Abstract
Objective
The craniovertebral junction (CVJ) presents intricate anatomical challenges. In severe or irreducible malformations, complications such as reduction loss and fixation failure may occur, necessitating revision surgery. The posterior facet joint distraction and fusion (PFDF) technique, offers a solely posterior approach for revisions. Hence, we delineate varied revision scenarios, proposing surgical strategies and technical details to enhance outcomes and mitigate risks, thereby enriching the neurosurgical community's repertoire.
Methods
This was a retrospective cohort study, analyzed patient data from Xuanwu Hospital, between 2017 to 2023. All patients had a history of surgical treatment for CVJ malformations, and experienced failure or loss of reduction. The distance from the odontoid process tip to the Chamberlain's line (DCL), the atlantodental interval (ADI), clivus‐canal angle, cervicomedullary angle, width of subarachnoid space, CVJ area, and width of syrinx were used for radiographic assessment. Japanese Orthopaedic Association (JOA) scores and SF‐12 scores were used for clinical assessment. Independent sample t‐tests were employed. A significance level of p < 0.05 indicates statistically significant differences.
Results
We analyzed data from 35 patients. For patients who underwent PFDF, the postoperative DCL, ADI, and clivus‐canal angle significantly improved. For all patients, the postoperative cervicomedullary angle, width of subarachnoid space, CVJ area, and width of syrinx all demonstrated significant improvement, indicating the relief of neural compression. All patients showed significant improvement in both symptoms and clinical assessments.
Conclusion
Severe atlantoaxial joint locking or ligament contracting are the fundamental cause of reduction and fixation failure. Anterior odontoidectomy is indicated for patients with robust bony fusion of the atlantoaxial joint in an unreduced position. The PFDF technique is safe and effective for patients with incomplete atlantoaxial bony fusion. Preoperative assessment of surgical feasibility and vertebral artery status ensures surgical safety and efficacy.
Keywords: Basilar invagination, Fixation, Posterior approach, Reduction, Revision
Severe atlantoaxial joint locking or ligament contracting are the fundamental cause of reduction and fixation failure.
Anterior odontoidectomy is indicated for patients with robust bony fusion of the atlantoaxial joint in an unreduced position, the PFDF technique indicated for patients with incomplete bony fusion.
Introduction
The complex anatomy of the craniovertebral junction (CVJ) region plays a crucial role in facilitating flexion and rotation movements of the spine. 1 , 2 , 3 Conditions such as basilar invagination and atlantoaxial dislocation are relatively common malformations in the CVJ region. 4 , 5 Surgery remains the sole effective treatment for CVJ malformations. 6 , 7 , 8 , 9 , 10 However, patients with challenging cases, such as severe or irreducible basilar invagination, atlantoaxial dislocation, face substantial surgical difficulties and a higher failure rate. Complications such as reduction loss and fixation failure may occur, necessitating revision surgery. 11 , 12 , 13 , 14 , 15 Scar tissue, ectopic bone formation, and alterations in anatomical landmarks resulting from prior surgeries lead to surgical exposure challenges. Additionally, severe osseous malformations often coincide with vertebral artery anomalies, further increasing surgical risks.
Traditional revisions involve anterior–posterior reduction and fixation or anterior odontoidectomy. Odontoidectomy is suitable for patients with robust bony fusion. In recent years, advancements in the posterior facet joint distraction and fusion (PFDF) technique have enabled difficult cases to be treated solely through the posterior approach. Our center has predominantly adopted the PFDF technique for revision surgeries, accumulating a wealth of experience. In this article, we retrospectively review revision cases, providing detailed insights into the various causes and types of revision surgeries. We propose targeted approaches for different types of revisions, analyze the outcomes of the patients underwent different surgical procedures, offer valuable technical guidance and feasible surgical strategy to our colleagues.
Materials and Methods
This study is a retrospective cohort study, approved by the Ethics Committee of Xuanwu Hospital, Capital Medical University, with the assigned ethics number LYS[2021]052. All patients signed informed consent forms.
This study analyzed patient data from Xuanwu Hospital, Capital Medical University, between 2017 and 2023. The patients included in the study met the following criteria: (i) diagnosed with basilar invagination and/or atlantoaxial dislocation; (ii) a history of surgical treatment for CVJ malformations; (iii) experienced failure or loss of reduction; and (iv) presented with significant neurological symptoms. Exclusion criteria were: (i) rheumatoid arthritis; (ii) CVJ trauma; (iii) osteoporosis; (iv) CVJ tumors; and (v) severe underlying diseases affecting overall health. The diagnostic criteria for basilar invagination were the distance from the odontoid process tip to the Chamberlain's line (DCL) by >5 mm, and for atlantoaxial dislocation, the atlantodental interval (ADI) >3 mm.
Operative Procedure
Posterior Facet Joint Distraction and Fusion (PFDF)
After general anesthesia, the patient was placed in a prone position. Following draping and disinfection, a midline posterior incision was made to remove scar tissue and extract any existing implants. Cervical traction was applied, gradually reaching up to one‐sixth of the patient's body weight (maximum 18 kg), maintaining cervical traction throughout the procedure. Deep scar tissue and ectopic bone callus were excised, exposing the bilateral vertebral arteries and lateral atlantoaxial joints. A 2 mm‐wide osteotome was inserted into the joint space and rotated to completely remove the articular cartilage. Once the endplates were prepared, a specially designed distractor was inserted into the joint space for rotational distraction, gradually increasing its size to open the joint space. After opening one side of the joint space, a spacer was placed to maintain that gap, followed by distraction on the contralateral side. The above steps were repeated for both sides of the joint space. Intraoperative CT examinations were used to assess the reduction effect of basilar invagination and atlantoaxial dislocation. Once the planned reduction position was achieved, fusion cages filled with autologous iliac bone were placed in the bilateral joint spaces, and the position was confirmed under fluoroscopy. Finally, the internal fixation system was implanted. After thorough saline irrigation, muscle, fascia, and skin were meticulously sutured layer by layer. (Figure 1).
