Abstract
Purpose
Chordomas are rare malignant tumors that occur primarily in the axial skeleton. We seek to analyze trends affecting five-year overall survival (5y OS) among patients with primary spinal chordomas (PSC) of the vertebrae and sacrum/pelvis.
Methods
The Surveillance, Epidemiology, and End Results (SEER) Program was used to identify patients with PSC (ICD-O-3 histology codes 9370/3, 9371/3, and 9372/3) of the spine or sacrum/pelvis. Multivariate and univariate survival analyses were conducted to assess demographic, disease, or treatment characteristic trends.
Results
Eight-hundred-ninety-six patients diagnosed with PSC were identified. Patients 0–54 years at diagnosis had improved 5y OS compared to those either 55–69 years (HR = 1.78; p = 0.046) or those between 70 and 85 + years (HR = 3.92; p < 0.001). Histology impacted 5y OS: Cox regression demonstrated variance among the three histologies assessed (p < 0.001), while univariate analysis demonstrated patients with dedifferentiated chordoma (1.0% of cohort; 33.3% [1.9,64.7]) and chondroid chordoma (2.0% of cohort; 52.5% [26.1,78.9]) had decreased 5y OS compared to those with general chordoma (72.2% [68.8,75.6]; p < 0.001). Nonmarried patients had decreased 5y OS on univariate analysis (65.2% [59.4,71.0] versus 76.2% [72.0,80.4]), with widowed patients being the primary driver of this on subanalysis. Treatment with gross total resection was associated with increased 5y OS (HR = 0.22, p < 0.001), as was treatment with radiotherapy (HR = 0.69, p = 0.030).
Conclusion
Patient age and marital status were significant demographic factors associated with changes in 5y OS among those with PSC. PSC histology is a potentially important prognostic factor in the management of disease.
Keywords: Spinal chordoma, Surgical oncology, SEER program, Population-level analysis, Histologic cancer analysis
Introduction
Chordomas are rare, slow-growing, low-grade malignant tumors originating from remnants of the embryonic notochord [1, 2]. These tumors predominantly occur along the axial skeleton, most frequently in the sacral region (55%), followed by the skull base (35%), and vertebral column (10%; 1,2). Although generally slow growing, chordomas can be locally invasive and aggressive, infiltrating proximal muscles, nerves, and vascular structures. The annual incidence rate of new chordoma diagnoses is approximately one to two cases per million each year, with a slightly higher frequency in males than females [2].
Previous SEER database research has identified that age, race, tumor size, extent of resection, and tumor stage are important prognostic factors for primary spinal chordomas. Older patients tend to have poorer survival outcomes due to increased comorbidities and compromised physiological conditions [1–7]. Additionally, a larger tumor diameter is also associated with a poorer prognosis [5]. A variety of studies have demonstrated the association of surgical resection with improved survival, with those who undergo gross total resection (GTR) showing better outcomes than those who undergo subtotal resection (STR) or do not receive surgery at all [3, 5–7]. A 2018 study using the SEER database found that surgical resection for sacral tumors was significantly associated with improved survival [2].
Despite the growing body of research on chordomas, there is still much to learn about the impact of various factors on patient survival. Further investigation is needed to better understand the influence of demographic characteristics, treatment modalities, and other prognostic indicators, on patient outcomes. To date, there have been no multi-center studies of primary spinal chordoma that explore tumor histology or the impact of median household income on overall survival.
This study aims to explore this gap by conducting a retrospective epidemiologic survival study of primary spinal chordomas. Building upon previous research using the SEER database, this study will analyze the specific characteristics of primary spinal chordomas and their associations with patient demographics, treatment modalities, histological subtype, primary location, and survival outcomes.
Materials and methods
Patient identification
This retrospective study utilized data queried from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) 17-registry Incidence database, which lists cases diagnosed between the years 2000 and 2020 [8]. Patients diagnosed with primary spinal chordoma (PSC) were identified using the International Classification of Diseases for Oncology, Third Edition (ICD-O-3) histology codes 9370/3: Chordoma, NOS, 9371/3: Chondroid chordoma, and 9372/3: Dedifferentiated chordoma, with the further specification of the primary site as the spine (C41.2) or sacrum/pelvis (C41.4 and C76.3) through the appropriate SEER site recode. Additionally, all cases were required to have a behavior code ICD-O-3 characterized as “Malignant.” The variables of interest were selected based on findings from previous studies and treatment factors associated with the standard of care [1, 5]. These variables are also the standard variables available via the SEER Program.
