Abstract
Background:
The mucogingival conditions associated with the recession defects at the mandibular anterior region, not only make plaque control difficult to be performed by the patient but also pose a problem in passively advancing the tissues at the recipient site. This surgical technique is used to treat multiple recession defects in the mandibular anterior region.
Materials and Methods:
Twenty-five sites in 17 subjects (11 women and 6 men) underwent modified bridge flap and de-epithelized gingival unit graft (d-GUG) as a single-step treatment modality to cover the denuded root surface, as well as increase the width of keratinized gingiva in recession type 1 gingival recession defects in the mandibular anterior region.
Results:
Nearly 60% of sites in our study showed complete root coverage, with a mean root coverage percentage of 88.08%. Furthermore, keratinized tissue width, keratinized tissue thickness as well as vestibular depth showed statistically significant increases as compared to baseline levels.
Conclusion:
Thus, the modified bridge flap technique using d-GUG within the limitations of our study design, showed promising results in terms of recession coverage as well as management of the difficult mucogingival conditions at the mandibular anterior region.
Keywords: Gingival recession, periodontal surgery, soft-tissue grafts
Introduction
Gingival recession, leading to denudation of the root surface, is not only an esthetic concern, but also disturbs the functional integrity due to the loss of protective keratinized gingiva. The recession defects of the lower jaw are usually associated with poor mucogingival conditions such as thin gingival biotype, active frenal pull, shallow vestibule, or inadequate keratinized gingiva[1,2] which may require more than one surgical procedure to completely and predictably cover the recession defect.
The coronally advanced flap (CAF) with subepithelial connective tissue graft (SECTG) remains the gold standard for covering the denuded root surface.[3] The modifications of CAF and minimally invasive root coverage techniques such as vestibular incision subperiosteal tunnel access[4] signify a marked evolution in root coverage procedures. The recipient site considerations of all the recent advances aim at preserving and rapidly re-establishing the blood supply for a better postoperative tissue viability.
SECTG presents with certain limitations such as insufficient donor tissue where there is inadequate thickness of palatal mucosa.[5,6] To overcome this limitation and to obtain a firmer, collagen-rich connective tissue, the use of de-epithelialized connective tissue grafts (CTGs) has been proposed.[7] These grafts obtained by de-epithelializing the free gingival grafts (FGG) are also less prone to postoperative shrinkage.[8] Gingival unit grafts (GUGs), a modification of FGG, include marginal and interdental gingiva along with palatal mucosa. First proposed by Allen in 2004,[9] GUG is considered a site-specific and “pre-contoured” graft, with increased ease of adaptation and suturing onto the root surface.[10] De-epithelialization of GUG provides a more “customized” collagen-rich connective tissue which follows the gingival scallop as well as fits into the interdental spaces.[11]
The mucogingival conditions associated with the recession defects at the mandibular anterior region, not only make plaque control difficult to be performed by the patient but also pose a problem in passively advancing the tissues at the recipient site. The newer techniques still have limited evidence to demonstrate their efficacy in treating multiple anatomic factors in the mandibular anterior region.[12,13] A new surgical technique has been proposed by the authors to address this problem.
This technique utilizes de-epithelized GUG (d-GUG) and a modified bridge flap procedure. The original lateral sliding bridge flap proposed by Marggraf[14] utilizes a semilunar incision in the vestibular fornix connected to intrasulcular incisions around the teeth by supraperiosteal dissection. The original technique also involves splitting of the papillae to enable coronal positioning of the entire “bridge.” The modification proposed in the present investigation avoids splitting of papillae to preserve the blood supply and coronal positioning is obtained by tooth anchoring sutures. Hence, the aim of the present study is to assess the efficacy of modified bridge flap and d-GUG as a single-step treatment modality to cover the denuded root surface, as well as increase the width of keratinized gingiva in recession type 1 (RT1) gingival recession defects. The secondary parameters assessed were the thickness of the gingiva and the depth of the vestibule.
