Abstract
Background
Therapeutic digital health applications (DiGAs) are expected to significantly enhance access to evidence-based care. Since 2020, German physicians and psychotherapists have been able to prescribe approved DiGAs, which are reimbursed by statutory health insurance. This study investigates the usage, knowledge and perception of DiGAs as well as the growing digitalization among internal medicine physicians in Germany.
Methods
A web-based survey was distributed at the 2024 annual congress of the German Society for Internal Medicine. Participants could respond by scanning a QR code or directly on a tablet.
Results
A total of 100 physicians completed the survey, with a mean age of 43.4 years. The majority were internal medicine physicians (85%). Of the respondents, 31% had already prescribed DiGAs, and 29% had tested one. Self-rated knowledge of DiGAs was low (median score 3.17/10). The main barriers identified were lack of knowledge about effective implementation (60%), lack of time for patient onboarding (27%), and concerns about patient adherence (21%). However, 92% believed that DiGAs could improve care, and 88% expressed interest in specific digital health training. The majority (64%) stated that digitalization had a positive impact on medical care and 39% of physicians expected their daily workload to decrease due to digitalization. In addition, 38% believed that the physician-patient relationship would improve as a result of digitalization.
Conclusions
While physicians widely acknowledged the potential benefits of DiGAs, adoption and understanding remain limited. Specific training in digital health is crucial to accelerate digitalization in internal medicine.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11807-1.
Keywords: Digital health applications, DiGA, Digitalization in medicine, Adoption barriers, German healthcare
Introduction
The integration of digital technologies into clinical routine, in particular therapeutic digital health applications, offers instant access to evidence-based, personalized treatment. In 2019, a new regulatory framework in Germany has enabled the prescription and reimbursement of approved digital health applications (DiGAs) under the statutory health insurance [1, 2]. The German Federal Institute for Drugs and Medical Devices (BfArM) oversees the evaluation of these applications, ensuring their safety and efficacy, and maintains a library of approved DiGAs [3]. In October 2024, 64 DiGAs have been approved, with the number steadily increasing. These approved DiGAs now include a growing range of internal medicine conditions such as diabetes, hypertension, and heart failure. Additionally, internal medicine physicians can prescribe mental health and orthopedic DiGAs to provide holistic treatment support and help bridge the gap while patients await specialist appointments.
Despite their considerable potential, the successful adoption of DiGAs relies on both healthcare professionals and patients. This challenge reflects a general trend in digital health, where the adoption of new technologies often faces barriers related to user familiarity, system integration issues, and concerns about effectiveness, data security and reliability [4–7]. While previous studies demonstrated the high patient acceptance of DiGAs [8–10], patient acceptance and consent are prerequisites for the effective sharing of personal health information (PHI) through health information exchanges (HIEs) [11]. A study by Busch-Castler et al. found that German patients were willing to share their PHI with HIEs under certain conditions, including perceived information security and a non-commercial organization as the recipient of the PHI [11]. The study also highlighted the importance of face-to-face interactions with physicians in increasing trust in digital health apps and PHI sharing. In contrast, little evidence exists regarding physicians’ usage and perception of DiGAs. Initial studies have focused on general practitioners and rheumatologists and identified implementation barriers such as inadequate reimbursement and poor knowledge [12, 13]. A comprehensive survey conducted in January 2021 examined the experiences of physicians and psychotherapists with DiGAs. However, this study did not address broader perceptions of digitalization in medicine, and its findings on DiGA usage may have shifted due to the rapid pace of digital health advancements [14]. Therefore, the aim of this study was to investigate the usage and perception of DiGAs as well as the increasing digitalization among German internal medicine physicians.
Methods
Design and setting
A web-based survey was completed by physicians attending the annual congress of the German Society for Internal Medicine (Deutsche Gesellschaft für Innere Medizin, DGIM) between April 13 and April 16, 2024. Participants could either complete their responses directly on an iPad on-site or scan a QR code to answer the questions anonymously on their own smart devices. The German Society for Internal Medicine is one of the largest European medicine societies with more than 30.000 active members [15]. The Philipps-University Marburg Research Ethics Committee confirmed that no ethical approval was required (24-34 ANZ) for this anonymous survey study.
