Abstract
Background
The relative contributions of common patient-reported social determinants of health on 30- and 90-day post-discharge outcomes among patients with acute coronary syndromes (ACS) is unclear.
Objective
The aim of this article is to examine the independent associations of social determinants with readmission or death, accounting for medical history.
Methods
Participants included adults who were hospitalized with ACS at an academic medical center. Domains measured were social support, health literacy/numeracy, and socioeconomic status (SES) (including education and difficulty paying bills). We employed multivariable Cox proportional hazard models to study associations with time to all-cause readmission or death, up to 30 or 90 days after discharge, and adjusted for demographics and medical history (prior admissions and Elixhauser comorbidity index).
Key Results
Among 1,168 patients with ACS and no history of heart failure, more prior admissions, and higher comorbidity index (the medical history domain) were associated with higher rates of 30- and 90-day readmission or death (domain p values <.01 and <.0001, respectively). The social support domain was not associated with outcomes. Higher health literacy and numeracy were associated with lower rates of 30- and 90-day readmission or death (domain p values .016 and .002, respectively). Higher education and less difficulty paying bills (the SES domain) was marginally associated with lower rates of 90-day readmission or death (domain, p = .052).
Conclusions
In addition to medical history, the domain of health literacy and numeracy was independently associated with readmission or death of patients with ACS during the 90 days after hospital discharge. [HLRP: Health Literacy Research and Practice. 2024;8(4):e212–e223.]
Plain language summary
Plain Language Summary: In this study of patients admitted to the hospital with heart conditions, we asked them about their social support, how they understood health information (health literacy), economic status, education, and difficulty paying bills. We found that patients with higher health literacy had less returns to the hospital or died less frequently within 30 and 90 days of their initial stay.
The postdischarge period after hospitalization is a vulnerable time for patients, when increased self-management requirements are common (Guo & Harris, 2016; Wiggins et al., 2013). The self-management tasks may be challenging for patients discharged with high-risk diagnoses such as acute coronary syndromes (ACS). Additionally, medication regimens may change significantly during hospitalization (Harris et al., 2013; Medication safety in transitions of care., 2019). Prior to discharge, patients often receive discharge education in a hurried manner, seldom tailored to their level of health literacy (Blake et al., 2010; Coleman, 2003; Coleman et al., 2013; Daliri et al., 2019; Eibergen et al., 2018). Moreover, once patients leave the hospital, their ability to self-manage may also be affected by the amount of social support they receive or resources available based on their socioeconomic status (SES) (Hardman, 2020; King et al., 2023; Salyer et al., 2012).
A wide array of social determinants of health can impact health outcomes, yet these factors are often not assessed or attended to during hospitalization (Adler et al., 2016; Horwitz et al., 2020). Low health literacy, numeracy, and social support have been associated with poor outcomes in diseases requiring self-management such as coronary artery disease (Aburadwan & Hayajneh, 2024; Beauchamp et al., 2022; Berkman et al., 2011). However, in hospital-based studies, the relationship between health literacy and readmissions has been inconsistent (Ghisi et al., 2018; Kanejima et al., 2022; McNaughton, Cawthon, et al., 2015; Sterling et al., 2018). SES, including income, employment, and education, can affect an individual's adherence to the recommended medical regimen and has been linked with readmissions and mortality (Chiu et al., 2022; Khera et al., 2017). Despite recognition of the importance of these individual risk factors, they frequently co-exist and have not been examined together to determine their relative and independent contributions to postdischarge outcomes for patients with cardiovascular disease.
Our objective was to examine the independent associations of health literacy, numeracy, social support, and SES with poor outcomes post-discharge, specifically unplanned readmission, or death, among patients hospitalized for ACS. We hypothesized that patients who had lower health literacy, numeracy, social support, or SES would have higher rates of readmission or death during the first 30- or 90-days postdischarge, after adjustment for demographic characteristics, medical comorbidities, and prior utilization.
Methods
Study Setting and Design
The Vanderbilt Inpatient Cohort Study (VICS) was a prospective longitudinal study of the impact of patient, social, and medical factors on post-discharge health outcomes such as quality of life, unplanned hospital utilization, and mortality in adults with ACS or acute decompensated heart failure (ADHF). The rationale and design of VICS are detailed elsewhere (Meyers et al., 2014). Briefly, the framework that guided this study posits that demographic factors such as age, race, ethnicity, and socioeconomic status may influence health status, social support, and health literacy. As a result, those three factors may affect how patients interact with health systems, health care providers, and their disease self-management. Taken together, all factors may impact health outcomes such as functional status, health-related quality of life, unplanned health care utilization, and mortality. The study was approved by the Vanderbilt University Medical Center Institutional Review Board.
Participants
Research staff screened patients admitted to Vanderbilt University Hospital who presented with symptoms consistent with ADHF or an intermediate or high likelihood of ACS. A study hospitalist or cardiologist confirmed the diagnosis by reviewing the electronic health record (EHR). Exclusion criteria included: age younger than 18 years, non-English speaker, hearing or vision impairment, unstable psychiatric illness, delirium, low likelihood of follow-up (e.g., no reliable telephone number), on hospice, too ill to complete an interview, or prior enrollment in the study. Once patients with cardiovascular disease agreed to participate, written informed consent was obtained during hospitalization. Enrollment spanned from October 2011 to December 2015. Herein, we report on results for participants with ACS. An analysis of participants with ADHF has been reported previously (Sterling et al., 2018).
During participants' hospitalization, research assistants administered a 45-minute baseline interview at the bedside. Baseline measures included demographic characteristics such as age, gender, and self-reported race.
Measures of Medical History
Participants reported their number of hospitalizations in the prior year. Additionally, a comorbidity index, based on 30 conditions identified by Elixhauser, was calculated from billing codes from the index hospitalization and prior utilization (van Walraven et al., 2009). This single numerical index calculated from the 30 Elixhauser comorbidities had equivalent discrimination when compared to the inclusion of the 30 variables individually (c-statistic 0.763 vs 0.760, respectively), while conserving degrees of freedom.
Measures of Social Support and Marital and Living Status
We determined social support of family and friends prior to hospitalization using measures that characterize instrumental as well as emotional support. Instrumental support is the tangible support received from other people, their informal support network, and unmet personal needs (Schultz et al., 2022). For instrumental support, we drew questions from: (1) the Health and Retirement Study, which quantified the number of friends and family members with whom they had close relationships (Juster & Suzman, 1995); and (2) the Midlife Development in the United States (MIDUS), which quantified the number and frequency of contacts, level of support from friends, families, and neighbors (Rossi, 2004). To assess emotional support (e.g. someone to listen to them, give advice, show love and affection), we drew questions from the ENRICHD Social Support Inventory (ESSI), which has a Cronbach α of 0.86 and Pearson correlation coefficient (ρ) of 0.62 with the Perceived Social Support Scale (Berkman et al., 2003; Blumenthal et al., 1987; The ENRICHD Investigators, 2000).
Additionally, we asked participants their marital status and whether they lived alone. From their responses we created home status, a two-level categorical variable: married or living with someone versus not married and living alone.
Measures of Health Literacy and Numeracy
Health literacy is “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (National Heart, Lung, and Blood Institute, 2000). During the baseline interview, we assessed subjective health literacy using the 3-item Brief Health Literacy Screen (BHLS), scored on a 5-point Likert scale (Chew et al., 2004). We report the sum on a scale ranging from 3 to 15 points, with higher scores indicating higher health literacy. In the hospital setting, the Cronbach α is 0.79, and the Pearson correlation coefficient (ρ) was 0.48 when compared to s-TOFHLA (Wallston et al., 2014).