Materials and Methods
Twenty-five sites in 17 subjects (11 women and 6 men) and 18–35 years (mean age: 30.6 ± 1.2 years) were included in the present study. The Institutional Ethics Committee reviewed and approved the study protocol. The study was conducted as per the Declaration of Helsinki of 1975, revised in 2013 and was registered with the Clinical Trials Registry of India (CTRI/2021/09/036599). The subjects willing to participate in the study signed a written informed consent. The subjects were selected from a pool of patients referred to the Department of Periodontics for recession coverage using CTG, based on the following inclusion and exclusion criteria.
Inclusion criteria
(1) Single/multiple (not more than 3) adjacent RT1 recession defects, associated with the presence of anatomic factors such as shallow vestibule/inadequate keratinized gingiva or aberrant frenum which might impair passive coronal positioning of the flap. (2) Non-smoker and nontobacco user subjects maintained good oral hygiene throughout the duration of the study period.
Exclusion criteria
(1) Prominent root surface which might require orthodontic correction before root coverage procedure, (2) presence of noncarious cervical lesions or root caries, (3) pregnant patients, and (4) patients with systemic conditions or using drugs which may be contraindication for periodontal surgery or may impair wound healing.
Phase I therapy
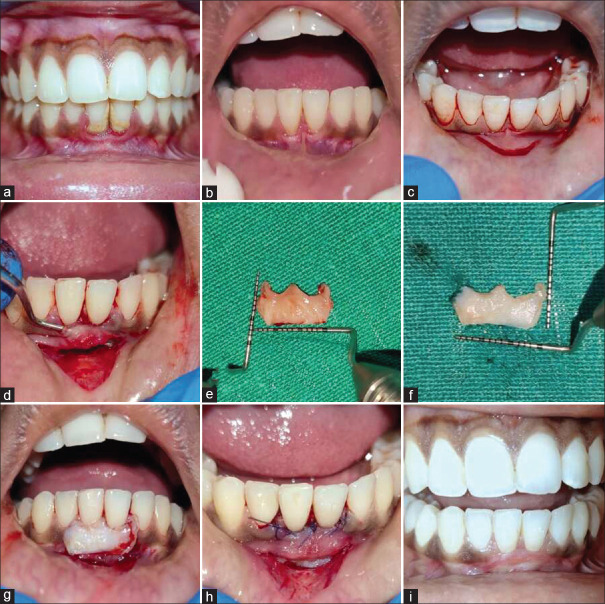
The selected patients underwent a session of scaling and root planning [Figure 1a] and were instructed on oral hygiene maintenance, where a change of brushing technique to modified bass method of toothbrushing was stressed upon. After 4 weeks [Figure 1b], the oral hygiene was monitored using plaque index (PI) and gingival index (GI)[15] and when the indices were below 20%, the patients were enrolled for the surgical procedure.
Figure 1.
(a) Case 1: Clinical photograph before Phase-1 therapy showing gingival recession in tooth number 31, 41 (b) after Phase 1 therapy showing gingival recession in tooth number 31, 41 (c) recipient site preparation-incision outline (d) elevation of the modified bridge flap (e) Harvested gingival unit graft from palate (f) de-epithelized gingival unit graft (g) graft placed at the recipient site (h) Graft sutured at recipient site (i) six months post-operative clinical photograph of recipient site of Case 1
Clinical measurements
All the measurements were performed by a single examiner, measured at the midbuccal level of the tooth, using a periodontal probe (UNC 15, Hu-Friedy) and rounded to the nearest 0.5 mm. Customized acrylic stents for each patient, with grooves corresponding to midbuccal surface of defect/s were made to ensure accurate readings. The following clinical parameters were measured before surgery (baseline), 3 months, and 6 months postoperative period: recession depth (RD) – the distance between CEJ and most apical portion of the gingival margin, recession width (RW) – width of recession defect at the level of CEJ, probing depth (PD) – distance from the gingival margin to bottom of the gingival sulcus, clinical attachment level (CAL) – sum of RD and PD, width of keratinized tissue (KTW) – the lower lip was stretched to demarcate the mucogingival junction and the distance from the gingival margin to the mucogingival junction was measured, vestibular depth (VD) – distance between the gingival margin to the concavity of mucobuccal fold at the depth of vestibule and thickness of keratinized tissue (KTT) – determined at a distance of 1.5 mm apical to gingival margin using short anesthesia needle and rubber disc stopper.[5] GI and PI were scored 4 weeks after the Phase I therapy (baseline) and 6 months post-surgery.
