Abstract
Heart failure (HF) is a significant global health concern, particularly in Asia, where over half of the world's population resides. Despite advances in treatment, the burden of HF is expected to rise in the region due to the aging population and an increase in non-communicable diseases associated with HF risk. This narrative review examines the current state of HF in Asia, highlighting differences in treatment utilization, underrepresentation of Asian individuals in clinical trials, emerging therapies, and implementation strategies, including the potential use of polypills and the need for expanded HF training opportunities for healthcare providers.
Keywords: Asia, Heart failure, Clinical trials, Implementation science
INTRODUCTION
Heart failure (HF) is an end-stage manifestation of cardiovascular disease and an increasingly significant cause of mortality and morbidity worldwide. Over 60 million individuals are estimated to be living with HF globally.1) Particularly in Asia, where more than half of the world’s population resides, there is an urgent need to mitigate the growing burden of HF. In this region, marked by an aging demographic, advancements in heart disease treatment, and increases in non-communicable disease burden, the burden of HF is anticipated to escalate significantly in coming decades. With this challenge ahead, we provide a narrative review on the current state of HF and propose strategies to improve HF care in Asia.
HF IN ASIA
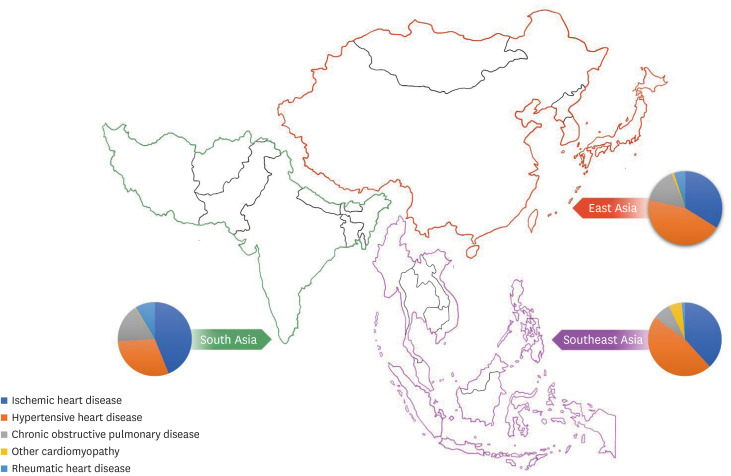
Most published epidemiological and treatment data related to HF report data only from Western countries. More recently, the establishment of regional registries has improved understanding of HF in Asia and provided a snapshot of the clinical characteristics of HF across Asia.2) In comparison to their counterparts in the United States, individuals living with HF in Asia tend to be younger by about a decade, exhibit a higher prevalence of rheumatic heart disease, comparable rates of diabetes and hypertension, and higher rates of smoking.3) The Asian Sudden Cardiac Death in HF (ASIAN-HF) registry, a prospective registry spanning 11 Asian countries with over 5,000 participants diagnosed with stage C HF, has provided important insights into the clinical presentation, management, and outcomes of HF, including HF with preserved ejection fraction (HFpEF).4,5,6) These data show that Asian HF phenotypes differ by regions and/or countries. For example, ischemic cardiomyopathy is the dominant form of HF in South and Southeast Asia when compared to East Asia, where non-ischemic disease and metabolic risks are more common (Figure 1).5,7,8) A similar trend is observed in the Korean data, demonstrating an increasing prevalence of HF patients (0.77% in 2022 to 2.58% in 2020), with the vast majority of hospitalization for acute HF attributed to non-ischemic cardiomyopathy.9,10) This nuanced understanding of “Asian” HF is needed when we discuss current and future treatment of HF in the region.11)
Figure 1. Leading etiologies of heart failure across Asian regions.
Data based on the Global Burden of Diseases study from Bragazzi et al.7) and Feng et al.8)
CURRENT HF THERAPY
The cornerstone of medical therapy for HF with reduced ejection fraction (HFrEF) involves a four-drug combination of an angiotensin-blocking drug (sacubitril-valsartan [ARNI], angiotensin converting enzyme inhibitor [ACE-i], or angiotensin receptor blocker [ARB], an evidence-based beta-blocker [BB], an aldosterone receptor antagonist [MRA], and a sodium-glucose transport protein 2 inhibitor [SGLT2i]).12) This aggressive four-drug strategy aims to mitigate disease progression in patients with HFrEF, through effects to reduce neurohormonal activation, hemodynamic derangement, electromechanical dissociation, and arrhythmia, which are common to all HFrEF patients, including Asians.
