Abstract
Objective:
Mental health problems and vocational disengagement are often linked for young people in a self-reinforcing cycle. Integrated Individual Placement and Support (IPS) services can help to not only overcome educational/vocational challenges but also improve mental wellbeing.
Methods:
In a matched cohort study, we compared improvement rates in mental health and wellbeing outcomes for young people aged 15 to 25 who had received at least two integrated IPS services with those who had received standard youth mental health services only. Data came from headspace, Australia’s National Youth Mental Health Foundation. The sample comprised 2128 participants: 544 received integrated IPS services; 1584 received standard mental health services.
Results:
Four out of five IPS clients (81%) achieved positive outcomes on at least one of three mental health measures, a significantly higher proportion than matched clients who received standard services (75%). Logistic regressions estimated a 22% to 36% higher likelihood of achieving significant improvement for IPS clients. Greater improvements were evident for quality of life and potentially psychosocial functioning, but not psychological distress.
Conclusions:
Integrating an IPS program within a clinical setting not only achieves positive vocational outcomes, but also supports improvements in quality of life, psychosocial functioning and psychological distress that are greater or equal to the outcomes achieved through standard clinical care.
Keywords: youth mental health, Individual Placement and Support, cohort study, mental health outcomes, wellbeing, quality of life
Introduction
The transition from adolescence to adulthood can be a challenging journey due to significant physical, cognitive, emotional, and social changes. 1 Vulnerability to mental ill-health peaks, with over one-third of young people experiencing their first mental disorder before the age of 14, rising to nearly one-half by age 18, and exceeding 60% by age 25. 2 This is also a critical period for vocational development, with young people making decisions regarding further education, career paths, and entry into the workforce. 3 Young people are much more likely to be affected by unemployment and underemployment than other age groups. In Organisation for Economic Co-operation and Development countries, an average of 10.7% of the youth labor force (15-24-years) is unemployed, compared to 4.1% of 25- to 75-year-olds. 4 In Australia, these figures are 9.6% and 2.7%, respectively. 4 Many young people face the double challenge of seeking gainful employment alongside emerging mental health problems.
Experiencing mental ill-health in youth has been linked with negative employment outcomes, including a reduced likelihood of participating in any employment or of being employed full-time, and an increased likelihood of being underemployed. 5 Conversely, not being able to obtain employment or engage in education can negatively impact a young person’s mental health. 6 An association has been suggested between unemployment and suicide, with a 10-year international study across 63 countries estimating that one in five suicides might be attributable to unemployment. 7
In addition to mental health problems, young people disengaged from education or employment are at increased risk of further negative outcomes, including social and economic exclusion, poor physical health, anti-social behavior, or becoming entrenched in a “low pay, no pay cycle,” impacting their ability to improve their life situation. 8 Participation in education and employment is a protective factor for positive mental health.9,10 Beyond financial security, paid work offers a structured daily routine, instills a sense of self-worth, facilitates regular social engagement, provides greater autonomy, and enhances social status, each contributing positively to mental health and well-being. 10 There are flow-on benefits to government from employment participation, which include increased taxation revenue and reduced outlays on social security, health, housing, and other social programs. 11
Individual Placement Support
The Individual Placement and Support (IPS) model focuses on employment support for people impacted by mental ill-health. IPS is an evidence-based vocational intervention that integrates vocational assistance with mental health treatment, providing client-driven employment preferences and ongoing support after gaining employment.12,13 It was established in the 1990’s to support adults with long-term mental ill-health and is now provided in at least 20 countries.14-20
Vocational outcomes of the IPS model have been extensively researched for adults with severe mental ill-health (ie, Modini et al, 10 Frederick and VanderWeele, 21 Brinchmann et al, 22 Metcalfe et al, 23 Suijkerbuijk et al, 24 de Winter et al, 25 Bond et al, 26 Kinoshita et al, 27 Marshall et al, 28 and Weld-Blundell et al 29 ). A meta-analysis from 25 Randomised Controlled Trials undertaken across a range of locations and populations concluded that IPS is significantly better than “treatment as usual,” achieving higher rates of competitive employment, decreased time to first competitive employment, longer job tenure, and higher income. 21 This study also found some evidence that IPS may improve quality of life, and possibly global functioning, but that more research with larger sample sizes was needed. 21
To date, limited studies have focused on the benefits of IPS for young adults with established mental illness, and even less evidence is available on the use and effectiveness of IPS for young people with earlier presentations. Nevertheless, the argument for providing vocational support to young people with developing mental health conditions within an early intervention framework is compelling, with the aim of ensuring that these vulnerable young people do not become vocationally derailed at this critical life-stage.
