Abstract
The concentration of PM2.5 (particulate matter with a diameter < 2.5 µm) on Sumatra Island has increased, mainly because of forest and peatland fires, transportation, and industry. Biomass burning releases partially burned carbon into the atmosphere, resulting in a smoky haze containing PM2.5. Air quality has deteriorated quickly, and PM2.5 has become a major health hazard in Indonesia. Studies on long-term exposure to PM2.5 have indicated its associations with both morbidity and mortality. Here, we measured long-term (2000–2014) exposure to PM2.5 on the basis of satellite-derived aerosol optical depth measurements (1 × 1 km2) used to predict ground-level PM2.5 concentrations. Additionally, population data on Sumatra Island residents from the fourth wave of the Indonesian Family Life Survey (IFLS) were obtained. We investigated the association between long-term PM2.5 exposure and mortality with a retrospective cohort study design. A total of 2409 subjects aged ≥ 40 years participated in the IFLS-3 beginning in November 2000, and we examined mortality outcomes until the IFLS-5 in September 2014. We used Cox regression models to calculate hazard ratios (HRs) of mortality associated with PM2.5 exposure. According to the adjusted model, the mortality HRs per 10 µg/m3 increase in PM2.5 concentration were 1.10 (95% CI 1.03, 1.17) for all natural causes, 1.17 (95% CI 1.05, 1.25) for cardiovascular causes, and 1.19 (95% CI 1.04, 1.36) for respiratory causes. Long-term exposure to PM2.5 was associated with all-natural, cardiovascular, and respiratory mortality on Sumatra Island, where PM2.5 levels exceed the WHO and US-EPA air quality standards.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10661-024-13323-5.
Keywords: Particulate matter, Natural causes, Cardiovascular causes, Respiratory causes, Mortality
Introduction
Exposure to air pollution is associated with increased cardiovascular mortality and morbidity (Cesaroni et al., 2014; Patanè, 2020; Tibuakuu et al., 2018). Globally, particulate air pollution is suggested to be responsible for > 4 million deaths every year (Jiang et al., 2016; Thangavel et al., 2022). Notably, particulate matter with a diameter of < 2.5 µm (PM2.5) can be deposited in the upper and lower airways. Because of its small size, it can enter the bloodstream via the alveolar capillaries and can reach more deeply into the lungs and circulation, with the potential to cause serious health problems (Anderson et al., 2012; Schulze et al., 2017; Xing et al., 2016). In addition to genetic and lifestyle risk factors, exposure to air pollution, specifically PM2.5, has been implicated in deleterious outcomes and has been linked to cardiovascular disease (CVD) and stroke mortality (Hayes et al., 2020; Lee et al., 2018). PM is often considered the most policy-relevant criterion among the World Health Organization criteria because it is emitted from the burning of fossil fuels in road traffic, shipping, and power generation. It affects almost all body organ systems (Babatola, 2018; Perera, 2017).
The mitigation of air pollution is urgently needed in Indonesia, where air quality has deteriorated quickly due to rapid industrialization and urbanization (Kim Oanh et al., 2006; Santoso et al., 2020; Sofia et al., 2020). On Sumatra Island, aerosol pollutants can linger in the environment for weeks to months at elevated levels, contributing to regional pollution (Crippa et al., 2016; Santoso et al., 2022; Sumaryati et al., 2019). There are no studies on the long-term effects of air pollution on mortality in Indonesia because of a lack of direct measurements (Purnomo et al., 2019; Siregar et al., 2022a, 2022b). However, prior to 2015, PM2.5 was not a priority in the Indonesian government’s air pollution management strategy (Purnomo et al., 2019). In the present study, long-term PM2.5 was estimated via high-resolution satellite data from the National Aeronautics and Space Administration (NASA) via the aerosol optical depth (AOD) satellite. It is possible to use AOD-PM2.5 concentration readings to estimate actual ambient PM2.5 levels in areas without ground-based air monitors. Studies have confirmed the relationship between AOD measurements and ground-based PM2.5 concentrations (Braggio et al., 2020). In addition, we assessed the long-term effects on mortality in a large elderly cohort (the Indonesian Family Life Survey (IFLS)) on Sumatra Island from 2000 to 2014, as most forest and peatland fires in Indonesia occur on this island.
Materials and methods
Study population
We included a total of 2409 subjects who participated in the third wave of the IFLS and were recontacted from June through November 2000 (Supplemental Material, Fig. 1S); we also examined mortality outcomes through record linkage to the death registry until September 2014. The adult participants were aged ≥ 40 years, completed the chronic-type conditions (B3B_CD3) questionnaire, and lived on Sumatra Island. This study excluded participants with incomplete information regarding the variables needed for assessment, those with invalid home address information, and those who moved to another city not included in the IFLS area. The complete IFLS data and guidelines are publicly available on the RAND Corporation website (https://www.rand.org/labor/FLS/IFLS/ifls5.html). RAND, Survey Meter, and Gadjah Mada University, which undertook IFLS-4 and IFLS-5, obtained ethical approval for these waves.
