Abstract
Background:
Early surgical management of full-thickness traumatic rotator cuff tears (RCTs) may optimize functional outcomes, prioritizing timely diagnoses. Ultrasound and magnetic resonance imaging (MRI) are highly sensitive and specific modalities for RCT diagnosis, yet MRI remains the gold standard diagnostic tool despite increased costs and potential delays in care. Ultrasound can provide same-day diagnosis, thus possibly expediting care.
Hypothesis:
The use of diagnostic shoulder ultrasound alone in the orthopaedic surgeon's office could increase the efficiency of diagnosis and care of traumatic full-thickness RCTs compared with MRI.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective chart review of patients with full-thickness traumatic RCT diagnosed via ultrasound or MRI who subsequently underwent rotator cuff repair with 1 of 2 ultrasound-trained surgeons between January 1, 2014, and December 31, 2019, was performed. Inclusion criteria included patients ≥18 years old, documentation of a first-time traumatic event, and the patient's desire to have immediate surgical management. Revision surgeries, long-term shoulder instability, and nontraumatic injuries were excluded. Basic demographic data were collected, and the number of preoperative office visits and the timing from initial evaluation to diagnosis and surgery were calculated for the ultrasound and the MRI cohorts. A power analysis of 0.8 with an alpha of .05 required 38 patients per group.
Results:
Overall, 133 patients were diagnosed via MRI compared with 76 via ultrasound. Besides body mass index, there were no significant differences in demographic variables or insurance status. Compared with the MRI cohort, patients in the ultrasound cohort received their diagnosis almost 2 weeks faster (P < .0001), were scheduled for surgery almost 3 weeks faster (P < .0001), and underwent surgery 2 weeks faster after initial evaluation (P < .0001) while requiring nearly half as many clinical visits (P < .0001). Regression analysis confirmed that ultrasound significantly reduced time to imaging, scheduling, and surgery after initial evaluation while requiring fewer clinical visits (P < .05).
Conclusion:
The study findings indicated that ultrasound was a time-saving alternative diagnostic modality for traumatic RCT compared with MRI without compromising standard of care. These results were achieved independent of patient insurance status, disability index, or other demographic variables.
Keywords: rotator cuff tear, ultrasound, MRI, cost, health economics, shoulder
Traumatic rotator cuff tears (RCTs) due to injury remain a common cause of shoulder pain and dysfunction, accounting for up to 40% of all RCTs, and they represent a leading cause of lost time from work or athletic activities.1,2 While controversy exists as to whether to surgically repair versus nonoperatively manage degenerative RCTs or tears in more elderly, inactive populations, there is literature suggesting operative repair of traumatic RCTs are warranted in order to maximize functional outcomes over long periods of time, allow patients to return to work sooner, and possibly incur less overall cost burden compared with prolonged nonoperative treatment.7,24,26
Timing to repair has also become a topic of debate. Recent literature has begun to show a trend toward worsening functional outcomes in patients who delay undergoing surgery for RCT. Gutman et al 17 demonstrated that ideal functional outcomes were seen in patients who underwent repair within 3 weeks of injury, with a significant drop-off in outcomes seen in patients who underwent surgery >4 months after traumatic RCT. Other studies have also suggested that 4 months may be the tipping point as to when outcomes begin to worsen.32,33
One limiting factor related to the timing of a patient's surgery is the necessary preoperative imaging. Magnetic resonance imaging (MRI) remains the gold standard for diagnosis of RCTs; however, MRIs do come at an increased cost while typically requiring separate appointments with variable wait times as well as a return visit to clinic for a surgical discussion based on the results.18,31 An alternative to MRI is the use of ultrasound to diagnose traumatic RCT. With increasing use in the orthopaedic clinic because of improvements in diagnostic accuracy, ultrasound can provide a point-of-care diagnosis within the same clinic visit at a significantly reduced cost to the patient, the clinician, and the institution.3,11,18 However, there is limited literature addressing whether ultrasound in practice improves efficiency of care and thus minimizes time to surgery in the clinical setting, and defrays costs as well.
The goal of this study is to investigate whether diagnostic shoulder ultrasound in the orthopaedic surgeon's office reduces the time from injury to surgical repair while using a significantly cheaper imaging modality compared with MRI. We hypothesized that ultrasound would lead to a faster diagnosis and time from injury to surgery compared with MRI.
