Abstract
Background/Aims
The trends in mortality of hepatocellular carcinoma (HCC) and biliary tract cancers stratified by sex and race/ethnicity in the US continue to evolve. We estimated the sex- and race/ethnicity-based trends in HCC and biliary tract cancers-related mortality in US adults with a focus on disease burden.
Methods
We performed a population-based analysis using the US national mortality records from 2018 to 2023. We identified HCC and biliary tract cancer using appropriate ICD-10 codes. Temporal trends in mortality were calculated by joinpoint analysis with annual percentage change (APC).
Results
Annual age-standardized mortality from HCC decreased steadily with an APC of –1.4% (95% confidence interval [CI] –2.0% to –0.7%). While there was a linear increase in intrahepatic cholangiocarcinoma-related mortality (APC 3.1%; 95% CI 1.2–4.9%) and ampulla of Vater cancer-related mortality (APC 4.1%, 95% CI 0.5–7.9%), gallbladder cancer-related mortality decreased (APC –1.9%; 95% CI –3.8% to –0.0%). Decreasing trends in mortality from HCC were noted in males, not females. HCC-related mortality decreased more steeply in racial and ethnic minority individuals compared with non-Hispanic White individuals. Racial and ethnic differences in trends in mortality for biliary tract cancers depended on the malignancy’s anatomical site.
Conclusions
While the annual mortality for HCC and gallbladder cancer demonstrated declining trends, ICC- and AVC-related mortality continued to increase from 2018 to 2023. Although racial and ethnic minority individuals in the US experienced disproportionately higher HCC and biliary tract cancer, recent declines in HCC may be primarily due to declines among racial and ethnic minority individuals and males.
Keywords: Liver cancer, Cholangiocarcinoma, Gallbladder cancer, NVSS, Death
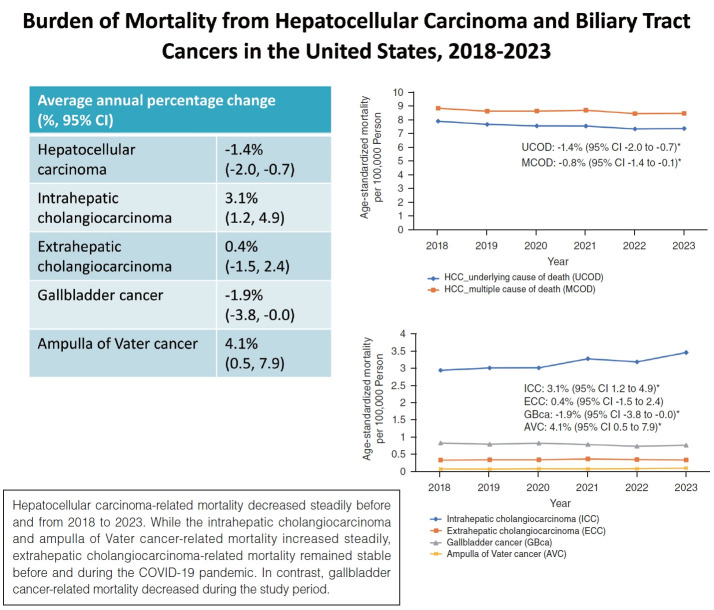
Graphical Abstract
INTRODUCTION
Hepatobiliary cancers, which include hepatocellular carcinoma (HCC) and biliary tract cancers, are associated with significant morbidity and mortality worldwide. Based on data published in the Global Cancer Statistics 2020 report, liver cancer is the sixth most prevalent cancer, with the third highest mortality rate [1]. While liver and intrahepatic bile duct cancers are not among the top 10 leading causes of new cancer cases in the United States (US) in 2024, it made the cut-off for the top 5 leading estimated cancer-related deaths in males and the top 7 estimated cancer-related deaths in females [2]. The incidence of liver and intrahepatic bile duct cancer has stabilized in males, while rates continue to increase in females by about 2% annually [2]. Age-standardized mortality from HCC increased from 4.14 per 100,000 individuals in 2009 to 4.90 per 100,000 individuals in 2018, with an average increase of annual percent change (APC) of 1.9% in the US [3]. Biliary tract cancers, which include intrahepatic cholangiocarcinoma (ICC), extrahepatic cholangiocarcinoma (ECC), gallbladder cancer, and ampulla of Vater cancer (AVC), as a group, have a significantly lower prevalence than HCC, but have a much higher fatality, presumably associated with late diagnosis at an advanced stage [4,5]. A recent study showed that there was a linear increase in mortality from ICC, but gallbladder cancer-related mortality steadily decreased during the same period between 2009 and 2017 in the US [6]. However, there was a lack of up-to-date trends in mortality from HCC and biliary tract cancers before and during the coronavirus disease 2019 (COVID-19) pandemic (2018–2023). In addition, recent reports up to 2018 have demonstrated a concerning higher mortality and steeper increasing trend in the mortality of HCC and biliary tract cancers among racial and ethnic minority individuals in the US [6,7]. Furthermore, the impact of the COVID-19 pandemic on HCC and biliary tract cancers-related mortality stratified by race and ethnicity and sex remains unknown. Therefore, there was an unmet need to investigate whether the change in mortality rates and trends in mortality due to HCC and biliary tract cancers among racial and ethnic minority individuals was noted before and during the COVID-19 pandemic.
The deleterious effects of COVID-19 pandemic-related resource reallocation may have been more pronounced in vulnerable racial and ethnic minority patients with cancer, resulting in an increase in all-cause mortality [8]. During the early phase of the COVID-19 pandemic, the management of COVID-19 was prioritized, which might have undermined the care of patients with HCC and biliary tract cancers. The inability to visit outpatient clinics for evaluation of early symptoms, diagnosis, and treatment as a result of social isolation or lockdowns may have negatively impacted the mortality trends in HCC and biliary tract cancers during the COVID-19 pandemic. Healthcare disruptions during the COVID-19 pandemic may have amplified the widening gaps in healthcare inequalities [9]. A recent study showed that non-COVID-19 excess deaths in the US during the COVID-19 pandemic were 2 to 4 times higher in non-Hispanic Black, non-Hispanic Asian, and Hispanic males and females compared with non-Hispanic White males and females [10]. Therefore, the burden of the COVID-19 pandemic on healthcare resources may have been detrimental and contributed to increasing the mortality associated with HCC and biliary tract cancers and further compounding the disparities in medical care across races and ethnicities. This study used the national mortality data from the National Vital Statistics System (NVSS) to calculate contemporary trends in HCC and biliary tract cancer-related mortality from 2018 to 2023 in the US. The aims of this study were (1) to investigate contemporary trends in mortality for HCC and biliary tract cancers and (2) to determine race and ethnicity- and sex-specific trends in mortality for HCC and biliary tract cancers.