Data analysis
Data was analyzed in SPSS (Version 29.0; Armonk, NY: IBM Corp.). A p-value of < 0.05 was used as the cutoff for statistical significance; 95% confidence intervals reported in brackets [95% CI]. Multivariate analysis was conducted via Cox regression based on five-year overall survival (5y OS). Kaplan-Meier (KM) survival curves were generated and compared using log-rank analysis for univariate and subanalysis. Surgical codes were determined based on the 2022 SEER Staging Manual [9]. Incomplete/missing entries were omitted from each individual analysis conducted.
Results
Cohort overview
Eight-hundred-ninety-six patients were identified with Primary Spinal Chordoma (PSC). Median five-year age bracket was 60–64 years, while cumulative five-year overall survival was 71.4% [68.0%,74.8%]. A summary of patient demographic and disease characteristic information can be found in Table 1. Patient age was divided into three approximately equal groups to allow for strong statistical comparison.
Table 1.
Demographic, disease, and treatment information for patients diagnosed with primary spinal chordoma
| Variable | Number (% of Cohort; n = 896) |
|---|---|
| Age at Diagnosis | |
| 0–54 Years | 287 (32.0%) |
| 55–69 Years | 302 (33.7%) |
| 70–85+ | 307 (34.3%) |
| Sex | |
| Female | 359 (40.1%) |
| Male | 537 (59.9%) |
| Race | |
| White | 765 (85.4%) |
| Asian or Pacific Islander | 87 (9.7%) |
| American Indian/Alaska Native | 2 (0.2%) |
| Black | 32 (3.6%) |
| Unknown | 10 (1.1%) |
| Primary Site | |
| Spine | 383 (42.7%) |
| Sacrum/Pelvis | 513 (57.3%) |
| Histology | |
| Chordoma, NOS | 869 (97.0%) |
| Chondroid Chordoma | 18 (2.0%) |
| Dedifferentiated Chordoma | 9 (1.0%) |
| Marital Status | |
| Single | 334 (37.3%) |
| Married | 516 (57.6%) |
| Unknown | 46 (5.1%) |
| Median Household Income | |
| < $40,000-$79,999 | 426 (47.5%) |
| $80,000-$120,000+ | 470 (52.5%) |
| Stage | |
| Localized | 368 (41.1%) |
| Regional | 303 (33.8%) |
| Distant | 75 (8.4%) |
| Unknown | 150 (16.7%) |
| Radiotherapy (RT) | |
| No RT | 434 (48.4%) |
| RT | 434 (48.4%) |
| Unknown | 28 (3.1%) |
| RT-Surgery Sequence | |
| Before Surgery | 35 (3.9%) |
| After Surgery | 247 (27.6%) |
| Before and After | 24 (2.7%) |
| N/A | 590 (65.8%) |
| Chemotherapy | |
| No Chemotherapy | 864 (94.4%) |
| Chemotherapy | 50 (5.6%) |
| Surgical Procedure | |
| None | 237 (26.5%) |
| Subtotal Resection | 315 (35.2%) |
| Gross Total Resection | 308 (34.4%) |
| Unknown | 36 (4.0%) |
*NOS: Not Otherwise Specified
Patient demographic, disease characteristic, and treatment information for patients diagnosed with Primary Spinal Chordoma in the US between 2000 and 2020, as identified via the Surveillance, Epidemiology, and End Results (SEER) Program
Multivariate analysis
Cox regression analysis with respect to five-year overall survival was conducted for patients identified with PSC and can be found in Table 2. Increasing age was associated with decreased survival, with patient age between 70 and 85 + years at diagnosis associated with significantly decreased 5y OS (hazard ratio (HR) = 3.92, p < 0.001).Both chondroid chordoma (HR = 3.56, p = 0.015) and dedifferentiated chordoma (HR = 5.16, p < 0.001) histologies were associated with decreased 5y OS compared to those patients with unspecified histology. Treatment with radiotherapy was associated with increased 5y OS as well (HR = 0.69, p = 0.030). Surgical procedures notably improved survival, with gross total resection (GTR) showing the greatest benefit (HR = 0.22, p < 0.001). Additionally, advanced disease stage was associated with increased mortality, as patients with distant disease had a higher hazard of death (HR = 2.87, p < 0.001). The primary site variable showed significance with spinal tumors having decreased survival compared to the pelvic/sacral tumors (HR = 1.48, p = 0.036).
