Abstract
The objective of this meta-analysis was to determine the effect of behavioral interventions in reducing risky sexual behavior and incident sexually transmitted infections (STI) among Latina women living in the United States. Studies were found by systematically searching the MEDLINE, EMBASE, and PsychInfo databases without language restriction. Two independent reviewers screened abstracts and full texts of articles to find randomized control trials testing the effects of behavioral interventions aimed at changing risky sexual behavior among Latinas. Articles were selected using prespecified inclusion criteria. Two independent reviewers extracted data from the included trials in duplicate using a standardized data extraction form. Six randomized control trials met the inclusion criteria for a total of 2,909 participants. Using random effects models with inverse variance weighting, we found a protective effect of the behavioral intervention on reported risky sexual behavior (odds ratio = 0.52; 95% confidence interval = 0.42, 0.64) and on incident nonviral STI (odds ratio = 0.65; 95% confidence interval = 0.46, 0.93). Behavioral interventions targeted toward Latina populations are effective in reducing risky sexual behaviors and incident STI and should be considered by policymakers as a potential tool for HIV/STI prevention in this population.
Keywords: behavioral intervention, condom use, Latina, meta-analysis, sexually transmitted infections
Latina women represent a high-risk subgroup for incident HIV and sexually transmitted infections (STIs). In the United States, Latinas are more than four times more likely to become infected with HIV than White women (Centers for Disease Control and Prevention [CDC], 2012). The high prevalence of STIs in this population further increases the risk of HIV transmission (CDC, 2011; Peragallo, Gonzalez-Guarda, McCabe, & Cianelli, 2012). Factors that increase the risk of HIV/STI among Latinas in the United States include low socioeconomic status, intimate partner violence, lack of knowledge of HIV, substance abuse, high reported concurrency among partners, and lack of awareness of their partner’s status (Adimora, Schoenbach, & Doherty, 2007; Campbell et al., 2008; CDC, 2013b; El-Sadr, Mayer, & Hodder, 2010; Hodder et al., 2010; Peragallo et al., 2012; Sareen, Pagura, & Grant, 2009). Cultural values and gender norms among Latinos, including those living the United States, have been shown to place Latinas at further risk of HIV/STI through a lack of empowerment, difficulty in negotiating condom use, and delayed testing and diagnosis (Cianelli, Ferrer, & McElmurry, 2008; Davila, 2005; Davila, Bonilla, Gonzalez-Ramirez, & Villarruel, 2007; Gonzalez-Guarda, Peragallo, Urrutia, Vasquez, & Mitrani, 2008; Hernandez, 2011; Moreno, 2007; Peragallo, 1996; Sowell, Holtz, & Velasquez, 2008).
Despite the potential for disease prevention, Latinas have been shown to be reluctant to discuss condom use with their partners (Deren, Shedlin, Decena, & Mino, 2005). Behavioral interventions aimed at increasing condom use among Latinas, therefore, have the potential for a substantial decrease in risk of HIV/STI acquisition.
The proposed mechanism of these behavioral interventions is primarily through culturally targeted interventions aimed at increasing partner communication, self-efficacy of condom use, HIV-related knowledge, knowledge of perceived barriers, and perceived HIV risk (Peragallo et al., 2012). There are several existing behavioral interventions designed for women, often Latina women in particular, that aim to increase the self-efficacy of condom use in an effort to decrease incident HIV/STIs (CDC, 2013a).
Meta-analyses on the effects of behavioral interventions on increasing condom use found that, in general, behavioral interventions increased condom use and decreased incident cases of HIV/STIs (Mize, Robinson, Bockting, & Scheltema, 2002; Scott-Sheldon, Huedo-Medina, Warren, Johnson, & Carey, 2011). Scott-Sheldon et al. (2011) and Mize et al. (2002) found that behavioral interventions seemed to be more effective in Latinos than other ethnic subgroups; however, only Mize et al. examined the effects of interventions targeted at women, including Latinas. Additionally, other reviews have found that behavioral interventions are more effective among Latinos if specific cultural needs are addressed in the intervention (Albarracin, Albarracin, & Durantini, 2008; Cardoza, Documet, Fryer, Gold, & Butler, 2012; Russell, Alexander, & Corbo, 2000).
Since these meta-analyses were published, several randomized control trials of behavioral interventions to increase condom use among Latina women have been published (Fisher et al., 2011; Peragallo et al., 2012; Wingood et al., 2011). Although prior meta-analyses have found that interventions appear to be efficacious among Latinos, no meta-analysis has focused specifically on the high-risk subgroup of Latina women. Given that recent studies focusing on this population have not been included in prior meta-analyses, this meta-analysis expands on previous work and provides a detailed examination of the literature and interventions targeted at Latinas. The purpose of this study was to investigate the efficacy of behavioral interventions aimed at promoting condom use and decreasing risky sexual behavior among Latinas in the United States through a meta-analysis of randomized controlled trials. The efficacy of behavioral interventions in reducing STI incidence was also assessed as a secondary outcome.
Method
Data Sources and Search Strategy
A comprehensive search of the literature using the MEDLINE, PsychInfo, and EMBASE databases (January 1950 through July 2013) and the National Institutes of Health (NIH) clinical trial registry (clinicaltrials.gov) was performed. Each database was searched using relevant medical subject headings and all fields keyword expansions of “behavioral intervention” AND “trial” AND (“condom use” OR “Sexually transmitted infections”) using search limits of “human” and “female.” The complete MEDLINE search can be found in the supplementary material (available online at http://heb.sagepub.com/supplemental). The search was not restricted by language, although all articles that met the inclusion criteria were published in English. Citations for conference abstracts, dissertations, and other potentially relevant literature were included in the search. References from retrieved articles and previous meta-analyses were checked for additional studies that met the inclusion criteria.