Cohort follow-up and mortality assessment
The baseline survey determined vital status by responses to follow-up questionnaires and other mailings to study participants. Book 3A consisted of Adult Information Part 1 (Retrospective Information), and Book 3B consisted of Adult Information Part 2 (Current Information). We calculated hazard ratios (HRs) for deaths categorized according to the International Statistical Classification of Diseases, 10th Revision (ICD-10; WHO 2010) to define deaths due to all-natural causes (codes A00-R99), CVDs (100–99), and respiratory diseases (J00-47, 80–99). Study participants were excluded from the analyses if they died within 1 year of enrollment or were lost to follow-up by the end of 2014.
Exposure assessment
The annual PM2.5 concentrations for Sumatra Island from 2000 to 2014 were derived via a prediction model that is based on satellite AOD measurements. This study employed Quantum Geographic Information System (QGIS) software (version 3.4.15) to process and analyze these AOD measurements. QGIS was used to convert the unitless AOD values into PM2.5 concentrations (µg/m3) and apply the inverse distance weighted (IDW) interpolation method to visualize the data across Sumatra Island. This open-source GIS software has proven essential for addressing spatial analysis challenges and generating insights into PM2.5 distributions (Talib et al., 2022). However, there are certain limitations in predicting PM2.5 from AOD. Research has consistently highlighted that smoke from forest fires can lead to overestimation or misinterpretation of PM2.5 concentrations derived from AOD. This occurs because the complex interaction between smoke and satellite observations complicates the accurate retrieval of aerosol properties (Braggio et al., 2020; Zhang et al., 2023).
To derive AOD values for the 1-km grid cells, we used the GADM version 2.8 map layer of Indonesia’s administrative areas. The GADM (Global Administrative Areas Database) provides high-resolution data for state administrative regions worldwide, covering all levels and periods (https://gadm.org/). We determined the AOD value for each 1-km grid cell by calculating the area-weighted average of the AOD values from the intersecting administrative polygons. Patients’ geocoded addresses were then matched to the corresponding PM2.5 concentration areas on the basis of spatial location and year (Siregar et al., 2022a, 2022b).
Study participants provided detailed address history upon study enrollment and addresses for the year prior; PM2.5 predictions were averaged for the year prior for each patient. The data on the exposure of PM2.5 concentrations from the QGIS software are provided in the Supplemental Material, Table S1.
Statistical analysis
The association of PM2.5 (2000–2014) with mortality was examined via proportional hazards regression models adjusted for a wide range of individual risk factors. Plots of cumulative log hazard against log survival time for categories of the explanatory variables indicated that the proportional hazards assumption held well. Both total and cause-specific mortality were assessed. Our basic models included age only. In the adjusted models, we added factors that we identified a priori as potential confounders, including sex (man, woman), body mass index (BMI), education (low if they had < 12 years of school attainment, high if they had ≥ 12 years of school attainment), smoking status (never, i.e., they never had a smoking habit; current, i.e., they currently had a smoking habit; or former, i.e., they formerly had a smoking habit), socioeconomic (SES) status (poor, average, rich), diabetes (yes/no), and hypertension (yes/no). BMI was treated as a quintile, given its potential nonlinear relationship with mortality. Since diabetes and hypertension might mediate the relationship between particle exposure and mortality, we examined models with and without adjustment for diabetes and hypertension.
We also conducted stratified analyses by age (< 65 and ≥ 65 years) and sex (male and female) to examine the associations between PM2.5 and mortality. We categorized BMI into two categories according to the standard definition: normal/underweight (BMI < 25) and overweight/obese (BMI ≥ 25).
A p value < 0.05 indicated statistical significance, and R Studio was used to perform all the statistical analyses.
Results and discussion
PM2.5 concentration retrieved from satellite AOD measurements
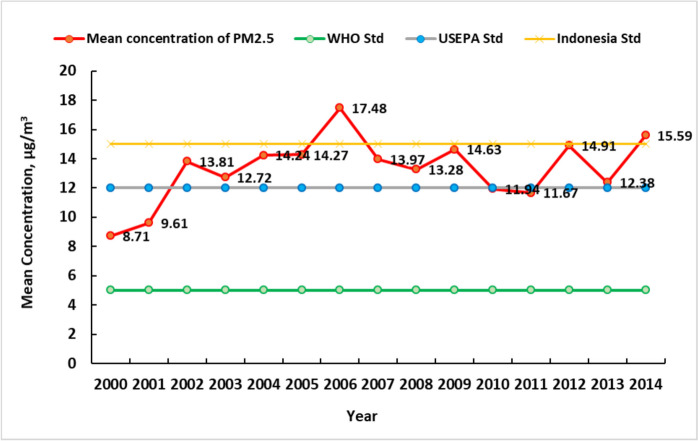
Figure 1 shows the distribution of the mean annual PM2.5 concentration from 2000 to 2014 for each 1 × 1 km2 grid throughout Sumatra Island, Indonesia. On Sumatra Island, the mean annual PM2.5 concentration was lowest in 2000, at 8.71 µg/m3, and was highest in 2006, at 17.48 µg/m3 (Fig. 2).
Fig. 1.
Annual average PM2.5 concentrations (2000–2014) on Sumatra Island
Fig. 2.