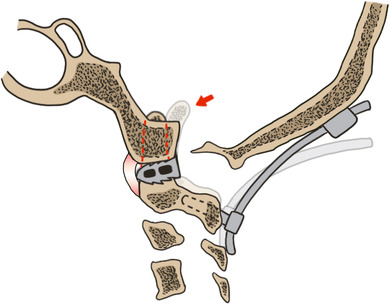
FIGURE 1.
Surgical techniques. (A, B) After removal of scar tissue and existing implants, individual intraarticular distractors were used to release the soft tissue and open the joint space. (C) Cages filled with autologous iliac bone were placed into the bilateral joints. (D) The internal fixation system was implanted.
Transnasal Endoscopic Odontoidectomy
In patients with robust bony fusion of the atlantoaxial joint, we performed transnasal endoscopic odontoidectomy. A bilateral nostril endoscopic technique was employed. The bilateral middle turbinates, inferior turbinates, and the anterior wall of the sphenoid sinus were preserved. The surgical trajectory was confirmed by the steep downward angle toward the lower clivus and was subsequently verified using intraoperative CT examination. The posterior nasopharyngeal fascia was then opened. The flap was elevated and reflected caudally to the level of the soft palate. The longus colli and capitis muscles were laterally reflected. The lower part of the clivus and assimilated C1 were visualized and removed using high‐speed drills and Kerrison rongeurs. The underlying odontoid process became visible. After removing most of the odontoid process using a high‐speed drill, the remaining cortical shell was sequentially excised along the vertical margins using the drill and Kerrison rongeurs. Decompression was confirmed by observing a reexpanded dural sac with pulsation and intraoperative CT examination. The operative cavity was covered with gelatin foam and the muscle‐mucosal flap, closing the surgical field. Bilateral nasal cavities were packed with expansion sponge.
Evaluation Criteria
The primary evaluation criteria include DCL, ADI, clivus‐canal angle, cervicomedullary angle, width of subarachnoid space, CVJ area, 16 and width of syrinx. (Figure 2) Secondary evaluation criteria encompass patient symptoms, the Japanese Orthopaedic Association (JOA) scores, and the short form‐12 (SF‐12) scores. All radiologic indicators were measured by two observers simultaneously to ensure the accuracy.
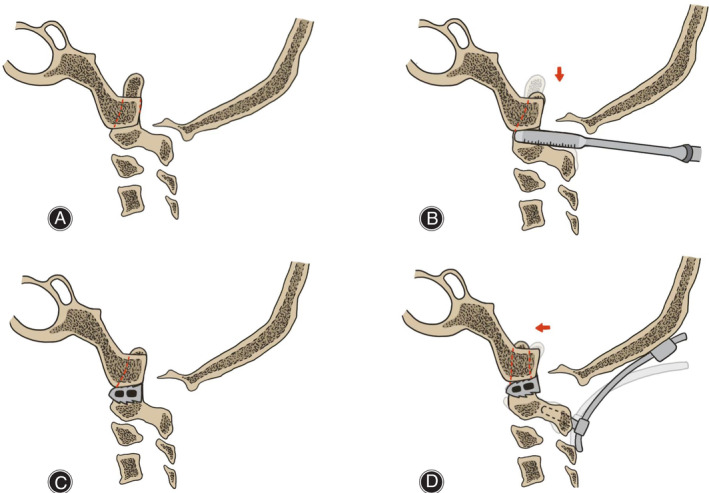
FIGURE 2.
Diagrams of the radiologic indicators. (A) Red dotted line, Chamberlain's line; red line, distance from the odontoid process tip to the Chamberlain's line (DCL); blue line, atlantodental interval (ADI); yellow line, clivus‐canal angle. (B) Yellow line, cervicomedullary angle; blue line, width of subarachnoid space, red area, CVJ area. 16 (C) Red line, width of syrinx.
Data Analysis
All data were analyzed using SPSS 29.0 software (IBM, Armonk, NY, USA). Consistency tests were employed for all radiologic indicators. Descriptive statistics are presented as mean ± standard deviation, and homogeneity of variance was assessed. Independent sample t‐tests were employed for pre‐ and postoperative comparisons. A significance level of p < 0.05 indicated statistically significant differences.
Result
Baseline Data
In this study, we analyzed data from 35 patients who experienced failed reduction of CVJ malformations. Among the patients, there were 20 males and 15 females, with an average age of 42.21 ± 13.90 years. Symptoms included limb numbness or weakness, trunk numbness, head, neck, trunk or limb pain, gait instability, dysphagia, as well as dizziness. Twenty‐nine patients had basilar invagination, 30 patients had atlantoaxial dislocation, three patients had atlantoaxial rotatory subluxation/fixation, seven patients had os odontoideum, 30 patients had C1 assimilation, and 16 patients had severe vertebral artery anomalies (including absence, high‐riding, fenestration, or significant aberrant course). (Table 1).
TABLE 1.