Table 2.
Cox regression analysis of five-year overall survival among patients with primary spinal chordoma
| Variable | p-value | Hazard Ratio |
|---|---|---|
| Age at Diagnosis | < 0.001 | N/A |
| 55–69 vs. 0–54 and 70–85+ | 0.046 | 1.78 |
| 70–85 + vs. 0–54 and 55–69 | < 0.001 | 3.92 |
| Sex | 0.35 | 1.18 |
| Race | 0.97 | N/A |
| Asian or Pacific Islander vs. White and Black | 0.81 | 0.94 |
| Black vs. White and Asian or Pacific Islander | 0.93 | 1.05 |
| Median Household Income ($80,000-$120,000 + vs. < $40,000-$79,999) | 0.74 | 1.06 |
| Marital Status (Married vs. Single) | 0.14 | 0.77 |
| Histology | < 0.001 | N/A |
| Chondroid Chordoma vs. NOS and Dedifferentiated Chordoma | 0.015 | 3.56 |
| Dedifferentiated Chordoma vs. NOS and Chondroid Chordoma | < 0.001 | 5.16 |
| Radiotherapy Yes vs. No | 0.030 | 0.69 |
| Chemotherapy Yes vs. No | 0.72 | 1.12 |
| Surgical Procedure | < 0.001 | N/A |
| STR vs. None and GTR | < 0.001 | 0.48 |
| GTR vs. None and STR | < 0.001 | 0.22 |
| Stage | < 0.001 | N/A |
| Regional vs. Localized and Distant | 0.008 | 1.67 |
| Distant vs. Localized and Regional | < 0.001 | 2.87 |
| Primary Site (Pelvis/Spine) | 0.036 | 1.48 |
Results from Cox regression analysis for five-year overall survival. Significant variables include age at diagnosis, median household income, histology, surgical procedure performed, stage, and primary site. Comparisons within categories are listed in the rows below italicized variables if relevant. Comparisons among three or more categories within a variable do not have an associated hazard ratio
Univariate survival analysis
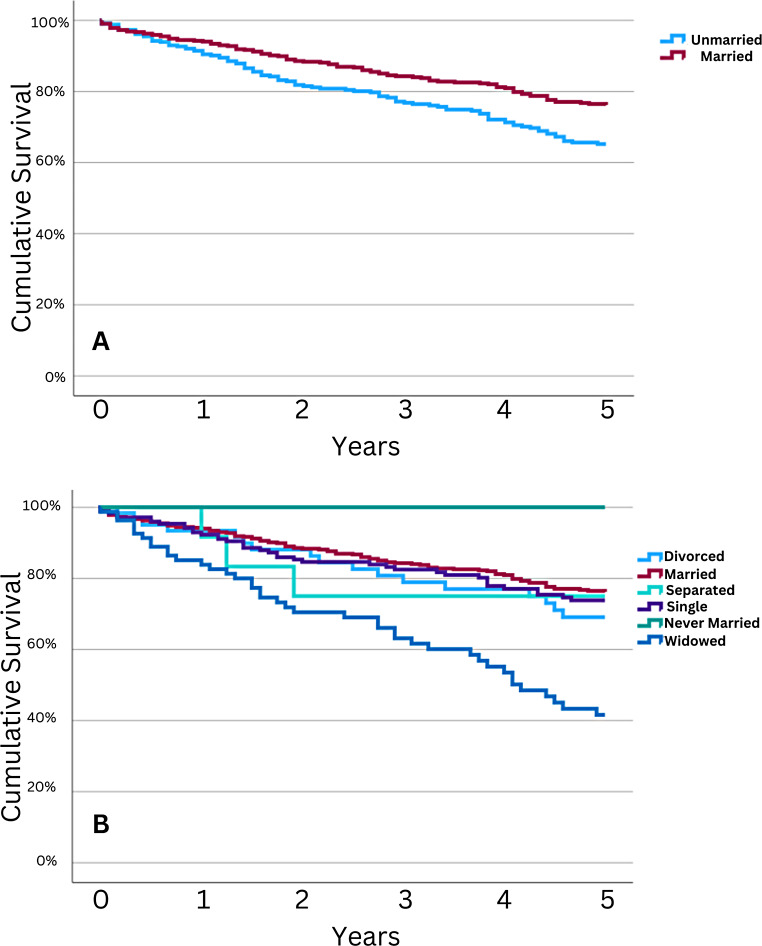
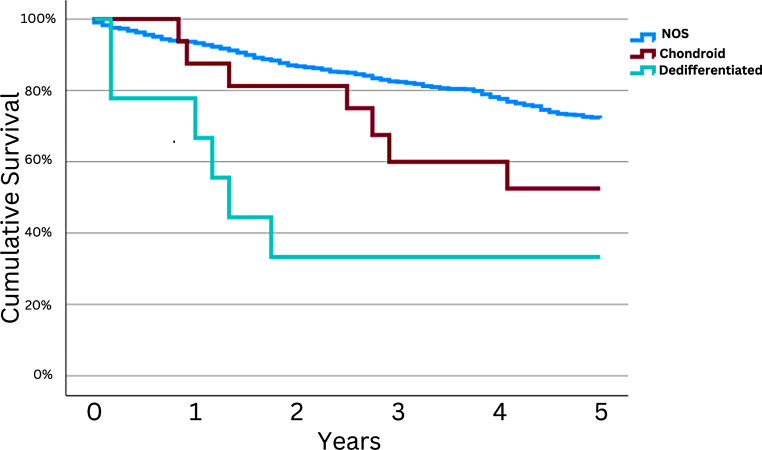
Univariate comparison of five-year overall survival (5y OS) can be found in Table 3. This analysis showed that age at diagnosis significantly impacted five-year OS, with patients aged 0–54 years and 55–69 years at diagnosis seeing increased 5y OS compared to those aged 70–85+ )84.5% and 79.0% versus 51.2%, respectively; p < 0.001). Concerning disease histology, patients with either chondroid chordomas or dedifferentiated chordomas had decreased 5y OS compared to those with unspecified histology (52.5% and 33.3% versus 72.2%, respectively; p < 0.001). Decreasing 5y OS was seen with increasing severity of summary stage, with those with local disease faring the best at 78.2%. Non-married patients had decreased 5y OS (65.2%) compared to married patients (76.2%; p = 0.001; see Fig. 1A). Subanalysis of marital status demonstrated widowed patients had significantly decreased 5y OS (41.6%) compared with all other marital statuses; married patients had the highest 5y OS at 76.2% (see Fig. 1B).
