Abstract
Background
Gadoxetic acid (EOB)-enhanced magnetic resonance imaging (MRI) (EOB-MRI) can be used as a one-stop examination for detecting liver tumors and evaluating liver function.
Purpose
The study aimed to assess the functional liver reserve (FLR) using the T1 map from the hepatobiliary phase of EOB-MRI by conducting a comparison with the results of conventional FLR tests and the technetium-99m (99mTc)-galactosyl serum albumin (GSA) scintigraphy.
Materials and methods
The retrospective data from 43 patients were included in the study. The regions of interest covered the entire liver. The data acquired from each EOB-MRI slice were summed to derive voxel-by-voxel values. The average sum of the T1 values (pre- and post-enhancement), ∆T1, and ∆T1 ratios were calculated. The HH15, LHL15, and LU15 values were calculated from the GSA scintigraphy. The results of conventional FLR tests, such as the indocyanine green retention rate at 15 min (ICGR15), the Child-Pugh classification (CPC), and the albumin-bilirubin (ALBI) and albumin-indocyanine green evaluation (ALICE) scores, were obtained.
Results
The T1 pre- and post-sum values showed a weak correlation with the LHL15 (r=0.36 and 0.38, respectively). A strong correlation was observed between the liver volume and the T1 pre- and post-sum values (r=0.86 and 0.76, respectively). A moderate correlation was observed between the T1 mean and the ALBI and ALICE values (r=0.58 and 0.49, respectively) and between the ∆T1 ratio and the CPC, ALBI, and ALICE values (r=−0.40, 0.58, and −0.55, respectively). The T1 post-sum values showed a moderate correlation with the ALBI scores (r=0.47) and a weak correlation with the ALICE scores (r=0.38). Furthermore, the LU15 values showed a weak correlation with the ICGR15 and model for end-stage liver disease (MELD) scores (r=−0.32 and −0.34, respectively).
Conclusions
Representative indices, such as the T1 mean and ∆T1 ratio, demonstrated a better relationship with conventional FLR indices compared with volumetric radiological indices. Therefore, we propose that the T1 post-sum can be used as an FLR index.
Keywords: 99mtc-gsa scintigraphy, functional liver reserve, gadoxetic acid, mri, t1 map
Introduction
Evaluation of the functional liver reserve (FLR) is important to eliminate the risk of postoperative liver failure [1]. Several indices have been proposed, such as the indocyanine green retention rate at 15 min (ICGR15), Child-Pugh classification (CPC) [1], model for end-stage liver disease (MELD) [2], albumin-bilirubin (ALBI) [3], albumin-indocyanine green evaluation (ALICE) [4], technetium-99m (99mTc)-galactosyl serum albumin (GSA) (99mTc-GSA) scintigraphy [5], and gadoxetic acid (EOB)-enhanced magnetic resonance imaging (MRI) (EOB-MRI) [6,7]. The ICGR15, CPC, MELD, ALBI, and ALICE are conventional indices based mainly on biochemical tests, while the 99mTc-GSA scintigraphy and EOB-MRI are based on radiological imaging. Evaluation of the FLR based on tomographic images is useful because it can be simulated preoperatively. A diseased liver has an inhomogeneous function [8]; therefore, examinations that evaluate the FLR, such as GSA scintigraphy, have the advantage of estimating postoperative remnant liver function. Several authors have previously reported on postoperative remnant liver function [9,10].
Furthermore, EOB-MRI exhibits excellent detection of primary liver and metastatic cancers, and its preoperative usefulness is widely recognized. The EOB is taken to the hepatocytes by transporters and excreted into the bile; therefore, liver function can be evaluated by quantifying the contrast media accumulated in the hepatocytes. Consequently, EOB-MRI can be used as a one-stop examination for liver tumor detection and liver function evaluation [8,11]. Several approaches have been attempted to evaluate liver function [11-16]. Among them, T1 mapping is not dependent on the MRI parameters; therefore, it is highly reliable and reproducible [16]. The T1 value measurement for the entire liver was obtained by the sum of each pixel of the MRI scan to evaluate the FLR. To examine the possibility of FLR assessment by quantifying the EOB taken up by the liver using T1 mapping, the T1 value index obtained from T1 mapping was compared with conventional FLR indices.
Materials and methods
Participants
This study was conducted according to the Declaration of Helsinki (as revised in 2013). In addition, the Institutional Ethical Review Board of Tokyo Medical University approved this study (approval number: T2020-0330) and waived the requirement for individual consent for the retrospective analysis.
