Abstract
Choroidal osteoma is a rare, benign, osseous choristoma presenting as an orange-yellow, well-defined fundus mass. It presents unilaterally in most cases, has a predilection for the female sex, and favor a juxtapapillary location, becoming clinically manifest when it involves the macula. Almost 60% of eyes with osteoma may suffer significant visual loss. Choroidal osteomas can easily be mistaken for other conditions with similar presentations. We herein report two rare cases presentation of choroidal osteoma: a 74-year-old male with 2-year blurred vision in the right eye (RE) initially misdiagnosed with age-related macular degeneration received intravitreal injections and after a multimodal evaluation, following cataract surgery in RE, confirmed to be choroidal osteoma and a 19-year-old female with a history of choroidal hemangioma presented with blurred vision in her left eye (LE), with examination revealed an irregular orange-yellow lesion along the superotemporal arcade with serous macular detachment, later diagnosed as choroidal osteoma.
Keywords: choroidal osteoma, osseous choristoma, visual loss, case reports
Introduction
Choroidal osteoma is a rare, benign, osseous choristoma presenting as an orange-yellow, well-defined fundus mass.1 It presents unilaterally in most cases, has a predilection for the female sex, and favor a juxtapapillary location, becoming clinically manifest when it involves the macula.2 Almost 60% of eyes with osteoma may suffer significant visual loss.3 One of the principal causes is the development of choroidal neovascularization.4
Choroidal osteomas can easily be mistaken for other conditions with similar presentations. Studies have estimated that up to 90% of eye care practitioners initially miss the diagnosis of choroidal osteoma, likely due to its inclusion in the broad differential diagnosis of ocular tumors and ocular calcification.5 The diagnosis of choroidal osteoma is mainly clinical. Over time, ocular ultrasound (US) and optical coherence tomography (OCT) have been widely used for diagnosis and follow-up.6,7
Case Description
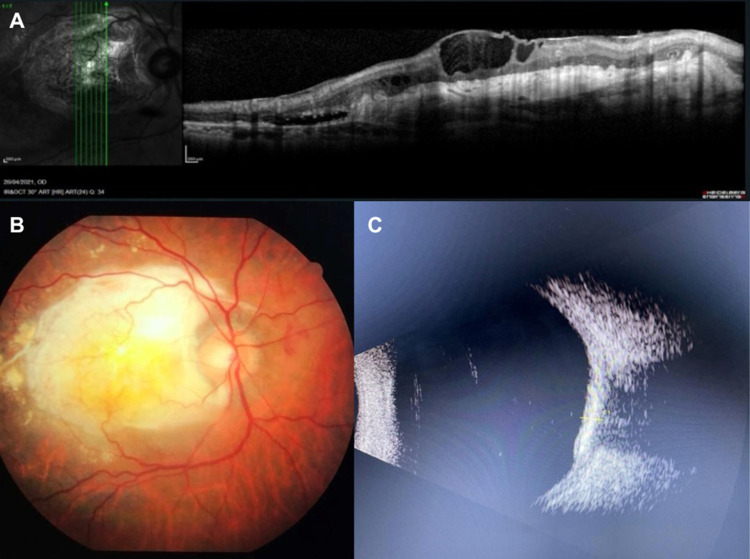
Case report 01: A 74-years old caucasian male with a 2 years history of blurred vision in the right eye (RE) was referred for evaluation and management of age-related macular degeneration after 4 intravitreal injections in other service. At presentation, best corrected visual acuity (BVCA) was counting fingers in his right eye (RE) and 20/40 in his left eye (LE). On slit-lamp exam nuclear cataract +2 and posterior subcapsular cataract +3 in his RE and nuclear cataract +2 in his OS. Fundus examination was normal in the left eye, while in the right eye revealed extensive macular white lesion. In addition to the indicated phacoemulsification with intraocular lens implantation in his RE, a multimodal evaluation was carried out with ultrasound, optical coherence tomography (OCT) and fluorescein angiography, which revealed that it was a choroidal osteoma (Figure 1). The presence of a choroidal osteoma explains the macular white lesion and is consistent with the imaging results.
Figure 1.
(A) Optical coherence tomography (OCT) showing subretinal fibrosis. (B) Retinography demonstrating choroidal osteoma. (C) Ocular ultrasound demonstrating high reflectivity lesion causing shadowing of posterior structures.