Methods
A retrospective chart review of medical records was conducted in order to identify patients diagnosed with traumatic full-thickness RCT who had a rotator cuff repair between January 1, 2014, and December 31, 2019, by 2 board-certified orthopaedic surgeons, one of whom primarily used MRI to diagnose patients (M.D.M.) while the other preferred to use ultrasound (I.N.V.) in their respective practices (though both surgeons employed both imaging tools). Ultrasounds were performed in the office during the initial visit with the surgeon. Patients were screened via the following Current Procedural Terminology codes: 23140, 23412, 23420, and 29827. Chart review included analysis of clinical notes, demographic data, insurance status (commercial vs government), and zip code (for calculation of adjusted state-specific disability index [area deprivation index] to ensure patients in both groups had similar access to care).
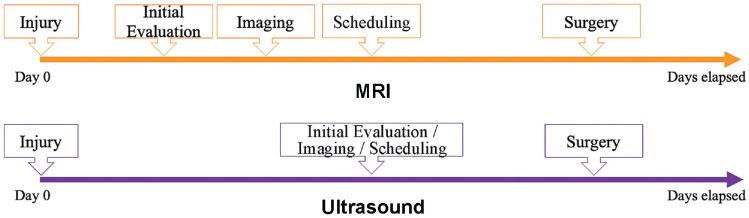
Inclusion criteria were as follows: patients ≥18 years of age, rotator cuff repair performed in the aforementioned time frame, a formal diagnosis of a full-thickness RCT by either diagnostic modality, a documented clinical depiction of a significant traumatic event without evidence of prior shoulder disease, and patients opting for immediate surgical management versus nonoperative treatment. Excluded were patients who had a diagnosis or had their imaging performed before evaluation by one of our surgeons, those who needed a revision repair, those with concurrent shoulder instability, those seeking coverage with workers’ compensation insurance, and those who opted to delay their surgery in order to seek nonoperative treatment first. We believed that patients who opted to delay their surgery or try nonoperative therapy first would confound analysis as to which modality gets patients to surgery sooner. The anticipated flow of clinical visits, diagnosis, and ultimate time to surgery is shown in Figure 1.
Figure 1.
Timeline from injury to surgery of the magnetic resonance imaging (MRI) and ultrasound cohorts.
Statistical Analysis
For statistical analysis, we sought multiple time points on chart review: injury date, date of initial evaluation by our orthopaedic surgeon or a member of the surgeon's staff, imaging modality (MRI vs ultrasound), the date a scheduling sheet was signed by the surgeon, and the date of surgery. The number of clinical visits before surgery was also documented. A mixed-effects model was used to account for multiple measurements over time in order to ascertain an interaction between number of days for each event between both diagnostic modalities. This accounted for item-level variability within patient and patient-level variability within groups. The threshold for statistically significant differences between groups was set at P < .05.
A power analysis of 0.8 with alpha .05 indicated 38 patients per group with an assumption that the ratio from time to first visit to surgery (measured in days) as well as the number of total clinic visits between both groups was ≥1.48 between MRI and ultrasound. Our power analysis and statistical analysis were performed by a statistician (G.A.R.)
Results
A total of 209 patients were included in the study: 133 in the MRI group and 76 in the ultrasound group. There was a significant group difference in body mass index, with the ultrasound group having significantly smaller values (P = .02); otherwise, no significant differences were noted in demographic characteristics or insurance status and area deprivation index for the state (Table 1). Of note, surgeon B had significantly more patients diagnosed via ultrasound compared with surgeon A (P < .001), which was anticipated, as the study was designed to compare the primary preferences of each surgeon's practice (surgeon B used ultrasound on a regular basis vs surgeon A). No patients who had an ultrasound required an MRI because of an unclear diagnosis.
Table 1.
Demographic Characteristics of the MRI Versus Ultrasound Cohorts a
| Total (N = 209) | MRI (n = 133; 63.64%) | Ultrasound (n = 76; 36.36%) | P | |
|---|---|---|---|---|
| Age, y | 61.56 ± 8.41 | 61.10 ± 9.10 | 62.35 ± 7.03 | .29 |
| Sex | .76 | |||
| Female | 52 (24.88) | 34 (25.56) | 18 (23.68) | |
| Male | 157 (75.12) | 99 (74.44) | 58 (76.32) | |
| Body mass index, kg/m2 | 29.95 ± 4.79 | 30.49 ± 5.03 | 29.02 ± 4.19 | .02 |
| Race | .24 | |||
| White | 192 (91.87) | 119 (89.47) | 73 (96.05) | |
| Black | 12 (5.74) | 10 (7.52) | 2 (2.63) | |
| Other | 5 (2.39) | 4 (3.01) | 1 (1.32) | |
| Ethnicity | .02 | |||
| Not Hispanic or Latino | 206 (98.56) | 133 (100.00) | 73 (96.05) | |
| Hispanic or Latino | 3 (1.44) | 0 (0.00) | 3 (3.95) | |
| Insurance | .92 | |||
| Commercial | 104 (49.76) | 65 (48.87) | 39 (51.32) | |
| Government | 81 (38.76) | 52 (39.10) | 29 (38.16) | |
| Other | 24 (11.48) | 16 (12.03) | 8 (10.53) | |
| Laterality | .92 | |||
| Left | 89 (42.58) | 57 (42.86) | 32 (42.11) | |
| Right | 120 (57.42) | 76 (57.14) | 44 (57.89) | |
| Surgeon | <.001 | |||
| Surgeon A | 92 (44.02) | 81 (60.90) | 11 (14.47) | |
| Surgeon B | 117 (55.98) | 52 (39.10) | 65 (85.53) | |
| ADI (New York State decile) | 7.91 ± 1.33 | 7.89 ± 1.31 | 7.95 ± 1.38 | .56 |
Data are presented as mean ± SD or n (%). Boldface P values indicate statistically significant difference between groups (P < .05). ADI, area deprivation index.