MATERIALS AND METHODS
Study data
The NVSS released a provisional dataset including underlying and multiple causes of death to provide near real-time US national mortality data with quality through the Wide-ranging Online Data for Epidemiologic Research (WONDER) during the COVID-19 pandemic [11]. Contemporary mortality status is available on WONDER at the national level from 2018 to 2023. The 2023 NVSS mortality dataset is currently provisional. To examine the trends in mortality rates due to HCC and biliary tract cancers based on their anatomical site, stratified by sex or race and ethnicity in US adults aged ≥25 years before and during the COVID-19 pandemic, we analyzed de-identified mortality records from the NVSS with death certificates through WONDER. Data for the population age <25 were unreliable due to the small number of deaths and were therefore excluded from this analysis. We excluded this data from our study because data for the “not stated” age category cannot be combined with any other age-specified age group. There are no exclusion criteria beyond age. The NVSS dataset encompasses over 99% of mortalities among US residents in all 50 states and the District of Columbia [12]. The NVSS dataset has coded the underlying cause of death and multiple cause of death using the International Classification of Diseases, Tenth Revision (ICD-10) based on the death certificate reports. Multiple cause of death due to HCC or biliary tract cancers is the total death count of individuals who had HCC or biliary tract cancers listed as multiple cause of death, which was combined with the underlying cause of death and contributing causes of death. Contributing cause of death were defined as individuals without HCC or biliary tract cancers listed as the underlying cause of death among individuals with HCC or biliary tract cancers listed on the multiple cause of death. Because all data are publicly available and de-identified, this study does not require approval by the Institutional Review Board at our institution.
Definitions of hepatocellular carcinoma and biliary tract cancers
We defined individuals with HCC and biliary tract cancers listed on the underlying or multiple cause of death. Multiple cause of death due to HCC or biliary tract cancers was defined as individuals who had HCC or biliary tract cancer listed as multiple cause of death, which consisted of the underlying cause of death or contributing causes. Using the ICD-10 codes that have been published [3,6,7,13], we defined HCC based on the ICD-10 code (C22.0, C22.9). Among individuals with HCC, we identified chronic hepatitis C virus (HCV) infection (B17.1, B18.2), metabolic-dysfunction-associated steatotic liver disease (MASLD; K76.0 and K75.81), chronic hepatitis B virus (HBV) infection (B16, B17.0, B18.0, B18.1), and alcohol-related liver disease (ALD; K70) using ICD-10 codes. We classified individuals with biliary tract cancers based on the codes (C22.1, C23, C24.0, C24.1). We identified ICC or ECC using the codes C22.1 and C24.0, respectively. We defined gallbladder cancer using the diagnostic code of C23. We defined AVC using ICD-10 code of C24.1. We defined COVID-19 deaths as ICD-10 code U07.1 using the underlying cause of death or multiple cause of death.
Race and ethnicity were stratified into five mutually exclusive cohorts: Hispanic (who could be of any race), non-Hispanic American Indian or Alaska Native, non-Hispanic Asian or Pacific Islander, non-Hispanic Black, and non-Hispanic White [14,15]. Because data for the “not stated” Hispanic origin category cannot be combined with any other race and ethnicity categories, we excluded this data from our analyses stratified by race and ethnicity. Data for the non-Hispanic American Indian or Alaska Native were unreliable due to a small number of events due to biliary tract cancers and, therefore, were excluded from the final analysis for biliary tract cancer-related mortality stratified by race and ethnicity. Statistics representing one through nine (1–9) deaths by age group are suppressed in the provisional mortality online database. Therefore, we were unable to investigate race and ethnicity- and sex-specific trends in mortality in AVC due to a small number of events. In addition, COVID-19-related mortality in ECC, gallbladder cancer, and AVC could not be estimated due to a small number of events.
Statistical analysis
To calculate annual age-standardized mortality, we divided the number of HCC- and biliary tract cancer-related deaths by the total US census population. We calculated age-specific mortality per 100,000 persons by age group (25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and ≥85 years), standardized to the age distribution of the 2010 US standard population using the direct method. We described the demographic characteristics of the study population according to HCC and biliary tract cancers as frequencies with percentages. Temporal mortality trends were determined using the National Cancer Institute’s joinpoint regression program (version 4.9.1.0) with average APC and the 95% confidence interval (CI) during the study period [16]. This regression fits a series of combined straight line(s) to trend temporal data, which determines whether a single or two trend segments best explain mortality because we set one joinpoint at maximum in this study [16,17].
RESULTS
Patient characteristics