Table 3.
Univariate five-year overall survival (OS) analysis among patients with primary spinal chordoma
| Variable | OS [95% CI] | Five-year OS log-rank p-value |
|---|---|---|
| Age at Diagnosis | < 0.001 | |
| 0–54 Years | 84.5% [79.7,89.3] | |
| 55–69 Years | 79.0% [73.8,84.2] | |
| 70–85+ | 51.2% [44.8,57.6] | |
| Sex | 0.53 | |
| Female | 70.1% [64.7,75.5] | |
| Male | 72.3% [68.1,76.5] | |
| Race | 0.41 | |
| White | 70.9% [67.3,74.5] | |
| Asian or Pacific Islander | 70.9% [59.7,82.1] | |
| American Indian/Alaska Native | N/A* | |
| Black | 83.1% [67.3,98.9] | |
| Histology | < 0.001 | |
| Chordoma NOS | 72.2% [68.8,75.6] | |
| Chondroid Chordoma | 52.5% [26.1,78.9] | |
| Dedifferentiated Chordoma | 33.3% [1.9,64.7] | |
| Marital Status | 0.001 | |
| Non-married | 65.2% [59.4,71.0] | |
| Married | 76.2% [72.0,80.4] | |
| Income | 0.081 | |
| < $40,000-$79,999 | 68.6% [63.8,73.4] | |
| $80,000-$120,000 | 74.4% [69.8,79.0] | |
| Stage | < 0.001 | |
| Localized | 78.2% [73.2,83.2] | |
| Regional | 73.4% [67.8,79.0] | |
| Distant | 41.4% [27.2,55.6] | |
| Chemotherapy | 0.016 | |
| No Chemotherapy | 72.3% [68.9,75.7] | |
| Chemotherapy | 55.3% [39.1,71.5] | |
| Surgical Procedure | < 0.001 | |
| None | 48.6% [41.0,56.2] | |
| Subtotal Resection | 73.6% [68.0%,79.2] | |
| Gross Total Resection | 85.6% [81.2,90.0] | |
| Primary Site | 0.79 | |
| Sacrum/Pelvis | 71.0% [66.6,75.4] | |
| Vertebrae | 72.0% [66.8,77.2] | |
| Radiotherapy (RT) | 0.33 | |
| No RT | 70.6% [65.8,75.4] | |
| RT | 71.8% [67.0,76.6] | |
| RT Order | < 0.001 | |
| RT before surg | 93.0% [83.4,100.0] | |
| RT after surg | 81.1% [75.5,86.7] | |
| RT before + after surg | 88.4% [72.8,100.0] | |
| N/A | 65.4% [61.0,69.8] | |
| Marital Status Subanalysis | < 0.001 | |
| Divorced | 69.1% [56.5,81.7] | |
| Married | 76.2% [72.0,80.4] | |
| Separated | 75.0% [50.0,100.0] | |
| Single (never married) | 73.8% [66.4,81.2] | |
| Unmarried | N/A* | |
| Widowed | 41.6% [29.4,53.8] |
*One case identified
This table summarizes factors affecting five-year survival in spinal chordoma patients. Age, stage, histology, chemotherapy, and surgical procedure are significantly associated with survival. Overall log-rank p-value is presented in the rightmost column
Fig. 1.