As shown in Table 2, patients in the ultrasound group had a significantly lower number of clinic visits before surgery (1.16 vs 2.3; P < .0001). Patients in the ultrasound group were evaluated in the clinic a mean of 12 days later than the MRI group (P < .0001), likely explained by potential differences in wait times for new patient visits between the practices of both surgeons. Despite this delay in evaluation, patients in the ultrasound group received their diagnosis almost 2 weeks sooner (P < .0001), were scheduled for surgery almost 3 weeks sooner (P < .0001), and underwent surgery 2 weeks faster (P < .0001) than the MRI cohort. It took on average 1 week to obtain an MRI for our patient population. The last finding, in particular, erased any delay in time noted from injury to evaluation between both cohorts, which accounts for both cohorts’ ultimately having an almost identical time from injury to surgery. Overall, regression analysis also confirmed that ultrasound significantly reduced time to imaging, scheduling, and surgery after initial evaluation while requiring fewer clinical visits (P < .05) (Appendix Table A1) after adjusting for age, race, sex, primary payor, laterality, surgeon, body mass index, and area deprivation index (New York State decile).
Table 2.
Unadjusted Outcomes for the MRI and Ultrasound Groups a
| MRI | Ultrasound | P | |
|---|---|---|---|
| Number of clinic visits before surgery | 2.30 ± 0.52 | 1.16 ± 0.37 | <.0001 |
| Days from injury to evaluation | 10 (2-31) | 22.5 (7-60) | <.0001 |
| Days from injury to imaging | 21 (12-38) | 22.5 (7-61) | .90 |
| Days from injury to scheduling for surgery | 35 (21-51) | 26.5 (9-61) | .07 |
| Days from injury to surgery | 64 (45-91) | 64.5 (37-102.5) | .66 |
| Days from evaluation to imaging | 7 (5-10) | 0 (0-0) | <.0001 |
| Days from evaluation to scheduling for surgery | 17 (12-25) | 0 (0-0) | <.0001 |
| Days from evaluation to surgery | 47 (33-67) | 33 (21.5-50) | <.0001 |
| Days from imaging to scheduling for surgery | 9 (5-14) | 0 (0-0) | <.0001 |
| Days from imaging to surgery | 37 (26-57) | 31.5 (20-50) | .05 |
| Days from scheduling to surgery | 26 (16-40) | 31 (19-48) | .12 |
Data are presented as mean ± SD or median (IQR). Boldface P values indicate statistically significant difference between groups (P < .05).
Patients in both cohorts were scheduled for surgery after imaging diagnosis in similar time frames and did not experience any delays from the scheduling itself to surgery, demonstrating that any differences in time gained or lost were primarily in the initial evaluation and diagnostic period (Figure 2 and Appendix Table A1).
Figure 2.
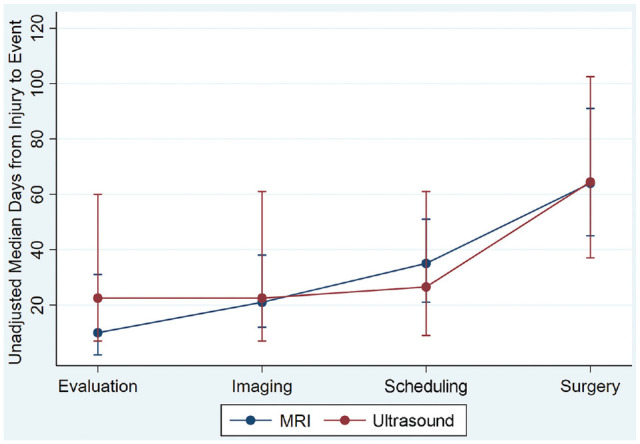
Predictive margins (at 95% CI) for adjusted median of cumulative days between events for the magnetic resonance imaging (MRI) and ultrasound cohorts. Error bars indicate IQR.