Baseline demographic, clinical, radiological, and surgical data of all patients.
| Demographic information | |
|---|---|
| Age/yrs | 42.21 ± 13.90 |
| Sex | |
| Male | 20 |
| Female | 15 |
| Malformations | |
| Basilar invaginati | 29 |
| Atlantoaxial dislocation/n | 30 |
| Atlantoaxial rotatory subluxation/fixation | 3 |
| Os odontoideum | 7 |
| C1 assimilation | 30 |
| Vertebral artery anomalies | 16 |
| Previous surgeries | |
| Posterior reduction and fixation | 30 |
| Posterior wiring and fusion | 2 |
| Posterior reduction and fixation, with foramen magnum decompression | 1 |
| Odontoidectomy and Fusion | 1 |
| Odontoidectomy and fusion, with foramen magnum decompression | 1 |
| Reason for revision | |
| Fixation failure | |
| Screw loosening | 1 |
| Screw breakage | 2 |
| Reduction failure | 32 |
| Symptoms | |
| Limb numbness | 14 |
| Limb weakness | 15 |
| Trunk numbness | 7 |
| Head, neck, trunk or limb pain | 8 |
| Gait instability | 12 |
| Dysphagia | 5 |
| Dizziness | 3 |
Note: Demographic, clinical, radiological, and surgical data of all patients.
Post‐admission imaging evaluations revealed three patients experienced screw loosening or breakage, indicating fixation failure. Thiry‐two patients had reduction failure (incomplete reduction). Thiry‐two patients exhibited no robust bony fusion in bilateral lateral atlantoaxial joints, while three did. For these three cases, since the lateral joints were already fused and could not be distracted for reduction, and the craniovertebral joints were stable, we performed a transnasal endoscopic odontoidectomy. Details of the previous surgeries are provided in Table 1.
Operative Data
All surgeries were performed by the same experienced neurosurgeon (Z.C.). For patients undergoing PFDF, the average operation time was 201.85 ± 73.73 min, with the average blood loss of 204.64 ± 276.32 mL. For patients undergoing transnasal endoscopic odontoidectomy, the average operation time was 227.00 ± 100.76 min, with the average blood loss of 106.67 ± 73.64 mL. The average follow‐up period was 6.80 ± 3.00 months (Range: 6 to 22 months). No malignant complications occurred postoperatively, and there were no infections in any of the patients.
Radiographic Assessments
The imaging measurements demonstrated high inter‐observer reliability, with an intraclass correlation coefficient value of 0.995 (p < 0.001). For patients undergoing PFDF surgery, in the postoperative CT examinations, significant reduction of both basilar invagination and atlantoaxial dislocation were observed: ADI reduced by 1.93 ± 2.37 mm, DCL reduced by 5.66 ± 3.85 mm, clivus‐canal angle increased by 11.71 ± 11.26°. In the postoperative MRI examination, significant relief of neural compression was observed: width of subarachnoid space increased by 0.87 ± 0.55 mm, cervicomedullary angle increased by 21.46 ± 13.50°, and CVJ area reduced by 0.51 ± 0.38 mm. Patients with combined syringomyelia also showed a noticeable improvement in width (average − 20.90 ± 21.77%). For patients undergoing odontoidectomy, the follow‐up MRI examination indicated significant improvement in spinal cord compression. No instances of reduction loss or fixation failure were detected during postoperative follow‐up examinations. Detailed data are presented in Tables 2 and 3 (Figures 3 and 4).
TABLE 2.
Radiographic assessments after PFDF.
| Variables | Preop | Postop | Difference | t‐value | p‐value | Follow‐up | Difference | t‐value | p‐value |
|---|---|---|---|---|---|---|---|---|---|
| Between preop and postop | Between preop and follow‐up | ||||||||
| ADI/mm | 4.82 ± 2.57 | 2.89 ± 2.10 | −1.93 ± 2.37 | −4.163 | p < 0.001 | 2.88 ± 2.11 | −1.94 ± 2.37 | −4.163 | p < 0.001 |
| DCL/mm | 9.86 ± 5.00 | 4.20 ± 4.83 | −5.66 ± 3.85 | −7.483 | p < 0.001 | 4.19 ± 4.82 | −5.67 ± 3.85 | −7.504 | p < 0.001 |
| Clivus‐canal angle/° | 126.96 ± 16.89 | 138.70 ± 14.92 | 11.71 ± 11.26 | 5.700 | p < 0.001 | 138.72 ± 14.94 | 11.74 ± 11.25 | 5.716 | p < 0.001 |
| Width of subarachnoid space/mm | 0.76 ± 0.51 | 1.63 ± 0.58 | 0.87 ± 0.55 | 7.726 | p < 0.001 | 1.80 ± 0.46 | 1.04 ± 0.50 | 10.268 | p < 0.001 |
| Cervicomedullary angle/° | 125.24 ± 12.78 | 146.70 ± 13.33 | 21.46 ± 13.50 | 7.788 | p < 0.001 | 147.51 ± 13.01 | 22.26 ± 13.34 | 8.174 | p < 0.001 |
| CVJ area/cm2 | 2.32 ± 0.60 | 1.81 ± 0.46 | −0.51 ± 0.38 | −6.454 | p < 0.001 | 1.69 ± 0.41 | −0.63 ± 0.40 | −7.517 | p < 0.001 |
| Width of syrinx of spinal cord/% | 57.78 ± 26.95 | 36.88 ± 24.67 | −20.90 ± 21.77 | −2.879 | p = 0.021 | 29.78 ± 18.89 | −28.00 ± 21.10 | −3.979 | p = 0.004 |
Abbreviations: ADI, the atlantodental interval; DCL, the distance from the odontoid process tip to the Chamberlain's line; Postop, postoperative; Preop, preoperative.
TABLE 3.