This study analyzed 18,527,426 deaths in US adults aged ≥25 years from 2018 to 2023. The study population consisted of 120,932 HCC-related deaths, 49,756 ICC-related deaths, 5,968 ECC-related deaths, 12,935 gallbladder cancer-related deaths, and 1,833 AVC-related deaths. Supplementary Table 1 provides the demographic characteristics of the study population. HCC was predominantly observed in males (72.1%). The proportion of deaths from ICC, ECC, and AVC had slightly higher proportions of males, whereas more females were observed in terms of deaths from gallbladder cancer. Although the proportion of non-Hispanic White individuals constituted the most prevalent race and ethnicity in both HCC and biliary tract cancers, non-Hispanic Black individuals and Hispanic individuals with HCC and gallbladder cancer represented approximately 15% of deaths in the respective categories.
Age-standardized mortality for hepatocellular carcinoma and biliary tract cancers
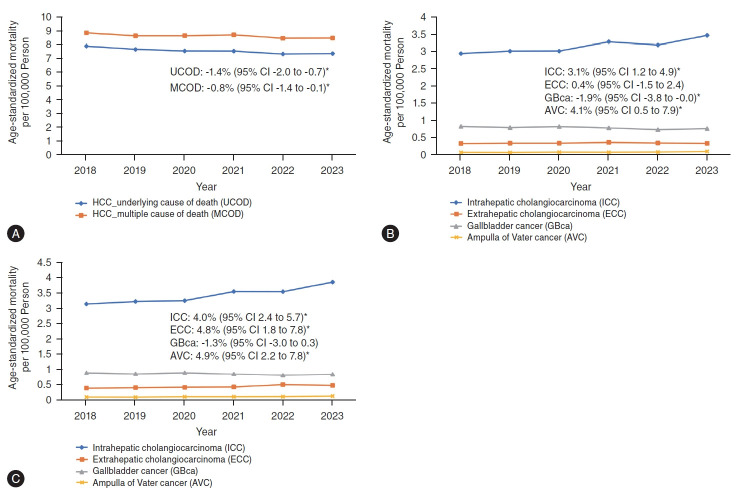
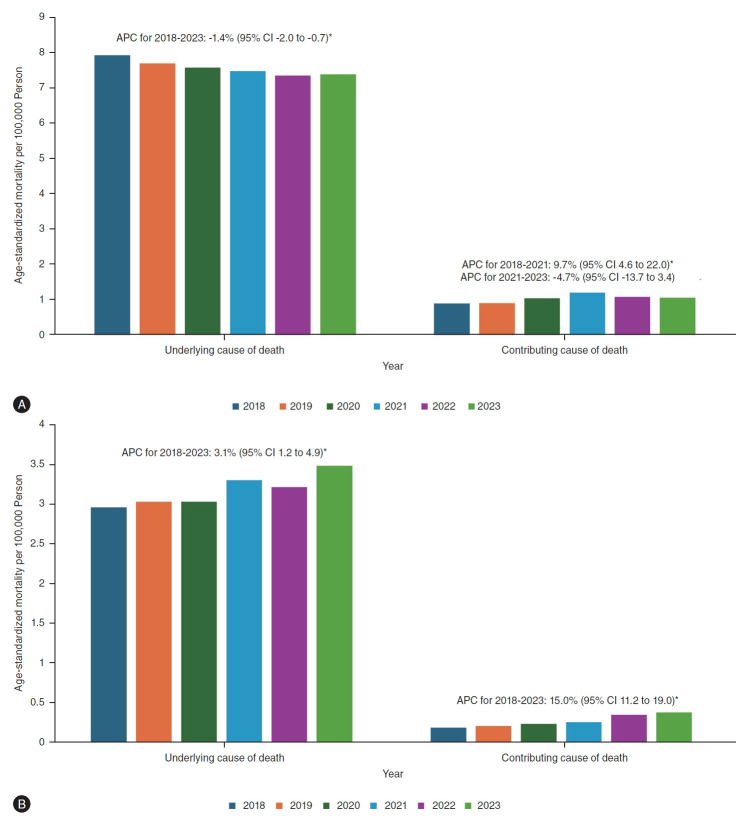
As indicated in Figure 1A and Table 1, the age-standardized mortality from HCC (defined as underlying cause of death) decreased from 7.95 per 100,000 persons in 2018 to 7.42 per 100,000 persons in 2023. Joinpoint analysis revealed a statistically significant average APC decrease of –1.4% (95% CI –2.0% to –0.7%) without any trend segment. When we defined HCC as multiple causes of death, the age-standardized mortality due to HCC slightly increased from 8.68 (2020) to 8.74 (2021) during the early phase of the COVID-19 pandemic and decreased to 8.50 (2022) during the late phase of the COVID-19 pandemic. The age-standardized HCC-related mortality, defined as multiple cause of death, decreased with an average APC of –0.8% (95% CI –1.4% to –0.1%), which was slightly lower than the average APC (–1.4%; 95% CI –2.0% to –0.7%) defined as underlying cause of death. When we assessed the mortality trends based on contributing cause of death due to HCC, we noted that the proportion of contributing cause of death from HCC among individuals with HCC listed on the multiple cause of death captured about 10.7% before the COVID-19 pandemic and 12.9% during the early phase of the COVID-19 pandemic. Contrary to decreasing trends in the underlying cause of death due to HCC (APC –1.4%; [95% CI –2.0% to –0.7%), age-standardized HCC-related mortality as the contributing cause of death sharply increased before and during the early phase of the COVID-19 pandemic with an increase of APC of 9.7% (95% CI 4.6% to 22.0% for 2018–2021; Fig. 2A) and remained stable during the late phase of COVID-19. As shown in Supplementary Figure 1A, COVID-19-related mortality among HCC as contributing cause of death peaked at 9.1% (COVID-19 listed as underlying cause of death) in 2020 and 17% (COVID-19 listed as multiple cause of death) in 2022. As shown in Figure 3, age-standardized HCC-related mortality due to HCV infection continuously decreased initially from 1.42 (2018) per 100,000 persons to 0.90 (2023) with an average APC of –8.5% (95% CI –8.5% to –8.5%) without any trend segment before and during the COVID-19 pandemic. In contrast, there was a linear increase in the age-standardized HCC-related mortality from MASLD (APC 9.7%; 95% CI 4.2% to 15.5%) without any trend segment before and during the COVID-19 pandemic. There were no significant trends in HCC-related mortality due to HBV and ALD.
Figure 1.
Annual age-standardized mortality for hepatocellular carcinoma and biliary tract cancers in the United States between 2018 and 2023. (A) Annual age-standardized mortality for hepatocellular carcinoma. (B) Annual age-standardized mortality for biliary tract cancers defined underlying cause of death. (C) Annual age-standardized mortality for biliary tract cancers defined multiple cause of death. AVC, ampulla of Vater cancer; ECC, extrahepatic cholangiocarcinoma; GBca, gallbladder cancer; ICC, intrahepatic cholangiocarcinoma; HCC, hepatocellular carcinoma; MCOD, multiple cause of death; UCOD, underlying cause of death. *P<0.05.
Table 1.
Age-standardized hepatocellular carcinoma and biliary tract cancer-related mortality rate and APC among US adults ≥25 years in 2018–2023
| No. deaths (age-standardized mortality rate per 100,000 persons) |
Average APC (95% CI) |
||||||
|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2018–2023 | |
| Underlying cause of death | |||||||
| Hepatocellular carcinoma | 20,122 (7.95) | 20,017 (7.72) | 20,142 (7.60) | 20,038 (7.59) | 20,216 (7.38) | 20,395 (7.42) | –1.4 (–2.0, –0.7)* |
| Intrahepatic cholangiocarcinoma | 7,459 (2.97) | 7,807 (3.04) | 7,955 (3.04) | 8,554 (3.31) | 8,609 (3.22) | 9,370 (3.49) | 3.1 (1.2, 4.9)* |
| Extrahepatic cholangiocarcinoma | 925 (0.37) | 966 (0.37) | 988 (0.37) | 1,037 (0.40) | 1,033 (0.38) | 1,004 (0.37) | 0.4 (–1.5, 2.4) |
| Gallbladder cancer | 2,174 (0.86) | 2,130 (0.82) | 2,258 (0.86) | 2,118 (0.82) | 2,077 (0.77) | 2,158 (0.79) | –1.9 (–3.8, –0.0)* |
| Ampullar of Vater cancer | 267 (0.11) | 266 (0.10) | 294 (0.11) | 286 (0.11) | 318 (0.12) | 371 (0.14) | 4.1 (0.5, 7.9)* |
| Multiple cause of death | |||||||
| Hepatocellular carcinoma | 22,482 (8.89) | 22,480 (8.67) | 22,997 (8.68) | 23,062 (8.74) | 23,268 (8.50) | 23,403 (8.52) | –0.8 (–1.4, –0.1)* |
| Intrahepatic cholangiocarcinoma | 7,967 (3.17) | 8,364 (3.26) | 8,589 (3.29) | 9,259 (3.58) | 9,594 (3.58) | 10,450 (3.89) | 4.0 (2.4, 5.7)* |
| Extrahepatic cholangiocarcinoma | 1,043 (0.41) | 1,101 (0.42) | 1,148 (0.43) | 1,180 (0.45) | 1,423 (0.53) | 1,359 (0.50) | 4.8 (1.8, 7.8)* |
| Gallbladder cancer | 2,327 (0.92) | 2,294 (0.89) | 2,439 (0.92) | 2,288 (0.88) | 2,291 (0.85) | 2,372 (0.87) | –1.3 (–3.0, 0.3) |
| Ampullar of Vater cancer | 291 (0.11) | 294 (0.11) | 336 (0.13) | 332 (0.13) | 360 (0.13) | 409 (0.15) | 4.9 (2.2, 7.8)* |
APC, annual percentage change; CI, confidence interval.
P<0.05.
Figure 2.
Age-standardized mortality due to hepatocellular carcinoma and intrahepatic cholangiocarcinoma as underlying or contributing cause of death in the United States from 2018 to 2023. (A) Hepatocellular carcinoma. (B) Intrahepatic cholangiocarcinoma. APC, annual percentage change; CI, confidence interval. *P<0.05.
Figure 3.