Survey
An initial survey draft was created by LC and JK. All authors provided improving comments and approved the final version. The final web-based survey was created using Google Forms and consisted of 16 questions, including 5 questions on personal characteristics (age, gender, work), 5 questions on DiGAs, 5 questions on digitalization in general, and 1 question on whether a dedicated workshop to integrate digital health technologies would be welcomed (translated version, see supplementary file 1).
Specifically, the DiGA-related questions asked whether physicians had ever prescribed or tested a DiGA, how they would rate their own level of knowledge about DiGAs on an 10-point Likert scale (0 = no knowledge, 10 = great knowledge) and what barriers they perceived in prescribing DiGAs. The digitalization-related questions focused on whether digitalization in general improves patient care (5-point Likert scale: 1 = very negative, 5 = very positive), and whether digitalization will reduce or increase physicians’ workload in the future (5-point Likert scale: 1 = my workload will increase due to digitalization, 5 = my workload will decrease due to digitalization), its expected effect on the doctor-patient relationship (5-point Likert scale: 1 = the doctor-patient relationship will significantly worsen due to digitalization, 5 = the doctor-patient relationship will significantly improve due to digitalization), and where they see the potential of digitalization, and what barriers they perceive, including optional free text responses.
Statistical analysis
The study followed the Checklist for Reporting Results of Internet E-Surveys to guide methodology and presentation of results [16]. Descriptive and summary statistics were used, with frequencies and percentages calculated for categorical variables. Analyses were performed using R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria) and Excel Windows (Microsoft Corporation, Redmond, WA, USA).
Results
Demographics
A total of 100 participants completed the survey, of whom 51% were male, 48% female and 1% identified as diverse. The mean age was 43.4 years. The majority of physicians (65%) were consultants, with 30% working at university hospitals and 85% in internal medicine (see Table 1 for detailed characteristics).
Table 1.
Physician characteristics
| Characteristics | Respondents, n (%) |
|---|---|
| Sex | |
| Female | 48 (48.0) |
| Male | 51 (51.0) |
| Diverse | 01 ( 1.0) |
| Age (years) | |
| 20-30 | 16 (16.0) |
| 31-40 | 35 (35.0) |
| 41-50 | 16 (16.0) |
| 51-60 | 24 (24.0) |
| >61 | 9 (9.0) |
| Medical Career Stages | |
| Resident physician | 29 (29.0) |
| Consultant physician | 65 (65.0) |
| Other Designations | 6 (6.0) |
| Specialization | |
| General Medicine | 7 (7.0) |
| Internal Medicine | 85 (85.0) |
| Other specialties | 8 (8.0) |
| Work environment | |
| Solo Practice | 13 (13.0) |
| Group Practice | 16 (16.0) |
| Medical Care Center | 7 (7.0) |
| Basic Care Hospital | 17 (17.0) |
| Tertiary Care Hospital | 17 (17.0) |
| University Hospital | 30 (30.0) |
DiGA use and knowledge
Of the physicians surveyed, 31% had previously prescribed DiGAs. Of these, 14% had prescribed DiGAs 10 or more times, with two physicians reporting around 100 DiGA prescriptions. Pearson correlation analysis showed a significant positive correlation between physician age and the number of DiGA prescriptions (r = 0.259, p = 0.009). Perceived knowledge about DiGAs was relatively low, with a median self-rating of 3/10 (IQR: 2-5). There was also a significant positive correlation observed between physician age and their self-rated knowledge of DiGAs (r = 0.378, p<0.001). In addition,the number of DiGA prescriptions was significantly positively correlated with perceived knowledge about DiGAs (r = 0.295, p = 0.003). Overall, 29% of physicians had tested at least one DiGA, and 13% had tested more than one DiGA. 92% of physicians believed that DiGAs had the potential to improve patient care.
Perceived barriers to DiGAs
The most commonly reported barriers to prescribing DiGAs (Table 2) were lack of knowledge (60%), lack of time to onboard patients (27%), and concerns about patient adherence (21%).
Table 2.
