Abstract
Objectives
The aim of this study was to translate the Exercise Benefits/Barriers Scale (EBBS) into Turkish and investigate the perceptions of Turkish-speaking patients with different axial spondyloarthritis (axSpA) subtypes regarding exercise benefits and barriers.
Patients and methods
This validation study was conducted between June 2018 and December 2021. Patients with axSpA were consecutively assessed regarding physical (age, sex and body mass index) and disease-related characteristics (disease activity, spinal mobility, functional status, quality of life, health status, emotional status, and kinesiophobia). Eligible participants were asked to complete the EBSS and other outcome measurements during their initial visits. EBBS was readministered 7 to 14 days later.
Results
One hundred forty-eight patients (89 males, 59 females; mean age: 44.3±11.8 years; range, 19 to 65 years) were included in the study. Of the patients, 108 had radiographic axSpA, and 40 had nonradiographic axSpA. EBBS-Barriers and EBBS-Benefits subscales demonstrated adequate internal consistency (Cronbach’s alphas of 0.82 and 0.95, respectively) and test-retest reliability (intraclass correlation coefficients of 0.837 and 0.807, respectively). No significant differences were observed between axSpA subtypes regarding EBBS-Barriers (p=0.12) and EBBS-Benefits (p=0.10) subscales. Significant relationships were detected between kinesiophobia and EBBS-Barriers scores (r=–0.424, p<0.01), as well as EBBS-Benefits scores (r=–0.344, p<0.01) for all patients. EBBS-Benefits scores were correlated to health status (r=–0.412, p=0.08) and quality of life (r=–0.394, p=0.01) in patients with nonradiographic axSpA.
Conclusion
According to our results, the Turkish EBBS is a valid and reliable tool for patients with axSpA. Perceptions of the patients with axSpA regarding exercise barriers and benefits do not differ according to the disease subtype. It appears that kinesiophobia may be an important parameter regarding exercise perception in axSpA.
Keywords: Arthritis, exercise, patient reported outcome, reliability, validity.
Introduction
Axial spondyloarthritis (axSpA) is the umbrella term for inflammatory arthritides of the spine, which share common genetic, epidemiological, radiological, and clinical features.[1,2] The prevalence of axSpA demonstrates great variation globally, with a wide range from 6.5 in Japan to 540 in Türkiye in every 100,000 individuals.[3] The radiological status of the spine determines the subtype of the disease as radiographic axSpA (r-axSpA, previously known as ankylosing spondylitis) and nonradiographic axSpA (nr-axSpA).[4,5]
The Assessment of SpondyloArthritis International Society (ASAS) and the European Alliance of Associations for Rheumatology (EULAR) recommend regular exercise as an essential part of the disease management in patients with axSpA.[6,7] Regular exercise not only leads to many health-promoting benefits, such as improved muscle strength, increased exercise capacity, decreased fatigue, and diminished depression, but also helps to decrease disease activity, improve spinal mobility, and enhance functional status in patients with axSpA.[8,9] However, numerous previous studies suggest that patients with axSpA are not as physically active as their healthy peers, and at least half of the patients with axSpA do not exercise as recommended.[5,10,11] Moreover, a recent study revealed that physical activity patterns show differences between patients with r-axSpA and nr-axSpA.[5] Thus, determining the perception of the patients with different disease subtypes regarding the benefits and barriers of exercise may be beneficial for implementing recommendations. However, to our knowledge, the differences in the perception of exercise benefits and barriers were not compared between axSpA subtypes.
Perceptions of exercise benefits and barriers of patients with axSpA were previously evaluated in a French-speaking cohort by using the Exercise Benefits/Barriers Scale (EBBS).[11] However, even though a previous attempt was made to translate EBBS into Turkish for a healthy population,[12] the utility of EBBS for Turkish-speaking patients with axSpA was not investigated. Therefore, this study aimed to achieve three main goals: (i) formally and systematically translating EBBS into the Turkish language and investigating its psychometric properties in Turkish-speaking patients with axSpA, (ii) comparing the perceptions regarding exercise barriers and benefits between different axSpA subtypes, and (iii) investigating the relationships between perceived barriers/benefits of exercise and disease-specific indices in patients with r-axSpA and nr-axSpA.
Patients and Methods
This validation study was performed at the İzmir Katip Çelebi University, Atatürk Training and Research Hospital between June 2018 and December 2021. Participants were recruited from the patients who were on regular followups at the rheumatology department. The inclusion criteria were as follows: (i) being between 18 and 65 years old and (ii) being classified as axSpA according to the ASAS axSpA classification criteria.[13] The exclusion criteria were as follows: (i) having additional health conditions that may affect performing regular exercise (e.g., pregnancy, neurological disorder, and acute orthopedic injury) and (ii) having difficulties in understanding/reading the Turkish language.