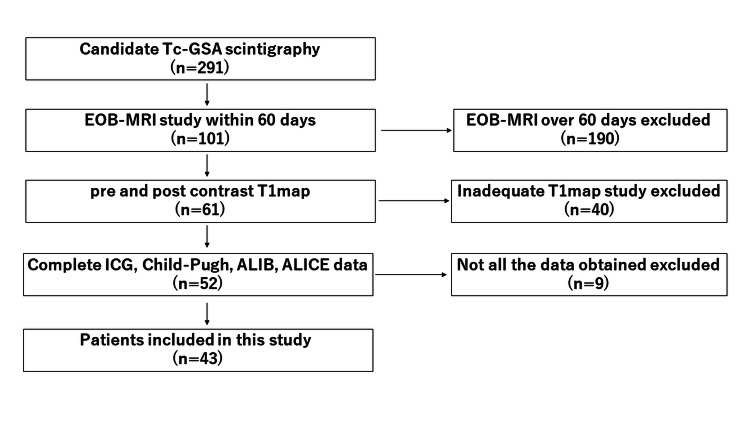
Patients were selected from radiological reporting system entries between January 2014 and April 2020 (Figure 1). The inclusion criterion was that GSA scintigraphy and EOB-MRI were performed on the patient. The exclusion criteria were as follows: (1) the time between the GSA scintigraphy and EOB-MRI was ≥60 d; (2) a T1 map was not obtained either before or after administration of the EOB; (3) preoperative portal vein embolization was performed; and (4) the patient's data did not include all the ICGR15, CPC, ALBI, and ALICE values.
Figure 1. Flowchart showing participant selection details.
GSA acquisition
The GSA single-photon emission computed tomography (SPECT) with high-resolution collimator and CT fusion images were acquired using a Symbia Intevo system (Siemens Healthcare AG, Munich, Germany), which combines SPECT with CT. The GSA scintigraphy was performed on patients after an overnight fast. First, 185 MBq of GSA (Nihon Medi-Physics Co., Ltd., Tokyo, Japan) was injected into the patient's antecubital vein. A bolus injection of radiotracer was followed by 20 mL of saline. Sequential anterior abdominal 64×64 matrix size images, including the liver and heart, were acquired every 30 s for 16 min using a gamma camera's large field of view (FOV). The hepatic SPECT data (60 steps, 15 s/step, 360°, 128×128 matrices) were acquired during the first 20-35 min. The SPECT images were reconstructed with attenuation and scatter correction using the ordered-subset expectation-maximization (OS-EM) algorithm (three iterations, eight subsets) with a 7-8-mm voxel size. Subsequently, CT was performed.
EOB-MRI acquisition
The MRIs were performed using a 3 Tesla (3T) MRI system (MAGNETOM Vida or MAGNETOM Skyra, Siemens AG, Erlangen, Germany); T1-weighted, T2-weighted, diffusion-weighted, and dynamic images were obtained. First, 0.025 mmol/kg of EOB was injected via the patient's antecubital vein. Then, contrast media was injected at 2 mL/s, followed by 40 mL of saline at the same speed. A T1 map was obtained before and 20 min after the injection of the contrast media. The parameters of the T1 map were as follows: TR/TE/FA 5.08 msec/2.34 msec/3°, 15°, matrix 156×256, FOV 380 mm, reduced FOV (RFOV) 81.3%, CAIPIRINHA 4 (2×2), slice thickness 4 mm, gap 0.8 mm, slice per slab 64, and scan time 21 s.
Analysis
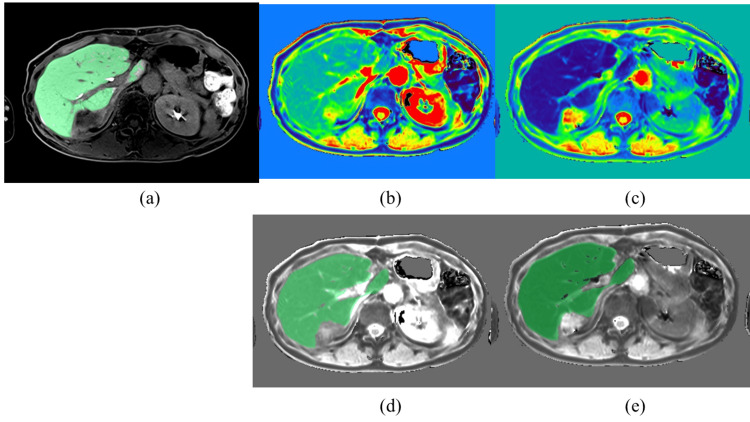
The region of interest (ROI) was set on the whole liver where the expected tumor and major vessels in the hepatobiliary phase were copied, and the ROI was pasted on the T1 map. After the T1 value at each voxel was measured (Figure 2), the indices were calculated using the following formulas: ΔT1=Σ voxel (T1 pre-contrast−T1 post-contrast), T1 sum=Σ voxel (T1 pre-contrast or T1 post-contrast), T1 mean=Σ voxel (T1 sum/total numbers of voxel), and ΔT1 ratio=(T1 pre-sum−T1 post-sum)/T1 pre-sum.
