. Phys Ther Res. 2006;19:8–12. 10.1298/ptr.e9884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersson E, Oddsson L, Grundström H, Thorstensson A. The role of the psoas and iliacus muscles for stability and movement of the lumbar spine, pelvis and hip. Scand J Med Sci Sports. 1995;5:10–6. 10.1111/j.1600-0838.1995.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 13.Ogawa T, Takao M, Otake Y, et al. Validation study of the CT-based cross-sectional evaluation of muscular atrophy and fatty degeneration around the pelvis and the femur. J Orthop Sci. 2020;25:139–44. 10.1016/j.jos.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Shih CH, Du YK, Lin YH, et al. Muscular recovery around the hip joint after total hip arthroplasty. Clin Orthop Relat Res. 1994;302:115–20. [PubMed] [Google Scholar]
- 15.Rasch A, Byström AH, Dalén NE, et al. Persisting muscle atrophy two years after replacement of the hip. J Bone Joint Surg Br. 2009;91:583–8. 10.1302/0301-620X.91B5.21477. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka S, Kayamoto A, Terai C, et al. Preoperative sarcopenia severity and clinical outcomes after total hip Arthroplasty. Nutrients. 2024;16(13):2085. 10.3390/nu16132085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visser AW, de Mutsert R, Loef M, et al. The role of fat mass and skeletal muscle mass in knee osteoarthritis is different for men and women: the NEO study. Osteoarthritis Cartilage. 2014;22:197–202. 10.1016/j.joca.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Arnold CM, Faulkner RA. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007;4(7):17. 10.1186/1471-2318-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kristensen MT, Foss NB, Kehlet H. Timed, “up & go” test as a predictor of falls within 6 months after hip fracture surgery. Phys Ther. 2007;87(1):24–30. 10.2522/ptj.20050271. [DOI] [PubMed] [Google Scholar]
- 20.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 21.Matsumoto T, Kaneuji A, Hiejima Y, et al. Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire (JHEQ): a patient-based evaluation tool for hip-joint disease. The Subcommittee on Hip Disease Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association. J Orthop Sci. 2012;17:25–38. 10.1007/s00776-011-0166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Momose T, Inaba Y, Choe H, et al. CT-based analysis of muscle volume and degeneration of gluteus medius in patients with unilateral hip osteoarthritis. BMC Musculoskelet Disord. 2017;18:457. 10.1186/s12891-017-1828-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohmori T, Kabata T, Kajino Y, et al. Contralateral lower-limb functional status before total hip arthroplasty: an important indicator for postoperative gait speed. J Bone Joint Surg Am. 2021;103:1093–103. 10.2106/JBJS.20.00949. [DOI] [PubMed] [Google Scholar]
- 24.Goodpaster BH, Kelley DE, Thaete FL, et al. Skeletal muscle attenuation determined by computed tomography is associated with skeletal muscle lipid content. J Appl Physiol. 1985;2000(89):104–10. 10.1152/jappl.2000.89.1.104. [DOI] [PubMed] [Google Scholar]
- 25.Miljkovic I, Zmuda JM. Epidemiology of myosteatosis. Curr Opin Clin Nutr Metab Care. 2010;13:260–4. 10.1097/MCO.0b013e328337d826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Foucher KC, Wimmer MA. Contralateral hip and knee gait biomechanics are unchanged by total hip replacement for unilateral hip osteoarthritis. Gait Posture. 2010;35:61–5. 10.1016/j.gaitpost.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Roos EM, Herzog W, Block JA, Bennell KL. Muscle weakness, afferent sensory dysfunction and exercise in knee osteoarthritis. Nat Rev Rheumatol. 2011;7:57–63. 10.1038/nrrheum.2010.195. [DOI] [PubMed] [Google Scholar]
- 28.Friesenbichler B, Casartelli NC, Wellauer V, et al. Explosive and maximal strength before and 6 months after total hip arthroplasty. J Orthop Res. 2018;36:425–31. 10.1002/jor.23626. [DOI] [PubMed] [Google Scholar]
- 29.Phelan EA, Mahoney JE, Voit JC, Stevens JA. Assessment and management of fall risk in primary care settings. Med Clin North Am. 2015;99(2):281–93. 10.1016/j.mcna.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;2015(80):896–903. 10.1093/ptj/80.9.896. [PubMed] [Google Scholar]
- 31.Poitras S, Au K, Wood K, et al. Predicting hospital length of stay and short-term function after hip or knee arthroplasty: are both performance and comorbidity measures useful? Int Orthop. 2018;42:2295–300. 10.1007/s00264-018-3833-y. [DOI] [PubMed] [Google Scholar]
- 32.Oosting E, Kapitein PJC, de Vries SV, Breedveld E. Predicting short stay total hip arthroplasty by use of the timed up and go-test. BMC Musculoskelet Disord. 2021;22:361. 10.1186/s12891-021-04240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahmood SS, Mukka SS, Crnalic S, et al. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthop. 2016;87:36–41. 10.3109/17453674.2015.1091955. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study available from the corresponding author on reasonable request.