Study Selection
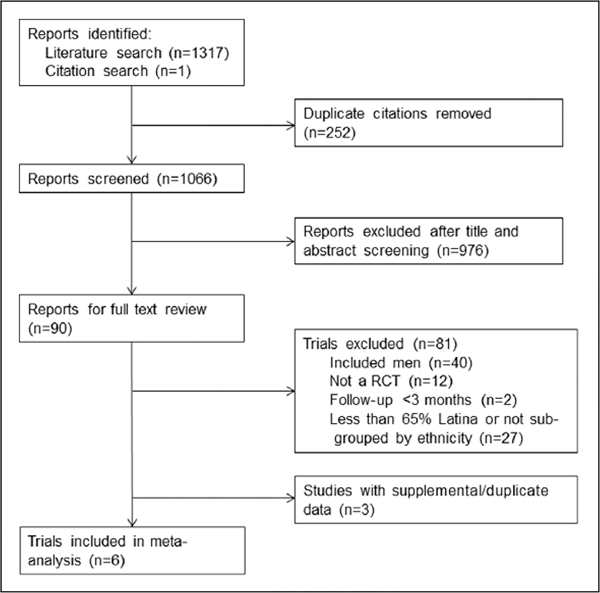
Two study investigators (MA, CG) independently screened 1,066 titles and abstracts and selected 90 articles for full-text review. Any disagreement between the investigators was resolved by consensus through a discussion of the article in question. The full text of the remaining 90 articles was reviewed by investigators (JH, LW), and disagreement was resolved by a third investigator (CG). Articles that met the following inclusion criteria were included in the meta-analysis: (a) intervention targeted to women, (b) randomized control trial, (c) intervention was behavioral in nature, (d) reported an outcome of condom use and/or STI acquisition, (e) follow-up ≥3 months, (f) the control group received standard of care or minimal intervention, (g) the study population was at least 65% Latina or results were stratified by race/ethnicity, (h) study was conducted in the U.S. noninstitutionalized population, and (i) study reported effect size and variance or the information needed to calculate summary measures. The inclusion criterion of 65% or more Latina in the study population cutoff was selected to be consistent with a previous meta-analysis on behavioral interventions in Latinos (Herbst et al., 2007). Figure 1 details the study selection process.
Figure 1.
Selection of studies for inclusion in the meta-analysis.
Data Collection
Data were extracted from the six articles that met the inclusion criteria by two investigators (DR, LW) independently and in duplicate using a standardized data collection form (attached in supplemental materials). The reviewers abstracted data on intervention type, duration, and content. The reviews also obtained data necessary to assess the quality of each trial, including randomization, blinding, clarity of eligibility criteria, adherence to the intervention, loss to follow-up, method used to obtain self-reported data, use of intention-to-treat analysis, and length of the recall period.
Reviewers collected data on the outcomes of interest: condom use, risky sex, and incident STI. They also recorded the study definition for each outcome and, if relevant, whether the effect measures were adjusted and unadjusted for confounders. Potential modifiers and mediators, including study population, baseline STI risk, mean age, socioeconomic status of participants, and length of the intervention were also collected. Any disagreement between the two investigators was resolved by a third reviewer (MA).
Data Analysis
Multiple measures of condom use were reported in the included studies necessitating the combination of related condom-use measures for meta-analysis. The primary outcome of interest was designated risky sexual behavior and included the following outcomes: never used condoms, inconsistent condom use, and noncompliance (sex with an untreated or incompletely treated partner after treatment for an STI). Respondents reporting any of these outcomes were coded as having risky sexual behavior in a dichotomous risky versus nonrisky sexual behavior variable. The secondary outcome of interest, incident STI, was created from the following reported measures: incident nonviral STI (Shain et al., 2004), incident chlamydia infection (Peragallo et al., 2012), and incident chlamydia or gonorrhea infection (Shain et al., 1999).
In studies where outcomes were measured at more than one follow-up time point (Peragallo et al., 2005; Peragallo et al., 2012; Shain et al., 1999; Shain et al., 2004; Wingood et al., 2011), the longest follow-up time was selected for the primary outcome analysis because it was felt to best represent sustained intervention effect. One study (Wingood et al., 2011) also reported multiple recall periods for behavioral outcomes at each of the follow-up time points. The shortest recall period was used for the analysis in an effort to select the measure with the least misclassification possible.
A sensitivity analysis based on follow-up time was planned a priori to see whether there was evidence of sustained effects of the intervention. Quality parameters were investigated through a posteriori sensitivity analyses of studies using blinding and by analyzing studies using intention-to-treat analysis to see if different effect sizes were estimated in these groupings of presumably higher quality studies. Additional a posteriori sensitivity analyses were conducted to examine substitution of alternate risky sexual behavior measures as well as to recall periods and year of publication, in order to determine whether outcome definition heterogeneity or extended recall time changed the results. A sensitivity analysis by study retention was considered but rejected because of the narrow range of participant retention in selected studies.
Estimates are reported as odds ratios (ORs) and as Cohen’s d standardized mean differences. The OR was selected for its ease in interpretability; however, because of heterogeneity in the outcome variables, Cohen’s d standardized mean differences are also presented. Wingood et al. (2011) reported adjusted OR in addition to unadjusted estimates. The adjusted OR was used for the meta-analysis. The OR for risky sex was either reported directly in the article or calculated using aggregate data on the number of participants in each group who reported the risky sex outcome at longest follow-up. The standard error was calculated using reported confidence intervals or from the same data used to calculate OR. Cohen’s d was calculated either from rate data or was converted from the OR, when rate data were not reported in the article (Sanchez-Meca, Marin-Martinez, & Chacon-Moscoso, 2003).
