Abstract
Objective
To evaluate the impact on rural Veterans' access to social work services of a Department of Veterans Affairs (VA) national program to increase social work staffing, by Veterans' rurality, race, and complex care needs.
Data Sources and Study Setting
Data obtained from VA Corporate Data Warehouse, including sites that participated in the social work program between October 1, 2016 and September 30, 2021.
Study Design
The study outcome was monthly number of Veterans per 1000 individuals with 1+ social work encounters. We used difference‐in‐differences to estimate the program effect on urban, rural, and highly rural Veterans. Among rural and highly rural Veterans, we stratified by race (American Indian or Alaskan Native, Asian, Black, Native Hawaiian or Other Pacific Islander, and White) and complex care needs (homelessness, high hospitalization risk, and dementia).
Data Collection
We defined a cohort of 740,669 Veterans (32,434,001 monthly observations) who received primary care at a participating site.
Principal Findings
Average monthly social work use was 8.7 Veterans per 1000 individuals. The program increased access by 49% (4.3 per 1000; 95% confidence interval, 2.2–6.3). Rural Veterans' social work access increased by 57% (5.0; 3.6–6.3). Among rural/highly rural Veterans, the program increased social work access for those with high hospitalization risk by 63% (24.5; 18.2–30.9), and for Veterans experiencing homelessness, 35% (13.4; 5.2–21.7). By race, the program increased access for Black Veterans by 53% (6.1; 2.1–10.2) and for Asian Veterans by 82% (5.1; 2.2–7.9).
Conclusions
At rural VA primary care sites with social work staffing below recommended levels, Black and Asian Veterans and those experiencing homelessness and high hospitalization risk may have unmet needs warranting social work services.
Keywords: econometric models, population health, primary health care, rural health, social work, Veterans
What is known on this topic
Rural Veterans experience social risks such as barriers to housing and financial difficulties.
The National Social Work Patient Aligned Care Team (PACT) Staffing Program approves funding to hire social workers embedded within PACTs serving rural populations to address social risks.
A previous evaluation of the program found reduced hospitalizations and emergency department visits among Veterans after program initiation.
What this study adds
Overall utilization of social work services increased among Veterans receiving care at sites participating in the staffing program.
Among rural and highly rural Veterans, social work utilization increased across racial sub‐groupings following program implementation
Rural and highly rural Veterans with complex care needs such as those living with dementia or experiencing housing instability had the greatest increases in social work utilization.
1. INTRODUCTION
Rural Veterans with complex care needs and adverse social circumstances—such as barriers to housing, access to food, social isolation, or financial difficulty—face geographic barriers to access and use healthcare services throughout the Department of Veterans Affairs (VA) health system. Social workers within primary care teams at rural, community‐based outpatient clinics and VA medical centers are suited to identify and address social determinants of health among these Veterans. Social workers in team‐based primary care settings support patients and caregivers through their clinical roles as behavioral health specialists, case managers, and community engagement specialists. 1
In 2016, the Department of VA National Social Work Program and the VA Office of Rural Health launched an initiative to address an identified shortage of social workers in rural VA primary care teams, or Patient Aligned Care Teams (PACTs). Through this initiative, the National Social Work PACT Staffing Program approves funding through a collaborative effort with the VA Office of Rural Health to hire social workers embedded within PACTs serving rural populations. Eligible sites include PACTs serving primarily rural Veterans that remain below the VA target staffing ratio of one social worker per two PACT teamlets. Each PACT teamlet consists of a primary care provider accompanied by a registered nurse, a clinical associate (such as a licensed practical nurse or medical assistant), and an administrative associate caring for a panel of 1200 Veterans. 2 A previous evaluation of the program's impact showed the addition of a social worker to a Veteran's primary care team led to 4.4% and 3% overall reductions in hospitalizations and emergency department visits, respectively. 3
Sites participating in the program under the agreement that the funded social work positions will serve a majority rural caseload. Beyond that mutually agreed benchmark, social workers embedded in outpatient clinics through the implementation efforts of the National Social Work PACT Staffing Program provide services under the direction of their Service Chiefs and the needs of their PACTs. Social workers' caseloads are determined by local practice and population needs rather than by national directives. We hypothesize that Veterans who experienced increased access to social work care as a result of the program intervention may have had previously unmet needs for services. Groups who experienced greater program impact may have had higher levels of unmet need prior to the staffing program.