Of note, male patients tended to present later for initial evaluation after injury and had a longer time from injury to surgical scheduling compared with female patients (P < .05). Diagnostic modality did not affect timing from scheduling to surgery. Government-based insurance nearly led to a delay in surgical timing regardless of diagnostic modality, but this was not statistically significant. Both groups had similar area deprivation index values.
Discussion
The most important finding in our study was the confirmation that the use of in-office ultrasound for diagnosis of traumatic RCTs can save time compared with MRI without compromising standard of care. We were able to show significant reductions in time to diagnosis and time from initial diagnosis to surgery while requiring nearly half as many clinical visits regardless of insurance status or disability index. Therefore, given the right context, ultrasound can provide a significantly faster diagnosis and time savings to clinicians and patients alike.
RCT remains one of the most common causes of shoulder pain and dysfunction, and the decision to nonoperatively manage or acutely fix RCTs depends on a multitude of patient-specific factors, including whether the tear is acute or degenerative in nature, the age of the patient, and whether the patient should attempt a course of physical therapy before considering surgery.29,36 There is literature suggesting that nontraumatic RCTs do well with nonoperative management 20 ; physical therapy is a reasonable option in managing certain traumatic RCTs,35,39 though a recent meta-analysis by Piper et al 34 suggested that full-thickness RCT ultimately benefits from operative management. Rationale for this in part involves the likely progression of fatty infiltration and tendon retraction the longer surgery is delayed, though other factors such as tear size also play a role. In particular, supraspinatus muscle atrophy and fatty infiltration are linked as important factors in predicting the success of a repair or, in some cases, the future reparability of RCTs.13,15,21,28 Animal models suggest that fatty infiltration can begin as soon as 6 weeks after initial injury, though it may take years before becoming symptomatic in chronic degenerative cases.27,38 Clinical outcomes are tied to these variables, with a recent study indicating that 20-year functional outcomes after repair of massive RCT are negatively affected by fatty infiltration and increase the risk of tendon retear rates. 4 It should also be noted that even in patients with preoperative signs of the above factors who undergo repair, there may be neither postoperative improvement nor reversal of muscle degeneration; these factors should thus guide the preoperative patient-physician consultation. 14
With this in mind, the timing of treatment of RCTs has been extensively studied in order to optimize clinical outcomes. Multiple studies allude to a more expedient approach to surgically managing traumatic RCTs, with variable timelines suggested as to when outcomes may be compromised.17,33 Murphy et al, 30 and Petersen and Murphy 33 found that tears repaired after 4 months influenced patient outcomes but notably found that RCT size and preoperative fatty infiltration did not correlate with postoperative function. Patel et al 32 also used the 4-month mark in their study for comparing groups, finding that earlier repair led to a shorter recovery time and less need for allograft augmentation in large tears (>3 cm), though no major differences in patient-reported outcomes were seen at midterm (2-year) follow-up. Duncan et al 9 suggested that 6 months may be the breaking point as to whether repairing these tears is effective in successfully treating these patients and supported the creation of an acute shoulder injury referral clinic to capture this specific patient population. In their 2023 meta-analysis, van der List et al 40 suggested that delaying surgery for 3 to 6 months did not lead to higher retear rates or inferior patient-reported outcomes, but delaying surgery for 1 year did, though the authors cited the heavy reliance of retrospective studies in their work. Dimmen et al 8 found no differences in clinical outcomes when repairs were performed within 3 weeks to 3 months, or after 3 months from injury, though they included asymptomatic degenerative tears that later became symptomatic as part of their acute injury group. However, a retrospective review by Gutman et al 17 demonstrated that though patients did benefit from surgery within 4 months of injury (as in the study by Petersen and Murphy), optimal functional outcomes were seen in patients who had surgery within 3 weeks after injury, suggesting a more aggressive timeline for surgical management of acute traumatic RCTs may be more beneficial. Overall, the literature has not settled on a standardized time frame as to when traumatic RCT injury needs to be repaired in order to maximize clinical outcomes; however, given time may play a role in patient outcomes, our study does show an opportunity to reduce time lost from initial evaluation to surgery with use of in-office ultrasound.