The natural log of the OR and standard error were used to pool the estimates using fixed effects and DerSermonian and Laird random effects models with inverse variance weighting. Heterogeneity was assessed using the Cochrane’s Q test and the I-squared statistic. A cut point of p < .10 was used to determine if significant herterogeneity was present. The random effects models are presented because the results are a more conservative estimate of the standard error.
The following subgroup analyses were preplanned: (a) interventions targeted specifically for Latinas and (b) baseline HIV/STI status preintervention. These subgroups were chosen because we hypothesize that interventions targeted to Latinas will more effective in this population than general interventions for women. We also believe that women with a previous STI at baseline are a higher risk population than women without an STI and therefore the effects of the intervention may differ between these two risk groups.
Publication bias was assessed using a funnel plot and the Begg and Egger tests with p-values cut point set at .10. This cut point was selected to minimize the potential for Type II error when assessing publication bias. Study quality was assessed using a checklist adapted to fit the needs of this meta-analysis (Jadad, Moher, & Klassen, 1998; Verhagen et al., 1998). All analyses were performed using Stata 11.2 (StataCorp, College Station, TX).
Results
The results from the search strategy and study selection are detailed in Figure 1. A total of six studies met the eligibility criteria for inclusion (Peragallo et al., 2005; Peragallo et al., 2012; Shain et al., 1999; Shain et al., 2004; Suarez-Al-Adam, Raffaelli, & O’Leary, 2000; Wingood et al., 2011). One study was found by searching the references of articles selected for full-text review (Suarez-Al-Adam et al., 2000).
Study Characteristics
Study characteristics are reported in Table 1. The total number of participants was 2,909, and the number of participants in the individual studies ranged from 60 to 775. The longest follow-up postintervention ranged from 3 months to 2 years. The studies by Peragallo et al. used the same intervention in different populations (Peragallo et al., 2005; Peragallo et al., 2011) and the studies by Shain et al. used the same intervention; however, an additional enhanced group was added as a separate intervention group in the 2004 study (Shain et al., 2004). The enhanced intervention group was given the same intervention as the standard group plus extra optional sessions. Participants in the standard and enhanced intervention group were combined and compared with the control group for this analysis.
Table 1.
Study Characteristics.
| Study | Year | N | Age (Mean ± SD) | Latina (%) | SES (%) | Education (Mean ± SD) | Study Population | Intervention Name | Intervention Description | Length of Intervention | Control Group | Outcome | Maximum Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peragallo | 2005 | 657 | ― | 100 | 70.5%a | 48.2%b | Community; Sexually active without condom use | SEPA | “Culturally tailored sessions on understanding their bodies, HIV/AIDS and STDs, condoms (myths and use), negotiating safer sex practices, violence prevention, and partner communication,” “Skills training . . . role-playing . . . consistent with Latinas’ values and beliefs” | 3+ sessions | HIV test counseling | Condom use: always (95% to 100%) versus inconsistent (0% to 95%) | 6 months |
| Peragallo | 2012 | 548 | 38.5 ± 8.5 | 100 | 69.5%c | 13.4 ±3.45 | Community; Sexually active | SEPA | “Culturally specific and theoretically based group intervention for Hispanic women . . . hands on activities, role playing . . . skills demonstration, homework to build self-efficacy and direct provision of information” | 5 sessions | One session intervention at month 12 | Any condom use; Chlamydia infection | 12 months |
| Shain | 1999 | 775 | 21.6 ± 0.43 | 69 | $254.5 ±$l7.7e | 10.8 ±0.11 | Clinic; Previous STI infection | Project SAFE | “A sex and culture-specific behavioral intervention . . . adapted [the] AIDS Risk Reduction Model . . . lively and open discussions, games, videotape watching, behavior modeling and role play. Learning was personalized” | 3 sessions | Standard STI counseling | Compliance; Five or more unprotected sexual acts; Chlamydia or gonorrhea infection | 24 months |
| Shain | 2004 | 617 | 21.0 ± 0.61 | 76 | $302.9 ±$23.7e | 10.7 ±0.18 | Clinic; Previous STI infection | Project SAFE 2 | Same intervention as described in Shain, 1999 | 3 sessions | Standard STI counseling | Compliance; Nonviral STI | 12 months |
| Suarez | 2000 | 60 | 34.5 | 100 | ― | 46.0%b | Community; Sexually active without condom use | ― | “Based on social cognitive theory . . . providing information and building skills to promote safer sex ... 3 weeks” | 7 sessions | Health-promotion also lasting 3 weeks | Safer sex (using condoms for all sex acts or abstaining from | 6 months |
| Wingood | 2011 | 252 | 30.3 ± 6.9 | 100 | 54.8%d | 43.8%b | Community; Sexually active | AMIGAS | “A culturally congruent HIV prevention intervention for Latin women . . . [focused on] healthy relationships, cultural and gender pride . . . video testimonials of Latina women who were living with HIV . . . explore how experiences affect risk . . . role-playing” | 4 sessions | 1 -session health intervention | Never used condoms; Consistent condom use (use of condoms for all sexual acts) | 6 months |
Note. Suarez et al. did not report the SD for age. SES = socioeconomic status; STD = sexually transmitted disease; STI = sexually transmitted infection.
At or below 100% of the poverty line.
Percentage less than high school.
Monthly income <$2,000.
On public assistance.
Mean monthly per capita income.
Although the specific interventions varied between studies, all of the interventions focused on increasing awareness of HIV/STI transmission and teaching skills in negotiating condom use. The number of sessions per intervention ranged from three to seven. The interventions of the included trials were designed to be culturally appropriate for the Latina participants with the exception of the Suarez-Al-Adam et al. (2000) study. A sensitivity analysis was performed without the Suarez-Al-Adam et al. study, and the results of the meta-analysis remained unchanged. The Shain et al. (1999, 2004) trials were conducted in public clinics with participants that were diagnosed with a nonviral STI at baseline. The study populations of the other included trials were recruited from communities. The differences in the community-based versus clinic-based populations were the basis for our subgroup analysis.
