Abstract
The European Society of Intensive Care Medicine (ESICM) has developed evidence-based recommendations and expert opinions about end-of-life (EoL) and palliative care for critically ill adults to optimize patient-centered care, improving outcomes of relatives, and supporting intensive care unit (ICU) staff in delivering compassionate and effective EoL and palliative care. An international multi-disciplinary panel of clinical experts, a methodologist, and representatives of patients and families examined key domains, including variability across countries, decision-making, palliative-care integration, communication, family-centered care, and conflict management. Eight evidence-based recommendations (6 of low level of evidence and 2 of high level of evidence) and 19 expert opinions were presented. EoL legislation and the importance of respecting the autonomy and preferences of patients were given close attention. Differences in EoL care depending on country income and healthcare provision were considered. Structured EoL decision-making strategies are recommended to improve outcomes of patients and relatives, as well as staff satisfaction and mental health. Early integration of palliative care and the use of standardized tools for symptom assessment are suggested for patients at high risk of dying. Communication training for ICU staff and printed communication aids for families are advocated to improve outcomes and satisfaction. Methods for enhancing family-centeredness of care include structured family conferences and culturally sensitive interventions. Conflict-management protocols and strategies to prevent burnout among healthcare professionals are also considered. The work done to develop these guidelines highlights many areas requiring further research.
Keywords: Intensive care unit, End of life, GRADE, Cultural variations, Decision-making, Palliative care, Communication, Family-centered care, Conflict management
Introduction
Death in the intensive care unit (ICU) usually occurs after treatment limitation decisions warranted by patient preferences or non-beneficial treatments [1]. The treatment plan shifts from a curative intent to end-of-life (EoL) and palliative care aimed at alleviating symptoms while also meeting the emotional, psychological, and spiritual needs of both the patient and the family [2, 3]. In the ICU, deciding to move from curative to EoL care is particularly challenging, because it involves withdrawing or withholding life-supporting treatments (LSTs) [3].
EoL care practices are shaped by ethical principles, legal frameworks, cultural norms, and available resources and therefore vary substantially across countries and healthcare systems [1, 4, 5]. Clinical teams share LST-limitation decisions with patients and families in some countries and make them alone in others [6]. Cross-country comparisons can help to improve practices by identifying correlations between specific EoL care patterns and outcomes. Some approaches emphasize patient autonomy and others a best-interest model [7]. No single approach is optimal for all patients, and clinical judgment is therefore needed to tailor EoL care decisions.
One objective of EoL care in the ICU is to support patients and families throughout the LST-limitation process in a way that fosters empathy and understanding, builds trust via effective communication, and provides support in initial stages of grieving [2, 9, 11, 12]. Timely shifting to EoL care as early as is warranted improves the experience of patients and families [8], who should receive continuous emotional support and frequent opportunities to voice their wishes and concerns [13, 14]. Interdisciplinary coordination helps to provide holistic care [11]. Finally, conflicts should be managed sensitively with special attention for and the well-being of the clinical team [16, 17].
The aim of this work was to develop guidelines for EoL and palliative care in the ICU, based on data published over the last two decades, including the corona virus disease 2019 (COVID-19) pandemic. The opinions of experts were sought when published evidence was inadequate. The goals of these guidelines are to improve quality of dying and death, minimize the adverse effects of the experience on families, support the well-being of healthcare professionals (HCPs), and serve as a resource for hospital administrators and healthcare policymakers.
Methods
Topic and panel composition
These guidelines were formulated by an international panel of experts on behalf of the European Society for Intensive Care Medicine (ESICM). The definitions of basic terms related to EoL in the ICU are summarized in Table 1. Seven domains were pre-defined and each was assigned to a group of experts in the panel. Each group was coordinated by a domain chair. A methodologist overviewed guideline development to ensure transparency of the methodology and reproducibility of the guidelines. Before each step of recommendation development, definitions, objectives, search strings, and study inclusion and exclusion criteria were determined. The definitions of recommendation strength were chosen before the recommendations were developed.
Table 1.
