Abstract
Objective
Lower limb discrepancy (LLD) was frequently observed in patients with idiopathic scoliosis (IS), potentially associated with etiopathogenesis. Although sole lifts had been proposed as a conservative treatment for IS, evidence supporting their efficacy was limited. This study aimed to assess the effects of sole lift intervention on pediatric patients with mild IS, specifically focusing on thoracolumbar/lumbar (TL/L) curvature.
Methods
Twenty patients, with an average age of 12.3 ± 3.1 years and presenting mild TL/L curve (15.6° ± 6.2°), were selected from a pool of 267 pediatric IS patients in the outpatient of our spine center from February 2023 to August 2023. Inclusion criteria comprised a main TL/L curve ranging between 10° and 40°, the lower limb positioned at the convexity of the main curve, and LLD of less than 2 cm; individuals requiring bracing or surgical intervention were excluded. Custom sole lifts were used to address the shorter lower limb with the objective of leveling the pelvis. Radiographic evaluations were conducted both before and after intervention using standing full spine posteroanterior radiographs and full leg length radiographs. Statistical analysis was undertaken to evaluate curve correction and its associations with other influencing factors.
Results
The mean structural and functional LLD were 7.1 ± 4.5 mm and 7.1 ± 4.1 mm, respectively. Among the 20 patients, four exhibited structural LLD greater than 10 mm. The average follow‐up duration was 6.4 ± 1.9 months (range: 3–8 months). Following sole lift intervention (7.0 ± 3.0 mm), a significant reduction was observed in the TL/L curve compared to the pre‐sole lifting measurements (15.6° ± 6.2° vs. 12.1° ± 7.2°, p < 0.001), as well as a notable decrease in the thoracic curve (12.2° ± 4.0° vs. 8.6° ± 6.3°, p = 0.064). Nine patients experienced a significant curve reduction of ≥5°, while eight showed a reduction between 0° and 5°; however, two patients exhibited no change in curve magnitude. Furthermore, the correction rate of the TL/L curve correlated significantly with functional LLD (r = −0.484, p = 0.030) and pelvic obliquity (r = −0.556, p = 0.011), highlighting the active pelvic compensation in maintaining balance between the spine and lower limbs. Conversely, no significant correlation was observed between curve correction and structural LLD (p > 0.05). Additionally, even after adjusting for other influencing factors, the TL/L Cobb angle remained significantly different between pre‐ and post‐sole lifting (p = 0.037).
Conclusion
This study confirmed the effectiveness of sole lift intervention in correcting TL/L and thoracic curves among the mild IS children with a main TL/L curve, providing a supplementary conservative treatment option for patients with the lower limb at the convexity of the main curve. Moreover, our findings underscored the active compensation of the lower limbs and the pelvis in the etiopathogenesis of IS, highlighting the importance of considering their influence in treatment strategies.
Keywords: conservative treatment, Idiopathic scoliosis, lower limb discrepancy, pelvic, sole lift
After sole lift intervention, there was a significant decrease in the TL/L Cobb magnitude from pre‐sole lifting to post‐sole lifting, with 45% of patients experiencing a notable reduction in curve magnitude of ≥5°. Although LLD might not directly contribute to the etiopathogenesis of IS, lower limb and pelvic compensation mechanisms had a crucial role in the correction of scoliosis.