DiGA perceptions
| Question and answers | n (%) |
|---|---|
| Do you think digital health applications can improve care? | |
| Yes | 92 (92%) |
| No | 8 (8%) |
| What do you see as the biggest barrier to the prescription of DiGAs?a | |
| Little knowledge about implementation | 60 (60%) |
| Lack of time for patient onboarding | 27 (27%) |
| Poor adherence of patients | 21 (21%) |
| Lack of trust in effectiveness | 19 (19%) |
| Lack of adherence of patients | 18 (18%) |
| Little/no remuneration | 14 (14%) |
| Complicated prescription process | 12 (12%) |
| Free text responsesb | 15 (15%) |
aMultiple answers were possible.
bOther barriers mentioned include financial concerns, doubts about effectiveness, technical difficulties as well as problems with communication and use
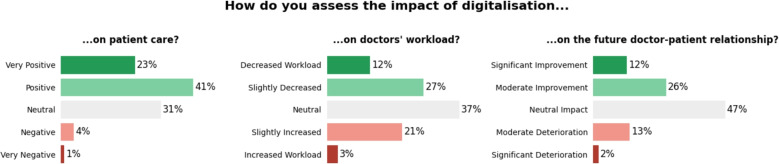
Perceived impact of digitalization
The majority of physicians (65%) answered that digitalization has had a positive impact on medical care (Fig. 1). In terms of workload, 24% of respondents expected their daily workload to increase as a result of digitalization, while 39% expected it to decrease. In addition, 38% of the respondents believed that digitalization would improve the physician-patient relationship , while 15% believed it would worsen it.
Fig. 1.
Perceived impact of digitalization of patient care
Perceived benefits and barriers of increasing digitalization of medicine
The main perceived benefits of digitalization were the reduction of repetitive tasks (68%), improved diagnostic and treatment decisions (42%), and better standardization of evidence-based decisions (36%). However, the main barriers were insufficient knowledge of how to use digital tools (51%), concerns about data security (46%), and lack of trust in digital tools (20%) (Table 3). The majority (88%) of physicians expressed interest in specific training on the use of digital tools in clinical practice.
Table 3.
Perceived benefits and barriers of increasing digitalization of medicine
| Question and answers | n (%) |
|---|---|
| What is the biggest advantage of digitalization in medicine for you?a | |
| Reduction of repetitive activities | 68 (68%) |
| Improved diagnosis/therapy decisions | 42 (42%) |
| Better standardization of clinical decisions (evidence-based medicine) | 36 (36%) |
| More personalized patient care | 30 (30%) |
| More cost-effective patient care | 23 (23%) |
| Free text responsesb | 6 (6%) |
| What is the biggest barrier to the general use of digitalization for you?a | |
| Insufficient knowledge on how to use digital tools | 51 (51%) |
| Data security | 46 (46%) |
| Lack of trust in digital tools | 20 (20%) |
| Fear of the influence of large technology companies | 16 (16%) |
| Responsibility issues when using digital tools | 16 (16%) |
| Fear of digital tools as a new control instance or gold standard that one has to adhere to | 15 (15%) |
| High costs | 12 (12%) |
| Free text responsesc | 3 (3%) |
aMultiple answers were possible.
bOther advantages mentioned include more time with patients, improved patient guidance, higher therapy adherence, and better monitoring and information transfer.
cOther barriers mentioned include poor usability, unreliability, and technical problems
Discussion
The primary objective of this survey study was to investigate the usage and perception of DiGAs in the context of the increasing digitalization in medicine among German internal medicine physicians. Internal medicine is heavily characterized by the management of chronic diseases, which are associated with significant healthcare costs [17]. While the benefits of lifestyle interventions for these conditions are well established [18], current treatments often remain medication-centric. DiGAs offer a promising tool for enhancing patient self-management, potentially unlocking the full potential of lifestyle interventions to complement conventional treatments. The potential of digital therapeutics is increasingly recognized in other countries, such as Belgium and France, which have also implemented regulatory and reimbursement frameworks to support their adoption [19].
The results revealed a significant discrepancy between physician’s belief in the potential of DiGAs to improve patient care (92%) and their actual usage (32% had previously prescribed a DiGA). A substantial proportion of respondents, particularly those working in hospitals, reported either never or rarely prescribing DiGAs. Several factors are likely to contribute to this low prescription rate with insufficient knowledge, limited trust in the efficacy of DiGAs, and concerns about patient adherence emerging as the primary barriers to adoption.