In this study, we examined how embedding social workers within rural PACTs through the implementation of the National Social Work PACT Staffing Program differentially affected the use of social work services among urban, rural, and highly rural Veterans receiving primary care at participating sites. Additionally, we examined the variable impacts of the program on subgroups of rural and highly rural Veterans representing diverse racial backgrounds and those with complex care needs, including Veterans experiencing homelessness or housing insecurity, Veterans with dementia, and Veterans at high medical risk of hospitalization or mortality.
2. METHODS
2.1. Study design
We conducted a retrospective cohort study documenting the impact of the National Social Work PACT Staffing Program on social work utilization among Veterans enrolled in primary care at a site that participated in the staffing program. This study was conducted as part of an evaluation comprising quality‐improvement activities on behalf of the VA National Social Work Program, and the Providence VA Medical Center Institutional Review Board determined the study exempt from review. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cohort studies.
2.2. Study setting, data, and participants
Nationally, the entire VA health system consists of 1321 total healthcare facilities including 172 VA medical centers and 1138 outpatient clinics. 4 Out of all outpatient clinics within the VA health system, 167 (15%) have participated in the National Social Work PACT Staffing Program. Among the sites that have never been funded, 397 (41%) are potentially eligible for the staffing program. 5 In order to be eligible for program funding, the clinics must have fewer than the recommended ratio of one full‐time‐equivalent social worker per two primary care providers and serve a substantial number of rural Veterans. Between October 1, 2016 and September 30, 2021, 151 outpatient clinics co‐located in VA medical centers as well as stand‐alone community‐based outpatient clinics participated in the National Social Work PACT Staffing Program. We identified all Veterans who had at least one primary care visit at a participating site at any point in the study period in order to assign a Veteran to an outpatient clinic. If a Veteran had primary care at more than one outpatient clinic, we assigned them to the site where they had the most visits or the most recent visit in case of a tie.
2.3. Intervention
For this study, the intervention was the National Social Work PACT Staffing Program which funded PACT social work positions for 3‐year terms at sites serving rural Veterans. Through the VHA Office of Rural Health, the program received funding to hire social workers at outpatient clinics co‐located in VA medical centers as well as stand‐alone, community‐based outpatient clinics. Many community‐based outpatient clinics and VA medical centers serve a substantial number of rural and urban Veterans. Thus, Veterans living in urban areas also receive the potential benefits of increased social work staffing. The program funded new social work positions for the first 3 years, after which the medical center committed to fund the positions from its local budget. New social workers were onboarded and trained within 1–2 months of being hired. Social workers were trained in the VA's Social Work Practice Model, which emphasizes comprehensive assessment of patients' clinical and psychosocial needs followed by ongoing case management and treatment planning.
2.4. Outcomes
We operationalized the outcome as the number of Veterans with one or more social work encounters per 1000 Veterans per month. We used PACT social work‐specific VA stop codes from medical record data to identify PACT social work encounters (Table S1).
2.5. Stratification of Veteran characteristics
We matched Veterans' residential ZIP codes to census tracts and categorized their rurality according to VA rurality definitions which employ Rural Urban Commuting Areas (RUCAs). Urban census tracts are those in which 30% or more of the population lives in a census‐defined urbanized area (population ≥50,000; RUCA = 1, 1.1); highly rural census tracts have less than 10% of the working population commuting to any community larger than an urbanized cluster (population ≤2500; RUCA = 10); and rural census tracts are those not designated urban nor highly rural (RUCA = 2, 2.1, 3, 4, 4.1, 5, 5.1, 6, 7, 7.1, 7.2, 8, 8.1, 8.2, 9, 10.1, 10.2, 10.3). 6 We excluded 0.7% of Veterans with missing address data or whose ZIP codes we could not match to RUCA census tracts.
From VA electronic medical records, we identified Veterans based on self‐identified race (American Indian or Alaska Native, Asian, Black, native Hawaiian or other Pacific Islander, and White), dementia diagnoses, Care Assessment Needs (CAN) scores ≥95, and housing status (homeless/unstably housed). Our measure of race represents a social construct, used as a proxy to measure the influence of structural racism experienced by Veterans in our study. 7 Although financial barriers to receiving care are minimized, Veterans nonetheless experience racial disparities in their clinical outcomes. 8 Race information is collected through clinical interactions, and though efforts are made to collect self‐reported race information in VA, race information is often recorded by a proxy respondent or a VA enrollment coordinator or clerk. 9 In this analysis, we categorized Veterans with multiple races based on their selected racial category with the lowest prevalence in our dataset. The ICD‐10 codes used to define dementia derive from a list the VA Corporate Data Warehouse (CDW) uses, 10 which has been employed in previous studies (Table S2). 3 , 11 CAN scores reflect an estimated probability of death or hospital admission within 90 days expressed as a percentile score for each Veteran. 12 We used the most recent non‐missing CAN score in the prior 12 months of the social work encounter.