Numeracy is “the ability to use and understand numbers in daily life” (Golbeck et al., 2005). We measured numeracy using the 3-item Subjective Numeracy Scale (SNS-3). This self-reported measure captures participants' quantitative abilities with numerical data and preferences for numerical information. The SNS-3 is reported as a mean on a scale of 1 to 6. The SNS-3's Cronbach's α for internal reliability ranges from 0.67 to 0.86 for 7 study samples, and it correlates very highly with the original longer measure, the SNS-8 (range of ρ = 0.89 − 0.95) (Fagerlin et al., 2007; McNaughton, Cavanaugh, et al., 2015).
Measures of SES
Participants reported their highest level of education achieved and employment status. We assessed financial strain with a question: “How difficult is it for you (and your family) to pay your monthly bills?” Responses were reverse coded and ranged from 1, very difficult, to 4, not at all difficult (Osborn et al., 2017).
Outcome Measures
The primary outcomes were a composite endpoint of all-cause readmission or death, assessed as time to event during the first 30 or 90 days after discharge. Readmission included hospitalization in any acute care hospital. Outcomes were compiled from the Vanderbilt EHR, participant report during follow-up phone calls, and a complete review of outside hospital records. Participants who died during the index hospitalization (n = 23) were excluded from these analyses because they did not enter the follow-up period.
Analysis
We describe the VICS participants with ACS using proportions for categorical variables and percentiles (i.e., 25th, 50th, 75th) for quantitative variables. To test for unadjusted, covariate associations with readmission/death at 30 and 90 days, we used Pearson Chi-Square test and Wilcoxon Rank-Sum test for the categorical and quantitative variables, respectively.
For primary analyses, we conducted multivariable Cox proportional hazards regression analyses to investigate associations between participant characteristics and the two dependent variables: time to readmission or death up to 30 days and time to readmission or death up to 90 days after discharge. We report hazard ratios, confidence intervals, and p values to describe adjusted associations with outcomes. Specifically, we report hazard ratios and confidence intervals associated with interquartile range changes in independent, continuous variables.
Guided by the study's conceptual framework, and in addition to examining individual independent variable associations with outcomes, we report outcome associations with five independent variable domains--demographics, medical history, social support, health literacy/numeracy, and SES. We conducted domain-outcome association tests using likelihood ratio tests (LRT) with degrees of freedom equal to the number of parameters estimated for the domain. For these domain-specific associations, the LRT compares a model that excludes all variables in the domain to a model that includes them all, in both cases adjusting for all other independent variables.
To further characterize the overall associations of the medical history, social support, health literacy/numeracy, and SES domains with time to readmission or death at 30 and 90 days, we examined association with simultaneous independent variable changes within each domain. Specifically, we examined time to readmission or death associations as follows: (1) for the medical history domain, a simultaneous 1 additional prior admission within 12 months and a 4.5 point increase in Elixhauser score; (2) for the social support domain, a 3 point increase in ESSI and living with someone versus living alone; (3) for the health literacy/numeracy domain, a 2.5 point increase in BHLS and 1 point increase in subjective numeracy; (4) for the SES domain, a 2 year increase in education and a 1 category increase in paying bills score (i.e. when reverse coded it is an increased ease of paying bills). The simultaneous changes in the quantitative variables correspond to approximately one-half interquartile range changes.
To avoid case-wise deletion of records with missing covariates we conducted multiple imputation with five imputation samples using a predictive mean matching algorithm (Harrell, 2016; Rubin & Schenker, 1991). Missingness rates were low. We conducted all analyses in R version 4.1.3 (R Core Team, 2022) with packages rms (Harrell, 2021) and survival (Therneau, 2021), and used 0.05-level significance tests.
Results
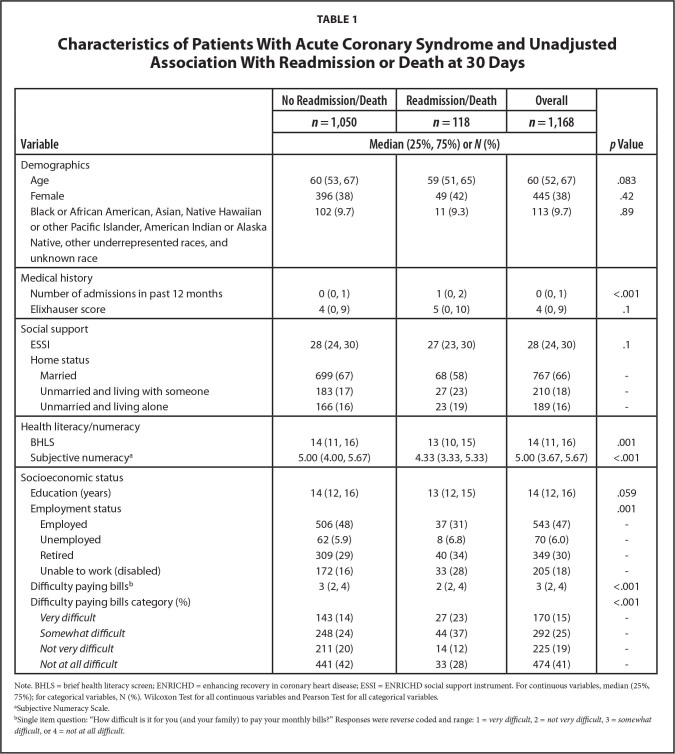
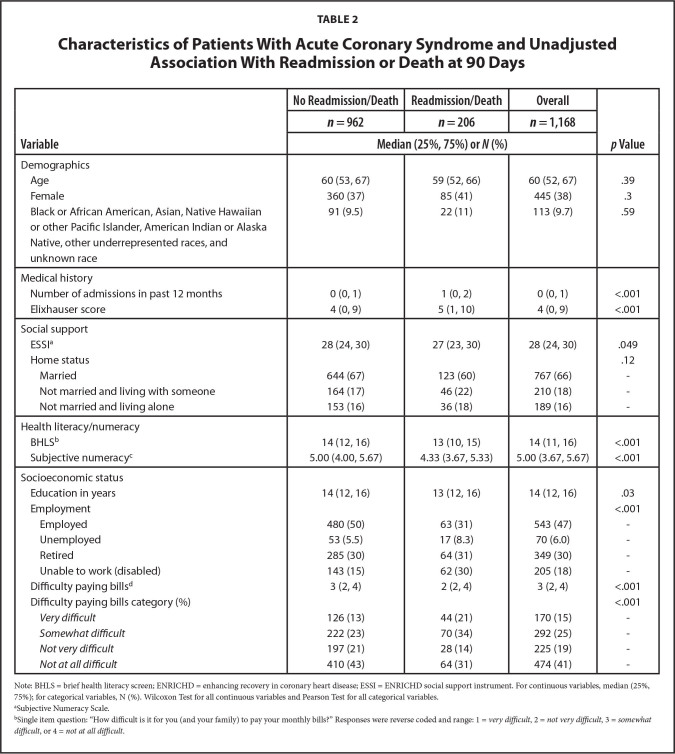
Figure 1 displays the study flow diagram. Of 44,600 patient charts screened, 12,736 (28.6%) had confirmed diagnoses of ACS and/or ADHF. Of 12,736 patients, nearly 30% (3,763) met all eligibility criteria, 80% of whom enrolled. Of the 3,000 participants in the cohort, 2,977 participants were discharged alive. For these analyses, 1168 (39%) had ACS with no prior diagnosis of congestive heart failure. Tables 1 and 2 describe the ACS sample stratified by 30-day and 90-day death/readmission status, respectively. Overall, participants had a median age of 60 years and a median of 14 years of education (Table 1). There were 113 (9.7%) participants who were Black or African American, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, other underrepresented races, and unknown race, and 445 (38%) were female. Approximately 10% of participants (n = 118) were readmitted or died within 30 days after discharge; 17% (n = 206) were readmitted or died within 90 days (Table 2). In unadjusted tests, we observed statistically significant differences in the distributions of income, employment status, number of admissions in the past 12 months, health literacy, numeracy and difficulty paying bills, between participants who were readmitted or died at 30 and 90 days. Additionally, at 90 days there were significant differences in education, Elixhauser score, and social support.