Figure 2. Axial cut MR images illustrate the whole liver T1 value measurement method.
(a) ROI was set on the entire liver where the expected tumor and major vessels in the hepatobiliary phase (green area) were copied.
(b) Pre-contrast T1 map (color map).
(c) Post-contrast T1 map (color map).
(d) ROI pasted on the pre-contrast T1 map (grayscale).
(e) ROI pasted on the post-contrast T1 map (grayscale).
MR: magnetic resonance; ROI: region of interest
The whole liver's volume was determined to evaluate the relationship between the liver volume and FLR. The volume was calculated semi-automatically based on the hepatobiliary phase by setting a threshold value and then excluding the major vessels and tumors. The following liver functional parameters of the GSA scintigraphy were calculated: HH15, representing the retention of the tracer in the blood; LHL15, representing the uptake of the tracer in the liver; and LU15, representing the cumulative liver uptake of the tracer between 15 and 16 min after injection. The parameters were calculated using the following formulas: HH15=heart count at 15 min/heart count at 3 min, LHL15=liver count at 15 min/sum of the liver and heart counts at 15 min, LU15=(total injection dose)×100%, where C(t) is the time-activity curve for the liver. The total injected dose was calculated as the difference in the radioactivity of the syringe before and after injection [17].
Results of the conventional FLR indices, including the ICGR15, CPC, MELD, ALBI, and ALICE, were obtained and calculated from the patient's medical records [4,18].
Statistical analysis
Data are presented as the mean±standard deviation. The Pearson product-moment correlation coefficient was used to evaluate the correlation between the GSA scintigraphy indices (HH15, LHL15, and LU15) and the EOB-MRI indices (T1 mean, T1 pre-sum, T1 post-sum, ΔT1, and ΔT1 ratio). In addition, the GSA scintigraphy and EOB-MRI indices were used to evaluate the correlation between the liver volume and conventional FLR indices by the Pearson product-moment correlation coefficient (r). The correlation strengths were determined r as follows: |r|≥0.7, strong; 0.7>|r|≥0.4, moderate; 0.4>|r|≥0.2, weak; and 0.2>|r|, no correlation.
Examinations that estimate remnant liver function, such as the LU15, T1 pre-sum, and T1 post-sum, were evaluated to determine whether a significant difference was present between the classified categories using a student t-test or a Kruskal-Wallis test when there was a significant correlation. Conventional FLR indices were classified into the following categories based on previous reports: (1) ICGR15 <20%, ≥20%; (2) CPC A, B; (3) MELD <10, ≥10; (4) ALBI 1, 2a, 2b; and (5) ALICE 1, 2, 3 [2,4,19,20]. Receiver operating characteristic (ROC) curves were created for the classifications found to be significant from these results; subsequently, the sensitivity and specificity were calculated by the Youden index.
The relationship between the FLR indices and postoperative complication score was evaluated using Spearman's rank correlation coefficient. The postoperative complication score was classified by the Clavien-Dindo grading system [21]. If a significant correlation was observed, the difference between the two grades provided by the Clavien-Dindo grading system, grade 1 and ≥grade 2, was compared by the Mann-Whitney U test. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 28.0 (Released 2021; IBM Corp., Armonk, New York, United States).
Results
Forty-three patients were enrolled in this study; the patients' diseases included hepatocellular carcinoma (12), metastatic tumor (23), cholangiocellular carcinoma (four), gallbladder carcinoma (two), and bile duct carcinoma (two). Of the 43 patients, 31 had no specific liver disease, and the underlying liver diseases of the remaining patients were hepatitis B (seven), hepatitis C (four), and alcoholic liver disease (one) (Table 1).
Table 1. Characteristics of the study sample.