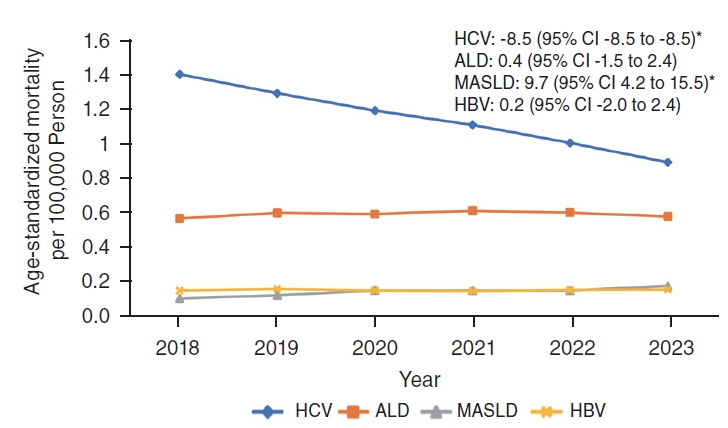
Age-standardized mortality for hepatocellular carcinoma stratified according to etiology in the United States between 2018 and 2023. ALD, alcohol-related liver disease; CI, confidence interval; HBV, hepatitis B virus infection; HCV, hepatitis C virus infection; MASLD, metabolic dysfunction-associated steatotic liver disease. *P<0.05.
The number of deaths due to ICC steadily increased from 7,459 in 2018 to 9,370 in 2023. The age-standardized mortality due to ICC (defined as underlying cause of death) increased from 2.97 (2018) per 100,000 persons and 3.04 (2019) before the COVID-19 pandemic and from 3.04 in 2020, 3.31 in 2021, to 3.49 in 2023 during the COVID-19 pandemic (Fig. 1B). There was a linear increase in the age-standardized ICC-related mortality (APC 3.1%; 95% CI 1.2% to 4.9% as underlying cause of death; APC 4.0%; 2.4% to 5.7% for multiple cause of death) without any trend segment. As shown in Figure 2B, age-standardized ICC-related mortality, defined as contributing cause of death, more steeply increased with an average APC of 15.0% (95% CI 11.2% to 19.0%) without any trend segment than mortality defined as underlying cause of death (APC 3.1%; 95% CI 1.2% to 4.9%). COVID-19-related mortality among ICC listed as contributing cause of death peaked at 9.2% (COVID-19 listed as underlying cause of death) and 17.9% (COVID-19 listed as multiple cause of death) in 2021 (Supplementary Fig. 1B).
The age-standardized ECC-related mortality remained stable from 2018 to 2023 (APC 0.4%; 95% CI –1.5% to 2.4%). When we defined ECC as multiple causes of death (Fig. 1C), age-standardized mortality increased significantly from 0.43 (2020) to 0.53 (2022) during the COVID-19 pandemic (APC 4.8%; 95% CI 1.8% to 7.8%) without any trend segment. The age-standardized mortality from AVC steadily increased from 2018 to 2023 without any trend segment (APC 4.1%; 95% CI 0.5% to 7.9% as underlying cause of death; APC 4.9%; 95% CI 2.2% to 7.8% as multiple cause of death). In contrast, the age-standardized mortality due to gallbladder cancer (defined as underlying cause of death) decreased from 0.86 (2018) per 100,000 persons to 0.79 (2023). Mortality due to gallbladder cancer steadily decreased without any trend segment (APC –1.9%; 95% CI –3.8% to –0.0% as underlying cause of death; –1.3%; 95% CI –3.0% to 0.3% as multiple cause of death).
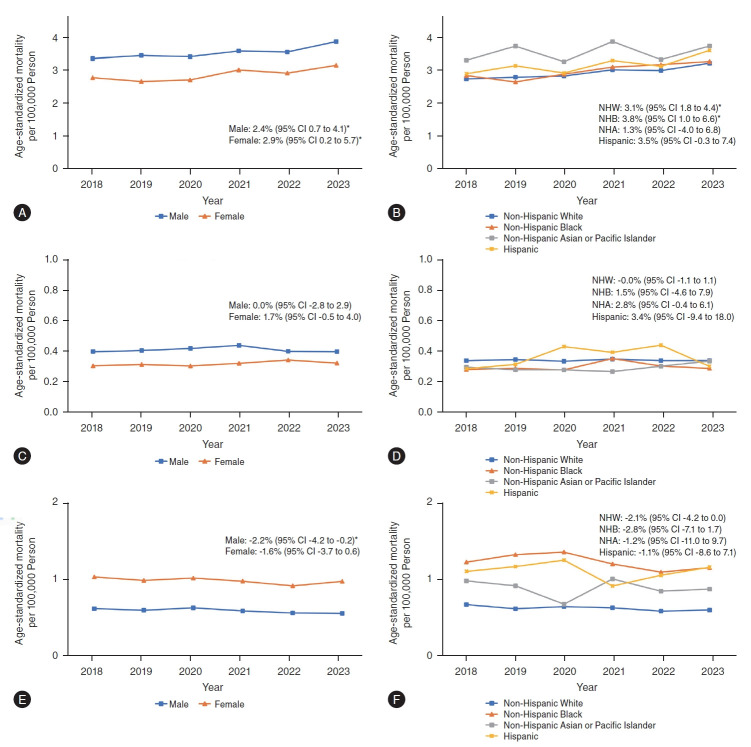
Age-standardized mortality for hepatocellular carcinoma and biliary tract cancers by sex
When we analyzed mortality by sex, HCC, ICC, and ECC-related mortality (defined as underlying cause of death) in males was higher than in females (Tables 2, 3 and Figs. 4, 5). Regarding HCC (Table 2 and Fig. 4), decreasing trends in mortality due to HCC were noted in males (APC –1.9%; 95% CI –2.7% to –1.2%) without any trend segment while these trends remained stable in females (APC 0.1%; 95% CI –0.7% to 0.9%). Increasing trends in ICC-related mortality were similar between males (APC 2.4%; 95% CI 0.7% to 4.1%) and females (APC 2.9%; 95% CI 0.2% to 5.7%, Table 3 and Fig. 5) without any trend segment. Regarding ECC (Table 3 and Fig. 5), trends in mortality remain stable in females and males. Gallbladder cancer-related mortality in females was higher compared to males, with decreasing trends in mortality that were steeper in men (APC –2.2%; 95% CI –4.2% to –0.2%) than in women (APC –1.6%; 95% CI –3.7% to 0.6%, Table 3 and Fig. 5) without any trend segment.
Table 2.
Age-standardized hepatocellular carcinoma-related mortality rate and APC among US adults ≥25 years in 2018–2023
| Age-standardized mortality rate (per 100,000 persons) |
Average APC (95% CI) |
||||||
|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2018–2023 | |
| Hepatocellular carcinoma | 7.95 | 7.72 | 7.60 | 7.59 | 7.38 | 7.42 | –1.4 (–2.0, –0.7)* |
| Race and ethnicity | |||||||
| Non-Hispanic White | 6.78 | 6.69 | 6.63 | 6.64 | 6.51 | 6.59 | –0.6 (–1.1, –0.1)* |
| Non-Hispanic Black | 11.20 | 10.79 | 9.87 | 9.32 | 9.15 | 9.36 | –3.9 (–6.6, –1.0)* |
| Non-Hispanic Asian | 9.68 | 9.29 | 9.27 | 9.25 | 8.52 | 8.34 | –2.8 (–4.3, –1.3)* |
| Non-Hispanic American Indian or Alaska Native | 12.73 | 12.14 | 13.52 | 12.34 | 11.25 | 9.68 | –4.7 (–9.8, 0.7) |
| Hispanic | 12.15 | 11.07 | 11.12 | 10.71 | 10.81 | 10.65 | –2.2 (–4.1, –0.3)* |
| Sex | |||||||
| Male | 12.63 | 12.27 | 11.95 | 11.71 | 11.46 | 11.51 | –1.9 (–2.7, –1.2)* |
| Female | 3.89 | 3.78 | 3.86 | 3.87 | 3.83 | 3.89 | 0.1 (–0.7, 0.9) |
APC, annual percentage change; CI, confidence interval.