IPS at headspace
Recognizing the high prevalence and peak vulnerability of young people to mental health disorders, the Australian Government initiated the headspace National Youth Mental Health Foundation in 2006. headspace is now the largest national network of primary care mental health services for youth world-wide 30 with 160 center-based services across Australia. headspace centers are community-based, integrated service hubs providing highly accessible, youth-friendly services to address the mental health and wellbeing needs of young people aged 12 to 25 years. Four core streams of integrated support are offered to all young people dependent on their situation, including mental health, physical and sexual health, alcohol and other drugs, and work and study. The center model was designed to encourage young people to seek help early in the development of mental health problems. 31
Fifty headspace centers offer the internationally standardized IPS model as a vocational stream. The Australian Government initially funded 14 trial IPS headspace sites in 2016. An independent evaluation reported that 43% of participants were placed into employment or education and, of those receiving employment, 50% maintained that employment for six months. Outcomes of the trial were significantly better than alternative employment pathways, and it was deemed a success in this early intervention setting. 32 Subsequently, funding was expanded to 24 and then, the current 50 sites.
The implementation of IPS at headspace adheres to the eight core principles of the IPS model 33 and focuses on providing vocational services that are time unlimited, have zero exclusion and integrate the vocational support with mental health support. The IPS work and study specialists work with young people to explore their individual preferences, interests and strengths and find suitable and competitive employment and/or education opportunities. The support includes resume writing and interview preparation. They also provide follow-up support once employment or education has been obtained. In addition to working directly with young people, the IPS work and study specialists visit local employers to build relationships in the community.
The Current Study
The current study’s aim was to investigate the effectiveness of the headspace IPS program in achieving mental health outcomes in comparison to those achieved with mental health treatment alone, using a matched cohort where baseline mental health is controlled for. It extends the prior evaluation and existing literature by focusing on mental health (rather than vocational) outcomes, which have so far been considered “secondary outcomes,” and uses a much larger sample. Another contribution to the literature is that this study examines evidence for the IPS program for young people with mild to moderate presentations of mental health issues, a target group for whom existing evidence is sparse.
Method
Participants
Participants comprised headspace clients who had received at least two integrated IPS services in addition to standard services and matched headspace clients who had received standard services only, at any of the 50 headspace centers delivering IPS. All clients accessing headspace services are eligible for IPS services and can self-refer or be referred by intake or clinical staff at any point throughout their clinical episode of care. Data were extracted in July 2022 and included all clients with recently completed episodes of care (within the last year) who were 15 to 25 years old at commencement (the eligible age range for IPS services). IPS clients with less than two integrated IPS services were filtered out, yielding a pool of 556 IPS clients and 7547 non-IPS clients in the full sample. Next, we matched the two groups based on key demographic and service-related characteristics, as well as baseline mental health status, in order to obtain comparable cohorts. 34 Matching was exact for gender and allowed for a tolerance factor for age (±3 years), baseline mental health status (±5 in K10) and the number of mental health sessions received (±3 sessions). Baseline differences in work and study status or whether the young person was looking for work were not part of the matching process as these form an integral part of self-selection into the program. Each IPS client was matched with up to five non-IPS clients, prioritizing exact matches and drawing randomly from non-exact matches if there were more than five eligible matches. Twelve IPS clients could not be matched based on these parameters. The final matched sample comprised 2128 young people, 544 IPS clients and 1584 non-IPS clients (Note that it is possible for an IPS client to have fewer than five matches within the selected tolerances, which explains why the sample of non-IPS clients is less than five times as large as the IPS sample.).
Procedure
When young people present at a headspace center, they are provided with an electronic device on which they answer a series of questions. Different question sets are presented depending on the visit number, with the first visit in each episode of care asking demographic and other background information. Service providers also input information at every visit. These data comprise the headspace national Minimum Data Set.
Young people provide consent to use their data for the primary purpose of service provision and outcome monitoring, but also for research purposes. Parental consent is not routinely sought for those under 18 years, who are assessed as mature minors unless otherwise indicated. Young people can opt out of data collection if they choose, or at the discretion of their parents. Ethics approval comprised initial approval through the headspace Board Research subcommittee; consent processes were then reviewed and endorsed by an independent body, the Australasian Human Research Ethics Consultancy Services.
Measures
Mental health measures were:
Psychological distress, using the Kessler 10-item psychological distress scale [K10 35 ], which measures self-reported depression and anxiety-related symptoms over the past 4 weeks on a scale of 1 to 5. A total score is calculated (min: 10, max: 50) with higher scores indicating higher psychological distress.
