Abstract
Objective
We aimed to determine anatomic features of the temporal branch (TB) of the facial nerve and its relation to various anatomic landmarks on the face in order to prevent damage in the surgical approach after head trauma or in planned neurosurgical interventions.
Methods
Nine male cadavers preserved with formalin, were bilaterally dissected under a microscope at the laboratory of anatomy department of the university. The anatomical features of the branch and branching pattern of facial nerve and its relationships with adjacent neurovascular structures were evaluated using descriptive statistical data.
Results
The mean distance at the lateral canthus level between the far most anterior branch and far most posterior branch of the TB (APD) was 14.93 mm. The mean distance to the tragus of the entrance point of the TB to the orbicularis oculi muscle (ETT) was 74.72 mm. The mean distance between the origin point of the TB to the tragus (TT) was 24.50 mm. The angle between the far most anterior branch and far most posterior branch at the level of the lateral canthus (APA) was minimum 15°, maximum 40° and the mean value of APA was 24.61°. The number of branches originating from the TB (NB) were one to three branches which lay under the zygomatic arch and two to five branches upper the zygomatic arch, respectively. The number of anastomosis between the TB and zygomatic branch (AN) varies between 1 and 4; AN was found to be less intense in 10 sides and very intense in eight sides.
Conclusion
The APA and APD value is mentioned for the first time in this study and nerve angle is considered to be as important as temporal branching in directing facial neurosurgical operations. We found that the unsafety zone may be exist for a 40 degree and 1.5 cm long area at the lateral canthus level, especially on the zygomatic arc where branching pattern is greater and 2.5 cm in front of the tragus. The data is significant for neurosurgeons to reach exactly this area without causing postoperative complications such as facial paralysis.
Keywords: Facial nerve, Anatomy, Cadavers, Neurosurgery
INTRODUCTION
The temporal branch (TB) of the facial nerve (FN) diverges from the main trunk below the zygomatic arch within the substance of the parotid gland and tracks superiorly and anteriorly, splitting into three to five rami. The TB innervates the upper orbicularis oculi, the frontalis, the corrugator supercilii, and the temporoparietalis muscles [6,29,35].
The temporal region is of significance in respect to many traumatic and elective surgical procedure due to the complexity of the facial plans covering the FN [22,25,32]. During brain surgery operations performed in the temporal region, this nerve branch may be protected or damaged, depending on the method chosen by the surgeon. The TB may be damaged during frontotemporal craniotomy and postoperative facial palsy may occur due to this reason [16]. The temporal area intervention to the anterior aspect of the circle of Willis for surgical approach of anterior circulation aneurysms causes damage of the TB. Therefore, it is quite difficult to prevent from nerve injury during the neurosurgical intervention [3,41].
Pterional craniotomy technique may injure the TB during intracranial aneurysm operations, and may cause paralysis of the frontalis, orbicularis oculi, and corrugator muscles. The technique may also result in paralysis of the upper eyelid, and facial lack of symmetry [14,39].
The most serious complication of a coronal incision is the injury to the TB, especially during lateral extension for exposing zygomatic arch [11,19,24]. The TB is also of importance during neurosurgical operations to access the lateral part of the anterior and middle cranial fossae using the transzygomatic approach [1,30]. During orbitozygomatic temporopolar intervention, protection of the TB is very significant in neurosurgical approach [16]. Dissecting the TB might be avoided by defining the crossing point of the TB on the upper margin of the zygomatic arch [34].
Therefore, a comprehensive understanding of its course is critical to reduce the chance of damage to the nerve. Several studies have been conducted to define the course of the TB and to propose strategies to protect it [12,13,18,20,27,28,36,37]. A significant variability in the course of the TB has been reported previously [27]. Knowledge about the detailed anatomy of the TB and its relations with the surrounding structures is beneficial to obtain the safe intervention of tissue and the protection of damage [32].
In the present study, we aimed to determine anatomical features and measurements of the TB such as origin points, localization, anastomotic and branching patterns and also reference bony landmarks which are the essential anatomical landmarks of our investigation.
MATERIALS AND METHODS
This research was conducted on approved cadavers in the research laboratory at Dokuz Eylül University Faculty of Medicine, Department of Anatomy. Department permission and permissions for cadaver use have been obtained and sent beforehand.
