Abstract
Cardiovascular diseases are the leading cause of death among women, and the incidence among younger women has shown the greatest increase over the last decades, in particular for acute myocardial infarction (AMI). Moreover, the prognosis of women post-AMI is poor when compared with men of similar ages. Since the 1990s, an abundant literature has highlighted the existing differences between sexes with regard to presentation, burden, and impact of traditional risk factors and of risk factors pertaining predominantly to women, the perception of risk by women and men, and the pathophysiological causations, their treatment, and prognosis. These data that have been accumulated over recent years highlight several targets for improvement. The objective of this collaborative work is to define the actions required to reverse the growing incidence of AMI in women and improve the patient pathway and care, as well as the prognosis. We aim to provide practical toolkits for different health professionals involved in the care of women, so that each step, from cardiovascular risk assessment to symptom recognition, to the AMI pathway and rehabilitation, thus facilitating that from prevention to intervention of AMI, can be optimized.
Keywords: Acute coronary syndromes, Women, Sex differences, Cardiovascular risk factor, Prevention
Graphical abstract
Graphical Abstract.
Learning points.
Global awareness of women’s cardiovascular (CV) health needs to be improved to adjust women’s perception of cardiovascular disease (CVD) risk.
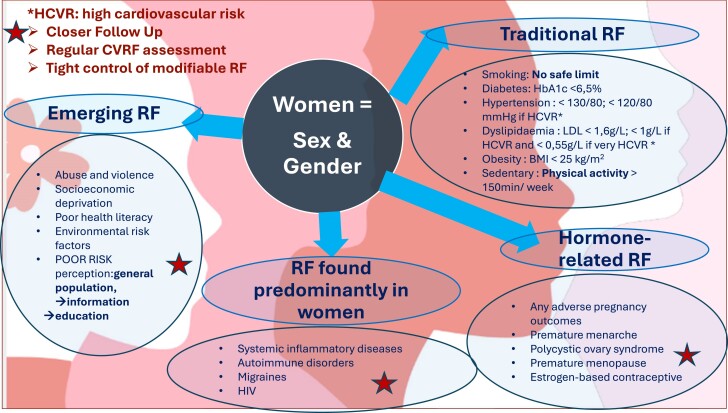
Women’s overall CV risk assessment should include their specific CV risk factors, and risk optimization strategies targeting modifiable risk factors should be emphasized.
Sex-specific risk factors and under-representation: women, especially from minority groups, face a higher burden of CV risk factors but are under-represented in clinical trials.
Diagnosis and treatment disparities: women often experience delays in treatment and less aggressive care and are less likely to receive guideline-directed therapies, leading to poorer outcomes.
Personalized care is crucial: addressing the unique risk profiles of women through adjusted pharmacotherapy, targeted prevention strategies, and improved cardiac rehabilitation is a key to improving outcomes.
Introduction
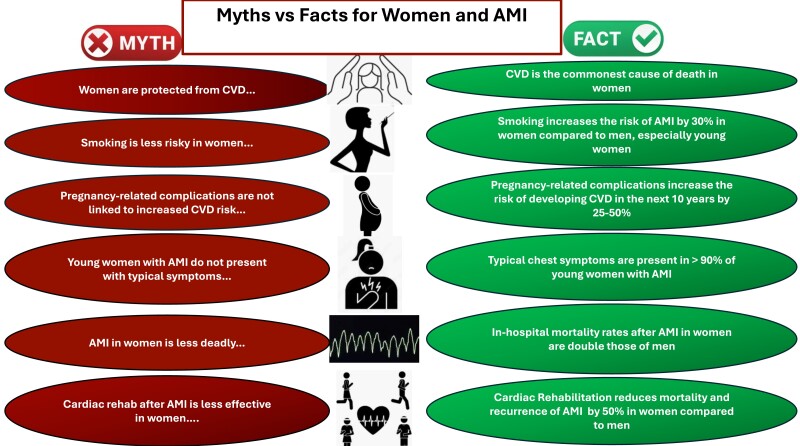
The leading cause of death in women is cardiovascular diseases (CVDs).1–5 Over the last decades, young women have experienced the highest rise in the incidence of acute myocardial infarction (AMI).1 Although perceived as having less risk, prognosis after AMI in women is worse than men of similar ages.6–9 Sex should be considered a significant biological variable as differences between the two sexes have been documented with regard to presentation,10,11 burden of cardiovascular risk factors (CVRFs),12,13 impact of traditional CVRF, and of CVRF pertaining predominantly to women.14,15 Difference in pathophysiology of AMI also should be acknowledged, in particular, the higher rates of myocardial infarction (MI) with non-obstructive coronary arteries (MINOCA), spontaneous coronary artery dissection (SCAD), embolic or spasm-related AMI.16–20 Likewise, differences in treatment delivered to women have also been reported to be associated with differences in outcome.7,21,22 Despite accumulation of scientific data, awareness and perception of cardiovascular (CV) risk has remained poor among women themselves, and the lowering of CVD burden has been limited in women, compared with men. This has resulted in a dedicated health campaign chaired by a Lancet Commission.23 Fields for improvement have been clearly identified, resulting in significant attention to sex-specific research, pathways, and treatment. In a CVD prevention strategy, an accurate risk assessment is essential in order to better understand 10 year fatal and non-fatal CVD risk in individuals without previous CVD. Recently, the updated prediction model SCORE2 included sex-specific CVRF modulators,24 but these conditions do not contribute to the final risk equation, so failing to provide a sex-specific assessment of risk in women and leading to an underestimation of the actual risk. Awareness of these specific risk enhancers is crucial in our goal of sex equality in the provision of CV health care.