P<0.05.
Table 3.
Age-standardized biliary tract cancer-related mortality rate and APC among US adults ≥25 years in 2018–2023
| Age-standardized mortality rate (per 100,000 persons) |
Average APC (95% CI) |
||||||
|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2018–2023 | |
| Intrahepatic cholangiocarcinoma | 2.97 | 3.04 | 3.04 | 3.31 | 3.22 | 3.49 | 3.1 (1.2, 4.9)* |
| Race and ethnicity | |||||||
| Non-Hispanic White | 2.92 | 2.98 | 3.01 | 3.21 | 3.19 | 3.42 | 3.1 (1.8, 4.4)* |
| Non-Hispanic Black | 3.03 | 2.82 | 3.07 | 3.30 | 3.37 | 3.48 | 3.8 (1.0, 6.6)* |
| Non-Hispanic Asian | 3.52 | 3.97 | 3.47 | 4.12 | 3.54 | 3.97 | 1.3 (–4.0, 6.8) |
| Hispanic | 3.08 | 3.34 | 3.11 | 3.51 | 3.32 | 3.84 | 3.5 (–0.3, 7.4) |
| Sex | |||||||
| Male | 3.38 | 3.46 | 3.43 | 3.60 | 3.57 | 3.88 | 2.4 (0.7, 4.1)* |
| Female | 2.80 | 2.69 | 2.73 | 3.04 | 2.94 | 3.18 | 2.9 (0.2, 5.7)* |
| Extrahepatic cholangiocarcinoma | 0.37 | 0.37 | 0.37 | 0.40 | 0.38 | 0.37 | 0.4 (–1.5, 2.4) |
| Race and ethnicity | |||||||
| Non-Hispanic White | 0.37 | 0.38 | 0.37 | 0.38 | 0.37 | 0.37 | –0.0 (–1.1, 1.1) |
| Non-Hispanic Black | 0.31 | 0.32 | 0.31 | 0.39 | 0.33 | 0.32 | 1.5 (–4.6, 7.9) |
| Non-Hispanic Asian | 0.33 | 0.31 | 0.31 | 0.29 | 0.33 | 0.37 | 2.8 (–0.4, 6.1) |
| Hispanic | 0.31 | 0.35 | 0.47 | 0.43 | 0.48 | 0.33 | 3.4 (–9.4, 18.0) |
| Sex | |||||||
| Male | 0.41 | 0.42 | 0.44 | 0.46 | 0.42 | 0.41 | 0.0 (–2.8, 2.9) |
| Female | 0.32 | 0.33 | 0.32 | 0.33 | 0.36 | 0.34 | 1.7 (–0.5, 4.0) |
| Gallbladder cancer | 0.86 | 0.82 | 0.86 | 0.82 | 0.77 | 0.79 | –1.9 (–3.8, –0.0)* |
| Race and ethnicity | |||||||
| Non-Hispanic White | 0.73 | 0.67 | 0.70 | 0.69 | 0.64 | 0.65 | –2.1 (–4.2, 0.0) |
| Non-Hispanic Black | 1.33 | 1.44 | 1.48 | 1.31 | 1.19 | 1.26 | –2.8 (–7.1, 1.7) |
| Non-Hispanic Asian | 1.07 | 1.00 | 0.74 | 1.10 | 0.92 | 0.95 | –1.2 (–11.0, 9.7) |
| Hispanic | 1.20 | 1.27 | 1.36 | 1.00 | 1.15 | 1.26 | –1.1 (–8.6, 7.1) |
| Sex | |||||||
| Male | 0.63 | 0.61 | 0.64 | 0.60 | 0.57 | 0.57 | –2.2 (–4.2, –0.2)* |
| Female | 1.06 | 1.01 | 1.04 | 1.00 | 0.94 | 1.00 | –1.6 (–3.7, 0.6) |
APC, annual percentage change; CI, confidence interval.
P<0.05.
Figure 4.
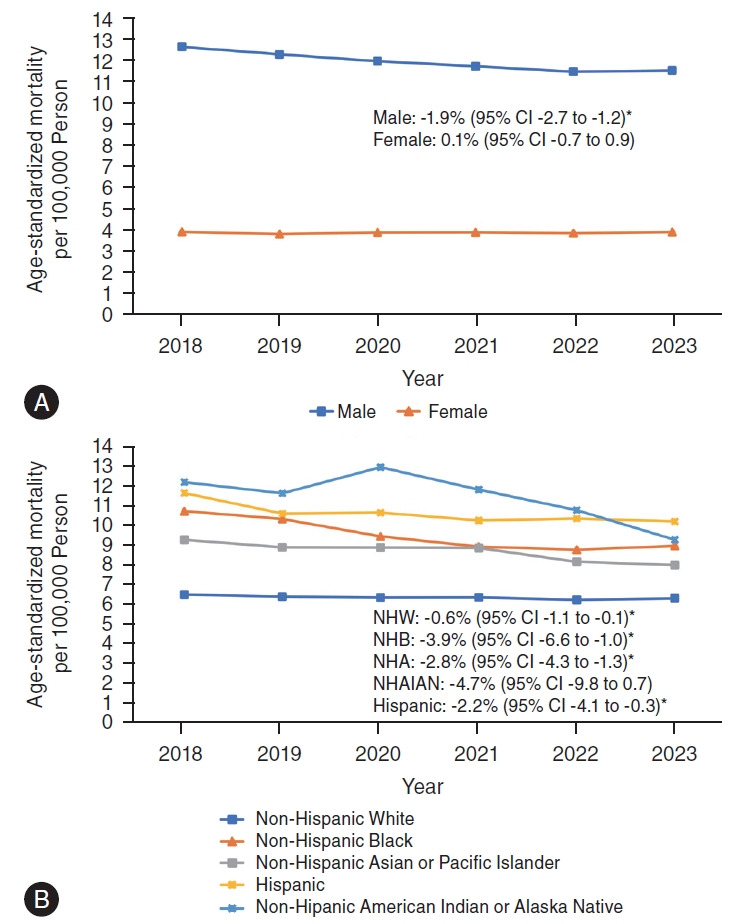
Annual age-standardized sex-based and race and ethnicity-based mortality for hepatocellular carcinoma in the United States between 2018 and 2023. (A) Sex-based mortality for hepatocellular carcinoma. (B) Race and ethnicity-based mortality for hepatocellular carcinoma. CI, confidence interval; NHA, non-Hispanic Asian; NHAIAN; non-Hispanic American Indian or Alaska Native; NHB, non-Hispanic Black; NHW, non-Hispanic White. *P<0.05.
Figure 5.