Introduction
Idiopathic scoliosis (IS) is a prevalent spinal deformity primarily affecting children, with its etiology still not fully understood but believed to be multifactorial and potentially associated with asymmetries in various body parts. 1 , 2 Burwell et al. 3 , 4 , 5 reported that idiopathic scoliosis associated with the body asymmetries, such as the neck, shoulders, scapula, breast, buttocks, pelvis, and lower extremities, indicating a complex etiology involving deformities beyond the spine. IS often progresses during childhood, leading to significant complications. Although observation and rehabilitation exercises are regularly prescribed for mild IS cases according to guidelines from the Scoliosis Research Society (SRS), their effectiveness remains uncertain. 1 , 2 , 6 , 7 , 8
Leg length discrepancy (LLD) is another common orthopaedic condition characterized by differences in lower limb lengths, 9 which could result in standing imbalance and biomechanical alterations. It affects individuals of all ages, with a higher prevalence among pediatric populations; various studies have reported a wide range of prevalence rates from 40% to 70%. 9 , 10 , 11 , 12 , 13 , 14 Previous studies have demonstrated a significant correlation between LLD and scoliosis. In 1982, Papaionnou et al. demonstrated that LLD‐induced scoliosis, termed functional scoliosis, was non‐structural and non‐progressive, implying that correcting LLD could potentially reduce lumbar curvature. 13 Similarly, Raczkowski et al. 10 found that correcting LLD helped reduce the curve magnitude in 316 patients with scoliosis (83.7%). However, 92.7% of the patients had LLD of greater than 1 cm, and the curve magnitude of the key parameter was not described in the study. Moreover, these corrections were just for functional scoliosis, and the exact relationship between LLD and structural scoliosis remained incompletely understood. 9 , 10
Sole lifts were commonly used to address LLD by equalizing leg lengths and relieving associated symptoms. By elevating the shorter limb, sole lifts aimed to reduce pelvic obliquity and mitigate compensatory spinal curvature observed in functional scoliosis. 15 However, the efficacy of sole lifts in preventing scoliosis progression remained a subject of debate, with conflicting evidence in the literature. 12 , 16 , 17 , 18 , 19
Based on our clinical observation, the sole lift seemed effective for IS patients with the lower limb at the convexity of the main thoracolumbar/lumbar (TL/L) curve. Therefore, given the clinical significance of LLD and its potential implications for IS treatment, this study aimed (i) to investigate the efficacy of sole lift intervention in treating pediatric patients with mild IS and primary TL/L curvature and (ii) to explore the complex relationship between LLD, the pelvis, and scoliosis, with the objective of studying the compensatory mechanisms among them.
Methods
Subjects
A total of 267 newly diagnosed IS children aged between 4 and 17 years were consecutively recruited at our center from February 2023 to August 2023. Diagnosis of IS was confirmed clinically by a senior spine surgeon. Inclusion criteria were: (i) untreated IS patients presenting for the first time; (ii) age between 4 and 17 years; (iii) main TL/L curve between 10° and 40°; and (iv) the lower limb at the convexity of the main curve. 20 Exclusion criteria included the requirement for bracing or surgical intervention, structural LLD ≥2 cm, medical conditions affecting bone metabolism and history of operations affecting the growth of the spine, pelvis, and/or lower limbs. Ethical approval was obtained from the Clinical Research Ethics Committee (No. 2023–0739), and written informed consent was obtained from all subjects and their guardians.
Radiologic Assessments
All patients underwent standing full‐spine and full leg length posteroanterior (PA) X‐ray radiographs. Patients were positioned naturally with their tiptoes symmetrically on the line parallel to the X‐ray cassette. Curve severity was graded using the Cobb angle on the full‐spine radiograph. Structural LLD was measured from the center of the femoral head to the center of the ankle joint on the full leg length radiograph, while functional LLD was measured as the vertical distance between the upper edge of the bilateral femoral heads. 12 , 21 , 22 Pelvic obliquity was defined as the angle between the horizontal reference line and the pelvic coronal reference line. 22 , 23 Trunk shift was defined as the distance between the C7 plumb line and the center sacral vertical line, with a shift to the concavity of the main TL/L curve denoted by a negative sign. 22 Other clinical and radiographic parameters collected included gender, age, Risser grade, the level of the upper end vertebra (UEV) and lower end vertebra (LEV), and the apex of the main curve. 24
Management of Sole Lift
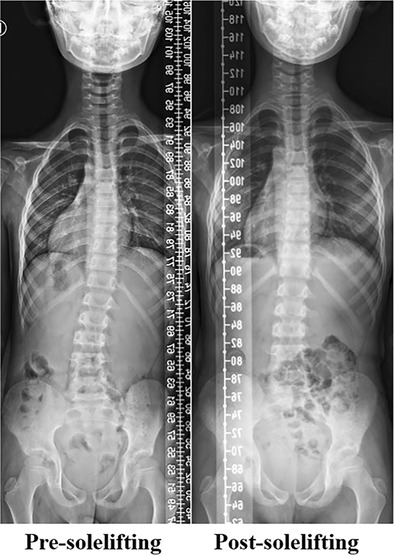
Custom sole lifts (made of ethylene vinyl acetate copolymer material, manufactured by China Jinhua Deren Rehabilitation Aids) were applied to the shorter lower limb with the aim of leveling the pelvis (Figure 1). Patients received detailed personalized instructions, with initial daily wear prescribed for at least 10 hours, and visited our clinic every 3–4 months. Adjustments to the size of the orthosis were made if the curve severity or pattern altered, if it did not meet the patient's growth, or if the patients complained of lower back pain. Standing PA X‐ray films were taken during follow‐up. Outcome assessment followed SRS criteria, 25 considering a decrease of ≥5° in the Cobb angle of the main curve at the latest follow‐up as effective management (and otherwise considered ineffective).