This call to action aims to improve understanding of CVR in women and its management. The objective of this collaborative work is to define more precisely the practical modalities required to change the epidemiological indices of AMI in women and those actions needed to improve each step from prevention to intervention: from accurate risk prediction to symptom recognition, to evolved patient pathways and care that ultimately improve CVD prognosis in women and provide practical toolkits to different health professionals.
Epidemiology of sex discrepancy in myocardial infarction: focus on social and regional features
Cardiovascular disease stands as the primary cause of death globally, with deaths escalating from ∼12.1 million in 1990 to 18.6 million in 2019, according to the World Health Organization (WHO).25 However, the impact of CVD varies substantially across the globe, emphasizing the need for region-specific health interventions.26 Eastern Europe maintains the highest CVD mortality rates, between 215.0 and 553.0 per 100 000, despite a 24.3% reduction in CV mortality, while Western Europe observed the lowest rates, ranging from 80.2 to 199.9 per 100 000, achieving a notable 60.2% decline.27 Prevalence of CVRF is increasing worldwide, especially modifiable CVRF such as high blood pressure, elevated cholesterol, tobacco use, high body mass index (BMI), diabetes mellitus, and low levels of physical activity.
From 1990 to 2019, the incidence of CVD in Western and Southern Europe was persistently higher among men than women.28 Obesity rates (BMI ≥ 30 kg/m²) have surged across these countries, with the 2019 WHO data indicating that over 20% of adults in Western and Southern European were classified as obese: this figure is surpassed in Ireland, Malta, and in the UK, where the rate is 25%. This rise in obesity is linked to an increasing prevalence of metabolic syndrome and in particular, diabetes, with 2019 figures showing rates varying from under 5% in countries like Belgium, France, Ireland, and Greece to 10.4% in Germany for both men and women and rising up to 23.1% in Norway.28
Eastern Europe stands as the global epicentre for CVD mortality, with ischaemic heart disease (IHD) mortality rates in women surpassing those in men, across nearly all Eastern European countries. A stark comparison between France and Lithuania illustrates the gender disparity is an 11-fold higher rate in Lithuanian women and an eight-fold difference in men, compared with their French counterparts. Eastern European women, particularly in Slovakia and Ukraine, exhibit significantly higher IHD mortality rates compared with men, highlighting a critical gender-based health issue.29 Over 70% of the risk for acute IHD events is attributed to traditional CVRF, including smoking, which shows a prevalence of 23% in North Eastern Europe to 39% in Serbia for women. Additionally, suboptimal lipid profiles are more common in Eastern Europe, particularly among women. A recent meta-analysis reported that females even with familial hypercholesterolaemia are less likely to receive intensive treatment in order to reach guideline-recommended LDL-cholesterol targets.30
Although traditional CVRFs have been shown to be prevalent in young adults with AMI regardless of sex, there are also non-traditional CVRFs relevant in young population such as HIV, systemic lupus erythematosus, and obstructive sleep apnoea or the use of recreational substances.31
Differences in the rates of CVRF also occur within groups of women. Women from ethnic and racial minorities bear a disproportionately higher burden of CVRF.32 Young women presenting with AMI often have more comorbidities compared with similarly aged men, with a higher prevalence of diabetes, hypertension, and/or chronic kidney disease,33 and these CVRFs in addition to smoking have a greater impact for young women.10 The burden of CVRF and comorbidities is further increased when it comes to young women from minority populations.
Young women and men presenting with AMI exhibit distinct psychosocial profiles.11 Among young women, there is a higher prevalence of depression and stress, alongside poorer physical and mental health status, resulting in lower overall quality of life.34
A comprehensive review published in 2022 examined pregnancy and reproductive risk factors for CVD in women.35 These CVRF identified that early menarche (<11 years of age), premature menopause (<40 years of age), polycystic ovarian syndrome, hypothalamic amenorrhoea, hypertensive disorders of pregnancy, gestational diabetes, preterm delivery, low- or high-birth weight of the foetus, use of oral contraceptives, and use of hormone replacement therapy were associated with increased CVD risk.