A notable deficiency in prior landmark trials is the underrepresentation of participants of Asian ancestry. Landmark trials such as CONSENSUS (enalapril), SOLVD (enalapril), COPERNICUS (carvedilol), MERIT-HF (metoprolol XL), and CIBIS-II (bisoprolol) either excluded Asians or included only a minimal number of patients of Asian ancestry from Western countries.13,14,15,16) In fact, many early trials did not report the racial breakdown of study participants, complicating assessment of real-world representativeness and reducing generalizability. Regulatory approval of HF treatments in Asia has relied heavily on data from Western populations. A systematic review of 656 cardiometabolic trials from 2011 to 2020 revealed disheartening statistics, with only 7.7% of all trial participants from Asian-Pacific countries despite the fact that the Asia-Pacific region bears the majority of the world’s cardiometabolic disease burden.17) Only 10.1% of authors in these studies represent collaborators from Asia-Pacific countries.17) Temporal analysis does, however, show increasing globalization of clinical trials and a growing recognition of the importance of diversity and inclusiveness, with a gradual increase in the participation of patients and investigators from Asia.
Contemporary trial data provide some reassurance. The prospective comparison of Angiotensin Receptor-neprilysin inhibitor with Angiotensin-converting–enzyme inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure trial (PARADIGM-HF) is one of the largest cardiovascular trials, enrolling over 8,400 patients across 47 countries on six continents, with approximately 18% of participants identifying as Asians.18) Asian participants in PARADIGM-HF exhibited different baseline characteristics when compared with participants from North America and Western Europe, being younger (65.1±11.4 vs. 57.8±11.9), with a lower burden of atrial fibrillation (40% vs. 17%), lower body-mass index (31±7 vs. 24±4), lower systolic blood pressure (118±15 vs. 117±15), and a higher resting heart rate (70±11 vs. 75±11). Despite these differences, the benefits of ARNI were not significantly modified by geographic variations (hazard ratio [HR], 0.67; 95% confidence interval [CI], 0.50–0.90 in North America; HR, 0.85; 95% CI, 0.69–1.04 in Asia; p=0.50).19)
Similar observations were made in other landmark HF trials, including the Dapagliozin and Prevention of Adverse Outcomes in Heart Failure (DAPA-HF), and Dapagliozin Evaluation to Improve the Lives of Patients with Preserved Ejection Fraction Heart Failure (DELIVER) trials, both of which included a larger number of Asian participants (n=2,390 [21.7%]). Once again, geographic heterogeneity in baseline characteristics, HF presentations, and concurrent HF treatment rates were evident.20) Dapagliflozin, when compared with placebo, demonstrated benefits on the primary composite outcome of worsening HF or death from cardiovascular causes in all geographic regions across all ejection fractions (HR, 0.85; 95% CI, 0.75–0.96 in Europe; HR, 0.75; 95% CI, 0.61–0.93 in North America; HR, 0.72; 95% CI, 0.58–0.89 in South America; HR, 0.74; 95% CI, 0.61–0.91 in Asia).20) As trials become more global, geographic analysis becomes essential to assess potential demographic, biological, or environmental factors that may attenuate or enhance the effects of pharmacologic interventions between populations.
Alongside SGLT2i such as dapagliflozin, other therapies for patients with HFpEF are emerging. Data on efficacy of spironolactone differ by region and require further exploration.21,22) Another therapeutic class, glucagon-like peptide 1 (GLP-1) agonists, has shown effectiveness in symptom improvement (Kansas City Cardiomyopathy Questionnaire Clinical Summary Score [KCCQ-CSS] 16.6 vs. 8.7), increased 6-minute walk (21.5 m vs. 1.2 m), and weight loss (−13.3% vs. −2.6%) in obesity-phenotype HFpEF patients—however, Asian participants were not recruited for this study.23) The potential of GLP-1 agonists as prevention therapy for cardiovascular disease is of intense interest, with one study demonstrating a 20% reduction in cardiovascular death, nonfatal myocardial infarction, or stroke for those with initial body-mass index >27.24) HF studies routinely show Asian populations with HF to be leaner than their Western counterparts. In fact, Asian patients with lean fat with a high weight-to-height ratio and low body mass index may have worse HF outcome.25) For this reason, the role of GLP-1 agonists in Asian clinical practice, considering factors such as access, knowledge about the medication, and prescription practices with potential variations in efficacy in the obesity phenotypes seen in Asian populations, remains to be addressed.26,27)