ICGR15: indocyanine green retention rate at 15 min; CPC: Child-Pugh classification; MELD: model for end-stage liver disease; ALBI: albumin-bilirubin; ALICE: albumin-indocyanine green evaluation; HCC: hepatocellular carcinoma; Mets: metastatic tumor; CCC: cholangiocellular carcinoma; GB Ca: gallbladder carcinoma; Bile duct Ca: bile duct carcinoma
| Parameters | ||
| Age (mean) | 64 | |
| Sex | Male | 24 |
| Female | 19 | |
| ICGR15 (%) | 11 | |
| CPC | A | 41 |
| B | 2 | |
| MELD score | <10% | 42 |
| ≥10% | 1 | |
| ALBI score | 1 | 25 |
| 2a | 9 | |
| 2b | 9 | |
| ALICE score | 1 | 19 |
| 2 | 22 | |
| 3 | 2 | |
| Underlying liver disease | Viral hepatitis B | 7 |
| Viral hepatitis C | 4 | |
| Alcoholic | 1 | |
| None | 31 | |
| Disease | HCC | 12 |
| Mets | 23 | |
| CCC | 4 | |
| GB Ca/Bile duct Ca | 2/2 | |
| Surgery | Yes | 30 |
| No | 13 | |
| Clavien-Dindo grade | 1 | 20 |
| 2 | 4 | |
| 3a | 6 |
Classification of conventional FLR
The mean ICGR15 for all the patients was 11.0±6.34%. Thirty-nine patients had <20%, and four patients had ≥20%. The numbers of patients classified into CPC A and B were 41 and 2, respectively. The mean MELD score of all the patients was 1.23±3.48, with 42 patients having a score of <10 and one patient having a score of ≥10. The mean ALBI grade of all the patients was −2.60±0.48, with 25, nine, and nine patients classified into grades 1, 2a, and 2b, respectively. The mean ALICE grade of all the patients was −2.15±0.40, with 19, 22, and two patients classified into grades 1, 2, and 3, respectively (Table 1).
Correlation between the T1 map and GSA scintigraphy
A significant weak correlation was observed between the T1 pre- and post-sum and the LHL15 (r=−0.36 and −0.38, p=0.02 and 0.01, respectively). The other combination of T1 mapping and GSA scintigraphy indices did not exhibit a significant correlation (Table 2).
Table 2. Correlation between T1 map and GSA scintigraphy indices.
Correlation coefficient (p-value), *p<0.05
HH15: heart count ratio after 15 min compared to after 3 min; LHL15: ratio of liver count to the sum of heart and liver count after 15 min; LU15: cumulative liver uptake of the tracer from 15 to 16 minutes after injection of 99mTc-GSA; GSA: galactosyl serum albumin; 99mTc-GSA: technetium-99m-galactosyl serum albumin
| HH15 | LHL15 | LU15 | |
| T1 mean | −0.15 (0.35) | −0.21 (0.18) | −0.05 (0.77) |
| T1 pre-sum | 0.24 (0.12) | −0.36* (0.02) | −0.29 (0.06) |
| T1 post-sum | 0.16 (0.31) | −0.38* (0.01) | −0.25 (0.11) |
| ΔT1 | 0.24 (0.13) | −0.23 (0.15) | −0.23 (0.14) |
| ΔT1 ratio | 0.05 (0.78) | 0.19 (0.23) | 0.08 (0.63) |
Influence of the liver volume
A strong correlation was observed between the liver volume and T1 pre- and post-sum (r=0.86 and 0.76, p<0.001 and <0.001, respectively). A moderate correlation was observed between the liver volume and ∆T1 (r=0.66, p<0.001), and a significant weak correlation was observed with HH15 and LU15 (r=0.33 and −0.30, p=0.03 and 0.047, respectively) (Table 3).
Table 3. Correlations between the radiological functional liver reserve and liver volume.
*p<0.05, **p<0.01
HH15: heart count ratio after 15 min compared to after 3 min; LHL15: ratio of liver count to the sum of heart and liver count after 15 min; LU15: cumulative liver uptake of the tracer from 15 to 16 minutes after injection of 99mTc-GSA; 99mTc-GSA: technetium-99m-galactosyl serum albumin
| Radiological index | Correlation coefficient | P-value |
| HH15 | 0.33* | 0.031 |
| LHL15 | −0.29 | 0.058 |
| LU15 | −0.31* | 0.047 |
| T1 mean | 0.07 | 0.669 |
| T1 pre-sum | 0.86** | <0.001 |
| T1 post-sum | 0.76** | <0.001 |
| ΔT1 | 0.67** | <0.001 |
| ΔT1 ratio | −0.19 | 0.226 |
Correlation between the radiological and conventional FLR indices
The T1 mean showed a moderate correlation with the ALBI and ALICE grades (r=0.58 and 0.49, p<0.001 and <0.001, respectively) and a weak correlation with the CPC (r=0.36, p=0.02). The T1 post-sum showed a moderate correlation with the ALBI grade (r=0.46, p=0.002) and a weak correlation with the ALICE grade (r=0.38, p=0.01). A mild correlation was observed between the ∆ T1 ratio and the CPC and ALBI and ALICE grades (r=−0.4, 0.58, and −0.55, p=0.008, <0.001, and <0.001, respectively). A significant weak correlation was observed between the HH15 value and ALICE grade (r=−0.33, p=0.03) and between the LU15 and ICGR15 values (r=−0.32, p=0.04) and the MELD score (r=−0.34, p=0.03) (Table 4).