Nine male cadavers fixed with formalin, were bilaterally dissected using a stereomicroscope (Zeiss. OPMI-PICO/S 100; Zeiss, Jena, Germany) at the anatomy department laboratory of the university faculty of medicine. Ethical approval was not obtained for this study, because only cadaveric material was used. The age and sex of the cadavers were unknown (the ages of only two male cadavers were known : 25 and 75 years. The ages of the other seven cadavers were not known), and none of the cadavers were abnormally deformed from previous surgery or trauma. The findings were recorded as descriptive statistics data. The lack of data on female gender in our study was noted as a limitation of our study.
The FN trunk was identified at the stylomastoid foramen, and the TB of the FN and also the surrounding tissue were visualized and traced distally under the operating microscope. Following parameters were measured and evaluated: NB, number of the branches of the TB; APD, the distance at the lateral canthus level between the far most anterior branch and far most posterior branch of the TB; APA, the angle between the far most anterior branch and far most posterior branch at the level of the lateral canthus; Dx, the distance of the point where the top TB branch enters the orbicularis oculi muscle (OOM) to the x coordinate line passing through the lateral canthus; Dy, the distance of the point where the top TB branch enters the OOM to the y coordinate line passing through the lateral canthus; ETT, the distance to the tragus of the entrance point of the TB to the OOM; TT, the distance between the origin point of the TB to the tragus; AN, the number and/or intensity of anastomoses between the TB and zygomatic branch (Figs. 1 and 2). AN less than three was accepted as ‘less intense’, and 3 or more were accepted as ‘very intense’. Evaluations were carried out for NB (originating from the TB) under the zygomatic arch and over the zygomatic arch.
Fig. 1.
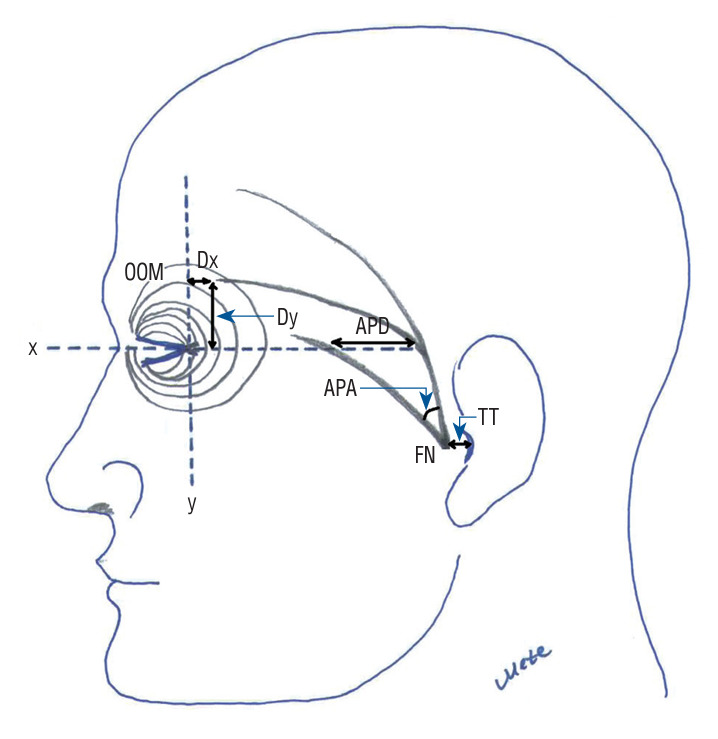
A representative image showing the temporal branch of the facial nerve. OOM : orbicularis oculi muscle, Dx : the distance to the x coordinate line passing from the lateral canthus, Dy : the distance to the y coordinate line passing from the lateral canthus, APD : the distance at the lateral canthus level between the far most anterior branch and far most posterior branch, APA : the angle between the far most anterior branch and far most posterior branch, FN : facial nerve, TT : the distance between the origin point of the temporal branch to the tragus.
Fig. 2.