Mean annual PM2.5 concentration trend on Sumatra Island from 2000 to 2014 compared with the WHO, US-EPA and Indonesian NAAQS standards
On Sumatra Island, the average PM2.5 concentration from 2000 to 2014 was 13.3 µg/m3. The annual PM2.5 concentration generally increased by 40% during the study period from 2000 to 2014, but it increased and then decreased in some years.
Baseline characteristics
In the first year, 15 deaths were excluded, and 20 participants lost to follow-up by the end of 2014 were excluded. A final sample of 2374 participants was included for PM2.5 estimation and analysis. Table 1 presents selected baseline participant characteristics according to whether the subjects died during follow-up.
Table 1.
Baseline characteristics of 2374 adult participants
| Characteristic | Total (n = 2374) | Death % (n = 487) | Nondeath % (n = 1887) |
|---|---|---|---|
| Sex | |||
| Female | 1226 (51.6) | 49.3 | 52.8 |
| Male | 1148 (48.4) | 50.7 | 47.2 |
| Age | |||
| 40–65 | 1743 (73.4) | 35.8 | 80.5 |
| ≥ 65 | 631 (26.6) | 64.2 | 19.5 |
| BMI | |||
| Under/normal weight (BMI < 25) | 1406 (59.2) | 56.3 | 60.6 |
| Overweight/Obese (BMI ≥ 25) | 968 (40.8) | 43.7 | 39.4 |
| Education | |||
| Low (if they had < 12 y) | 2046 (86.2) | 66.1 | 93.5 |
| High (if they had ≥ 12 y) | 328 (13.8) | 33.9 | 6.5 |
| SES | |||
| Low | 791 (33.3) | 30.3 | 34.0 |
| Medium | 1101 (46.4) | 46.5 | 47.2 |
| High | 482 (20.3) | 23.2 | 18.8 |
| Smoking behavior | |||
| Never | 1243 (52.4) | 30.6 | 60.7 |
| Current | 993 (41.8) | 54.2 | 37.4 |
| Former | 138 (5.8) | 15.2 | 1.9 |
| Residency area | |||
| Urban | 988 (41.6) | 38.4 | 42.0 |
| Rural | 1386 (58.4) | 61.6 | 58.0 |
| Chronic conditions | |||
| Hypertension | |||
| Yes | 521 (21.9) | 18.3 | 22.0 |
| No | 1853 (78.1) | 81.7 | 78.0 |
| Diabetes | |||
| Yes | 97 (2.7) | 3.7 | 2.4 |
| No | 2277 (97.3) | 96.3 | 97.6 |
A total of 487 subjects died during follow-up, among whom 460 died from all-natural causes, 144 from CVDs, 197 from respiratory diseases, 43 from lung cancer, and 27 from external causes (Table 2). As expected, the deceased subjects were male, older, and overweight/obese; were more likely to be current/past smokers; had a higher prevalence of diabetes and hypertension; had lower education levels; had low/medium SES; and lived in rural areas.
Table 2.
Mortality outcomes after 14 years of follow-up at the end of the study in 2014
| ICD-10 codes | Mortality cause | No. of deaths | Percent |
|---|---|---|---|
| A00-R99 | All-natural causes | 460 | 94.5 |
| 100–99 | Cardiovascular diseases | 144 | 29.6 |
| J00–47, 80–99 | Respiratory diseases | 197 | 40.5 |
| C34.0–9 | Lung cancer | 43 | 8.8 |
| S00-T99 | External causes | 27 | 5.5 |
| All included codes | All causes | 487 |
Associations between PM2.5 and mortality
According to both the basic and adjusted models, particulate air pollution was found to be associated with an increased risk of cardiopulmonary mortality (Table 3). In the adjusted model, an increase of 10 µg/m3 in PM2.5 corresponded to 10% (95% CI 1.03, 1.17), 17% (95% CI 1.05, 1.25), and 19% (95% CI 1.04, 1.36) increased risks of natural, cardiovascular, and respiratory mortality, respectively.
Table 3.
Hazard ratios (95% CI) of mortality associated with a 10-µg/m3 increase in the average PM2.5 level at baseline (deaths within the first year were excluded)
| Cause of death | Basic modela | Adjusted modelb | Adjusted modelc |
|---|---|---|---|
| All natural causes | 1.16 (1.10, 1.23)** | 1.13 (1.05, 1.30)** | 1.10 (1.03, 1.17)** |
| Cardiovascular Diseases | 1.23 (1.08, 1.40)** | 1.20 (1.07, 1.33)** | 1.17 (1.05, 1.25)** |
| Respiratory Diseases | 1.26 (1.22, 1.30)** | 1.23 (1.06, 1.42)** | 1.19 (1.04, 1.36)* |
| Lung cancer | 1.05 (0.95, 1.16) | 1.03 (0.90, 1.18) | 1.02 (0.79, 1.32) |
| External causes | 1.04 (0.89, 1.22) | 1.02 (0.86, 1.21) | %1.%2 (0.75, 1.36) |
*p < 0.05; **p < 0.01
aCovariates included age
bCovariates included age, sex, BMI, education, SES, smoking status, and residence area
cCovariates included age, sex, BMI, education, SES, smoking status, residence area, diabetes, and hypertension
In stratified analyses (Table 4), the association between a 10 µg/m3 increase in PM2.5 and mortality was closer to null in both age groups (< 65 and ≥ 65 years) for all mortality outcomes, with significant differences by age for cardiovascular mortality (HR = 1.33; 95% CI 1.12, 1.58 vs. HR = 1.17; 95% CI 1.00, 1.37; interaction p value 0.048) and respiratory mortality (HR = 1.40; 95% CI 1.01, 1.94 vs. HR = 1.11; 95% CI 0.99, 1.24; interaction p value 0.035). There is a lack of studies proving consistent differences in associations between PM2.5 and any of the outcomes according to sex (Table 4) or education level (see Supplemental Material, Table S2) (Wong et al., 2015).