First, we stratified analyses according to rurality status. Next, among the sub‐sample of rural and highly rural Veterans, we stratified further by the self‐identified race categories defined above. Finally, we analyzed rural and highly rural Veterans with dementia diagnoses, those who experienced homelessness or housing insecurity, and those with CAN scores ≥95.
2.6. Statistical analyses
To visualize the data and explore patterns, we plotted the number of encounters per 1000 Veterans by the number of months since the social worker's start date. Plots were created for the overall sample and for each Veteran subgroup (rurality, race among rural and highly rural Veterans, high‐utilization groups among rural and highly rural Veterans). We used a difference‐in‐differences approach to measure the change in social work encounters after the intervention, compared to trends at sites that had not yet started the program. The program had staggered start dates because additional funds became available over time and because of idiosyncratic variations in the timing for recruitment, hiring, and onboarding of new social workers. This staggered intervention allowed us to adjust for both time‐constant differences among sites and national trends in the use of social work services across the VA. The exposure variable was an indicator for the month that a site hired its first social worker using program funds. To allow for a training period for new social workers, we excluded observations from a site in the first month of the first social worker's start date.
We estimated program impact using a doubly robust estimator that used not‐yet‐treated sites as the comparison group. 13 This estimator avoids the pitfalls of traditional “two‐way fixed effects” regression models, such as negative weights on some treatment groups in the case of post‐treatment trends in the outcome. With this approach, sites were grouped by the month when they started the program. The effects of the program were estimated for each group and month, using the not‐yet‐treated sites as the comparison sample. For the full sample, we estimated the cumulative average treatment effect for each month of program participation and plotted these effects in an event‐study figure. For each subgroup, we report the group's average rate of social work encounters and the aggregated group‐time‐average treatment effects, an overall mean weighted by the number of Veterans in the groups. Models controlled for age and gender. Our estimation strategy is discussed in more detail in the online supplement.
To assess statistical significance, we clustered standard errors by site, as this was the level of the intervention. We used two‐sided T‐tests of the coefficients with the null hypothesis zero effect, and calculated 95% confidence intervals (CI) (alpha = 0.05) for point estimates assuming T‐distributed standard errors. We calculated CI for the doubly robust estimates using 1000 bootstrap iterations. Statistical analyses were performed using R version 3.6.1.
3. RESULTS
The analysis sample included 740,669 Veterans with a total of 32,434,001 monthly observations from October 2016 to September 2021 (Table 1). We report the number of sites and observations by month in the Figures S1 and S2. The mean age was 64 years (standard deviation [SD] = 16.09) and 94% were male. Racial and ethnic demographics included 1% American Indian or Alaska Native, 0.6% Asian, 6.7% Black, 1.2% Native Hawaiian or other Pacific Islander, 84.7% White, and 5.8% of Veterans were missing race data. Rural and highly rural Veterans comprised 55.2% and 9.1% of the sample, respectively. 2.4% of Veterans in the sample had a dementia diagnosis, 3.6% experienced homelessness or housing insecurity, and 4.5% had a CAN score ≥95.
TABLE 1.
Characteristics of Veterans in sample.