Ultrasound has become an increasingly popular diagnostic modality for the diagnosis and treatment of multiple orthopaedic-related issues such as rotator cuff injuries.11,44 Though MRI remains the reference standard for diagnosis of RCT while also being able to evaluate bony and other soft tissue pathologies such as articular cartilage or labral defects (particularly in younger patients), the expense of obtaining MRIs; their availability to patients; and contraindications to their use such as pacemakers, implants, or severe claustrophobia (despite newer acoustic noise reduction and short magnetic bore rates) have encouraged physicians to explore ultrasound as a faster and cheaper alternative for RCT diagnosis.6,12,23 Most importantly, recent literature now suggests that radiologists and orthopaedic surgeons alike are demonstrating much more prowess in both diagnosing and managing RCT with ultrasound alone, with data suggesting the diagnostic accuracy of full-thickness RCT is now similar between MRI and ultrasound.5,11,37,44 In fact, a recent survey involving members of the American Shoulder and Elbow Surgeons 16 suggested that 55% of members already use ultrasound for diagnostic purposes in the shoulder, though the leading reason for current lack of ultrasound use was a lack of confidence in assessing its ability to determine the reparability of a tear and whether there is already too much fatty infiltration present and thus high risk of failure. 19 However, published literature 41 shows that ultrasound has appropriately assessed at least fatty degeneration. 41 Murphy et al 30 originally demonstrated that an orthopaedic surgeon can obtain equivalent accuracy between ultrasound and MRI in the diagnosing of RCTs after performing 50 to 100 scans, which further work does seem to support, 22 hopefully encouraging future practicing surgeons to adopt ultrasound into their practice.
From a cost perspective, the literature is increasingly showing, for both clinicians and patients, that ultrasound significantly reduces health care–related expenditures. MRI scans remain significantly more expensive than ultrasound, and diagnostic imaging with MRI remains the most expensive cost associated with preoperative evaluation of RCT, with the number of outpatient visits being the second-most expensive charge. 42 For clinicians, ultrasound use amounts to increased revenue and averted costs, as a clinician can be reimbursed for one's procedural diagnosis while spending less time awaiting a diagnosis and more time enacting a patient-specific plan. 18 At our institution, an outpatient MRI scan costs US$1895 (2024 currency rate) versus an estimated US$256 for diagnosis of RCT via surgeon-performed outpatient ultrasound (of note, cost and reimbursement can be variable), which does not factor in the cost of delayed imaging results for not only RCT patients but also patients waiting to undergo MRI for any reason. The model by Huynh et al 18 does address the sunk cost of purchasing and managing an ultrasound machine in the clinic, which requires years to pay off if only assessing RCTs. However, one can also alleviate costs by seeking reimbursement for ultrasound-guided acromioclavicular and glenohumeral joint injections, though this may vary based on insurance reimbursement policies. Further, only bicipital groove injections under ultrasound lead to superior outcomes, and there is a theoretical concern that ultrasound use in clinic can decrease clinic efficiency, though there is limited literature to support this claim. 10
From a patient's perspective, ultrasound diagnosis of RCT may lead to significant cost reductions as well. For patients, major costs associated with delays in surgical diagnosis and management relate to productivity losses because of absenteeism from work, with estimates of US$8524 spent/lost in the delay from diagnosis to surgery for full-thickness RCT. 31 Additional time out of work spent going to multiple appointments, time spent undergoing the MRI, and travel savings (time spent out of work, transporation costs, etc) going to those appointments represent additional expenses and wages lost that are worsened when having to undergo an MRI for diagnosis. 18 In 2021, Huynh et al 18 calculated a net cost-benefit difference of US$3058 after 1 year of ultrasound implementation, which increased to US$218,162 after 5 years (>50% of these savings are due to avoiding separate radiology and additional follow-up visits with the surgeon). Furthermore, patients without insurance or those with high premiums associated with MRI use are more likely to have worse clinical and patient-reported outcomes in part because of a delay in care, which also decreases the ability to return to work, one of the most important societal postoperative metrics in RCT repair.25,43 Our study findings therefore demonstrate that ultrasound can have the ability to significantly curtail both health care expenditures and patient costs.
Limitations
There are multiple limitations to this study—namely, its retrospective nature in assessing only patients who already had an associated RCT diagnosis and underwent surgery. The lack of prospective data did not allow us to adequately explore the sensitivity/specificity of ultrasound versus MRI diagnosis of RCT in our patient population, nor did it allow for the collection of postoperative outcomes to assess if a delayed surgery due to imaging (or delayed access to care) affected postoperative outcomes or not. Though both surgeons contributed to both arms of the study, it should be noted that one surgeon performed ultrasounds with higher frequency than the other and that the indications for either ultrasound or MRI were not standardized, adding additional bias to the study. Furthermore, because of the time when patient data were collected at our institution for this patient population, we were also unable to provide more rigorous financial data related to this population subset supporting the institutional financial savings. This will be a point of interest in future work. Finally, it is important to acknowledge that there was a significant difference in time from initial injury to evaluation between imaging modality groups in part because of scheduling availability of our 2 surgeons as well as the fact that scheduling availability made it difficult to surgically attend to most patients within 3 weeks of injury. It is reasonable to argue that quicker access to a shoulder surgeon in general can effectively reduce time from injury to surgery regardless of imaging modality; however, this point is variable by practice and location. Therefore, the results of this study may not apply to other practices with different levels of resource availability.