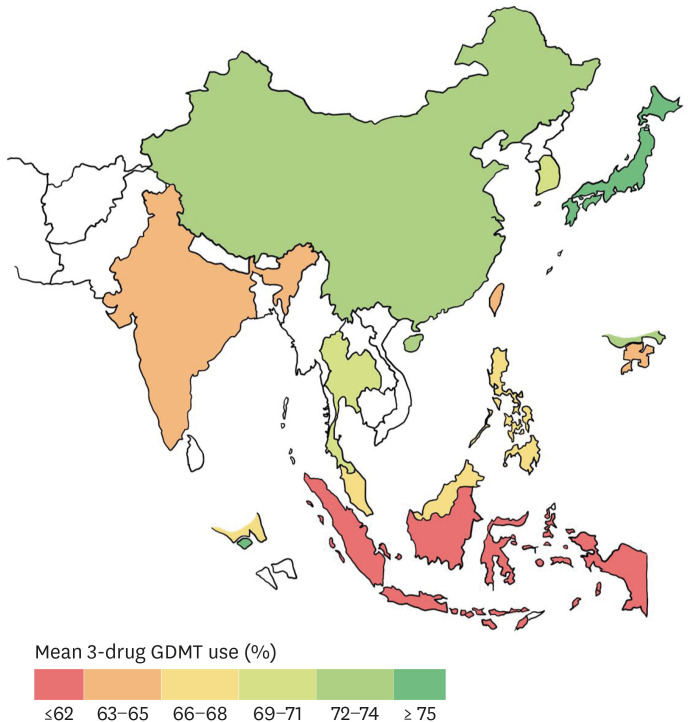
Despite the expanding toolbox available to physicians for HF management, data from Asia indicate suboptimal use of guideline-concordant therapy. In a 2018 study, prescription rates for ACE-i/ARB, BB, and MRA were 77%, 79%, 58%, respectively, with substantial country-to-country variability in Asia (Figure 2).28) Furthermore, less than one quarter of patients achieved recommended doses.28) The use of implantable cardioverter-defibrillator (ICD) devices for prevention of sudden cardiac death varies significantly across Asian countries, from 1.5% in Indonesia to 52.5% in Japan of eligible patients, as noted in ASIAN-HF.29) This is reinforced by a geographic analysis of PARADIGM-HF reporting that the Asia-Pacific region had the lowest ICD use (1.7%) despite the known mortality benefit for eligible patients with non-ischemic or ischemic cardiomyopathy.19,30,31) Potential factors for low ICD uptake, particularly in those with structural heart disease at risk for sudden cardiac death, may be lack of reimbursement, along with physician and patient beliefs about the role of ICD.30)
Figure 2. Mean 3-drug guideline directed medical therapy use by country.
Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, β-blocker and mineralocorticoid receptor antagonist uptake across Asian countries as reported in the ASIAN-HF registry.28)
GDMT = guideline-directed medical therapy; ASIAN-HF = Asian Sudden Cardiac Death in Heart Failure.
IMPROVING DATA IN “ASIAN” HF
Enhancing the quality and granularity of data on HF among Asian populations is paramount to developing targeted and effective strategies to prevent and manage this complex condition globally.32) To achieve this, there is a need to recognize the diversity within the Asian region, including different risk factor prevalence and regional HF risk profiles. Regional HF patient registries in Asia demonstrate that the dominant HF phenotype in South Asia differs significantly from the dominant HF phenotype in East Asia. Having an ongoing repository of diverse data will continue to improve data quality and will be instrumental in developing tailored interventions to specific subgroups (e.g. emphasis on coronary artery disease vs. hypertension treatment) within the population. Beyond clinical risk factors for HF, which include comorbidities and genetic predisposition, regional variance in non-clinical factors like socio-economic status, dietary and exercise norms, and access to and experience of healthcare systems may have a profound impact on prognosis in patients with HF. Only recently is recognition that subgroup analysis within Asian populations is imperative—highlighting that this demographic is not monolithic in nature.33)
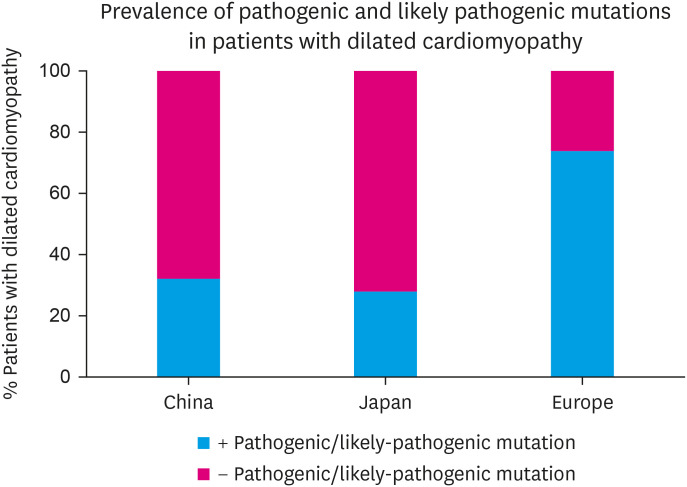
A clear example is current understanding of genetic mechanisms for cardiomyopathy in Asia. While race and ethnicity are a social construct, geographic differences in genetic variants do exist.34) Genotyping rates are low in Asian countries and most available genetic data are from Japan and China (Figure 3).34) Most pathologic and likely-pathologic variants described to date have been derived from white European populations and are found infrequently in patients of Asian ancestry with clear familial transmission of disease and seem to have different frequency characteristics.34,35,36) For example, variants in the lamin A/C gene are prevalent in Japan with familial dilated cardiomyopathy whereas variants in the titin gene are more prevalent in dilated cardiomyopathy patients who are White.34) And even when the disease appears familial, the rate of gene hits remains low in Asian populations.34,37) There are likely unique disease-causing variants to be identified in Asia.