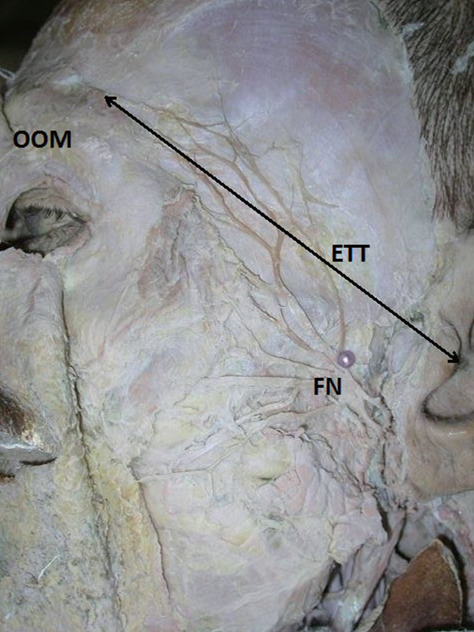
A cadaver image showing the dissection of the facial nerve. OOM : orbicularis oculi muscle, ETT : the direct distance to the tragus of the entrance point of the temporal branch to the orbicularis oculi muscle, FN : facial nerve.
The distances between bony landmarks were measured using a digital Vernier caliper (Mitutoyo, Kawasaki, Japan) accurate to 0.01 mm. A protractor was used for measuring the angles. Data was statistically evaluated via SPSS ver. 22.0 (IBM Corp, Armonk, NY, USA). Descriptive analysis were carried out after completing dissections and taking measurements.
RESULTS
The distance between anatomical landmarks with TB were shown in Table 1. The angle between the far most anterior branch and far most posterior branch at the level of the lateral canthus (APA) was minimum 15°, maximum 40° and the mean value of APA was 24.61°. The number of branches originating from the TB (NB) were one to three branches which lay under the zygomatic arch and two to five branches upper the zygomatic arch, respectively. The number of anastomosis between the TB and zygomatic branch (AN) varies between 1 and 4; AN was found to be less intense in 10 sides and very intense in eight sides. When the right and left sides of the same patient were compared, no statistically significant difference was detected. Again, no significant difference was found when all right (n=9) and left (n=9) subjects were compared with each other.
Table 1.
Descriptive statistical data between the temporal branch with the neighbor orientation points
| Measurements related to temporal branch (mm) (n=18) | Minimum (mm) | Maximum (mm) | Mean (mm) |
|---|---|---|---|
| APD | 7.90 | 22.00 | 14.93 |
| Dx | 10.70 | 30.40 | 16.74 |
| Dy | 7.00 | 23.30 | 16.10 |
| ETT | 56.10 | 99.80 | 74.72 |
| TT | 18.28 | 31.50 | 24.50 |
APD : the distance at the lateral canthus level between the far most anterior branch and far most posterior branch of the TB, Dx : the distance of the point where the top TB branch enters the orbicularis oculi muscle to the x coordinate line passing through the lateral canthus, Dy : the distance of the point where the top TB branch enters the orbicularis oculi muscle to the y coordinate line passing through the lateral canthus, ETT : the distance to the tragus of the entrance point of the temporal branch to the orbicularis oculi muscle, TT : the distance between the origin point of the temporal branch to the tragus, n : number of cases, bilaterally
DISCUSSION
The TB has not been clearly and detailed identified in the literature. In a few studies implied the termination of frontal branch, which is also used instead of the TB [4,9,12,13,17,31,33,36,38]. Pitanguy and Ramos [28] called the TB as temporofrontal branch. In a recent study, classical TB described and termed as temporofacial trunk and it was defined to give off the temporal and frontal branches. Also, the frontal branch which was originated from this trunk defined as to innervate expression muscles in the fronto-orbital region [7].
However, all this knowledge regarding the terminology and nomenclature of the TB of the FN has not been recorded in Terminology Anatomica [10]. For clinical arenas and anatomy, a novel agreement on the terminology and nomenclature is needed. In the present study, we used to term this branch as ‘the temporal branch’ in order to base current and classical terminology.