Annual age-standardized sex-based and race and ethnicity-based mortality for biliary tract cancers in the United States between 2018 and 2023. (A) Sex-based mortality for intrahepatic cholangiocarcinoma. (B) Race and ethnicity-based mortality for intrahepatic cholangiocarcinoma. (C) Sex-based mortality for extrahepatic cholangiocarcinoma. (D) Race and ethnicity-based mortality for extrahepatic cholangiocarcinoma. (E) Sex-based mortality for gallbladder cancer. (F) Race and ethnicity-based mortality for gallbladder cancer. CI, confidence interval; NHA, non-Hispanic Asian; NHB, non-Hispanic Black; NHW, non-Hispanic White. *P<0.05.
Age-standardized mortality for hepatocellular carcinoma and biliary tract cancers by race and ethnicity
Racial and ethnic differences in age-standardized HCC-related mortality are shown in Table 2 and Figure 4. In 2018, compared with the other racial and ethnic groups, non-Hispanic American Indian or Alaska Native individuals had the highest mortality (12.73 per 100,000), followed by Hispanic individuals (12.15), non-Hispanic Black individuals (11.20) and non-Hispanic Asian individuals (9.68), and lowest among non-Hispanic White individuals (6.78). While the mortality due to HCC steadily decreased across all races and ethnicities, the decline in the trends of HCC-related mortality varied by race and ethnicity. Age-standardized mortality decreased more steeply in non-Hispanic American Indian and Alaskan Native individuals (APC –4.7%; 95% CI –9.8% to 0.7%), non-Hispanic Black individuals (APC –3.9%; 95% CI –6.6% to –1.0%) and non-Hispanic Asian individuals (APC –2.8%; 95% CI –4.3% to –1.3%) followed by Hispanic individuals (APC –2.2%; 95% CI –4.1% to –0.3%) and at the lowest rate in non-Hispanic White individuals (APC –0.6%; 95% CI –1.1% to –0.1%) without any trend segment.
Racial and ethnic differences in mortality for biliary tract cancers depended on the malignancy’s anatomical site (Table 3 and Fig. 5). In 2023, compared with the other racial and ethnic groups, non-Hispanic Asian individuals had higher mortality rates for ICC (3.97 per 100,000 vs. 3.84 for Hispanic individuals, and 3.48 for non-Hispanic Black individuals), for ECC (0.37 vs. 0.37 for non-Hispanic White individuals, and 0.33 for Hispanic individuals). Mortality related to ICC increased steadily in non-Hispanic Black individuals (APC 3.8%; 95% CI 1.0% to 6.6%) and non-Hispanic White individuals (APC 3.1%; 95% CI 1.8% to 4.4%) with statistical significance. In contrast, age-standardized mortality due to ECC remained relatively stable across race and ethnicity. In 2023, compared with the other racial and ethnic groups, Hispanic individuals and non-Hispanic Black individuals had higher mortality rates for gallbladder cancer (1.26 vs. 0.65 for non-Hispanic White individuals). The mortality for gallbladder cancer decreased steadily across all races and ethnicities during the study period without statistical significance (Table 3 and Fig. 5).
DISCUSSION
In this population-based national study, we estimated up-to-date mortality trends in HCC and biliary tract cancers in the US. Annual mortality due to HCC has decreased steadily before and during the COVID-19 pandemic. While the mortality associated with ICC and AVC increased linearly, ECC-related mortality remained stable during the study. In contrast, mortality due to gallbladder cancer decreased steadily before and during the COVID-19 pandemic.
Contrary to decreasing trends in the underlying cause of death due to HCC, HCC-related mortality as the contributing cause of death sharply increased before and during the early phase of the COVID-19 pandemic. Contributing cause of death due to ICC increased more steeply than the underlying cause of death due to ICC during the COVID-19 pandemic. COVID-19-related mortality among patients with HCC consisted of up to 9% as the underlying cause of death and 17% as the multiple cause of death. During the COVID-19 pandemic, the inability to visit healthcare providers for the care of other diseases (cardiovascular disease, extrahepatic cancer, etc.) and the increase in COVID-19-related deaths may provide a plausible explanation for the discrepancy between underlying cause of death and multiple cause of death, which consisted of the underlying cause of death or contributing causes. Although these data suggested the impact of COVID-19 on mortality among individuals with HCC and ICC, further studies are needed to determine the impact of COVID-19 on mortality in HCC and biliary tract cancers.
Recent reports from the Surveillance, Epidemiology, and End Results (SEER) dataset 1992–2018 and 2000–2019 showed that the incidence of HCC in the US began to decline to start in 2015 [18,19]. These data from the SEER database were limited due to the unavailability of the etiology of liver disease in patients with HCC [18,19]. In comparison to the previous study that reported plateauing trends in mortality due to HCC from 2009 to 2018 [3], this study showed a decrease in HCC-related mortality from 2018 to 2023. A previous study reported an increase in HCC-related mortality due to HCV infection at an annual rate of 5.4% (95% CI 3.6% to 7.3%) from 2009 to 2014, followed by a decrease from 2014 to 2018 in the annual rate of –3.5% (95% CI –5.9% to –1.1%) [3]. We found that HCC-related mortality from HCV infection continuously decreased with an average APC of –8.5% before and during the COVID-19 pandemic. While HCV infection remains the leading etiology of HCC in the US, the improvement in sustained virological response due to direct-acting antiviral agents against HCV infection has resulted in about 50–80% risk reduction of HCC in this subset [20,21]. However, although the continued decline in HCC-related mortality due to HCV infection may offset rising rates of HCC-related mortality due to MASLD, we noted that HCC-related mortality due to MASLD accelerated during the COVID-19 pandemic. In another study using the SEER dataset, while the proportion of HCC diagnosed at stage 1 increased from 1992 to 2019, the proportion of HCC diagnosed at stage 4 decreased [22]. Therefore, an overall improvement in the efficacy of HCV treatment and early diagnosis may partly explain our results that showed a decrease in age-standardized mortality from HCC with an average APC decrease of –1.4% (95% CI –2.0% to –0.7%).
The mortality rate due to HCC among males was over 3-fold higher than in females. Instead, we found decreasing trends in mortality due to HCC in males, while these trends remained stable in females. A recent study reported increasing HCC incidence among females between 2014 and 2019 (APC 2.0%) compared to stable trends in incidence among males (APC 0.0%) during the same period [2], which potentially mirrors the lack of decline in recent mortality rates in females. A recent US multicenter study showed that females had a significantly higher frequency of MASLD as an etiology of HCC and noncirrhotic HCC than males [23]. Stable trends in mortality in females may be explained by a steady increase in HCC-related mortality due to MASLD. Although cautious interpretation is needed due to underestimation of MASLD, we noted a clue of a steady increase in HCC-related mortality due to MASLD in females (Supplementary Fig. 2). Further studies are needed to provide further evidence.
We found that the racial and ethnic minority groups in the US have a disproportionately higher burden of HCC-related mortality. In comparison to the previously reported trends in the incidence rates from five years ago [19], our study showed a markedly steeper decline in racial and ethnic minority groups-specific mortality trends associated with HCC among non-Hispanic Black individuals, non-Hispanic Asian individuals, and Hispanic individuals versus non-Hispanic White individuals. The continuing decrease in mortality associated with HCC was driven mainly by decreasing trends among racial and ethnic minority individuals and males.