Definitions
| Withholding treatment | Decision made not to start or increase a life-sustaining intervention |
| Withdrawing treatment | Decision that was made to actively stop a life-sustaining intervention presently being given |
| Active shortening of the dying process | Circumstance in which someone performes an act with the specific intent of shortening the dying process |
| Palliative care | Specialized medical care for people with a serious illness focused on providing relief from the symptoms and stress of the illness. The goal is to improve quality of life for both the patients and their families |
| End-of-life care | End-of-life care includes the decision-making as to the limitation of life-sustaining therapies and the physical, emotional, social, and spiritual support for patients and their families |
| Advanced directives | A legal document that states a person’s wishes about receiving medical care if that person is no longer able to make medical decisions; it may also give a person (such as a spouse, relative, or friend) the authority to make medical decisions for another person when that person can no longer make decisions (power of attorney) |
| Conflict | Dispute, disagreement, incompatibility, opposition, or difference of opinion involving more than one individual and related to the patient's management or to interpersonal conflict |
| Appropriate care | A patient care that is proportional to the expected survival and quality of life of the patient and in line with the patient's and relatives’ values |
| Burnout | A psychological syndrome arising in response to chronic emotional and interpersonal stressors on the job and is characterized by three different features: emotional exhaustion, depersonalization, and lack of personal and professional completion |
| Decision-making | A stepwise practice of gathering and interpreting information, weighing different options, and ultimately taking a (shared) evidence-based and personalized decision |
Research-question selection and literature search
For each domain, the relevant group formulated questions according to the Patients or Population-Intervention-Comparison-Outcome (PICO) format. Each PICO question was discussed and approved by the domain chair and group, methodologist, and full panel. For each PICO, two domain-group members performed a systematic literature search using the PubMed search engine, with pre-defined search strings and study inclusion and exclusion criteria. Each domain group chose to focus on randomized controlled trials (RCTs). When sufficient RCTs were not available, observational and qualitative studies could be included.
The quality of retrieved articles was graded according to the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) method (10.1016/j.jclinepi.2010.04.026), by two members of the relevant domain group, with disagreements resolved by a third member or the methodologist.
