Abstract
Patient: Male, 79-year-old
Final Diagnosis: COVID-19
Symptoms: Nephrotic syndrome
Clinical Procedure: —
Specialty: Hematology
Objective:
Unusual clinical course
Background:
Focal segmental glomerulosclerosis (FSGS) very rarely occurs in patients with multiple myeloma. Much more common are renal impairments secondary to monoclonal light-chain tubulopathy, AL amyloidosis, light-chain deposition disease, and the so-called monoclonal gammopathy of renal significance.
Case Report:
We report the case of a 79-year-old myeloma patient without noticeable medical problems but with a long history of myeloma treatment beginning 13 years ago. In the ninth line of therapy, he was successfully treated with belamaf mafodotin, an anti-BCMA monoclonal antibody coupled to monomethyl auristatin F. After 1.5 years of treatment, without any eye toxicity, and while he was in complete hematologic remission, he experienced a very severe COVID-19 infection followed 1 month later by a nephrotic syndrome. The renal biopsy revealed a FSGS not otherwise specified. He was successfully treated symptomatically. One and a half years later, and without treatment for 1 year, he is still in hematologic remission, with a remaining renal insufficiency.
Conclusions:
Our patient had a particularly long response to belamaf mafodotin of more than 2.5 years, which is still ongoing. This is particularly remarkable because the very unusual acute renal impairment was not myeloma related. This is a very rare case of FSGS in a myeloma patient, potentially linked to a COVID-19 infection considering the chronology of the events and the immunosuppressive status secondary to the malignancy and its treatment.
Key words: Multiple Myeloma, Segmental Glomerulosclerosis
Introduction
Multiple myeloma (MM) is the second most common hematologic malignancy in developed countries after chronic lymphocytic leukemia. It is a plasma cell neoplasm normally affecting elderly people, with a peak incidence at around 70 years of age. The disease usually starts with asymptomatic monoclonal gammopathy of undetermined significance (MGUS) [1] or smoldering myeloma [2], with initiating genetic abnormalities consisting of hyperdiploidy or immunoglobulin gene translocations [3], and progressively evolves into symptomatic MM with bone lesions, hypercalcemia, anemia, and renal insufficiency. Significant advances have been made in the treatment of MM with the arrival of proteasome inhibitors, immunomodulatory drugs (IMiDs), CD38-targeted therapy, and, more recently, anti-BCMA treatments [4], which have led to better response and survival. However, all patients systematically relapse and a cure remains elusive [5]. Renal impairment is always investigated and often already established at diagnosis. When faced with renal insufficiency during therapy for myeloma, it is essential to look first for relapse or progression of the myeloma, treatment-related factors (eg, bisphosphonate and thrombotic microangiopathy carfilzomib-related), infections, or so-called gammopathy of renal significance (MGRS) [6]. Other diseases, not myeloma-related, can also be the cause. We report the case of a patient treated with belantamab mafodotin who had MM in remission and presented an atypical nephrotic syndrome with focal segmental glomerulosclerosis (FSGS) not otherwise specified. The aim of the report is to discuss the cause (s) of FSGS.