Hospitalization rates for acute coronary syndrome (ACS) have significantly decreased over the past two decades for the general population.36 However, alarming trends emerge when focusing on young female patients. The US data show declining ACS hospitalizations among males aged 35–54, but not among females in the same age group. Conversely, ST-elevation MI (STEMI) rates increased annually by 3.6% from 2004 to 2014, in women, particularly in younger women (aged 45–54 years old) with smoking and obesity strongly linked to STEMI presentation.1 Similar observations were found in the analysis of 177 602 women with primary diagnosis with STEMI in the years 2008–19, showing the proportion of hospitalizations increased in women aged 18–34 (4.7–5.5%; P < 0001) and 35–44 years (21.2–22.7%; P < 0001)8
Comparable findings were reported in a comprehensive French nationwide study conducted between 2004 and 2014. It revealed a 6.3% rise in age-standardized admissions for ACS among women under 65 years old, resulting in nearly double the mortality rate compared with men in the <50 age group.1
Care pathway for myocardial infarction in women
Issue of delays
Despite reductions in CV mortality related to ACS, the diagnostic and therapeutic pathway for women remains hampered by delays. Low awareness of personal risk and misinterpretation of symptoms contribute to delayed presentation to specialized centres. Additionally, women are less likely than men to receive guideline-directed therapy.22,37
Issue of diagnosis of myocardial infarction, the ‘atypical presentation of MI’
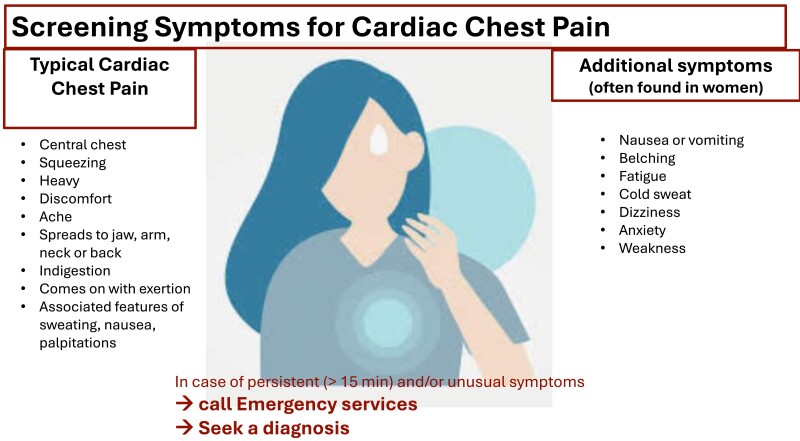
Fifty per cent of patients admitted to the emergency departments with suspected ACS, are women: women most likely present with non–ST-elevation MI (NSTEMI) and unstable angina.38 Women presenting ACS may have traditional and/or sex-specific risk factors (Figure 1) and more frequently than men have non-atherosclerotic involvement of coronary arteries. In female patients, the diagnosis of AMI is complicated by the presence of additional symptoms, such as epigastric discomfort, palpitations, fatigue, dizziness, and pain or discomfort in the jaw, neck, arms, or between the shoulder blades, alongside the more conventional chest pain described as pressure, tightness, or discomfort (Figure 2).39,40 Chest tightness symptoms are equally seen in women and men, but because of more additional symptoms and a higher number of symptoms reported being added to the misperception of the risk (Figure 3), the diagnosis of AMI becomes more challenging6,17,41 (Figure 4).
Figure 1.
Screening cardiovascular risk factors in women: which are the cardiovascular risk factor: the traditional, the specifics, and the emerging? Actionable points to reduce the risk.
Figure 2.
Empowering recognition of symptoms of acute myocardial infarction in women: the classical chest symptoms and the frequent associated symptoms. Importance of prompt medical seek.
Figure 3.
Acute myocardial infarction in women is shrouded in ignorance. Raising awareness and understanding of acute myocardial infarction are keys to improving care pathways and prognosis. The cornerstone of launching a global awareness campaign on women and acute myocardial infarction is to debunk the myths and spread the facts.
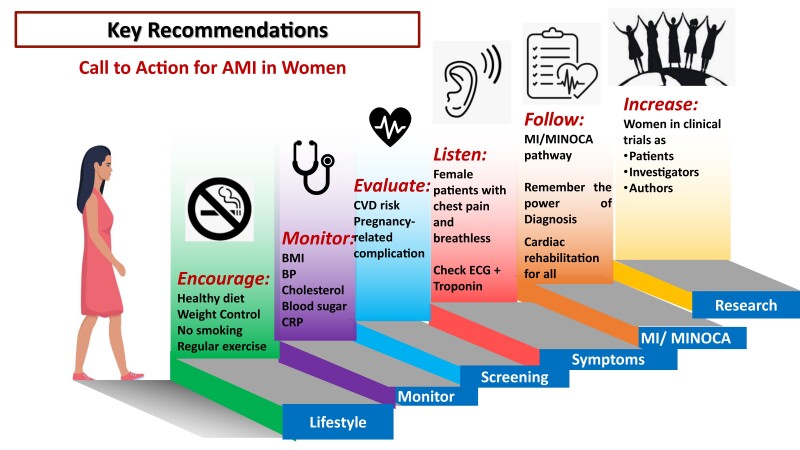
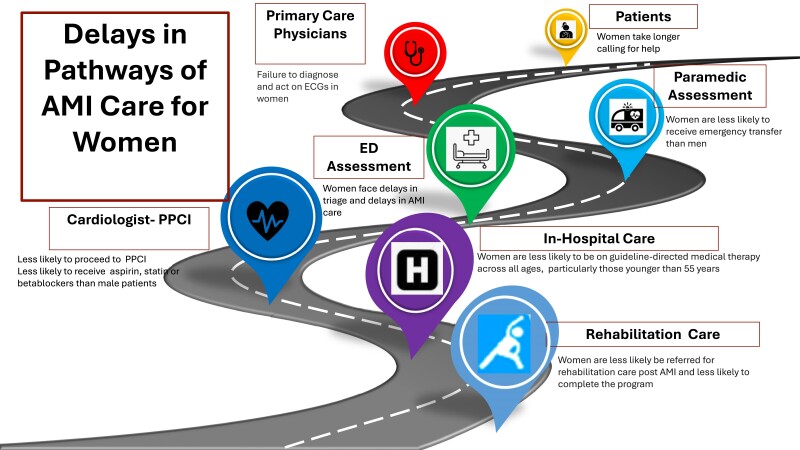
Figure 4.