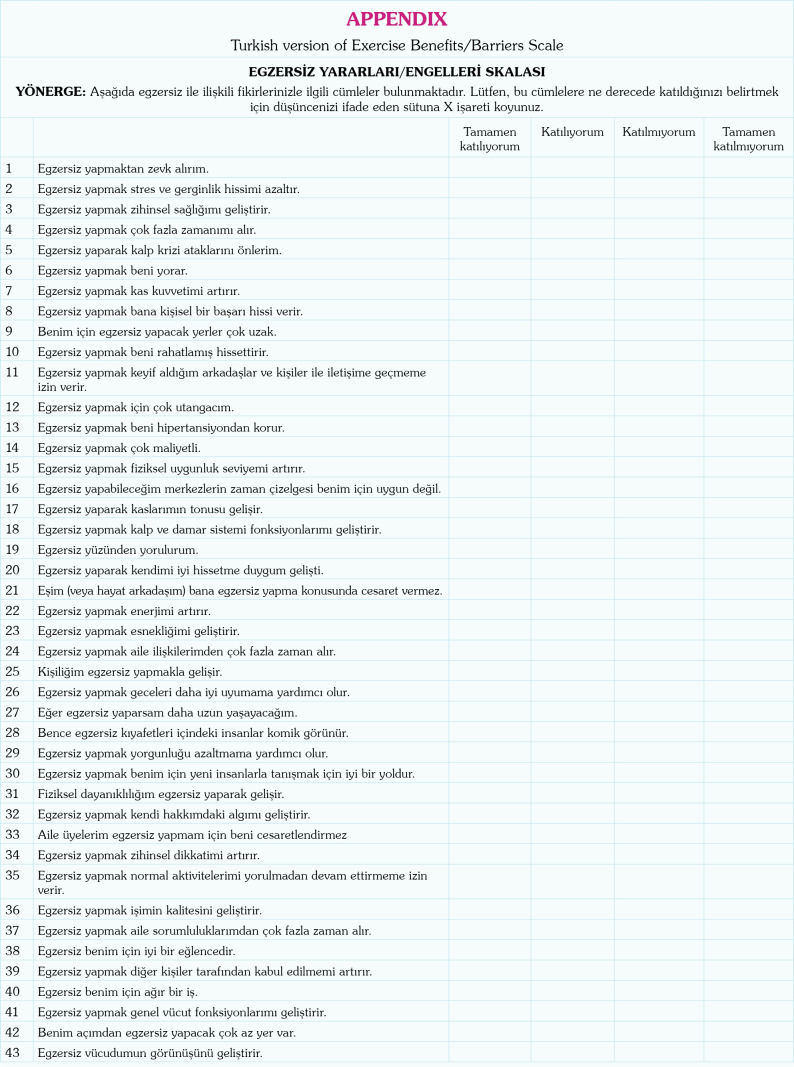
Exercise Benefits/Barriers Scale was developed in 1987 by Sechrist et al.[14] to evaluate the perceptions of individuals on the benefits and barriers of the exercise. The permissions were obtained from Dr. Sechrist prior to the study via electronic mail. The psychometric properties of the original EBBS were reported to be acceptable (intraclass correlation coefficient [ICC]=0.89, Cronbach’s alpha= 0.954).[14] The EBBS has a 4-point Likert-type layout with answers ranging from 4 (strongly agree) to 1 (strongly disagree). EBBS consists of two main parts, EBBS-Benefits subscale (29 items; scores ranging from 14 to 56) and EBBS-Barriers subscale (14 items; scores ranging from 29 to 116). EBBS-Barriers subscale items (items: 4, 6, 9, 12, 14, 16, 19, 21, 24, 28, 33, 37, 40, and 42) are reverse-scored. Missing data are handled in one of two ways. If more than 5% of the items are unanswered, it is recommended that the response be discarded.[14] If the missing item response rate is less than 5%, median substitution prevents falsely low scores. These subscales are generally used separately. Lower scores indicate a higher exercise barrier perception for the EBBS-Barriers subscale, and higher scores suggest a more positive perception regarding exercise for the EBBSBenefits subscale.
The protocol described by Beaton et al.[15] was employed for the translation of the EBBS. First, the original English version of the EBBS was translated into Turkish by two independent native Turkish speakers (one with a medical background, one without) who had excellent proficiency in English. Disagreements between translators were resolved by a third person. Following the generation of the initial Turkish version, two different independent translators who had proficiency in the Turkish language and native speakers of the English language without a medical background translated EBBS back into English. A committee formed of researchers and the translators of the study checked the back-translated version for any major disagreements or poor wording choices. Following these steps, 30 healthy individuals assessed the form in terms of language use and clarity, and none suggested any major revisions. Following minor revisions, the final version of the Turkish EBBS was generated and used in the present study (Appendix). The face validity of the final version of Turkish EBBS was reassessed by 44 patients with axSpA at the end of the study.
Physical features (age, sex and body mass index), and disease-related characteristics (axSpA subtype and medications) were recorded using a structured form. The following aspects of the disease were evaluated: (i) disease activity with the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI);[16] (ii) spinal mobility with the Bath Ankylosing Spondylitis Metrology Index (BASMI);[17] (iii) functional status with the Bath Ankylosing Spondylitis Functional Index (BASFI);[18] (iv) disease-related quality of life with the Ankylosing Spondylitis Quality of Life Questionnaire (ASQoL);[19] (v) health status with the ASAS Health Index (ASAS-HI);[20] (vi) emotional status with the Hospital Anxiety and Depression Scale (HADS);[21] (vii) kinesiophobia with the Tampa Scale of Kinesiophobia (TSK).[22,23] Higher scores in BASDAI, BASMI, BASFI, ASQoL, HADS, and TSK indicate poorer outcomes, whereas lower scores in ASAS-HI are associated with a poorer health status.
Eligible participants were asked to complete the EBSS and other outcome measurements during their initial visits. The EBBS was subsequently readministered seven to 14 days after the initial visit to investigate test-retest reliability.
Statistical analysis
Statistical analysis was performed using SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA). The normality of distribution was analyzed using the Kolmogorov-Smirnov test and histograms. As data were normally distributed, continuous data were expressed as mean ± standard deviation (SD). Face validity was considered ≥75% agreement of the patients that no changes were needed on the final version of Turkish EBBS. Internal consistency was checked with corrected item-total correlation levels (r≥0.30)[24] and Cronbach’s alpha values (≥0.80).[25] ICCs in 95% confidence interval (CI) (two-way mixedeffects model, single measures) were used to examine the test-retest reliability.