Figure 3. Known genetic contributions to dilated cardiomyopathy in Asian (China and Japan) and European populations.
Lower prevalence of pathogenic and likely-pathogenic mutations seen in Asian cohorts with dilated cardiomyopathy relative to their European counterparts. Adapted from Tan et al.34 )
FOCUS ON IMPLEMENTATION STRATEGIES
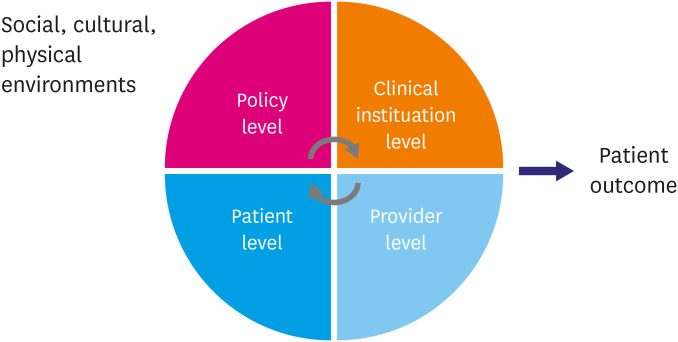
There are many effective therapies for patients living with HF—treatments that enhance symptoms, improve quality of life, and positively impact mortality. This is particularly relevant in Asia, where the burden of HF is expected to increase. Closing the knowledge-action gap in the utilization of evidenced-based therapies is important for maximizing the positive impact of well-established treatments on HF patients. The Safety, Tolerability and Efficacy of Up-Titration of Guideline-Directed Medical Therapies for Acute Heart Failure (STRONG-HF) and Empagliflozin in Patients Hospitalized for Acute Heart Failure (EMPULSE) studies remind us that it is not only four-drug therapy but how it is provided affects patient outcomes.38,39) Translating scientific evidence into routine clinical practice remains a challenge worldwide (Figure 4).40) Asia is no exception and addressing this gap necessitates a collaborative effort involving health systems, patients, and other stakeholders (Table 1).
Figure 4. Implementation framework for heart failure care.
Adapted from Chan et al.40)
Table 1. Potential challenges and strategies for improving heart failure care in Asia.
| Challenges | Potential strategies to address challenges |
|---|---|
| Limited heart failure data in Asia | • Improve granularity and quality of heart failure registry data with the ability to harmonize other regional heart failure registries. |
| • Recognize the diversity of Asian ancestry and its implication on heart failure presentation, management, and outcome. | |
| • Improve understanding of environmental, dietary, genetic factors on heart failure in Asia. | |
| • Investment of genomic research infrastructure including development of biobanks for various Asian communities. | |
| • Continue participation in global clinical trials for heart failure. Current trial participants are representative of clinical practice. | |
| Non-optimal guideline directed medication and device use | • Emphasis on implementation science research to contextualize and scale-up interventions to improve guideline directed care in each country. |
| • Address patient-related, treatment-related, healthcare-related factors unique to Asian countries that may lead to non-optimal use of medication and device use. | |
| • Heart failure polypill in development to address adherence and reduce pill burden. | |
| • Improve standards of heart failure care through a multidisciplinary team approach. | |
| Inadequate training opportunities for providers | • Expand training programs for healthcare providers, including non-cardiologists, in heart failure management. |
| • Re-vamp training pathways to attract talents to heart failure. | |
| Lack of awareness about heart failure among patients | • Launch public awareness campaigns to increase knowledge about heart failure symptoms and management options. |
| • Emphasis on Stage A heart failure and prevention | |
| • Address risk factors to heart failure including high blood pressure and lipids and diabetes etc. | |
| Limited research in heart failure implementation science | • Formal training in research and implementation science and support research capacity in Asia. |
One innovative treatment strategy is combining guideline directed medical therapies into a “polypill” to reduce pill burden and improve adherence to HF drug therapy (Table 2).41) This approach aims to reduce the pill burden on patients, thereby potentially improving adherence to the prescribed medications. The use of a polypill is particularly relevant in the context of Asia, as suggested by the ASIAN-HF registry, where up to 70% of eligible patients with HFrEF could benefit from this approach.6) The concept of a polypill becomes even more promising with the inclusion of atherosclerotic cardiovascular disease polypills in the World Health Organization Model List of Essential Medicines in 2023. This recognition highlights the potential importance and impact of such combination therapies in managing cardiovascular diseases globally.42,43) It is important to note that the success and feasibility of implementing such strategies may vary across different Asian countries due to significant differences in economic development and the architecture of each healthcare system. Factors such as HF-related health expenditures and the duration of HF-related hospitalization can differ widely around the globe.44) A HFrEF polypill is a promising concept but is not ready for clinical implementation at this time.