Acute myocardial infarction pathway: improvement includes action points at each stage in order to avoid delays in access to acute myocardial infarction care: patient and system delays; improve diagnostic work-up in the case of myocardial infarction associated with non-obstructive coronary arteries to investigate the underlying mechanism and provide appropriate medical therapy; and increase participation in the cardiovascular rehabilitation programme.
Myocardial infarction with non-obstructive coronary arteries, more prevalent in women, particularly in non-Caucasian patients, is a heterogeneous entity with a different pathophysiology and risk profile compared with obstructive coronary artery disease. The underlying mechanisms range from functional alterations at the level of epicardial coronary arteries to microvascular dysfunction. The diagnosis of MINOCA requires a comprehensive multi-modality work-up42 including a detailed clinical assessment, evaluation of the left ventricular function, careful review of coronary angiography, timely cardiovascular magnetic resonance (CMR)43 and intra-coronary imaging, and provocative testing. Cardiovascular magnetic resonance is of major value in confirming the differential diagnosis of MINOCA, such as Takotsubo syndrome and myocarditis.
Issues of invasive treatment and underuse of imaging
In the ‘traditional presentation’ of ACS, with obstructive coronary artery disease, women are more often treated conservatively compared with men. The higher likelihood of being denied primary percutaneous coronary intervention (PCI) and evidence-based pharmacological treatment contribute to the sex-related mortality gap. This may reflect the older age at presentation of some female patients presenting with AMI. While early revascularization is beneficial for women with NSTEMI, they are still less likely to undergo revascularization than men, underscoring disparities in care.22,37 If MINOCA is a possible diagnosis42 intra-vascular imaging (IVI), aside from optimizing PCI, can uncover the underlying mechanisms of MINOCA, with one-third of cases linked to plaque rupture or erosion.20,42 Intra-vascular imaging is also helpful in diagnosing SCAD when angiography is inconclusive.20 Beside, in MINOCA cases, providing use of non-invasive imaging completes the diagnostic work-up, in particular CMR which not only investigate the underlying diagnosis but also afford tailored medical therapy and also could be safely use in young and/or pregnant patients.44 Association of IVL and CMR allows to identify the endotype of MINOCA in 85% of cases.19 However, underuse of IVI and limited inclusion of women in randomized controlled trials create a significant knowledge gap regarding sex differences in plaque morphology.45
Issue of pharmacological treatment
In women, evidence-based therapies has been systematically reported to be underprecribed5,8,9,46–48. Delay in diagnosis and treatment is associated with late administration of antithrombotic agents during ongoing cardiac ischaemia.49 Particularly in the context of MINOCA and given the lack of robust randomized controlled trials, women often face a higher risk of receiving inadequate or poorly tailored treatments. Treatment strategies should prioritize emergency stabilization, exclude alternative diagnoses, target underlying causes, and implement appropriate secondary prevention therapies. Statins and angiotensin converting enzyme inhibitors and angiotensin receptor blockers show promise in reducing event rates, but caution is warranted due to registry limitations.50 Furthermore, as statins are not recommended for women of childbearing age in the absence of effective contraception, this limitation may explain why they are prescribed less frequently in younger women and thus explain some of the poorer lipid control.30
Personalized pharmacotherapy, intensive CVRF control, and cardiac rehabilitation are crucial.
Prognosis
Worldwide data have consistently shown worse outcomes in women who suffer an ACS. In particular, women who do not present with chest pain have a higher risk of in-hospital death across all age groups: absence of chest pain is a stronger predictor of mortality in young women compared with men.51 Furthermore, women have a higher mortality during the initial 24 h of hospitalization following a STEMI.7,52 When evaluating specific CVRF, the long-term mortality in diabetic patients is twice as high as non-diabetic, with a more profound difference in women. Given the delayed presentation of women, lower frequency of revascularization in women, and fewer guideline-directed medical therapies (GDMTs) prescribed for women admitted with an ACS, it is no surprise that the overall mortality rates are higher.
The rates of stroke and vascular complications have been noted to be higher in women undergoing revascularization. However, these results have been inconsistent around the globe. It is critical to generate randomized accurate data in order to avoid further disparities in the delivery of timely care and revascularization for women presenting with an ACS.49
Beyond revascularization and GDMT, cardiac rehabilitation has demonstrated well-known benefits. The reduction in total mortality obtained by participation in cardiac rehabilitation programme has been reported to be more pronounced in women, compared with men (hazard ratio 0.54 vs. 0.81, respectively).53
However, these programmes remain under-utilized by women. When compared with men, more women who participate in such programmes are obese, with suboptimal cardiorespiratory fitness. Since sex-specific analyses noted similar physical and mental health improvements after rehabilitation, it is imperative that such programmes are prescribed more frequently for women.54
Patients’ view: the importance of education and comprehensive care for women
Educating the whole society, particularly young women, about the risk and symptoms of a heart attack and the associated risk factors is as crucial as imparting this knowledge to healthcare professionals. It is essential to engage cardiologists, gynaecologists, obstetricians, and general practitioners in this effort to promote awareness and prevention.
Enhancing women’s health awareness can significantly improve the care of women facing increased CV risk burden, particularly in scenarios such as adverse pregnancy outcomes, hormonal changes, and more. Such initiatives are expected to translate into improved health outcomes and prognoses for this population.