Case Report
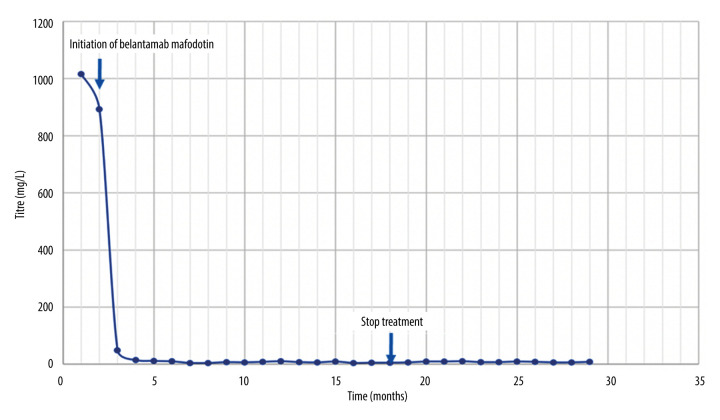
Our 79-year-old man of African ancestry, with a follow-up starting in 2011, was under treatment for IgG kappa MM and had a history of type 2 diabetes, arterial hypertension, and heart failure. He initially presented bone lesions and his blood tests showed a monoclonal spike of 34 g/L, an excess of kappa free light chains (FLC) (511 mg/L, normal: 3.3–19.4 mg/L), a normal creatinine level, tubular proteinuria (1 g/24 h, normal <0.15 g/d), and a medullary plasma cell count of 38%. The karyotype was not determined and the ISS score was 1. He received induction treatment with bortezomib and dexamethasone followed by a myeloablative dose of melphalan and autologous hematopoietic stem cell transplantation, leading to a very good partial response. Since then, many relapses have occurred and he has received many different lines of therapy to which he responded temporarily. Notably, he was treated with bortezomib and dexamethasone followed by maintenance therapy with bortezomib at first relapse in 2014. In 2015, he was treated with lenalidomide and dexamethasone and later in 2017 with daratumumab and bortezomib. In 2019, he had a short course of pomalidomide and began therapy with bendamustine and prednisone, but this was quickly replaced by carfilzomib and 1 year later by Selinexor in combination with bortezomib. Most of these treatments had some efficacy, resulting in remission lasting about 1 year on average. After using most of the available therapeutic arsenal, treatment with belantamab mafodotin was initiated in May 2021. Surprisingly, this monotherapy, administered intravenously at a dose of 2.5 mg/kg every 3 weeks, led to normalization of the patient’s clonal kappa light chain (the Ig phenotype had been switched to kappa light chain only), which decreased from 892 mg/L FLC to 15 mg/L in 1.5 months. This complete remission has since been maintained, currently for a total of 2.5 years, without any notable complications and with a very good corneal eye condition using preventive hydrating eye drops (Figure 1). While he was under treatment with belantamab mafodotin, he contracted a severe COVID-19 infection; therefore, the therapy was discontinued in November 2022. At that time, he was still in hematologic remission.
Figure 1.
Kappa free light-chain levels decrease after the first injection of belantamab mafodotin.
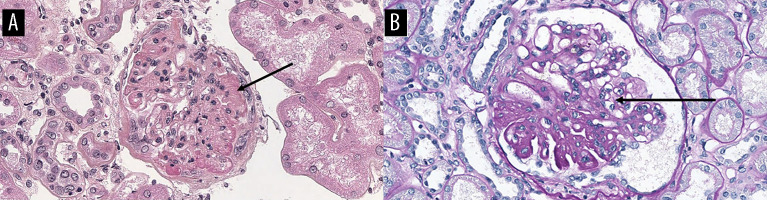
One month later, he suddenly developed generalized edema, revealing a secondary nephrotic syndrome with an albuminemia of 20 g/L (normal: 35–53 g/L), a proteinuria of 3.23 g/24 h, glomerular proteinuria (mostly albumin), a proteinuria to creatininuria ratio of 4.8 (normal <0.02 g/mmol), an albuminuriato-creatininuria ratio of 3.5 (normal <3 mg/mmol), and a serum creatininemia of 182 µmol/L (normal <104 micromol/L) (without hematuria or hypertension). An abdominal ultrasound scan revealed ascites related to the nephrotic syndrome and cortico-sinusal dedifferentiation of both kidneys, which remained normal-sized. A cardiac ultrasound scan showed moderate left ventricular hypertrophy with preserved cardiac function (LVEF 56%). Cardiac MRI revealed no evidence of cardiac amyloidosis. A biopsy of the accessory salivary glands showed no evidence of AL amyloidosis. Light microscopy of a renal biopsy showed focal segmental glomerulosclerosis not otherwise specified (FSGS NOS) without deposits, with chronic glomerular sclerosis lesions affecting one-third of the glomeruli (7 stamps on 20 glomeruli analyzed) and interstitial fibrosis occupying one-third of the cortex. The tubules had no tubular casts. An immunofluorescence assay showed fairly abundant endomembrane deposits of IgM and rarely IgA in the sclerohyaline glomerular lesions, but without deposition of IgG, C1q, kappa or lambda clonality, amyloid deposits, or plasma cell infiltration (Figure 2A, 2B). APOL1 genetic phenotyping was low