There was little heterogeneity among the potential modifiers and mediators of intervention efficacy, which, in combination with the small sample size, limited the ability to detect which factors may be important to the success of the intervention.
Pooled Effects
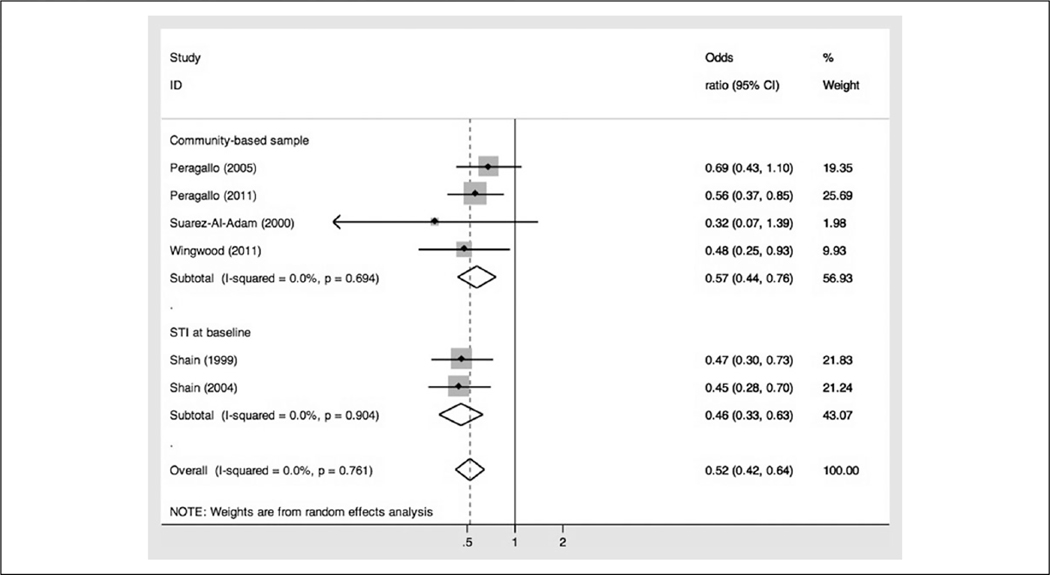
Individually, each study found a protective effect of the behavioral intervention on risky sex. However, the point estimates were varied, and some studies did not have statistically significant findings. The pooled effect showed little heterogeneity (I-squared = 0.0%) and the pooled OR and 95% confidence interval using random effects modeling was 0.52 (0.42, 0.64) for all included trials (Figure 2). Both subgroups, STI at baseline and no STI at baseline, had statistically significant protective effects against risky sex (Figure 2). The STI at baseline group had a slightly more protective effect than the community-based group with an OR of 0.46 (0.33, 0.63) and 0.57 (0.44, 0.76), respectively. The pooled Cohen’s d was 0.36 (0.25, 0.47), indicating a moderate difference in risky sexual behavior between groups.
Figure 2.
The effect of behavioral interventions on risky sex.
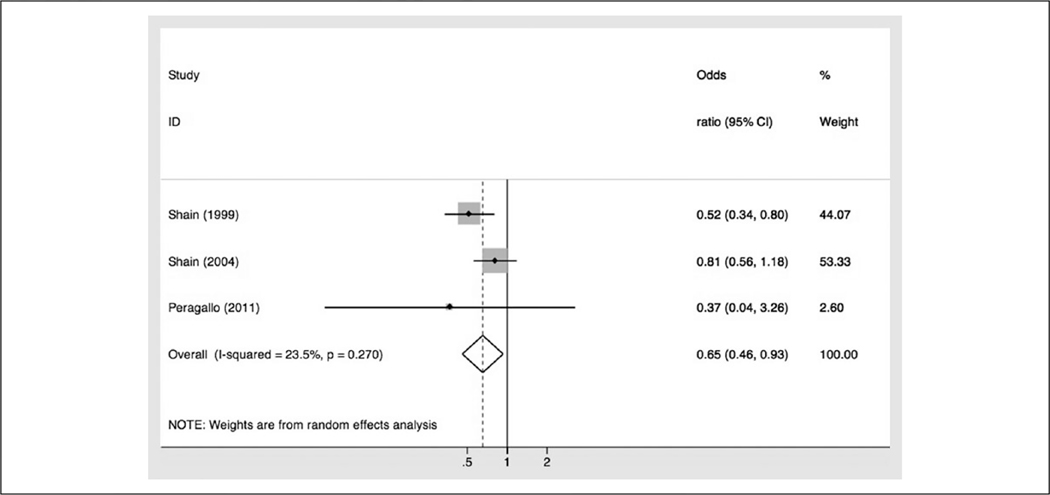
Three studies measured nonviral STI incidence during the follow-up period (Peragallo et al., 2012; Shain et al., 1999; Shain et al., 2004). The two Shain et al. studies were appropriately powered to detect a difference in STI incidence between the intervention and control groups. The Peragallo et al. study from 2011 also assessed incident STI; however, they were underpowered to detect an effect of the behavioral intervention on STI acquisition. The pooled random effects model showed a protective effect with an OR of 0.65 (0.46, 0.93) (Figure 3). There was some heterogeneity (I-squared = 23.5% [0.0% to 65.0%]), which informed the decision to use the random effects model. The pooled Cohen’s d was 0.24 (0.02, 0.47), indicating a small difference between STI acquisition between the intervention and control group.
Figure 3.
Behavioral interventions on incident sexually transmitted infections.