Table 2. Ongoing trials utilizing the heart failure polypill strategy.
| Trials | Trial details | |
|---|---|---|
| Polypill Strategy for the Evidence-Based Management of Heart Failure With Reduced Ejection Fraction in an Underserved Patient Population (NCT04633005, USA) | • Ongoing | |
| • Polypill vs. usual care | ||
| • Polypill: metoprolol succinate, empagliflozin, spironolactone | ||
| • Primary outcome: | ||
| ∘ Left ventricular ejection fraction (measured by cardiac MR) | ||
| • Secondary outcomes: | ||
| ∘ NTproBNP | ||
| ∘ Medication adherence | ||
| ∘ KCCQ questionnaire | ||
| ∘ Six-minute walk distance | ||
| ∘ HF hospitalization rate | ||
| ∘ Left ventricular ejection fraction (measured by echocardiography) | ||
| Developing a Heart Failure Polypill to Improve Outcomes at a Safety Net Hospital: A Pilot Crossover Randomized Controlled Trial (NCT06029712, USA) | • Ongoing | |
| • Polypill vs. usual care (2×2 crossover design) | ||
| • Patients with HFrEF +/− HIV | ||
| • Polypill: over-encapsulation of heart failure medications (beta blocker, SGLT2i, spironolactone, and ACE/ARB/ARNI) | ||
| • Primary outcome: | ||
| ∘ Pill count (adherence) | ||
| • Secondary outcomes: | ||
| ∘ Morisky medication adherence questionnaire | ||
| ∘ Self-reported adherence | ||
| ∘ Treatment satisfaction | ||
| ∘ Heart failure readmission rate | ||
| ∘ KCCQ questionnaire | ||
| ∘ Blood pressure, heart rate, weight, NTproBNP | ||
| ∘ Adverse events | ||
| ∘ Total daily pill burden | ||
| Polypill Strategy for Prevention of Cardiomyopathy Among Patients With Diabetes at Risk of Heart Failure (NCT06143566, USA) | • Ongoing. | |
| • Polypill vs. usual care | ||
| • Polypill: polycapsule containing finerenone, empagliflozin, and losartan | ||
| • Primary outcome: | ||
| ∘ Oxygen uptake during peak exercise | ||
| • Secondary and other outcomes | ||
| ∘ Urine albumin to creatinine ratio | ||
| ∘ Medication adherence | ||
Source: https://www.clinicaltrials.gov.
NTproBNP = N-terminal prohormone of brain natriuretic peptide; KCCQ = Kansas City Cardiomyopathy Questionnaire; HF = heart failure; HFrEF = heart failure with reduced ejection fraction; HIV = human immunodeficiency virus; SGLT2i = sodium-glucose transport protein 2 inhibitor; ACE = angiotensin converting enzyme; ARB = angiotensin receptor blocker; ARNI = sacubitril-valsartan.
On a patient and provider level, continued education and access to HF specific training will improve care and support burdened healthcare systems is needed.45) In the United States, acknowledging the increasing number of HF patients and the decline in interest in a career HF, there is a concerted effort to improve multidisciplinary HF care as well as re-vamping training pathways to attract talent.46,47,48) Formal training opportunities in HF in Asia are limited, leading to a mismatch between available training and the increasing HF burden. Expanding HF training opportunities to non-cardiologists may be needed to fill in the gaps in the HF workforce.
MAKING ASIA A LEADER IN HF CARE
There are many lessons to learn from the “Asian” HF experience. The absolute burden of HF is likely greater in Asia than in other world regions, and for this reason, evidence generation in the region is vital. The paucity of data among Asians living outside of Asia with HF underscores the importance of Asian data in informing care in the United States and other countries with large Asian immigrant populations. To generate such knowledge, a global lens in clinical science is necessary, with Asian countries participating as equals in clinical trials to bring novel therapies to Asian persons early, including rigorous study of the potential use of traditional Asian therapies.