Figure 1.

Custom orthosis for sole lift.
Statistical Analysis
The data was expressed as mean ± standard deviation. For data that was normally or approximately normally distributed, a two‐tailed paired sample t‐test was used to study the difference between the pre‐ and post‐sole lifting, and a two‐tailed Student t‐test was used to study the difference between the effective and ineffective patients. For skewed data or those with unconfirmed normality, the Mann–Whitney test was used for group comparison. The χ 2‐test was used to compare the incidence of gender between two groups. Multilinear regression analysis was used to compare the difference in the post‐sole lifting TL/L Cobb angle (dependent variable) between the effective and ineffective group (Groupeffective/ineffective, independent variable) with controlling the other influencing factors (independent variable). In the regression model, the effective patient was assigned a value of “0” and the ineffective was assigned a value of “1.” All statistical analysis was performed with SPSS 19.0 software (SPSS, Chicago, IL, USA). For all tests, p < 0.05 was considered statistically significant.
Results
Efficacy of Sole Lift Intervention on Curve Correction
The demographic and anthropometric characteristics of the patients are summarized in Table 1. A total of 20 patients were included, comprising 10 boys and 10 girls, with an average age of 12.3 ± 3.1 years (range: 7–17 years). Of the 20 patients, 15 had structural LLD of ≤10 mm, and four patients had structural LLD of >10 mm. Only one patient had equal lower limb lengths. The average follow‐up period was 6.4 ± 1.9 months (range: 3–8 months).
Table 1.
The demographic and anthropometric characteristics of all the pediatric mild IS patients
| Parameters | All (N = 20) | Effective group (N = 9) | Ineffective group (N = 11) | p‐value |
|---|---|---|---|---|
| Age (years) | 12.3 ± 3.1 | 12.1 ± 3.4 | 12.4 ± 2.8 | >0.05 a |
| Gender (female, male) | 10, 10 | 6, 3 | 4, 7 | >0.05 |
| Risser grade | 2.3 ± 3.1 | 2.2 ± 2.1 | 2.3 ± 2.0 | >0.05 |
| TL/L Cobb angle (°) | 15.6 ± 6.2 | 15.6 ± 5.7 | 15.6 ± 7.1 | >0.05 a |
| Thoracic Cobb angle (°) | 12.2 ± 4.0 | 12.3 ± 4.7 | 12.0 ± 3.6 | >0.05 a |
| Structural LLD (mm) | 7.1 ± 4.5 | 4.8 ± 3.2 | 9.3 ± 4.6 | 0.020 a |
| Functional LLD (mm) | 7.1 ± 4.1 | 6.4 ± 3.9 | 7.7 ± 3.4 | >0.05 a |
| Trunk shift (mm) | 5.4 ± 13.0 | 3.7 ± 13.2 | 7.3 ± 13.3 | >0.05 a |
| Pelvic obliquity (°) | 3.0 ± 1.6 | 2.4 ± 1.5 | 3.7 ± 1.4 | 0.070 a |
| TL/L UEV | 12 ± 1.4 | 12 ± 1.3 | 11 ± 1.5 | >0.05 b |
| TL/L LEV | 16 ± 0.9 | 16 ± 0.9 | 16 ± 0.8 | >0.05 |
| TL/L Apex | 14 ± 1.3 | 15 ± 1.3 | 14 ± 1.2 | >0.05 |
| Sole lift (mm) | 7.0 ± 3.0 | 6.1 ± 2.6 | 7.9 ± 3.1 | >0.05 a |
Note: If the vertebra number is ≤12, it refers to thoracic vertebrae; and if the vertebra number is >12, it represents lumbar vertebrae (i.e., 11 means T11, 13 means L1, and 14 means L2). IS, idiopathic scoliosis; LEV, lower end vertebra; LLD, lower limb discrepancy; TL/L, thoracolumbar/lumbar; UEV, upper end vertebra
Comparisons between the effective and ineffective patients using independent‐sample t‐tests
Using Wilcoxon rank‐sum test
Using χ 2‐test.