ICCs were interpreted as follows: >0.90, excellent; 0.90-0.71, good; 0.70-0.51, moderate; 0.50-0.31, fair; ≤0.30, negligible.[26] Standard error measurement (SEM) refers to the amount of variability in a test administered to a group that is caused by measurement error when a test is repeated. SEM was calculated using the following formula: SEM=SD×√(1-ICC).[27] Minimal detectable change (MDC) is a statistical estimation of the smallest amount of change that should be present between two performed measurements that indicates a significant change in ability or a true change of the results. MDC in 95% CI values were calculated using the following formula: MDC=1.96×SEM×√2.[27]
Two distinct criteria were employed to evaluate the presence of floor and ceiling effects. First, the percentage of participants who achieved the minimum and maximum scores for each measurement was calculated. Consistent with previous research,[28] values exceeding 15% were considered indicative of the presence of either a floor or ceiling effect. The second criterion was based on absolute skewness (γ1) values. It was posited that a γ1 value exceeding +1 signified the presence of a floor effect, while a γ1 value below –1 signified the presence of a ceiling effect.[29]
Welch one-way analysis of variance test was used to compare EBBS-Barriers and EBBS-Benefits scores between the r-axSpA and nr-axSpA subtypes. Mean differences in 95% CIs and effect sizes (Cohen’s d) were calculated using the following formula: d=(Mean1-Mean2)/√[(SD1 2+SD2 2)/2)].[30] Categorical data, such as sex, were compared using the chi-square test. A p-value <0.05 was considered statistically significant.
The level of correlations between BASDAI, BASMI, BASFI, ASQoL, ASAS-HI, HADS, and TSK and EBBS-Barriers and EBBS-Benefits scores were analyzed using Pearson correlation coefficient (r) to investigate potential associations. Correlation coefficients were interpreted as follows: >0.90, excellent; 0.90-0.71, good; 0.70-0.51, moderate; 0.50-0.31, fair; ≤0.30, negligible.[26]
Results
The study was completed with 148 patients (89 males, 59 females mean age: 44.3±11.8 years; range, 19 to 65 years) with axSpA (108 with r-axSpA and 40 with nr-axSpA). There were significant differences in sex distribution (p<0.01) and BASMI scores (p<0.01) between subtypes (Table 1). No other significant differences were detected between axSpA subtypes (p>0.05, Table 1). Five patients were not on any medication, 48 were using nonsteroid anti-inflammatory drugs, four were using diseasemodifying antirheumatic drugs, 81 patients were on tumor necrosis factor-alpha inhibitors, and nine were using other biological agents.
Table 1. Physical and disease-related characteristics.
| r-axSpA (n=108) | nr-axSpA (n=40) | All axSpA (n=148) | |||||
| n | Mean±SD | n | Mean±SD | p* | n | Mean±SD | |
| Physical characteristics | |||||||
| Age (year) | 45.24±12.11 | 41.75±10.63 | 0.09b | 44.3±11.8 | |||
| Sex Male Female |
75 33 |
14 26 |
<0.01a |
89 59 |
|||
| Body mass index (kg/m2) | 27.11±4.74 | 25.98±4.83 | 0.20b | 26.81±4.78 | |||
| Disease-related characteristics | |||||||
| BASDAI | 2.94±2.22 | 2.78±2.05 | 0.69b | 2.9±2.18 | |||
| BASFI | 2.73±2.28 | 2.25±2.02 | 0.22b | 2.6±2.22 | |||
| BASMI | 3.47±1.92 | 2.33±1.36 | <0.01b | 3.16±1.85 | |||
| ASQoL | 6.53±5.36 | 6.3±5.23 | 0.81b | 6.47±5.31 | |||
| ASAS-HI | 6.29±4.03 | 6.17±4.4 | 0.89b | 6.25±4.12 | |||
| HADS-anxiety | 6.49±3.96 | 6.93±4.04 | 0.56b | 6.6±3.97 | |||
| HADS-depression | 6.14±4.35 | 6.07±4.64 | 0.93b | 6.13±4.41 | |||
| Tampa Scale of Kinesiophobia | 40.23±6.37 | 38.47±6.09 | 0.13b | 39.76±6.32 | |||
| r-axSpA: Radiographic axial spondylo arthritis; nr-axSpA: Nonradiographic axial spondyloarthritis; axSpA: Axial spondylo arthritis; SD: Standard deviation; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; BASFI: Bath Ankylosing Spondylitis Functional Index; BASMI: Bath Ankylosing Spondylitis Metrology Index; ASQoL: Ankylosing Spondylitis Quality of Life Questionnaire; ASAS HI: The Assessment of SpondyloArthritis international Society Health Index; HADS: Hospital Anxiety and Depression Scale; * p<0.05; a: Chi-square test; b: Welch One-Way ANOVA test. | |||||||
The face validity of the final version of Turkish EBBS was assessed by 44 patients (26 males, 18 females; mean age: 43.8±9.9 years; range, 19 to 65 years) with axSpA (36 with r-axSpA and 8 with nr-axSpA) at the end of the study. Seventeen (39%) of the patients had a primary education (8 years of education), 11 (25%) had a secondary education (high school or equivalent 12 years of education), and 16 (36%) had a higher education degree (bachelor or higher with at least 14 years of education). Thirty-three (75%) of patients did not offer any changes to the final version of the Turkish EBBS. Three (7%) patients recommended minor word changes (e.g., using “to motivate” instead of “to encourage”). Three (7%) patients indicated that some items (items 13, 25, 28, and 29) sounded irrelevant/funny. One (2%) patient declared that some items inquired the same things and that the number of items could be decreased. One patient reported that EBBS might not be suitable for patients with advanced disease, and one patient raised concerns that the questions were not for every level of education. One patient suggested a dichotomous (yes/no) way of answering would be easier.
The internal consistencies of both EBBSBarriers and EBBS-Benefits were good, with Cronbach’s alpha values of 0.82 and 0.95, respectively. Item-total correlation analyses demonstrated that the extraction of the items did not cause a significant increase (≥10%) in total correlation (Tables 2, 3).