Several authors have reported an average number of three rami of TB (or frontal branch) [4,9,12,13,17,28,31,33,36]. Ammirati et al. [1] defined the TB pierces the parotidomasseteric fascia usually below the zygomatic arch and then directly divides into its terminal rami as the anterior, middle, and posterior. The anterior ramus reaches the corrugator supercilii and OOMs and innervates them. The middle ramus named as frontal ramus innervates the frontalis muscle. The posterior ramus does not carry any objective significance in human [1]. Pekar et al. [26] defined the same classification of TB as Ammirati et al. [1], but differently they noted the posterior branch innervates the anterior and the superior auricular and the tragus muscles. Some authors produced that there are three rami of the TB of the FN within the galeal plane of the scalp as the auricularis, frontalis, and orbicularis [5]. Sabini et al. [29] determined the TB of the FN to consist of no less than two branches. Farahvash et al. [8] declareted that the TBs on the zygomatic arch numbered as 1 to 3. Tzafetta and Terzis [38] and Hwang [15] found that the number of the TBs varied from two to four. The authors claimed that this diversity might play important role in the complexity of facial motion and the orchestration of a significant number of paired muscles [15,38]. de Bonnecaze et al. [7] reported that the TB often divides into two, three or four distinct branches. Gosain et al. [13] suggested that the rami of the TB were counted as 2–4 at the lower margin of the zygomatic arch and 2–5 at the upper margin of the zygomatic arch in the study. The results are similar to our study data. But differently, we observed one to three branches which lay under the zygomatic arch and two to five branches upper the zygomatic arch. Lans et al. [21] defined two to five TBs arising from the FN trunk. Their results are similar with notifications from the other publications. When compared with the cadaver studies by Ishikawa [17], Tzafetta and Terzis [38], and Hwang [15], they found that the branches to the corrugator supercilii muscle (CSM) and run below to the uppermost TB of the FN. The branches supply the OOM and the medial portion of the frontalis muscle [15,17,21,38].
Yaşargil et al. [40] defined three rami of the TB of the FN, with the middle which innervate to the frontalis muscle and anterior to the orbicularis oculi and CSMs, rami running in the hypodermic tissue over the zygomatic arch, 1 cm ventral to the superficial temporal artery. The third ramus called as posterior innervates to the anterior and superior auricular and tragus muscles [1].
Zani et al. [41] announced that the TBs above the zygomatic arch are quite thin and this causes injury of the nerves. Number of the TBs was between 1–4 [41]. In the present study we found that 2 to 5 of the TBs lay above the zygomatic arch e also found the rami of the TB vary between one to five branches. Additionally, we observed that when TB had five branches, this always took place at the region above the zygomatic arch. In this study, as the TB crosses the zygomatic arch, the nerve gives off multiple distinct branches, anastomosing with one another as they coursed superiorly. This multiplicity of branches is consistent with the findings of other authors [2,13,29] and differs notably from those reported by Pitanguy and Ramos [28], who defined a single branch. Sabini et al. [29] found an extension of a ramus posterior to the anterior hairline in eight of 12 sides. This finding is in contradiction to our study and Furnas [12], who noted that the area behind the temporal hairline was safe for dissection.
The course of the TB can be estimated using external landmarks as described by Pitanguy and Ramos [28]. An imaginary line starting from a point 0.5 cm below the tragus in the direction of the eyebrow, passing 1.5 cm above the lateral extremity of the eyebrow estimates the path of the nerve in the soft tissue [28]. In another anatomical study, Pérez-Rull et al. [27] reported their results as easy reference points available both superficially and in the depths, allowing a simple, non-complicated localization of the TB and its anastomosis in a precise manner on the mandibular condyle, the zygomatic arch and the temporal region. In this study, we used useful landmarks such as, zygomatic arch, OOM and lateral canthus.
There are limited numbered publication regarding relationship between the TB and the supraorbital keyhole intervention in neurosurgical approach (SOKA). Several authors claimed that SOKA does not impress the TBs and by this may not result in facial paralysis, although there have been patients with temporary or permanent loss of forehead wrinkling representing that SOKA has the potential to injury the frontalis muscle branch of the TB. Lin et al. [23] measured distance between the anterior ramus of the TB and the zygomatic process of the frontal bone as 19.5±3.6 mm. Their result indicates that if the incision is made more than 13 mm lateral to the zygomatic process, there is a risk of injury to the frontalis muscle branch, which arises from the anterior ramus of the TB [23].