Conclusion
The study findings indicated that ultrasound use for the diagnosis of acute traumatic RCT has the potential to save time for clinicians and patients alike by reducing diagnostic imaging costs, the number of clinical visits required before surgery, and the time lost from evaluation to surgery. These results were achieved independent of insurance status and area deprivation index. In-office ultrasound use for RCT diagnosis warrants further evaluation as it relates to ultimate outcomes and overall cost savings.
Appendix
Table A1.
Results of Regression Analysis a
| Variable | Visits Before Surgery | Cumulative Days From Injury to Surgery | ||
|---|---|---|---|---|
| IRR (95% CI) | P | Coefficient (95% CI) | P | |
| Imaging modality | ||||
| MRI | Reference | Reference | ||
| Ultrasound | 0.490 (0.377 to 0.638) | <.01 | 15.684 (3.412 to 27.956) | .012 |
| Event | ||||
| Evaluation | — | — | Reference | |
| Imaging | — | — | 9.142 (5.937 to 12.346) | .0001 |
| Scheduling | — | — | 20.362 (17.157 to 23.567) | .0001 |
| Surgery | — | — | 50.921 (47.717 to 54.126) | .0001 |
| Days between modality × event | ||||
| MRI to evaluation | — | — | Reference | |
| MRI to imaging | — | — | Reference | |
| MRI to scheduling | — | — | Reference | |
| MRI to surgery | — | — | Reference | |
| Ultrasound to evaluation | — | — | Reference | |
| Ultrasound to imaging | — | — | −8.234 (–13.471 to −2.996) | .002 |
| Ultrasound to scheduling | — | — | −17.823 (–23.060 to −12.585) | .0001 |
| Ultrasound to surgery | — | — | −14.342 (–19.580 to −9.105) | .0001 |
| Age | 1.003 (0.989 to 1.017) | .661 | 0.152 (–0.547 to 0.851) | .670 |
| Race | ||||
| White | Reference | Reference | ||
| Black | 0.986 (0.637 to 1.527) | .951 | −3.524 (–25.865 to 18.817) | .757 |
| Other | 1.078 (0.582 to 1.998) | .810 | −8.310 (–41.517 to 24.896) | .624 |
| Sex | ||||
| Female | Reference | Reference | ||
| Male | 1.030 (0.808 to 1.311) | .814 | −12.067 (–24.036 to −0.097) | .048 |
| Insurance | ||||
| Commercial | Reference | Reference | ||
| Government | 0.907 (0.702 to 1.171) | .454 | −5.999 (–18.502 to 6.504) | .347 |
| Other | 0.993 (0.711 to 1.388) | .968 | −11.611 (–28.626 to 5.405) | .181 |
| Laterality | ||||
| Left | Reference | Reference | ||
| Right | 1.010 (0.810 to 1.258) | .931 | −0.503 (–11.399 to 10.393) | .928 |
| Surgeon | ||||
| A | Reference | Reference | ||
| B | 1.031 (0.821 to 1.293) | .794 | 1.460 (–10.216 to 13.136) | .806 |
| Body mass index, kg/m2 | 0.998 (0.977 to 1.019) | .828 | 0.431 (–0.645 to 1.507) | .432 |
| ADI (New York State decile) | 1.008 (0.931 to 1.091) | .845 | 0.467 (–3.412 to 4.346) | .813 |
Dashes indicate areas not applicable. Boldface P values indicate statistically significant difference compared with reference variable (P < .05). ADI, area deprivation index; IRR, injury rate ratio; MRI, magnetic resonance imaging.
Footnotes
Final revision submitted March 29, 2024; accepted April 15, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.D.M. has received consulting fees and nonconsulting fees from Arthrex. I.N.V. has received consulting fees from FH Orthopedics, Zimmer Biomet, and Arthrex; nonconsulting fees from Arthrex, Smith & Nephew, and Arthrosurface; and royalties from Smith+Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the University of Rochester (ref No. STUDY00007659).