Surgical procedure
The surgical procedure was performed by a single experienced clinician.
Preparation of recipient site
After administering adequate local infiltration anesthesia (2% lignocaine hydrochloride with 1:100,000 epinephrine), the recipient site was outlined using a semilunar incision covering one tooth on either side of the recession defect/s on the alveolar and/or labial mucosa at a distance of 10–15 mm from the gingival margin [Figure 1c]. The distance between the incision and gingival margin of the affected tooth/teeth was based on the initial RD and the amount of VD present. This allowed sufficient mobility and vascularity of the flap to cover the recession defect as well as ensured adequate perfusion of the graft beneath. The second incision was an intrasulcular incision extending to one tooth on either side of the affected area without splitting the interdental papillae. A supraperiosteal partial thickness dissection was done through the sulcular incision till it connected with the vestibular incision [Figure 1d]. In areas where the tissue thickness did not permit a partial thickness dissection, full thickness elevation was performed. The papillae in the surgical area were gently undermined using microsurgical blade. A completely prepared recipient area allowed tension-free flap mobilization to cover the recession defect. Care was taken to keep the continuity of the papillae as well as the flap intact to ensure maximum blood supply to the graft.
Preparation of donor site
The palatal premolar region was anesthetized. The required length and width of the graft were measured using a periodontal probe and bleeding points were marked at the donor area. A no. 15 C Bard Parker (BP) blade was used to trace the outline of the graft to a depth of approximately 1.5–2 mm. The papillae were first reflected; the gingival margin carefully detached and the outlined graft was thus harvested using BP blade no. 15 C [Figure 1e]. Once harvested, the graft was de-epithelized using new no. 15 C blade and the undersurface of the graft were trimmed to remove any loose tissue tags or adipose tissue [Figure 1f]. Hemostasis was achieved at the donor site using saline-soaked gauze pressed for 5 min and was covered using a customized acrylic stent.
Securing of the graft
The prepared graft was inserted beneath the partial thickness recipient site [Figures 1g and 2a and b], and the flap was mobilized coronally to cover the graft and recession defect, secured using sling suture engaging both the graft and overlying flap [Figure 1h]. Additional sutures without engaging the graft were also done such as horizontal adapting sutures [Figure 3c] and/or tooth anchoring sutures [Figure 4c] as and when required. The area was covered using a periodontal pack.
Figure 2.
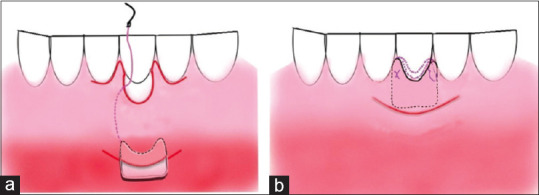
(a) Schematic diagram showing insertion of the de-epithelized gingival unit graft through the vestibular incision (b) schematic diagram showing suturing of the graft to the recipient site
Figure 3.
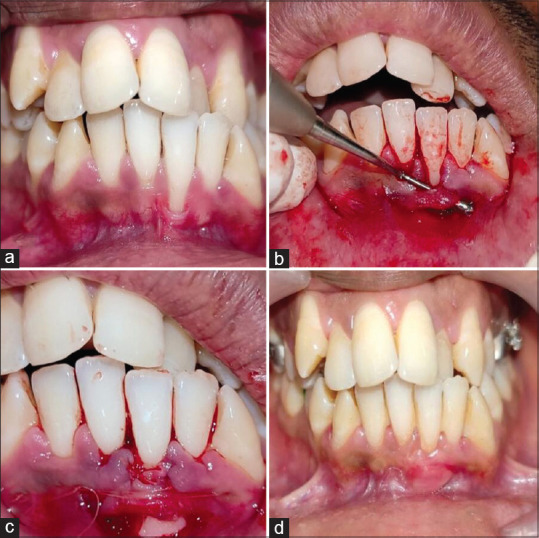
(a) Case 2: Clinical photograph showing gingival recession in tooth number 31 (b) elevation of modified bridge flap (c) graft sutured at recipient site with additional horizontal adapting sutures (d) six months postoperative clinical photograph of recipient site of case 2
Figure 4.