Most recently, the use of Qiliqiangxin, a Chinese medication made up of 11 herbal ingredients, was shown to reduce hospitalization and mortality in HFrEF patients as an adjunctive HF medication, as presented at the European Society of Cardiology Congress in 2023.49) Although detailed results have not been published, the study does raise the question of whether there are additional traditional medications that might be repurposed for HF. Most recently, the use of another traditional medicine, Tonxingluo, and its potential benefits have been highlighted in JAMA for patients with acute myocardial infarction—although this study has been met with skepticism.50,51) Use of Yoga and Tai Chi as cardiac rehabilitation has also been explored.52,53) While these studies are exciting, reproducibility of these studies in diverse populations is needed to confirm efficacy and safety of such adjunctive therapies. When such studies are conducted in Asian countries, data transparency is essential to global acceptance, particularly when mechanisms are not well understood.
CONCLUSION
HF presents a substantial and growing challenge in Asia, requiring concerted efforts from patient-provider level to institutional-policy level interventions to combat the increasing HF burden. While promising therapies are emerging, there remains a need for improved HF data in the region, more inclusive clinical trials to promote knowledge exchange, and an emphasis on implementation strategies effective in diverse settings. Asia too can become an equitable leader in HF care, paving the way for improved outcomes and quality of life for patients across the region and patients around the globe.
Footnotes
Presentation: Parts of the review paper has been presented during Heart Failure Seoul 2023 Meeting.
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Yoo SGK, Sweitzer NK.
- Project administration: Yoo SGK.
- Visualization: Ahmed MO.
- Writing - original draft: Yoo SGK.
- Writing - review & editing: Yoo SGK, Ahmed MO, Sweitzer NK.
References
- 1.Zhao D. Epidemiological features of cardiovascular disease in Asia. JACC Asia. 2021;1:1–13. doi: 10.1016/j.jacasi.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mentz RJ, Roessig L, Greenberg BH, et al. Heart failure clinical trials in east and southeast Asia: understanding the importance and defining the next steps. JACC Heart Fail. 2016;4:419–427. doi: 10.1016/j.jchf.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Atherton JJ, Hayward CS, Wan Ahmad WA, et al. Patient characteristics from a regional multicenter database of acute decompensated heart failure in Asia Pacific (ADHERE International-Asia Pacific) J Card Fail. 2012;18:82–88. doi: 10.1016/j.cardfail.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Lam CSP, Anand I, Zhang S, et al. Asian sudden cardiac death in heart failure (ASIAN-HF) registry. Eur J Heart Fail. 2013;15:928–936. doi: 10.1093/eurjhf/hft045. [DOI] [PubMed] [Google Scholar]
- 5.Tromp J, Tay WT, Ouwerkerk W, et al. Multimorbidity in patients with heart failure from 11 Asian regions: a prospective cohort study using the ASIAN-HF registry. PLoS Med. 2018;15:e1002541. doi: 10.1371/journal.pmed.1002541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vijay A, Tay WT, Teng TK, et al. Polypill eligibility for patients with heart failure with reduced ejection fraction in the ASIAN-HF registry: a cross-sectional analysis. Glob Heart. 2023;18:33. doi: 10.5334/gh.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bragazzi NL, Zhong W, Shu J, et al. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. Eur J Prev Cardiol. 2021;28:1682–1690. doi: 10.1093/eurjpc/zwaa147. [DOI] [PubMed] [Google Scholar]
- 8.Feng J, Zhang Y, Zhang J. Epidemiology and burden of heart failure in Asia. JACC Asia. 2024;4:249–264. doi: 10.1016/j.jacasi.2024.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee CJ, Lee H, Yoon M, et al. Heart failure statistics 2024 update: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2024;6:56–69. doi: 10.36628/ijhf.2024.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure registry (KorAHF) Korean Circ J. 2017;47:341–353. doi: 10.4070/kcj.2016.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoo SGK, Lam CSP, Sweitzer NK. “Asian” heart failure. Circulation. 2024;150:177–179. doi: 10.1161/CIRCULATIONAHA.123.068576. [DOI] [PubMed] [Google Scholar]