Table 4. Correlations between radiological and conventional functional liver reserve indices.
Correlation coefficient, (p-value), *p<0.05
ALBI: albumin-bilirubin; ALICE: albumin-indocyanine green evaluation; CPC: Child-Pugh classification; HH15: heart count ratio after 15 min compared to after 3 min; ICGR15: indocyanine green retention rate at 15 min; LHL15: ratio of liver count to the sum of heart and liver count after 15 min; LU15: cumulative liver uptake of the tracer from 15 to 16 minutes after injection of 99mTc-GSA; 99mTc-GSA: technetium-99m-galactosyl serum albumin; MELD: model for end-stage liver disease
| ICGR15 | CPC | MELD score | ALBI score | ALICE score | |
| HH15 | −0.11 (0.50) | −0.18 (0.24) | −0.04 (0.80) | −0.26 (0.09) | −0.33* (0.03) |
| LHL15 | −0.28 (0.07) | −0.10 (0.52) | −0.28 (0.07) | −0.11 (0.49) | −0.10 (0.51) |
| LU15 | −0.32* (0.04) | 0.14 (0.36) | −0.34* (0.03) | 0.12 (0.46) | −0.06 (0.73) |
| T1 mean | 0.08 (0.60) | 0.36* (0.02) | 0.07 (0.67) | 0.58* (<0.001) | 0.49* (<0.001) |
| T1 pre-sum | −0.05 (0.75) | −0.10 (0.54) | 0.23 (0.15) | 0.17 (0.28) | 0.09 (0.57) |
| T1 post-sum | 0.12 (0.44) | 0.15 (0.33) | 0.20 (0.21) | 0.46* (0.002) | 0.38* (0.01) |
| ΔT1 | −0.20 (0.21) | −0.30 (0.05) | 0.18 (0.26) | −0.16 (0.32) | −0.21 (0.17) |
| ΔT1 ratio | −0.26 (0.09) | −0.40* (0.008) | −0.06 (0.72) | 0.58* (<0.001) | −0.55* (<0.001) |
Evaluating the methods for estimating remnant liver function, such as the LU15 and T1 sum, demonstrated a significant correlation between the LU15 and ICGR15 values and the T1 post-sum and ALBI and ALICE grades. The LU15 values <20% and ≥20% were 24.75 and 19.88, respectively, which was significant (p<0.001). The T1 post-sum values of the ALBI grades 1, 2a, and 2b were 2.07, 2.5, and 2.8×107, respectively; a significant difference was observed between grades 1 and 2b (p=0.006). The T1 post-sum values of the ALICE grades 1, 2, and 3 were 2.06, 2.46, and 3.04×108, respectively; a significant difference was observed between grades 1 and 2 (p=0.02).
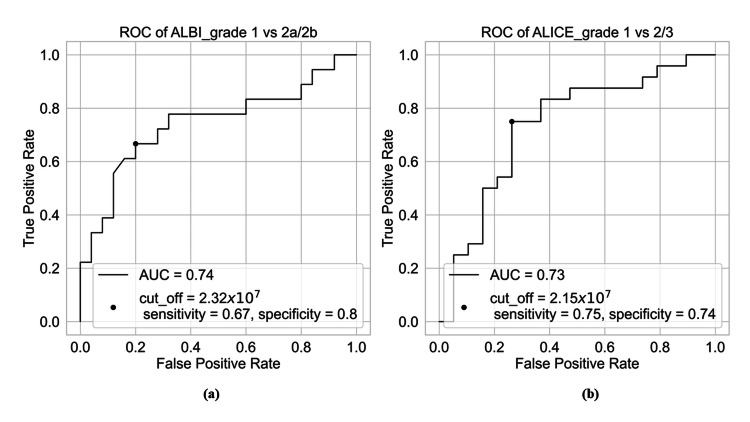
The Az value distinguishing ALBI grades 1 and 2a or 2b was 0.74 (95% CI: 0.58-0.90) if the cutoff value was 2.32×107; the sensitivity was 0.67 and the specificity was 0.8 (Figure 3a). In contrast, the Az value distinguishing between ALICE grades 1 and 2 or grade 3 was 0.74 (95% CI: 0.58-0.89) if the cutoff value was 2.15×107; the sensitivity was 0.75 and the specificity was 0.74 (Figure 3b).