(a) Case 3: Clinical photograph showing gingival recession in tooth number 31, 32, 41 (b) elevation of modified bridge flap (c) graft sutured at recipient site along with tooth anchoring sutures (d) six months post-operative clinical photograph of recipient site of case 3
Postoperative maintenance
Patients were advised analgesics and antibiotics for 5 days. Chlorhexidine 0.2% rinse was advised for 2 weeks. The modified bass technique of toothbrushing was advised in all areas of the mouth except the surgical site. Sutures were removed after 2 weeks. Normal oral hygiene measures resumed after 4 weeks. The patient was recalled every 2 weeks postsuture removal for the initial 2 months and every month till 6 months postoperative [Figure 1i].
Statistical analysis
The data were collected and entered in Microsoft Excel version 2007 (Windows) and imported to SPSS version 27 Armonk, New York, USA (IBM corporation) for further analysis. All the continuous variables were expressed in terms of mean and standard deviation. The distribution of continuous variables was assessed using the Shapiro–Wilks test, and statistical tests were used based on the normality criteria. Comparison of means through time within the group was measured using the Freidman test since all the continuous variables had skewed distribution. Pairwise comparison was also conducted. P <0.05 was considered statistically significant.
Results
Table 1 summarizes the comparison of different parameters at baseline; 3-month and 6-month follow-up. The three representative cases with their 6-month follow-up clinical photographs are depicted in Figures 1a-1i, 3a-3d and 4a-4d. Twenty-five recession defects in 17 patients were treated and analyzed for effectiveness of the novel surgical technique. All the patients completed the 6-month follow-up with uneventful healing both at recipient [Figures 1i, 3d and 4d] and donor site [Figure 5]. RD and RW showed a statistically significant improvement when compared to baseline both at 3 and 6 months (P < 0.001). The reduction in RD was associated with concomitant gain in CALs and an increase in KTW at 3 and 6 months (P < 0.001). There was a statistically significant reduction in PD measurements from baseline to 6-month period (P = 0.001). The VD and KTT also showed a statistically significant increase when compared to baseline at 3-month and 6-month period (P < 0.001). The mean GI and PI scores did not show any significant change during the 6-month period.
Table 1.
Comparison of different parameters at baseline, 3 month- and 6-month follow-up
| Baseline | 3 months | 6 months | P | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Baseline versus 3 months | Baseline versus 6 months | 3 months versus 6 months | ||||
| RD (mm) | 3.24±0.83 | 0.72±0.45 | 0.40±0.50 | <0.001* | <0.001* | 0.774 |
| RW (mm) | 2.84±0.55 | 0.72±0.45 | 0.40±0.50 | <0.001* | <0.001* | 0.774 |
| CAL (mm) | 4.84±1.12 | 2.24±0.69 | 1.44±0.58 | <0.001* | <0.001* | 0.014* |
| KTW (mm) | 1.84±0.53 | 3.46±0.69 | 3.68±0.57 | <0.001* | <0.001* | 0.472 |
| PD (mm) | 1.60±0.54 | 1.36±0.39 | 1.04±0.20 | 0.231 | 0.001* | 0.143 |
| VD (mm) | 4.02±0.82 | 7.56±1.07 | 7.76±1.38 | <0.001* | <0.001* | 0.999 |
| Gingival thickness (mm) | 0.68±0.24 | 1.48±0.30 | 1.56±0.33 | <0.001* | <0.001* | 0.999 |
| GI (mm) | 0.63±0.18 | 0.51±0.21 | 0.024 | |||
| PI | 0.63±0.18 | 0.59±0.21 | 0.396 | |||
*P≤0.05 is statistically significant. SD: Standard deviation; RD: Recession depth; RW: Recession width; CAL: Clinical attachment level; KTW: Keratinized tissue width; PD: Probing depth; VD: Vestibular depth; GI: Gingival index; PI: Plaque index
Figure 5.