Lans et al. [21] measured the distance between the inferior TB and the lateral orbital border 15 to 26 mm. Furnas [12] suggests to stay superior part of the temporal root of the zygoma, 1 cm dorsal and superior to the ventral hairline at the zygomatic arch, and 2 cm dorsal and superior to the lateral margin of the eyebrow during surgical operation. Pitanguy and Ramos [28] used an imaginary line binding a point 0.5 cm below the tragus with a point 1.5 cm above the lateral limbs of the eyebrow to assign a target point the course of the TB of the FN. Correia Pde and Zani [4] located the TB of the FN in a region marked by two distinct imaginary lines lengthening from the earlobe to the lateral end of the eyebrow and to the supreme forehead wrinkle. Bernstein and Nelson [2] studied the course of the TB of the FN and defined that “the TB of the FN locates within an area bounded by an imaginary line from the earlobe to the lateral margin of the eyebrow inferiorly and a second imaginary line from the tragus to the lateral coronal suture just above and behind the supreme forehead wrinkle.”
Ammirati et al. [1] found that the point where the TB, which delivers the anterior and middle rami, is lied 1.1 cm as mean value below the reference line as range between 0.5 and 1.9 cm and mean 2.4 cm ventral to the tragus as range between 1.5 and 3.5 cm. The point where the topmost branch of the TB pierces the galea aponeurotica to reach the frontalis muscle is located mean 2.4 cm above the reference line as range between 1.0–3.7 cm and mean 1.5 cm dorsal to the lateral canthus as range between 0.5–3.6 cm [1]. Schmidt et al. [33] and Hwang [15] also defined that the TBs toward the OOM run superiorly 1.50 to 3.74 cm the lateral canthus. Hwang [15] found that the highest level of the branches of the TB that inserted the OOM on the x axis and the y axis with the origin of the lateral canthus is 2.51 ±0.23 cm and 2.70±0.35 cm. Our findings were not similar their values (Dx 16.74±4.76 mm and Dy 16.10±4.14 mm). This difference may base on distinct geographic population and regional features. Farahvash et al. [8] found that distance from the most proximate branch of the TB to the tragus was 20.62±3.84 mm on the right and 21.33±3.10 mm on the left. Similarly, we measured the distance between the origin point of the TB to the tragus and the nerve as 24.50±3.60 mm in our study.
The FN and its’ branches are of significance for many surgical operations. TB is one of the five branches of the FN and its’ injury results in serious cosmetic problems because of its’ relatively long course and little number of terminal rami and no anastomoses with other branches of FN [6]. The rami of the TB are most at risk as they cross the zygomatic arch. The most dangerous and vulnerable area for the TB of the FN described as over the zygomatic arch and temple. The reason for this is here the nerves are very superficial, their depth are only as far as the skin and the thin superficial temporalis fascia component of the SMAS. Damage of the TB of the FN results in clinically significant paralysis of the frontalis, orbicularis oculi, and CSMs [1].
There are limited numbered publication regarding relationship between the TB and the supraorbital keyhole intervention in neurosurgical approach (SOKA). Several authors claimed that SOKA does not impress the TBs and by this may not result in facial paralysis, although there have been patients with temporary or permanent loss of forehead wrinkling representing that SOKA has the potential to injury the frontalis muscle branch of the TB. Lin et al. [23] measured distance between the anterior ramus of the TB and the zygomatic process of the frontal bone as 19.5±3.6 mm. Their result indicates that if the incision is made more than 13 mm lateral to the zygomatic process, there is a risk of injury to the frontalis muscle branch, which arises from the anterior ramus of the TB [23].
Dahlke and Murray [6] suggested that, an area as a danger zone can be approximated by drawing a line from the tragus to a lateral point along the highest forehead wrinkle and a line from the earlobe to the lateral eyebrow. Between these two lines, over the zygomatic arch and the temple, is the danger zone where damage to the temporal nerve is most likely to occur. The branches of FN innervate the muscles from the deep surface; thus, the nerves are protected distally by the muscle mass during superficial skin surgeries. This is evident along the medial portion of the zygomatic arch, where motor nerves are protected by the OOM [6]. de Bonnecaze et al. [7] considered that there is no exact anatomical safety field in the temporal region for surgical intervention in their study.