Quality of Studies and Risk of Bias
Among the included studies, all had adequate randomization methods, clearly stated eligibility criteria, and descriptions of losses and exclusions. Although studies had relatively high retention (ranging from 69.1% to 91.2%), only two used intention-to-treat analysis. Three studies (50%) did not use any blinding of participants or assessors. Quality measures for each study are described in Table 2.
Table 2.
Quality Assessment of Studies.
| Study | Blinding | Adequate Randomization | Intention to Treat Analysis | Eligibility Criteria Clearly Specified | Power Calculations Described | Longest Follow-Up Time (Months) | Recall for Self-Reported Outcomes (Months) | Study Retention (%) | Description of Losses and Exclusions |
|---|---|---|---|---|---|---|---|---|---|
| Peragallo et al. (2005) | No | Yes | No | Yes | Yes | 6 | 3 | 69.1 | Yes |
| Peragallo et al. (2012) | No | Yes | Yes | Yes | Yes | 12 | 3 | 69.5 | Yes |
| Shain et al. (1999) | Single | Yes | No | Yes | No | 12 | 12 | 89.0a | Yes |
| Shain et al. (2004) | Single | Yes | No | Yes | No | 24 | 12 | 91.2a | Yes |
| Suarez-Al-Adam et al. (2000) | No | Yes | No | Yes | No | 3 | 1 | 76.6 | Yes |
| Wingood et al. (2011) | Double | Yes | Yes | Yes | No | 6 | 1.3 | 88.9 | Yes |
Analysis on behavioral outcome used only participants with high compliance.
Sensitivity analyses were performed to assess the robustness of our findings with respect to outcome variable selection and relevant quality measures (Table 3). None of the sensitivity analyses had results that varied significantly from the pooled effect measure.
Table 3.
Sensitivity Analyses.
| Number of Studies | Pooled OR (95% CI) | Heterogeneity: p Value of Q Statistic | |
|---|---|---|---|
| Intention to treat analysis | 2 | 0.54 (0.38, 0.77) | .682 |
| Only follow-up ≥1 year | 3 | 0.49 (0.38, 0.64) | .721 |
| Studies published in the past 10 years | 4 | 0.55 (0.43, 0.69) | .616 |
| Interventions designed for Latinas | 5 | 0.53 (0.43, 0.65) | .706 |
| Shain et al. (1999) outcome: ≥5 unprotected sex acts | 6 | 0.55 (0.45, 0.68) | .779 |
| Wingood: 90-day recall | 6 | 0.53 (0.43, 0.65) | .769 |
| Wingood: Inconsistent condom use, 30-day recall | 6 | 0.50 (0.41, 0.62) | .449 |
| Wingood: Inconsistent condom use, 90-day recall | 6 | 0.47 (0.36, 0.63) | .160 |
| Pooled | 6 | 0.52 (0.42, 0.64) | .761 |
Note. OR = odds ratio; CI = confidence interval.
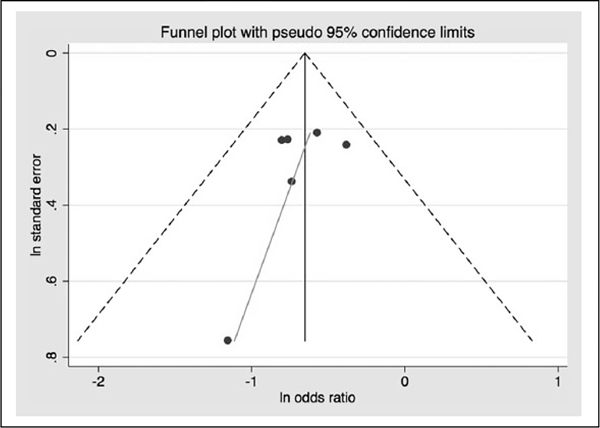
Publication bias was assessed using a funnel plot and the Begg and Egger’s tests. The funnel plot (Figure 4) shows little evidence of publication bias. Similarly, the Begg and Egger’s tests had nonsignificant p values, .707 and .403, respectively. Although the statistical findings were nonsignificant, the Begg and Egger’s tests are underpowered to detect publication bias since only six studies are included in the meta-analysis.
Figure 4.
Funnel plot.
Discussion
This meta-analysis aimed to determine the impact of behavioral interventions targeted at reducing sexual risk factors and STIs among Latina women living in the United States. We found that women in the behavioral intervention groups were less likely to engage in risky sexual behavior and less likely to acquire a nonbacterial STI than those in the standard of care groups.
Our results are consistent with findings from other meta-analyses on behavioral interventions to reduce risky sexual behaviors that included studies intervening on both genders and multiple ethnic groups in the United States (Albarracin et al., 2008; Cardoza et al., 2012; Crepaz et al., 2007; Crepaz et al., 2009; Herbst et al., 2007; Huedo-Medina et al., 2010; Mize et al., 2002; Neumann et al., 2002; Noar, 2008; Russell et al., 2000; Scott-Sheldon et al., 2011). Our findings are consistent with a 2007 systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics by Herbst et al. (2007). Herbst et al. reported a 31% reduced odds of acquiring an incident STI and a 25% reduced odds of displaying risky sexual behavior, which is similar to results obtained in this meta-analysis. Another more recent meta-analysis from 2011 demonstrated the efficacy of behavioral interventions to increase condom use and reduce STIs within a wide range of populations (Scott-Sheldon et al., 2011), and it further suggested that interventions were more successful in HIV reduction in samples with a greater proportion of Latino participants. These findings are concordant with Mize et al.’s 2002 meta-analysis that found that interventions to increase risk reduction behaviors were more effective among Latina samples compared with other ethnicities.