| All Veterans with 1+ primary care visit at a participating site | Site status based on participation in National Social Work PACT Staffing Program | Standardized mean difference before versus after funding | ||
|---|---|---|---|---|
| Before funding | After funding | |||
| Veterans, N | 740,699 | 426,197 | 715,952 | |
| Veteran‐months, N | 32,434,001 | 8,555,727 | 23,878,274 | |
| Age, mean (SD) | 64.32 (16.09) | 65.34 (15.43) | 63.95 (16.30) | 0.087 |
| Gender: male, N (%) | 30,470,181 (93.9) | 8,090,301 (94.6) | 22,379,880 (93.7) | 0.036 |
| Rurality status | ||||
| Urban, N (%) | 11,339,559 (35.0) | 2,421,792 (28.3) | 8,917,767 (37.3) | 0.222 |
| Rural, N (%) | 17,914,720 (55.2) | 5,072,403 (59.3) | 12,842,317 (53.8) | |
| Highly rural, N (%) | 2,960,144 (9.1) | 1,029,947 (12.0) | 1,930,197 (8.1) | |
| Race | ||||
| American Indian or Alaska Native, N (%) | 321,012 (1.0) | 86,235 (1.0) | 234,777 (1.0) | 0.077 |
| Asian, N (%) | 178,519 (0.6) | 32,909 (0.4) | 145,610 (0.6) | |
| Black or African American, N (%) | 2,182,727 (6.7) | 533,955 (6.2) | 1,648,772 (6.9) | |
| Native Hawaiian and other Pacific Islander, N (%) | 397,971 (1.2) | 80,983 (0.9) | 316,988 (1.3) | |
| White, N (%) | 27,458,106 (84.7) | 7,392,035 (86.4) | 20,066,071 (84.0) | |
| Missing, N (%) | 1,895,666 (5.8) | 429,610 (5.0) | 1,466,056 (6.1) | |
| Dementia a , N (%) | 765,423 (2.4) | 216,596 (2.5) | 548,827 (2.3) | 0.015 |
| CAN Score ≥95, N (%) | 1,459,132 (4.5) | 411,915 (4.8) | 1,047,217 (4.4) | 0.020 |
| Unstably housed or homeless a , N (%) | 1,150,635 (3.6) | 254,103 (3.0) | 896,532 (3.7) | 0.014 |
Abbreviations: CAN, Care Assessment Need; PACT, Patient Aligned Care Team; SD, standard deviation.
In 12 months prior to index month.
Overall, an average of 8.7 Veterans per 1000 had one or more PACT social work visits per month prior to program implementation (Table 2). Following the intervention, we estimated an increase of 4.3 Veterans per 1000 (95% CI, 2.2–6.3) with the outcome, controlling for national time trends and Veteran characteristics. This represents a 49% increase relative to the mean.
TABLE 2.
Association between an additional social worker and Veterans with 1+ social worker encounter per month between October 1, 2016 and September 30, 2021.
| No. monthly observations | No. Veterans with any social work encounters, per 1000 individuals per month | |||
|---|---|---|---|---|
| Sample average | Change associated with program intervention (95% CI) | Percent change | ||
| Model 1: Overall | 32,434,001 | 8.7 | 4.3 (2.2–6.3) | 49% |
| Model 2: Rurality | ||||
| Urban | 11,339,559 | 8.9 | 6.1 (3.2–9.0) | 69% |
| Rural | 17,914,720 | 8.7 | 5.0 (3.6–6.3) | 57% |
| Highly rural | 2,960,144 | 7.5 | 1.4 (−1.5 to 4.2) | 19% |
| Model 3: Race among rural and highly rural Veterans | ||||
| American Indian or Alaskan Native | 244,535 | 10.6 | 7.3 (−2.1 to 16.6) | 69% |
| Asian | 78,859 | 6.2 | 5.1 (2.2–7.9) | 82% |
| Black | 657,382 | 11.5 | 6.1 (2.1–10.2) | 53% |
| Native Hawaiian or other Pacific Islander | 162,749 | 10.0 | 4.9 (0.0–9.9) | 49% |
| White | 18,508,952 | 8.3 | 4.3 (3.0–5.6) | 52% |
| Model 4: High‐utilization groups among rural and highly rural Veterans | ||||
| Dementia diagnosis | 477,915 | 40.2 | 8.5 (−1.6 to 18.7) | 21% |
| CAN Score ≥ 95 | 873,782 | 39.1 | 24.5 (18.2–30.9) | 63% |
| Homeless or unstably housed | 430,817 | 38.3 | 13.4 (5.2–21.7) | 35% |
Abbreviations: CAN, Care Assessment Need; CI, confidence interval\.
In Figure 1, we plot the total PACT social work encounters per month per 1000 Veterans by sub‐group before and after the start of the program. Month 0 represents the first month with a program‐funded social worker. Panel A shows all Veterans in the sample stratified by rurality status, Panel B shows rural and highly rural Veterans stratified by race, and Panel C shows rural and highly rural Veterans stratified by complex care needs (dementia, high CAN score, and homelessness/housing insecurity). In Panels A and B, the rate of encounters increases steeply in the month 0 by nearly two‐ to four‐fold the rate of encounters in the prior month, decreases in months 1 and 2, and stays constant from months 3 through 35. In Panel C, the three high‐complexity groups show a similar pattern but with a less dramatic spike in the first 3 months.