Quality of life, using MyLifeTracker [MLT 36 ], a self-report measure of quality of life covering 5 areas of importance to young people which is reported on a sliding scale from 0 to 100. An average score is calculated, with higher scores indicating better quality of life.
Psychosocial functioning, using the Social and Occupational Functioning Scale [SOFAS 37 ], a practitioner rating of current client functioning on a scale from 1 to 100, with lower scores representing lower functioning and higher scores representing superior functioning in a wide range of activities.
Vocational outcomes for IPS clients were measured via the following question completed by the vocational worker at episode completion: What was the main outcome that the young person achieved during their IPS episode? For non-IPS clients, vocational outcomes were not the key focus of the intervention and were only collected through self-reported work and study status at first and last measurement.
The key service-related variable was number of mental health sessions, which counts how many individual service sessions received by the young person were mental health related.
Demographic characteristics included age, gender (female, male, gender diverse), LGBTIQA+ status, Aboriginal and Torres Strait Islander background, and whether the young person was engaged in study or work at first presentation.
Data Analysis
SPSS Statistics 28.0.1.1 was used for data analysis. Descriptive statistics for the IPS and non-IPS cohorts are presented, followed by percentage of significant improvement for each group, and odds ratios (OR) from standard logistic regressions controlling for potential confounding by the matching variables, as well as baseline mental health measures that were not part of the matching algorithm (We chose psychological distress [K10] as the representative baseline mental health measure in the matching algorithm, to avoid the curse of dimensionality from attempting to match on too many variables. Hence, baseline quality of life [MLT] and psychosocial functioning [SOFAS] were not matched on, and must be controlled for statistically to determine outcomes.). Since the data pool is large and we allow for tolerance in the matching process, the standard analysis is appropriate and more efficient than a matched analysis (such as conditional logistic regression). 38 Young people’s mental health outcomes were determined by comparing the first and last measurement for each of the three mental health measures. An improvement in a client’s score was significant if it was greater than at least half a standard deviation of the respective measure’s baseline for the entire headspace population in the sampling period (for psychological distress, the headspace baseline standard deviation was 8.4, for quality of life 18.8, and for psychosocial functioning 11.6). An improvement of at least half a standard deviation is considered a moderate effect size and a minimally important difference to measure changes in health-related quality of life. 39
We report on a summary measure of improving significantly on at least one of the three outcome measures as an overall indication of whether any success was achieved, as well as on each of the outcome measures individually. The three outcome measures characterize different dimensions of a young person’s mental health and wellbeing. By receiving IPS support or standard mental health treatment, a young person might improve on some, but not all dimensions.
Results
Descriptive Statistics
Summary statistics for the matching variables across IPS and non-IPS clients in the matched sample are reported in Panel A of Table 1. A statistical test of equality of gender distribution between the two client groups was not significant, = 0.519, P = .772; in both groups, approximately 62% were female, 35% were male, and 3% identified as gender diverse. Statistical tests of equality of means for age, psychological distress at presentation, and number of mental health services received showed that while some differences existed (as expected, given the tolerance factors), these were of small magnitude. On average, IPS clients were four months older than non-IPS clients, had received one additional mental health service in their episode of care, and had presented with an approximately equivalent level of psychological distress with a mean K10 score of 31 (very high distress). To account for the potential of confounding, we report odds ratios of logistic regressions controlling for the matching variables.
Table 1.
Descriptive Statistics.