Early diagnosis of cholangiocarcinoma may be challenging due to multiple reasons, including hard-to-access/image anatomical location, the silent clinical presentation with late onset of symptoms, paucicellular nature, and lack of consensus on surveillance strategies [24]. Consistent with the increasing incidence rate [6], the increasing trends in mortality due to ICC may be associated with late diagnosis and limited treatment options following the diagnosis. In this study, the racial and ethnic minority groups in the US were noted to have a disproportionately higher burden of ICC-and gallbladder cancer-related mortality. Additionally, we observed a higher increasing trend in ICC-related mortality in non-Hispanic Black individuals. Contrary to HCC or other biliary tract cancers, approximately two-thirds of deaths due to gallbladder cancer occurred among females. We noted a faster decrease in mortality due to gallbladder cancer in males than in females. Consistent with our study, there were race and ethnicity-specific and sex-specific differences in the incidence and survival of biliary tract cancers in the US [25,26]. Future studies are needed to improve our understanding of the specific root cause(s) associated with race- and ethnicity-based differences in the mortality of patients with HCC and biliary tract cancers.
The decreasing incidence of gallbladder cancer may be associated with the concomitant increase in cholecystectomy for gallstone and gallbladder polyps, which are known risk factors for gallbladder cancer [27,28]. Our study showed a slight increase in gallbladder cancer-related mortality in 2020. Because most elective and emergency surgeries, including cholecystectomy, were halted and delayed during the COVID-19 pandemic [29], gallbladder cancer-related incidence and mortality may be affected during and after the pandemic. Future studies are needed to confirm this hypothesis.
The main strength of our study is that it includes an up-to-date report of the national longitudinal mortality trends in HCC and biliary tract cancers by sex or race and ethnicity. This allowed us to evaluate population-based data and gain a unique insight into mortality due to HCC or biliary tract cancers based on sex and race/ethnicity. Because we utilized the recent NVSS 2018–2023 dataset, we were able to investigate the contemporary burdens of HCC- and biliary tract cancer-related mortality before and during the COVID-19 pandemic. However, the present study had several limitations. First, the underlying or multiple cause of death may be subject to underestimation and misclassification. Such problems can be mitigated when analyzing trends in which underestimation has been assumed to be relatively constant over the study period. Second, regarding low mortality from ECC, the current ICD-10 system did not have any codes for specific perihilar and hilar cholangiocarcinoma [30]. Future ICD-11 should have clear codes for perihilar and distal cholangiocarcinoma. Third, data for the non-Hispanic American Indian or Alaska Native were unreliable due to a small number of events due to biliary tract cancers and, therefore, were excluded from the final analysis for biliary tract cancer-related mortality stratified by race and ethnicity. We were also unable to investigate race and ethnicity-specific or sex-specific trends in mortality due to AVC because of a small number of events. In addition, COVID-19-related mortality in ECC, gallbladder cancer, and AVC could not be estimated due to a small number of events. Fourth, the provisional dataset for 2023 national mortality may be incomplete and likely not include all deaths that occurred during a given period (accessed in May 2024). This 2023 NVSS mortality provisional dataset may be posed to reporting lag. Therefore, this result using the 2023 NVSS mortality provisional dataset should be interpreted cautiously. Fifth, the low mortality rates from MASLD are consistent with significant underreporting of this etiology on death certificates, leading to underestimation of the true prevalence of MASLD by utilizing ICD codes. In addition, we were unable to capture all etiologies of chronic liver disease among individuals with HCC due to the inherent limitation of this database based on death certificates. These limitations may be alleviated because these underestimations were supposed to be constant during the study period. Therefore, these results need to be interpreted cautiously.
In conclusion, while overall HCC-related mortality tended to decline after the introduction of potent antiviral agents, ICC- and AVC-related mortality have increased steadily. Recent declines in HCC may be primarily due to declines among racial and ethnic minority individuals and males. Mortality for ECC remained stable, while gallbladder cancer-related mortality constantly decreased before and during the COVID-19 pandemic. In addition, racial and ethnic minority individuals in the US have a disproportionately high burden of HCC and biliary tract cancer-related mortality. In the future, an attempt to formally study and more clearly understand the reason(s) for the differences in mortality among racial and ethnic minority individuals with HCC and biliary tract cancers may help gain further insight into crucial mechanistic pathways and/or gaps in linkage-to-care.
Abbreviations
- APC
annual percentage change
- AVC
ampulla of Vater cancer
- CI
confidence interval
- COVID-19
coronavirus disease 2019
- ECC
extrahepatic cholangiocarcinoma
- HCC
hepatocellular carcinoma
- ICC
intrahepatic cholangiocarcinoma
- ICD-10
International Classification of Diseases
- NVSS
National Vital Statistics System
Study Highlights
• In this population-based US national study (n=18,527,426), annual mortality due to HCC decreased steadily before and during the COVID-19 pandemic. While the mortality associated with intrahepatic cholangiocarcinoma and ampulla of Vater cancer increased linearly, extrahepatic cholangiocarcinoma-related mortality remained stable during the study. In contrast, mortality due to gallbladder cancer decreased steadily. Racial and ethnic minority individuals in the US have a disproportionately higher burden of mortality resulting from HCC and biliary tract cancers. Recent declines in HCC may be primarily due to declines among racial and ethnic minority individuals and males.
Footnotes
Authors’ contribution
Donghee Kim and Aijaz Ahmed were responsible for the study concept and design, data acquisition, statistical analysis, interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, study supervision, and approval of the final draft manuscript.
Richie Manikat, Karn Wijarnpreecha, and George Cholankeril were responsible for the interpretation and presentation of data, critical revision of the manuscript for important intellectual content, and approval of the final manuscript.
Conflicts of Interest
The authors have no conflicts to disclose.
SUPPLEMENTAL MATERIAL
Supplementary material is available at Clinical and Molecular Hepatology website (http://www.e-cmh.org).
Data Transparency Statement: The National Vital Statistics System mortality dataset are publicly available at the National Center for Health Statistics of the Center for Disease Control and Prevention (https://www.cdc.gov/nchs/nvss/index.htm).
The Proportion of COVID-19-related mortality as underlying or multiple cause of death among individuals with hepatocellular carcinoma or intrahepatic cholangiocarcinoma in the United States from 2018 to 2023. (A) Hepatocellular carcinoma. (B) Intrahepatic cholangiocarcinoma.
Age-standardized sex-based mortality for hepatocellular carcinoma due to metabolic dysfunction-associated steatotic liver disease in the United States between 2018 and 2023. CI, confidence interval.