Actions to overcome disparities experienced by women
In view of the alarming increase in the number of MIs and the disparities observed among women, our committee advocates urgent, targeted action (Figure 5). Our priorities are to improve public awareness of CVD through patient and public engagement and to improve screening for traditional and specific CVD risk factors in order to better control the incidence and prognosis of CVD. The actions needed to improve the course of CVD in women should be inspired by the successful example of breast cancer awareness and screening campaigns, which have led to significant improvements in management and prognosis: public health should give priority to cardiovascular health information and screening. The public and healthcare providers should be made more aware of the importance of controlling modifiable risk factors for CVD through education campaigns. These campaigns should stress the importance of regular physical activity, a healthy diet, and regular check-ups to control blood pressure, blood sugar, and cholesterol levels. Targeted interventions should give priority to those populations most at risk. At the same time, a number of avenues for improvement have been identified in the field of research, and the first and foremost is the improvement of gender equity through better representation of women in clinical trials55 and specific analysis of data in research.
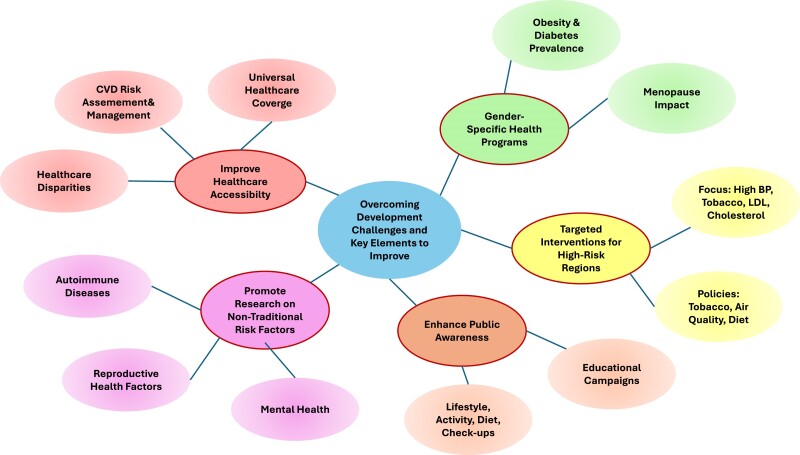
Figure 5.
The call to action proposes complementary actions at different levels to try to control epidemiological growth and improve women’s treatment, care, and prognosis, with the aim of reinforcing gender equity in cardiovascular health care.
Conclusions
Cardiovascular disease, particularly AMI, has seen a significant rise among younger women, with worse prognoses compared with men of similar age. Numerous studies highlight sex-specific differences in CVRF, presentation, and treatment outcomes. Despite some advances, disparities remain in diagnosis, treatment, and outcomes, underlining the need for a comprehensive, multi-disciplinary approach to women’s healthcare. Women are often under-represented in clinical trials and receive less aggressive treatment. Addressing these gaps requires sex-specific risk assessments, improved awareness, and tailored interventions across all levels of care. This document aims to guide healthcare professionals in improving the prevention, diagnosis, and treatment of CVD in women, fostering equality in cardiovascular health care.
Lead author biography

An interventional cardiologist. She is a consultant at the Institut de Cardiologie at la Pitié-Salpêtrière, Sorbonne University, Paris, France. Her areas of research are mechanical cardiac support in cardiogenic shock in fundamental research and coronary heart disease in women in clinical research. She led the French Metaregistre and the WAMIF study (JAHA 2024): the first study describing the characteristic of women under 50 with acute myocardial infarction. She is involved in overcoming gender discrimination in patient care as well as interventional careers. She participated or led some EAPCI Consensus Document. She is the Chair of the EAPCI Patient Advocacy Committee for the 2024 -26 term.
Contributor Information
Stephane Manzo-Silberman, Sorbonne University, Paris, France; Institute of Cardiology Hôpital Pitié-Salpêtrière (AP-HP), ACTION Study Group, Women as One, 75651 Paris CEDEX 13, France.
Michal Hawranek, Department of Cardiology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland.
Shrilla Banerjee, Department of Cardiology, Surrey and Sussex Healthcare NHS Trust, Redhill, Surrey.
Marta Kaluzna-Oleksy, 1st Department of Cardiology, Poznan University of Medical Sciences, Poznan, Poland.
Mirvat Alasnag, Cardiac Center, King Fahd Armed Forces Hospital, Jeddah, Saudi Arabia.
Valeria Paradies, Department of Cardiology, Maasstad Hospital, Rotterdam, the Netherlands.
Biljana Parapid, Division of Cardiology, University Clinical Center of Serbia; Faculty of Medicine, University of Belgrade, Belgrade, Serbia.
Pierre Sabouret, Institute of Cardiology Hôpital Pitié-Salpêtrière (AP-HP), ACTION Study Group, National College of French Cardiologists, Paris, France.
Agnieszka Wolczenko, Nationwide Association of Patients with Heart and Vascular Diseases EcoSerce, Milosc, Poland; Global Heart Hub, FH Europe Foundation.
Vijay Kunadian, Faculty of Medical Sciences, Cardiothoracic Centre, Freeman Hospital, Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK.
Izabella Uchmanowicz, Faculty of Nursing and Midwives, Department of Nursing, Wroclaw Medical University, Wrocław, Poland.
Jacky Nizard, Sorbonne University, Paris, France; Department of Gynecology and Obstetrics, APHP, Pitié-Salpêtrière Hospital, Paris, France.