Following sole lift intervention, there was a significant decrease in the TL/L Cobb angle from pre‐sole lifting measurements (15.6° ± 6.2°) to the post‐sole lifting (12.1° ± 7.2°, p < 0.001), corresponding to a correction rate of 23.4% ± 25.9%. Similarly, the thoracic Cobb angle showed a notable decrease compared with post‐sole lifting measurements (12.2° ± 4.0° vs. 8.6° ± 6.3°, p = 0.064), with a correction rate of 33.8% ± 50.8% (Table 2).
Table 2.
Comparisons of the radiographic features between the pre‐ and post‐sole lifting idiopathic scoliosis patients
| Parameters | Pre‐sole lifting | Post‐sole lifting | Correction rate | p‐value |
|---|---|---|---|---|
| TL/L Cobb angle (°) | 15.6 ± 6.2 | 12.1 ± 7.2 | 23.4% ± 25.9% | <0.001 |
| Thoracic Cobb angle (°) | 12.2 ± 4.0 | 8.6 ± 6.3 | 33.8% ± 50.8% | 0.064 |
| Trunk shift (mm) | 5.4 ± 13.0 | 2.6 ± 16.9 | — | 0.547 |
| Pelvic obliquity (°) | 3.0 ± 1.6 | 1.8 ± 1.6 | — | 0.002 |
| Functional LLD (°) | 7.1 ± 4.1 | 3.1 ± 3.9 | — | <0.001 |
Note: IS, idiopathic scoliosis; LLD, lower limb discrepancy; TL/L, thoracolumbar/lumbar. All comparisons were using paired‐sample t‐tests.
According to the SRS criteria, 25 9 of 20 patients showed significant curve reduction of ≥5°, demonstrating effective treatment response to sole lift (Figure 2), and eight patients showed a reduction between 0 and 5°. Two patients showed no change in curve magnitude, likely due to advanced skeletal maturity, characterized by a Risser sign of 4 and being 2 years post‐menarche. Meanwhile, one 10‐year‐old female patient exhibited curve progression from 10° to 15°, attributed to her significant growth potential. Pelvic obliquity and functional LLD were also decreased significantly from pre‐ to post‐sole lifting (p < 0.05).
Figure 2.
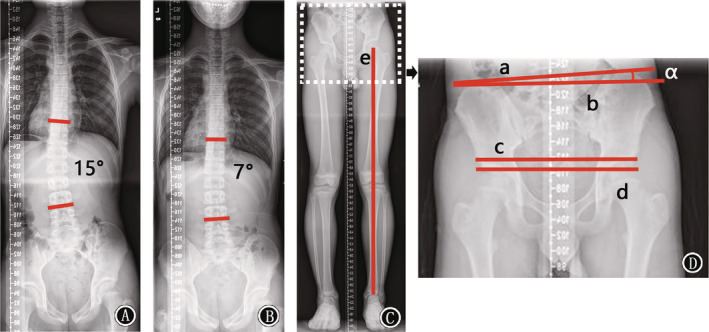
A 15‐year‐old male adolescent idiopathic scoliosis. (A) Pre‐sole lifting standing full‐spine radiograph; thoracolumbar/lumbar (TL/L) curve magnitude of 15°. (B) After 7 months of follow‐up with sole lift management, the TL/L curve reduced to 7°. (C) Pre‐sole lifting full leg length radiograph, where “e” is the line from the center of the femoral head to the center of the ankle joint, representing the lower limb length. (D) Measurement of pelvic obliquity (α), defined as the angle between the pelvic coronal reference line (line a) and the horizontal reference line (line b); functional lower limb discrepancy (LLD) is the vertical distance between the upper edge of the bilateral femoral heads (lines c and d).
Relationship between Lower Limb Discrepancy, Pelvis and Scoliosis
Further analysis comparing the effective and ineffective treatment groups revealed a significant difference in structural LLD, with the effective patients exhibiting smaller LLD (4.8 ± 3.2 mm vs. 9.3 ± 4.6 mm, p = 0.020, Table 1). This suggested that when there was a smaller LLD, more corrective force generated by the sole lift intervention would be transmitted to TL/L spine. Correlation analysis demonstrated significant correlations between the correction rates of TL/L and thoracic curves, functional LLD, and pelvic obliquity (r = 0.4–0.6, p < 0.05). However, no significant correlation was found between the correction rate and structural LLD (p > 0.05). Moreover, there were significant correlations between structural and functional LLD as well as pelvic obliquity (r = 0.6–0.7, p < 0.05), suggesting the pelvis actively compensated to maintain balance between the spine and lower limbs. Trunk shift exhibited negative correlations with TL/L UEV (r = −0.505, p = 0.027), LEV (r = −0.521, p = 0.022), and apex (r = −0.554, p = 0.014), indicating that a lower position of the TL/L curve corresponded to decreased trunk shift. Additionally, trunk shift was negatively correlated with pelvic obliquity (r = −0.469, p = 0.043), suggesting that smaller pelvic obliquity was linked to more significant trunk shift.
