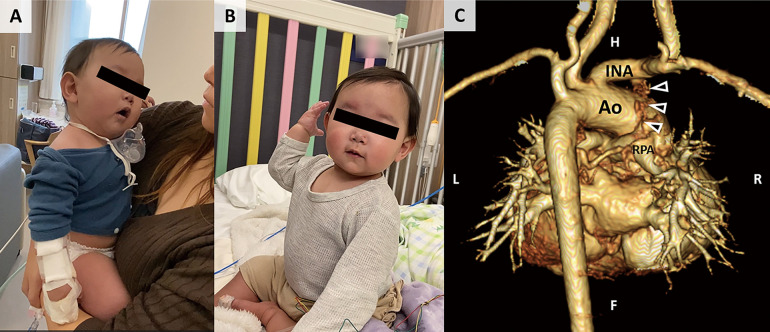
A 13-month-old girl with tetralogy of Fallot (TOF) had undergone the modified Blalock–Taussig shunt procedure when she was 3 months old and presented to the pediatric department (Yamaguchi University) with SpO2 60%. After a bout of crying, she showed a paroxysm of hyperpnea (rapid and deep respiration), irritability, and increasing cyanosis, followed by lethargy (Figure A; Supplementary Movie). The systolic heart murmur at the left sternal border was diminished and oxygen saturation decreased to 30%. She was held in a knee-chest position with oxygen administration, as well as sedatives, propranolol, and plasma volume expander. Her oxygen saturation increased to 75% with improvement in symptoms (Figure B). Contrast-enhanced computed tomography revealed complete occlusion of the shunt (Figure C).
Figure.
(A) Paroxysm of hyperpnea (rapid and deep respiration), irritability, and increasing cyanosis, followed by lethargy. (B) Sedatives, propranolol, and plasma volume expander were administered, and oxygen saturation increased to 75% with improvement in the symptoms. (C) Near-total occlusion of the modified Blalock–Taussig shunt (arrowheads). Ao, aorta; INA, innominate artery; RPA, right pulmonary artery.
Children with TOF have a risk developing hypoxic spells. Hypoxic spells usually occur after crying, feeding, or defecation. A severe spell occasionally leads to convulsions, cerebrovascular events, or even death. The differential diagnoses of pediatric hypoxic spells include breath-holding, seizures, cardiac arrhythmias, gastroesophageal reflux, neurological and metabolic disorders, infections, sudden infant death syndrome, anatomic abnormalities, toxic exposure, and hematologic disorders. Comprehensive assessment, including medical history, physical examination, and diagnostic tests, is crucial to identify the underlying cause.
In the present patient, disappearance of the continuous murmur suggested near-total occlusion of the modified Blalock–Taussig shunt. The systolic heart murmur at the left sternal border was diminished due to the decreased blood flow through the right ventricular outflow tract. Emergency intracardiac correction was performed, and the patient was subsequently discharged without neurological sequelae.
Funding / Acknowledgments
None.
Ethics
Written informed consent was obtained from the patient’s parent.
Supplementary Files
Supplementary Movie.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Movie.