In the present study, we observed the number of branches of the TB as higher over the zygomatic arch and we measured the angle between the far most anterior and the far most posterior branches of the TB to vary between 15–40°. In the light of our findings, it is possible to describe a ‘danger zone’ located over the zygomatic arch (especially where TB gives off more branches). It can be described as the danger zone is within 40° angle consisted of two intersecting lines, the first is the vertical line 2.5 cm anterior to tragus and second line towards to OOM. In the light of this knowledge, the unsafety zone may be exist for a 40 degree and 1.5 cm long area at the lateral canthus level, especially on the zygomatic arc where branching pattern is greater and 2.5 cm in front of the tragus.
CONCLUSION
The APA and APD value are mentioned for the first time in this study and nerve angle is considered to be as important as temporal branching in directing facial neurosurgical operations. The data is significant for neurosurgeons to reach exactly this area without causing postoperative complications such as facial paralysis. Additionally, the results of this study are also useful during common surgical practices such as neurosurgical approach to access the lateral part of the anterior and middle cranial fossae by using the trans zygomatic intervention and contralateral neurotomy for frontal symmetry. We hope this manuscript will be a useful learning resource for surgical students and can guide surgeons to avoid TB damage.
Footnotes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : FA, SK; Data curation : FA, SK; Formal analysis : NGK; Funding acquisition : FA, SK, NGK; Methodology : FA, SK; Project administration : FA, SK; Visualization : FA, SK, NGK; Writing - original draft : FA, SK; Writing - review & editing : FA, SK, NGK
Data sharing
None
Preprint
None
References
- 1.Ammirati M, Spallone A, Ma J, Cheatham M, Becker D. An anatomicosurgical study of the temporal branch of the facial nerve. Neurosurgery. 1993;33:1038–1043. doi: 10.1227/00006123-199312000-00012. discussion 1044. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein L, Nelson RH. Surgical anatomy of the extraparotid distribution of the facial nerve. Arch Otolaryngol. 1984;110:177–183. doi: 10.1001/archotol.1984.00800290041009. [DOI] [PubMed] [Google Scholar]
- 3.Chehrazi BB. A temporal transsylvian approach to anterior circulation aneurysms. Neurosurgery. 1992;30:957–961. doi: 10.1227/00006123-199206000-00029. [DOI] [PubMed] [Google Scholar]
- 4.Correia Pde C, Zani R. Surgical anatomy of the facial nerve, as related to ancillary operations in rhytidoplasty. Plast Reconstr Surg. 1973;52:549–552. doi: 10.1097/00006534-197311000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Coscarella E, Vishteh AG, Spetzler RF, Seoane E, Zabramski JM. Subfascial and submuscular methods of temporal muscle dissection and their relationship to the frontal branch of the facial nerve. Technical note. J Neurosurg. 2000;92:877–880. doi: 10.3171/jns.2000.92.5.0877. [DOI] [PubMed] [Google Scholar]
- 6.Dahlke E, Murray CA. Facial nerve danger zone in dermatologic surgery: temporal branch. J Cutan Med Surg. 2011;15:84–86. doi: 10.2310/7750.2011.10064. [DOI] [PubMed] [Google Scholar]
- 7.de Bonnecaze G, Chaput B, Filleron T, Al Hawat A, Vergez S, Chaynes P. The frontal branch of the facial nerve: can we define a safety zone? Surg Radiol Anat. 2015;37:499–506. doi: 10.1007/s00276-014-1386-3. [DOI] [PubMed] [Google Scholar]