ORCID iDs: Linda Zhang  https://orcid.org/0000-0002-7139-3687
https://orcid.org/0000-0002-7139-3687
Ilya N. Voloshin  https://orcid.org/0000-0003-0161-4314
https://orcid.org/0000-0003-0161-4314
References
- 1. Abdelwahab A, Ahuja N, Iyengar KP, Jain VK, Bakti N, Singh B. Traumatic rotator cuff tears—current concepts in diagnosis and management. J Clin Orthop Trauma. 2021;18:51-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92(9):1894-1908. [DOI] [PubMed] [Google Scholar]
- 3. Chiu CH, Chen P, Chen AC, et al. Shoulder ultrasonography performed by orthopedic surgeons increases efficiency in diagnosis of rotator cuff tears. J Orthop Surg Res. 2017;12(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Collin P, Betz M, Herve A, et al. Clinical and structural outcome 20 years after repair of massive rotator cuff tears. J Shoulder Elbow Surg. 2020;29(3):521-526. [DOI] [PubMed] [Google Scholar]
- 5. de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192(6):1701-1707. [DOI] [PubMed] [Google Scholar]
- 6. Dewey M, Schink T, Dewey CF. Claustrophobia during magnetic resonance imaging: cohort study in over 55,000 patients. J Magn Reson Imaging. 2007;26(5):1322-1327. [DOI] [PubMed] [Google Scholar]
- 7. Dey Hazra RO, Dey Hazra ME, Hanson JA, et al. Minimum 10-year outcomes after arthroscopic repair of partial-thickness supraspinatus rotator cuff tears. Am J Sports Med. 2023;51(9):2404-2410. [DOI] [PubMed] [Google Scholar]
- 8. Dimmen S, Owesen C, Lundgreen K, Jenssen KK. No difference in clinical outcome after rotator cuff repair performed within or later than 3 months after trauma: a retrospective cohort study. Knee Surg Sports Traumatol Arthrosc. 2023;31(2):672-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Duncan NS, Booker SJ, Gooding BW, Geoghegan J, Wallace WA, Manning PA. Surgery within 6 months of an acute rotator cuff tear significantly improves outcome. J Shoulder Elbow Surg. 2015;24(12):1876-1880. [DOI] [PubMed] [Google Scholar]
- 10. Fan D, Liu X, Ma J, et al. Ultrasound guidance is not superior in subacromial bursa and intraarticular injections but superior in bicipital groove: a meta-analysis of randomized controlled trials. Arthroscopy. 2022;38(5):1642-1657. [DOI] [PubMed] [Google Scholar]
- 11. Farooqi AS, Lee A, Novikov D, et al. Diagnostic accuracy of ultrasonography for rotator cuff tears: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(10):23259671211035106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fischer CA, Weber MA, Neubecker C, Bruckner T, Tanner M, Zeifang F., Ultrasound vs. MRI in the assessment of rotator cuff structure prior to shoulder arthroplasty. J Orthop. 2015;12(1):23-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007;16(6):691-696. [DOI] [PubMed] [Google Scholar]
- 14. Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35(5):719-728. [DOI] [PubMed] [Google Scholar]
- 15. Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12(6):550-554. [DOI] [PubMed] [Google Scholar]
- 16. Griffith DE, Aksamit T, Brown-Elliott BA, et al. ; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367-416. [DOI] [PubMed] [Google Scholar]
- 17. Gutman MJ, Joyce CD, Patel MS, et al. Early repair of traumatic rotator cuff tears improves functional outcomes. J Shoulder Elbow Surg. 2021;30(11):2475-2483. [DOI] [PubMed] [Google Scholar]
- 18. Huynh KA, Yoon AP, Seyferth AV, Chung KC. Cost-benefit analysis of ultrasonography in the hand clinic. Plast Reconstr Surg. 2021;147(4):894-902. [DOI] [PubMed] [Google Scholar]
- 19. Kruse KK, Dilisio MF, Wang WL, Schmidt CC. Do we really need to order magnetic resonance imaging? Shoulder surgeon ultrasound practice patterns and beliefs. JSES Open Access. 2019;3(2):93-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kukkonen J, Ryösä A, Joukainen A, et al. Operative versus conservative treatment of small, nontraumatic supraspinatus tears in patients older than 55 years: over 5-year follow-up of a randomized controlled trial. J Shoulder Elbow Surg. 2021;30(11):2455-2464. [DOI] [PubMed] [Google Scholar]
- 21. Kuptniratsaikul V, Laohathaimongkol T, Umprai V, Yeekian C, Prasathaporn N. Pre-operative factors correlated with arthroscopic reparability of large-to-massive rotator cuff tears. BMC Musculoskelet Disord. 2019;20(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kurz AZ, Kelly MJ, Hackett L, Murrell GA. Effect of surgeon-sonographer interaction on ultrasound diagnosis of rotator cuff tears: a five-year cohort study in 775 shoulders. J Shoulder Elbow Surg. 2016;25(9):1385-1394. [DOI] [PubMed] [Google Scholar]