Figure 3. ROC curve analysis for classifying ALBI and ALICE indices into grades 1 and 2 or above.
(a) Az value distinguishing ALBI grades 1 and 2a or 2b was 0.74 if the cutoff value was 2.32×107, sensitivity was 0.67, and specificity was 0.8.
(b) Az value distinguishing ALICE grades 1 and 2 or 3 was 0.73 if the cutoff value was 2.15×107, sensitivity was 0.75, and specificity was 0.74.
ROC: receiver operating characteristic; ALBI: albumin-bilirubin; ALICE: albumin-indocyanine green evaluation
Postoperative complications, classified using the Clavien-Dindo grading system, occurred in 20, four, and six cases in grades 1, 2, and 3, respectively. No indices showed significant differences between grade 1 and Grades 2 or 3.
Discussion
This study's findings demonstrated that the T1 post-sum can evaluate FLR; therefore, it can be used to estimate remnant liver function. Previously, authors have reported that only LU15 could evaluate remnant liver function while considering focal liver function and simulating liver resection [10]. The T1 post-sum showed a stronger correlation between the LU15 values and the conventional FLR indices in cases of relatively maintained liver function, such as in patients with CPC A.
The T1 sum strongly correlates with liver volume regardless of whether the measurement is performed before or after contrast enhancement. This correlation is more robust compared with that of GSA scintigraphy, possibly because of spatial resolution differences in each modality and the uptake mechanisms, i.e., EOB is taken up by the organic anion transporting polypeptide (OATP) 1B3 [22], while GSA binds to the asialoglycoprotein receptors on the membranes of hepatocytes [17]. Furthermore, GSA underestimates the function of the liver's left lobe and overestimates that of the right lobe [23]. Considering that a significant factor in surgical decisions is remnant liver volume, EOB-MRI is more suitable for evaluating remnant liver function compared with GSA scintigraphy [10,11,24].
This study's findings clarified that surrogate values, such as the T1 mean and ΔT1 ratio, correlate more strongly with conventional functional liver indices compared with the T1 sum. Representative values, such as average value and T1 shortening ratio, have been previously reported to correlate well [11-16]. No previously reported studies have used the sum of the T1 values for each pixel for the total amount of the entire liver. A surrogate value is based on the premise that the function of the entire liver is homogenous. Therefore, if the ROI is set on a locally strong fibrosis area in inhomogeneous parenchyma, the liver function may be underestimated [8].
The EOB-MRI and ICGR15 values showed weak correlations with the FLR indices, partially because they have the same transporter, OATP1 [22,25]. Kim et al. have reported that EOB-MRI's signal intensity is a better predictor of postoperative complications compared with ICGR15 results [6]. However, this study's findings showed no significant difference in the FLR indices between patients with and without complications; these results contradict those reported by Kim et al. [6]; this is perhaps because the liver function of the patients in this study was better compared with their patients.
Furthermore, the T1 post-sum significantly correlated with both the ALBI and ALICE grades. ALBI and ALICE grades can further stratify CPC A, which is indicated for surgery [4,18]. Therefore, the T1 post-sum may allow for the subclassification of patients' eligibility for surgery. The ALBI and ALICE grades are indicators based on albumin and are likely strongly influenced by the serum albumin levels. Albumin and bilirubin have been reported as confounding factors for the contrast effect in the hepatobiliary phase; therefore, the T1 post-sum can be used as an index of FLR [26].
This study's limitations include that it used retrospective data and the number of participants included was small. However, this study's results are valuable in that they show the efficacy of the T1 post-sum index obtained using EOB-MRI by comparing it with the conventionally used FLR indices. Unlike several previous studies, this study successfully evaluated the estimation of remnant liver function. In the future, a reliable cutoff T1 post-sum value should be set by collecting data from more cases. Another limitation is that the T1 post-sum may be affected by the contrast media in the bile duct, causing a weaker correlation between the liver volume and the T1 pre-sum. However, we suggest that this limitation can be ignored because the T1 post-sum correlates strongly with the liver volume.