Radiographic and clinical assessments after odontoidectomy.
| Variables | Preop | Postop | Difference | t‐value | p‐value | Follow‐up | Difference | t‐value | p‐value |
|---|---|---|---|---|---|---|---|---|---|
| Between preop and postop | Between preop and follow‐up | ||||||||
| Width of subarachnoid space/mm | 0.74 ± 0.55 | 3.75 ± 1.16 | 3.01 ± 1.65 | 3.160 | p = 0.044 | 3.84 ± 1.01 | 3.10 ± 1.63 | 3.293 | p = 0.041 |
| Cervicomedullary angle/° | 123.98 ± 7.58 | 150.70 ± 7.34 | 26.72 ± 14.82 | 3.124 | p = 0.044 | 151.91 ± 6.75 | 27.93 ± 14.18 | 3.413 | p = 0.038 |
| CVJ area/cm2 | 3.38 ± 1.01 | 1.50 ± 0.35 | −1.87 ± 0.71 | −4.572 | p = 0.022 | 1.45 ± 0.34 | −1.92 ± 0.71 | −4.719 | p = 0.021 |
| JOA | 11.67 ± 0.58 | 14.67 ± 0.58 | 3.00 ± 1.00 | 5.196 | p = 0.035 | ||||
| SF‐12 | 72.87 ± 1.56 | 82.02 ± 1.56 | 9.15 ± 2.15 | 7.370 | p = 0.018 | ||||
Abbreviations: Follow‐up, at last follow‐up; JOA, the Japanese Orthopedic Association score; SF‐12, the Short Form‐12 score; Postop, postoperative; Preop, preoperative.
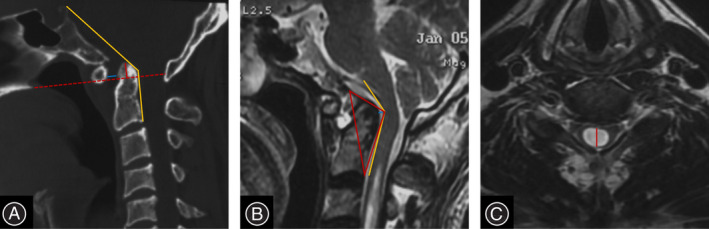
FIGURE 3.
A 50‐year‐old male presented with limbs and trunk numbness, undergone two operations. (A, B) CT and MRI image before first operation, showing basilar invagination, atlantoaxial dislocation and syringomyelia. (C) CT image after first operation (posterior reduction and fixation), showing partially reduction of basilar invagination and atlantoaxial dislocation, with empty lateral joint spaces. (D, E) CT and MRI image of 2 months after first operation, showing loss of reduction and lateral joint spaces. (F) CT image after second operation (posterior reduction and fixation, with bone grafting in lateral joint spaces), showing partially reduction of basilar invagination and atlantoaxial dislocation. (G, H) CT and MRI image of 4 months after second operation, showing screw breakage. (I, J) CT and MRI image after PFDF, showing reduction of basilar invagination and atlantoaxial dislocation, with relief of neural compression. (K, L) CT and MRI image during follow‐up, showing bone fusion in bi‐lateral joints, and reduction of syrinx. (M) Photo during PFDF, showing the broken screw.
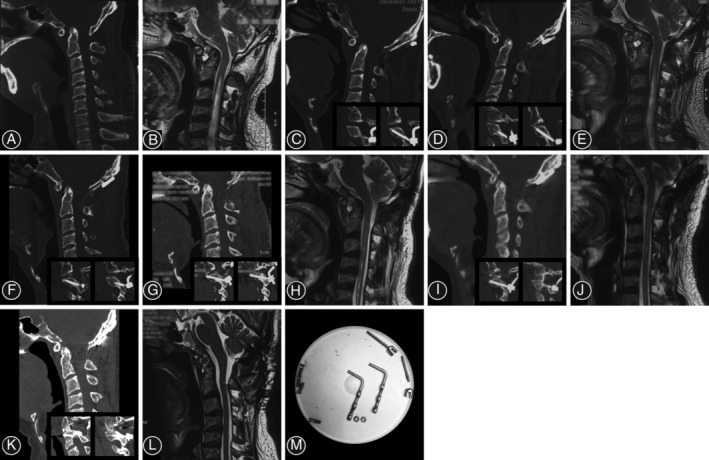
FIGURE 4.
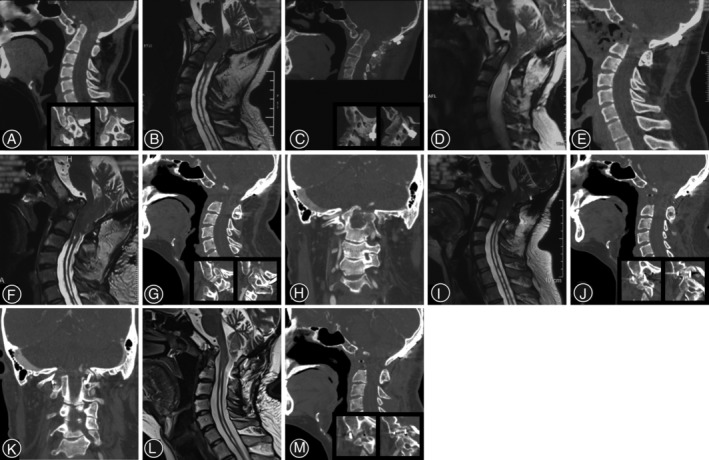
A 27‐year‐old male presented with gait instability and dysphagia, having undergone two operations. (A, B) CT and MRI image before first operation, showing basilar invagination and syringomyelia, with C1 assimilation and locked bi‐lateral joints. (C) CT image after first operation (posterior reduction and fixation, with foramen magnum decompression), showing dissatisfied reduction of basilar invagination. (D) MRI image of 3 months after first operation, showing enlargement of syrinx. (E, F): CT and MRI image after second operation (odontoidectomy), showing incomplete removal of the odontoid process, and unresolved neural compression. (G–I) CT and MRI image before PFDF, showing lock of bi‐lateral joints, coronal malformation of axis, neural compression, and persistent syrinx. (J–L) CT and MRI image after PFDF, showing reduction of basilar invagination, implantation of cages in bi‐lateral joints, with relief of neural compression. (M) CT image during follow‐up, showing bone fusion in bi‐lateral joints.