Multiple linear regression analysis with adjustment for other influencing factors confirmed the significant difference between pre‐ and post‐sole lifting TL/L Cobb angles (p = 0.037, Table 3), suggesting the effectiveness of sole lift intervention in correcting the TL/L curve.
Table 3.
Comparisons between the effective and ineffective idiopathic scoliosis patients after adjustments of the other influencing factors
| Parameters | Constant | Groupeffective/ineffective | TL/L Cobb angle | p‐value | Adjusted R 2 | |
|---|---|---|---|---|---|---|
| Post‐sole lifting TL/L Cobb angle | B | −5.016 | 4.917 | −0.991 | <0.001 | 0.878 |
| P | 0.092 | 0.037 | <0.001 |
Note: Multilinear regression analysis with a stepwise method was used
In the regression model, the dependent variable was the post‐sole lifting TL/L Cobb angle, and independent variables were the TL/L Cobb angle and groupeffective/ineffective in which the effective subject was assigned a value of “0” and the ineffective was assigned a value of “1.”
TL/L, thoracolumbar/lumbar.
Discussion
This study investigated the effectiveness of sole lift interventions in pediatric patients with a main TL/L curvature. The results suggested that sole lifts could effectively manage and potentially correct mild TL/L curvature in pediatric IS patients, emphasizing the significance of considering biomechanical compensation of LLD and pelvic adjustments in IS treatment strategies.
Efficacy of Sole Lift Intervention on Curve Correction
Leg length discrepancy is a common orthopaedic condition and particularly prevalent among pediatric populations. Various studies have reported a wide range of prevalence rates of 40% to 70%, highlighting the variability in defining LLD. 9 , 10 , 11 , 12 , 13 A 2005 meta‐analysis by Knutson 14 found a high prevalence of LLD in the general population, with only a small percentage of individuals having equal leg lengths. Including a total of 573 patients, 90% of patients had at least a 1‐mm LLD and approximately 50% of the population had a 4 mm discrepancy or less. The present study revealed a high prevalence of LLD (95%) among IS patients, consistent with previous findings, 9 , 10 , 11 , 12 , 13 suggesting that LLD might be unrelated to the occurrence of IS.
The progression of IS has long been studied, with peripubertal longitudinal growth potential and initial larger curve magnitude being key determining factors. 6 , 8 , 26 Several studies have shown that the probability of curve progression decreases with increasing age or advancing Risser grade6, 8 Additionally, premenarchal status has been confirmed as a high risk factor for curve progression. 8 Beyond these biological factors, larger curve magnitude was identified as the greatest risk factor for curve progression, irrespective of growth status and curve pattern. 26 It has also been reported that greater progression occurs in patients with double‐curve or right thoracic pattern. 26 The findings from these studies implied that the risk of curve progression increased with greater growth potential and curve magnitude and was associated with specific curve patterns. In our study, age and Risser grade were significantly positively correlated with TL/L and thoracic curve severity, consistent with previous research. 6 , 8 , 26 , 27 However, our study found no significant correlation between LLD, whether structural or functional, and curve severity, aligning with previous research. 28 These findings indicated that LLD might not play a significant role in IS progression.