FIGURE 1.
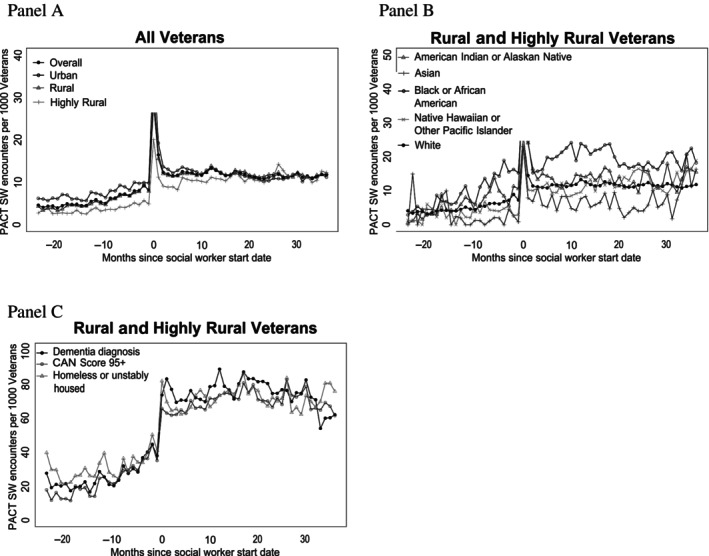
Overall number of Patient Aligned Care Team (PACT) social work (SW) encounters per 1000 Veterans relative to site participation in the staffing program where month 0 represents the start date for a newly hired social worker stratified by rurality status (Panel A), race/ethnicity among rural and highly rural Veterans (Panel B), and rural and highly rural Veterans with complex care needs (Panel C).
Figure 2 shows the overall effect of the program by month of participation for the full sample, where month 0 is the month just prior to the start of the first program‐funded social worker at each site. Each point represents the difference‐in‐difference in the proportion of Veterans with social work for that month, relative to changes for sites that had not yet started the program. The figure shows slight (not statistically significant) increases in social work engagement between 18 and 10 months preceding the program, and differences close to 0 in the 9 months directly preceding the program. After program initiation, we saw overall program effects between 5 and 11 Veterans per 1000 for 30 months followed by a decrease toward baseline in months 31–45.
FIGURE 2.
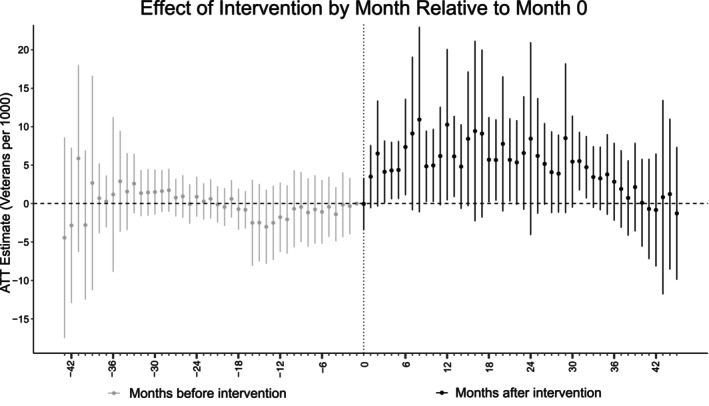
Dynamic event‐study plot of the cumulative effect of the program by month of participation, where month 0 is the month just prior to the start of the first program‐funded social worker at each site. Each point represents the difference‐in‐differences in the proportion of Veterans per 1000 with 1+ social work encounter for that month, relative to changes for sites that had not yet started the program. ATT, average treatment effect on the treated.
In Table 2, we report difference‐in‐difference estimates among the sub‐groups. Analyses based on rurality status showed that average rates of social work engagement were similar among urban, rural, and highly rural Veterans, with 8.9, 8.7, and 7.5 Veterans per 1000 per month having social work visits, respectively. Veterans in urban areas experienced an estimated increase of 6.1 Veterans per 1000 (95% CI, 3.2–9.0), a 69% increase relative to the average rate. Rural Veterans experienced an estimated increase of 5.0 Veterans per 1000 per month (95% CI, 3.6–6.3), a 57% relative increase. Finally, no statistically significant differences in social work engagement were observed among the highly rural Veterans sub‐group which had an estimated increase of 1.4 Veterans per 1000 per month (95% CI, −1.5 to 4.2).