Figure 1.
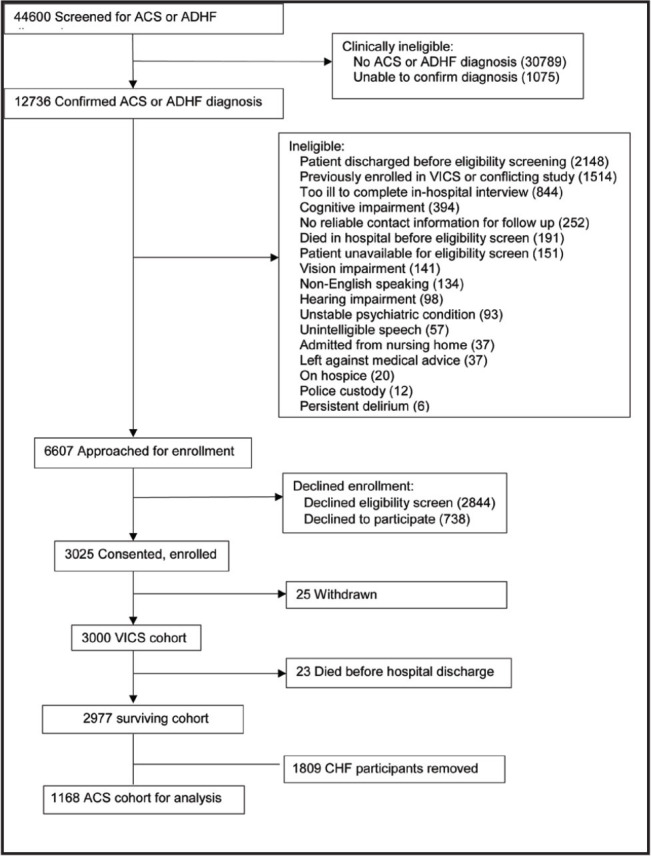
Study flow diagram. The authors recruited, consented, and enrolled 3,000 patients with ACS or ADHF to the VICS cohort, of which 1,168 with ACS were analyzed. ACS = acute coronary syndrome, ADHF = acute decompensated heart failure, VICS = Vanderbilt Inpatient Cohort Study.
Table 1.
Characteristics of Patients With Acute Coronary Syndrome and Unadjusted Association With Readmission or Death at 30 Days
| Variable | No Readmission/Death | Readmission/Death | Overall | p Value |
|---|---|---|---|---|
|
| ||||
| n= 1,050 | n= 118 | n= 1,168 | ||
|
| ||||
| Median (25%, 75%) or N(%) | ||||
|
| ||||
| Demographics | ||||
| Age | 60 (53, 67) | 59 (51, 65) | 60 (52, 67) | .083 |
| Female | 396 (38) | 49 (42) | 445 (38) | .42 |
| Black or African American, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, other underrepresented races, and unknown race | 102 (9.7) | 11 (9.3) | 113 (9.7) | .89 |
|
| ||||
| Medical history | ||||
| Number of admissions in past 12 months | 0 (0, 1) | 1 (0, 2) | 0 (0, 1) | <.001 |
| Elixhauser score | 4 (0, 9) | 5 (0, 10) | 4 (0, 9) | .1 |
|
| ||||
| Social support | ||||
| ESSI | 28 (24, 30) | 27 (23, 30) | 28 (24, 30) | .1 |
| Home status | ||||
| Married | 699 (67) | 68 (58) | 767 (66) | - |
| Unmarried and living with someone | 183 (17) | 27 (23) | 210 (18) | - |
| Unmarried and living alone | 166 (16) | 23 (19) | 189 (16) | - |
|
| ||||
| Health literacy/numeracy | ||||
| BHLS | 14 (11, 16) | 13 (10, 15) | 14 (11, 16) | .001 |
| Subjective numeracya | 5.00 (4.00, 5.67) | 4.33 (3.33, 5.33) | 5.00 (3.67, 5.67) | <.001 |
|
| ||||
| Socioeconomic status | ||||
| Education (years) | 14 (12, 16) | 13 (12, 15) | 14 (12, 16) | .059 |
| Employment status | .001 | |||
| Employed | 506 (48) | 37 (31) | 543 (47) | - |
| Unemployed | 62 (5.9) | 8 (6.8) | 70 (6.0) | - |
| Retired | 309 (29) | 40 (34) | 349 (30) | - |
| Unable to work (disabled) | 172 (16) | 33 (28) | 205 (18) | - |
| Difficulty paying billsb | 3 (2, 4) | 2 (2, 4) | 3 (2, 4) | <.001 |
| Difficulty paying bills category (%) | <.001 | |||
| Very difficult | 143 (14) | 27 (23) | 170 (15) | - |
| Somewhat difficult | 248 (24) | 44 (37) | 292 (25) | - |
| Not very difficult | 211 (20) | 14 (12) | 225 (19) | - |
| Not at all difficult | 441 (42) | 33 (28) | 474 (41) | - |
Note. BHLS = brief health literacy screen; ENRICHD = enhancing recovery in coronary heart disease; ESSI = ENRICHD social support instrument. For continuous variables, median (25%, 75%); for categorical variables, N (%). Wilcoxon Test for all continuous variables and Pearson Test for all categorical variables.
Subjective Numeracy Scale.
Single item question: “How difficult is it for you (and your family) to pay your monthly bills?” Responses were reverse coded and range: 1 = very difficult, 2 = not very difficult, 3 = somewhat difficult, or 4 = not at all difficult.
Table 2.
