Abstract
Background
In Guinea, despite women’s recourse to antenatal care (ANC), little remains known about the use of focused antenatal care (FANC), contained in the ANC package.
Aim
The aim of this study was to analyse the frequency and factors associated with FANC, using data from the Demographic and Health Survey (DHS) 2018.
Setting
This study was conducted in Guinea.
Methods
This was a secondary analysis of data from the DHS conducted in 2018 in Guinea. It included all women who achieved at least one ANC visit in the last 2 years prior to the survey. Multivariate logistic regression was received to identify factors associated with FANC. Stata 16 software was used for the analysis.
Results
This study shows that in Guinea, between 2016 and 2018 only 33% of women undergoing ANC received a FANC. The most commonly used service was blood pressure measurement (93%), while the least commonly used service was deworming (42%). Factors associated with FANC were living in the Kindia region (odds ratio = 1.7; 95% confidence interval: 1.04–2.97); not intending to become pregnant for this pregnancy; belonging to a poor household; and having made 3, 4 or more ANC visits.
Conclusion
This study reports a low proportion of women receiving the full package of ANC.
Contribution
In order to improve this indicator, greater efforts need to be made in certain regions of the country to target pregnant women who achieve fewer ANC visits, carry pregnancies that were not intentional or belong to poorer households.
Keywords: focused antenatal care, frequency, factors associated, Demographic and Health Survey, Guinea
Introduction
Worldwide, 33 women die every hour from causes related to pregnancy, childbirth or postpartum.1 Since 2016, the World Health Organization (WHO) has been recommending focused antenatal care (FANC) for all pregnant women at antenatal clinics.1,2 Focused antenatal care enables serological screening for syphilis, prevention of malaria, anti-tetanus vaccination, prevention of mother-to-child transmission of HIV and detection of malnutrition. It consists of measuring – during antenatal care (ANC) – blood pressure, weight, height, uterine height, abdominal circumference, auscultating foetal sounds, assessing the physical condition, administering tetanus vaccine, providing sulphadoxine–pyrimethamine (SP) and long-acting insecticide-treated mosquito nets to prevent malaria, and providing ferric folic acid (FFA). These services help to monitor the progress of the pregnancy and prepare the woman to accept medical assistance during childbirth.1,2
However, the provision of maternal health services to pregnant women by healthcare providers in low-income countries still leaves much to be desired in terms of both quality of care and effective coverage of services.3 A study in 10 low-income countries in Asia and Africa reported that although a proportion of pregnant women reported having had four or more ANC visits, the care provided did not meet the standards of quality required.3
In Africa, several studies have reported on FANC; for example, in Mozambique, it was reported in 2019 that the majority of women reported having an ANC visit and that only 13% of them received quality services during these visits.4 In 2016 in Kenya, Chorongo et al. reported that 3 out of 10 women had used FANC services.2 Similarly, in a district of Malawi in 2017, only 8% of women who came for initial visits received FANC.5
There are several reasons for this FANC coverage. A study carried out in the context of limited resources reported that beliefs, traditions, customs and norms and the misallocation of resources were associated with the provision of respectful, quality maternal health services to women.6 Chorongo et al. pointed out that in Kenya, religion, women’s lack of knowledge about the components of FANC, long waiting times and unavailability of services were associated with non-receipt of FANC.2 As in Nigeria in 2023, Nwabueze et al. reported late onset of ANC, long waiting times and overcrowded facilities as factors influencing the provision of FANC,7 and Hussen et al. in 2022 in Ethiopia, reported poor infrastructure, inadequate skilled personnel, stockouts of consumables and non-functioning basic emergency obstetric care facilities as factors in poor quality maternal health services in the least developed countries.8 Konlan et al. in Ghana also reported that long distances to health facilities were one of the factors negatively influencing receipt of FANC by pregnant women.9
In 2011, Fores et al. in Ethiopia reported that women whose spouses were present during ANC were more likely to undergo urine and blood tests.10
In Guinea, FANC services are offered to pregnant women at the time of their consultation.11 However, little is documented about the provision of these services at either national level or regional level. Indeed, studies reporting on ANC focused on the number of ANC visits and not on the use of the services contained in the ANC package.12,13,14 As a result, aspects of the FANC such as the level of use of the various services in the package, the proportion of women covered by the full package and the factors favouring the use of the full ANC package remain to be documented. This study therefore aims to fill this knowledge gap by analysing the use of FANC services in Guinea, using data from the Demographic and Health Survey (DHS) 2018. The results of this study would help guide ANC policies and practices in Guinea. The objective of this study was to determine the frequency and factors associated with the use of FANC services (blood pressure measuring, urine and blood sampling, receipt of FFA, deworming and SP tablets) among women attending at least one ANC visit in Guinea between 2016 and 2018.