Clinical Assessments
During follow‐up, all patients showed significant improvement in symptoms. For patients undergoing PFDF surgery, the average JOA score increased from 13.50 ± 2.72 preoperatively to 15.14 ± 2.19 at the last follow‐up, the average SF‐12 score improved from 80.97 ± 13.40 preoperatively to 93.17 ± 14.25 at the last follow‐up. Similarly, patients who underwent odontoidectomy also experienced noticeable symptom improvement. Detailed data are presented in Tables 3 and 4.
TABLE 4.
Clinical assessments after PFDF.
| Variables | Preop | Follow‐up | Difference | t‐value | p‐value |
|---|---|---|---|---|---|
| Between Preop and Follow‐up | |||||
| JOA | 13.50 ± 2.47 | 15.14 ± 2.19 | 1.63 ± 1.91 | 4.553 | p < 0.001 |
| SF‐12 | 80.97 ± 13.40 | 93.17 ± 14.25 | 12.20 ± 10.60 | 3.818 | p = 0.003 |
Note: Clinical data of all patients who underwent PFDF.
Abbreviations: Follow‐up, at last follow‐up; JOA, the Japanese Orthopedic Association score; SF‐12, the Short Form‐12 score; Postop, postoperative; Preop, preoperative.
Discussion
In this study, we analyzed the surgical result of patients with failed atlantoaxial reduction, explored the difficulties in the revision surgery, proposed the surgical strategy and the associated risks and considerations. For different types of patients, both PFDF and odontoidectomy can achieve effective outcomes.
Previously, numerous articles have focused on the treatment of CVJ malformations, reporting various surgical techniques and concepts, which significantly enhance the success rate of treating CVJ malformations. 6 , 7 , 8 , 9 , 17 , 18 , 19 , 20 However, for challenging cases, where complex bony abnormalities are involved, the success rate of surgical treatment remains suboptimal. Patients with reduction failure or reduction loss, as well as those with unresolved or aggravated symptoms, require revision surgical interventions. 11 , 12 , 13 , 14 There is still a limited number of articles addressing revision strategies.
Difficulties in Treatment
For these patients, surgery stands as the sole effective method for revision treatment. These patients predominantly present with severe malformations, rendering the reduction process during surgery notably challenging. Both the failure rate of reduction and the recurrence rate of malformation are significantly increased. The underlying cause lies in the presence of severe atlantoaxial joint locking or contracture of the atlantoaxial ligaments. 21 , 22 , 23 Without thorough intra‐articular distraction, even substantial cervical traction fails to achieve reduction. Consequently, persistent malformation, neural compression, and unresolved neurological symptoms necessitate urgent revision surgery. Markedly lateral joint malformation showed in our cohort, characterized by sagittal joint inclination at an average of 131.47°.
Additionally, among the presented cases, three patients experienced implant fracture after their previous surgery. The primary contributing factor was the separation of the lateral atlantoaxial joints following the previous surgery, resulting in inadequate joint support and a lack of intervertebral space stability. 24 , 25 , 26 Consequently, the entire stress burden within the atlantoaxial region fell upon the internal fixation system before bony fusion could occur. This strain led to loosening of the internal fixation system, ultimately resulting in malformation recurrence.
For such patients, relying solely on posterior approaches to expand the internal fixation system proves insufficient for achieving rapid and robust bony fusion. Several factors contribute to this challenge:
Insufficient joint space support: the distraction during previous surgery results in empty lateral joint spaces, with residual soft tissue remaining. Consequently, bony fusion cannot occur within the joint space.
The posterior fixation system cannot guarantee sufficient stability. Additionally, lateral bone grafting alone cannot guarantee bony fusion.
Inadequate release of lateral joint constraints: reliance on cervical traction and posterior expansion alone does not effectively release the lateral joint constraints, resulting in stress during reduction. Failure to adequately release the lateral joint, coupled with reliance solely on cervical traction and posterior distraction for reduction, results in stress during deformity reduction.
Due to the lack of supporting structures between the lateral joints, the aforementioned internal stresses, as well as the dynamic stresses generated by cervical movements, are entirely borne by the internal fixation system. This leads to failure of the internal fixation system and subsequent loss of reduction. Frequently, this results in gradual deterioration of nerve compression and neurological symptoms in patients, even after immediate relief following surgery, necessitating revision with surgical treatment.
Surgical Strategies for Revision
Previous literature has reported cases of failed reduction and subsequent revision in the CVJ region. 11 , 12 , 13 , 14 , 27 , 28 , 29 , 30 , 31 The primary surgical strategies can be categorized as follows: anterior odontoidectomy, anterior approach distraction and fixation, and posterior approach distraction and fixation.