Characteristics of Patients With Acute Coronary Syndrome and Unadjusted Association With Readmission or Death at 90 Days
| Variable | No Readmission/Death | Readmission/Death | Overall | p Value |
|---|---|---|---|---|
|
| ||||
| n = 962 | n = 206 | n = 1,168 | ||
|
| ||||
| Median (25%, 75%) or N (%) | ||||
|
| ||||
| Demographics | ||||
| Age | 60 (53, 67) | 59 (52, 66) | 60 (52, 67) | .39 |
| Female | 360 (37) | 85 (41) | 445 (38) | .3 |
| Black or African American, Asian, Native Hawaiian | 91 (9.5) | 22 (11) | 113 (9.7) | .59 |
| or other Pacific Islander, American Indian or Alaska Native, other underrepresented races, and unknown race | ||||
|
| ||||
| Medical history | ||||
| Number of admissions in past 12 months | 0 (0, 1) | 1 (0, 2) | 0 (0, 1) | <.001 |
| Elixhauser score | 4 (0, 9) | 5 (1, 10) | 4 (0, 9) | <.001 |
|
| ||||
| Social support | ||||
| ESSIa | 28 (24, 30) | 27 (23, 30) | 28 (24, 30) | .049 |
| Home status | .12 | |||
| Married | 644 (67) | 123 (60) | 767 (66) | - |
| Not married and living with someone | 164 (17) | 46 (22) | 210 (18) | - |
| Not married and living alone | 153 (16) | 36 (18) | 189 (16) | - |
|
| ||||
| Health literacy/numeracy | ||||
| BHLSb | 14 (12, 16) | 13 (10, 15) | 14 (11, 16) | <.001 |
| Subjective numeracyc | 5.00 (4.00, 5.67) | 4.33 (3.67, 5.33) | 5.00 (3.67, 5.67) | <.001 |
|
| ||||
| Socioeconomic status | ||||
| Education in years | 14 (12, 16) | 13 (12, 16) | 14 (12, 16) | .03 |
| Employment | <.001 | |||
| Employed | 480 (50) | 63 (31) | 543 (47) | - |
| Unemployed | 53 (5.5) | 17 (8.3) | 70 (6.0) | - |
| Retired | 285 (30) | 64 (31) | 349 (30) | - |
| Unable to work (disabled) | 143 (15) | 62 (30) | 205 (18) | - |
| Difficulty paying billsd | 3 (2, 4) | 2 (2, 4) | 3 (2, 4) | <.001 |
| Difficulty paying bills category (%) | <.001 | |||
| Very difficult | 126 (13) | 44 (21) | 170 (15) | - |
| Somewhat difficult | 222 (23) | 70 (34) | 292 (25) | - |
| Not very difficult | 197 (21) | 28 (14) | 225 (19) | - |
| Not at all difficult | 410 (43) | 64 (31) | 474 (41) | - |
Note: BHLS = brief health literacy screen; ENRICHD = enhancing recovery in coronary heart disease; ESSI = ENRICHD social support instrument. For continuous variables, median (25%, 75%); for categorical variables, N (%). Wilcoxon Test for all continuous variables and Pearson Test for all categorical variables.
Subjective Numeracy Scale.
Single item question: “How difficult is it for you (and your family) to pay your monthly bills?” Responses were reverse coded and range: 1 = very difficult, 2 = not very difficult, 3 = somewhat difficult, or 4 = not at all difficult.
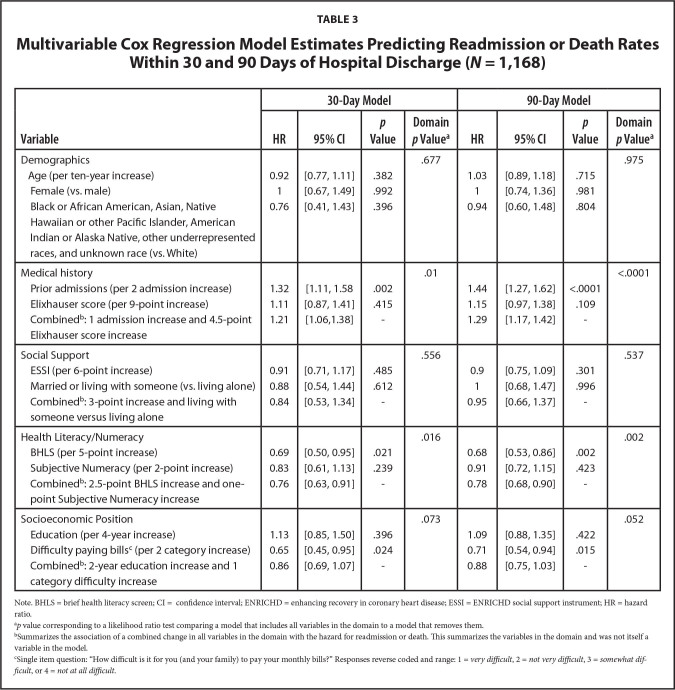
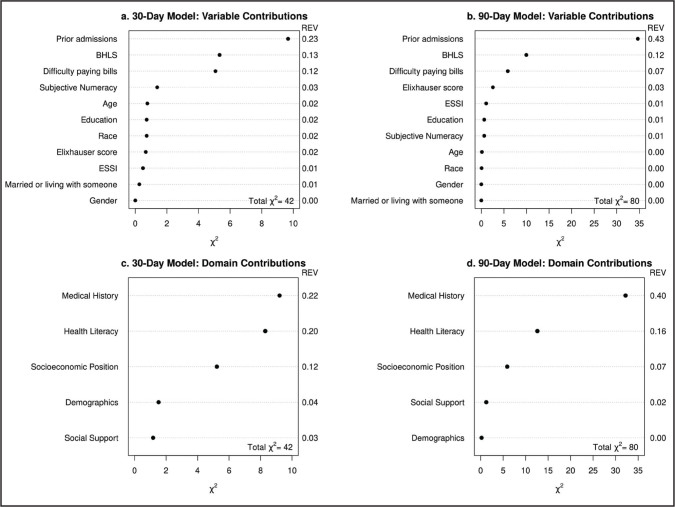
Table 3 shows results from the multivariable Cox models for the 30- and 90-day outcomes. We display estimated hazard ratios, 95% confidence intervals and p values for individual variable associations with instantaneous rates of readmission or death within 30 and 90 days of discharge. We also report likelihood ratio test p values corresponding to outcome associations with key domains (i.e., groups of variables) and hazard ratio and 95% confidence interval estimates to characterize outcome associations with simultaneous changes in multiple variables within the social support, health literacy, and SES domains. For the 30-day analysis, prior admissions were positively associated with readmission or death (HR = 1.32, 95% confidence interval [CI]: 1.11 − 1.58 per 2 prior admissions within the last year). The health literacy/numeracy domain was significantly associated with readmission or death (domain p = 0.016). A simultaneous increase in BHLS (2.5 points) and subjective numeracy (1 point) was associated with a hazard ratio of 0.76 (95% CI: 0.63 – 0.91). We did not observe an association between the social support or SES domains and readmission or death at 30 days after discharge. Figure 2 shows individual variable and domain associated Chi-Square statistics as well as a measure of relative explained variability. We observed that the health literacy/numeracy domain explains far more variability than either of the socioeconomic position and social support domains (Figures 2A and 2C), although medical history explained the most variability in time to readmission/death by 30 days post discharge.
Table 3.