(a) Outline of the graft at the donor site (b) donor site healing at 2 weeks (c) donor site healing at 2 months
Discussion
Optimization of blood supply to the graft by minimally invasive recipient site preparation forms the basis for all the surgical procedures involving coronal positioning of flap/tunnel. The most predictable outcome for covering the denuded roots has been achieved using CAF with CTG. The predictability originates from its ability to maintain a bilaminar blood supply, thus increasing the chances of flap and/or graft survival on the avascular bed.
The surgical technique proposed in the present study is a modification of the lateral bridging flap technique first proposed by Marggraff[14] The lateral bridging flap technique was proposed as a single surgical step to cover gingival recession, without any requirement for prior augmentation of attached gingiva. The modification proposed by the authors in the present study was to undermine the papillae without splitting the interdental tissues to create a space for the graft. A similar modification of the lateral bridging technique was proposed by Bethaz et al.,[16] where the authors used a vestibular incision, supraperiosteal separation along with undermining of interdental papilla without splitting the interdental tissues. They, however, used a SECTG and stabilized the recipient site using sling suspended sutures and horizontal mattress sutures anchored to the periosteum.
In any root coverage surgical procedure, tension-free coronal mobilization of soft tissues plays a pivotal role in achieving CRC.[17] Use of CTG under a CAF reduces the apical shift of the gingival margin in comparison to CAF alone.[18] In the present study, the semilunar vestibular incision enabled the recipient site to be displaced tension free even in difficult areas of mandibular anteriors where there is often the presence of inadequate VD and other mucogingival problems. The use of interdental sling sutures and tooth anchoring sutures apart from being less technique sensitive (compared to periosteal sutures used by Bethaz et al.),[16] helped in stabilizing the coronally displaced tissues throughout the healing period. 60% of sites in our study showed CRC as compared to 73.3% of sites in the previous study using similar modifications. Higher sample size and lesser follow-up period in the present study may be attributed to the difference in the number of sites showing CRC.
Retention of periosteum on the recipient bed ensures rapid revascularization,[19] but an attempt to elevate the partial thickness envelope in areas with thin friable gingiva may lead to necrosis.[20] In the present study, though few sites with thin gingiva were reflected subperiosteally, the intact papillary blood supply and absence of any vertical incisions at the site helped in the optimization of blood supply to the recipient area. The greater area of contact of the graft with the recipient bed increases the predictability of root coverage. In addition to the provision of a larger area for graft attachment, the use of marginal gingiva and interdental papilla in the GUG which resembles the vascular configuration of the recipient site both in size and number leads to rapid revascularization of the graft.[9,21] Although GUG recipient sites demonstrate improved outcomes, harvesting of GUG carries a risk of denudation of roots followed by exposure of underlying bone. Harvesting of GUG by performing superficial beveled incisions without exposing the underlying bone does not result in any undesirable recession at the donor sites as reported by numerous clinical trials.[9,21,22,23] Harvesting of GUG by performing superficial beveled incisions without exposing the underlying bone does not result in any undesirable recession at the donor sites as reported by numerous clinical trials. The healing was uneventful in both donor and recipient sites.
The mean percentage of root coverage (MRC) obtained using the novel technique was 88.08%, which was comparable to the MRC obtained by Bethaz et al.[16] (90.6% ±16.8%) with a concomitant increase in KTW of 3.68 ± 0.57. The ratio of graft tissue area and visible denuded area is a significant factor for optimal root coverage.[24] The use of d-GUG increases the graft tissue area and allows more contact of the graft with the vascular bed, thus increasing the chances of graft survival and subsequently better root coverage. Harvesting of GUG requires superficial beveled incisions at the palatal marginal and interdental papillae regions, which makes the technique easy and less invasive to be used even in the presence of a thin palatal fibromucosa. Thus, the difference in de-epithelialized FGG and GUG may become more significant when treating areas with wide or multiple recession defects.
The mean PI and GI scores remained unchanged from baseline to 6 months indicating that the increased KTW and VD levels allowed oral hygiene maintenance on the part of the patient throughout the study period.