Anterior odontoidectomy is indicated for patients with robust bony fusion of the atlantoaxial joint in an unreduced position, that destruction is not feasible. 31 , 32 This method directly alleviates the neural compression caused by the odontoid process. However, this method carries risks of dural sac injury and infection, and its application is limited due to the high surgical complexity. 33 , 34 , 35 Additionally, following occipitocervical bony fusion, the extension range of the CVJ region is affected, thereby increasing the difficulty of the transoral approach. In such cases, the transnasal endoscopic approach is more suitable. In odontoidectomy, the application of intraoperative CT navigation allows for more precise removal of the odontoid process, thereby achieving more complete decompression and enhancing surgical safety. In this study, three cases showed robust bony fusion of bilateral atlantoaxial joint in preoperative examinations. All three patients experienced significant symptom relief following transnasal endoscopic odontoidectomy.
For patients with incomplete, insufficiently atlantoaxial bony fusion, distraction with fixation can be employed. Previous literature has reported significant therapeutic efficacy with the combined approach of anterior distraction followed by anterior or posterior fixation. 12 , 13 , 17 , 19 The advantage of anterior distraction lies in its ability to release tension on the anterior ligamentous complex of the atlantoaxial joint, thereby enhancing the reduction rate. However, this technique is associated with complex surgical approaches (anterior–posterior or, if removal of the posterior internal fixation systems is necessary, posterior–anterior–posterior), substantial operative difficulty, and a risk of complications such as infection.
In 2019, Goel et al. reported successful outcomes by combining posterior distraction with atlantoaxial screw fixation for revision surgery in these patients. 28 They emphasized that distracting the atlantoaxial joint posteriorly can enhance the reduction rate in cases of atlantoaxial dislocation. In 2017, we introduced the PFDF technique, which has demonstrated satisfactory surgical outcomes in treating various types of CVJ region anomalies. 9 , 23 , 36 , 37 , 38 , 39 , 40 , 41 This technique demonstrates continued effectiveness for patients with failed reduction as revision surgery.
The successful reduction of CVJ malformations hinges on achieving complete reduction and dispersing stress. PFDF technique offers the following advantages in this challenging condition: (i) lateral joint release and distraction facilitate the relief of joint locks and soft tissue tension, can convert irreducible osseous malformations into a reducible state when supplemented with intraoperative cervical traction; (ii) lateral joint release and distraction reduce stress generated in the lateral joints and anterior soft tissues; (iii) interarticular fusion cage placement provides support within the joint space, facilitating stress dispersion and maintaining the reduced position; (iv) interarticular fusion cage with autologous bone grafts confirm Wolff's law. The compressive stress in lateral joints promotes bony fusion; and (v) the posterior‐only approach reduces surgical risk and complexity. Revision surgery using this technique in 32 cases with incomplete bony fusion achieved significant relief of neural compression, and all patients experienced significant symptom relief. During follow‐up, no instances of reduction loss or fixation failure were observed. Bony fusion across the lateral joints was evident at 6 months postoperatively, providing adequate stability within the surgical segment.
Limitations
However, PFDF technique still has some limitations. First, as previously mentioned, for patients with bony fusion of the lateral joints or those with intractable lateral joint locking, the PFDF technique may encounter difficulties in clinical practice. Second, there is a certain risk associated with surgical manipulation of the lateral joints in patients with severe abnormal vertebral artery course. Third, Severe CVJ abnormalities increase the difficulty of posterior fixation and also place higher demands on the stability of the fixation system. Furthermore, cage implantation may increase the economic burden on patients to some extent.
When performing revision surgery, attention should be paid to the following aspects: (i) preoperative application of CT three‐dimensional reconstruction to evaluate whether solid bony fusion has formed between bilateral joints, as well as the feasibility of posterior distraction and reduction. For patients with fused or intractable locked lateral joints, odontoidectomy remains a viable option; (ii) preoperative CTA reconstruction and intraoperative precise exposure under microscopic visualization aids in recognizing the aberrantly coursing or scar‐encased vertebral arteries, thereby preventing vertebral artery injury; (iii) after dismantling the prior fixation system and removing all bone callus, the application of cervical traction facilitates distraction and release through the atlantoaxial joint space; (iv) adequate release of locked joints and soft tissue tension contribute to the successful reduction of osseous malformations; and (v) flexible selection of screw placement and fixation segments ensures surgical safety and local stability. This is a single center retrospective cohort study. Based on the previous results, we intend to conduct a multicenter randomized controlled trial to provide more robust evidence regarding the treatment and protocol of CVJ malformations. For patients who have experienced fixation failure, long‐term follow‐up after revision surgery is necessary to monitor the reliability of the new internal fixation system, or occurrence of any complications.
Conclusion
Severe atlantoaxial joint locking or ligament contracting are the fundamental cause of reduction and fixation failure. Anterior odontoidectomy is indicated for patients with robust bony fusion of the atlantoaxial joint in an unreduced position. PFDF technique is safe and effective for patients with incomplete atlantoaxial bony fusion. It demonstrates favorable reduction outcomes in CVJ malformations. Preoperative assessment of surgical feasibility and vertebral artery status, along with precise intraoperative techniques and adequate distraction, ensures surgical safety and efficacy.
Author Contributions
BZ, YD, WD and ZC were responsible for conceptualization. WD and ZC were responsible for obtaining funding and supervising the study. All authors were responsible of acquiring and analysis of data. BZ and YD were responsible of drafting, and BZ, YD, WD and ZC were responsible of the revision of the work.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors and are in agreement with the manuscript.
Acknowledgments
This study was supported by National Key R&D Program of China, “Research on Prevention and Control of Common Diseases”, Supported by Ministry of Science & Technology of PRC, (2023YFC2509700), Beijing Natural Science Foundation Grant (L212039), National High Level Hospital Clinical Research Funding (2022‐PUMCH‐D‐004), Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (XMLX202138), The “Young Talents” Program, supported by Beijing Municipal Hospital Administration (QML20210801), Research and application of clinical characteristic diagnosis and treatment Program, Supported by Beijing Municipal Science & Technology Commission (Z221100007422019), The CAMS Innovation Fund for Medical Sciences (CIFMS #2021‐1‐I2M‐025).