Latina women have been shown to face unique cultural challenges in negotiating condom use with their partner (Cianelli et al., 2008; Gonzalez-Guarda et al., 2008; Hernandez, 2011; Moreno, 2007; Peragallo, 1996; Sowell et al., 2008), which reinforces the importance of interventions that address these culture- and gender-specific issues. Five of the six trials included in this meta-analysis used ethnographic data from Latinas to inform their interventions so that they addressed the appropriate cultural context within which sexual decision making takes place (Peragallo et al., 2005; Peragallo et al., 2012; Shain et al., 1999; Shain et al., 2004; Wingood et al., 2011). When we restricted our analysis to the five studies using interventions targeting Latinas, the resulting protective OR was very similar to our overall results.
Prior research has indicated that interventions are more successful in lowering incident STIs in participants with a baseline STI diagnosis but are not more successful in improving sexual risk behaviors in participants with a baseline STI diagnosis (Scott-Sheldon et al., 2011). Our subgroup analysis by STI status at baseline showed that effect sizes and confidence intervals for risky sexual behavior were quite similar between the subgroups, suggesting that there was not a difference in effect sizes, which is consistent with existing literature. We did not perform a statistical test for significance between subgroups by STI status at baseline for the outcome of risky sexual behavior because of the small number of studies in this subgroup analysis. Since only three studies reported STI outcomes, we were not able to examine a similar relationship for the STI outcome.
We did not find a dose–response effect with respect to the number of sessions for each intervention; however, we were likely underpowered to detect a dose–response relationship. The number of sessions ranged from three to seven, and there does not appear to be an increased protective effect from the longer interventions. Determining the optimal length and most efficacious content of interventions was out of the scope of this meta-analysis, but it is an important area of research before any widespread implementation of behavioral interventions.
Our study findings should be interpreted in light of limitations of the underlying literature. The individual studies may suffer from social desirability bias. It is possible that women assigned to the intervention group feel more obligated to report a decrease in risky sexual behavior than participants in the control group. This differential misclassification would bias the results away from the null, creating an exaggerated effect measure. Social desirability bias was minimized in the Wingood et al. study through the use of audio-computer assisted self-interviewing (ACASI; Wingood et al., 2011). ACASI has been shown to elicit more accurate responses from participants, decreasing social desirability bias (Kissinger et al., 1999). Although the studies included in this meta-analysis likely suffer from social desirability bias to some extent, the biological data on incident STI provided an objective measure that supports the primary finding that behavioral interventions reduce risky sex behaviors. We found a decrease in incident STI among those in the intervention groups. Presumably, this means that these women increased condom use and decreased other risky sexual practices, which provides evidence that, despite potential social desirability bias, behavioral interventions decrease risky sexual behavior.
We originally aimed to assess increase in condom use as our primary outcome but the wide variability in the definition of condom use made it challenging to create a consistent condom use variable for analysis. Similarly, there was variability in the length of follow-up of the studies. The follow-up period ranged from 3 months to 2 years. Assessing the long-term sustainability of the behavioral intervention is vital to predicting the effects of the intervention on HIV/STI prevention. A sensitivity analysis found a similar protective effect of behavioral interventions when using only follow-up greater than or equal to 1 year; therefore, we can conclude that the effects of the intervention appear to be sustainable for at least 1 year following the completion of the intervention.
Of note, only two studies correctly used intention-to-treat analysis for assessment of the behavioral intervention. The other studies analyzed only the women who attended all of the intervention sessions, which may result in an overestimation of the protective effect of the intervention.
Finally, the use of an odds ratio as opposed to a risk ratio likely overestimates the protective effect of the behavioral interventions. Since the protective effect was large and the upper bounds of the confidence interval did not approach the null, there would still likely be a significant protective effect of behavioral interventions had we been able to use a risk ratio as our effect estimate.
Despite these limitations, this is the first meta-analysis, to our knowledge, that evaluated the effect of behavioral interventions aimed at reducing risky sex behaviors in the Latina population in the United States. Latinos currently represent 17% of the U.S. population, and it is estimated that their population will increase to nearly one third of the U.S. population by 2060 (U.S. Census Bureau, 2012). Given that HIV/STIs disproportionately affect Latinas and that their population is expected to grow significantly, it is imperative that evidence-based efforts be made to decrease the risk of HIV/STI in this population. Additionally, this population is important to study as they have unique challenges in negotiating condom use and decreasing their risk of HIV/STI acquisition. Our findings support the implementation of culturally specific behavioral interventions aimed at reducing the risk of HIV/STI transmission in Latina populations.
The effect measures from the individual studies were relatively similar, which contributed to the low heterogeneity among included studies. Despite the low heterogeneity, we chose to use random effects modeling and still found highly statistically significant findings. We performed numerous sensitivity analyses, none of which showed a substantial change in effect estimate or confidence interval width compared with the pooled estimate. This speaks of the robustness of our findings with respect to the selection of the outcome variables.
Conclusions
We conclude that behavioral interventions targeted to address the challenges of preventing STIs in Latina populations in the United States successfully reduce risky sexual behaviors and incidence STIs. The protective effects have been shown to persist for as long as 2 years following the intervention and are of near equal magnitude regardless of whether the intervention is implemented in women with STI at baseline or community-based populations, indicating that these interventions may be useful in a variety of settings. Prevention of HIV/STI in Latina populations is important, especially as this population continues to grow in the United States. The SEPA intervention from the Peragallo et al. (2005, 2012) studies and the AMIGAS intervention from the Wingood et al. (2011) study are endorsed by the Centers for Disease Control and Prevention and the Miami-Dade County Health Department, respectively, and are available options for public health practitioners to implement. These behavioral interventions, among others, were efficacious in reducing the odds of risky sexual behavior and STI acquisition among Latinas.