Multivariable Cox Regression Model Estimates Predicting Readmission or Death Rates Within 30 and 90 Days of Hospital Discharge (N = 1,168)
| Variable | 30-Day Model | 90-Day Model | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| HR | 95% CI | p Value | Domain p Valuea | HR | 95% CI | p Value | Domain p Valuea | |
|
| ||||||||
| Demographics | .677 | .975 | ||||||
| Age (per ten-year increase) | 0.92 | [0.77, 1.11] | .382 | 1.03 | [0.89, 1.18] | .715 | ||
| Female (vs. male) | 1 | [0.67, 1.49] | .992 | 1 | [0.74, 1.36] | .981 | ||
| Black or African American, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, other underrepresented races, and unknown race (vs. White) | 0.76 | [0.41, 1.43] | .396 | 0.94 | [0.60, 1.48] | .804 | ||
|
| ||||||||
| Medical history | .01 | <.0001 | ||||||
| Prior admissions (per 2 admission increase) | 1.32 | [1.11, 1.58 | .002 | 1.44 | [1.27, 1.62] | <.0001 | ||
| Elixhauser score (per 9-point increase) | 1.11 | [0.87, 1.41] | .415 | 1.15 | [0.97, 1.38] | .109 | ||
| Combinedb: 1 admission increase and 4.5-point | 1.21 | [1.06,1.38] | - | 1.29 | [1.17, 1.42] | - | ||
| Elixhauser score increase | ||||||||
|
| ||||||||
| Social Support | .556 | .537 | ||||||
| ESSI (per 6-point increase) | 0.91 | [0.71, 1.17] | .485 | 0.9 | [0.75, 1.09] | .301 | ||
| Married or living with someone (vs. living alone) | 0.88 | [0.54, 1.44] | .612 | 1 | [0.68, 1.47] | .996 | ||
| Combinedb: 3-point increase and living with someone versus living alone | 0.84 | [0.53, 1.34] | - | 0.95 | [0.66, 1.37] | - | ||
|
| ||||||||
| Health Literacy/Numeracy | .016 | .002 | ||||||
| BHLS (per 5-point increase) | 0.69 | [0.50, 0.95] | .021 | 0.68 | [0.53, 0.86] | .002 | ||
| Subjective Numeracy (per 2-point increase) | 0.83 | [0.61, 1.13] | .239 | 0.91 | [0.72, 1.15] | .423 | ||
| Combinedb: 2.5-point BHLS increase and one-point Subjective Numeracy increase | 0.76 | [0.63, 0.91] | - | 0.78 | [0.68, 0.90] | - | ||
|
| ||||||||
| Socioeconomic Position | .073 | .052 | ||||||
| Education (per 4-year increase) | 1.13 | [0.85, 1.50] | .396 | 1.09 | [0.88, 1.35] | .422 | ||
| Difficulty paying billsc (per 2 category increase) | 0.65 | [0.45, 0.95] | .024 | 0.71 | [0.54, 0.94] | .015 | ||
| Combinedb: 2-year education increase and 1 category difficulty increase | 0.86 | [0.69, 1.07] | - | 0.88 | [0.75, 1.03] | - | ||
Note. BHLS = brief health literacy screen; CI = confidence interval; ENRICHD = enhancing recovery in coronary heart disease; ESSI = ENRICHD social support instrument; HR = hazard ratio.
p value corresponding to a likelihood ratio test comparing a model that includes all variables in the domain to a model that removes them.
Summarizes the association of a combined change in all variables in the domain with the hazard for readmission or death. This summarizes the variables in the domain and was not itself a variable in the model.
Single item question: “How difficult is it for you (and your family) to pay your monthly bills?” Responses reverse coded and range: 1 = very difficult, 2 = not very difficult, 3 = somewhat difficult, or 4 = not at all difficult.
Figure 2.
Individual variable and domain contributions to the explained variation in the time to readmission or death models. We report the Chi-square statistics and the relative explained variation (REV). REV was calculated by the Chi-square statistic contributed by each variable and each domain divided by the total Chi-square for the whole model.
The 90-day Cox proportional hazard model was similar to the 30-day model; however, due to the larger number of events by 90 days, confidence interval widths are smaller. Prior admissions were significantly associated with readmission or death (HR = 1.44, 95% CI: 1.27 − 1.62 per 2 prior admissions), and higher BHLS scores were associated with lower rates of readmission or death (HR = 0.68, 95% CI: 0.53 − 0.86 per 5-point change). Overall, the medical history and health literacy/numeracy domains were associated with 90-day readmission or death (domain, p < .0001 and p < .002, respectively), though the SES domain was marginally associated (domain, p = .052). A simultaneous increase in BHLS (2.5 points) and subjective numeracy (1 point) scores was associated with a hazard ratio of 0.78 (95% CI: 0.68 – 0.90), and a simultaneous increase in education (2 years) and difficulty paying bills (1 category increase) was associated with a hazard ratio of 0.88 (95% CI: 0.75 − 1.03), which was marginally significant. We observed in Figure 2 that medical history explained the most variability in time to readmission/death (Figures 2B and 2D), but that the health literacy/numeracy domain explained far more variability than socioeconomic position and social support domains.
Discussion
In this large cohort study of participants with ACS, we found complex associations between social determinants of health and post-discharge outcomes. After adjustment for prior health care utilization and medical comorbidities, the domain of health literacy/numeracy was independently associated with hospital readmission or death through 90 days post-discharge. SES was associated with outcomes in unadjusted analyses but was not statistically significant (p = 0.052 and p = .072) in adjusted analyses. Surprisingly, social support, measured in a variety of ways, was unrelated to readmission or death when adjusting for other factors. This research demonstrates that, when these common social determinants of health are considered together, health literacy/numeracy has the most dominant and consistent effect on the post-discharge outcomes examined.
Our findings have implications for the ongoing national dialogue on how social determinants of health affect hospital readmission rates and which factors may be most important to measure and address in hospitalized patients. Models for readmission vary in their predictive ability, depending on which types of variables are included. In our prior systematic review, we reported the majority of models used comorbidities and prior utilization to predict readmission with modest discrimination (c-statistics 0.6–0.77) (Kansagara et al., 2011). Interestingly, models that utilized administrative data as well as social determinants of health have demonstrated better predictive abilities. Yet, thus far there has been no agreement on what the most predictive social determinants of health are (Joynt et al., 2017). No published models have included health literacy, which our findings suggest is an important omission.
We found an independent association between health literacy/numeracy and outcomes among participants with ACS. Previously using data on participants from the same cohort who had acute decompensated heart failure (ADHF), we had also found health literacy was associated with greater medical complexity, including being admitted for ADHF for the index hospitalization and more hospitalizations in the prior year (Mayberry et al., 2018). Our prior finding supports the notion that health literacy has already exerted an effect on medical complexity which leads to readmissions and/or death. Moreover, the health literacy/numeracy domain is thought to affect post-discharge outcomes through effects on patients' self-management of their medical conditions. For example, medication use or ability to detect and respond to warning signs of clinical decompensation. The current results are consistent with other investigations which have demonstrated associations between health literacy and readmission rates for ACS (Kanejima et al., 2022; Mitchell et al., 2012). Further investigations into the mechanism by which health literacy/numeracy impacts self-management activities and risk for readmission are warranted for patients with cardiovascular disease. A few potential mediators particularly warranting study, which are known to be more common among patients with low health literacy/numeracy, are medication errors, medication nonadherence (particularly unintentional nonadherence), and missed follow-up appointments (Knolhoff et al., 2016; Lindquist et al., 2012; Mixon et al., 2014).
Our hypothesis that a=dverse post-discharge outcomes would be related to poorer social support was noted in unadjusted results at 90 days, but its effect was attenuated by other factors in the adjusted models, which was surprising. Being a widow(er) or nonmarried have also been associated previously with increased risk of mortality in ACS (Hadi Khafaji et al., 2012; Marcus et al., 2019). Perhaps the measures we utilized did not adequately capture the challenges patients with ACS face with regard to social support.
We examined the overall direct effects of the specified social determinants of health on readmissions and mortality. From the same cohort, we found that health literacy indirectly affects 1-year mortality via worse health behaviors, lower perceived health competence, and more medical complexity, including comorbidities and being admitted for ADHF, but not via social support (Mayberry et al., 2018). In the present analysis, we did not examine moderating variables, such as severity of illness; therefore, it may be premature to conclude that social support is not predictive of post-discharge outcomes. Among patients with severe illness, prognosis may be determined primarily by physiologic factors, whereas in patients with less severe illness, health literacy and numeracy may play a greater role in prognosis through their effect on self-management. At present, we maintain that assessing social determinants of health for patients is critical to providing appropriate and equitable care (Brandt et al., 2023), and they may manifest in other ways not measured here, ranging from patient satisfaction to medication safety. For example, health literacy sensitive materials should be used for patient discharge education as a commonsense approach (Glick et al., 2019; Wiggins et al., 2013). Additionally, social services and care transitions teams should determine hospitalized patients' social support to maximize success after discharge.