Contributor Information
Wanru Duan, Email: duanwanru@xwhosp.org.
Zan Chen, Email: chenzan66@163.com.
References
- 1. Menezes AH, Traynelis VC. Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b). Childs Nerv Syst. 2008;24(10):1091–1100. [DOI] [PubMed] [Google Scholar]
- 2. Lopez AJ, Scheer JK, Leibl KE, Smith ZA, Dlouhy BJ, Dahdaleh NS. Anatomy and biomechanics of the craniovertebral junction. Neurosurg Focus. 2015;38(4):E2. [DOI] [PubMed] [Google Scholar]
- 3. Dahdaleh NS, El‐Tecle N, Cloney MB, Shlobin NA, Koski TR, Wolinsky JP. Functional anatomy and biomechanics of the craniovertebral junction. World Neurosurg. 2023;175:165–171. [DOI] [PubMed] [Google Scholar]
- 4. Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014;4(3):197–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meng H, Xin Z, Zhang B, Qi M, Du Y, Duan W, et al. A Global Bibliometric and Visualization Analysis of Craniovertebral Junction Bony Abnormalities Based on VOSviewer and Citespace. World Neurosurg. 2024;185:e1361–e1371. [DOI] [PubMed] [Google Scholar]
- 6. Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281–286. [DOI] [PubMed] [Google Scholar]
- 7. Chandra PS, Kumar A, Chauhan A, Ansari A, Mishra NK, Sharma BS. Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation: a novel pilot technique. Neurosurgery. 2013;72(6):1040–1053. [DOI] [PubMed] [Google Scholar]
- 8. Salunke P, Sahoo S, Khandelwal NK, Ghuman MS. Technique for direct posterior reduction in irreducible atlantoaxial dislocation: multi‐planar realignment of C1‐2. Clin Neurol Neurosurg. 2015;131:47–53. [DOI] [PubMed] [Google Scholar]
- 9. Chen Z, Duan W, Chou D, Guan J, Liu Z, Jian Q, et al. A safe and effective posterior intra‐articular distraction technique to treat congenital atlantoaxial dislocation associated with basilar invagination: case series and technical nuances. Oper Neurosurg. 2021;20(4):334–342. [DOI] [PubMed] [Google Scholar]
- 10. Algattas HN, Alattar AA, Okonkwo DO, Wang EW, Snyderman CH, Hamilton DK, et al. A novel classification and management scheme for craniocervical junction disorders with ventral neural element compression. J Neurosurg. 2024;140(2):585–594. [DOI] [PubMed] [Google Scholar]
- 11. Hedequist D, Bekelis K, Emans J, Proctor MR. Single stage reduction and stabilization of basilar invagination after failed prior fusion surgery in children with Down's syndrome. Spine. 2010;35(4):E128–E133. [DOI] [PubMed] [Google Scholar]
- 12. Tan M, Jiang X, Yi P, Yang F, Tang X, Hao Q, et al. Revision surgery of irreducible atlantoaxial dislocation: a retrospective study of 16 cases. Eur Spine J. 2011;20(12):2187–2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yang J, Ma X, Xia H, Wu Z, Ai F, Yin Q. Transoral anterior revision surgeries for basilar invagination with irreducible atlantoaxial dislocation after posterior decompression: a retrospective study of 30 cases. Eur Spine J. 2014;23(5):1099–1108. [DOI] [PubMed] [Google Scholar]
- 14. Duan W, Chou D, Jiang B, Liu Z, Zhao X, Xia Z, et al. Posterior revision surgery using an intraarticular distraction technique with cage grafting to treat atlantoaxial dislocation associated with basilar invagination. J Neurosurg Spine. 2019;1–9:525–533. [DOI] [PubMed] [Google Scholar]
- 15. Berjano P, Bassani R, Casero G, Sinigaglia A, Cecchinato R, Lamartina C. Failures and revisions in surgery for sagittal imbalance: analysis of factors influencing failure. Eur Spine J. 2013;22(Suppl 6):S853–S858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chang P‐Y, Yen Y‐S, Wu J‐C, Chang H‐K, Fay L‐Y, Tu T‐H, et al. The importance of atlantoaxial fixation after odontoidectomy. J Neurosurg Spine. 2016;24(2):300–308. [DOI] [PubMed] [Google Scholar]
- 17. Wang C, Yan M, Zhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine. 2006;31(11):E306–E313. [DOI] [PubMed] [Google Scholar]
- 18. Jian FZ, Chen Z, Wrede KH, Samii M, Ling F. Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery. 2010;66(4):678–687. [DOI] [PubMed] [Google Scholar]
- 19. Wei G, Shi C, Wang Z, Xia H, Yin Q, Wu Z. Surgical outcome and prognostic analysis of transoral atlantoaxial reduction plate system for basilar invagination: a voxel‐based morphometry study. J Bone Jt Surg Am. 2016;98(20):1729–1734. [DOI] [PubMed] [Google Scholar]
- 20. Yin YH, Tong HY, Qiao GY, Yu XG. Posterior reduction of fixed atlantoaxial dislocation and basilar invagination by atlantoaxial facet joint release and fixation: a modified technique with 174 cases. Neurosurgery. 2016;78(3):391–400. [DOI] [PubMed] [Google Scholar]
- 21. Xia ZY, Duan WR, Zhao XH, Jian FZ, Chen Z. Computed tomography imaging study of basilar invagination and atlantoaxial dislocation. World Neurosurg. 2018;114:e501–e507. [DOI] [PubMed] [Google Scholar]