| Sample | IPS | Non-IPS | Statistical test for equality | ||
|---|---|---|---|---|---|
| N | 544 | 1584 | |||
| Panel A. Matching Variables | |||||
| Measure | n | % | n | % | P-value ( -test) |
| Gender | |||||
| Female | 346 | 63.6 | 980 | 61.9 | .772 |
| Male | 182 | 33.5 | 555 | 35.0 | |
| Gender diverse | 16 | 2.9 | 49 | 3.1 | |
| Measure | Mean | SD | Mean | SD | P-value (t-test) |
| Age | 19.7 | 2.7 | 19.4 | 2.7 | .032 |
| Psychological distress (K10) (baseline) | 31.0 | 8.0 | 30.7 | 7.7 | .467 |
| Number of mental health services | 12.7 | 12.7 | 11.4 | 10.4 | .013 |
| Panel B. Other demographic and baseline variables | |||||
| Measure | n | % | n | % | P-value ( -test) |
| LGBTIQA+ status | |||||
| Is LGBTIQA+ | 153 | 31.0 | 426 | 29.4 | .515 |
| Aboriginal and Torres Strait Islander status | |||||
| Is Indigenous | 52 | 9.6 | 92 | 5.8 | .002 |
| Engaged in study or work | |||||
| Fully engaged (study or full-time work) | 278 | 51.2 | 1011 | 63.9 | |
| Partially engaged (part-time or casual work; no study) | 100 | 18.4 | 254 | 16.1 | |
| Not engaged | 165 | 30.4 | 318 | 20.1 | <0.001 |
| Looking for work | 342 | 63.9 | 607 | 38.6 | <0.001 |
| Measure | Mean | SD | Mean | SD | P-value (t-test) |
| Quality of life (MLT) (baseline) | 45.6 | 18.4 | 48.5 | 18.0 | .002 |
| Psychosocial functioning (SOFAS) (baseline) | 63.0 | 11.5 | 64.7 | 11.4 | .002 |
Panel B of Table 1 presents summary statistics for other demographic and baseline measures that were not used as part of the matching process. Both groups comprised approximately equal proportions of clients identifying as LGBTIQA+ (30%), but the IPS sample had more Indigenous young people (IPS: 10%; Non-IPS: 6%). In both cohorts, the majority of clients were engaged in some form of study or work (IPS: 70%; Non-IPS: 80%), but a substantially higher proportion of IPS clients indicated they were looking for work (IPS: 64%; Non-IPS: 39%), which may include looking for more or better work, or changing from study to work (The high percentage of engagement in study or work in both cohorts is driven by high engagement in study [IPS: 46%; Non-IPS: 54%] and casual work [IPS: 23%; Non-IPS: 30%]. Full-time [IPS: 6%; Non-IPS: 15%] and part-time work [IPS: 10%; Non-IPS: 12%] were less common. While high baseline engagement in an IPS sample may seem surprising, it can be explained by the fact that this is a relatively young age group where study is common, and where vocational outcomes sought through the IPS program may include changes to better-fitting jobs/study programs or an increase in work hours.). These differences in work and study status (and goals) between the cohorts are a natural consequence of selecting into the program. In terms of quality of life and psychosocial functioning, the IPS group had a slightly lower baseline measurement. To account for these baseline differences in mental health, we report odds ratios of logistic regressions controlling for baseline quality of life and psychosocial functioning (in addition to the matching variables).
At the conclusion of their IPS episode, the vocational outcome achieved for almost two thirds (65%) of IPS clients was that they had obtained a job (56%) or commenced study (9%). An additional almost 8% had other positive work or study outcomes recorded. Just over one quarter did not achieve a work and study outcome. For the non-IPS clients, 12% reported a positive change in their work and study status.
Mental Health Outcomes
Comparison of significant improvement rates for IPS and non-IPS clients revealed a mental health benefit of integrated IPS services larger than the outcomes achieved through standard clinical care (Table 2). About 81% of IPS clients experienced an improvement on at least one of the three mental health measures, a significantly higher proportion than the 75% of controls. This represents a 22% to 36% higher likelihood of achieving significant improvement on any mental health outcome from receiving integrated IPS services compared to standard mental health services (OR controlling for matching variables: 1.361, P = .014; OR controlling for matching variables + baseline MLT, SOFAS: 1.220, P = .124).
Table 2.
Percentage With Significant Improvement in Mental Health Outcomes, IPS Versus Non-IPS.
| Measure | Percentage improved |
Odds ratio (standard logistic regression) |
||
|---|---|---|---|---|
| % | n | Controlling for matching variables | Controlling for matching variables + baseline MLT, SOFAS | |
| At least one outcome measure | ||||
| IPS | 80.7 | 439 | 1.361* | 1.220 |
| Non-IPS | 75.3 | 1193 | ||
| Quality of life (MLT) | ||||
| IPS | 58.3 | 317 | 1.356** | 1.243* |
| Non-IPS | 50.3 | 797 | ||
| Psychosocial functioning (SOFAS) | ||||
| IPS | 53.9 | 293 | 1.360** | 1.238 |
| Non-IPS | 46.1 | 730 | ||
| Psychological distress (K10) | ||||
| IPS | 39.0 | 212 | 1.038 | 1.040 |
| Non-IPS | 37.4 | 593 | ||
Significant at P < .01; *Significant at P < .05.
The additional benefit of integrated IPS services is concentrated on quality-of-life outcomes where the IPS group achieved higher rates of significant improvement than the non-IPS group (58% vs 50%; P < .001), and psychosocial functioning outcomes (54% vs 46%; P < .001). Significant improvement in quality of life implies at least a 9.4-point increase on the MLT scale, and in psychosocial functioning at least a 5.8-point increase on the SOFAS scale. Psychological distress improved at the same rate for IPS clients as for non-IPS clients.
