1. Introduction
Lenticular dissection and extraction are the most challenging steps in lenticule based refractive surgery.1 Inadvertent posterior dissection before anterior separation from the overlying cap is the most common underlying mechanism for cap lenticular adhesion and difficult lenticule extraction.2 Intraoperative white ring, meniscus, shimmer and stop signs have been elucidated to identify the correct plane of dissection.3 We hereby describe “Bubble sign” during SILK (smooth incision lenticular keratomileusis) to aid in lenticule surgery.
2. Material & methods
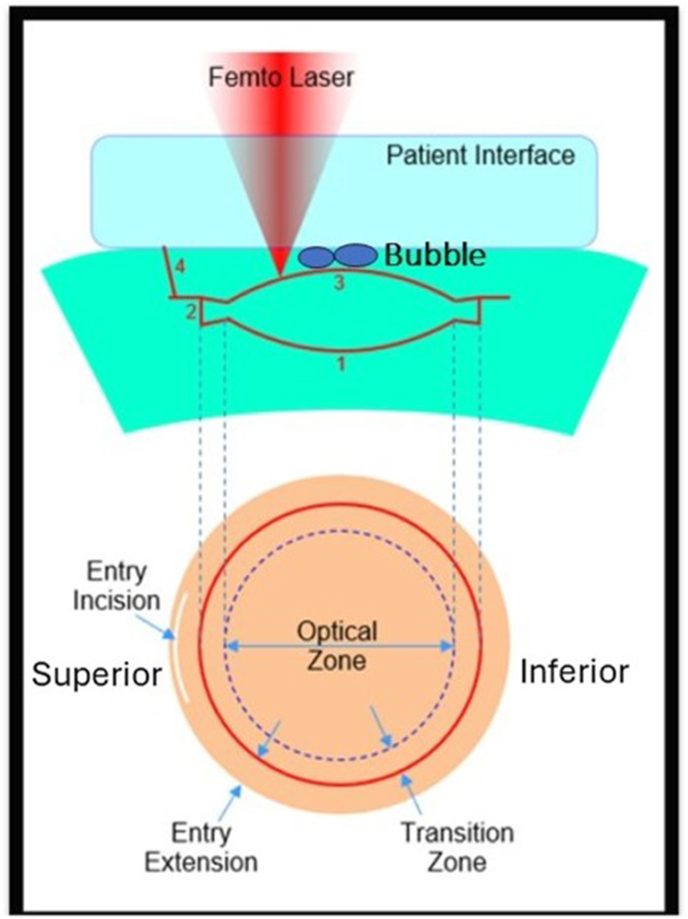
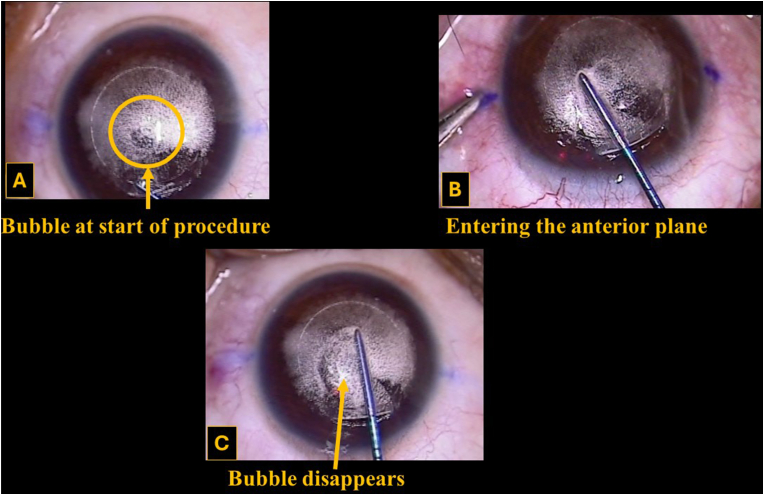
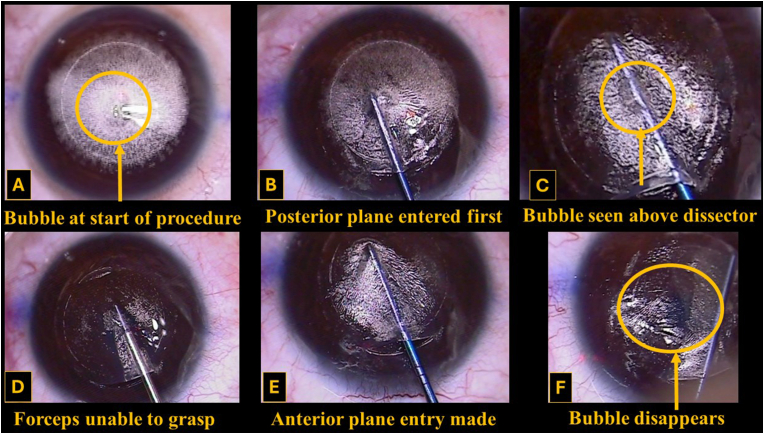
SILK was performed on 110 eyes of 55 patients. The lenticule was created with the ELITA femtosecond LASER (Johnson and Johnson Surgical Vision, Inc. Milpitas CA, USA) using a radial scanning pattern. Intended cap thickness was 110 μm, lenticule and cap diameter were 6.0 and 7.6 mm respectively. Entry incision of 4 mm was created superiorly. During the raster pattern the posterior cut was done first, followed by the ring resection (transition zone), anterior cut and finally the entry incision (Fig. 1). At the end of LASER application a bubble was noted in the anterior plane between the cap and anterior lenticule surface in 100 eyes. The bubble collapsed immediately when the dissector passed the center of the cornea (Fig. 2 and Video 1), in the anterior plane. In cases with inadvertent posterior dissection the bubble persisted (Fig. 3, Fig. 4 and Video 2).