Research methods and design
Study design
This was a secondary analysis of data from Guinea DHS 2018. The DHS is a nationally representative cross-sectional household survey.
Study setting
Guinea is located in West Africa and had an estimated population of 13 million in 2014, 51.5% of whom were women.15 The majority of the population live in rural areas and are below the poverty line. The country comprises 33 prefectures organised into 7 administrative regions and 5 special communes forming the special region of Conakry. The government health system is organised into three levels: the primary level, comprising 407 rural and urban health centres, 26 district hospitals and 9 communal medical centres; the secondary level, comprising 8 regional hospitals; and the tertiary level, comprising 3 national hospitals.16
In general, 33% of women have their first birth before reaching the age of 18 years, and almost 30% of antenatal visits are initiated at the 4th month of pregnancy; 8 out of 10 women attended one ANC visit during pregnancy, but only 35% achieve four ANC visits.16 In terms of reproductive health, the total fertility rate is 4.8 children per woman. Men and women want an average of 5.4 and 7.1 children, respectively.17
Study population
The study population included all women aged 15–49 years with the most recent live birth, attending at least one ANC visit for that birth, in the last 2 years preceding the Guinea DHS 2018.
Study variables
Dependent variable
Our variable of interest was the use of all FANC services. This was a composite variable defined from the FANC service variables reported in the DHS 2018. They include blood pressure measurement, urine and blood sample collection, administration of FFA or dewormer and SP tablets. The ‘use of all FANC services’ was recoded as 1 ‘Yes’ if the woman was offered all of the single services listed; it was recoded as 0 ‘No’ if the woman did not receive one or more of these services.
Independent variables
Our independent variables were socio-demographic (age, level of education, marital status, socio-economic level, profession, residence, administrative region), desire for pregnancy and distance between home and health facility.
Data analysis
The characteristics of the study population were summarised as percentages with 95% confidence intervals (CI). Univariate and multivariate logistic regressions were used to identify factors associated with the use of FANC services. The study sample was weighted before analyses. All variables with a p-value ≤ 0.20 were included in the logistic regression model. The unadjusted and adjusted odds ratios (OR) were derived. The significance level was set at 5% with a 95% CI. Data were processed and analysed using Stata 17 software (Stata Corp, College Station, Texas, United States [US]).
Ethical considerations
This study followed all ethical standards for research without direct contact with human or animal subjects.
Results
Socio-demographic characteristics of the sample
A total of 2634 women (weighted number) were included in this study. Women aged between 25 years and 34 years were the most represented (42.3%). More than half (71.8%) had no formal education (Table 1). The majority (93.9%) were married and 43.7% had had 2 to 4 births.
TABLE 1.