Martine Gilard, INSERM UMR 1304 GETBO, Medical University of Brest, Brest, France.
Roxana Mehran, Icahn School of Medicine at Mount Sinai, New York, NY USA.
Alaide Chieffo, Interventional Cardiology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; University Vita-Salute San Raffaele, Milan, Italy.
Data availability
No new data were generated or analysed in support of this research.
Funding
Funding and support by TERUMO: support for meeting, publication, communication, and symposia.
References
- 1. Gabet A, Danchin N, Juilliere Y, Olie V. Acute coronary syndrome in women: rising hospitalizations in middle-aged French women, 2004–14. Eur Heart J 2017;38:1060–1065. [DOI] [PubMed] [Google Scholar]
- 2. Wilmot KA, O'Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation 2015;132:997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khan SU, Yedlapati SH, Lone AN, Khan MS, Wenger NK, Watson KE, Gulati M, Hays AG, Michos ED. A comparative analysis of premature heart disease- and cancer-related mortality in women in the USA, 1999–2018. Eur Heart J Qual Care Clin Outcomes 2022;8:315–323. [DOI] [PubMed] [Google Scholar]
- 4. GBD 2017 Causes of Death Collaborators . Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet 2018;392:1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arora S, Stouffer GA, Kucharska-Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, Caughey MC. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation 2019;139:1047–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, Daneshvar M, Spertus JA, D’Onofrio G. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO study (variation in recovery: role of gender on outcomes of young AMI patients). Circulation 2018;137:781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Manzo-Silberman S, Couturaud F, Charpentier S, Auffret V, El Khoury C, Le Breton H, Belle L, Marlière S, Zeller M, Cottin Y, Danchin N, Simon T, Schiele F, Gilard M. Influence of gender on delays and early mortality in ST-segment elevation myocardial infarction: insight from the first French Metaregistry, 2005–2012 patient-level pooled analysis. Int J Cardiol. 2018;262:1–8. [DOI] [PubMed] [Google Scholar]
- 8. Abe T, Olanipekun T, Adedinsewo D, Ogunmoroti O, Udongwo N, Effoe V, Rice B, Onuorah I, Ghali JK, Mehta PK, Michos ED. Trends and outcomes of ST-segment-elevation myocardial infarction among young women in the United States. J Am Heart Assoc 2023;12:e026811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Donataccio MP, Puymirat E, Parapid B, Steg PG, Eltchaninoff H, Weber S, Ferrari E, Vilarem D, Charpentier S, Manzo-Silberman S, Ferrières J, Danchin N, Simon T. In-hospital outcomes and long-term mortality according to sex and management strategy in acute myocardial infarction. Insights from the French ST-elevation and non-ST-elevation Myocardial Infarction (FAST-MI) 2005 registry. Int J Cardiol 2015;201:265–270. [DOI] [PubMed] [Google Scholar]
- 10. Palmer J, Lloyd A, Steele L, Fotheringham J, Teare D, Iqbal J, Grech ED. Differential risk of ST-segment elevation myocardial infarction in male and female smokers. J Am Coll Cardiol 2019;73:3259–3266. [DOI] [PubMed] [Google Scholar]
- 11. Manzo-Silberman S, Couturaud F, Bellemain-Appaix A, Vautrin E, Gompel A, Drouet L, Marliere S, Sollier CBD, Uhry S, Eltchaninoff H, Bergot T, Motreff P, Lahlou N, Cottin Y, Mounier-Vehier C, Gilard M, Montalescot G. Characteristics of young women presenting with acute myocardial infarction. The prospective, multicenter, observational young women presenting acute myocardial infarction in France study. J Am Heart Assoc 2024;13:e034456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lu Y, Li SX, Liu Y, Rodriguez F, Watson KE, Dreyer RP, Khera R, Murugiah K, D'Onofrio G, Spatz ES, Nasir K, Masoudi FA, Krumholz HM. Sex-specific risk factors associated with first acute myocardial infarction in young adults. JAMA Netw Open 2022;5:e229953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ 2018;363:k4247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fraser A, Nelson SM, Macdonald-Wallis C, Cherry L, Butler E, Sattar N, Lawlor DA. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon longitudinal study of parents and children. Circulation 2012;125:1367–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leifheit-Limson EC, D'Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM, Lichtman JH. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol 2015;66:1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bairey Merz CN. Women and ischemic heart disease paradox and pathophysiology. JACC Cardiovasc Imaging 2011;4:74–77. [DOI] [PubMed] [Google Scholar]
- 17. DeFilippis EM, Collins BL, Singh A, Biery DW, Fatima A, Qamar A, Berman AN, Gupta A, Cawley M, Wood MJ, Klein J, Hainer J, Gulati M, Taqueti VR, Di Carli MF, Nasir K, Bhatt DL, Blankstein R. Women who experience a myocardial infarction at a young age have worse outcomes compared with men: the Mass General Brigham YOUNG-MI registry. Eur Heart J 2020;41:4127–4137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Manzo-Silberman S. Percutaneous coronary intervention in women: is sex still an issue? Minerva Cardioangiol 2020;68:393–404. [DOI] [PubMed] [Google Scholar]