- 8.Farahvash MR, Yaghoobi A, Farahvash B, Farahvash Y, Hadadi Abiyaneh S. The extratemporal facial nerve and its branches: analysis of 42 hemifacial dissections in fresh Persian (Iranian) cadavers. Aesthet Surg J. 2013;33:201–208. doi: 10.1177/1090820X12473104. [DOI] [PubMed] [Google Scholar]
- 9.Fatah MF. Innervation and functional reconstruction of the forehead. Br J Plast Surg. 1991;44:351–358. doi: 10.1016/0007-1226(91)90148-d. [DOI] [PubMed] [Google Scholar]
- 10.Federative Committee on Anatomical Terminology (FCAT) Terminologia Anatomica. New York: Thieme Stuttgart; 1998. p. 136. [Google Scholar]
- 11.Frodel JL, Marentette LJ. The coronal approach. Anatomic and technical considerations and morbidity. Arch Otolaryngol Head Neck Surg. 1993;119:201–207. doi: 10.1001/archotol.1993.01880140091014. discussion 140. [DOI] [PubMed] [Google Scholar]
- 12.Furnas DW. Landmarks for the trunk and the temporofacial division of the facial nerve. Br J Surg. 1965;52:694–696. doi: 10.1002/bjs.1800520915. [DOI] [PubMed] [Google Scholar]
- 13.Gosain AK, Sewall SR, Yousif NJ. The temporal branch of the facial nerve: how reliably can we predict its path? Plast Reconstr Surg. 1997;99:1224–1233. doi: 10.1097/00006534-199704001-00003. discussion 1234-1236. [DOI] [PubMed] [Google Scholar]
- 14.Horimoto C, Toba T, Yamaga S, Tsujimura M. Subfascial temporalis dissection preserving the facial nerve in pterional craniotomy--technical note. Neurol Med Chir (Tokyo) 1992;32:36–37. doi: 10.2176/nmc.32.36. [DOI] [PubMed] [Google Scholar]
- 15.Hwang K. Surgical anatomy of the facial nerve relating to facial rejuvenation surgery. J Craniofac Surg. 2014;25:1476–1481. doi: 10.1097/SCS.0000000000000577. [DOI] [PubMed] [Google Scholar]
- 16.Ikeda K, Yamashita J, Hashimoto M, Futami K. Orbitozygomatic temporopolar approach for a high basilar tip aneurysm associated with a short intracranial internal carotid artery: a new surgical approach. Neurosurgery. 1991;28:105–110. doi: 10.1097/00006123-199101000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Ishikawa Y. An anatomical study on the distribution of the temporal branch of the facial nerve. J Craniomaxillofac Surg. 1990;18:287–292. doi: 10.1016/s1010-5182(05)80533-5. [DOI] [PubMed] [Google Scholar]
- 18.Jiang P, Tong XK, Zhao ML. The course and clinical significance of the temporal branch of the facial nerve. Chin J Clin Anat. 1997;15:81. [Google Scholar]
- 19.Kerawala CJ, Grime RJ, Stassen LF, Perry M. The bicoronal flap (craniofacial access): an audit of morbidity and a proposed surgical modification in male pattern baldness. Br J Oral Maxillofac Surg. 2000;38:441–444. doi: 10.1054/bjom.2000.0315. [DOI] [PubMed] [Google Scholar]
- 20.Knize DM. Muscles that act on glabellar skin: a closer look. Plast Reconstr Surg. 2000;105:350–361. doi: 10.1097/00006534-200001000-00056. [DOI] [PubMed] [Google Scholar]
- 21.Lans J, Schellekens PP, de Ru JA, Bleys RL. Motor innervation of the corrugator supercilii muscle in relation to orbital landmarks: guidelines for surgical denervation. J Craniofac Surg. 2016;27:1331–1335. doi: 10.1097/SCS.0000000000002727. [DOI] [PubMed] [Google Scholar]
- 22.Lei T, Gao JH, Xu DC, Zhong SZ, Li XJ, Chen B, et al. The frontal-temporal nerve triangle: a new concept of locating the motor and sensory nerves in upper third of the face rhytidectomy. Plast Reconstr Surg. 2006;117:385–394. doi: 10.1097/01.prs.0000200807.14826.f9. [DOI] [PubMed] [Google Scholar]
- 23.Lin Y, Zhang W, Luo Q, Jiang J, Qiu Y. Extracranial microanatomic study of supraorbital keyhole approach. J Craniofac Surg. 2009;20:215–218. doi: 10.1097/SCS.0b013e318191cf8a. [DOI] [PubMed] [Google Scholar]