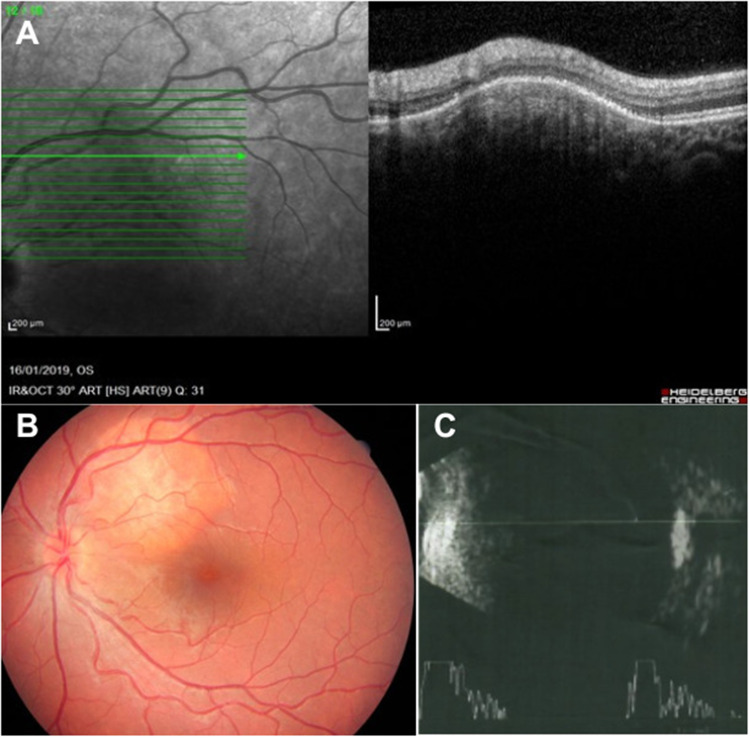
Case report 02: A 19-years old caucasian female with a 1 month history of blurred vision and metamorphopsia in the left eye (LE). Referred a diagnosis of choroidal hemangioma 2 years ago. At presentation, best corrected visual acuity (BVCA) was 20/20 in her right eye (RE) and 20/40 with metamorphopsia in her left eye (LE). The anterior segment examination was unremarkable in both eyes. Fundus examination was normal in the right eye, while in the left eye revealed an orange-yellow lesion, with not well-defined margins, extending from them disc along the superotemporal arcade up to the midperiphery sparing the macula.
The ultrasound examination demonstrated an area of high reflectivity on the ocular wall, causing posterior shadowing, suggestive of calcification. The OCT revealed hyperreflective lines in the choroid, photoreceptor atrophy and choroidal compression in the area corresponding to the lesion, with serous macular detachment (Figure 2). The diagnostic hypothesis was choroidal osteoma associated with serous macular detachment. The combination of imaging findings—particularly the OCT revealing hyperreflective lines, photoreceptor atrophy, and serous macular detachment—aligns with the known characteristics of choroidal osteomas. The presence of serous macular detachment further supports the diagnosis, as these lesions can induce retinal complications. The patient was treated with an intravitreal injection of Bevacizumab with improvement in vision and serous detachment.
Figure 2.
(A) Optical coherence tomography (OCT). (B) Retinography demonstrating choroidal osteoma. (C) Ocular ultrasound with low gain demonstrating calcification.
Conclusions
Choroidal osteoma is often confused with other lesions mainly with an atypical presentation. Therefore, a multimodal evaluation is important, especially with low-gain ultrasound for diagnostic confirmation. These cases illustrate the diverse presentations of choroidal osteoma and the necessity of a thorough multimodal evaluation for accurate diagnosis. By integrating ultrasound, OCT, and fluorescein angiography, clinicians can effectively differentiate choroidal osteoma from other similar lesions and provide appropriate management.
Funding Statement
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed Consent Statement
Written informed consent was obtained from the patient for the publication of this paper. Approval to publish the case details was not required in our institution.
Disclosure
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Papastefanou V, Pefkianaki M, Al Harby L, et al. Intravitreal bevacizumab monotherapy for choroidal neovascularisation secondary to choroidal osteoma. Eye. 2016;30:843–849. doi: 10.1038/eye.2016.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baum M, Pinkerton AR, Berler DK, Kramer KK. Choroidal osteomas. Ann Ophthalmol. 1979;11:1849–1851. [PubMed] [Google Scholar]
- 3.Aylward GW, Chang TS, Pautler SE, Gass JD. A long-term follow-up of choroidal osteoma. Arch Ophthalmol. 1998;116(10):1337–1341. doi: 10.1001/archopht.116.10.1337 [DOI] [PubMed] [Google Scholar]
- 4.Shields CL, Sun H, Demirci H, Shields JA. Factors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes with choroidal osteoma. Arch Ophthalmol. 2005;123(12):1658–1666. doi: 10.1001/archopht.123.12.1658 [DOI] [PubMed] [Google Scholar]
- 5.Alameddine RM, Mansour AM, Kahtani E, Salman A, Jaroudi M. Review of choroidal osteomas. Middle East Afr J Ophthalmol. 2014;21(3):244–250. doi: 10.4103/0974-9233.134686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olguin-Manríquez F, Enríquez AB, Crim N, et al. Multimodal imaging in choroidal osteoma. Int J Retina Vitreous. 2018;4:30. PMID: 30128167; PMCID: PMC6092861. doi: 10.1186/s40942-018-0132-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shields CL, Shields JA. Choroidal Osteoma. In: Albert D, Miller J, Azar D, Young LH, editors. Albert and Jakobiec’s Principles and Practice of Ophthalmology. Cham: Springer; 2021. doi: 10.1007/978-3-319-90495-5_261-1 [DOI] [Google Scholar]