Conclusions
Representative indices, such as the T1 mean and ∆T1 ratio, show better relationships with conventional FLR indices compared with volumetric radiological indices. The T1 post-sum, which is the sum of the T1 values for each pixel of the whole liver in the EOB-MRI's hepatobiliary phase, can be used as an index of the FLR.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. The Institutional Ethical Review Board of Tokyo Medical University issued approval T2020-0330.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: Department of Radiology, Tokyo Medical University declare(s) a grant from GE Healthcare Pharma. Kazuhiro Saito declare(s) personal fees from Bayer. Department of Radiology, Tokyo Medical University declare(s) a grant from Bayer. Kazuhiro Saito declare(s) personal fees from Eisai. Department of Radiology, Tokyo Medical University declare(s) a grant from Eisai. Department of Radiology, Tokyo Medical University declare(s) a grant from Nihon Medi-Physics.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Kazuhiro Saito, Kei Takase
Acquisition, analysis, or interpretation of data: Kazuhiro Saito, Kei Takase, Yu Tajima, Yoichi Araki, Kenji Uchida, Daisuke Hakamata, Katsutoshi Sugimoto, Daisuke Yuunaiyama, Yuki Takara
Drafting of the manuscript: Kazuhiro Saito, Kei Takase, Yu Tajima, Kenji Uchida, Daisuke Hakamata, Daisuke Yuunaiyama, Yuki Takara
Critical review of the manuscript for important intellectual content: Kazuhiro Saito, Kei Takase, Yu Tajima, Yoichi Araki, Kenji Uchida, Daisuke Hakamata, Katsutoshi Sugimoto
References
- 1.Assessment of preoperative liver function for surgical decision making in patients with hepatocellular carcinoma. Kokudo T, Hasegawa K, Shirata C, et al. Liver Cancer. 2019;8:447–456. doi: 10.1159/000501368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Model for end-stage liver disease (MELD) and allocation of donor livers. Wiesner R, Edwards E, Freeman R, et al. Gastroenterology. 2003;124:91–96. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 3.Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. Johnson PJ, Berhane S, Kagebayashi C, et al. J Clin Oncol. 2015;33:550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Assessment of preoperative liver function in patients with hepatocellular carcinoma - the albumin-indocyanine green evaluation (ALICE) grade. Kokudo T, Hasegawa K, Amikura K, et al. PLoS One. 2016;11:0. doi: 10.1371/journal.pone.0159530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benefit of technetium-99m galactosyl human serum albumin scintigraphy instead of indocyanine green test in patients scheduled for hepatectomy. Ohkura Y, Mizuno S, Kishiwada M, et al. Hepatol Res. 2014;44:0–28. doi: 10.1111/hepr.12248. [DOI] [PubMed] [Google Scholar]
- 6.Prediction of posthepatectomy liver failure: MRI with hepatocyte-specific contrast agent versus indocyanine green clearance test. Kim DK, Choi JI, Choi MH, Park MY, Lee YJ, Rha SE, Jung SE. AJR Am J Roentgenol. 2018;211:580–587. doi: 10.2214/AJR.17.19206. [DOI] [PubMed] [Google Scholar]
- 7.Estimation of liver function using T1 mapping on Gd-EOB-DTPA-enhanced magnetic resonance imaging. Katsube T, Okada M, Kumano S, et al. Invest Radiol. 2011;46:277–283. doi: 10.1097/RLI.0b013e318200f67d. [DOI] [PubMed] [Google Scholar]
- 8.Preoperative remnant liver function evaluation using a routine clinical dynamic Gd-EOB-DTPA-enhanced MRI protocol in patients with hepatocellular carcinoma. Wang Y, Zhang L, Ning J, et al. Ann Surg Oncol. 2021;28:3672–3682. doi: 10.1245/s10434-020-09361-1. [DOI] [PubMed] [Google Scholar]
- 9.(99m)Tc-GSA SPECT/CT fusion imaging for hepatectomy candidates with extremely deteriorated ICG value. Sumiyoshi T, Okabayashi T, Negoro Y, et al. Jpn J Radiol. 2018;36:537–543. doi: 10.1007/s11604-018-0753-0. [DOI] [PubMed] [Google Scholar]