Table 4.
Hazard ratio (95% CI) per 10 µg/m3 increase in PM2.5 in stratified analysis by age or sex with exposure at baseline
| Cause of death | Age < 65 years | Age ≥ 65 years | Interactiona | Male | Female | Interactiona |
|---|---|---|---|---|---|---|
| All natural causes | 1.21 (1.05, 1.39)** | 1.12 (1.02, 1.23)* | 0.08 | 1.26 (1.06, 1.50)** | 1.10 (1.02, 1.19)* | 0.84 |
| Cardiovascular | 1.33 (1.12, 1.58)** | 1.17 (1.00, 1.37) | 0.048 | 1.15 (1.03, 1.29)* | 1.29 (1.05, 1.58)* | 0.45 |
| Respiratory | 1.40 (1.01, 1.94)* | 1.11 (0.99, 1.24) | 0.035 | 1.26 (1.02, 1.56)* | 1.04 (0.84, 1.29) | 0.21 |
| Lung cancer | 1.03 (0.92, 1.15) | 0.98 (0.91, 1.05) | 0.21 | 1.20 (0.88, 1.64) | 1.46 (0.96, 2.22) | 0.57 |
| External causes | 0.88 (0.48, 1.61) | 1.08 (0.86, 1.36) | 0.73 | 1.01 (0.66, 1.55) | 1.05 (0.36, 3.06) | 0.91 |
ap value for the interaction term in the model for the combined dataset
*p < 0.05; **p < 0.01
In this study, we showed that greater exposure to ambient PM2.5 was associated with mortality from natural (10% increase per 10 µg/m3 PM2.5) and cardiovascular causes (17% increase) and with mortality due to respiratory disease (19% increase), specifically in people ≥ 65 years of age. This result was slightly greater than that of a meta-analysis of 84 cohort studies that reported a 10% increase (95% CI 1.02, 1.19) in CVD mortality and a 7% increase (95% CI 1.04, 1.09) in all-cause mortality per 10 µg/m3 increase in PM2.5 (Pranata et al., 2020).
The survival probability at 168 months is shown in Fig. 3. The results revealed a greater decrease in the survival probability for all causes of death in male participants than in female participants.
Fig. 3.
Probability of survival (Kaplan‒Meier) of all causes of death according to sex. The y-axis indicates the survival probability along the x-axis from baseline to years of follow-up. The differences between sexes were tested by the log-rank test (p value < 0.0001)
The risk we identified for respiratory mortality was similar to that reported in other Chinese studies and higher than that reported in a study in Hong Kong (Li et al., 2019, 2021; Mokoena et al., 2019). The heterogeneity in effect sizes for respiratory mortality among studies may be due to the various characteristics of the study context, such as exposure assessment methodology, air pollution levels and components, and population sensitivity to air pollution. On Sumatra Island, the air pollution sources may differ from those in other countries, with higher air pollution contributions from biomass burning (forest and peatland fires) and motor vehicle exhaust.
In a previous study, we reported that the relative reduction in respiratory mortality was greater in the < 64-year age group than in the ≥ 65-year age group (Hoek et al., 2013; Mokoena et al., 2019; Wang et al., 2017), suggesting heterogeneity of air pollution effects among age groups. In our stratified analysis, participants ≥ 65 years of age were potentially at lower risk from air pollution than those < 65 years, probably due to a healthy survival effect. Particularly for older people, caution is needed when interpreting mortality effects across long study periods, which may vary because of changes in the susceptibility of survivors in different periods of follow-up. Our results revealed no sex differences. Indeed, the current evidence for sex differences in susceptibility is weak and inconsistent among studies (Wong et al., 2015).
Among males and females, respiratory mortality was greater in males than in females. In Indonesia, smoking rates in females are lower than those in males and internationally. Anecdotal evidence suggests that their disinclination to smoke is commonly attributed to cultural values, which stigmatize women smokers as morally flawed while at the same time sanctioning smoking by men (Ayuningtyas et al., 2021; Barraclough, 1999; Holipah et al., 2020).
Compared with association studies of short-term effects, even fewer studies in Indonesia have examined the association between long-term exposure to air pollution and human health. To date, there has been only one published air pollution cohort study in Indonesia (Haryanto & Djafri, 2020).