Socio-demographic characteristics of women having attended at least one antenatal care visit for their most recent live birth, 2018 Demographic and Health Survey (N = 2634)§.
| Variables | n | % |
|---|---|---|
| Age group during pregnancy (years) | ||
| 15–19 | 499 | 19.4 |
| 20–24 | 625 | 23.9 |
| 25–29 | 671 | 25.2 |
| 30–34 | 451 | 17.1 |
| 35 or more | 388 | 14.5 |
| Education level | ||
| No formal education | 1898 | 71.8 |
| Primary | 345 | 13.0 |
| Secondary | 332 | 12.7 |
| Higher | 59 | 2.6 |
| Profession | ||
| Housewife | 750 | 27.3 |
| Trader or shopkeeper | 57 | 2.4 |
| Farmer | 26 | 1.0 |
| Service provider† | 1125 | 4.4 |
| Other professions‡ | 676 | 25.0 |
| Marital status | ||
| Unmarried | 158 | 6.1 |
| Married | 2476 | 93.9 |
| Residence area | ||
| Urban | 819 | 31.6 |
| Rural | 1815 | 68.4 |
| Administrative region | ||
| Boké | 369 | 10.5 |
| Conakry | 239 | 12.2 |
| Faranah | 366 | 10.8 |
| Kankan | 450 | 19.1 |
| Kindia | 372 | 16.0 |
| Labé | 308 | 10.6 |
| Mamou | 246 | 7.0 |
| N’Zérékoré | 284 | 14.0 |
| Parity during ANC | ||
| No birth | 515 | 19.9 |
| 1 previous birth | 504 | 19.1 |
| 2 to 4 previous births | 1148 | 43.7 |
| 5 or more previous births | 467 | 17.3 |
| Household wealth index | ||
| Poor | 1140 | 43.1 |
| Medium | 521 | 19.6 |
| Rich | 973 | 37.3 |
| Distance to the health facility perceived as a problem | ||
| Yes | 1221 | 44.3 |
| No | 1413 | 56.7 |
| Desired this pregnancy | ||
| Yes | 2196 | 83.3 |
| No | 438 | 16.7 |
ANC, antenatal care.
, Service provider;
, Other professions;
, Weighted number.
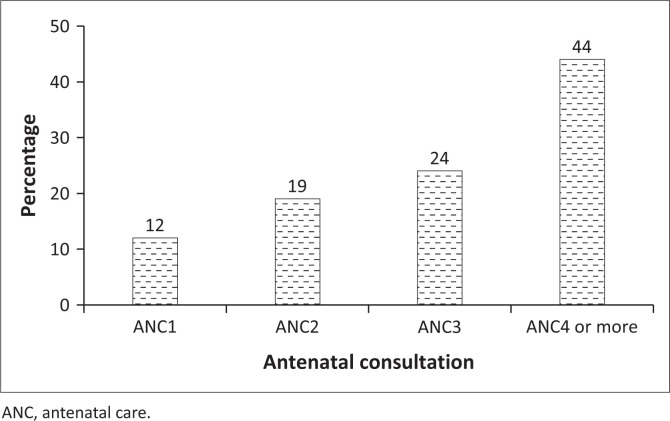
Antenatal care coverage per number of visits
Among women who had undergone ANC between 2016 and 2018, 12% had completed only one ANC visit; 19% and 24% had completed only 2 and 3 ANC visits, respectively (Figure 1). Those who had completed 4 or more ANC visits accounted for 44%.
FIGURE 1.
Antenatal care coverage by number of visits for the most recent births among women who attended at least one antenatal care visit, 2018 Demographic and Health Survey, Guinea.