- 19. Reynolds HR, Maehara A, Kwong RY, Sedlak T, Saw J, Smilowitz NR, Mahmud E, Wei J, Marzo K, Matsumura M, Seno A, Hausvater A, Giesler C, Jhalani N, Toma C, Har B, Thomas D, Mehta LS, Trost J, Mehta PK, Ahmed B, Bainey KR, Xia Y, Shah B, Attubato M, Bangalore S, Razzouk L, Ali ZA, Merz NB, Park K, Hada E, Zhong H, Hochman JS. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of myocardial infarction with nonobstructive coronary arteries in women. Circulation 2021;143:624–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reynolds HR, Srichai MB, Iqbal SN, Slater JN, Mancini GB, Feit F, Pena-Sing I, Axel L, Attubato MJ, Yatskar L, Kalhorn RT, Wood DA, Lobach IV, Hochman JS. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation 2011;124:1414–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chandrasekhar J, Gill A, Mehran R. Acute myocardial infarction in young women: current perspectives. Int J Womens Health 2018;10:267–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sambola A, Halvorsen S, Adlam D, Hassager C, Price S, Rosano G, Schiele F, Holmvang L, de Riva M, Rakisheva A, Sulzgruber P, Swahn E. Management of cardiac emergencies in women: a clinical consensus statement of the Association for Acute CardioVascular Care (ACVC), the European Association of Percutaneous Cardiovascular Interventions (EAPCI), the Heart Failure Association (HFA), and the European Heart Rhythm Association (EHRA) of the ESC, and the ESC Working Group on Cardiovascular Pharmacotherapy. Eur Heart J Open 2024;4:oeae011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vogel B, Acevedo M, Appelman Y, Bairey Merz CN, Chieffo A, Figtree GA, Guerrero M, Kunadian V, Lam CSP, Maas AHEM, Mihailidou AS, Olszanecka A, Poole JE, Saldarriaga C, Saw J, Zühlke L, Mehran R. The Lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet 2021;397:2385–2438. [DOI] [PubMed] [Google Scholar]
- 24. SCORE2 Working Group and ESC Cardiovascular Risk Collaboration . SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J 2021;42:2439–2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. World Health Organization . Cardiovascular Diseases. 2021.
- 26. Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, Ainslie J, Banning AP, Budaj A, Buechel RR, Chiariello GA, Chieffo A, Christodorescu RM, Deaton C, Doenst T, Jones HW, Kunadian V, Mehilli J, Milojevic M, Piek JJ, Pugliese F, Rubboli A, Semb AG, Senior R, ten Berg JM, Van Belle E, Van Craenenbroeck EM, Vidal-Perez R, Winther S; ESC Scientific Document Group . 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J 2024;45:3415–3537. [DOI] [PubMed] [Google Scholar]
- 27. Mensah GA, Fuster V, Murray CJL, Roth GA; Global Burden of Cardiovascular Diseases and Risks Collaborators . Global burden of cardiovascular diseases and risks, 1990–2022. J Am Coll Cardiol 2023;82:2350–2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Timmis A, Kazakiewicz D, Torbica A, Townsend N, Huculeci R, Aboyans V, Vardas P. Cardiovascular disease care and outcomes in West and South European countries. Lancet Reg Health Eur 2023;33:100718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cenko E, Manfrini O, Fabin N, Dorobantu M, Kedev S, Milicic D, Vasiljevic Z, Bugiardini R. Clinical determinants of ischemic heart disease in Eastern Europe. Lancet Reg Health Eur 2023;33:100698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Iatan I, Akioyamen LE, Ruel I, Guerin A, Hales L, Coutinho T, Brunham LR, Genest J. Sex differences in treatment of familial hypercholesterolaemia: a meta-analysis. Eur Heart J 2024;45:3231–3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mahtta D, Ramsey D, Krittanawong C, Al Rifai M, Khurram N, Samad Z, Jneid H, Ballantyne C, Petersen LA, Virani SS. Recreational substance use among patients with premature atherosclerotic cardiovascular disease. Heart 2021;107:650–656. [DOI] [PubMed] [Google Scholar]
- 32. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 33. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bucholz EM, Strait KM, Dreyer RP, Lindau ST, D'Onofrio G, Geda M, Spatz ES, Beltrame JF, Lichtman JH, Lorenze NP, Bueno H, Krumholz HM. Editor’s choice-sex differences in young patients with acute myocardial infarction: a VIRGO study analysis. Eur Heart J Acute Cardiovasc Care 2017;6:610–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. O’Kelly AC, Michos ED, Shufelt CL, Vermunt JV, Minissian MB, Quesada O, Smith GN, Rich-Edwards JW, Garovic VD, El Khoudary SR, Honigberg MC. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res 2022;130:652–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chi GC, Kanter MH, Li BH, Qian L, Reading SR, Harrison TN, Jacobsen SJ, Scott RD, Cavendish JJ, Lawrence JM, Tartof SY, Reynolds K. Trends in acute myocardial infarction by race and ethnicity. J Am Heart Assoc 2020;9:e013542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Huded CP, Johnson M, Kravitz K, Menon V, Abdallah M, Gullett TC, Hantz S, Ellis SG, Podolsky SR, Meldon SW, Kralovic DM, Brosovich D, Smith E, Kapadia SR, Khot UN. 4-Step protocol for disparities in STEMI care and outcomes in women. J Am Coll Cardiol 2018;71:2122–2132. [DOI] [PubMed] [Google Scholar]