Table 2. Internal consistency of EBBS-Barriers subscale (n=148).
| Scale mean if item deleted | Scale variance if item deleted | Corrected item-total correlation | Cronbach’s alpha if item deleted | |
| Item 4 | 37.01 | 26.72 | 0.45 | 0.81 |
| Item 6 | 37.34 | 27.46 | 0.32 | 0.82 |
| Item 9 | 37.00 | 25.73 | 0.57 | 0.80 |
| Item 12 | 36.64 | 26.41 | 0.46 | 0.81 |
| Item 14 | 36.71 | 26.44 | 0.51 | 0.81 |
| Item 16 | 36.95 | 26.25 | 0.44 | 0.81 |
| Item 19 | 37.23 | 26.25 | 0.46 | 0.81 |
| Item 21 | 36.82 | 27.31 | 0.28 | 0.83 |
| Item 24 | 36.76 | 28.16 | 0.25 | 0.82 |
| Item 28 | 36.55 | 26.58 | 0.44 | 0.81 |
| Item 33 | 36.76 | 26.60 | 0.41 | 0.81 |
| Item 37 | 36.80 | 25.26 | 0.62 | 0.80 |
| Item 40 | 36.95 | 25.45 | 0.56 | 0.80 |
| Item 42 | 36.89 | 25.61 | 0.53 | 0.81 |
| Cronbach’s alpha for total EBBS-Barriers subscale | 0.82 | |||
| EBBS: Exercise Benefits/Barriers Scale. | ||||
Table 3. Internal consistency of EBBS-Benefits subscale (n=148).
| Scale mean if item deleted | Scale variance if item deleted | Corrected item-total correlation | Cronbach’s alpha if item deleted | |
| Item 1 | 82.97 | 155.16 | 0.62 | 0.95 |
| Item 2 | 82.80 | 154.77 | 0.67 | 0.95 |
| Item 3 | 82.79 | 156.07 | 0.63 | 0.95 |
| Item 5 | 82.86 | 158.61 | 0.53 | 0.95 |
| Item 7 | 82.70 | 157.59 | 0.69 | 0.95 |
| Item 8 | 82.84 | 155.40 | 0.71 | 0.95 |
| Item 10 | 82.74 | 155.07 | 0.72 | 0.95 |
| Item 11 | 82.98 | 156.87 | 0.56 | 0.95 |
| Item 13 | 82.89 | 158.56 | 0.58 | 0.95 |
| Item 15 | 82.69 | 157.03 | 0.64 | 0.95 |
| Item 17 | 82.75 | 156.91 | 0.68 | 0.95 |
| Item 18 | 82.64 | 158.75 | 0.64 | 0.95 |
| Item 20 | 82.79 | 153.51 | 0.77 | 0.95 |
| Item 22 | 82.82 | 155.46 | 0.67 | 0.95 |
| Item 23 | 82.71 | 155.48 | 0.76 | 0.95 |
| Item 25 | 83.26 | 156.83 | 0.54 | 0.95 |
| Item 26 | 82.84 | 154.57 | 0.74 | 0.95 |
| Item 27 | 83.00 | 156.56 | 0.52 | 0.95 |
| Item 29 | 83.03 | 154.31 | 0.69 | 0.95 |
| Item 30 | 83.09 | 157.62 | 0.48 | 0.95 |
| Item 31 | 82.68 | 155.02 | 0.79 | 0.95 |
| Item 32 | 82.79 | 156.59 | 0.69 | 0.95 |
| Item 34 | 83.09 | 161.11 | 0.31 | 0.96 |
| Item 35 | 82.85 | 155.20 | 0.72 | 0.95 |
| Item 36 | 82.84 | 155.88 | 0.70 | 0.95 |
| Item 38 | 82.97 | 154.82 | 0.73 | 0.95 |
| Item 39 | 83.41 | 160.42 | 0.38 | 0.95 |
| Item 41 | 82.72 | 156.55 | 0.73 | 0.95 |
| Item 43 | 82.76 | 156.89 | 0.65 | 0.95 |
| Cronbach’s alpha for total EBBS-Barriers subscale | 0.95 | |||
| EBBS: Exercise Benefits/Barriers Scale. | ||||
Test-retest reliability of EBBS was analyzed in 57 patients with axSpA. ICC analyses revealed that both EBBS-Barriers (ICC=0.837, 95% CI: 0.738-0.900) and EBBS-Benefits (ICC=0.807, 95% CI: 0.693-0.882) scales showed good to excellent reliability. The details of reliability analyses and the calculated SEM and MDC values are presented in Table 4.
Table 4. Test-retest reliability, SEM, and MDC (n=57).
| Test | Re-test | |||||||
| Mean±SD | Mean±SD | ICC | 95% CI | SEM | 95% CI | MDC | 95% CI | |
| EBBS-Barriers | 36.77±4.31 | 39.5±4.24 | 0.837 | 0.738-0.900 | 1.74 | 1.36-2.2 | 6.82 | 5.33-8.62 |
| EBBS-Benefits | 83.52±9.82 | 85.47±8.69 | 0.807 | 0.693-0.882 | 4.31 | 3.37-5.44 | 16.89 | 13.21-21.32 |
| SEM: Standard error measurement; MDC: Minimal detectable change; SD: Standard deviation; EBBS: Exercise Benefits/Barriers scale; ICC: Intraclass correlation coefficient; CI: Confidence interval. | ||||||||
None of the patients received a maximum or minimum score neither in EBBS-Barriers nor EBBS-Benefits subscales, indicating the absence of a floor-ceiling effect. The γ1 value was calculated as -0.885 for EBBS-Barriers and –0.257 for EBBS-Benefits, signifying the lack of a floor or ceiling effect.