When we stratified rural and highly rural Veterans by race, White and Asian Veterans had the lowest rates of social work encounters with 8.3 and 6.2 Veterans per 1000 with one or more PACT social work visits in a month. Black Veterans had the highest average at 11.5 Veterans per 1000 with one or more social work visits followed by American Indian or Alaska Native Veterans at 10.6 per 1000 and Native Hawaiian or Pacific Islander Veterans at 10.0 per 1000. Black Veterans experienced the greatest absolute program effect with an estimated additional 6.2 Veterans per 1000 (95% CI, 2.1–10.2) with one or more PACT social work visits in a month. Asian Veterans experienced the greatest relative change in social work utilization following the intervention with an 82% increase represented by an additional 5.1 Veterans per 1000 (95% CI, 2.2–7.9).
Rural and highly rural Veterans with complex care needs had higher average rates of social work engagement than the overall cohort. Among Veterans with dementia diagnoses, 40.2 Veterans per 1000 individuals per month had social work encounters, and they experienced a program impact of an additional 8.5 Veterans per 1000 (95% CI, −1.6 to 18.7) with social work encounters. Veterans experiencing homelessness or housing insecurity averaged 39.1 Veterans per 1000 individuals per month with social work encounters. The program impact in this group was an increase of 13.4 Veterans per 1000 per month (95% CI, 5.2–21.7), a 35% relative increase. Veterans with high medical risk of mortality or hospital admission (CAN scores ≥95) averaged 38.8 Veterans per 1000 individuals per month with social work encounters. This group experienced the greatest estimated program effect with 24.5 additional Veterans per 1000 (95% CI, 18.2–30.9) with one or more social work visits in a month. The relative magnitude was a 63% increase relative to the mean.
4. DISCUSSION
We found that embedding one or more additional social workers in VA primary care teams increased access to social work services (as measured by the Veterans at the site with any social work encounters in a month) by nearly 50%. The dynamic event‐study plot of overall program effects (Figure 2) displayed a sharp increase in social work utilization after hiring a social worker with program funding, but the effect began to diminish after the third year.
The findings of the paper complement the study conducted by Cornell and colleagues that found the social work staffing program contributed to decreases in emergency department and hospitalizations among Veterans. 3 Taken together, these studies suggest hiring additional social workers to achieve target staffing ratios within rural primary care teams has led to better health outcomes by providing Veterans better access to PACT social work services.
The limited duration of the external funding may have contributed to the return to baseline observed in our study. Although national program funding for social workers expired after 3 years, many sites continued funding social work positions permanently using their own resources. The medical center may have (1) chosen not to keep the position at all (2) kept the position and added new duties outside of PACT or (3) reassigned other social workers according to medical center needs. Additionally, new facility‐wide requirements could have increased the workload required of PACT social workers impacting their time with Veterans. The apparent relative decrease could also represent increases in the comparison group, as sites may have identified other mechanisms to increase their staffing ratios outside the program. The slight upward trend 18–10 months prior to the official intervention start date could be related to some “anticipation” effects, such as communication and meetings with sites and tools and education from program support staff, that may have increased outreach to new Veteran populations.
The number of PACT social work encounters per 1000 Veterans remained consistently elevated across sub‐groups following a site's participation in the staffing program (Figure 2). While the initial spike in encounters during months 0 and 1 contributes to our estimated program effect, it does not entirely explain the overall increases in social work engagement we observed. This spike could result from an initial backlog of unmet needs for social work services prior to program participation that results in new social workers building their caseloads with initial needs assessments, followed by an increase in coordinating and case‐management activities in the following months. Some types of care coordination and case management encounters comprise significant time and effort but are not recorded as patient encounters.
Both urban and rural Veterans experienced substantial increases in social work engagement. While program funding specifically targeted sites serving primarily rural and highly rural Veterans, urban Veterans within the cohort also experienced a substantial increase in service use and had a greater relative increase in the rate of social work engagement compared to rural and highly rural Veterans. Highly rural Veterans experienced the smallest impact, and our estimate was not statistically significant. That may reflect the difficulty of outreach to highly rural communities even with full staffing or possibly a lower level of need in that group. Additionally, community services tend to be more concentrated in urban areas with fewer available services in highly rural areas. Veterans residing in these areas may engage less frequently with social workers compared to their urban counterparts due to a lack of local services available to address their individual needs. Another possible reason is that in addition to the shortage of social work staff in rural areas that the Office of Rural Health originally sought to address, there was also a substantial unmet need for services in urban areas.