The results of our study from a satellite-based measure of PM2.5 provide new evidence on mortality from the long-term effects of PM2.5 exposure. On Sumatra Island, pollution levels are generally heterogeneous; additionally, while our approach applies to an older population with limited mobility, it may be less so for highly mobile populations.
In recent years, Indonesia has been undergoing a stage of transition from economic development to include environmental issues, for which tighter air quality standards are needed. Reliable estimates of the health effects of air pollution from epidemiologic studies are urgently needed to provide essential scientific evidence for environmental accountability and health impact assessments of new air quality objectives. Quantitative knowledge about the relationship between exposure to air pollution and health outcomes is crucial for assessing the health impact of air pollution and its implications for relevant policy-making. Our study fills a critical gap in missing long-term effect estimates for Indonesia and the impact on life expectancy and value of life years, which could be gained because of a reduction in pollutants due to government intervention. The estimates from this study can also support the cost–benefit ratio for achieving clean air and form the basis for important public health information, including air pollution risk communication.
Strengths and limitations
The main strength of our study was the assessment of all the causes of death according to the ICD-10 codes, which eliminated the possibility of misclassification of cases and measurement errors; however, when interpreting the results, such possible errors should be considered. There are several limitations of our study. First, the pollution levels used were based on city-wide averages (reflecting background exposure levels) rather than personal exposure measurements. Consequently, this was expected to result in exposure measurement error and bias in terms of the precision and strength of the risk estimates. Second, the cause of death was self-reported by the family member and the village head office administration on the basis of the doctor’s diagnosis, and a questionnaire was used to collect information on the covariates. Thus, recall bias was possible, considering that people with a low SES might have been less informed about the exact mortality diagnosis. Third, we could not explore the associations of air pollutants with the causes of mortality subtypes due to the limited detail and number of cases, which involved different pathogens. Fourth, this study did not include alcohol and physical activity because controlling for too many potential confounders can lead to or aggravate data sparsity or multicollinearity problems, particularly when the number of covariates is large in relation to the study size (Greenland et al., 2016). However, from the observation of IFLS data comparing smokers and nonsmokers, the percentage of alcohol and tobacco expenditures is greater in smokers (Dartanto et al., 2018; Martini et al., 2022).
Policy implications
Our study provides accurate data on CVD and mortality as a result of long-term PM2.5 exposure, which is exacerbated by forest and peatland fires, particularly on Sumatra Island, Indonesia. We expect our results to fill the gap in the literature regarding the relationship between long-term exposure to PM2.5 and CVD and mortality among adults on Sumatra Island, Indonesia. Our findings may have implications for environmental and social policies and for steps that the Indonesian government can take to protect human health. This study can help raise awareness among health professionals and stakeholders regarding the impacts of PM2.5 exposure and may promote the development of policies to address this problem and prevent adverse health outcomes later in life. Owing to deteriorating air quality, these findings also provide advice to the government to maintain long-term local PM2.5 data management for all regions in Indonesia so that the data used to support air quality management policies are not as scarce as they are currently available.
Input related to PM2.5 quality control efforts can be provided to the Indonesian government in the form of appropriate measures to improve public and environmental health. For example, the Indonesian government needs to develop several technical guidelines under the mandate of government regulation PP No. 22 of 2021 concerning air pollution control because the national ambient air quality standard policy is still below international standards. In Indonesia, the maximum standard PM2.5 in the atmosphere for the mean annual concentration was set at 15 µg/m3 and 55 µg/m3 for 24 h. According to the USEPA, it is 12 µg/m3 for the mean annual concentration and 35 µg/m3 for 24 h, and according to the WHO, it is 5 µg/m3 for the mean annual concentration. These data can urge the government to immediately implement measures and concrete actions to save forests from extinction and prevent forest and peatland fires.
Hypertension and smoking are the most notable risk factors for stroke and coronary artery disease (Hajar, 2017). The nationwide approach to hypertension prevention and control has contributed to a substantial decline in stroke mortality in Japan (Ohira & Iso, 2013). Recent antismoking campaigns have contributed to a decline in the smoking rate among men (Bala et al., 2017; Chiang & Chang, 2016; Durkin et al., 2009). Intensive prevention programs for hypertension and smoking should continue to prevent future cases of CVD in Indonesia.
Urgent mitigation recommendation
During forest fire events, safeguarding public health, especially in remote areas, is crucial, and this work is a follow-up study of our previous research (Sepridawati Siregar et al., 2022a, 2022b; Siregar et al., 2022a, 2022b). To address this, several key actions should be taken. First, isolation shelters should be constructed with air filtration systems to remove PM2.5 and other pollutants. These buildings need to be well-sealed to prevent smoke infiltration. Shelters should be positioned in easily accessible locations for emergencies and setting up community centers with air filtration for those who do not have personal shelters should be considered. These facilities are equipped with medical supplies, clean drinking water, and communication tools (Xiang et al., 2021). The second, temporary shelters, use portable air purifiers, and air conditioning units to maintain breathable air quality. The filters should be regularly checked and replaced to ensure that they remain effective. The community should be educated about the locations and use of these temporary shelters during fire events (Prathibha et al., 2024). The third goal is to develop early warning systems that integrate satellite data, weather forecasts, and fire detection technologies to provide timely alerts on fire risk and air quality. Localized alert systems can be implemented via mobile apps, text messages, or local radio to inform residents of imminent fire risks and offer instructions on protective measures (Aryanti et al., 2021). Fourth, in terms of health precautions and personal protection, N95 masks should be distributed to reduce PM2.5 inhalation and provide guidance on their proper use (Kunstler et al., 2022). The wearing of long-sleeved shirts, hats, and other protective clothing to minimize exposure to smoke and ash should be encouraged. Medical care for individuals with respiratory conditions should be provided, and mobile health units or telemedicine services for remote areas should be set up. Additionally, access to clean water and nutritious food to support overall health and resilience during fire events should be ensured (Kodros et al., 2021).