Treatment approaches for juvenile and adolescent IS varied widely, ranging from observation to rehabilitation exercises and bracing. 8 , 25 , 29 , 30 Bracing was considered the most effective non‐surgical treatment for curves >20° or 25°. However, patients with mild curves of <20° had limited effective treatment options to slow or halt curve progression. The use of sole lift intervention for controlling curve progression remains controversial. Some studies have reported its ineffectiveness due to poor correlation with TL/L scoliosis, 28 while, other studies have shown promising results. 18 , 19 , 31 Park et al. 19 demonstrated a significant reduction in the Cobb angle in scoliosis patients treated with custom‐made foot orthoses. In this randomized controlled study of 26 patients aged between 13 and 60 years, it was found that the foot orthoses could significantly reduce the scoliosis angle by approximately 7° with the follow‐up of 4 weeks. D'Amico et al. 31 reached a similar conclusion. Nevertheless, these studies lacked detailed information on scoliosis etiology, curve patterns, and differential diagnosis of functional scoliosis, which are essential factors for assessing treatment effectiveness. In a retrospective study by Lee et al., 18 foot orthosis was found to significantly reduce curve magnitude from 22.03° ± 4.39° initially to 18.86° ± 7.53 after wearing foot orthoses in 52 juvenile IS patients. However, details regarding the curve pattern and the relationship between the spine, pelvis, and lower limbs were not thoroughly described. 20 Moreover, a substantial number of patients with curves >25° did not receive bracing treatment as recommended. 18
The present study focused on pediatric IS patients with a main TL/L curve, using sole lift intervention for correction. To ensure patient homogeneity, only those with the lower limb at the convexity were included in the study. Our results showed that most patients (17 of 20) experienced curve reduction after sole lift intervention, suggesting its effectiveness in this specific subgroup of patients. Therefore, it was suggested that the sole lift on the convexity was an effective treatment for the main TL/L IS patients with the lower limb at the convexity, which was significantly more effective than the observation and rehabilitation exercises. 8 , 25 , 29 , 30 The mechanism behind this effectiveness might involve the production of an inverted correction force on the TL/L curve by the sole lift at the convexity, resolution of functional scoliosis components, and interruption of the curve progression cycle. 18
Furthermore, our study observed significant improvements in thoracic and TL/L curvature in most patients within 3–8 months after the sole lift intervention. This suggested that sole lift management might lead to curvature improvement within 6 months in pediatric IS patients with mild TL/L curvature.
Relationship between Lower Limb Discrepancy, Pelvis and Scoliosis
Correlation analysis revealed that the rate of curve correction was negatively correlated with functional LLD and pelvic obliquity but showed no correlation with structural LLD. This demonstrated that the correction force from the lower limbs after sole lift could not directly act with the spine without the pelvic compensation. Therefore, functional LLD and pelvic obliquity were believed to represent pelvic compensation capacity in the coronal plane, serving as crucial links between sole lift intervention and spinal correction, 32 , 33 which indicated that smaller functional LLD and pelvic obliquity meant the better correction effects of sole lift. Hence, patients with structural LLD of ≥2 cm were excluded from our study design to minimize interference from functional scoliosis on the results.
Additionally, our findings demonstrated a negative relationship between trunk shift and the position of the TL/L curve, suggesting that smaller trunk shifts were associated with a lower position of TL/L curvature. Meanwhile, trunk shift was also negatively correlated with pelvic obliquity. These findings revealed a complete spinal–pelvic compensation link involving trunk shift and pelvis. When the pelvis compensated more, the spine would save more compensation by utilizing trunk shift; conversely, increased trunk shift might occur to compensate when the pelvis compensated less, maintaining balance in the spinal–pelvic link. 33
Limitations and Strengths
Our study exhibited two primary limitations that merit further discussion. First, the modest number of participants and the relatively brief follow‐up period might compromise the robustness of our findings. These constraints hindered a comprehensive evaluation of all factors potentially influencing the efficacy of sole lift interventions. Consequently, larger cohorts and extended study durations are essential to validate the efficacy of sole lift interventions and to elucidate their relationship with various influencing factors, as well as other potential benefits for patients. Second, our research was confined to pediatric IS patients with a main TL/L curve and lower limb at the convexity. This specificity might restrict the generalizability of our results to other IS patient groups. Therefore, future studies are necessary to evaluate the effectiveness of sole lift interventions across diverse patient types and to establish the most suitable indications for this novel treatment approach. 20
However, this study exhibited several strengths that bolstered its significance and credibility within the field. First, by specifically focusing on the main TL/L IS patients with the lower limb at the convexity, the research enabled a detailed exploration of sole lift efficacy within a well‐defined group. This targeted approach facilitated a deeper understanding of how sole lifts influence this subset of IS cases. Second, with a follow‐up period of up to 6 months, the study provided valuable insights into the short‐term effects of sole lift intervention. This timeframe was sufficient to observe potential changes in curvature and to assess the sustainability of the intervention's effects. Third, by collecting a comprehensive range of data, including spinal curve measurements, pelvic obliquity, and LLD, the study presented a holistic view of the biomechanical changes induced by sole lift intervention, potentially informing a management strategy for IS.