- 23. Levine BD, Motamedi K, Seeger LL. Imaging of the shoulder: a comparison of MRI and ultrasound. Curr Sports Med Rep. 2012;11(5):239-243. [DOI] [PubMed] [Google Scholar]
- 24. Lin EC, Mall NA, Dhawan A, et al. Arthroscopic primary rotator cuff repairs in patients aged younger than 45 years. Arthroscopy. 2013;29(5):811-817. [DOI] [PubMed] [Google Scholar]
- 25. Mandalia K, Ames A, Parzick JC, Ives K, Ross G, Shah S. Social determinants of health influence clinical outcomes of patients undergoing rotator cuff repair: a systematic review. J Shoulder Elbow Surg. 2023;32(2):419-434. [DOI] [PubMed] [Google Scholar]
- 26. Mather RC, 3rd, Koenig L, Acevedo D, et al. The societal and economic value of rotator cuff repair. J Bone Joint Surg Am. 2013;95(22):1993-2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010;468(6):1498-1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Meyer DC, Wieser K, Farshad M, Gerber C. Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med. 2012;40(10):2242-2247. [DOI] [PubMed] [Google Scholar]
- 29. Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331(7525):1124-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Murphy RJ, Daines MT, Carr AJ, Rees JL. An independent learning method for orthopaedic surgeons performing shoulder ultrasound to identify full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 2013;95(3):266-272. [DOI] [PubMed] [Google Scholar]
- 31. Parikh N, Martinez DJ, Winer I, Costa L, Dua D, Trueman P. Direct and indirect economic burden associated with rotator cuff tears and repairs in the US. Curr Med Res Opin. 2021;37(7):1199-1211. [DOI] [PubMed] [Google Scholar]
- 32. Patel V, Thomas C, Fort H, et al. Early versus delayed repair of traumatic rotator cuff tears. Does timing matter on outcomes? Eur J Orthop Surg Traumatol. 2022;32(2):269-277. [DOI] [PubMed] [Google Scholar]
- 33. Petersen SA, Murphy TP. The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg. 2011;20(1):62-68. [DOI] [PubMed] [Google Scholar]
- 34. Piper CC, Hughes AJ, Ma Y, Wang H, Neviaser AS. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2018;27(3):572-576. [DOI] [PubMed] [Google Scholar]
- 35. Ranebo MC, Bjornsson Hallgren HC, Holmgren T, Adolfsson LE. Surgery and physiotherapy were both successful in the treatment of small, acute, traumatic rotator cuff tears: a prospective randomized trial. J Shoulder Elbow Surg. 2020;29(3):459-470. [DOI] [PubMed] [Google Scholar]
- 36. Rees JL. The pathogenesis and surgical treatment of tears of the rotator cuff. J Bone Joint Surg Br. 2008;90(7):827-832. [DOI] [PubMed] [Google Scholar]
- 37. Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1316-1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rubino LJ, Stills HF, Jr, Sprott DC, Crosby LA. Fatty infiltration of the torn rotator cuff worsens over time in a rabbit model. Arthroscopy. 2007;23(7):717-722. [DOI] [PubMed] [Google Scholar]
- 39. Ryosa A, Laimi K, Aarimaa V, Lehtimaki K, Kukkonen J, Saltychev M. Surgery or conservative treatment for rotator cuff tear: a meta-analysis. Disabil Rehabil. 2017;39(14):1357-1363. [DOI] [PubMed] [Google Scholar]
- 40. van der List JP, Kok LM, Alta TDW, van der List MPJ, van Noort A. Role of delay between injury and surgery on the outcomes of rotator cuff repair: a systematic review and meta-analysis. Am J Sports Med. 2023;51(5):1328-1339. [DOI] [PubMed] [Google Scholar]
- 41. Wall LB, Teefey SA, Middleton WD, et al. Diagnostic performance and reliability of ultrasonography for fatty degeneration of the rotator cuff muscles. J Bone Joint Surg Am. 2012;94(12):e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yeranosian MG, Terrell RD, Wang JC, McAllister DR, Petrigliano FA. The costs associated with the evaluation of rotator cuff tears before surgical repair. J Shoulder Elbow Surg. 2013;22(12):1662-1666. [DOI] [PubMed] [Google Scholar]
- 43. Ziedas AC, Castle JP, Abed V, et al. Race and socioeconomic status are associated with inferior patient-reported outcome measures following rotator cuff repair. Arthroscopy. 2023;39(2):234-242. [DOI] [PubMed] [Google Scholar]
- 44. Zoga AC, Kamel SI, Hynes JP, Kavanagh EC, O’Connor PJ, Forster BB. The evolving roles of MRI and ultrasound in first-line imaging of rotator cuff injuries. AJR Am J Roentgenol. 2021;217(6):1390-1400. [DOI] [PubMed] [Google Scholar]