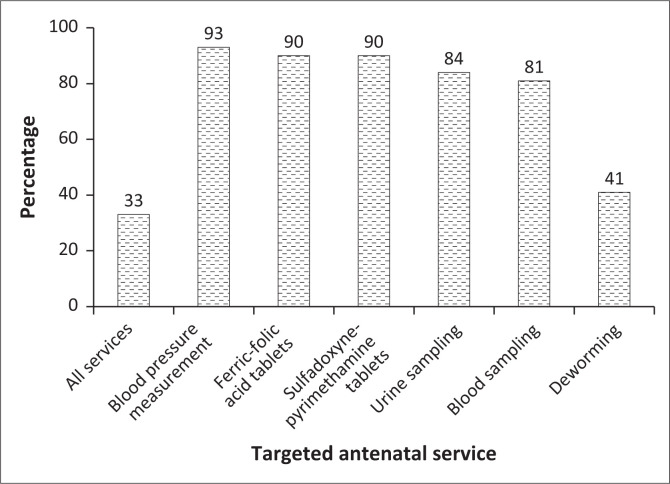
Use of focused antenatal care services
Only a third of the women (33%) who had undergone ANC received all FANC services reported in this survey (Figure 2). Blood pressure measurement was the most used service (93%) and the least used service was deworming (42%).
FIGURE 2.
Uptake of focused antenatal care services for the most recent live birth among women who achieved at least one antenatal care visit, 2018 Demographic and Health Survey, Guinea.
Factors associated with the use of the full package of antenatal care services
In the univariate analysis, the factors associated with the use of all FANC services were education level, residence area, administrative region, household wealth index, number of ANC visits and desire for pregnancy.
However, with the multivariate regression, the factors associated with the use of the package of ANC services were administrative region, number of ANC visits, household wealth index and desire for pregnancy (Table 2).
TABLE 2.
Univariate and multivariate analyses of factors associated with the use of all focused antenatal care services among 15–49 year-old women for their most recent live birth during the last 24 months that preceded the 2018 Demographic and Health Survey, Guinea (N = 2634).
| Variables | Received all FANC services (yes) |
||||||
|---|---|---|---|---|---|---|---|
| Effective | Crude OR | 95% CI | p | Adjusted OR | 95% CI | p | |
| Age group during pregnancy (years) | |||||||
| 15–19 | 499 | 0.9 | 0.65–1.22 | 0.473 | - | - | - |
| 20–24 | 625 | 1.1 | 0.85–1.42 | 0.464 | - | - | - |
| 25–29 | 671 | 1.0 | 0.77–1.33 | 0.924 | - | - | - |
| 30–34 | Ref | - | - | - | - | - | - |
| 35 or more | 273 | 0.9 | 0.67–1.26 | 0.606 | - | - | - |
| Profession | |||||||
| Housewife | 750 | 0.9 | 0.68–1.12 | 0.289 | 0.8 | 0.60–1.01 | 0.060 |
| Trader or shopkeeper | 57 | 1.4 | 0.71–2.69 | 0.327 | 0.8 | 0.42–1.78 | 0.689 |
| Farmer | 26 | 1.9 | 0.67–5.05 | 0.227 | 1.2 | 0.42–3.25 | 0.765 |
| Service provider | 1125 | Ref | - | - | Ref | - | - |
| Other professions | 676 | 1.4 | 1.02–1.79 | 0.032 | 1.0 | 0.76–1.62 | 0.996 |
| Education level | |||||||
| No formal education | 1898 | 0.5 | 0.26–0.90 | 0.022 | 0.8 | 0.37–1.67 | 0.531 |
| Primary | 345 | 0.7 | 0.33–1.26 | 0.205 | 0.9 | 0.40–1.91 | 0.728 |
| Secondary | 332 | 0.8 | 0.40–1.44 | 0.411 | 0.8 | 0.39–1.70 | 0.592 |
| Higher | 59 | Ref | - | - | Ref | - | - |
| Residence area | |||||||
| Urban | 819 | Ref | - | - | Ref | - | - |
| Rural | 1815 | 0.5† | 0.34–0.59 | 0.001 | 0.7† | 0.70–0.47 | 0.065 |
| Marital status | |||||||
| Unmarried | 158 | 1.2 | 0.84–1.79 | 0.274 | - | - | - |