- 12.Youn JC, Kim D, Cho JY, et al. Korean Society of Heart Failure guidelines for the management of heart failure: treatment. Korean Circ J. 2023;53:217–238. doi: 10.4070/kcj.2023.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Consensus Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. N Engl J Med. 1987;316:1429–1435. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 14.Packer M, Fowler MB, Roecker EB, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002;106:2194–2199. doi: 10.1161/01.cir.0000035653.72855.bf. [DOI] [PubMed] [Google Scholar]
- 15.Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in-congestive heart failure (MERIT-HF) Lancet. 1999;353:2001–2007. [PubMed] [Google Scholar]
- 16.The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomised trial. Lancet. 1999;353:9–13. [PubMed] [Google Scholar]
- 17.Azzopardi R, Nicholls SJ, Nerlekar N, et al. Asia-Pacific investigators and Asian enrollment in cardiometabolic trials: insights from publications between 2011 and 2020. JACC Asia. 2023;3:724–735. doi: 10.1016/j.jacasi.2023.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008. doi: 10.1056/NEJMoa1911303. [DOI] [PubMed] [Google Scholar]
- 19.Kristensen SL, Martinez F, Jhund PS, et al. Geographic variations in the PARADIGM-HF heart failure trial. Eur Heart J. 2016;37:3167–3174. doi: 10.1093/eurheartj/ehw226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kondo T, Wang X, Yang M, et al. Efficacy of dapagliflozin according to geographic location of patients with heart failure. J Am Coll Cardiol. 2023;82:1014–1026. doi: 10.1016/j.jacc.2023.05.056. [DOI] [PubMed] [Google Scholar]
- 21.Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–1392. doi: 10.1056/NEJMoa1313731. [DOI] [PubMed] [Google Scholar]
- 22.Pfeffer MA, Claggett B, Assmann SF, et al. Regional variation in patients and outcomes in the treatment of preserved cardiac function heart failure with an aldosterone antagonist (TOPCAT) trial. Circulation. 2015;131:34–42. doi: 10.1161/CIRCULATIONAHA.114.013255. [DOI] [PubMed] [Google Scholar]
- 23.Kosiborod MN, Abildstrøm SZ, Borlaug BA, et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023;389:1069–1084. doi: 10.1056/NEJMoa2306963. [DOI] [PubMed] [Google Scholar]
- 24.Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389:2221–2232. doi: 10.1056/NEJMoa2307563. [DOI] [PubMed] [Google Scholar]
- 25.Chandramouli C, Tay WT, Bamadhaj NS, et al. Association of obesity with heart failure outcomes in 11 Asian regions: a cohort study. PLoS Med. 2019;16:e1002916. doi: 10.1371/journal.pmed.1002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 27.Arnold SV, Tang F, Cooper A, et al. Global use of SGLT2 inhibitors and GLP-1 receptor agonists in type 2 diabetes. Results from DISCOVER. BMC Endocr Disord. 2022;22:111. doi: 10.1186/s12902-022-01026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teng TK, Tromp J, Tay WT, et al. Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: a cohort study. Lancet Glob Health. 2018;6:e1008–e1018. doi: 10.1016/S2214-109X(18)30306-1. [DOI] [PubMed] [Google Scholar]
- 29.Chia YMF, Teng TK, Tan ESJ, et al. Disparity between indications for and utilization of implantable cardioverter defibrillators in Asian patients with heart failure. Circ Cardiovasc Qual Outcomes. 2017;10:e003651. doi: 10.1161/CIRCOUTCOMES.116.003651. [DOI] [PubMed] [Google Scholar]
- 30.Ueda N, Noda T, Kusano K, Yasuda S, Kurita T, Shimizu W. Use of implantable cardioverter-defibrillators for primary prevention of sudden cardiac death in Asia. JACC Asia. 2023;3:335–345. doi: 10.1016/j.jacasi.2023.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Golwala H, Bajaj NS, Arora G, Arora P. Implantable cardioverter-defibrillator for nonischemic cardiomyopathy: an updated meta-analysis. Circulation. 2017;135:201–203. doi: 10.1161/CIRCULATIONAHA.116.026056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal A, Tromp J, Almahmeed W, et al. Toward a universal definition of etiologies in heart failure: categorizing causes and advancing registry science. Circ Heart Fail. 2024;17:e011095. doi: 10.1161/CIRCHEARTFAILURE.123.011095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kwan TW, Wong SS, Hong Y, et al. Epidemiology of diabetes and atherosclerotic cardiovascular disease among Asian American adults: implications, management, and future directions: a scientific statement from the American Heart Association. Circulation. 2023;148:74–94. doi: 10.1161/CIR.0000000000001145. [DOI] [PubMed] [Google Scholar]
- 34.Tan K, Foo R, Loh M. Cardiomyopathy in Asian cohorts: genetic and epigenetic insights. Circ Genom Precis Med. 2023;16:496–506. doi: 10.1161/CIRCGEN.123.004079. [DOI] [PubMed] [Google Scholar]