No significant differences were detected between r-axSpA and nr-axSpA subtypes regarding EBBS-Barriers (p=0.12, d=0.27) and EBBS-Benefits scores (p=0.10, d=0.29, Table 5).
Table 5. Comparison of EBBS scores between r-axSpA and nr-axSpA subtypes.
| r-axSpA (n=108) | nr-axSpA (n=40) | |||||
| Mean±SD | Mean±SD | p* | Mean differences | 95% CI | Cohen’s d | |
| EBBS-Barriers (score) | 36.59±5.39 | 37.92±4.2 | 0.12 | -1.33 | -3.2 to 0.53 | 0.27 |
| EBBS-Benefits (score) | 84.87±13.58 | 88.4±10.76 | 0.10 | -3.52 | -7.78 to 0.74 | 0.29 |
| EBBS: Exercise Benefits/Barriers scale; r-axSpA: Radiographic axial spondyloarthritis; nr-axSpA: Nonradiographic axial spondyloarthritis; SD: Standard deviation; CI: Confidence interval; * Welch One-Way ANOVA test; p<0.05; d: effect size. | ||||||
ASAS-HI scores (r=–0.412, p=0.01) and ASQoL scores (r=–0.394, p=0.01) showed fair relationships with EBBS-Benefits scores for patients with nr-axSpA. While there were other statistically significant relationships between exercise perception and other disease indices, all were on a negligible level (r<0.30, Table 6).
Table 6. Associations of EBBS-Barriers and EBBS-Benefits with the disease indices.
| r-axSpA (n=108) | nr-axSpA (n=40) | All axSpA (n=148) | |||||
| EBBS-Barriers | EBBS-Benefits | EBBS-Barriers | EBBS-Benefits | EBBS-Barriers | EBBS-Benefits | ||
| TSK* | r | -0.394 | -0.329 | -0.502 | -0.357 | -0.424 | -0.344 |
| p | <0.01 | <0.01 | <0.01 | 0.02 | <0.01 | <0.01 | |
| BASDAI | r | -0.175 | -0.001 | -0.172 | -0.295 | -0.176 | -0.065 |
| p | 0.07 | >0.99 | 0.29 | 0.07 | 0.03 | 0.43 | |
| BASFI | r | -0.105 | -0.126 | -0.148 | -0.258 | -0.123 | -0.162 |
| p | 0.29 | 0.20 | 0.36 | 0.11 | 0.14 | 0.05 | |
| BASMI | r | -0.185 | -0.208 | -0.121 | -0.141 | -0.198 | -0.221 |
| p | 0.06 | <0.01 | 0.46 | 0.39 | 0.02 | 0.01 | |
| ASQoL | r | -0.223 | -0.239 | -0.250 | -0.394 | -0.228 | -0.273 |
| p | 0.02 | 0.01 | 0.12 | 0.01 | <0.01 | <0.01 | |
| ASAS-HI | r | -0.251 | -0.258 | -0.282 | -0.412 | -0.255 | -0.291 |
| p | 0.01 | 0.01 | 0.08 | 0.01 | <0.01 | <0.01 | |
| HADS-anxiety | r | -0.187 | -0.257 | -0.290 | -0.267 | -0.201 | -0.249 |
| p | 0.05 | 0.01 | 0.07 | 0.10 | 0.01 | <0.01 | |
| HADS-depression | r | -0.165 | -0.285 | -0.123 | -0.237 | -0.154 | -0.271 |
| p | 0.09 | <0.01 | 0.45 | 0.14 | 0.06 | <0.01 | |
| EBBS: Exercise Benefits/Barriers scale; r-axSpA: Radiographic axial spondyloarthritis; nr-axSpA: Nonradiographic axial spondyloarthritis; axSpA: Axial spondyloarthritis; TSK: Tampa scale of kinesiophobia; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; BASFI: Bath Ankylosing Spondylitis Functional Index; BASMI: Bath Ankylosing Spondylitis Metrology Index; ASQoL: Ankylosing Spondylitis Quality of Life Questionnaire; ASAS-HI: The Assessment of SpondyloArthritis international Society Health Index; HADS: Hospital Anxiety and Depression Scale; r: Pearson correlation coefficient; Written in bold: p<0.05 and r>0.3. * The level of correlations between EBBS scores and TSK were calculated for convergent validity analysis. | |||||||
The five barriers with the lowest mean values and five benefits with the highest mean values that were reported by the patients with axSpA are presented in Table 7.
Table 7. Top 5 Exercise Barriers and Benefits perceptions of patients with axSpA.
| Mean score | SD | |
| Barriers | ||
| 1. Exercise tires me | 2.38 | 0.68 |
| 2. I am fatigued by exercise | 2.49 | 0.73 |
| 3. Exercising takes too much of my time | 2.70 | 0.66 |
| 4. Places for me to exercise are too far away | 2.72 | 0.69 |
| 5. Exercise facilities do not have convenient schedules for me | 2.77 | 0.75 |
| Benefits | ||
| 1. Exercising improves functioning of my cardiovascular system | 3.19 | 0.53 |
| 2. My physical endurance is improved by exercising | 3.14 | 0.62 |
| 3. Exercising increases my level of physical fitness | 3.14 | 0.62 |
| 4. Exercise increases my muscle strength | 3.13 | 0.55 |
| 5. Exercise improves my flexibility | 3.12 | 0.61 |
| 5*. Exercise improves overall body functioning for me | 3.09 | 0.61 |
| axSpA: Axial spondyloarthritis; SD: Standard deviation; * Radiographic axSpA patients ranked this item fifth according to benefit | ||
Discussion
The present study had three main goals regarding exercise benefits and barriers perceptions of patients with axSpA. To achieve these goals, EBBS was systematically and formally translated into Turkish, and its psychometric properties were tested. According to our results, the Turkish version of EBBS showed adequate validity and reliability for both EBBS-Barriers and EBBS-Benefits subscales without any floor or ceiling effects in patients with axSpA. Second, no differences were observed in EBBS scores between r-axSpA and nr-axSpA subtypes. Lastly, exercise barriers and benefits perceptions of the r-axSpA and nr-axSpA patients correlated to kinesiophobia at a fair to moderate level. No other high-level correlations were observed between investigated variables in axSpA subtypes, except for the fair level of correlations between health status, quality of life, and EBBS-Benefits scores.