Conclusion
In an observation window from 2000 to 2014 and according to an IFLS population-based cohort of participants aged ≥ 40 years, exposure to PM2.5 estimated from NASA satellite data in the area of residence was associated with mortality from all-natural, cardiovascular, and respiratory causes. The effect estimates corroborate the existing evidence for a causal relationship between PM2.5 and adverse health outcomes and support the formulation and implementation of policies to mitigate PM2.5 pollutants and their disease burden.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
Sepridawati Siregar: Investigation, Data Curation, Formal analysis, Writing—Original Draft; Nora Idiawati: Writing—Review & Editing, Visualization; Abiyu Kerebo Berekute: Writing—Review & Editing, Visualization; Muchsin Maulana: Writing—Review & Editing, Visualization; Wen-Chi Pan: Conceptualization, Supervision; Kuo-Pin Yu: Conceptualization, Supervision, Data Curation, Formal analysis, Writing—Original Draft.
Funding
Open Access funding enabled and organized by National Yang Ming Chiao Tung University. This work was supported by the National Science and Technology Council (grant nos.:111–2221-E-A49 -053 -MY3).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anderson, J. O., Thundiyil, J. G., & Stolbach, A. (2012). Clearing the air: A review of the effects of particulate matter air pollution on human health. Journal of Medical Toxicology,8(2), 166–175. 10.1007/s13181-011-0203-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aryanti, A., Mekongga, I., & Dewi, R. (2021). GPS-Based fire detection system (global positioning system) and SMS gateway. IOP Conference Series: Materials Science and Engineering,1108, 012023. 10.1088/1757-899X/1108/1/012023
- Ayuningtyas, D. A., Tuinman, M. A., Prabandari, Y. S., & Hagedoorn, M. (2021). Smoking cessation experience in Indonesia: Does the non-smoking wife play a role? Frontiers in Psychology,12, 618182. 10.3389/fpsyg.2021.618182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babatola, S. S. (2018). Global burden of diseases attributable to air pollution. Journal of Public Health in Africa,9(3), 813. 10.4081/jphia.2018.813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bala, M. M., Strzeszynski, L., & Topor-Madry, R. (2017). Mass media interventions for smoking cessation in adults. Cochrane Database of Systematic Reviews,11(11), CD004704. 10.1002/14651858.CD004704.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barraclough, S. (1999). Women and tobacco in Indonesia. Tobacco Control,8(3), 327–332. 10.1136/tc.8.3.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braggio, J. T., Hall, E. S., Weber, S. A., & Huff, A. K. (2020). Contribution of satellite-derived aerosol optical depth PM2.5 Bayesian concentration surfaces to respiratory-cardiovascular chronic disease hospitalizations in Baltimore. Maryland. Atmosphere (Basel),11(2), 209. 10.3390/atmos11020209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesaroni, G., Forastiere, F., Stafoggia, M., Andersen, Z. J., Badaloni, C., Beelen, R., & Peters, A. (2014). Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ,348, f7412. 10.1136/bmj.f7412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang, C. Y., & Chang, H. Y. (2016). A population study on the time trend of cigarette smoking, cessation, and exposure to secondhand smoking from 2001 to 2013 in Taiwan. Population Health Metrics,14, 38. 10.1186/s12963-016-0109-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crippa, P., Castruccio, S., Archer-Nicholls, S., Lebron, G. B., Kuwata, M., Thota, A., & Spracklen, D. V. (2016). Population exposure to hazardous air quality due to the 2015 fires in Equatorial Asia. Scientific Reports,6, 37074. 10.1038/srep37074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dartanto, T., Moeis, F. R., Nurhasana, R., Satrya, A., & Thabrany, H. (2018). Parent smoking behavior and children’s future development: evidence from Indonesia Family Life Survey (IFLS). Tobacco Induced Diseases, 16(Suppl 3), A78. 10.18332/tid/94561
- Durkin, S. J., Biener, L., & Wakefield, M. A. (2009). Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. American Journal of Public Health,99(12), 2217–2223. 10.2105/AJPH.2009.161638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland, S., Daniel, R., & Pearce, N. (2016). Outcome modelling strategies in epidemiology: Traditional methods and basic alternatives. International Journal of Epidemiology,45(2), 565–575. 10.1093/ije/dyw040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajar, R. (2017). Risk factors for coronary artery disease: Historical perspectives. Heart Views,18(3), 109–114. 10.4103/heartviews.Heartviews_106_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haryanto, B., & Djafri, D. (2020). Air pollution and school children respiratory diseases in Indonesia: A cohort study. ASM Science Journal,13(Specialissue5), 24–29. [Google Scholar]