The observed prescription rate of 31% was lower than in a previous study of general physicians [20], the physician group with the highest prescription rate, followed by orthopaedic surgeons [21]. The lower prescription rate in this study is in line with the results of another survey study among rheumatologists [13]. The observed prescription rate here was 7%, however this study was already published in 2022. This difference may be due to the fact that specialists in secondary care may not consider themselves responsible for treating all conditions in increasingly multimorbid patients. In addition, the availability of DiGAs is currently limited to certain indications, meaning that some specialists may not have access to relevant DiGAs for their primary disease spectrum. Another factor is that many of the physicians in our study worked in hospitals, dealing primarily with inpatients. While DiGA prescriptions are predominantly used in outpatient settings, it is also possible for inpatients. However, the lack of interoperability between hospital software systems significantly hampers the adoption of DiGAs in inpatient care [22].
While physicians were generally positive about the increasing digitalization of medicine, they also expressed concerns about a potential increase in their workload. Lack of time and the high workload were identified as major organizational barriers to adoption [12]. Several other key barriers to widespread implementation of DiGAs were reported, including lack of knowledge, complexity of the prescription process, reimbursement issues and concerns about patient adherence. These findings highlight the urgent need for comprehensive training and education programs to address the knowledge gaps and improve familiarity with digital health tools.
A recent comprehensive mixed-methods study, which included a literature review, supports these findings by identifying low familiarity with digital health solutions as the most commonly cited social barrier, followed by a general lack of awareness [12]. In our survey, a strong majority (88%) of physicians expressed interest in receiving specific digital health training. As previous studies has shown [12], such training is a critical step in overcoming the knowledge gaps identified as the main barrier to DiGA adoption. The development of comprehensive training programs that equip physicians with the necessary knowledge and skills to effectively integrate DiGAs into their practice should be a priority. These training initiatives could be delivered through various formats, such as workshops, online courses, and hands-on training sessions. Professional societies and health care institutions can play a key role in designing and implementing these educational programs, although current efforts remain underutilised [13].
Although this study provides valuable insights, it is important to acknowledge its limitations. As a small cross-sectional study conducted at a single medical conference, the results may not be fully representative of the broader physician population. Additionally, the self-reported nature of the data is also subject to potential bias, and the sample may have been affected by a selection bias, as it is not clear how many physicians declined to participate. Although the conference was specifically dedicated to internal medicine, 15% of the participating physicians were from other specialties. Furthermore, the majority of participants were consultants, representing a narrower subset of the overall physician population. Although the age range of participants was diverse, the mean age was significantly lower than the average age of practicing physicians [23], potentially leading to an overestimation of digital health adoption and affinity [24]. Overall the majority of physicians did however not yet prescribe a DiGA. Future research should aim to validate these findings in larger, more diverse samples and explore the impact of specific interventions such as educational programs, on DiGA adoption rates. Qualitative studies could also provide deeper insights into the specific needs and concerns of different physician subgroups, such as hospital-based versus private practice. Understanding these nuances can inform the development of more targeted support and education programs.
Conclusion
This survey highlights the implementation gap of DiGAs among German internal medicine physicians. While there is strong confidence in the ability of DiGAs to improve patient care, only one third of respondents had prescribed them. A main barrier appeared to be a lack of knowledge - a challenge that could be effectively addressed through targeted educational programs, which were widely welcomed by internal medicine physicians. This result in in line with a 2024 study where DiGA prescibers were interviewed [25]. This qualitative study also highlighted lack of time and physician reimbursement as major implementation barriers. Addressing these knowledge gaps through comprehensive education is essential to accelerate the adoption of digital health tools in clinical practice [14].
Supplementary Information
Acknowledgements
We thank all the participants for their support of this study.
Authors’ contributions
LC and JK recruited the participants, analysed, and interpreted the data, and were primarily responsible for writing the manuscript and incorporating feedback from co- authors. FL, NS, JL, FM, IG, MH and SK were involved in the conceptualisation and design of the study, the development of the methodology, and contributed to the writing of the final manuscript, as well as provided supervision and mentorship. JK was responsible for the original idea and overall study design. All authors have reviewed and approved the manuscript.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Open Access funding enabled and organized by Projekt DEAL.