- 10.Prognostic value of future liver remnant LU15 index of 99mTc-galactosyl serum albumin scintigraphy for predicting posthepatectomy liver failure. Tomita K, Chiba N, Ochiai S, et al. PLoS One. 2021;16:0. doi: 10.1371/journal.pone.0247675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Functional remnant liver volumetry using Gd-EOB-DTPA-enhanced magnetic resonance imaging (MRI) predicts post-hepatectomy liver failure in resection of more than one segment. Araki K, Harimoto N, Kubo N, et al. HPB (Oxford) 2020;22:318–327. doi: 10.1016/j.hpb.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Quantitative evaluation of liver function with T1 relaxation time index on Gd-EOB-DTPA-enhanced MRI: comparison with signal intensity-based indices. Kamimura K, Fukukura Y, Yoneyama T, et al. J Magn Reson Imaging. 2014;40:884–889. doi: 10.1002/jmri.24443. [DOI] [PubMed] [Google Scholar]
- 13.Assessing liver function in liver tumors patients: the performance of T1 mapping and residual liver volume on Gd-EOBDTPA-enhanced MRI. Duan T, Jiang H, Xia C, et al. Front Med (Lausanne) 2020;7:215. doi: 10.3389/fmed.2020.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Measuring hepatic functional reserve using T1 mapping of Gd-EOB-DTPA enhanced 3T MR imaging: a preliminary study comparing with (99m)Tc GSA scintigraphy and signal intensity based parameters. Nakagawa M, Namimoto T, Shimizu K, et al. Eur J Radiol. 2017;92:116–123. doi: 10.1016/j.ejrad.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Measuring hepatic functional reserve using low temporal resolution Gd-EOB-DTPA dynamic contrast-enhanced MRI: a preliminary study comparing galactosyl human serum albumin scintigraphy with indocyanine green retention. Saito K, Ledsam J, Sourbron S, Hashimoto T, Araki Y, Akata S, Tokuuye K. Eur Radiol. 2014;24:112–119. doi: 10.1007/s00330-013-2983-y. [DOI] [PubMed] [Google Scholar]
- 16.Preliminary clinical study of the safety of hepatectomy predicted by gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced T1 mapping magnetic resonance imaging. Liu J, Li Q, Shi N, Chen Y, Li Y, Zhang M, Huang Y. JGH Open. 2021;5:382–389. doi: 10.1002/jgh3.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.A new liver functional study using Tc-99m DTPA-galactosyl human serum albumin: evaluation of the validity of several functional parameters. Koizumi K, Uchiyama G, Arai T, Ainoda T, Yoda Y. Ann Nucl Med. 1992;6:83–87. doi: 10.1007/BF03164647. [DOI] [PubMed] [Google Scholar]
- 18.Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Wang YY, Zhong JH, Su ZY, et al. Br J Surg. 2016;103:725–734. doi: 10.1002/bjs.10095. [DOI] [PubMed] [Google Scholar]
- 19.One thousand fifty-six hepatectomies without mortality in 8 years. Imamura H, Seyama Y, Kokudo N, et al. Arch Surg. 2003;138:1198–1206. doi: 10.1001/archsurg.138.11.1198. [DOI] [PubMed] [Google Scholar]
- 20.Albumin-bilirubin (ALBI) grade as part of the evidence-based clinical practice guideline for HCC of the Japan Society of Hepatology: a comparison with the liver damage and Child-Pugh classifications. Hiraoka A, Kumada T, Kudo M, et al. Liver Cancer. 2017;6:204–215. doi: 10.1159/000452846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Dindo D, Demartines N, Clavien PA. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hepatic uptake of the magnetic resonance imaging contrast agent Gd-EOB-DTPA: role of human organic anion transporters. Leonhardt M, Keiser M, Oswald S, et al. Drug Metab Dispos. 2010;38:1024–1028. doi: 10.1124/dmd.110.032862. [DOI] [PubMed] [Google Scholar]
- 23.Accurate estimation of functional liver volume using Gd-EOB-DTPA MRI compared to MDCT/(99m)Tc-SPECT fusion imaging. Morine Y, Enkhbold C, Imura S, et al. Anticancer Res. 2017;37:5693–5700. doi: 10.21873/anticanres.12006. [DOI] [PubMed] [Google Scholar]
- 24.The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Schindl MJ, Redhead DN, Fearon KC, Garden OJ, Wigmore SJ. Gut. 2005;54:289–296. doi: 10.1136/gut.2004.046524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Transporters involved in the hepatic uptake of (99m)Tc-mebrofenin and indocyanine green. de Graaf W, Häusler S, Heger M, et al. J Hepatol. 2011;54:738–745. doi: 10.1016/j.jhep.2010.07.047. [DOI] [PubMed] [Google Scholar]
- 26.Serum albumin, total bilirubin, and patient age are independent confounders of hepatobiliary-phase gadoxetate parenchymal liver enhancement. Matoori S, Froehlich JM, Breitenstein S, et al. Eur Radiol. 2019;29:5813–5822. doi: 10.1007/s00330-019-06179-8. [DOI] [PubMed] [Google Scholar]