Five-year OS in Primary Spinal Chordoma Patients Stratified by Marital Status. Kaplan-Meier curves depicting OS for patients diagnosed with primary spinal chordoma stratified by marital status at diagnosis. A: Comparison of unmarried patients to those that were married at diagnosis. Unmarried patients had decreased 5y OS (65.2% [59.4,71.0]) compared to those that were married at diagnosis (76.2% [72.0,80.4]). B: Comparison of patients further stratified by marital status (separated, single (never married), etc.). Widowed patients had significantly decreased 5y OS (41.6% [29.4,53.8]) compared to all other categories, and comparison amongst these groups was statistically significant (p < 0.001)
Treatment with chemotherapy was associated with decreased 5y OS (55.3% versus 72.3%). Comparison between surgical techniques (none versus subtotal resection versus gross total resection, GTR) demonstrated GTR to offer superior 5y OS (85.6%; p < 0.001). Analysis of patient sex, race, median household income, disease location, and treatment with radiotherapy (RT) did not demonstrated differences in 5y OS. While treatment with RT did not demonstrate survival benefit, when assessed, neoadjuvant RT offered the highest benefit to 5y OS (93.0%), while patients not treated with both surgery and RT fared the worst (65.4% 5y OS).
Demographic factor analysis
The majority of patients diagnosed with primary spinal chordoma were between 55 and 85 + years old, with a noticeable decrease in survival rates as age increased. Multivariate Cox regression analysis found a statistically significant association between increasing age and decreased survival, with hazard ratios (HR) of 1.78 for the 55-69-year-old group and 3.92 for the 70–85 + year-old group, compared to the 0-54-year-old group (p < 0.001; see Table 2). Kaplan-Meier analysis showed a significant difference in five-year survival rates between the age groups, with the oldest age group (70–85+) having the poorest survival (51.2% [44.8,57.6], p < 0.001; see Table 3). No difference in 5y OS was present with respect to sex (p = 0.35), race (p = 0.97), median household income (p = 0.74), or marital status on multivariate analysis (p = 0.14; see Table 2). On univariate analysis, marital status (married versus non-married) was significant (p < 0.001), with married patients having increased 5y OS (76.2% versus 65.2%, respectively). Further analysis demonstrated widowed patients to be a significant driver of this trend, with 45y OS of 41.6% reported for this group.
Histology and stage
The vast majority of patients (97.0%) were diagnosed with Chordoma NOS with a smaller number of patients having Chondroid Chordoma (2.0%) or Dedifferentiated Chordoma (1.0%). Cox regression analysis showed overall histological significance with five-year OS (p < 0.001), with both chondroid (HR = 3.56, p = 0.015) and dedifferentiated chordoma (HR = 5.16, p < 0.001) linked to higher mortality compared to unspecified chordoma histologies (see Table 2). This trend was further assessed on univariate analysis, with patients diagnosed with dedifferentiated chordomas having the lowest associated 5y OS (33.3%) compared to 52.5% for chondroid chordomas and 72.2% for unspecified chordoma histologies (p < 0.001; see Fig. 2).
Fig. 2.