Table 1 showed that baseline psychological distress was equivalent in both groups, yet baseline quality of life and psychosocial functioning was lower in the IPS group than the non-IPS group. When controlling for baseline quality of life and baseline functioning as potential confounders in the analysis, the odds ratios reduced and remained statistically significant for quality of life (OR controlling for matching variables + baseline MLT, SOFAS: 1.243, P = .043) but (marginally) not for psychosocial functioning (OR controlling for matching variables + baseline MLT, SOFAS: 1.238, P = .054).
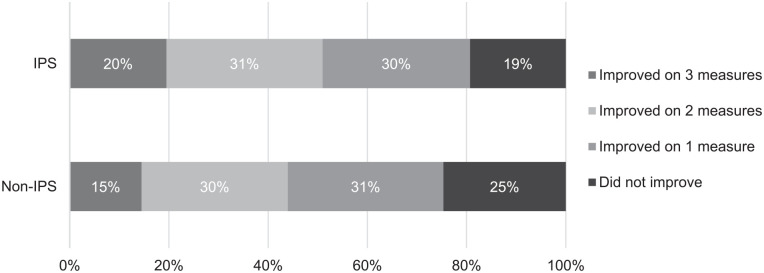
A fifth (20%) of IPS clients improved significantly on all three measures, 31% improved on two, and 30% on one; 19% did not improve on any measure. For the non-IPS clients, similar proportions improved significantly on one or two outcomes, but fewer improved on all three (15%) and more did not improve significantly on any measure (25%) (Figure 1).
Figure 1.
Percentage of clients achieving significant improvement by number of mental health outcome measures.
Table 3 presents the percentage of significant improvement and odds ratio for subgroups of young people, including those not engaged in study or work and looking for work at baseline, who are Indigenous, are male and female. The strongest improvements in at least one outcome measure were for IPS clients who were not engaged in study or work and were looking for work and male IPS clients, 85% and 86%, respectively.
Table 3.
Percentage of IPS Clients With Significant Improvement by Subgroups.
| Measure | IPS in subgroup: percentage improved |
IPS vs. non-IPS in subgroup: odds ratio (standard logistic regression) |
||
|---|---|---|---|---|
| % | n | Controlling for matching variables | Controlling for matching variables + baseline MLT, SOFAS | |
| At least one outcome measure | ||||
| Not engaged in work or study and looking for work | 85.4 | 111 | 2.035* | 2.029* |
| Indigenous | 78.9 | 41 | 1.642 | 1.468 |
| Male | 85.7 | 156 | 1.713* | 1.570 |
| Female | 78.9 | 273 | 1.302 | 1.142 |
| Quality of life (MLT) | ||||
| Not engaged in work or study and looking for work | 60.0 | 78 | 1.484 | 1.477 |
| Indigenous | 61.5 | 32 | 1.657 | 1.544 |
| Male | 63.7 | 116 | 1.584** | 1.556* |
| Female | 55.5 | 192 | 1.246 | 1.210 |
| Psychosocial functioning (SOFAS) | ||||
| Not engaged in work or study and looking for work | 56.9 | 74 | 1.759* | 1.936* |
| Indigenous | 44.2 | 23 | 1.217 | 0.770 |
| Male | 51.7 | 94 | 1.451* | 1.322 |
| Female | 59.3 | 205 | 1.357* | 1.107 |
| Psychological distress (K10) | ||||
| Not engaged in work or study and looking for work | 36.9 | 48 | 0.733 | 0.734 |
| Indigenous | 42.3 | 22 | 2.277* | 2.693* |
| Male | 41.8 | 76 | 0.979 | 0.971 |
| Female | 38.4 | 133 | 1.124 | 1.130 |
Significant at P < .01. *Significant at P < .05.
IPS clients not engaged in study or work and looking for work were approximately twice as likely to improve on one of the outcomes than their non-IPS counterparts (OR controlling for matching variables: 2.035, P = .023; OR controlling for matching variables + baseline MLT, SOFAS: 2.029, P = .029). The higher likelihood of significant improvement for IPS clients in this subgroup is particularly pronounced in psychosocial functioning (OR controlling for matching variables: 1.759, P = .017; OR controlling for matching variables + baseline MLT, SOFAS: 1.935, P = .015).
Male IPS clients were more likely to see significant improvement in quality of life than their non-IPS counterparts (OR controlling for matching variables: 1.584, P = .010; OR controlling for matching variables + baseline MLT, SOFAS: 1.556, P = .020). Three in five female IPS clients achieved significant improvement in psychosocial functioning, however, after controlling for baseline psychosocial functioning this did not result in a statistically significant higher likelihood than female clients in standard clinical care (OR controlling for matching variables: 1.357, P = .015; OR controlling for matching variables + baseline MLT, SOFAS: 1.107, P = .448).