- Hayes, R. B., Lim, C., Zhang, Y., Cromar, K., Shao, Y., Reynolds, H. R., & Thurston, G. D. (2020). PM25 air pollution and cause-specific cardiovascular disease mortality. International Journal of Epidemiology,49(1), 25–35. 10.1093/ije/dyz114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek, G., Krishnan, R. M., Beelen, R., Peters, A., Ostro, B., Brunekreef, B., & Kaufman, J. D. (2013). Long-term air pollution exposure and cardio-respiratory mortality: A review. Environmental Health,12(1), 43. 10.1186/1476-069X-12-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holipah, H., Sulistomo, H. W., & Maharani, A. (2020). Tobacco smoking and risk of all-cause mortality in Indonesia. PLoS ONE,15(12), e0242558. 10.1371/journal.pone.0242558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, X. Q., Mei, X. D., & Feng, D. (2016). Air pollution and chronic airway diseases: What should people know and do? Journal of Thoracic Disease,8(1), E31-40. 10.3978/j.issn.2072-1439.2015.11.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Oanh, N. T., Upadhyay, N., Zhuang, Y. H., Hao, Z. P., Murthy, D. V. S., Lestari, P., & Dung, N. T. (2006). Particulate air pollution in six Asian cities: Spatial and temporal distributions, and associated sources. Atmospheric Environment,40(18), 3367–3380. 10.1016/j.atmosenv.2006.01.050 [Google Scholar]
- Kodros, J. K., O’Dell, K., Samet, J. M., L’Orange, C., Pierce, J. R., & Volckens, J. (2021). Quantifying the health benefits of face masks and respirators to mitigate exposure to severe air pollution. Geohealth,5(9), e2021GH000482. 10.1029/2021GH000482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunstler, B., Newton, S., Hill, H., Ferguson, J., Hore, P., Mitchell, B. G., & Turner, T. (2022). P2/N95 respirators & surgical masks to prevent SARS-CoV-2 infection: Effectiveness & adverse effects. Infect Dis Health,27(2), 81–95. 10.1016/j.idh.2022.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, K. K., Miller, M. R., & Shah, A. S. V. (2018). Air pollution and stroke. J. Stroke,20(1), 2–11. 10.5853/jos.2017.02894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, L., Liu, Y., Wu, P., Peng, Z., Wang, X., Chen, T., & Yu, H. (2019). Influenza-associated excess respiratory mortality in China, 2010–15: A population-based study. Lancet Public Health,4(9), e473–e481. 10.1016/S2468-2667(19)30163-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, B., Yang, J., Dong, H., Li, M., Cai, D., Yang, Z., & Wang, B. (2021). PM2.5 constituents and mortality from a spectrum of causes in Guangzhou, China. Ecotoxicology and Environmental Safety,222, 112498. 10.1016/j.ecoenv.2021.112498 [DOI] [PubMed] [Google Scholar]
- Martini, S., Artanti, K. D., Hargono, A., Widati, S., Ahsan, A., & Prabandari, Y. S. (2022). Association between percentage of smokers and prevalence of smoking attributable morbidity in Indonesia: One decade after implementation of smoke-free area regulation. BMC Public Health,22(1), 2202. 10.1186/s12889-022-14435-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokoena, K. K., Ethan, C. J., Yu, Y., Shale, K., & Liu, F. (2019). Ambient air pollution and respiratory mortality in Xi’an, China: A time-series analysis. Respiratory Research,20(1), 139. 10.1186/s12931-019-1117-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohira, T., & Iso, H. (2013). Cardiovascular disease epidemiology in Asia: An overview. Circulation Journal,77(7), 1646–1652. 10.1253/circj.cj-13-0702 [DOI] [PubMed] [Google Scholar]
- Patanè, S. (2020). Long-term exposure to PM2.5 and CVD. Journal of the American College of Cardiology,75(22), 2876–2877. 10.1016/j.jacc.2020.03.075 [DOI] [PubMed] [Google Scholar]
- Perera, F. (2017). Pollution from fossil-fuel combustion is the leading environmental threat to global pediatric health and equity: Solutions exist. International Journal of Environmental Research and Public Health,15(1), 16. 10.3390/ijerph15010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pranata, R., Vania, R., Tondas, A. E., Setianto, B., & Santoso, A. (2020). A time-to-event analysis on air pollutants with the risk of cardiovascular disease and mortality: A systematic review and meta-analysis of 84 cohort studies. Journal of Evidence-Based Medicine,13(2), 102–115. 10.1111/jebm.12380 [DOI] [PubMed] [Google Scholar]
- Prathibha, P., Turner, M., Wei, L., Davis, A., Vinsonhaler, K., Batchelder, A., & Holder, A. L. (2024). Usage and impact of a do-it-yourself air cleaner on residential PM25 in a smoke-impacted community. Atmospheric Environment,333, 120650. 10.1016/j.atmosenv.2024.120650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purnomo, H., Okarda, B., Shantiko, B., Achdiawan, R., Dermawan, A., Kartodihardjo, H., & Dewayani, A. (2019). Forest and land fires, toxic haze and local politics in Indonesia. International Forestry Review,21(4), 486–500. 10.1505/146554819827906799 [Google Scholar]