Univariate Survival OS Curve for Primary Spinal Chordomas Stratified by Histological Type. Kaplan-Meier OS curve depicting overall survival for Primary Spinal Chordoma patients stratified by histological types: Not Otherwise Specified, Chondroid, and Dedifferentiated Chordoma, demonstrating a significant difference in survival outcomes across time points (p < 0.001). 5y OS for Chordoma, NOS: 72.2% [68.8,75.6]; Chondroid Chordoma: 52.5% [26.1,78.9]; Dedifferentiated Chordoma: 33.3% [1.9,64.7]
The majority of patients in the cohort were diagnosed with localized disease (41.1%), followed by regional (33.8%) and distant (8.4%) disease. Cox regression analysis showed a statistically significant association between stage and survival (p < 0.001, see Table 2). This analysis found that distant disease, compared to local disease, was associated with increased mortality (HR = 2.87; p < 0.001). Patients with regional disease also had decreased 5y OS comparatively (HR = 1.67, p = 0.008). This trend was evident on univariate analysis as well, with patients with distant disease having significantly decreased 5y OS (41.4%) compared to both those with local and regional disease.
Radiotherapy (RT) and chemotherapy
Almost half of the patients (48.4%) received RT for treatment. This was associated with increased 5y OS (HR = 0.69, p = 0.030), though on univariate analysis this trend did not persist (p = 0.33).
Only a small percentage of patients (5.6%) received chemotherapy. Cox regression analysis did not find a statistically significant association between chemotherapy use and overall survival (p = 0.72, see Table 2). On univariate analysis, treatment with chemotherapy was associated with decreased 5y OS, with those treated with chemotherapy having a 5y OS of 55.3% versus 72.3% for those not receiving chemotherapy (p = 0.016).
Surgical procedure analysis
The study found that a majority of patients underwent either subtotal resection (STR) or gross total resection (GTR), with 35.2% and 34.4% receiving those respective treatments. Both STR and GTR had significantly reduced hazard ratios compared to those who received no surgery, with hazard ratios of 0.48 (p < 0.001) and 0.22 (p < 0.001), respectively (see Table 2). Univariate analysis demonstrated the same trend, with those treated with GTR faring better than those treated with STR (5y OS = 85.6% versus 73.6%, respectively).
Primary site
Analysis of PTC primary site demonstrated the majority of tumors were located in the sacrum/pelvis (57.3%) compared to the spine (42.7%; see Table 1). Cox regression analysis found a significant association between primary site and survival (p = 0.036), with a higher hazard ratio associated with patients diagnosed with a tumor in the pelvis compared to those with vertebral tumors (HR = 1.48, see Table 2). However, this trend did not persist on univariate survival analysis (p = 0.79).
Discussion
This analysis demonstrated increased five-year overall survival among patients with PSC on Cox regression analysis with respect to increasing patient age, disease histology, increasingly severe disease stage, PSC of the sacrum/pelvis compared to PSC of the vertebrae, and lack of surgical treatment. On multivariate analysis, increased patient age was associated with increased mortality (p < 0.001), with patients in the youngest age group (0–54 years of age at diagnosis) faring the best compared to both patients aged 55–69 years (HR = 1.78; p = 0.046) and those aged 70–85+ (HR = 3.92; p < 0.001). On univariate analysis, patients aged 70–85 + at diagnosis (5y OS: 51.2% [44.8,57.6]) had significantly increased mortality as compared to those aged 55–69 years (79.0% [73.8,84.2]) and those aged 0–54 years (84.5% [79.7,89.3]; p < 0.001). This trend is consistent with previous studies [1–3, 5–7], and is likely secondary to increased frailty and morbidities associated with patients diagnosed with cancer at an older age. These findings emphasize the importance of early diagnosis and intervention for chordoma, particularly in older patients, as they are at an increased risk for poorer survival.
While marital status was not significant on multivariate analysis (p = 0.14), on univariate analysis among all marital status subtypes (divorced, married, single (never married), etc.) demonstrated variation in 5y OS, with widowed individuals demonstrating significantly reduced 5y OS (41.6%) compared to those either separated, married, or single. Married patients had the highest survival (76.2% [72.0,80.4]. This finding suggests that socioeconomic factors, beyond the impact of age, may influence survival in chordoma patients.