Data availability
The raw data analysed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The Philipps-University Marburg Research Ethics Committee confirmed that no ethical approval was required (24-34 ANZ) for this anonymous survey study. Informed consent was obtained from all participants prior to the start of the study.
Consent for publication
Not required.
Competing interests
JK declares research support from Abbvie, Vila Health, honoraria and consulting fees from Abbvie, AstraZeneca, BMS, Boehringer Ingelheim, Chugai, GAIA, Galapagos, GSK, Janssen, Lilly, Medac, Novartis, Pfizer, Sobi, Rheumaakademie, UCB, Vila Health and Werfen. The remaining authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bundesministerium für Gesundheit, editors. Act to Improve Healthcare Provision through Digitalisation and Innovation (Digital Healthcare Act - DVG). https://www.bundesgesundheitsministerium.de/en/digital-healthcare-act.html. Accessed 27 Sep 2024.
- 2.Bundesministerium für Gesundheit, editors. Digitale-Gesundheitsanwendungen-Verordnung (DiGAV). https://www.bundesgesundheitsministerium.de/service/gesetze-und-verordnungen/detail/digitale-gesundheitsanwendungen-verordnung-digav.html. Accessed 27 Sep 2024.
- 3.Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM), editors. DiGA-Verzeichnis. https://diga.bfarm.de/de/verzeichnis. Accessed 27 Sep 2024.
- 4.Schramm L, Carbon C-C. Critical success factors for creating sustainable digital health applications: a systematic review of the German case. Digit Health. 2024;10:20552076241249604. 10.1177/20552076241249604. [DOI] [PMC free article] [PubMed]
- 5.Sauermann S, Herzberg J, Burkert S, Habetha S. DiGA - A Chance for the German Healthcare System. J Eur CME. 2022;11(1):2014047. 10.1080/21614083.2021.2014047. [DOI] [PMC free article] [PubMed]
- 6.Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, Hinder S, Fahy N, Procter R, Shaw S. Beyond Adoption: A New Framework for Theorizing and Evaluating Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies. J Med Internet Re. 2017;19(11):367. 10.2196/jmir.8775. [DOI] [PMC free article] [PubMed]
- 7.Kessel R, Roman-Urrestarazu A, Anderson M, Kyriopoulos I, Field S, Monti G, Reed SD, Pavlova M, Wharton G, Mossialos E. Mapping Factors That Affect the Uptake of Digital Therapeutics Within Health Systems: Scoping Review. J Med Internet Res. 2023;25:48000. 10.2196/48000. [DOI] [PMC free article] [PubMed]
- 8.Kernder A, Morf H, Klemm P, Vossen D, Haase I, Mucke J, Meyer M, Kleyer A, Sewerin P, Bendzuck G, Eis S, Knitza J, Krusche M. Digital rheumatology in the era of COVID-19: results of a national patient and physician survey. RMD Open. 2021;7(1). 10.1136/rmdopen-2020-001548https://rmdopen.bmj.com/content/7/1/e001548.full.pdf. [DOI] [PMC free article] [PubMed]
- 9.Knitza J, Simon D, Lambrecht A, Raab C, Tascilar K, Hagen M, Kleyer A, Bayat S, Derungs A, Amft O, Schett G, Hueber AJ. Mobile Health Usage, Preferences, Barriers, and eHealth Literacy in Rheumatology: Patient Survey Study. JMIR Mhealth Uhealth. 2020;8(8):19661 10.2196/19661. [DOI] [PMC free article] [PubMed]
- 10.Uncovska M, Freitag B, Meister S, Fehring L. Patient Acceptance of Prescribed and Fully Reimbursed mHealth Apps in Germany: An UTAUT2-based Online Survey Study. J Med Syst. 2023;47(1):14. 10.1007/s10916-023-01910-x. [DOI] [PMC free article] [PubMed]
- 11.Busch-Casler J, Radic M. Trust and Health Information Exchanges: Qualitative Analysis of the Intent to Share Personal Health Information. J Med Internet Res. 2023;25:41635. 10.2196/41635. [DOI] [PMC free article] [PubMed]