| Married | 2476 | Ref | - | - | - | - | - |
| Administrative region | |||||||
| Boké | 369 | 0.3† | 0.17–0.54 | 0.001 | 0.6 | 0.35–1.21 | 0.173 |
| Conakry | 239 | Ref | - | - | Ref | - | - |
| Faranah | 366 | 0.7 | 0.40–1.09 | 0.113 | 1.6 | 0.90–2.77 | 0.112 |
| Kankan | 450 | 0.5 | 0.29–0.81 | 0.006 | 1.0 | 0.54–1.69 | 0.877 |
| Kindia | 372 | 1.1 | 0.66–1.70 | 0.000 | 1.8† | 1.08–3.05 | 0.025 |
| Labé | 308 | 0.3 | 0.17–0.49 | 0.796 | 0.6 | 0.35–1.11 | 0.107 |
| Mamou | 246 | 0.6 | 0.37–1.02 | 0.065 | 1.3 | 0.73–2.46 | 0.350 |
| N’Zérékoré | 284 | 1.1 | 0.66–1.87 | 0.001 | 2.8† | 1.51–5.13 | 0.001 |
| Distance to the health facility perceived as a problem | |||||||
| Yes | 1221 | 1.0 | 0.75–1.22 | 0.736 | - | - | - |
| No | 1413 | Ref | - | - | - | - | - |
| Number of ANC visits achieved | |||||||
| 1 visit | 324 | - | - | - | Ref | - | - |
| 2 visits | 502 | 1.4 | 0.91–2.22 | 0.113 | 1.3 | 0.82–1.92 | 0.296 |
| 3 visits | 660 | 2.7† | 1.78–4.21 | 0.001 | 2.4† | 1.63–3.65 | 0.001 |
| 4 visits or more | 1148 | 4.3† | 2.81–6.54 | 0.001 | 3.5† | 2.38–5.29 | 0.001 |
| Household wealth index | |||||||
| Poor | 1140 | 0.4† | 0.32–0.56 | 0.001 | 0.6† | 0.44–0.85 | 0.001 |
| Medium | 521 | 0.6† | 0.47–0.81 | 0.001 | 0.8 | 0.59–1.13 | 0.217 |
| Rich | 973 | Ref | - | - | Ref | - | - |
| Parity during ANC | |||||||
| No birth | 515 | Ref | - | - | - | - | - |
| 1 previous birth | 504 | 1.1 | 0.83–1.50 | 0.452 | - | - | - |
| 2–4 previous births | 1148 | 1.0 | 0.78–1.29 | 0.942 | - | - | - |
| 5 or more previous births | 467 | 0.8 | 0.62–1.15 | 0.295 | - | - | - |
| Desired this pregnancy | |||||||
| Yes | 2196 | Ref | - | - | Ref | - | - |
| No | 438 | 0.8 | 0.60–1.02 | 0.081 | 0.7† | 0.56–0.99 | 0.042 |
FANC, focused antenatal care; ANC, antenatal care; CI, confidence interval; OR, odds ratio; Ref, reference.
, p < 0.05.
Women in the N’Zérékoré region were three times more likely to receive all FANC services (odds ratio [OR] = 3; 95% confidence interval [CI]: 1.51–5.13; p = 0.001) compared with those in Conakry (Table 2). Similarly, women in Kindia were 1.8 (OR = 1.7; 95% CI: 1.08–3.05; p = 0.025) times more likely to receive all FANC services than women in Conakry.
Women who had undergone three ANCs visits and those who had undergone four or more ANCs visits were 2.4 (OR = 2.4; 95% CI: 1.63–3.65; p = 0.000) and 3.5 (OR = 3.5; 95% CI: 2.38–5.29; p = 0.000) times more likely to receive all FANC services, respectively, compared with those who had received one visit (Table 2).
Compared with rich women, poor women were 40% (OR = 0.6; 95% CI: 0.44 – 0.85; p = 0.001) less likely to receive all FANC services (Table 2).