Supplementary Material
Acknowledgments
We would like to thank Dr. Tanika Kelly for her guidance and feedback.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: National Institutes of Health (NIH)/National Institute on Drug Abuse (NIDA) Ruth L. Kirschstein National Research Service Award (F30DA033729) provided stipend and tuition support for Meghan Althoff while completing an MD/PhD dual degree. NIH/NIDA Interdisciplinary Research Training Institute on Hispanic Drug Abuse (R25DA026401) provided mentorship and training on drug abuse research to Meghan Althoff. NIH/NIDA R21DA030269 provided funding to Patricia Kissinger to conduct HIV/STI research among the Latino migrant population in New Orleans.
Footnotes
Authors’ Note
The views expressed in this article are the authors’ own and do not reflect the views of the National Institutes of Health, the funding agency.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplementary Material
The supplementary material for this article is available online at http://heb.sagepub.com/supplemental.
References
- Adimora AA, Schoenbach VJ, & Doherty IA (2007). Concurrent sexual partnerships among men in the United States. American Journal of Public Health, 97, 2230–2237. doi: 10.2105/AJPH.2006.099069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracin J, Albarracin D, & Durantini M (2008). Effects of HIV-prevention interventions for samples with higher and lower percents of Latinos and Latin Americans: A meta-analysis of change in condom use and knowledge. AIDS and Behavior, 12, 521–543. doi: 10.1007/s10461-007-9209-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, & Wagman J (2008). The intersection of intimate partner violence against women and HIV/AIDS: A review. International Journal of Injury Control and Safety Promotion, 15, 221–231. doi: 10.1080/17457300802423224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoza VJ, Documet PI, Fryer CS, Gold MA, & Butler J 3rd. (2012). Sexual health behavior interventions for U.S. Latino adolescents: A systematic review of the literature. Journal of Pediatrric and Adolescenct Gynecology, 25, 136–149. doi: 10.1016/j.jpag.2011.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2011). HIV among Latinos (HIV/AIDS Fact Sheets). Atlanta, GA: Author. [Google Scholar]
- Centers for Disease Control and Prevention. (2012). Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012, 17(4). [Google Scholar]
- Centers for Disease Control and Prevention. (2013a). Complete listing of risk reduction evidence-based behavioral interventions (Compendium of Evidence-Based HIV Behavioral Interventions). Atlanta, GA: Author. [Google Scholar]
- Centers for Disease Control and Prevention. (2013b). HIV among women (HIV/AIDS Fact Sheets). Atlanta, GA: Author. [Google Scholar]
- Cianelli R, Ferrer L, & McElmurry BJ (2008). HIV prevention and low-income Chilean women: Machismo, marianismo and HIV misconceptions. Culture, Health and Sexuality, 10, 297–306. doi: 10.1080/13691050701861439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Horn AK, Rama SM, Griffin T, Deluca JB, Mullins MM, & Aral SO (2007). The efficacy of behavioral interventions in reducing HIV risk sex behaviors and incident sexually transmitted disease in Black and Hispanic sexually transmitted disease clinic patients in the United States: A meta-analytic review. Sexually Transmitted Diseases, 34, 319–332. doi: 10.1097/01.olq.0000240342.12960.73 [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marshall KJ, Aupont LW, Jacobs ED, Mizuno Y, Kay LS, . . . O’Leary A (2009). The efficacy of HIV/ STI behavioral interventions for African American females in the United States: A meta-analysis. American Journal of Public Health, 99, 2069–2078. doi: 10.2105/ajph.2008.139519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davila YR (2005). The social construction and conceptualization of sexual health among Mexican American women. Research and Theory for Nursing Practice, 19, 357–368. [DOI] [PubMed] [Google Scholar]
- Davila YR, Bonilla E, Gonzalez-Ramirez D, & Villarruel A (2007). HIV-IPV prevention: Perceptions of what Latinas want and need. Hispanic Health Care International, 5, 101–108. doi: 10.1891/1540-4153.5.3.101 [DOI] [Google Scholar]
- Deren S, Shedlin M, Decena CU, & Mino M (2005). Research challenges to the study of HIV/AIDS among migrant and immigrant Hispanic populations in the United States. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 82, iii13–iii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sadr WM, Mayer KH, & Hodder SL (2010). AIDS in America—Forgotten but not gone. New England Journal of Medicine, 362, 967–970. doi: 10.1056/NEJMp1000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher HH, Patel-Larson A, Green K, Shapatava E, Uhl G, Kalayil EJ, . . . Chen B (2011). Evaluation of an HIV prevention intervention for African Americans and Hispanics: Findings from the VOICES/VOCES community-based organization behavioral outcomes project. AIDS and Behavior, 15, 1691–1706. doi: 10.1007/s10461-011-9961-7 [DOI] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM, Peragallo N, Urrutia MT, Vasquez EP, & Mitrani VB (2008). HIV risks, substance abuse, and intimate partner violence among Hispanic women and their intimate partners. Journal of the Association of Nurses in AIDS Care: JANAC, 19, 252–266. doi: 10.1016/j.jana.2008.04.001 [DOI] [PubMed] [Google Scholar]
- Herbst JH, Kay LS, Passin WF, Lyles CM, Crepaz N, & Marin BV (2007). A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS and Behavior, 11, 25–47. doi: 10.1007/s10461-006-9151-1 [DOI] [PubMed] [Google Scholar]