Most of the patients (75%) who performed the face validity assessment agreed that the final version of Turkish EBBS was clearly understandable and did not need any changes. Eleven (25%) patients raised minor concerns (word modifications or opinions about how to collect the data). However, after a small discussion, they all agreed that the Turkish version of EBBS can be used for assessing the perception of exercise barriers/benefits of patients with axSpA.
Previous studies reported comparable results regarding the validity and reliability of EBBS. In the original study of EBBS in healthy adults, Sechrist et al.[14] found the internal consistency of EBBS-Barriers and EBBS-Benefits subscales as 0.95 and 0.88, respectively. Farahani et al.[31] also calculated the Cronbach’s alpha levels for EBBS-Barriers and EBBS-benefits subscales as 0.94 and 0.82 in healthy women. They also calculated the test-retest reliability of EBBS as 0.79 and 0.74 for the benefits and barriers subscales, respectively. Similar to our results, Ortabag et al.[12] reported that their version of Turkish EBBS showed adequate internal validity (Cronbach’s alphas =0.87 for total EBBS, 0.95 for EBBS-Benefits, and 0.80 for EBBS-Barriers) and test-retest reliability (ICCs of 0.85 for total EBBS, 0.94 for EBBS-Benefits, and 0.79 for EBBS-Barriers) for healthy military nursing students. To our knowledge, SEM and MDC values for EBBS-Barriers and EBBS-Benefits subscales were calculated for the first time in our study. We believe these values may help in interpreting the results of EBBS scores in future research and clinical settings.
As far as we are aware, only Fabre et al.[11] interrogated the perceptions of patients with axSpA regarding exercise barriers and benefits using EBBS in a French speaking cohort. The authors reported the mean EBBS-Barriers score as 30.6 and the mean EBBS-Benefits score as 86.2. These values are slightly better compared to the results of the present study. These slight differences might be attributed to cultural variances between populations; however, the mean differences of Fabre et al.[11] were lower than the SEM and MDC values that were calculated for EBBS in our study. Thus, it can be concluded that exercise barriers and benefits perception of patients with axSpA are comparable between these two populations. Additionally, they detected main exercise barriers as “physical exertion” and “lack of exercise milieu,” and exercise benefits as “improvements in physical performance and health” similar to the results of our study. These results underline the importance of fatigue and exercise capacity as possible targets to be improved, particularly for patients with axSpA with a higher perception of exercise barriers.
The present study compared the EBBSBarriers and EBBS-Benefits scores between patients with axSpA with and without radiographic involvement. Although patients with nr-axSpA presented slightly better scores in EBBS Barriers and EBBS-Benefits subscales, no significant differences were detected between subtypes, and the mean differences were smaller than the calculated MDC values. Our results indicate that both axSpA subtypes have similar perceptions regarding barriers or benefits of exercise. Thus, regardless of the subtype, any patient with axSpA may benefit from further patient education regarding the beneficial effects of the exercise and how to tackle the exercise barriers.
EBBS-Barriers and EBBS-Benefits scores correlated to kinesiophobia at a fair level but not to disease activity, function, spinal mobility, quality of life, or emotional status. To our knowledge, this is the first study to investigate the relationship between exercise barriers/benefits perception and these parameters. Previous studies focused on the relationships between disease-related indices and levels of physical activity and obtained mixed results. Some authors reported no relationships between disease-related indices and physical activity,[10,11,32] while some detected low levels of correlations in patients with axSpA.[5,33,34] However, higher kinesiophobia levels appear to have negative effects on physical activity levels in patients with axSpA[5] and other populations.[35,36] On the other hand, performing a large number of correlation analyses without adjusting for multiple tests may have increased the risk of obtaining pseudosignificant correlations. Evaluating physical activity, kinesiophobia, and exercise barriers/benefits together may help clinicians observe the status of the patients more clearly.
The most important limitation of the present study was the lack of an objective measurement of physical activity. The International Physical Activity Questionnaire (IPAQ) was employed to evaluate the physical activity in previous studies in patients with axSpA. However, different studies showed that IPAQ was not a sensitive measurement for physical activity assessment.[37,38] Thus, the effects of exercise barriers/benefits perceptions of patients with axSpA on physical activity are yet to be investigated in future studies. It is recommended to include at least five patients for each item in the questionnaire, and we aimed to reach at least 215 patients with axSpA.[39] However, the present study was conducted mostly during the COVID-19 (coronavirus disease 2019) pandemic (between June 2018 and December 2021); therefore, we did not reach the planned sample size. Limiting the upper age to be included in the study to 65 years may be counted as another limitation of the study. However, people older than 65 years are considered geriatric patients, and physiological changes due to old age may interfere with the outcomes. Thus, we decided not to include elderly patients to investigate the effects of axSpA solely. Investigating the face validity at the end of the study is also a methodological limitation. However, no major changes were requested by the patients regarding understandability. Lastly, structural validity of the Turkish EBBS could not be investigated due to the relatively small sample size to avoid presenting dubious results.