Study Strengths and Limitations
Our study's strengths include a large sample size including 38% women, minimal missing or incomplete data, multiple measures of health literacy and social support, and outcome assessment including data from any reported hospital. In fact, for the overall study 29% of first readmissions captured were to another facility. In contrast, we must consider the potential limitations. The participants came from one referral hospital, though they originated from more than 20 states. We excluded 2% of eligible patients from enrollment who lacked a stable phone number for follow up. These individuals might have experienced greater impact of social determinants of health on outcomes, so excluding them may bias our results toward the null. We focused on one health condition, ACS, so it is unclear how generalizable our results are to a wider hospitalized population. We had time horizons of 30- and 90-days follow-up for our readmissions and mortality data; however, these time points are relevant to current policies regarding readmission penalties and episodes of care. As with many psychosocial factors, mediating factors may influence the effect of social support and health literacy on outcomes (e.g. adherence, self-management), which we did not examine. We did not include environmental or neighborhood SES factors. Finally, the study relied on data from participant self-report, which is subject to reporting bias, although we used well-validated instruments, and patient-level social data are superior to community-level data (Kostelanetz et al., 2021).
Conclusion
In this cohort of participants hospitalized with ACS, we determined that health literacy/numeracy was significantly associated with readmission or mortality in the 30-to-90-day postdischarge period, when adjusting for other factors. Other social determinants of health were not consistently related to outcomes. Health literacy/numeracy warrant greater attention amidst growing national efforts to screen social determinants of health in hospital settings.
Acknowledgments
The authors acknowledge the work of coauthor Kenneth A. Wallston, PhD, who died October 27, 2020. The authors thank the study research analysts and project coordinators: Courtney Cawthon, Catherine Couey, Monika Rizk, Hannah Rosenberg, Daniel Lewis, Blake Hendrickson, Olivia Dozier, Vanessa Fuentes, Cardella Leak, Mary Lou Jacobsen, Catherine Evans, Joanna Lee, Emily Lucianno, and Erin Acord.
Funding Statement
Funding: This study was supported by grant R01 HL109388 from the National Heart, Lung, and Blood Institute and in part by grants UL1 TR000445-06 from the National Center for Advancing Translational Sciences, K23AG048347 from the Eisenstein Women's Heart Fund, and K23AG040157 from the National Institute on Aging. ASM was supported by a Veterans Affairs Health Services Research and Development Service Career Development Award at the Tennessee Valley Healthcare System, Department of Veterans Affairs (CDA 12-168).
References
- Aburadwan , M. K. , & Hayajneh , F. A. ( 2024. ). Health literacy among patients with acute coronary artery diseases: predictors, consequences, and enhancing strategies: A review of the literature . Critical Care Nursing Quarterly , 47 ( 1 ), 71 – 82 . 10.1097/CNQ.0000000000000492 PMID: [DOI] [PubMed] [Google Scholar]
- Adler , N. E. , Cutler , D. M. , Jonathan , J. E. , Galea , S. , Glymour , M. , Koh , H. K. , & Satcher , D . ( 2016. ). Addressing social determinants of health and health disparities . Discussion paper: Vital Directions for Health and Health Care Series. https://nam.edu/wp-content/uploads/2016/09/Addressing-Social-Determinants-of-Health-and-Health-Disparities.pdf
- Beauchamp , A. , Talevski , J. , Niebauer , J. , Gutenberg , J. , Kefalianos , E. , Mayr , B. , Sareban , M. , & Kulnik , S. T. ( 2022. ). Health literacy interventions for secondary prevention of coronary artery disease: A scoping review . Open Heart , 9 ( 1 ), e001895 . 10.1136/openhrt-2021-001895 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman , L. F. , Blumenthal , J. , Burg , M. , Carney , R. M. , Catellier , D. , Cowan , M. J. , Czajkowski , S. M. , DeBusk , R. , Hosking , J. , Jaffe , A. , Kaufmann , P. G. , Mitchell , P. , Norman , J. , Powell , L. H. , Raczynski , J. M. , Schneiderman , N. , & the Enhancing Recovery in Coronary Heart Disease Patients Investigators (ENRICHD) . ( 2003. ). Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial . Journal of the American Medical Association , 289 ( 23 ), 3106 – 3116 . 10.1001/jama.289.23.3106 PMID: [DOI] [PubMed] [Google Scholar]
- Berkman , N. D. , Sheridan , S. L. , Donahue , K. E. , Halpern , D. J. , & Crotty , K. ( 2011. ). Low health literacy and health outcomes: An updated systematic review. [pii] . Annals of Internal Medicine , 155 ( 2 ), 97 – 107 . 10.7326/0003-4819-155-2-201107190-00005 PMID: [DOI] [PubMed] [Google Scholar]
- Blake , S. C. , McMorris , K. , Jacobson , K. L. , Gazmararian , J. A. , & Kripalani , S. ( 2010. ). A qualitative evaluation of a health literacy intervention to improve medication adherence for underserved pharmacy patients . Journal of Health Care for the Poor and Underserved , 21 ( 2 ), 559 – 567 . 10.1353/hpu.0.0283 PMID: [DOI] [PubMed] [Google Scholar]
- Blumenthal , J. A. , Burg , M. M. , Barefoot , J. , Williams , R. B. , Haney , T. , & Zimet , G. ( 1987. ). Social support, type A behavior, and coronary artery disease . Psychosomatic Medicine , 49 ( 4 ), 331 – 340 . 10.1097/00006842-198707000-00002 PMID: [DOI] [PubMed] [Google Scholar]
- Brandt , E. J. , Tobb , K. , Cambron , J. C. , Ferdinand , K. , Douglass , P. , Nguyen , P. K. , Vijayaraghavan , K. , Islam , S. , Thamman , R. , Rahman , S. , Pendyal , A. , Sareen , N. , Yong , C. , Palaniappan , L. , Ibebuogu , U. , Tran , A. , Bacong , A. M. , Lundberg , G. , & Watson , K. ( 2023. ). Assessing and addressing social determinants of cardiovascular health: JACC state-of-the-art review . Journal of the American College of Cardiology , 81 ( 14 ), 1368 – 1385 . 10.1016/j.jacc.2023.01.042 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew , L. D. , Bradley , K. A. , & Boyko , E. J. ( 2004. ). Brief questions to identify patients with inadequate health literacy . Family Medicine , 36 ( 8 ), 588 – 594 PMID: [PubMed] [Google Scholar]
- Chiu , I. M. , Barbayannis , G. , Cabrera , J. , Cosgrove , N. M. , Kostis , J. B. , Sargsyan , D. , Kostis , W. J. , & the Myocardial Infarction Data Acquisition System (MIDAS 43) Study Group . ( 2022. ). Relation of socioeconomic status to 1-year readmission and mortality in patients with acute myocardial infarction . The American Journal of Cardiology , 175 , 19 – 25 . 10.1016/j.amjcard.2022.03.044 PMID: [DOI] [PubMed] [Google Scholar]