Women with unintended pregnancies were 30% (OR = 0.7; 95% CI: 0.56 – 0.99; p = 0.042) less likely to use all FANC services compared with those with intended pregnancies (Table 2).
Discussion
This study shows that between 2016 and 2018, one-third of women undergoing ANC received all FANC services; blood pressure was measured in almost all women; however, less than half of women received deworming tablets. Women who were more likely to receive all FANC services were those living in the Kindia or N’Zérékoré regions and who had made three, four or more ANC visits. However, those who had not desired to get pregnant and belonged to a poor household were less likely to receive all FANC services.
This study reveals that despite the use of ANC, women are not receiving all the services recommended for ANC. This underlines the challenge of access to services among women undergoing ANC (33%). Indicators found in our study are better than those reported in Mozambique and Ghana in 2019 and Ethiopia in 2021, where only 13%, 12.6% and 6.1% of women had received quality ANC, respectively.4,18,19 However, our results would differ from those found by Radovith et al. in India, where 9 out of 10 women would have benefited from all FANC services. Our results can be explained by different factors. Firstly, it could be because of the lack or shortage of inputs (reagents, strips) and drugs (FFA, SP and dewormer) and the lack of equipment (tensiometer, microscope) in the health facilities. Secondly, it could be linked to non-compliance with ANC service standards and procedures by health staff. Thirdly, cultural factors influencing women’s perception of these services could lead them to refuse certain services contained in the FANC. Fourthly, logistical factors could compromise the timely delivery of inputs and medicines for ANC, leading to their stockouts.
Under-use of the services contained in the ANC package could indeed expose women, even if they do undergo ANC, to the risk of illnesses such as anaemia (e.g., if they do not take FFA, SP tablets and deworming tablets), malaria and parasitosis. Qualitative studies would be needed to better explore the realities associated with the shortage of inputs and medicines, as well as the adherence of healthcare providers to the guidelines for the provision of ANC services; this would enable a better understanding of the influence of these realities on women’s use of FANC services.
Our results also show that less than half of the women who underwent at least one ANC visit received deworming medicines. This indicator is lower than the one reported in 2014 in Nepal.20 This low rate of deworming could be partly because of stock-out or low supply of deworming medicines in health facilities. It is therefore necessary to make deworming medicines available in health facilities.
In our study, almost one out of every two women attending ANC was from a poor household. Women from richer households were more likely to use all FANC services than women from poorer households. These results are comparable to those found in Ghana in 2018 where wealth had a positive association with the use of ANC services.21 The low uptake of FANC services by these poor women can be explained by certain staff attitudes, such as discrimination against poorer women and the high cost of certain examinations (blood and urine tests).22,23 This calls for the need not only to promote among health staffs the provision of respectful and equitable ANC services but also to ensure that ANC services are offered free of charge.
Limitations and strengths
The main limitation is that the data analysed being secondary, it was not possible to take into account in the analysis the other WHO-recommended FANC services, given these information pieces were not collected during the DHS. The services on which information was not collected were weight measurement, abdominal circumference and the receipt of various vaccines. In addition, possible reporting and recall bias could be a limitation to this study; also, the DHS cannot determine a cause-and-effect relationship because data are collected retrospectively. However, the national representativeness of DHS is a major strength as such study provides useful information to guide national and sub-national FANC programming and stimulate further study.
Conclusion
This study shows that, between 2016 and 2018, only one-third of women who had at least one ANC visit in Guinea had received all FANC services. Deworming was the least offered service. Factors associated with receiving all services were region, poverty, unwanted pregnancy and having three and four or more ANC visits.
In the Guinean context, there is a need to prevent health facilities from running out of ANC drugs, particularly for deworming, and to provide these facilities with essential equipment (tensiometer, microscope, laboratory reagents). It is also important to continuously disseminate ANC standards and procedures to health providers, so that they can provide comprehensive, high-quality ANC services.
