Abstract
Testicular tuberculosis is a rare form of genital tuberculosis. Ultrasound is a crucial tool for evaluating male genital disorders. Contrast-enhanced ultrasonography (CEUS), which provides real-time monitoring of microvascular hemodynamics, provides rich information about microcirculation, helping distinguish testicular tuberculosis from other testicular conditions such as tumors and inflammation. This study reports on a rare case of testicular tuberculosis diagnosed through CEUS. A 31-year-old male patient presented with two months of persistent right scrotal pain and swelling. Conventional scrotal ultrasound showed an enlarged right testicle with heterogeneous echogenicity and abundant color Doppler blood flow signals. CEUS demonstrated rapid contrast agent filling in the right testicle, followed by the appearance of several irregular regions, indicating perfusion deficits in these areas. Histopathological confirmation through ultrasound-guided biopsy revealed granulomatous inflammation with caseous necrosis, which is consistent with the diagnosis of testicular tuberculosis. As a real-time monitoring technique for microvascular hemodynamics, CEUS provides valuable microcirculatory information that enhances diagnostic accuracy and enables the formulation of appropriate treatment plans for testicular tuberculosis versus other testicular pathologies.
Keywords: Testicular tuberculosis, Ultrasound, Contrast-enhanced ultrasound (CEUS), Granulomatous inflammation, Caseous necrosis
Testicular tuberculosis, a rare manifestation of genitourinary tuberculosis, is less prevalent in clinical practice compared to renal and prostatic tuberculosis [1]. However, due to the outstanding advantages of ultrasound in the assessment of superficial organs, particularly in the diagnosis of male genital diseases, it has become a pivotal tool for initial screening and evaluation of testicular disorders. Ultrasound is non-invasive, real-time, and repeatable, offering detailed images of testicular anatomy and is valuable for identifying and localizing testicular masses, inflammation, and injuries [2].
CEUS by monitoring microvascular hemodynamics in real time and providing rich information about microcirculation, aids in differentiating testicular tuberculosis from other testicular conditions such as tumors and inflammations, thereby furnishing clinicians with more accurate diagnostic evidence to facilitate rational treatment planning [3], [4].
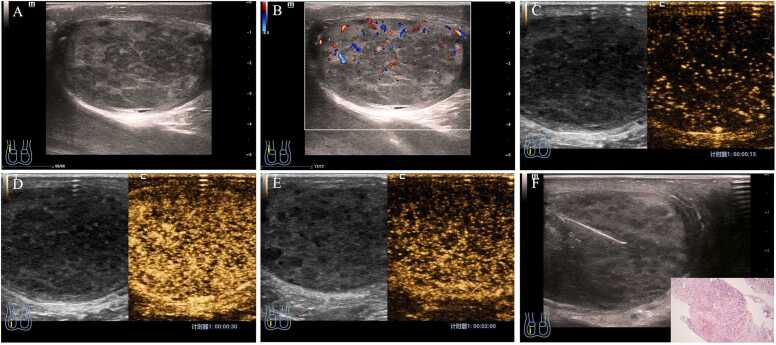
A 31-year-old male patient presented with a two-month history of pain and swelling in the right scrotum without obvious precipitating factors, no fever, no difficulty urinating, and no cough with sputum production. The patient sought medical attention due to exacerbation of scrotal discomfort. A chest computed tomography (CT) scan revealed minor chronic infiltrative pulmonary lesions. Laboratory tests indicated a positive T-SPOT.TB result, whereas Xpert MTB/RIF and mycobacterial DNA tests were negative. The patient underwent scrotal ultrasound examination using a Resona 7s system (Shenzhen Mindray Bio-Medical Electronics), which showed the right testicle measuring approximately 5.1 × 3.0 cm in size, with heterogeneous echotexture and abundant color Doppler blood flow signals (Fig. 1A,B). Contrast-enhanced ultrasound (CEUS) using SonoVue (Bracco) demonstrated rapid filling of the contrast agent within the right testicle, followed by visualization of a few irregular areas of enhancement, and subsequently slow washout of the contrast agent (Fig. 1C−E), attached is a detailed video(Video 1). Following these findings, the patient underwent a testicular biopsy, and the pathological results suggested granulomatous inflammation with caseous necrosis (Fig. 1F). The patient was actively treated for tuberculosis with a regimen including isoniazid, rifampicin, and levofloxacin.