- Santoso, M., Lestiani, D. D., Damastuti, E., Kurniawati, S., Kusmartini, I., DwiAtmodjo, D. P., & Hopke, P. K. (2020). Long term characteristics of atmospheric particulate matter and compositions in Jakarta, Indonesia. Atmospheric Pollution Research,11(12), 2215–2225. 10.1016/j.apr.2020.09.006 [Google Scholar]
- Santoso, M., Hopke, P. K., Damastuti, E., Lestiani, D. D., Kurniawati, S., Kusmartini, I., & Riadi, A. (2022). The air quality of Palangka Raya, Central Kalimantan, Indonesia: The impacts of forest fires on visibility. Journal of the Air & Waste Management Association,72(11), 1191–1200. 10.1080/10962247.2022.2077474 [DOI] [PubMed] [Google Scholar]
- Schulze, F., Gao, X., Virzonis, D., Damiati, S., Schneider, M. R., & Kodzius, R. (2017). Air quality effects on human health and approaches for its assessment through microfluidic chips. Genes (Basel),8(10), 244. 10.3390/genes8100244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siregar, S., Idiawati, N., Lestari, P., Berekute, A. K., Pan, W.-C., & Yu, K.-P. (2022a). Chemical composition, source appointment and health risk of PM2.5 and PM2.5–10 during forest and peatland fires in Riau, Indonesia. Aerosol and Air Quality Research,22(9), 220015. 10.4209/aaqr.220015 [Google Scholar]
- Siregar, S., Idiawati, N., Pan, W. C., & Yu, K. P. (2022b). Association between satellite-based estimates of long-term PM2.5 exposure and cardiovascular disease: Evidence from the Indonesian Family Life Survey. Environmental Science and Pollution Research,29(14), 21156–21165. 10.1007/s11356-021-17318-4 [DOI] [PubMed] [Google Scholar]
- Sofia, D., Gioiella, F., Lotrecchiano, N., & Giuliano, A. (2020). Mitigation strategies for reducing air pollution. Environmental Science and Pollution Research International,27(16), 19226–19235. 10.1007/s11356-020-08647-x [DOI] [PubMed] [Google Scholar]
- Sumaryati, S., Cholianawati, N., & Indrawati, A. (2019). The impact of forest fire on air-quality and visibility in Palangka Raya. Journal of Physics: Theories and Applications,3(1), 16. 10.20961/jphystheor-appl.v3i1.38071 [Google Scholar]
- Talib, N., Sa’aidi, N. A. M., Narashid, R. H., Zaki, N. A. M., Saad, N. M., Abdullah, S., & Mohd, F. A. (2022). Relationship between particulate matter (PM2.5) concentration and aerosol optical depth (AOD) throughout Peninsular Malaysia. IOP Conference Series: Earth and Environmental Science.1019, 012017. 10.1088/1755-1315/1019/1/012017
- Thangavel, P., Park, D., & Lee, Y. C. (2022). Recent insights into particulate matter (PM2.5)-mediated toxicity in humans: An overview. International Journal of Environmental Research and Public Health,19(12), 7511. 10.3390/ijerph19127511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibuakuu, M., Michos, E. D., Navas-Acien, A., & Jones, M. R. (2018). Air pollution and cardiovascular disease: A focus on vulnerable populations worldwide. Current Epidemiology Reports,5(4), 370–378. 10.1007/s40471-018-0166-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y., Shi, L., Lee, M., Liu, P., Di, Q., Zanobetti, A., & Schwartz, J. D. (2017). Long-term exposure to PM2.5 and mortality among older adults in the southeastern US. Epidemiology,28(2), 207–214. 10.1097/ede.0000000000000614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, C. M., Lai, H. K., Tsang, H., Thach, T. Q., Thomas, G. N., Lam, K. B., & Lam, T. H. (2015). Satellite-based estimates of long-term exposure to fine particles and association with mortality in elderly Hong Kong residents. Environmental Health Perspectives,123(11), 1167–1172. 10.1289/ehp.1408264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang, J., Huang, C. H., Shirai, J., Liu, Y., Carmona, N., Zuidema, C., & Seto, E. (2021). Field measurements of PM2.5 infiltration factor and portable air cleaner effectiveness during wildfire episodes in US residences. Science of the Total Environment,773, 145642. 10.1016/j.scitotenv.2021.145642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing, Y. F., Xu, Y. H., Shi, M. H., & Lian, Y. X. (2016). The impact of PM2.5 on the human respiratory system. Journal of Thoracic Disease,8(1), E69-74. 10.3978/j.issn.2072-1439.2016.01.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, D., Wang, W., Xi, Y., Bi, J., Hang, Y., Zhu, Q., Liu, Y. (2023). Wildfire worsens population exposure to PM2.5 pollution in the Continental United States. This is a preprint; it has not been peer reviewed by a journal. 10.21203/rs.3.rs-3345091/v2
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.