- 12.Weik L, Fehring L, Mortsiefer A, Meister S. Understanding inherent influencing factors to digital health adoption in general practices through a mixed-methods analysis. NPJ Digit Med. 2024;7(1):47. 10.1038/s41746-024-01049-0. [DOI] [PMC free article] [PubMed]
- 13.Richter JG, Chehab G, Stachwitz P, Hagen J, Larsen D, Knitza J, Schneider M, Voormann A, Specker C. One year of digital health applications (DiGA) in Germany - Rheumatologists’ perspectives. Front Med. 2022;9. 10.3389/fmed.2022.1000668. [DOI] [PMC free article] [PubMed]
- 14.Dahlhausen, F, Zinner M, Bieske L, Ehlers JP, Boehme P, Fehring L. Physicians’ attitudes toward prescribable mhealth apps and implications for adoption in germany: Mixed methods study. JMIR Mhealth Uhealth. 2021;9(11):33012. 10.2196/33012. [DOI] [PMC free article] [PubMed]
- 15.Deutsche Gesellschaft für Innere Medizin e.V. (DGIM), editors. Die DGIM - Wer sind wir? https://www.dgim.de/ueber-uns/#:~:text=Die%20Deutsche%20Gesellschaft%20f%C3%BCr%20Innere,medizinisch%2Dwissenschaftlichen%20Fachgesellschaften%20in%20Europa. Accessed 27 Sep 2024.
- 16.Eysenbach G. Improving the Quality of Web Surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):34. 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed]
- 17.Martin S, Phillips J, Robert L, Petterson S, Levin Z, Bazemore AW. Primary Care Spending in the United States, 2002-2016. JAMA Intern Med. 2020;180(7):1019–1020. 10.1001/jamainternmed.2020.1360. [DOI] [PMC free article] [PubMed]
- 18.Rozanski A, Blumenthal JA, Hinderliter AL, Cole S, Lavie CJ. Cardiology and lifestyle medicine. Prog Cardiovasc Dis. 2023;77:4–13. 10.1016/j.pcad.2023.04.004. [DOI] [PubMed]
- 19.Tarricone R, Petracca F, Weller H-M. Towards harmonizing assessment and reimbursement of digital medical devices in the EU through mutual learning. NPJ Digit Med. 2024;7(1):268. 10.1038/s41746-024-01263-w. [DOI] [PMC free article] [PubMed]
- 20.Brecher A-L, Herrgen J, Mueller T. DiGA diga in Primary Care and the Influence of Patient-Related Factors - Results of a Survey of Family Doctors. Stud Health Technol Inform. 2024;313:55–61. 10.3233/SHTI240012. [DOI] [PubMed]
- 21.GKV-Spitzenverband, editors. DiGA-Bericht des GKV-Spitzenverbandes. https://www.gkv-spitzenverband.de/krankenversicherung/digitalisierung/kv_diga/diga.jsp. Accessed 27 Sep 2024.
- 22.Schlieter H, Kählig M, Hickmann E, Fürstenau D, Sunyaev A, Richter P, Breitschwerdt R, Thielscher C, Gersch M, Maaß W, Reuter-Oppermann M, Wiese L. Digitale Gesundheitsanwendungen (DiGA) im Spannungsfeld von Fortschritt und Kritik. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2024;67(1):107–14. 10.1007/s00103-023-03804-2. [DOI] [PMC free article] [PubMed]
- 23.Young A, Chaudhry HJ, Pei X, Arnhart K, Dugan M, Simons KB. FSMB Census of Licensed Physicians in the United States, 2020. J Med Regul. 2021;107(2):57–64. 10.30770/2572-1852-107.2.57.
- 24.Estrela M, Semedo G, Roque F, Ferreira PL, Herdeiro MT. Sociodemographic determinants of digital health literacy: A systematic review and meta-analysis. Int J Med Inform. 2023;177:105124. 10.1016/j.ijmedinf.2023.105124. [DOI] [PubMed]
- 25.Boy K, May S, Labinsky H, Morf H, Heinze M, Leipe J, Kuhn S, Schett G, Knitza J, Muehlensiepen, F. Back on track – digital health applications to treat back pain of rheumatic patients? Results of a qualitative interview study. Rheumatol Int. 2024. 10.1007/s00296-024-05726-x. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data analysed during the current study are available from the corresponding author upon reasonable request.