risk for renal complication: G0/G2. Symptomatic treatment of the nephrotic syndrome with furosemide plus an ACE inhibitor, and without immunosuppressive drug use, led to good reduction of the edema. The cause of this event remains undetermined. One year later, the renal function was stable: albuminemia was 37 g/L, serum creatininemia was 213 micromol/L (eGFR=25 mL/mn), proteinuria was 1.4 g/L, and proteinuria/creatininuria was 0.18 g/mmol, without hematuria. At the last follow-up in April 2024, his hypertension was well controlled, he had no hematuria, serum creatinine was 242 micromol/L (eGFR=21 mL/mn), proteinuria was 0.46 g/L, and proteinuria/creatininuria was 0.06 g/mmol. Currently, the patient is still in hematologic remission despite discontinuing belantamab mafodotin therapy 2 years ago.
Figure 2.
Light microscopy image of the patient’s renal biopsy showing focal segmental glomerulosclerosis not otherwise specified (FSGS NOS) with sclerosis, hyalinosis, adhesion, and slight podocyte hyperplasia (arrow) (hematoxylin and eosin staining (A) and periodic acid-Schiff staining, ×100 (B)).
Discussion
This case report helps understand the causes of FSGS in a myeloma patient. Belantamab mafodotin is a monoclonal antibody targeting B-cell maturation antigen (BCMA), which is specifically expressed on plasma cells. It is composed of a humanized afucosylated IgG1 conjugated with an inhibitor of micro-tubule polymerization, monomethyl auristatin F (MMAF) [7]. It binds specifically to BCMA and acts through various mechanisms: release of MMAF into the plasma cells, antibody-dependent cellular cytotoxicity (ADCC), antibody-dependent phagocytosis, and immunogenic cell death [7]. This case is interesting for the length and depth of response to belantamab mafodotin (2.5 years, including 1 year treatment-free) without any corneal complications and for the appearance of a secondary nephrotic syndrome.
In the DREAMM-2 study comparing 2 doses of belantamab mafodotin (2.5 vs 3.4 mg/kg) in patients with refractory or relapsed MM after treatment with proteasome inhibitors, IMiDs, or anti-CD38 therapy, the overall response rate in both groups was around 33%. The median progression-free survival was 3 months in both groups and the median overall survival was 9.5 months [8]. Our patient achieved a response of more than 2.5 years, with a rapid and deep response after only 2 months of therapy. Notably, he did not present any corneal toxicity despite the long period of treatment. Patients in the DREAMM-2 study, on the other hand, displayed keratopathy or changes in their corneal epithelium (43% Grade 1 and 27% Grade 2) in 70% of cases [8]. Real-world data on belantamab mafodotin presented by the Mayo Clinic were similar to the data from the DREAMM-1 and -2 studies: one-third of these multi-refractory patients responded overall, but the duration of response was very short, only 3 months on an average [9].
FSGS, a common histological finding in patients with proteinuria, is a non-inflammatory glomerulopathy that can lead to end-stage renal disease, although it can respond to therapy. It may be caused by a variety of conditions and can be idiopathic, but it has rarely been associated with hematologic disorders and especially not with plasma cell disorders. In 2005, a retrospective study of the Mayo Clinic cross-referencing patients having idiopathic FSGS and monoclonal plasma cell disease found 4 MM and 9 MGUS in the 13 patients with FSGS [10]. Interestingly, the renal lesions improved in patients treated for myeloma and relapsed when the myeloma relapsed [10]. Two other reports described cases of patients diagnosed with monoclonal gammopathy and steroid resistant nephrotic syndrome where FSGS was found in the renal biopsy [11,12]. Proteinuria decreased in both patients when anti-myeloma treatment was started, the therapeutic effect of cyclophosphamide on FSGS during MM supporting an association between the 2.