In conclusion, EBBS-Barriers and EBBSBenefits scales were demonstrated to be valid and reliable in Turkish-speaking patients with axSpA. Furthermore, the SEM and MDC values were introduced for the first time. The most important barriers to exercise in Turkish patients with axSpA appear to be fatigue due to exercise and lack of exercise milieu, while the main exercise benefits were related to opinions of improvements in physical fitness and general health. It appears that the disease subtype does not significantly affect exercise perception in Turkish patients with axSpA. Lastly, EBBSBarriers and EBBS-Benefits scores are mostly associated with kinesiophobia. Thus, we recommend that fear of movement, fatigue, and exercise capacity should also be considered prior to exercise prescription/consultation, regardless of the axSpA subtype. The results obtained in this study may also help identify problems with adherence to exercise and determine optimal facilitators in patients with axSpA. Future studies should explore other psychometric properties of EBBS, such as sensitivity and specificity in the axSpA population, investigate the effects of different approaches on regulating barrier/benefit perceptions, and explore the possible differences between cultures regarding exercise perceptions.
APPENDIX. Turkish version of Exercise Benefits/Barriers Scale .
Footnotes
Ethics Committee Approval: The study protocol was approved by the İzmir Katip Çelebi University Non-Intervantional Studies Ethics Committee (date: 21.03.2018, no: 117). The study was conducted in accordance with the principles of the Declaration of Helsinki.
Informed Consent: A written informed consent was obtained from each patient.
Author Contributions: Idea/concept, supervision: D.B., Design: D.B., D.O.K., S.A. Data collection: D.C.S., E.D.E., G.D., E.A.A., S.G.; Analysis and/or interpretation, writing the article: D.C.S.; Literature review: D.B, D.C.S.; Critical review: D.B., D.O.K., S.A.
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
Citation: Sarac DC, Durak Ediboglu E, Ozer Kaya D, Duran G, Akatay EA, Gucenmez S, et al. Validity and reliability of the Turkish version of Exercise Benefits/Barriers Scale: Perceived exercise benefits and barriers of patients with different axial spondyloarthritis subtypes. Arch Rheumatol 2024;39(3):447-458. doi: 10.46497/ ArchRheumatol.2024.10720.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet. 2017;390:73–84. doi: 10.1016/S0140-6736(16)31591-4. [DOI] [PubMed] [Google Scholar]
- 2.Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: A systematic review and meta-analysis. Ann Rheum Dis. 2015;74:65–73. doi: 10.1136/annrheumdis-2013-203582. [DOI] [PubMed] [Google Scholar]
- 3.Bohn R, Cooney M, Deodhar A, Curtis JR, Golembesky A. Incidence and prevalence of axial spondyloarthritis: Methodologic challenges and gaps in the literature. Clin Exp Rheumatol. 2018;36:263–274. [PubMed] [Google Scholar]
- 4.Michelena X, López-Medina C, Marzo-Ortega H. Non-radiographic versus radiographic axSpA: What's in a name. iv18-24Rheumatology (Oxford) 2020;59(Suppl4) doi: 10.1093/rheumatology/keaa422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuksel Karsli T, Bayraktar D, Ozer Kaya D, Oz HE, Gucenmez S, Gercik O, et al. Comparison of physical activity levels among different sub-types of axial spondyloarthritis patients and healthy controls. Mod Rheumatol. 2021;31:1202–1207. doi: 10.1080/14397595.2021.1891676. [DOI] [PubMed] [Google Scholar]
- 6.Millner JR, Barron JS, Beinke KM, Butterworth RH, Chasle BE, Dutton LJ, et al. Exercise for ankylosing spondylitis: An evidence-based consensus statement. Semin Arthritis Rheum. 2016;45:411–427. doi: 10.1016/j.semarthrit.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 7.van der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van den Bosch F, Sepriano A, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2017;76:978–991. doi: 10.1136/annrheumdis-2016-210770. [DOI] [PubMed] [Google Scholar]
- 8.Sveaas SH, Bilberg A, Berg IJ, Provan SA, Rollefstad S, Semb AG, et al. High intensity exercise for 3 months reduces disease activity in axial spondyloarthritis (axSpA): A multicentre randomised trial of 100 patients. Br J Sports Med. 2020;54:292–297. doi: 10.1136/bjsports-2018-099943. [DOI] [PubMed] [Google Scholar]
- 9.Perrotta FM, Musto A, Lubrano E. New insights in physical therapy and rehabilitation in axial spondyloarthritis: A review. Rheumatol Ther. 2019;6:479–486. doi: 10.1007/s40744-019-00170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phang JK, Khor AYK, Kwan YH, Ng CT, Fong W. Physical activity in patients with axial spondyloarthritis in a multi-ethnic south-east Asian country. BMC Rheumatol. 2021;5:38–38. doi: 10.1186/s41927-021-00211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fabre S, Molto A, Dadoun S, Rein C, Hudry C, Kreis S, et al. Physical activity in patients with axial spondyloarthritis: A cross-sectional study of 203 patients. Rheumatol Int. 2016;36:1711–1718. doi: 10.1007/s00296-016-3565-5. [DOI] [PubMed] [Google Scholar]
- 12.Ortabag T, Ceylan S, Akyüz A, Bebis H. The validity and reliability of the exercise benefits/barriers scale for Turkish Military nursing students. S Afr J Res Sport Phys Educ Recreation. 2010;32:55–70. doi: 10.4314/sajrs.v32i2.59297. [DOI] [Google Scholar]
- 13.Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann Rheum Dis. 2009;68:777–783. doi: 10.1136/ard.2009.108233. [DOI] [PubMed] [Google Scholar]
- 14.Sechrist KR, Walker SN, Pender NJ. Development and psychometric evaluation of the exercise benefits/ barriers scale. Res Nurs Health. 1987;10:357–365. doi: 10.1002/nur.4770100603. [DOI] [PubMed] [Google Scholar]