- 22. Sarat Chandra P, Bajaj J, Singh PK, Garg K, Agarwal D. Basilar invagination and atlantoaxial dislocation: reduction, deformity correction and realignment using the DCER (distraction, compression, extension, and reduction) technique with customized instrumentation and implants. Neurospine. 2019;16(2):231–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Guan J, Jian F, Yao Q, Yuan C, Zhang C, Ma L, et al. Quantitative reduction of basilar invagination with atlantoaxial dislocation by a posterior approach. Neurospine. 2020;17(3):574–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bo X, Wang W, Chen Z, Liu Z. Compression‐distraction reduction surgical verification and optimization to treat the basilar invagination and atlantoaxial dislocation: a finite element analysis. Biomed Eng Online. 2016;15(Suppl 2):168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bo X, Wang W, Chen Z, Liu Z. Research on the strategy of reduction operation of basilar invagination combined with atlantoaxial dislocation. J Mech Med Biol. 2020;20(5):2050028. [Google Scholar]
- 26. Zhao G, Song M, Duan W, Chen Z, Xue Y. Biomechanical investigation of intra‐articular cage and cantilever technique in the treatment of congenital basilar invagination combined with atlantoaxial dislocation: a finite element analysis. Med Biol Eng Comput. 2022;60(8):2189–2199. [DOI] [PubMed] [Google Scholar]
- 27. Ma X, Yin Q, Xia H, Wu Z, Yang J, Liu J, et al. The application of atlantoaxial screw and rod fixation in revision operations for postoperative re‐dislocation in children. Arch Orthop Trauma Surg. 2015;135(3):313–319. [DOI] [PubMed] [Google Scholar]
- 28. Goel A, Dhar A, Shah A, Rai S, Bakale N, Vaja T. Revision for failed craniovertebral junction stabilization: a report of 30 treated cases. World Neurosurg. 2019;127:e856–e863. [DOI] [PubMed] [Google Scholar]
- 29. Du YQ, Qiao GY, Yin YH, Li T, Yu XG. Posterior atlantoaxial facet joint reduction, fixation and fusion as revision surgery for failed suboccipital decompression in patients with basilar invagination and atlantoaxial dislocation: operative nuances, challenges and outcomes. Clin Neurol Neurosurg. 2020;194:105793. [DOI] [PubMed] [Google Scholar]
- 30. Zou X, Wang B, Yang H, Ge S, Ouyang B, Chen Y, et al. Transoral intraarticular cage distraction and C‐JAWS fixation for revision of basilar invagination with irreducible atlantoaxial dislocation. BMC Musculoskelet Disord. 2020;21(1):766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Duan W, Chou D, Jian F, Chen Z. Navigated transoral odontoidectomy to treat congenital basilar invagination after failed posterior reduction and fusion. Neurosurg Focus: Video. 2020;3(1):V8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aldahak N, Richter B, Bemora JS, Keller JT, Froelich S, Abdel Aziz KM. The endoscopic endonasal approach to cranio‐cervical junction: the complete panel. Pan Afr Med J. 2017;27:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shriver MF, Kshettry VR, Sindwani R, Woodard T, Benzel EC, Recinos PF. Transoral and transnasal odontoidectomy complications: a systematic review and meta‐analysis. Clin Neurol Neurosurg. 2016;148:121–129. [DOI] [PubMed] [Google Scholar]
- 34. Tubbs RS, Demerdash A, Rizk E, Chapman JR, Oskouian RJ. Complications of transoral and transnasal odontoidectomy: a comprehensive review. Childs Nerv Syst. 2016;32(1):55–59. [DOI] [PubMed] [Google Scholar]
- 35. Grose E, Moldovan ID, Kilty S, Agbi C, Lamothe A, Alkherayf F. Clinical outcomes of endoscopic endonasal Odontoidectomy: a single‐center experience. World Neurosurg. 2020;137:e406–e415. [DOI] [PubMed] [Google Scholar]
- 36. Xinghua Z, Zhiyuan X, Fengzeng J, Zan C, Nuerosugery DO, Hospital X, et al. The study and design of atlantoaxial lateral mass intervertebral fusion cage for BI‐AAD patients. Chin J Neurosurg Dis Res. 2017;16(6):485–489. [Google Scholar]
- 37. Duan W, Chou D, Jian F, Chen Z. Posterior intra‐articular distraction with cage placement to treat congenital atlantoaxial dislocation associated with basilar invagination. Neurosurg Focus: Video. 2020;3(1):V2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Liu Z, Zhao X, Guan J, Duan W, Goel A, Xia Z, et al. Quantitative reduction of basilar invagination: correction target of Clivo‐axial angle. Clin Spine Surg. 2020;33(8):E386–E390. [DOI] [PubMed] [Google Scholar]
- 39. Liu Z, Jian Q, Duan W, Guan J, Zhang C, Zhang B, et al. Atlantoaxial dislocation with bony fusion of C1/2 facet joints treated with posterior joint release, distraction and reduction. Spine Surg Relat Res. 2022;6(2):175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang B, Qi M, Xin Z, Du Y, Zhang C, Liu Z, et al. Intra‐articular distraction versus decompression to treat basilar invagination without atlantoaxial dislocation: a retrospective cohort study of 54 patients. Neurospine. 2023;20(2):498–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zhou M, Sun P, Du Y, Zeng G, Chen Z, Duan W. Posterior intra‐articular distraction technique to treat pediatric atlantoaxial instability. Childs Nerv Syst. 2024;40:2153–2160. [DOI] [PubMed] [Google Scholar]