The renal lesions in patients with monoclonal gammopathy are mostly related to the monoclonal protein and are normally secondary to myeloma cast nephropathy, monoclonal immunoglobulin deposition, or amyloidosis [13]. MGRS is less frequent [14]. Specifically, a nephrotic syndrome can occur in myeloma and is mostly related to AL amyloidosis or light and/or heavy chain deposition disease, but this was not the case in our patient. Other lesions not related to the protein deposits or their properties are mainly hypercalcemia, acute tubular necrosis, hypertensive arteriosclerosis, diabetic nephropathy, exposure to contrast products for CT scans, and non-steroid anti-inflammatory drugs [15]. The use of bisphosphonate (pamidronate) to treat hypercalcemia and bone lesions has been linked in MM to a characteristic collapsing variant of FSGS [15].
The present case showed no evidence of a link between the monoclonal gammopathy and the renal disease. The patient was in hematologic remission and had not received any nephrotoxic drugs and, in particular, no bisphosphonate. There are some very rare cases of light-chain crystal podocytopathy [16], which can present as FSGS with a nephrotic syndrome, but the histology found was not suggestive of this rare entity or of MGRS, although electron microscopy was not performed. The patient had experienced a recent COVID-19 infection, which might explain the FSGS (COVAN: COVID-associated nephropathy [17,18]). In a patient series, the authors described 6 patients of recent African ancestry who developed COVID-19-associated acute kidney injury with podocytopathy, collapsing glomerulopathy, or both. They demonstrated an association between high-risk gene variants in the APOL1 gene, which encodes the APOL1 protein, and collapsing glomerulopathy [19]. We suspect that myeloma and its treatment-induced immunosuppressive status might have contributed to the COVID-19 infection and subsequent nephrotic syndrome.
The presence of BCMA has been described on podocytes in a pediatric population and can induce a nephrotic syndrome, but the relationship between belantamab mafodotin and this type of FSGS is not known and is difficult to verify [20]. Our patient’s renal function remained stable at around 25 mL/min.
Conclusions
We present the case of a MM patient treated successfully with belantamab mafodotin who, while in hematologic remission, developed a nephrotic syndrome secondary to focal segmental glomerulosclerosis. A COVID-19 infection had occurred 1 month before the acute kidney injury and is the most likely explanation for the FSGS NOS. Our patient’s immune suppressive status, related to the myeloma disease and its treatment, might explain this viral infection and the subsequent renal complication very rarely seen in patients with monoclonal gammopathy.
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Department and Institution Where Work Was Done
Department of Hematology, Pitié Salpêtrière University Hospital, Sorbonne University, Paris, France.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Kyle RA, Larson DR, Therneau TM, et al. Long-term follow-up of monoclonal gammopathy of undetermined significance. N Engl J Med. 2018;378(3):241–49. doi: 10.1056/NEJMoa1709974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kyle RA, Remstein ED, Therneau TM, et al. Clinical course and prognosis of smoldering (asymptomatic) multiple myeloma. N Engl J Med. 2007;356:2582–90. doi: 10.1056/NEJMoa070389. [DOI] [PubMed] [Google Scholar]
- 3.Morgan GJ, Walker BA, Davies FE. The genetic architecture of multiple myeloma. Nat Rev Cancer. 2012;12:335–48. doi: 10.1038/nrc3257. [DOI] [PubMed] [Google Scholar]