Conclusion
In conclusion, our study was promising and offered valuable evidence supporting the effectiveness of sole lift interventions as a supplementary conservative management strategy for pediatric IS patients with main TL/L curve and lower limb at the convexity. Moreover, our results highlighted the active compensation of the lower limbs and pelvis in the etiopathogenesis of IS, emphasizing the importance of considering their influence in developing treatment strategies.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Ethics Statement
Ethical approval was obtained from the Clinical Research Ethics Committee (No. 2023‐0739), and written informed consent was obtained from all subjects and their guardians.
Author Contributions
All authors contributed significantly and met the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors. All authors agree to the final submitted manuscript. Concept and design: WZW, LCZ, and CJN. Acquisition, analysis, or interpretation of data: WZW, CQX, and CWS. Drafting of the manuscript: WZW. Critical revision of the manuscript for important intellectual content: CG, ZN and LJ. Statistical analysis: WZW and LH. Supervision: LFC.
Supporting information
Data S1. Supporting information.
Data S2. Supporting information.
Acknowledgements
This work was supported by the Key Research and Development Program of Zhejiang Province (Grant No. 2024C03078) and the Medical and Health Research Project of Zhejiang Province (Grant No. 2021423642).
References
- 1. Ogilvie JW. What's important: moving beyond “idiopathic” in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2020;102(3):269–270. [DOI] [PubMed] [Google Scholar]
- 2. Weinstein SL, Dolan LA. The evidence base for the prognosis and treatment of adolescent idiopathic scoliosis: the 2015 Orthopaedic Research and Education Foundation clinical research award. J Bone Joint Surg Am. 2015;97(22):1899–1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burwell RG, Dangerfield PH, Freeman BJ, et al. Etiologic theories of idiopathic scoliosis: the breaking of bilateral symmetry in relation to left‐right asymmetry of internal organs, right thoracic adolescent idiopathic scoliosis (AIS) and vertebrate evolution. Stud Health Technol Inform. 2006;123:385–390. [PubMed] [Google Scholar]
- 4. Burwell RG, Dangerfield PH, Moulton A, Grivas TB, Cheng JC. Whither the etiopathogenesis (and scoliogeny) of adolescent idiopathic scoliosis? Incorporating presentations on scoliogeny at the 2012 IRSSD and SRS meetings. Scoliosis. 2013;8(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burwell RG, Aujla RK, Freeman BJ, Dangerfield PH, Cole AA, Kirby AS, et al. Patterns of extra‐spinal left‐right skeletal asymmetries and proximo‐distal disproportion in adolescent girls with lower spine scoliosis: ilio‐femoral length asymmetry & bilateral tibial/foot length disproportion. Stud Health Technol Inform. 2006;123:101–108. [PubMed] [Google Scholar]
- 6. Hresko MT. Clinical practice. Idiopathic scoliosis in adolescents. N Engl J Med. 2013;368(9):834–841. [DOI] [PubMed] [Google Scholar]
- 7. Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369(16):1512–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008;371(9623):1527–1537. [DOI] [PubMed] [Google Scholar]
- 9. Gordon JE, Davis LE. Leg length discrepancy: the natural history (and what do we really know). J Pediatr Orthop. 2019;39(6, Suppl 1):S10–S13. [DOI] [PubMed] [Google Scholar]
- 10. Raczkowski JW, Daniszewska B, Zolynski K. Functional scoliosis caused by leg length discrepancy. Arch Med Sci. 2010;6(3):393–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bhave A, Paley D, Herzenberg JE. Improvement in gait parameters after lengthening for the treatment of limb‐length discrepancy. J Bone Joint Surg Am. 1999;81(4):529–534. [DOI] [PubMed] [Google Scholar]
- 12. Wynes J, Schupp A. Assessment of pediatric limb length inequality. Clin Podiatr Med Surg. 2022;39(1):113–127. [DOI] [PubMed] [Google Scholar]
- 13. Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb‐length inequality. J Bone Joint Surg Am. 1982;64(1):59–62. [PubMed] [Google Scholar]
- 14. Knutson GA. Anatomic and functional leg‐length inequality: a review and recommendation for clinical decision‐making. Part II. The functional or unloaded leg‐length asymmetry. Chiropr Osteopat. 2005;13:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gibson PH, Papaioannou T, Kenwright J. The influence on the spine of leg‐length discrepancy after femoral fracture. J Bone Joint Surg Br. 1983;65(5):584–587. [DOI] [PubMed] [Google Scholar]