- 38. Smilowitz NR, Mahajan AM, Roe MT, Hellkamp AS, Chiswell K, Gulati M, Reynolds HR. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION registry-GWTG (acute coronary treatment and intervention outcomes network registry-get with the guidelines). Circ Cardiovasc Qual Outcomes 2017;10:e003443. [DOI] [PubMed] [Google Scholar]
- 39. Ferry AV, Anand A, Strachan FE, Mooney L, Stewart SD, Marshall L, Chapman AR, Lee KK, Jones S, Orme K, Shah ASV, Mills NL. Presenting symptoms in men and women diagnosed with myocardial infarction using sex-specific criteria. J Am Heart Assoc 2019;8:e012307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Writing Committee Members; Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, Blankstein R, Boyd J, Bullock-Palmer RP, Conejo T, Diercks DB, Gentile F, Greenwood JP, Hess EP, Hollenberg SM, Jaber WA, Jneid H, Joglar JA, Morrow DA, O’Connor RE, Ross MA, Shaw LJ. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol 2021;78:e187–e285. [DOI] [PubMed] [Google Scholar]
- 41. Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, Blankstein R, Boyd J, Bullock-Palmer RP, Conejo T, Diercks DB, Gentile F, Greenwood JP, Hess EP, Hollenberg SM, Jaber WA, Jneid H, Joglar JA, Morrow DA, O’Connor RE, Ross MA, Shaw LJ. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2021;144:e368–e454. [DOI] [PubMed] [Google Scholar]
- 42. Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, Claeys MJ, Dan G-A, Dweck MR, Galbraith M, Gilard M, Hinterbuchner L, Jankowska EA, Jüni P, Kimura T, Kunadian V, Leosdottir M, Lorusso R, Pedretti RFE, Rigopoulos AG, Rubini Gimenez M, Thiele H, Vranckx P, Wassmann S, Wenger NK, Ibanez B; ESC Scientific Document Group . 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J Acute Cardiovasc Care 2024;13:55–161. [DOI] [PubMed] [Google Scholar]
- 43. La S, Beltrame J, Tavella R. Sex-specific and ethnicity-specific differences in MINOCA. Nat Rev Cardiol 2024;21:192–202. [DOI] [PubMed] [Google Scholar]
- 44. Bairey Merz CN, Gulati M, Wei J. MINOCA: diagnostic work-up, risk stratification and tailored therapies. Vascul Pharmacol 2023;153:107243. [DOI] [PubMed] [Google Scholar]
- 45. Rashid M, Stevens C, Zaman S, Pinilla-Echeverri N, Velagapudi P, Chieffo A, Shoaib A, Ludman P, Mills NL, Nolan J, Kinnaird T, Mamas M. Sex differences in use of intracoronary imaging in patients undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 2022;15:1290–1292. [DOI] [PubMed] [Google Scholar]
- 46. Cenko E, Yoon J, Kedev S, Stankovic G, Vasiljevic Z, Krljanac G, Kalpak O, Ricci B, Milicic D, Manfrini O, van der Schaar M, Badimon L, Bugiardini R. Sex differences in outcomes after STEMI: effect modification by treatment strategy and age. JAMA Intern Med 2018;178:632–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. D'Onofrio G, Safdar B, Lichtman JH, Strait KM, Dreyer RP, Geda M, Spertus JA, Krumholz HM. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation 2015;131:1324–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pancholy SB, Shantha GP, Patel T, Cheskin LJ. Sex differences in short-term and long-term all-cause mortality among patients with ST-segment elevation myocardial infarction treated by primary percutaneous intervention: a meta-analysis. JAMA Intern Med 2014;174:1822–1830. [DOI] [PubMed] [Google Scholar]
- 49. Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, Lindley KJ, Vaccarino V, Wang TY, Watson KE, Wenger NK; American Heart Association Cardiovascular Disease in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, and Council on Quality of Care and Outcomes Research . Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation 2016;133:916–947. [DOI] [PubMed] [Google Scholar]
- 50. Lindahl B, Baron T, Erlinge D, Hadziosmanovic N, Nordenskjold A, Gard A, Jernberg T. Medical therapy for secondary prevention and long-term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation 2017;135:1481–1489. [DOI] [PubMed] [Google Scholar]
- 51. Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA 2000;283:3223–3229. [DOI] [PubMed] [Google Scholar]
- 52. Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, Simes RJ, White HD, Van de Werf F, Topol EJ, Hochman JS, Newby LK, Harrington RA, Califf RM, Becker RC, Douglas PS. Sex differences in mortality following acute coronary syndromes. JAMA 2009;302:874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ekblom O, Cider A, Hambraeus K, Back M, Leosdottir M, Lonn A, Börjesson M. Participation in exercise-based cardiac rehabilitation is related to reduced total mortality in both men and women: results from the SWEDEHEART registry. Eur J Prev Cardiol 2022;29:485–492. [DOI] [PubMed] [Google Scholar]
- 54. Way KL, Reed JL. Meeting the needs of women in cardiac rehabilitation. Circulation 2019;139:1247–1248. [DOI] [PubMed] [Google Scholar]
- 55. Khan SU, Khan MZ, Raghu Subramanian C, Riaz H, Khan MU, Lone AN, Khan MS, Benson E-M, Alkhouli M, Blaha MJ, Blumenthal RS, Gulati M, Michos ED. Participation of women and older participants in randomized clinical trials of lipid-lowering therapies: a systematic review. JAMA Netw Open 2020;3:e205202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.