- Hernandez CM (2011). HIV/AIDS in childbearing Hispanic/Latinas: An emerging crisis. MCN. American Journal of Maternal Child Nursing, 36, 354–358. doi: 10.1097/NMC.0b013e31822d67aa [DOI] [PubMed] [Google Scholar]
- Hodder SL, Justman J, Haley DF, Adimora AA, Fogel CI, Golin CE, . . . El-Sadr WM (2010). Challenges of a hidden epidemic: HIV prevention among women in the United States. Journal of Acquired Immune Deficiency Syndromes, 55, S69–S73. doi: 10.1097/QAI.0b013e3181fbbdf9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huedo-Medina TB, Boynton MH, Warren MR, Lacroix JM, Carey MP, & Johnson BT (2010). Efficacy of HIV prevention interventions in Latin American and Caribbean nations, 1995–2008: A meta-analysis. AIDS and Behavior, 14, 1237–1251. doi: 10.1007/s10461-010-9763-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Moher D, & Klassen TP (1998). Guides for reading and interpreting systematic reviews: II. How did the authors find the studies and assess their quality? Archives of Pediatrics & Adolescent Medicine, 152, 812–817. [DOI] [PubMed] [Google Scholar]
- Kissinger P, Rice J, Farley T, Trim S, Jewitt K, Margavio V, & Martin DH (1999). Application of computer-assisted interviews to sexual behavior research. American Journal of Epidemiology, 149, 950–954. [DOI] [PubMed] [Google Scholar]
- Mize SJ, Robinson BE, Bockting WO, & Scheltema KE (2002). Meta-analysis of the effectiveness of HIV prevention interventions for women. AIDS Care, 14, 163–180. doi: 10.1080/09540120220104686 [DOI] [PubMed] [Google Scholar]
- Moreno CL (2007). The relationship between culture, gender, structural factors, abuse, trauma, and HIV/AIDS for Latinas. Qualitative Health Research, 17, 340–352. doi: 10.1177/1049732306297387 [DOI] [PubMed] [Google Scholar]
- Neumann MS, Johnson WD, Semaan S, Flores SA, Peersman G, Hedges LV, & Sogolow E (2002). Review and meta-analysis of HIV prevention intervention research for heterosexual adult populations in the United States. Journal of Acquired Immune Deficiency Syndromes, 30, S106–S117. [PubMed] [Google Scholar]
- Noar SM (2008). Behavioral interventions to reduce HIV-related sexual risk behavior: Review and synthesis of meta-analytic evidence. AIDS and Behavior, 12, 335–353. doi: 10.1007/s10461-007-9313-9 [DOI] [PubMed] [Google Scholar]
- Peragallo N (1996). Latino women and AIDS risk. Public Health Nursing, 13, 217–222. [DOI] [PubMed] [Google Scholar]
- Peragallo N, Deforge B, O’Campo P, Lee SM, Kim YJ, Cianelli R, & Ferrer L (2005). A randomized clinical trial of an HIV-risk-reduction intervention among low-income Latina women. Nursing Research, 54, 108–118. [DOI] [PubMed] [Google Scholar]
- Peragallo N, Gonzalez-Guarda RM, McCabe BE, & Cianelli R (2012). The Efficacy of an HIV risk reduction intervention for Hispanic women. AIDS and Behavior. 16, 1316–1326. doi: 10.1007/s10461-011-0052-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell LD, Alexander MK, & Corbo KF (2000). Developing culture-specific interventions for Latinas to reduce HIV high-risk behaviors. Journal of the Association of Nurses in AIDS Care: JANAC, 11, 70–76. [DOI] [PubMed] [Google Scholar]
- Sanchez-Meca J, Marin-Martinez F, & Chacon-Moscoso S (2003). Effect-size indices for dichotomized outcomes in meta-analysis. Psychological Methods, 8, 448–467. doi: 10.1037/1082-989x.8.4.448 [DOI] [PubMed] [Google Scholar]
- Sareen J, Pagura J, & Grant B (2009). Is intimate partner violence associated with HIV infection among women in the United States? General Hospital Psychiatry, 31, 274–278. doi: 10.1016/j.genhosppsych.2009.02.004 [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Huedo-Medina TB, Warren MR, Johnson BT, & Carey MP (2011). Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: A meta-analysis, 1991 to 2010. Journal of Acquired Immune Deficiency Syndromes, 58, 489–498. doi: 10.1097/QAI.0b013e31823554d7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shain RN, Piper JM, Holden AE, Champion JD, Perdue ST, Korte JE, & Guerra FA (2004). Prevention of gonorrhea and chlamydia through behavioral intervention: Results of a two-year controlled randomized trial in minority women. Sexually Transmitted Diseases, 31, 401–408. [DOI] [PubMed] [Google Scholar]
- Shain RN, Piper JM, Newton ER, Perdue ST, Ramos R, Champion JD, & Guerra FA (1999). A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women. New England Journal of Medicine, 340, 93–100. doi: 10.1056/nejm199901143400203 [DOI] [PubMed] [Google Scholar]
- Sowell RL, Holtz CS, & Velasquez G (2008). HIV infection returning to Mexico with migrant workers: An exploratory study. Journal of the Association of Nurses in AIDS Care, 19, 267–282. doi: 10.1016/j.jana.2008.01.004 [DOI] [PubMed] [Google Scholar]
- Suarez-Al-Adam M, Raffaelli M, & O’Leary A (2000). Influence of abuse and partner hypermasculinity on the sexual behavior of Latinas. AIDS Education and Prevention, 12, 263–274. [PubMed] [Google Scholar]
- U.S. Census Bureau. (2012). 2012 National population projections. Washington, DC: Author. Retrieved from http://www.census.gov/population/projections/data/national/2012.html [Google Scholar]
- Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, & Knipschild PG (1998). The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology, 51, 1235–1241. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Villamizar K, Er DL, DeVarona M, Taveras J, . . . Jean R (2011). Efficacy of a health educator-delivered HIV prevention intervention for Latina women: A randomized controlled trial. American Journal of Public Health, 101, 2245–2252. doi: 10.2105/ajph.2011.300340 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.