- 16. Young RS, Andrew PD, Cummings GS. Effect of simulating leg length inequality on pelvic torsion and trunk mobility. Gait Posture. 2000;11(3):217–223. [DOI] [PubMed] [Google Scholar]
- 17. Zabjek KF, Leroux MA, Coillard C, Martinez X, Griffet J, Simard G, et al. Acute postural adaptations induced by a shoe lift in idiopathic scoliosis patients. Eur Spine J. 2001;10(2):107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee JG, Yun YC, Jo WJ, Seog TY, Yoon YS. Correlation of radiographic and patient assessment of spine following correction of nonstructural component in juvenile idiopathic scoliosis. Ann Rehabil Med. 2018;42(6):863–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Park SM, Ahn SH, Lee AY, Park IS, Cho YW. Raster‐stereographic evaluation of the effects of biomechanical foot orthoses in patients with scoliosis. J Phys Ther Sci. 2016;28(7):1968–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Juhl JH, Ippolito Cremin TM, Russell G. Prevalence of frontal plane pelvic postural asymmetry—part 1. J Am Osteopath Assoc. 2004;104(10):411–421. [PubMed] [Google Scholar]
- 21. Sheha ED, Steinhaus ME, Kim HJ, Cunningham ME, Fragomen AT, Rozbruch SR. Leg‐length discrepancy, functional scoliosis, and low Back pain. JBJS Rev. 2018;6(8):e6. [DOI] [PubMed] [Google Scholar]
- 22. Sekiya T, Aota Y, Yamada K, Kaneko K, Ide M, Saito T. Evaluation of functional and structural leg length discrepancy in patients with adolescent idiopathic scoliosis using the EOS imaging system: a prospective comparative study. Scoliosis Spinal Disord. 2018;13:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Karkenny AJ, Magee LC, Landrum MR, Anari JB, Spiegel D, Baldwin K. The variability of pelvic obliquity measurements in patients with neuromuscular scoliosis. JB JS Open Access. 2021;6(1):e20.00143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schwender JD, Denis F. Coronal plane imbalance in adolescent idiopathic scoliosis with left lumbar curves exceeding 40 degrees: the role of the lumbosacral hemicurve. Spine (Phila Pa 1976). 2000;25(18):2358–2363. [DOI] [PubMed] [Google Scholar]
- 25. Richards BS, Bernstein RM, D'Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on bracing and nonoperative management. Spine (Phila Pa 1976). 2005;30(18):2068–2075. [DOI] [PubMed] [Google Scholar]
- 26. Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66(7):1061–1071. [PubMed] [Google Scholar]
- 27. Soucacos PN, Zacharis K, Soultanis K, Gelalis J, Xenakis T, Beris AE. Risk factors for idiopathic scoliosis: review of a 6‐year prospective study. Orthopedics. 2000;23(8):833–838. [DOI] [PubMed] [Google Scholar]
- 28. Hoikka V, Ylikoski M, Tallroth K. Leg‐length inequality has poor correlation with lumbar scoliosis. A radiological study of 100 patients with chronic low‐back pain. Arch Orthop Trauma Surg. 1989;108(3):173–175. [DOI] [PubMed] [Google Scholar]
- 29. Korbel K, Kozinoga M, Stolinski L, Kotwicki T. Scoliosis Research Society (SRS) criteria and Society of Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) 2008 guidelines in non‐operative treatment of idiopathic scoliosis. Pol Orthop Traumatol. 2014;79:118–122. [PubMed] [Google Scholar]
- 30. Carragee EJ, Lehman RA Jr. Spinal bracing in adolescent idiopathic scoliosis. N Engl J Med. 2013;369(16):1558–1560. [DOI] [PubMed] [Google Scholar]
- 31. D'Amico M, Roncoletta P, Di Felice F, Porto D, Bellomo R, Saggini R. Leg length discrepancy in scoliotic patients. Stud Health Technol Inform. 2012;176:146–150. [PubMed] [Google Scholar]
- 32. Qiu XS, Wang ZW, Qiu Y, Wang WJ, Mao SH, Zhu ZZ, et al. Preoperative pelvic axial rotation: a possible predictor for postoperative coronal decompensation in thoracolumbar/lumbar adolescent idiopathic scoliosis. Eur Spine J. 2013;22(6):1264–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang ZW, Wang WJ, Sun MH, Liu Z, Zhu ZZ, Zhu F, et al. Characteristics of the pelvic axial rotation in adolescent idiopathic scoliosis: a comparison between major thoracic curve and major thoracolumbar/lumbar curve. Spine J. 2014;14(9):1873–1878. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.
Data S2. Supporting information.