The study found that a diagnosis of dedifferentiated chordoma was significantly associated with decreased survival (HR = 5.16; p < 0.001). This aligns with previous research highlighting the aggressive nature of this histological subtype in 18 subjects [10]. The five-year survival rate for dedifferentiated chordoma were 33.3% [1.9,64.7]. Chondroid chordomas were also associated with decreased 5y OS when compared to unspecified chordoma histologies (52.5% [26.1,78.9]. These findings underscore the importance of accurate histopathological classification for guiding treatment strategies and prognostication. This information could potentially be incorporated into the treatment and prognosis of patients with PSC and potentially chordomas in general.
The study also confirmed the critical role of surgical intervention in improving survival outcomes. Patients who underwent either subtotal resection (STR) or gross total resection (GTR) showed significantly reduced hazard ratios compared to those who received no surgery (p < 0.001). The hazard ratios were 0.48 (p < 0.001) for STR and 0.22 (p < 0.001) for GTR. Furthermore, Kaplan-Meier analysis demonstrated a significant difference in five-year survival rates based on surgical procedure (p < 0.001), with the highest 5-year survival rate observed in patients who underwent GTR (85.6% [81.2,90.0]), followed by STR (73.6% [68.0,79.2]), and the lowest in those who received no surgery (48.6% [41.0,56.2]). These results are consistent with previous studies emphasizing the importance of surgical resection in improving survival for spinal chordoma [3, 5–7]. Radiotherapy (RT) was also associated with increased survival (HR = 0.69, p = 0.030), and while this trend did not persist with univariate analysis (p = 0.33), subanalysis of patients treated with both surgery and RT demonstrated treatment with both modalities was associated with increased 5y OS, with neoadjuvant RT having the highest 5y OS (93.0% [83.4,100.0]). This is contrary to previous literature, which has not established a clear association between treatment with both RT and surgery to hold mortality benefit [11, 12].
The study also found a significant association between stage and overall survival (p < 0.001), highlighting the importance of early detection and intervention, a sentiment echoed by previous research emphasizing the importance of early detection and intervention for chordoma [1–3]. Patients diagnosed with distant disease had decreased survival both on multivariate (HR = 2.87, p < 0.001) and univariate (5y OS = 41.4% [27.2,55.6], p < 0.001) compared to those with localized disease. While chemotherapy use was statistically insignificant in the Cox regression model (p = 0.72, Table 3), Kaplan-Meier analysis showed a significant difference in 5-year survival between those who received chemotherapy fairing worse (55.3% [39.1,71.5]) than those who did not (72.3% [68.9,75.7], p = 0.016). There is an anticipated negative selection bias for patients receiving only chemotherapy as treatment; furthermore this phenomenon is possibly due to its usage among a small percentage of patients who likely had advanced disease, a finding also noted in previous studies [13].
Finally, the study found that a tumor located in the spine was associated with a significantly higher hazard ratio compared to tumors located in the sacrum/pelvis region (HR = 1.48, p = 0.036). This finding is consistent with a previous study that found a similar association between tumor location and survival [5]. This may be secondary to the complex anatomy of the sacrum, potentially greater risk of local invasion, and the difficulty in achieving complete resection in this region.
While this study offers valuable insights, it is important to acknowledge its limitations. The study relied on a multi-center database, potentially limiting the depth of information about individual patient-level factors. The national survival data does not include information related to hospital quality or patient volume for this condition. However, it is important to note that better outcomes for rare cancers are typically achieved in tertiary institutions with high patient volumes and specialized expertise [14, 15]. The ability to assess for differences between centers is not possible secondary to the de-identification of patient data within the SEER Program. Additionally, data on treatment-associated morbidity and patient frailty are lacking, although the authors recognize the significant influence of these factors on the choice of treatment modalities. Furthermore, the SEER Program does not provide specific details on the doses or agents used in the treatments, particularly with RT and chemotherapy. Finally, the curative intention of all treatments is assumed, as the SEER Program does not give any information on the curative or palliative intent with any therapies.
Acknowledgements
None.
Author contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by M.C.L., while data analysis was performed by K.E.A. The first draft of the manuscript was written by K.E.A. and M.C.L., and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
The datasets generated during and/or analysed during the current study are available in the SEER Program repository, https://seer.cancer.gov/.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All personal identifying information for patients was anonymized by Surveillance, Epidemiology, and End Results, so ethical approval and informed consent were waived.
Consent to participate
Informed consent was waived due to approved use of publicly accessible database and retrospective nature of the study.