By race, the greatest increase was among Veterans self‐identified as Asian (who also had the lowest baseline rate of social work encounters), and among American Indian and Alaska Native Veterans, though that effect was not precisely estimated because these Veterans tend to be concentrated at a small number of sites (e.g., clinics in Oklahoma and Alaska). Asian Americans are less likely to seek public services for which they are eligible than non‐Hispanic White Americans. This disparity is likely related to language barriers, higher uninsurance rates, and discrimination from providers. Further, cultural factors may influence help‐seeking among subgroups of Asian Americans. For example, seeking mental health care is stigmatized in many Asian cultures. Increasing social work staffing may help increase outreach to Asian Veterans who otherwise could not seek or be able to access care. 14
Black Veterans experienced the highest baseline level of utilization and the greatest overall program effect. Structural racism, institutional policies that confer unfair treatment to others based on their racial or ethnic group, has disproportionately exposed Black individuals to adverse social and health conditions in the United States. Elevated utilization among this subgroup of Veterans may reflect an increased need for services. 15 Increasing social work staffing in PACT teams may help alleviate longstanding health disparities between racial and ethnic groups.
Veterans in rural and highly rural areas who had dementia, experienced homelessness or housing insecurity, or had CAN scores ≥95 exhibited substantially higher social work utilization rates than the overall cohort before the implementation of the staffing program. Despite this, these groups with complex care needs experienced increases in their levels of social work program effects roughly two to six times greater than the overall program effect. One reason for this increase is that the staffing program emphasized using tools such as the CAN score to proactively identify and reach out to Veterans with complex care needs. When staffed at recommended levels, social workers have more time for proactive outreach and clinical interventions that impact Veterans unmet needs.
Differences in referral patterns may explain geographic and racial differences in the impact of the staffing program. Within the VA, PACT social workers' caseloads are built, broadly, by three processes: (1) other VA clinicians can generate referrals to social workers, (2) social workers proactively identify Veterans for assessment and reach out by telephone or offer services when the patient comes to the clinic for an appointment, or (3) Veterans or their family and caregivers request social work services directly.
While nearly any VA clinician can order a social work consult, social work referrals from primary care providers are most common. Several factors influence referral practices including the following: clinical practice guidelines, screening and clinical reminders, individual clinicians' perceptions of Veterans' needs and desire to connect with social work, their relationships with social workers, and their understanding of clinical social work practice. For example, a VA study found that clinicians' practices varied widely with respect to referral of patients with alcohol use disorder to behavioral health providers (a role often filled by a social worker). 16 Primary care clinicians may have differing understandings of the interventions and resources that their social work team members can offer. 17
As a quasi‐experimental retrospective analysis, a limitation of this study lies in the lack of randomization of program participation among our study cohort. Sites were not randomly selected for program participation, and as discussed above, Veterans were not randomly selected for social work services. Thus, there are limitations to inferring causal effects, as the addition of social work staff may have also coincided with other changes in staffing or clinical practice at sites. Additionally, there are limitations to generalizability because sites that were eligible for the program were understaffed with respect to PACT social work and served rural populations; furthermore, those that applied for funding may have differed in their leadership from those that did not. Additionally, there is substantial homogeneity within racial and ethnic groups within our study that cannot be captured in our data due to sample size restrictions.
5. CONCLUSIONS
The VA PACT Social Work Staffing Program increased access to social work services across a wide array of Veteran populations. As a proxy for understanding where social work services were needed most, this study provides useful guidance for future work evaluating social workers' impact on healthcare service utilization, and the results have been shared with leaders in the VA Office of Patient Care Services. Since social workers assume a wide variety of responsibilities within primary care teams, identifying and measuring their impact on patient care can prove challenging. By elucidating which populations were impacted the greatest, this study will help direct future research toward better understanding of the impacts of social workers on those populations.
FUNDING INFORMATION
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development CDA 22‐157 (PYC) and Quality Enhancement Research Initiative (PEC‐018), the VA National Social Work Program VA Office of Rural Health. Additional funding and support for ANH were provided by the Brown University Primary Care‐Population Medicine Graduate Study Program. The contents of this research do not represent the views of VA or the United States Government.
Supporting information
Data S1. Supporting information.
ACKNOWLEDGMENTS
We would like to thank Taylor Rickard for research and program management support.