A notable result is the relative benefit of receiving integrated IPS services for Aboriginal or Torres Strait Islander young people: while the sample is small and underpowered, the point estimates of odds ratios suggest that young Indigenous IPS clients have a 47% to 64% higher likelihood of improving significantly on at least one mental health outcome measure than their non-IPS counterparts. Unlike any other subpopulation or the IPS population as a whole, this appears to be driven by being more than twice as likely to improve on psychological distress, which is statistically significant when baseline mental health is controlled for (OR controlling for matching variables: 2.277, P = .044; OR controlling for matching variables + baseline MLT, SOFAS: 2.693, P = .020).
Discussion
This cohort study reports the first large scale findings on the effectiveness of an IPS program in achieving mental health outcomes in a large sample of young people with emerging mental health issues, comparing IPS clients with a matched cohort of young people receiving standard mental health treatment. This comparison revealed that four out of five IPS clients (81%) achieved positive mental health outcomes on at least one of the three mental health measures, a significantly higher proportion than among the matched clients who received standard services (75%). The benefit of integrated IPS services is demonstrated through greater improvements in quality of life (58% vs 50%), and psychosocial functioning (54% vs 46%), although the latter relationship is somewhat weakened after controlling for baseline differences. Psychological distress improved at the same rate for both IPS clients and non-IPS clients. The strongest improvements in mental health were achieved for young people who were not engaged in work or study at presentation but looking for work, and next for young males. Although the sample was small, Aboriginal and Torres Strait Islander young people were also more likely to achieve positive mental health outcomes, particularly in terms of a reduction in psychological distress.
Considering the natural, initial differences in work and study status (and goals) of the two cohorts, achieving positive vocational outcomes through the IPS program may be a key mechanism to the greater improvement in quality of life and psychosocial functioning. In this study, almost two thirds of the IPS clients attained a job (56%) or commenced study (9%) after the support they received through the IPS program (which are similar outcomes as previously reported 33 ). The specific aim of this study was to examine what mental health outcomes are achieved for young people accessing headspace integrated IPS services, and to compare them to the mental health achievements of a comparable cohort of young people with similar baseline mental health who received standard mental health services only, as a benchmark for what is possible. To what extent the positive mental health outcomes in the IPS cohort can be attributed to positive vocational outcomes achieved through the IPS program remains undetermined and may be the aim of future research. Regardless of the mechanism, the greater or equal mental health improvements found in this study provide further evidence of the effectiveness of the IPS model and widen its applicability to young people with emerging mental health issues accessing primary care early intervention services. This extends previous research that indicates suitability of the model for young people with severe mental ill-health and first episode psychosis,40,41 filling a key evidence gap about the IPS program. 21
Limitations
Our study has some limitations that are important to acknowledge. As with any localized program, to what extent the findings would replicate in a different context is indeterminable. headspace is unique world-wide in its scale and spread across the country, and is the main service provider of mental health services for young people in Australia. Another limitation is the mental health outcome measures used, which were restricted by those collected in the headspace national minimum data set. Further research is needed to explore the sustainability of the vocational outcomes in the headspace context as well as the longitudinal impacts on clients’ mental health and well-being.
Conclusion
headspace has successfully implemented a real-world application of the IPS model integrated within almost one-third (fifty services) of its national, primary care, early intervention youth mental health services. Findings suggest that integration of an IPS vocational program within a clinical setting not only achieves positive work and study outcomes, but also support improvements in quality of life, and potentially psychosocial functioning, that are larger than the outcomes achieved in a comparable cohort of young people receiving standard clinical care. Given the critical nature of vocational attainment in adolescence and early adulthood, and the particular vulnerability of young people with mental health issues to vocational disengagement, integrating IPS within youth mental health services seems warranted.
Acknowledgments
This research was supported by headspace National Youth Mental Health Foundation. headspace is funded by the Australian Government.
Footnotes
Data Availability Statement: The data used in this study are not publicly available due to privacy and confidentiality restrictions.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded as an internal Quality Assurance project by headspace National Youth Mental Health Foundation.
Ethical Approval and Informed Consent Statements: All data reported in this study is being collected and used with consent of the participants. The data collection process received ethics approval through the headspace Board Research subcommittee. An independent body, the Australasian Human Research Ethics Consultancy Services, also reviewed and endorsed the consent procedures.