- 35.Haas J, Frese KS, Peil B, et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Hear J. 2015;36:1123–1135a. doi: 10.1093/eurheartj/ehu301. [DOI] [PubMed] [Google Scholar]
- 36.Moon I, Lee SY, Kim HK, et al. Trends of the prevalence and incidence of hypertrophic cardiomyopathy in Korea: a nationwide population-based cohort study. PLoS One. 2020;15:e0227012. doi: 10.1371/journal.pone.0227012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tomar S, Klinzing DC, Chen CK, et al. Causative variants for inherited cardiac conditions in a Southeast Asian population cohort. Circ Genom Precis Med. 2022;15:e003536. doi: 10.1161/CIRCGEN.121.003536. [DOI] [PubMed] [Google Scholar]
- 38.Mebazaa A, Davison B, Chioncel O, et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet. 2022;400:1938–1952. doi: 10.1016/S0140-6736(22)02076-1. [DOI] [PubMed] [Google Scholar]
- 39.Voors AA, Angermann CE, Teerlink JR, et al. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: a multinational randomized trial. Nat Med. 2022;28:568–574. doi: 10.1038/s41591-021-01659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan WV, Pearson TA, Bennett GC, et al. ACC/AHA special report: clinical practice guideline implementation strategies: a summary of systematic reviews by the NHLBI implementation science work group: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;69:1076–1092. doi: 10.1016/j.jacc.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 41.Pandey A, Keshvani N, Wang TJ. Should polypills be used for heart failure with reduced ejection fraction? Circulation. 2022;146:276–278. doi: 10.1161/CIRCULATIONAHA.122.059661. [DOI] [PubMed] [Google Scholar]
- 42.Castellano JM, Pocock SJ, Bhatt DL, et al. Polypill strategy in secondary cardiovascular prevention. N Engl J Med. 2022;387:967–977. doi: 10.1056/NEJMoa2208275. [DOI] [PubMed] [Google Scholar]
- 43.Huffman MD, Yusuf S. Polypills: essential medicines for cardiovascular disease secondary prevention? J Am Coll Cardiol. 2014;63:1368–1370. doi: 10.1016/j.jacc.2013.08.1665. [DOI] [PubMed] [Google Scholar]
- 44.Reyes EB, Ha JW, Firdaus I, et al. Heart failure across Asia: same healthcare burden but differences in organization of care. Int J Cardiol. 2016;223:163–167. doi: 10.1016/j.ijcard.2016.07.256. [DOI] [PubMed] [Google Scholar]
- 45.Raja Shariff RE, Hui Beng K, Mohd Ghazi A. The great Asian mismatch: training versus care in heart failure. J Card Fail. 2022;28:1378–1381. doi: 10.1016/j.cardfail.2022.05.007. [DOI] [PubMed] [Google Scholar]
- 46.Echols MR, Ogunniyi MO. Role and contribution of the general heart failure cardiologist: further expansion of the multidisciplinary heart failure approach. J Card Fail. 2022;28:659–663. doi: 10.1016/j.cardfail.2021.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Il’Giovine ZJ, Menon V. The intersection of heart failure and critical care: the contemporary cardiac intensive care unit and the opportunity for a unique training pathway. J Card Fail. 2021;27:1152–1155. doi: 10.1016/j.cardfail.2021.03.014. [DOI] [PubMed] [Google Scholar]
- 48.Blumer V, Kittleson MM, Teerlink JR, et al. A roadmap to reinvigorating training pathways focused on the care of patients with heart failure: shifting from failure to function. J Card Fail. 2023;29:527–530. doi: 10.1016/j.cardfail.2022.12.009. [DOI] [PubMed] [Google Scholar]
- 49.Yao W, Cheang I, Liao S, et al. Study protocol for a randomized controlled trial: Qiliqiangxin in heart failUre: assESsment of reduction in morTality (QUEST) BMC Complement Med Ther. 2020;20:38. doi: 10.1186/s12906-020-2821-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang Y, Li X, Chen G, et al. Traditional Chinese Medicine Compound (Tongxinluo) and clinical outcomes of patients with acute myocardial infarction: the CTS-AMI randomized clinical trial. JAMA. 2023;330:1534–1545. doi: 10.1001/jama.2023.19524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bach RG. Traditional Chinese medicine meets evidence-based medicine in the acutely infarcted heart. JAMA. 2023;330:1529–1530. doi: 10.1001/jama.2023.20838. [DOI] [PubMed] [Google Scholar]
- 52.Prabhakaran D, Chandrasekaran AM, Singh K, et al. Yoga-based cardiac rehabilitation after acute myocardial infarction: a randomized trial. J Am Coll Cardiol. 2020;75:1551–1561. doi: 10.1016/j.jacc.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yeh GY, McCarthy EP, Wayne PM, et al. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171:750–757. doi: 10.1001/archinternmed.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]