Characteristics of deaths in the United States for hepatocellular carcinoma and biliary tract cancers as an underlying cause of death from 2018 to 2023 (total population=18,527,426)
REFERENCES
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12–49. doi: 10.3322/caac.21820. [DOI] [PubMed] [Google Scholar]
- 3.Kim D, Konyn P, Cholankeril G, Wong RJ, Younossi ZM, Ahmed A, Hepatocellular Carcinoma Research Committee for Chronic Liver Disease Foundation Decline in annual mortality of hepatitis C virus-related hepatocellular carcinoma in the United States, from 2009 to 2018. Gastroenterology. 2020;159:1558–1560.e2. doi: 10.1053/j.gastro.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Van Dyke AL, Shiels MS, Jones GS, Pfeiffer RM, Petrick JL, Beebe-Dimmer JL, et al. Biliary tract cancer incidence and trends in the United States by demographic group, 1999-2013. Cancer. 2019;125:1489–1498. doi: 10.1002/cncr.31942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hemming AW. Biliary tract and primary liver tumors: Who, what, and why? Surg Oncol Clin N Am. 2019;28:519–538. doi: 10.1016/j.soc.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 6.Kim D, Konyn P, Cholankeril G, Bonham CA, Ahmed A. Trends in the mortality of biliary tract cancers based on their anatomical site in the United States from 2009 to 2018. Am J Gastroenterol. 2021;116:1053–1062. doi: 10.14309/ajg.0000000000001151. [DOI] [PubMed] [Google Scholar]
- 7.Kim D, Li AA, Perumpail BJ, Gadiparthi C, Kim W, Cholankeril G, et al. Changing trends in etiology-based and ethnicity-based annual mortality rates of cirrhosis and hepatocellular carcinoma in the United States. Hepatology. 2019;69:1064–1074. doi: 10.1002/hep.30161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maddock J, Parsons S, Di Gessa G, Green MJ, Thompson EJ, Stevenson AJ, et al. Inequalities in healthcare disruptions during the COVID-19 pandemic: evidence from 12 UK population-based longitudinal studies. BMJ Open. 2022;12:e064981. doi: 10.1136/bmjopen-2022-064981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shiels MS, Haque AT, Haozous EA, Albert PS, Almeida JS, García-Closas M, et al. Racial and ethnic disparities in excess deaths during the COVID-19 pandemic, March to December 2020. Ann Intern Med. 2021;174:1693–1699. doi: 10.7326/M21-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmad FB, Cisewski JA, Miniño A, Anderson RN. Provisional mortality data - United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:519–522. doi: 10.15585/mmwr.mm7014e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu J, Murphy SL, Kochanek KD, Arias E. Deaths: Final data for 2019. Natl Vital Stat Rep. 2021 Jul 26; doi: 10.15620/cdc:106058. doi: [DOI] [PubMed] [Google Scholar]
- 13.Kim D, Adejumo AC, Yoo ER, Iqbal U, Li AA, Pham EA, et al. Trends in mortality from extrahepatic complications in patients with chronic liver disease, from 2007 through 2017. Gastroenterology. 2019;157:1055–1066.e11. doi: 10.1053/j.gastro.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 14.Yang Q, Tong X, Schieb L, Vaughan A, Gillespie C, Wiltz JL, et al. Vital signs: Recent trends in stroke death rates - United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;66:933–939. doi: 10.15585/mmwr.mm6635e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flanagin A, Frey T, Christiansen SL, AMA Manual of Style Committee Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA. 2021;326:621–627. doi: 10.1001/jama.2021.13304. [DOI] [PubMed] [Google Scholar]
- 16.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 17.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28:3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alvarez CS, Petrick JL, Parisi D, McMahon BJ, Graubard BI, McGlynn KA. Racial/ethnic disparities in hepatocellular carcinoma incidence and mortality rates in the United States, 1992-2018. Hepatology. 2022;76:589–598. doi: 10.1002/hep.32394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Brien TR, Devesa SS, Koshiol J, Marrero JA, Shiels MS. Decreasing incidence of hepatocellular carcinoma among most racial groups: SEER-22, 2000-2019. Cancer Med. 2023;12:19960–19967. doi: 10.1002/cam4.6537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calvaruso V, Cabibbo G, Cacciola I, Petta S, Madonia S, Bellia A, et al. Incidence of hepatocellular carcinoma in patients with HCV-associated cirrhosis treated with direct-acting antiviral agents. Gastroenterology. 2018;155:411–421.e4. doi: 10.1053/j.gastro.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Romano A, Angeli P, Piovesan S, Noventa F, Anastassopoulos G, Chemello L, et al. Newly diagnosed hepatocellular carcinoma in patients with advanced hepatitis C treated with DAAs: A prospective population study. J Hepatol. 2018;69:345–352. doi: 10.1016/j.jhep.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Alvarez CS, Ruhl J, Flynn G, Graubard BI, McGlynn KA. Trends in hepatocellular carcinoma stage by racial/ethnic group in the United States, 1992-2019. JHEP Rep. 2023;5:100868. doi: 10.1016/j.jhepr.2023.100868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phipps M, Livanos A, Guo A, Pomenti S, Yeh J, Dakhoul L, et al. Gender matters: Characteristics of hepatocellular carcinoma in women from a large, multicenter study in the United States. Am J Gastroenterol. 2020;115:1486–1495. doi: 10.14309/ajg.0000000000000643. [DOI] [PubMed] [Google Scholar]
- 24.Ilyas SI, Khan SA, Hallemeier CL, Kelley RK, Gores GJ. Cholangiocarcinoma - evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2018;15:95–111. doi: 10.1038/nrclinonc.2017.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antwi SO, Mousa OY, Patel T. Racial, ethnic, and age disparities in incidence and survival of intrahepatic cholangiocarcinoma in the United States; 1995-2014. Ann Hepatol. 2018;17:604–614. doi: 10.5604/01.3001.0012.0929. [DOI] [PubMed] [Google Scholar]
- 26.Nassour I, Mokdad AA, Minter RM, Polanco PM, Augustine MM, Mansour JC, et al. Racial and ethnic disparities in a national cohort of ampullary cancer patients. J Surg Oncol. 2018;117:220–227. doi: 10.1002/jso.24835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henley SJ, Weir HK, Jim MA, Watson M, Richardson LC. Gallbladder cancer incidence and mortality, United States 1999-2011. Cancer Epidemiol Biomarkers Prev. 2015;24:1319–1326. doi: 10.1158/1055-9965.EPI-15-0199. [DOI] [PubMed] [Google Scholar]
- 28.Alexander S, Lemmens VE, Houterman S, Nollen L, Roumen R, Slooter GD. Gallbladder cancer, a vanishing disease? Cancer Causes Control. 2012;23:1705–1709. doi: 10.1007/s10552-012-0049-0. [DOI] [PubMed] [Google Scholar]
- 29.Ilyas Khan A, Thomas C, O’Connor H, Dowker F, Horgan L, Khan MA. Impact of the COVID-19 pandemic on the management of gallbladder, biliary tract, and pancreatic diseases. Cureus. 2023;15:e43473. doi: 10.7759/cureus.43473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khan SA, Genus T, Morement H, Murphy A, Rous B, Tataru D. Global trends in mortality from intrahepatic and extrahepatic cholangiocarcinoma. J Hepatol. 2019;71:1261–1262. doi: 10.1016/j.jhep.2019.07.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Proportion of COVID-19-related mortality as underlying or multiple cause of death among individuals with hepatocellular carcinoma or intrahepatic cholangiocarcinoma in the United States from 2018 to 2023. (A) Hepatocellular carcinoma. (B) Intrahepatic cholangiocarcinoma.
Age-standardized sex-based mortality for hepatocellular carcinoma due to metabolic dysfunction-associated steatotic liver disease in the United States between 2018 and 2023. CI, confidence interval.
Characteristics of deaths in the United States for hepatocellular carcinoma and biliary tract cancers as an underlying cause of death from 2018 to 2023 (total population=18,527,426)