Honken AN, Halladay CW, Wootton LE, et al. Differential effects of a social work staffing intervention on social work access among rural and highly rural Veterans: A cohort study. Health Serv Res. 2024;59(Suppl. 2):e14327. doi: 10.1111/1475-6773.14327
REFERENCES
- 1. Fraser MW, Lombardi BM, Wu S, Zerden LS, Richman EL, Fraher EP. Integrated primary care and social work: a systematic review. J Soc Soc Work Res. 2018;9(2):175‐215. doi: 10.1086/697567 [DOI] [Google Scholar]
- 2. Department of Veterans Affairs, Veterans Health Administration . Patient Aligned Care Team (PACT) Handbook. VHA Handbook 1101.10[1]. VHA; 2024. Accessed April 7, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2977 [Google Scholar]
- 3. Cornell PY, Halladay CW, Ader J, et al. Embedding social workers in veterans health administration primary care teams reduces emergency department visits. Health Aff. 2020;39(4):603‐612. doi: 10.1377/hlthaff.2019.01589 [DOI] [PubMed] [Google Scholar]
- 4. About Veterans Health Administration . U.S. Department of Veterans Affairs. Accessed February 13, 2024. https://www.va.gov/health/aboutvha.asp
- 5. Cornell PY, Hua CL, Halladay CW, et al. Benefits and challenges in the use of RE‐AIM for evaluation of a national social work staffing program in the veterans health administration. Front Health Serv. 2023;3:1225829. doi: 10.3389/frhs.2023.1225829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. 2010 Rural‐Urban Commuting Area (RUCA) Codes. United States Department of Agriculture. August 17, 2020. Accessed February 5, 2023, https://www.ers.usda.gov/data‐products/rural‐urban‐commuting‐area‐codes/documentation/
- 7. Flanagin A, Frey T, Christiansen SL; Committee AMAMoS . Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA. 2021;326(7):621‐627. doi: 10.1001/jama.2021.13304 [DOI] [PubMed] [Google Scholar]
- 8. Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff. 2011;30(4):707‐715. doi: 10.1377/hlthaff.2011.0074 [DOI] [PubMed] [Google Scholar]
- 9. Mor M. Assessing Race and Ethnicity in VA Data. Database and Methods Cybersecurity Series. ViREC Database and Methods Seminar. 2024. Accessed February 2, 2024. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=6512 [Google Scholar]
- 10. Wagner TH, Gehlert E, Rosen A, Valenstein M. Updating the Psychiatric Case Mix System (PsyCMS) Mental Health and Substance Use Grouper for ICD‐10‐CM. Technical Report 31. Health Economics Resource Center, U.S. Department of Veterans Affairs. November 2016. Accessed November 2, 2023. https://www.herc.research.va.gov/include/page.asp?id=technical-report-psycms-icd10
- 11. Jutkowitz E, Halladay C, McGeary J, O'Toole T, Rudolph JL. Homeless veterans in nursing homes: care for complex medical, substance use, and social needs. J Am Geriatr Soc. 2019;67(8):1707‐1712. doi: 10.1111/jgs.15993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang L, Porter B, Maynard C, et al. Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368‐373. doi: 10.1097/MLR.0b013e31827da95a [DOI] [PubMed] [Google Scholar]
- 13. Callaway B, Sant'Anna PH. Difference‐in‐differences with multiple time periods. J Econom. 2021;225(2):200‐230. [Google Scholar]
- 14. Clough J, Lee S, Chae DH. Barriers to health care among Asian immigrants in the United States: a traditional review. J Health Care Poor Underserved. 2013;24(1):384‐403. doi: 10.1353/hpu.2013.0019 [DOI] [PubMed] [Google Scholar]
- 15. Zambrana RE, Williams DR. The intellectual roots of current knowledge on racism and health: relevance to policy and the national equity discourse. Health Aff. 2022;41(2):163‐170. doi: 10.1377/hlthaff.2021.01439 [DOI] [PubMed] [Google Scholar]
- 16. Claiborne N, Videka L, Postiglione P, Finkelstein A, McDonnell P, Krause RD. Alcohol screening, evaluation, and referral for veterans. J Soc Work Pract Addict. 2010;10(3):308‐326. doi: 10.1080/1533256X.2010.500963 [DOI] [Google Scholar]
- 17. Keefe B, Geron SM, Enguidanos S. Integrating social workers into primary care: physician and nurse perceptions of roles, benefits, and challenges. Soc Work Health Care. 2009;48(6):579‐596. doi: 10.1080/00981380902765592 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.