- Coleman , E. A. ( 2003. ). Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs . Journal of the American Geriatrics Society , 51 ( 4 ), 549 – 555 . 10.1046/j.1532-5415.2003.51185.x PMID: [DOI] [PubMed] [Google Scholar]
- Coleman , E. A. , Chugh , A. , Williams , M. V. , Grigsby , J. , Glasheen , J. J. , McKenzie , M. , & Min , S. J. ( 2013. ). Understanding and execution of discharge instructions . American Journal of Medical Quality , 28 ( 5 ), 383 – 391 . 10.1177/1062860612472931 PMID: [DOI] [PubMed] [Google Scholar]
- Daliri , S. , Bekker , C. L. , Buurman , B. M. , Scholte Op Reimer , W. J. M. , van den Bemt , B. J. F. , & Karapinar-Çarkit , F. ( 2019. ). Barriers and facilitators with medication use during the transition from hospital to home: A qualitative study among patients . BMC Health Services Research , 19 ( 1 ), 204 . 10.1186/s12913-019-4028-y PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eibergen , L. , Janssen , M. J. A. , Blom , L. , & Karapinar-Çarkit , F. ( 2018. ). Informational needs and recall of in-hospital medication changes of recently discharged patients . Research in Social & Administrative Pharmacy , 14 ( 2 ), 146 – 152 . 10.1016/j.sapharm.2017.01.006 PMID: [DOI] [PubMed] [Google Scholar]
- Fagerlin , A. , Zikmund-Fisher , B. J. , Ubel , P. A. , Jankovic , A. , Derry , H. A. , & Smith , D. M. ( 2007. ). Measuring numeracy without a math test: Development of the subjective numeracy scale . Medical Decision Making , 27 ( 5 ), 672 – 680 . 10.1177/0272989X07304449 PMID: [DOI] [PubMed] [Google Scholar]
- Ghisi , G. L. M. , Chaves , G. S. D. S. , Britto , R. R. , & Oh , P. ( 2018. ). Health literacy and coronary artery disease: A systematic review . Patient Education and Counseling , 101 ( 2 ), 177 – 184 . 10.1016/j.pec.2017.09.002 PMID: [DOI] [PubMed] [Google Scholar]
- Glick , A. F. , Brach , C. , Yin , H. S. , & Dreyer , B. P. ( 2019. ). Health literacy in the inpatient setting: Implications for patient care and patient safety . Pediatric Clinics of North America , 66 ( 4 ), 805 – 826 . 10.1016/j.pcl.2019.03.007 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golbeck , A. L. , Ahlers-Schmidt , C. R. , Paschal , A. M. , & Dismuke , S. E. ( 2005. ). A definition and operational framework for health numeracy . American Journal of Preventive Medicine , 29 ( 4 ), 375 – 376 . S0749-3797(05)00257-6[pii] 10.1016/j.amepre.2005.06.012 PMID: [DOI] [PubMed] [Google Scholar]
- Guo , P. , & Harris , R. ( 2016. ). The effectiveness and experience of self-management following acute coronary syndrome: A review of the literature . International Journal of Nursing Studies , 61 , 29 – 51 . 10.1016/j.ijnurstu.2016.05.008 PMID: [DOI] [PubMed] [Google Scholar]
- Hadi Khafaji , H. A. , Al Habib , K. , Asaad , N. , Singh , R. , Hersi , A. , Al Falaeh , H. , Al Saif , S. , Al-Motarreb , A. , Almahmeed , W. , Sulaiman , K. , Amin , H. , Al-Lawati , J. , Al-Sagheer , N. Q. , Alsheikh-Ali , A. A. , & Al Suwaidi , J. ( 2012. ). Marital status and outcome of patients presenting with acute coronary syndrome: An observational report . Clinical Cardiology , 35 ( 12 ), 741 – 748 . 10.1002/clc.22034 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardman , R. , Begg , S. , & Spelten , E. ( 2020. ). What impact do chronic disease self-management support interventions have on health inequity gaps related to socioeconomic status: A systematic review . BMC Health Services Research , 20 ( 1 ), 150 . 10.1186/s12913-020-5010-4 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell , F. E. ( 2016. ). Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis ( 2nd ed. ). Springer Cham; ., 10.1007/978-3-319-19425-7 [DOI] [Google Scholar]
- Harrell , F. E. , Jr. ( 2021. ). rms: Regression modeling strategies (version R package 6.2-0) . https://CRAN.R-project.org/package=rms
- Harris , C. M. , Sridharan , A. , Landis , R. , Howell , E. , & Wright , S. ( 2013. ). What happens to the medication regimens of older adults during and after an acute hospitalization? Journal of Patient Safety , 9 ( 3 ), 150 – 153 . 10.1097/PTS.0b013e318286f87d PMID: [DOI] [PubMed] [Google Scholar]
- Horwitz , L. I. , Chang , C. , Arcilla , H. N. , & Knickman , J. R. ( 2020. ). Quantifying health systems' investment in social determinants of health, by sector, 2017–19 . Health Affairs , 39 ( 2 ), 192 – 198 . 10.1377/hlthaff.2019.01246 PMID: [DOI] [PubMed] [Google Scholar]
- Joynt , K. E. , De Lew , N. , Sheingold , S. H. , Conway , P. H. , Goodrich , K. , & Epstein , A. M. ( 2017. ). Should Medicare value-based purchasing take social risk into account? The New England Journal of Medicine , 376 ( 6 ), 510 – 513 . 10.1056/NEJMp1616278 PMID: [DOI] [PubMed] [Google Scholar]
- Juster , F. T. , & Suzman , R. ( 1995. ). An overview of the health and retirement survey . The Journal of Human Resources , 30 ( suppl ), S7 – S56 . 10.2307/146277 [DOI] [Google Scholar]
- Kanejima , Y. , Shimogai , T. , Kitamura , M. , Ishihara , K. , & Izawa , K. P. ( 2022. ). Impact of health literacy in patients with cardiovascular diseases: A systematic review and meta-analysis . Patient Education and Counseling , 105 ( 7 ), 1793 – 1800 . 10.1016/j.pec.2021.11.021 PMID: [DOI] [PubMed] [Google Scholar]
- Kansagara , D. , Englander , H. , Salanitro , A. , Kagen , D. , Theobald , C. , Freeman , M. , & Kripalani , S. ( 2011. ). Risk prediction models for hospital readmission: A systematic review . Journal of the American Medical Association , 306 ( 15 ), 1688 – 1698 . 10.1001/jama.2011.1515 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khera , R. , Jain , S. , Pandey , A. , Agusala , V. , Kumbhani , D. J. , Das , S. R. , Berry , J. D. , de Lemos , J. A. , & Girotra , S. ( 2017. ). Comparison of readmission rates after acute myocardial infarction in 3 patient age groups (18 to 44, 45 to 64, and ≥65 years) in the United States . The American Journal of Cardiology , 120 ( 10 ), 1761 – 1767 . 10.1016/j.amjcard.2017.07.081 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- King , L. , Harrington , A. , Nicholls , S. , Thornton , K. , & Tanner , E. ( 2023. ). Towards reduction of preventable hospital readmission: Older people and family members' views on planned self-management of care at home . Journal of Clinical Nursing , 32 ( 15–16 ), 4599 – 4613 . 10.1111/jocn.16492 PMID: [DOI] [PubMed] [Google Scholar]
- Knolhoff , J. B. , Djenic , B. , Hsu , C. H. , Bouton , M. E. , & Komenaka , I. K. ( 2016. ). Missed appointments in a breast clinic: Patient-related factors . The American Journal of the Medical Sciences , 352 ( 4 ), 337 – 342 . 10.1016/j.amjms.2016.07.003 PMID: [DOI] [PubMed] [Google Scholar]