Acknowledgements
The authors would like to thank the Demographic and Health Survey (DHS) Programme for making the database available to them.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors’ contributions
M.B., M.D.B., B.S.C. and K.S.K. contributed to the study design. J.B.D.L., B.S.C., R.D., T.S., F.B., S.C., M.B. and K.S.K. contributed to the data analysis. All authors contributed to the interpretation of the data, drafting and revision of the article. All authors agreed to this version of the article being published.
Data availability
Data from the Guinea Demographic and Health Survey (DHS) analysed during this study are available and accessible on the DHS Programme website (https://dhsprogram.com/Data/terms-of-use.cfm).
Disclaimer
The views and opinions expressed in this study are those of the authors and are the product of professional research. It does not necessarily reflect the official policy or position of any affiliated institution, funder, agency or that of the publisher. The authors are responsible for this study’s results, findings and content.
Funding Statement
Funding information This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
How to cite this article: Baldé M, Loua JBD, Sidibé T, et al. Frequency and factors associated with focused antenatal care in Guinea: Analysis of the DHS 2018. J Public Health Africa. 2024;15(1), 505. https://doi.org/10.4102/jphia.v15i1.505
References
- 1.World Health Organization . Mortalité maternelle [homepage on the Internet]. 2023. [cité 2024 Mar 08]. Available from: https://www.who.int/fr/news-room/fact-sheets/detail/maternal-mortality
- 2.Chorongo D, Okinda FM, Kariuki EJ, et al. Factors influencing the utilization of focused antenatal care services in Malindi and Magarini sub-counties of Kilifi county, Kenya. Pan Afr Med J. 2016;25(Suppl 2):14. 10.11604/pamj.supp.2016.25.2.10520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benova L, Tunçalp Ö, Moran AC, Campbell OMR. Not just a number: Examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Health. 2018;3(2):e000779. 10.1136/bmjgh-2018-000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reis-Muleva B, Vilela Borges AL, Simões Duarte L, Da Silva dos Santos CC, De Castro Nascimento N. Assessment of the quality of antenatal care in Mozambique. Midwifery. 2023;118:103598. 10.1016/j.midw.2023.103598 [DOI] [PubMed] [Google Scholar]
- 5.Mamba KC, Muula AS, Stones W. Facility-imposed barriers to early utilization of focused antenatal care services in Mangochi District, Malawi – A mixed methods assessment. BMC Pregnancy Childbirth. 2017;17(1):444. 10.1186/s12884-017-1631-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gamberini C, Angeli F, Ambrosino E. Exploring solutions to improve antenatal care in resource-limited settings: An expert consultation. BMC Pregnancy Childbirth. 2022;22(1):449. 10.1186/s12884-022-04778-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nwabueze CO, Okeke CC, Nwevo CO, Nwodo LA, Nwekpa WC, Nwaiwu PI. Assessing focused antenatal care awareness and utilization among pregnant women in Enugu State, Nigeria: A cross-sectional survey. Cureus. 2023;15(5):e38403. 10.7759/cureus.38403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hussen MA, Worku BT. Quality of antenatal care service and factors associated with client satisfaction at public health facilities of Bele Gasgar District. J Patient Exp. 2022;9:23743735221083163. 10.1177/23743735221083163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Konlan KD, Saah JA, Amoah RM, et al. Factors influencing the utilization of focused antenatal care services during pregnancy, a study among postnatal women in a tertiary healthcare facility, Ghana. Nurs Open. 2020;7(6):1822–1832. 10.1002/nop2.569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forbes F, Wynter K, Wade C, Zeleke BM, Fisher J. Male partner attendance at antenatal care and adherence to antenatal care guidelines: Secondary analysis of 2011 Ethiopian Demographic and Health Survey data. BMC Pregnancy Childbirth. 2018;18(1):145. 10.1186/s12884-018-1775-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Normes et Procédures en Santé de la Reproduction 2016 Guinée [homepage on the Internet]. Ministère de la santé. Direction Nationale de la Santé Familiale et de la Nutrition; 2016. [cité 2024 Mar 25]. Available from: https://scorecard.prb.org/wp-content/uploads/2018/05/Normes-et-Proce%CC%81dures-en-Sante%CC%81-de-la-Reproduction-2016.-Guine%CC%81e.pdf [Google Scholar]