Fig. 1.
Schematic representation of Lenticule creation during Smooth Incision Lenticular Keratomileusis (SILK) with bubble between cap and anterior lenticule surface.
1. Posterior lenticular resection
2. Ring resection
3. Anterior lenticular resection with entry extension
4. Entry resection.
Fig. 2.
Bubble between cap and anterior plane and its collapse during anterior plane dissection.
Fig. 3.
Inadvertent posterior plane entry with persistence of bubble at the centre of the cornea and its collapse with anterior plane dissection.
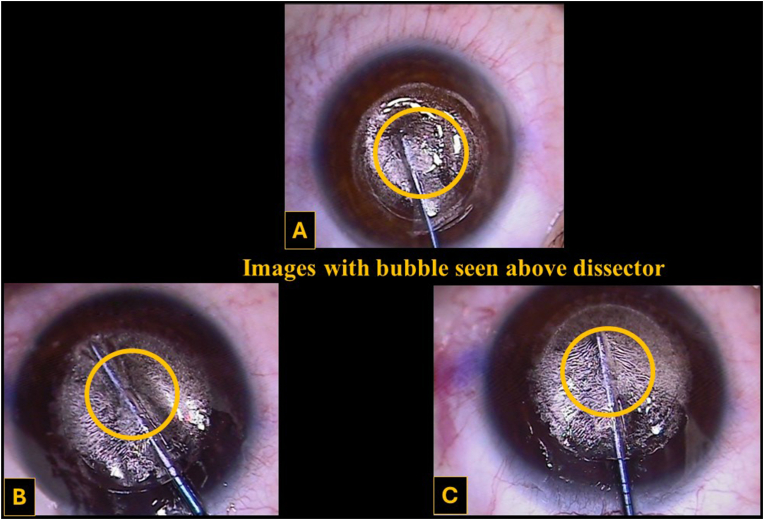
Fig. 4.
Persistence of bubble at the center of the cornea above the dissector with inadvertent entry into posterior plane.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ajoc.2024.102194
The following are the supplementary data related to this article:
Video 1: Demonstrating presence of bubble in the anterior plane and its collapse on correct anterior dissection.
1
Video 2: Demonstrating persistence of anterior bubble with inadvertent initial dissection of posterior plane with subsequent inability to extract lenticule. Eventual collapse of anterior plane bubble once the correct anterior dissection is performed.
2
3. Discussion
Various intraoperative signs have been described to make lenticule surgery easier.3 Observation of the central bubble and its collapse is an important and novel guide to correctly identify the anterior plane. The radial raster pattern, biconvex shape of the lenticule, ledge like ring resection cut and lack of a venting mechanism probably causes accumulation of gas bubbles in the centre of the cornea (Fig. 1). We have never observed a bubble form in the posterior plane. We suspect the thicker posterior corneal stroma may be the mechanism for not allowing bubble formation in the posterior plane. Flat applanation may also be a contributing factor for bubble formation. This sign can help the surgeon take corrective action in case the posterior plane is entered before the anterior plane (Fig. 3, Fig. 4 and Video 2). If the bubble is visible above the dissector as it crosses the centre of the cornea, the surgeon can stop and not proceed further with posterior plane dissection. Subsequently, the anterior plane can be entered from the other side of the entry cut. Once the dissector reaches the central cornea in the anterior plane the bubble collapses and the dissection can proceed normally.
4. Conclusion
The “Bubble sign” during SILK prevents accidental dissection of the posterior plane prior to anterior plane dissection.
Financial disclosure
No author has a financial or proprietary interest in any material or method mentioned.
CRediT authorship contribution statement
Rushad Shroff: Writing – original draft, Methodology, Investigation, Conceptualization. Ritu Arora: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. Apoorva Agrawal: Writing – original draft, Data curation. Palak Gupta: Writing – original draft, Data curation.
Patient consent
Written consent to publish this case has not been obtained. This report does not contain any personal identifying information.
Declaration of competing interest
The following authors have no financial disclosures (RS, RA, AA, PG).
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Funding
No funding or grant support
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors have no conflict of interest.
Acknowledgements
None.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ajoc.2024.102194.
Contributor Information
Rushad Shroff, Email: rushad09@gmail.com.
Ritu Arora, Email: dr_rituarora@yahoo.com.
Apoorva Agrawal, Email: doctorgirl.apoorva@gmail.com.
Palak Gupta, Email: palakg2017@gmail.com.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Titiyal J.S., Kaur M., Rathi A., Falera R., et al. Learning curve of small incision lenticule extraction: challenges and complications. Cornea. 2017;36:1377–1382. doi: 10.1097/ICO.0000000000001323. [DOI] [PubMed] [Google Scholar]
- 2.Shetty R., Negalur N., Shroff R., et al. Cap lenticular adhesion during small incision lenticular extraction surgery: causative factors and outcomes Asia Pac. J Ophthalmol (Phila) 2017;6:233–237. doi: 10.22608/APO.201619. [DOI] [PubMed] [Google Scholar]
- 3.Asif M.I., Bafna R.K., Mehta J.S., Reddy J., Titiyal J.S., et al. Complications of small incision lenticule extraction. Indian J Ophthalmol. 2020 Dec;68(12):2711–2722. doi: 10.4103/ijo.IJO_3258_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1: Demonstrating presence of bubble in the anterior plane and its collapse on correct anterior dissection.
1
Video 2: Demonstrating persistence of anterior bubble with inadvertent initial dissection of posterior plane with subsequent inability to extract lenticule. Eventual collapse of anterior plane bubble once the correct anterior dissection is performed.
2