CAF, as a surgical procedure, in areas with shallow vestibule results in thicker, though still movable mucosal tissue and inadequate VD although root coverage may have been achieved.[25] FGG traditionally has been used to address the mucogingival problems of the mandibular anterior region, either as a single-step or two-step procedures.[25] FGG, as procedure, also carries with it a few limitations of being less esthetic[26] and low predictability when used for root coverage purpose.[27] In our study, along with KTW, an increase in VD and the KTT improvement at the end of 6 months was statistically significant when compared to the baseline values. The ability to treat multiple mucogingival problems in multiple teeth with a single-step procedure resulting in acceptable esthetics displays the versatility of the technique.
Out of 25 treated sites, 8 sites showed an apical scar formation, corresponding to the site of vestibular incision. A similar finding was also reported by the authors in a previous study when using a similar technique. However, the possible benefits far outweigh the concerns about the tissue appearance of the mandibular vestibule area, which is not visible during smile.
Conclusion
This surgical intervention using a modified bridge flap with d-GUG, within the limitations of our study design, showed promising results in terms of recession coverage as well as management of the difficult mucogingival conditions at the mandibular anterior region. Further studies with a control group and followed up for a longer time period will provide additional insights to better understand the untested aspects of the given surgical procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zucchelli G, Cesari C, Amore C, Montebugnoli L, De Sanctis M. Laterally moved, coronally advanced flap: A modified surgical approach for isolated recession-type defects. J Periodontol. 2004;75:1734–41. doi: 10.1902/jop.2004.75.12.1734. [DOI] [PubMed] [Google Scholar]
- 2.Cortellini P, Tonetti M, Prato GP. The partly epithelialized free gingival graft (pe-FGG) at lower incisors. A pilot study with implications for alignment of the mucogingival junction. J Clin Periodontol. 2012;39:674–80. doi: 10.1111/j.1600-051X.2012.01896.x. [DOI] [PubMed] [Google Scholar]
- 3.Chambrone L, Salinas Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, et al. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev. 2018;10:CD007161. doi: 10.1002/14651858.CD007161.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31:653–60. [PubMed] [Google Scholar]
- 5.Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, et al. Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: A comparative randomized-controlled clinical trial. J Clin Periodontol. 2010;37:728–38. doi: 10.1111/j.1600-051X.2010.01550.x. [DOI] [PubMed] [Google Scholar]
- 6.Harris RJ. A comparison of two techniques for obtaining a connective tissue graft from the palate. Int J Periodontics Restorative Dent. 1997;17:260–71. [PubMed] [Google Scholar]
- 7.Bosco AF, Bosco JM. An alternative technique to the harvesting of a connective tissue graft from a thin palate: Enhanced wound healing. Int J Periodontics Restorative Dent. 2007;27:133–9. [PubMed] [Google Scholar]
- 8.Azar EL, Rojas MA, Patricia M, Carranza N. Histologic and histomorphometric analyses of de-epithelialized free gingival graft in humans. Int J Periodontics Restorative Dent. 2019;39:221–6. doi: 10.11607/prd.3544. [DOI] [PubMed] [Google Scholar]
- 9.Allen AL. Use of the gingival unit transfer in soft tissue grafting: Report of three cases. Int J Periodontics Restorative Dent. 2004;24:165–75. [PubMed] [Google Scholar]
- 10.Katti N, Mohanty D, Agrawal P, Raj SC, Pradhan SS, Baral D. Successful management of gingival recession with interdental attachment loss using gingival unit grafts. J Indian Soc Periodontol. 2022;26:373–7. doi: 10.4103/jisp.jisp_539_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agrawal P, Katti N, Mohanty D, Pradhan SS, Raj SC, Satyarup D, et al. Treatment of localized gingival recession using gingival unit grafts: An 18-month follow-up study. J Contemp Dent Pract. 2022;23:49–55. [PubMed] [Google Scholar]