- 4.Moreau P, Garfall AL, van de Donk NWCJ, et al. Teclistamab in relapsed or refractory multiple myeloma. N Engl J Med. 2022;387L:495–505. doi: 10.1056/NEJMoa2203478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van de Donk NWCJ, Pawlyn C, Yong KL. Multiple myeloma. Lancet. 2021;397(10272):410–27. doi: 10.1016/S0140-6736(21)00135-5. [DOI] [PubMed] [Google Scholar]
- 6.Leung N, Bridoux F, Batuman V, et al. The evaluation of monoclonal gammopathy of renal significance: A consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat Rev Nephrol. 2019;15(1):45–59. doi: 10.1038/s41581-018-0077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Markham A. Belantamab mafodotin: First approval. Drugs. 2020;80(15):1607–13. doi: 10.1007/s40265-020-01404-x. [DOI] [PubMed] [Google Scholar]
- 8.Lonial S, Lee HC, Badros A, et al. Longer-term outcomes with single-agent belantamab mafodotin in patients with relapsed or refractory multiple myeloma: 13-month follow-up from the pivotal DREAMM-2 study. Cancer. 2021;127(22):4198–212. doi: 10.1002/cncr.33809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vaxman I, Abeykoon J, Dispenzieri A, et al. “Real-life” data of the efficacy and safety of belantamab mafodotin in relapsed multiple myeloma – the Mayo Clinic experience. Blood Cancer J. 2021;11(12):196. doi: 10.1038/s41408-021-00592-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dingli D, Larson DR, Plevak MF, et al. Focal and segmental glomerulosclerosis and plasma cell proliferative disorders. Am J Kidney Dis. 2005;46(2):278–82. doi: 10.1053/j.ajkd.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Shah R, Shah N, Shah A, Mehta AN. Steroid-resistant nephrotic syndrome secondary to primary focal segmental glomerulosclerosis and smoldering multiple myeloma. Proc (Bayl Univ Med Cent) 2014;27(1):19–21. doi: 10.1080/08998280.2014.11929039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oweis AO, Al Shelleh SA, Aldaoud N, et al. Multiple myeloma in a patient with focal segmental glomerulosclerosis: A case report. Am J Case Rep. 2018;19:946–50. doi: 10.12659/AJCR.909696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nasr SH, Valeri AM, Sethi S, et al. Clinicopathologic correlations in multiple myeloma: A case series of 190 patients with kidney biopsies. Am J Kidney Dis. 2012;59(6):786–94. doi: 10.1053/j.ajkd.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Leung N, Bridoux F, Nasr SH. Monoclonal gammopathy of renal significance. N Engl J Med. 2021;384:1931–41. doi: 10.1056/NEJMra1810907. [DOI] [PubMed] [Google Scholar]
- 15.Nasr SH, Preddie DC, Markowitz GS, et al. Multiple myeloma, nephrotic syndrome and crystalloid inclusions in podocytes. Kidney Int. 2006;69:616–20. doi: 10.1038/sj.ki.5000144. [DOI] [PubMed] [Google Scholar]
- 16.Nasr SH, Kudose S, Javaugue V, et al. Pathological characteristics of light chain crystalline podocytopathy. Kidney Int. 2023;103(3):616–26. doi: 10.1016/j.kint.2022.11.026. [DOI] [PubMed] [Google Scholar]
- 17.Nadim MK, Forni LG, Mehta RL, et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat Rev Nephrol. 2020;16:747–64. doi: 10.1038/s41581-020-00356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas AD, Trainor R, Sheingold Z, et al. A case of COVID-19-associated focal segmental glomerulosclerosis. Cureus. 2023;15(4):e37547. doi: 10.7759/cureus.37547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shetty AA, Tawhari I, Safar-Boueri L, et al. COVID-19-associated glomerular disease. J Am Soc Nephrol. 2021;32(1):33–40. doi: 10.1681/ASN.2020060804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forero-Delgadillo J, Ochoa V, Restrepo JM, et al. B-cell activating factor (BAFF) and its receptors’ expression in pediatric nephrotic syndrome is associated with worse prognosis. PLoS One. 2022;17(11):e0277800. doi: 10.1371/journal.pone.0277800. [DOI] [PMC free article] [PubMed] [Google Scholar]