ORCID iD: Nic Telford  https://orcid.org/0000-0001-8370-1934
https://orcid.org/0000-0001-8370-1934
References
- 1. Larsen B, Luna B. Adolescence as a neurobiological critical period for the development of higher-order cognition. Neurosci Biobehav Rev. 2018;94:179-195. doi: 10.1016/j.neubiorev.2018.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Solmi M, Radua J, Olivola M, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281-295. doi: 10.1038/s41380-021-01161-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patton CV. Basic Methods of Policy Analysis and Planning. 3rd ed. Sawicki DS, ed. Routledge; 2016. [Google Scholar]
- 4. OECD. Unemployment rate by age group (indicator). 2024. doi: 10.1787/997c8750-en [DOI] [Google Scholar]
- 5. Gibb SJ, Fergusson DM, Horwood LJ. Burden of psychiatric disorder in young adulthood and life outcomes at age 30. Br J Psychiatry. 2010;197(2):122-127. doi: 10.1192/bjp.bp.109.076570 [DOI] [PubMed] [Google Scholar]
- 6. Milner A, Law P, Reavley N. Young workers and mental health: a systematic review of the effect of employment and transition into employment on mental health. 2018. Accessed March 4, 2024. https://www.vichealth.vic.gov.au/sites/default/files/Young-Workers-Mental-Health-Systemic-Review.pdf (vichealth.vic.gov.au)
- 7. Nordt C, Warnke I, Seifritz E, et al. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000-11. Lancet Psychiatry. 2015;2(3):239-245. doi: 10.1016/s2215-0366(14)00118-7 [DOI] [PubMed] [Google Scholar]
- 8. Powell A, Muir K, Salignac F, et al. Young People’s Economic Engagement. Centre for Social Impact, UNSW; 2017. doi: 10.26190/5c4920284e94d [DOI] [Google Scholar]
- 9. Bond GR, Drake RE. Making the case for IPS supported employment. Adm Policy Ment Health. 2014;41(1):69-73. doi: 10.1007/s10488-012-0444-6 [DOI] [PubMed] [Google Scholar]
- 10. Modini M, Joyce S, Mykletun A, et al. The mental health benefits of employment: results of a systematic meta-review. Australas Psychiatry. 2016;24(4):331-336. doi: 10.1177/1039856215618523 [DOI] [PubMed] [Google Scholar]
- 11. Gray M, Hunter BH, Biddle N. The Economic and Social Benefits of Increasing Indigenous Employment. Centre for Aboriginal Economic Policy Research; 2014. [Google Scholar]
- 12. Drake R, Bond G, Becker D. Individual Placement and Support: An Evidence Based Approach to Supported Employment. Oxford University Press; 2012. [Google Scholar]
- 13. Drake RE, Becker DR, Bond GR. Introducing Individual Placement and Support (IPS) supported employment in Japan. Psychiatry Clin Neurosci. 2019;73(2):47-49. doi: 10.1111/pcn.12792 [DOI] [PubMed] [Google Scholar]
- 14. Bond GR, Becker DR, Drake RE, et al. Implementing supported employment as an evidence-based practice. Psychiatr Serv. 2001;52(3):313-322. doi: 10.1176/appi.ps.52.3.313 [DOI] [PubMed] [Google Scholar]
- 15. Burns T, Catty J, Becker T, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370(9593):1146-1152. doi: 10.1016/s0140-6736(07)61516-5 [DOI] [PubMed] [Google Scholar]
- 16. Latimer EA, Lecomte T, Becker DR, et al. Generalisability of the individual placement and support model of supported employment: results of a Canadian randomised controlled trial. Br J Psychiatry. 2006;189:65-73. doi: 10.1192/bjp.bp.105.012641 [DOI] [PubMed] [Google Scholar]
- 17. Tsang HWH, Chan A, Wong A, et al. Vocational outcomes of an integrated supported employment program for individuals with persistent and severe mental illness. J Behav Ther Exp Psychiatry. 2009;40(2):292-305. doi: 10.1016/j.jbtep.2008.12.007 [DOI] [PubMed] [Google Scholar]
- 18. Killackey E, Jackson HJ, McGorry PD. Vocational intervention in first-episode psychosis: individual placement and support v. treatment as usual. Br J Psychiatry. 2008;193(2):114-120. doi: 10.1192/bjp.bp.107.043109 [DOI] [PubMed] [Google Scholar]
- 19. Waghorn G, Collister L, Killackey E, et al. Challenges to implementing evidence-based supported employment in Australia. J Vocat Rehabil. 2007;27(1):29-37. [Google Scholar]
- 20. Porteous N, Waghorn G. Developing evidence-based supported employment services for young adults receiving public mental health services. N Z J Occup Ther. 2009;56:34-39. [Google Scholar]
- 21. Frederick DE, VanderWeele TJ. Supported employment: meta-analysis and review of randomized controlled trials of individual placement and support. PLoS One. 2019;14(2):e0212208. doi: 10.1371/journal.pone.0212208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brinchmann B, Widding-Havneraas T, Modini M, et al. A meta-regression of the impact of policy on the efficacy of individual placement and support. Acta Psychiatr Scand. 2020;141(3):206-220. doi: 10.1111/acps.13129 [DOI] [PubMed] [Google Scholar]