- 12.Grovogui FM, Benova L, Manet H, et al. Determinants of facility-based childbirth among adolescents and young women in Guinea: A secondary analysis of the 2018 Demographic and Health Survey. PLOS Glob Public Health. 2022;2(11):e0000435. 10.1371/journal.pgph.0000435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cisse D, Toure AA, Diallo A, et al. Evaluation of maternal and child care continuum in Guinea: A secondary analysis of two demographic and health surveys using the composite coverage index (CCI). BMC Pregnancy Childbirth. 2023;23(1):391. 10.1186/s12884-023-05718-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Camara BS, Benova L, Delvaux T, et al. Women’s progression through the maternal continuum of care in Guinea: Evidence from the 2018 Guinean Demographic and Health Survey. Trop Med Int Health. 2021;26(11):1446–1461. 10.1111/tmi.13661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Recensement général de la population et de l’habitation 2014 [homepage on the Internet]. Guinée: Institut national des statistiques, 2014. [cité 2024 Mar 25]; p. 122. Available from: https://www.stat-guinee.org/images/Documents/Publications/INS/rapports_enquetes/RGPH3/INS_RGPH_2014_decret.pdf [Google Scholar]
- 16.Annuaire_Statistique_2020.pdf [homepage on the Internet]. [cité 2024 Mar 19]. Available from: https://www.stat-guinee.org/images/Documents/Publications/INS/annuelles/annuaire/Annuaire_Statistique_2020.pdf
- 17.Institut National de la Statistique/INS et ICF . Guinea Demographic and Health Survey (EDS V) 2016–18 [homepage on the Internet]. 2019. [cité 2024 Mar 19]. Available from: https://dhsprogram.com/publications/publication-fr353-dhs-final-reports.cfm
- 18.Okawa S, Gyapong M, Leslie H, et al. Effect of continuum-of-care intervention package on improving contacts and quality of maternal and newborn healthcare in Ghana: A cluster randomised controlled trial. BMJ Open. 2019;9(9):e025347. 10.1136/bmjopen-2018-025347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tessema AM, Gebeyehu A, Mekonnen S, Alemu K, Tigabu Z. Intervention fidelity and its determinants of focused antenatal care package implementation, in South Wollo zone, Northeast Ethiopia. BMC Pregnancy Childbirth. 2021;21(1):150. 10.1186/s12884-021-03637-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joshi C, Torvaldsen S, Hodgson R, Hayen A. Factors associated with the use and quality of antenatal care in Nepal: A population-based study using the Demographic and Health Survey data. BMC Pregnancy Childbirth. 2014;14(1):1–11. 10.1186/1471-2393-14-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duodu PA, Bayuo J, Mensah JA, et al. Trends in antenatal care visits and associated factors in Ghana from 2006 to 2018. BMC Pregnancy Childbirth. 2022;22(1):59. 10.1186/s12884-022-04404-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Midhet F, Hanif M, Khalid SN, Khan RS, Ahmad I, Khan SA. Factors associated with maternal health services utilization in Pakistan: Evidence from Pakistan maternal mortality survey, 2019. PLoS One. 2023;18(11):e0294225. 10.1371/journal.pone.0294225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bobo FT, Yesuf EA, Woldie M. Inequities in utilization of reproductive and maternal health services in Ethiopia. Int J Equity Health. 2017;16(1):105. 10.1186/s12939-017-0602-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from the Guinea Demographic and Health Survey (DHS) analysed during this study are available and accessible on the DHS Programme website (https://dhsprogram.com/Data/terms-of-use.cfm).