Fig. 1.
Ultrasonographic (US) images of a 31-year-old male patient diagnosed with testicular tuberculosis. (A) B-mode ultrasound imaging revealed an enlarged testicle, measuring 5.1 × 8.0 cm, with an uneven internal echotexture, marked by the presence of numerous hypoechoic nodules diffusely scattered throughout the testicular parenchyma. (B) Color Doppler ultrasound demonstrated a rich blood flow signal pattern within the testis, indicating increased vascularity. (C-E) Contrast-enhanced ultrasound exhibited a non-uniform enhancement pattern, where the hypoechoic nodules diffusely present in the testis did not take up the contrast agent, suggestive of compromised perfusion within these areas. Figs. C, D and E show the arrival time of contrast agent of 15 s, 30 s and 120 s respectively. (F) An ultrasound-guided puncture biopsy confirmed the diagnosis of granulomatous inflammation accompanied by caseous necrosis. The lower right corner displays a histopathological image of testicular tuberculosis (HE, ×200).
Supplementary material related to this article can be found online at doi:10.1016/j.idcr.2024.e02089.
The following is the Supplementary material related to this article Video S1.
.
Ethical approval statement
This research was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Hangzhou Red Cross Hospital. Written informed consent for publication was obtained from the patients or their legal guardians. The patient's clinical and imaging information is protected by Chinese laws and is considered their personal data.
Consent
Written informed consent for publication was obtained from the patients and/or their legal guardians for publication. The patients’ clinical and imaging information are the patient’s private data, which are protected by Chinese laws.
Author agreement statement
We, the undersigned, declare that this manuscript is original, has not been published before, and is not currently under consideration for publication elsewhere. We confirm that the manuscript has been read and approved by all the named authors, and that there are no other individuals who meet the criteria for authorship but are not listed. We can also confirm that the order of authors listed in the manuscript has been approved by all of us. We understand that the Corresponding Author is the sole point of contact for the editorial process. They are responsible for communicating with other authors regarding progress, revisions, and final approval of proofs.
Funding source
This research was funded by funding from the Joint Pre-Research Foundation of Zhejiang University (ZAYY229) and the Hangzhou Medical and Health Science and Technology Project (A20220044, A20240074). The study funder had no involvement in the design, data collection, data analysis, data interpretation, or report writing of this study. The corresponding author had complete access to all study data and took the final responsibility for submitting it for publication.
CrediT authorship contribution statement
Xu Zhang: Funding acquisition, Project management, Resources, Supervision, Writing − review & editing; Dongming Su, Tu Ni, Yi Hu: Data curation, Formal analysis. All authors contributed equally to this work.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The author expressed gratitude to many members of our ultrasound team who helped with enrollment and evaluation of participants, and ultimately, the participants themselves.
Data availability
The corresponding author provides supplementary data for the current study upon reasonable request.
References
- 1.Li S., Chen B., Fang X., et al. A better understanding of testicular and/or epididymal tuberculosis based on clinical, ultrasonic, computed tomography, and magnetic resonance imaging features at a high-volume institute in the modern era. Quant Imaging Med Surg. 2021;11(6):2465–2476. doi: 10.21037/qims-20-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim S.H., Pollack H.M., Cho K.S., et al. Tuberculous epididymitis and epididymo-orchitis: sonographic findings. J Urol. 1993;150(1):81–84. doi: 10.1016/s0022-5347(17)35404-6. [DOI] [PubMed] [Google Scholar]
- 3.Park S.B., Lee W.C., Kim J.K., et al. Imaging features of benign solid testicular and paratesticular lesions. Eur Radio. 2011;21(10):2226–2234. doi: 10.1007/s00330-011-2155-x. [DOI] [PubMed] [Google Scholar]
- 4.Ramachandran A., Das C.J., Razik A. Male genital tract tuberculosis: a comprehensive review of imaging findings and differential diagnosis. Abdom Radio. 2021;46(4):1677–1686. doi: 10.1007/s00261-020-02811-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The corresponding author provides supplementary data for the current study upon reasonable request.