- 23. Metcalfe JD, Drake RE, Bond GR. Economic, labor, and regulatory moderators of the effect of Individual Placement and Support among people with severe mental illness: a systematic review and meta-analysis. Schizophr Bull. 2018;44(1):22-31. doi: 10.1093/schbul/sbx132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Suijkerbuijk YB, Schaafsma FG, van Mechelen JC, et al. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta-analysis. Cochrane Database Syst Rev. 2017;9(9):Cd011867. doi: 10.1002/14651858.CD011867.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. de Winter L, Couwenbergh C, van Weeghel J, et al. Who benefits from individual placement and support? A meta-analysis. Epidemiol Psychiatr Sci. 2022;31:e50. doi: 10.1017/s2045796022000300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bond GR, Drake RE, Becker DR. Generalizability of the Individual Placement and Support (IPS) model of supported employment outside the US. World Psychiatry. 2012;11(1):32-39. doi: 10.1016/j.wpsyc.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kinoshita Y, Furukawa TA, Kinoshita K, et al. Supported employment for adults with severe mental illness. Cochrane Database Syst Rev. 2013;2013(9):CD008297. doi: 10.1002/14651858.CD008297.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Marshall T, Goldberg RW, Braude L, et al. Supported employment: assessing the evidence. Psychiatr Serv. 2014;65(1):16-23. doi: 10.1176/appi.ps.20130026S [DOI] [PubMed] [Google Scholar]
- 29. Weld-Blundell I, Shields M, Devine A, et al. Vocational interventions to improve employment participation of people with psychosocial disability, autism and/or intellectual disability: a systematic review. Int J Environ Res Public Health. 2021;18(22):12083. doi: 10.3390/ijerph182212083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rickwood D, Paraskakis M, Quin D, et al. Australia’s innovation in youth mental health care: the headspace centre model. Early Interv Psychiatry. 2019;13(1):159-166. doi: 10.1111/eip.12740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rickwood D, McEachran J, Saw A, et al. Sixteen years of innovation in youth mental healthcare: outcomes for young people attending Australia’s headspace centre service. PLoS One. 2023;18(6):e0282040. doi: 10.1371/journal.pone.0282040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. KPMG Final Report for the Evaluation of the Individual Placement and Support Trial. KPMG. 2019. Accessed March 7, 2024. https://www.dss.gov.au/sites/default/files/documents/08_2019/individual-placement-and-support-trial-evaluation-report-june-2019.pdf (dss.gov.au)
- 33. Simmons MB, Chinnery G, Whitson S, et al. Implementing a combined individual placement and support and vocational peer work program in integrated youth mental health settings. Early Interv Psychiatry. 2023;17(4):412-421. doi: 10.1111/eip.13387 [DOI] [PubMed] [Google Scholar]
- 34. Iwagami M, Shinozaki T. Introduction to matching in case-control and cohort studies. Ann Clin Epidemiol. 2022;4(2):33-40. doi: 10.37737/ace.22005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959-976. doi: 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- 36. Kwan B, Rickwood DJ, Telford NR. Development and validation of MyLifeTracker: a routine outcome measure for youth mental health. Psychol Res Behav Manag. 2018;11:67-77. doi: 10.2147/PRBM.S152342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149:1148-1156. doi: 10.1176/ajp.149.9.1148 [DOI] [PubMed] [Google Scholar]
- 38. Pearce N. Analysis of matched case-control studies. BMJ. 2016;352:i969. doi: 10.1136/bmj.i969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582-592. doi: 10.1097/01 [DOI] [PubMed] [Google Scholar]
- 40. Bond GR, Drake RE, Campbell K. Effectiveness of individual placement and support supported employment for young adults. Early Interv Psychiatry. 2016;10(4):300-307. doi: 10.1111/eip.12175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Killackey E, Allott K, Jackson H, et al. Individual placement and support for vocational recovery in first-episode psychosis. Randomised controlled trial. Br J Psychiatry. 2019;214(2):76-82. doi: 10.1192/bpj/2018.191 [DOI] [PubMed] [Google Scholar]