- 24.Martou G, Antonyshyn OM. Advances in surgical approaches to the upper facial skeleton. Curr Opin Otolaryngol Head Neck Surg. 2011;19:242–247. doi: 10.1097/MOO.0b013e328347f895. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell DA, Barnard NA, Bainton R. An audit of 50 bitemporal flaps in primary facial trauma. J Craniomaxillofac Surg. 1993;21:279–283. doi: 10.1016/s1010-5182(05)80347-6. [DOI] [PubMed] [Google Scholar]
- 26.Pekar L, Bláha M, Schwab J, Melechovský D. Craniotomy and the temporal branch of the facial nerve. Rozhl Chir. 2004;83:205–208. [PubMed] [Google Scholar]
- 27.Pérez-Rull J, Brette MD, Levignac J, Hadjean E, Miron C, Freyss G. Surgical landmarks of the temporo-frontal branch of the facial nerve. Ann Chir Plast Esthet. 1992;37:11–17. [PubMed] [Google Scholar]
- 28.Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plast Reconstr Surg. 1966;38:352–356. doi: 10.1097/00006534-196610000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Sabini P, Wayne I, Quatela VC. Anatomical guides to precisely localize the frontal branch of the facial nerve. Arch Facial Plast Surg. 2003;5:150–152. doi: 10.1001/archfaci.5.2.150. [DOI] [PubMed] [Google Scholar]
- 30.Salas E, Ziyal IM, Bejjani GK, Sekhar LN. Anatomy of the frontotemporal branch of the facial nerve and indications for interfascial dissection. Neurosurgery. 1998;43:563–568. doi: 10.1097/00006123-199809000-00089. discussion 568-569. [DOI] [PubMed] [Google Scholar]
- 31.Saylam C, Ucerler H, Orhan M, Ozek C. Anatomic guides to precisely localize the zygomatic branches of the facial nerve. J Craniofac Surg. 2006;17:50–53. doi: 10.1097/01.scs.0000193556.32293.9c. [DOI] [PubMed] [Google Scholar]
- 32.Schleicher W, Feldman M, Rhodes J. Review of facial nerve anatomy: trauma to the temporal region. Eplasty. 2013;13:ic54. [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt BL, Pogrel MA, Hakim-Faal Z. The course of the temporal branch of the facial nerve in the periorbital region. J Oral Maxillofac Surg. 2001;59:178–184. doi: 10.1053/joms.2001.18271. [DOI] [PubMed] [Google Scholar]
- 34.Sekiya T, Iwabuchi T, Okabe S, Takiguchi M, Oda N. Facial nerve preservation in the region of the zygomatic arch. No Shinkei Geka. 1990;18:1029–1033. [PubMed] [Google Scholar]
- 35.Standring S. Gray’s Anatomy, ed 39. London: Elsevier Churchill Livingstone; 2008. pp. 513–514. [Google Scholar]
- 36.Stuzin JM, Wagstrom L, Kawamoto HK, Wolfe SA. Anatomy of the frontal branch of the facial nerve: the significance of the temporal fat pad. Plast Reconstr Surg. 1989;83:265–271. doi: 10.1097/00006534-198902000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Tellioğlu AT, Tekdemir I, Erdemli EA, Tüccar E, Ulusoy G. Temporoparietal fascia: an anatomic and histologic reinvestigation with new potential clinical applications. Plast Reconstr Surg. 2000;105:40–45. doi: 10.1097/00006534-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Tzafetta K, Terzis JK. Essays on the facial nerve: part I. Microanatomy. Plast Reconstr Surg. 2010;125:879–889. doi: 10.1097/PRS.0b013e3181ccdc78. [DOI] [PubMed] [Google Scholar]
- 39.Wildan T, Nasser N. Aberrant temporal branch of facial nerve. Br J Oral Maxillofac Surg. 2016;54:e61–e63. doi: 10.1016/j.bjoms.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Yaşargil MG, Reichman MV, Kubik S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg. 1987;67:463–466. doi: 10.3171/jns.1987.67.3.0463. [DOI] [PubMed] [Google Scholar]
- 41.Zani R, Fadul R, Jr, Da Rocha MA, Santos RA, Alves MC, Ferreira LM. Facial nerve in rhytidoplasty: anatomic study of its trajectory in the overlying skin and the most common sites of injury. Ann Plast Surg. 2003;51:236–242. doi: 10.1097/01.SAP.0000063755.42122.5F. [DOI] [PubMed] [Google Scholar]