- 15.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25:3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 16.Akkoc Y, Karatepe AG, Akar S, Kirazli Y, Akkoc N. A Turkish version of the Bath Ankylosing Spondylitis Disease Activity Index: Reliability and validity. Rheumatol Int. 2005;25:280–284. doi: 10.1007/s00296-003-0432-y. [DOI] [PubMed] [Google Scholar]
- 17.Jenkinson TR, Mallorie PA, Whitelock HC, Kennedy LG, Garrett SL, Calin A. Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index. J Rheumatol. 1994;21:1694–1698. [PubMed] [Google Scholar]
- 18.Yanik B, Gürsel YK, Kutlay S, Ay S, Elhan AH. Adaptation of the Bath Ankylosing Spondylitis Functional Index to the Turkish population, its reliability and validity: Functional assessment in AS. Clin Rheumatol. 2005;24:41–47. doi: 10.1007/s10067-004-0968-6. [DOI] [PubMed] [Google Scholar]
- 19.Duruöz MT, Doward L, Turan Y, Cerrahoglu L, Yurtkuran M, Calis M, et al. Translation and validation of the Turkish version of the Ankylosing Spondylitis Quality of Life (ASQOL) questionnaire. Rheumatol Int. 2013;33:2717–2722. doi: 10.1007/s00296-013-2796-y. [DOI] [PubMed] [Google Scholar]
- 20.Akgul O, Bodur H, Ataman S, Yurdakul FG, Capkin E, Gurer G, et al. Clinical performance of ASAS Health Index in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: Real-world evidence from Multicenter Nationwide Registry. Rheumatol Int. 2020;40:1793–1801. doi: 10.1007/s00296-020-04680-8. [DOI] [PubMed] [Google Scholar]
- 21.Aydemir O, Güvenir T, Küey L, Kültür S. Hastane anksiyete ve depresyon ölçeği Türkçe formunun geçerlilik ve güvenilirlik çalişmasi. Turk Psikiyatri Derg. 1997;8:280–287. [Google Scholar]
- 22.Tunca Yılmaz Ö, Yakut Y, Uygur F, Uluğ N. Tampa Kinezyofobi Ölçeği’nin Türkçe versiyonu ve test-tekrar test güvenirliği. Fizyoter Rehabil. 2011;22:44–49. [Google Scholar]
- 23.Swinnen TW, Vlaeyen JWS, Dankaerts W, Westhovens R, de Vlam K. Activity limitations in patients with axial spondyloarthritis: A role for fear of movement and (re)injury beliefs. J Rheumatol. 2018;45:357–366. doi: 10.3899/jrheum.170318. [DOI] [PubMed] [Google Scholar]
- 24.Everitt BS. The Cambridge Dictionary of Statistics. 2. Cambridge: Cambridge University Press; 2002. [Google Scholar]
- 25.Nunnally JC, Bernstein IH. Psychometric theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- 26.Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71. [PMC free article] [PubMed] [Google Scholar]
- 27.Ries JD, Echternach JL, Nof L, Gagnon Blodgett M. Test-retest reliability and minimal detectable change scores for the timed "up & go" test, the six-minute walk test, and gait speed in people with Alzheimer disease. Phys Ther. 2009;89:569–579. doi: 10.2522/ptj.20080258. [DOI] [PubMed] [Google Scholar]
- 28.McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: Are available health status surveys adequate. Qual Life Res. 1995;4:293–307. doi: 10.1007/BF01593882. [DOI] [PubMed] [Google Scholar]
- 29.Bulmer MG. Principles of Statistics. New York: Dover Publications; 1979. [Google Scholar]
- 30.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863–863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farahani LA, Parvizy S, Mohammadi E, Asadi-Lari M, Kazemnejad A, Hasanpoor-Azgahdy SB, et al. The psychometric properties of exercise benefits/ barriers scale among women. Electron Physician. 2017;9:4780–4785. doi: 10.19082/4780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swinnen TW, Scheers T, Lefevre J, Dankaerts W, Westhovens R, de Vlam K. Physical activity assessment in patients with axial spondyloarthritis compared to healthy controls: A technology-based approach. e85309PLoS One. 2014;9 doi: 10.1371/journal.pone.0085309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arends S, Hofman M, Kamsma YP, van der Veer E, Houtman PM, Kallenberg CG, et al. Daily physical activity in ankylosing spondylitis: Validity and reliability of the IPAQ and SQUASH and the relation with clinical assessments. R99Arthritis Res Ther. 2013;15 doi: 10.1186/ar4279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coulter EH, McDonald MT, Cameron S, Siebert S, Paul L. Physical activity and sedentary behaviour and their associations with clinical measures in axial spondyloarthritis. Rheumatol Int. 2020;40:375–381. doi: 10.1007/s00296-019-04494-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knapik A, Dąbek J, Brzęk A. Kinesiophobia as a problem in adherence to physical activity recommendations in elderly polish patients with coronary artery disease. Patient Prefer Adherence. 2019;13:2129–2135. doi: 10.2147/PPA.S216196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Larsson C, Ekvall Hansson E, Sundquist K, Jakobsson U. Impact of pain characteristics and fear-avoidance beliefs on physical activity levels among older adults with chronic pain: A population-based, longitudinal study. BMC Geriatr. 2016;16:50–50. doi: 10.1186/s12877-016-0224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bayraktar D, Yuksel Karsli T, Ozer Kaya D, Sarac DC, Gucenmez S, Gercik O, et al. Is the international physical activity questionnaire (IPAQ) a valid assessment tool for measuring physical activity of patients with axial spondyloartritis. Musculoskelet Sci Pract. 2021;55:102418–102418. doi: 10.1016/j.msksp.2021.102418. [DOI] [PubMed] [Google Scholar]
- 38.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int J Behav Nutr Phys Act. 2011;8:115–115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Rourke N, Hatcher L, Stepanski EJ. A Step-byStep Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling. North Carolina: SAS Institute and Wiley; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.