Consent to publish
Consent to publish was waived due to approved use of publicly accessible database and retrospective nature of the study.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McMaster ML, Goldstein AM, Bromley CM et al (2001) Chordoma: incidence and survival patterns in the United States, 1973–1995. Cancer Causes Control CCC 12:1–11. 10.1023/a:1008947301735 [DOI] [PubMed] [Google Scholar]
- 2.Zuckerman SL, Bilsky MH, Laufer I (2018) Chordomas of the Skull Base, Mobile Spine, and Sacrum: an Epidemiologic Investigation of Presentation, Treatment, and Survival. World Neurosurg 113:e618–e627. 10.1016/j.wneu.2018.02.109 [DOI] [PubMed] [Google Scholar]
- 3.McGirt MJ, Gokaslan ZL, Chaichana KL (2011) Preoperative grading scale to predict survival in patients undergoing resection of malignant primary osseous spinal neoplasms. Spine J off J North Am Spine Soc 11:190–196. 10.1016/j.spinee.2011.01.013 [DOI] [PubMed] [Google Scholar]
- 4.Deb S, Brewster R, Pendharkar AV et al (2019) Socioeconomic predictors of Surgical Resection and Survival for patients with Osseous spinal neoplasms. Clin Spine Surg Spine Publ 32:125–131. 10.1097/BSD.0000000000000738 [DOI] [PubMed] [Google Scholar]
- 5.Huang J-F, Chen D, Sang C-M et al (2019) Nomogram for Individualized Prediction and prognostic factors for survival in patients with primary spinal chordoma: a Population-based longitudinal cohort study. World Neurosurg 128:e603–e614. 10.1016/j.wneu.2019.04.217 [DOI] [PubMed] [Google Scholar]
- 6.Mukherjee D, Chaichana KL, Parker SL et al (2013) Association of surgical resection and survival in patients with malignant primary osseous spinal neoplasms from the Surveillance, Epidemiology, and end results (SEER) database. Eur Spine J off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22:1375–1382. 10.1007/s00586-012-2621-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan Y, Lu L, Chen J et al (2018) Analysis of prognostic factors for survival in patients with primary spinal chordoma using the SEER Registry from 1973 to 2014. J Orthop Surg 13:76. 10.1186/s13018-018-0784-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Surveillance E, Results E (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER Research Data, 17 Registries, Nov 2023 Sub (2000–2021) - Linked To County Attributes - Time Dependent (1990–2022) Income/Rurality, 1969–2022 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2024, based on the November 2023 submission
- 9.Appendix C: Site Specific Coding Modules - 2022 SEER Coding and Staging Manual. In: SEER. https://seer.cancer.gov/archive/manuals/2022/appendixc.html. Accessed 14 Jun 2024
- 10.Hanna SA, Aston WJS, Briggs TWR, et al (2008) Sacral chordoma: can local recurrence after sacrectomy be predicted? Clin Orthop 466:2217–2223. 10.1007/s11999-008-0356-7 [DOI] [PMC free article] [PubMed]
- 11.Gendreau J, Kuo CC, Mehkri Y, et al (2023) Radiotherapy after gross-total resection and subtotal resection of spinal chordoma: a SEER database analysis of overall survival outcomes. J Neurosurg Spine 39:411–418. 10.3171/2023.5.SPINE2396 [DOI] [PubMed]
- 12.Gendreau JL, Gowda K, Kazemi F, et al (2024) Fractionated radiotherapy after gross-total resection of spinal chordoma: a systematic review of survival outcomes using individualized patient data. J Neurosurg Spine 1–8. 10.3171/2024.4.SPINE2491 [DOI] [PubMed]
- 13.Stacchiotti S, Casali PG (2011) Systemic therapy options for unresectable and metastatic chordomas. Curr Oncol Rep 13:323–330. 10.1007/s11912-011-0176-x [DOI] [PubMed]
- 14.Weitz J, Koch M, Friess H, Büchler MW (2004) Impact of volume and specialization for cancer surgery. Dig Surg 21:253–261. 10.1159/000080198 [DOI] [PubMed]
- 15.Stacchiotti S, Casali PG, Lo Vullo S, et al (2010) Chordoma of the mobile spine and sacrum: a retrospective analysis of a series of patients surgically treated at two referral centers. Ann Surg Oncol 17:211–219. 10.1245/s10434-009-0740-x [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available in the SEER Program repository, https://seer.cancer.gov/.