- 12.Agusto M, Salman A, Parker D, Choi D, Schincaglia GP. Root coverage predictability in the treatment of gingival recessions on mandibular anterior teeth. JDR Clin Trans Res. 2022;7:224–33. doi: 10.1177/23800844211009437. [DOI] [PubMed] [Google Scholar]
- 13.Rimbert M, Barré R. New surgical approach for mandibular anterior root coverage by modified tunnel technique with simultaneous frenuloplasty: Technical description and 5-year recall case report. Clin Adv Periodontics. 2021;11:155–60. doi: 10.1002/cap.10163. [DOI] [PubMed] [Google Scholar]
- 14.Marggraf E. A direct technique with a double lateral bridging flap for coverage of denuded root surface and gingiva extension. Clinical evaluation after 2 years. J Clin Periodontol. 1985;12:69–76. doi: 10.1111/j.1600-051x.1985.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 15.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38:l610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 16.Bethaz N, Romano F, Ferrarotti F, Mariani GM, Aimetti M. A mucogingival technique for the treatment of multiple recession defects in the mandibular anterior region: A case series with a 2-year follow-up. Int J Periodontics Restorative Dent. 2014;34:345–52. doi: 10.11607/prd.1920. [DOI] [PubMed] [Google Scholar]
- 17.Pini Prato G, Pagliaro U, Baldi C, Nieri M, Saletta D, Cairo F, et al. Coronally advanced flap procedure for root coverage. Flap with tension versus flap without tension: A randomized controlled clinical study. J Periodontol. 2000;71:188–201. doi: 10.1902/jop.2000.71.2.188. [DOI] [PubMed] [Google Scholar]
- 18.Cortellini P, Tonetti M, Baldi C, Francetti L, Rasperini G, Rotundo R, et al. Does placement of a connective tissue graft improve the outcomes of coronally advanced flap for coverage of single gingival recessions in upper anterior teeth?A multi-centre, randomized, double-blind, clinical trial. J Clin Periodontol. 2009;36:68–79. doi: 10.1111/j.1600-051X.2008.01346.x. [DOI] [PubMed] [Google Scholar]
- 19.Nelson SW. The subpedicle connective tissue graft. A bilaminar reconstructive procedure for the coverage of denuded root surfaces. J Periodontol. 1987;58:95–102. doi: 10.1902/jop.1987.58.2.95. [DOI] [PubMed] [Google Scholar]
- 20.Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994;14:216–27. [PubMed] [Google Scholar]
- 21.Kuru B, Yıldırım S. Treatment of localized gingival recessions using gingival unit grafts: A randomized controlled clinical trial. J Periodontol. 2013;84:41–50. doi: 10.1902/jop.2012.110685. [DOI] [PubMed] [Google Scholar]
- 22.Jenabian N, Bahabadi MY, Bijani A, Rad MR. Gingival unit graft versus free gingival graft for treatment of gingival recession: A randomized controlled clinical trial. J Dent (Tehran) 2016;13:184–92. [PMC free article] [PubMed] [Google Scholar]
- 23.Sriwil M, Fakher MA, Hasan K, Kasem T, Shwaiki T, Wassouf G. Comparison of free gingival graft and gingival unit graft for treatment of gingival recession: A randomized controlled trial. Int J Periodontics Restorative Dent. 2020;40:e103–10. doi: 10.11607/prd.4180. [DOI] [PubMed] [Google Scholar]
- 24.Yotnuengnit P, Promsudthi A, Teparat T, Laohapand P, Yuwaprecha W. Relative connective tissue graft size affects root coverage treatment outcome in the envelope procedure. J Periodontol. 2004;75:886–92. doi: 10.1902/jop.2004.75.6.886. [DOI] [PubMed] [Google Scholar]
- 25.Camargo PM, Melnick PR, Kenney EB. The use of free gingival grafts for aesthetic purposes. Periodontol 2000. 2001;27:72–96. doi: 10.1034/j.1600-0757.2001.027001072.x. [DOI] [PubMed] [Google Scholar]
- 26.Kerner S, Sarfati A, Katsahian S, Jaumet V, Micheau C, Mora F, et al. Qualitative cosmetic evaluation after root-coverage procedures. J Periodontol. 2009;80:41–7. doi: 10.1902/jop.2009.080413. [DOI] [PubMed] [Google Scholar]
- 27.Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: A systematic review. J Clin Periodontol. 2002;29(Suppl 3):178–94. doi: 10.1034/j.1600-051x.29.s3.11.x. [DOI] [PubMed] [Google Scholar]