- Kostelanetz , S. , Di Gravio , C. , Schildcrout , J. S. , Roumie , C. L. , Conway , D. , & Kripalani , S. ( 2021. ). Should we implement geographic or patient-reported social determinants of health measures in cardiovascular patients . Ethnicity & Disease , 31 ( 1 ), 9 – 22 . 10.18865/ed.31.1.9 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindquist , L. A. , Go , L. , Fleisher , J. , Jain , N. , Friesema , E. , & Baker , D. W. ( 2012. ). Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge medications . Journal of General Internal Medicine , 27 ( 2 ), 173 – 178 . 10.1007/s11606-011-1886-3 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus , G. , Litovchik , I. , Pereg , D. , Beigel , R. , Sholmo , N. , Iakobishvili , Z. , Goldenberg , I. , Fuchs , S. , & Minha , S. ( 2019. ). Impact of marital status on the outcome of acute coronary syndrome: Results from the acute coronary syndrome Israeli survey . Journal of the American Heart Association , 8 ( 14 ), e011664 . 10.1161/JAHA.118.011664 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberry , L. S. , Schildcrout , J. S. , Wallston , K. A. , Goggins , K. , Mixon , A. S. , Rothman , R. L. , & Kripalani , S. V. I. C. S. ( 2018. ). Health literacy and 1-year mortality: Mechanisms of association among adults hospitalized for cardiovascular disease . Mayo Clin Proc 2018, Online First (Nov 7). 10.1016/j.mayocp.2018.07.024 [DOI] [PMC free article] [PubMed]
- McNaughton , C. D. , Cavanaugh , K. L. , Kripalani , S. , Rothman , R. L. , & Wallston , K. A. ( 2015. ). Validation of a short, 3-item version of the subjective numeracy scale . Medical Decision Making , 35 ( 8 ), 932 – 936 . 10.1177/0272989X15581800 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton , C. D. , Cawthon , C. , Kripalani , S. , Liu , D. , Storrow , A. B. , & Roumie , C. L. ( 2015. ). Health literacy and mortality: A cohort study of patients hospitalized for acute heart failure . Journal of the American Heart Association , 4 ( 5 ), e001799 . 10.1161/JAHA.115.001799 PMID: . Erratum for: J Am Heart Assoc . 2015. ; 4 ( 6 ): e000682 . doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers , A. G. , Salanitro , A. , Wallston , K. A. , Cawthon , C. , Vasilevskis , E. E. , Goggins , K. M. , Davis , C. M. , Rothman , R. L. , Castel , L. D. , Donato , K. M. , Schnelle , J. F. , Bell , S. P. , Schildcrout , J. S. , Osborn , C. Y. , Harrell , F. E. , & Kripalani , S. ( 2014. ). Determinants of health after hospital discharge: Rationale and design of the Vanderbilt In-patient Cohort Study (VICS) . BMC Health Services Research , 14 , 10 . 10.1186/1472-6963-14-10 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell , S. E. , Sadikova , E. , Jack , B. W. , & Paasche-Orlow , M. K. ( 2012. ). Health literacy and 30-day post discharge hospital utilization . Journal of Health Communication , 17 ( Suppl. 3 ), 325 – 338 . 10.1080/10810730.2012.715233 PMID: [DOI] [PubMed] [Google Scholar]
- Mixon , A. S. , Myers , A. P. , Leak , C. L. , Lou Jacobsen , J. M. , Cawthon , C. , Goggins , K. M. , Nwosu , S. , Schildcrout , J. S. , Schnelle , J. F. , Speroff , T. , & Kripalani , S. ( 2014. ). Characteristics associated with post discharge medication errors . Mayo Clinic Proceedings , 89 ( 8 ), 1042 – 1051 . 10.1016/j.mayocp.2014.04.023 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute . ( 2000. ). Morbidity and mortality: chartbook on cardiovascular, lung, and blood diseases . https://archive.org/details/morbiditymortali00nati_1/page/n7/mode/2up [Google Scholar]
- Osborn , C. Y. , Kripalani , S. , Goggins , K. M. , & Wallston , K. A. ( 2017. ). Financial strain is associated with medication nonadherence and worse self-rated health among cardiovascular patients . Journal of Health Care for the Poor and Underserved , 28 ( 1 ), 499 – 513 . 10.1353/hpu.2017.0036 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . ( 2022. ). R: A language and environment for statistical computing (version 4.1.3) . R Foundation for Statistical Computing; . [Google Scholar]
- Rossi , A. S. ( 2004. ). Social responsibility to family and community . In Brim O. G. , Ryff C. D. , & Kessler R. C. (Eds.), How healthy are we? A national study of well-being at midlife (pp. 550 – 585 ). University of Chicago Press; . [Google Scholar]
- Rubin , D. B. , & Schenker , N. ( 1991. ). Multiple imputation in healthcare databases: An overview and some applications . Statistics in Medicine , 10 ( 4 ), 585 – 598 . 10.1002/sim.4780100410 PMID: [DOI] [PubMed] [Google Scholar]
- Salyer , J. , Schubert , C. M. , & Chiaranai , C. ( 2012. ). Supportive relationships, self-care confidence, and heart failure self-care . The Journal of Cardiovascular Nursing , 27 ( 5 ), 384 – 393 . 10.1097/JCN.0b013e31823228cd PMID: [DOI] [PubMed] [Google Scholar]
- Schultz , B. E. , Corbett , C. F. , & Hughes , R. G. ( 2022. ). Instrumental support: A conceptual analysis . Nursing Forum , 57 ( 4 ), 665 – 670 . 10.1111/nuf.12704 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling , M. R. , Safford , M. M. , Goggins , K. , Nwosu , S. K. , Schildcrout , J. S. , Wallston , K. A. , Mixon , A. S. , Rothman , R. L. , & Kripalani , S. ( 2018. ). Numeracy, health literacy, cognition, and 30-day readmissions among patients with heart failure . Journal of Hospital Medicine , 13 ( 3 ), 145 – 151 . 10.12788/jhm.2932 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- The ENRICHD investigators . ( 2000. ). Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods . American Heart Journal , 139 ( 1 Pt 1 ), 1 – 9 . S0002870300594150 [pii] [DOI] [PubMed] [Google Scholar]
- Therneau , T . ( 2021. ). A package for survival analysis in R (version R package 3.2-13) . https://CRAN.R-project.org/package=survival
- van Walraven , C. , Austin , P. C. , Jennings , A. , Quan , H. , & Forster , A. J. ( 2009. ). A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data . Medical Care , 47 ( 6 ), 626 – 633 . 10.1097/MLR.0b013e31819432e5 PMID: [DOI] [PubMed] [Google Scholar]
- Wallston , K. A. , Cawthon , C. , McNaughton , C. D. , Rothman , R. L. , Osborn , C. Y. , & Kripalani , S. ( 2014. ). Psychometric properties of the brief health literacy screen in clinical practice . Journal of General Internal Medicine , 29 ( 1 ), 119 – 126 . 10.1007/s11606-013-2568-0 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins , B. S. , Rodgers , J. E. , DiDomenico , R. J. , Cook , A. M. , & Page , R. L. , II . ( 2013. ). Discharge counseling for patients with heart failure or myocardial infarction: A best practices model developed by members of the American College of Clinical Pharmacy's cardiology practice and research network based on the hospital to home (H2H) initiative . Pharmacotherapy , 33 ( 5 ), 558 – 580 . 10.1002/phar.1231 PMID: [DOI] [PubMed] [Google Scholar]
- World Health Organization . ( 2019. ). Medication safety in transitions of care . https://www.who.int/publications/i/item/WHO-UHCSDS-2019.9 [Google Scholar]