When the PICO question allowed and RCTs were available, the methodologist was to perform a systematic review and meta-analysis.
Development of recommendations or expert suggestions
Each domain group formulated recommendations for each PICO based on the results of the literature review and meta-analyses. Three main criteria were considered: the certainty of the evidence as assessed by the methodologist, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) level, and expert opinion. The proposed recommendations with the underlying summarized evidence were discussed by the full panel during meetings that were recorded to ensure accurate documentation. The results of these meetings were used to revise the proposed recommendations.
The final recommendations were submitted to a vote by the full panel. Approval of at least 80% of the panel members was required. It was planned that recommendations with lower approval rates were reformulated and re-submitted until at least 80% approval was achieved.
The final recommendations were categorized as high-level evidence (high level of evidence from two or more high-quality studies allowing a firm recommendation) or low-level evidence (low level of evidence from a single high-quality study or two intermediate-quality studies allowing a suggestion). When no high-quality studies and less than two intermediate-quality studies were available, the opinion of the panel experts was sought and the resulting recommendation was formulated as a suggestion (“expert opinion on clinical application”).
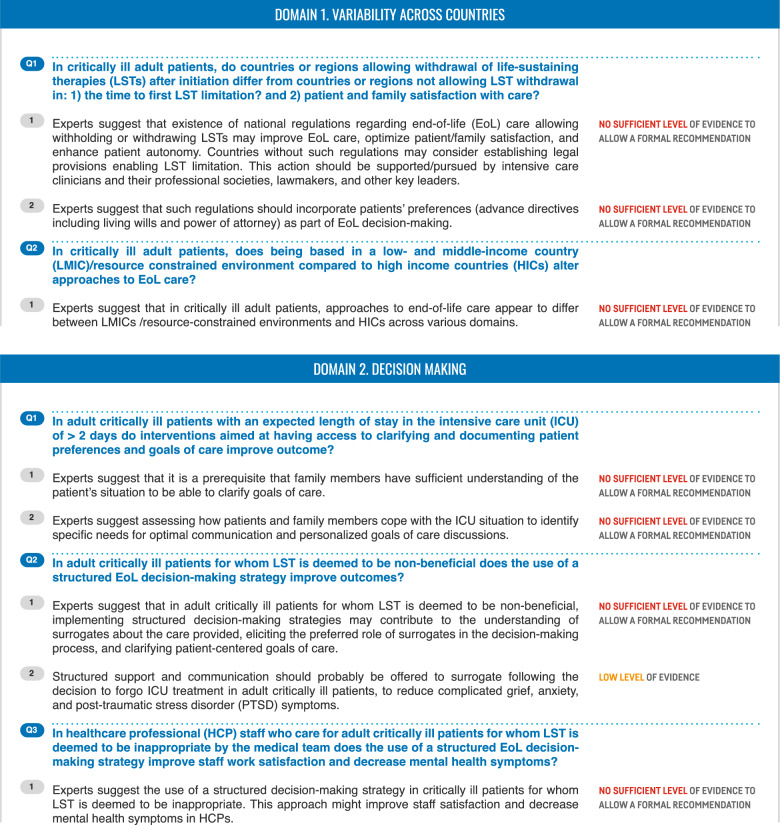
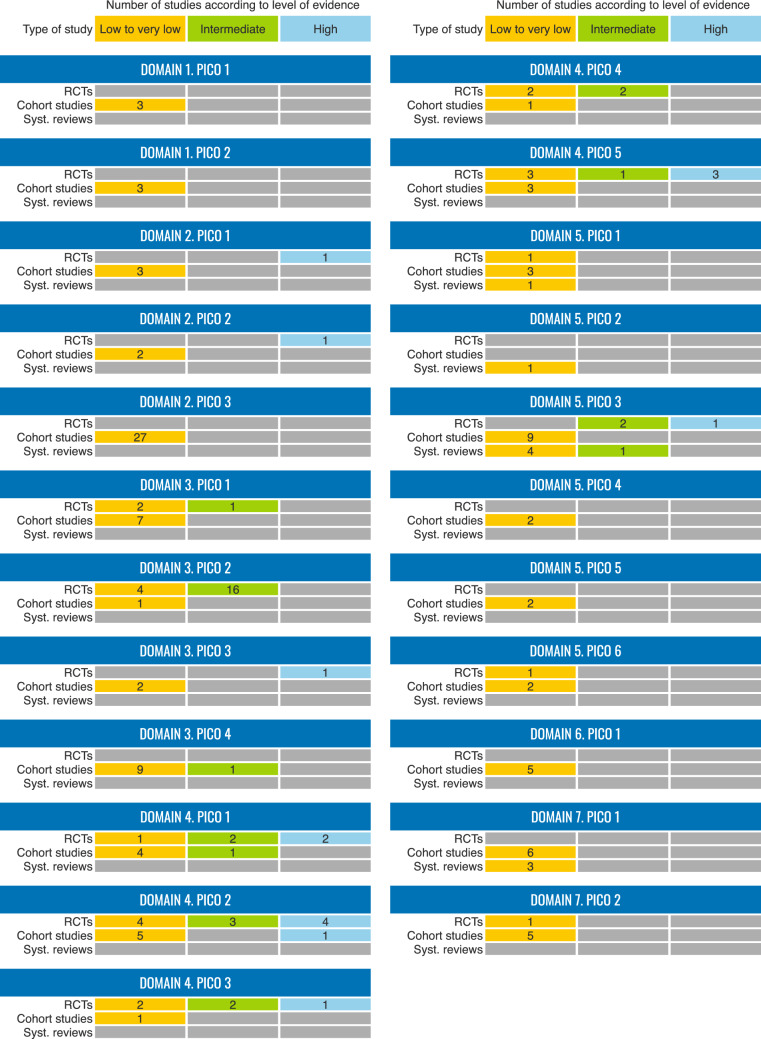
The executive summary of recommendations and the evidence summary are shown in Tables 2 and 3, respectively. Evidence plot reporting findings in PICOs with low- or high-level evidence recommendations is depicted in Fig. 1.
Table 2.
Executive summary of recommendations
Table 3.
Evidence summary
Fig. 1.
Evidence plot reporting findings in PICOs with low- or high-level evidence recommendations
Domain 1: Variability across countries
In critically ill adult patients, do countries or regions allowing withdrawal of life-sustaining therapies (LSTs) after initiation differ from countries or regions not allowing LST withdrawal in: (1) the time to first LST limitation? and (2) patient and family satisfaction with care?
Outcomes
Time to the decision to withdraw LSTs.
Patient and family satisfaction with care.
Background
Variations have been reported in the incidence of foregoing LST, time to LST limitation, and mortality after foregoing LST [1, 14–16]. In a study of European ICUs comparing EoL practices in 1999–2000 vs. 2015–2016, the more recent period was characterized by significantly higher proportions of foregoing LST and time reduction from ICU admission to the first LST limitation [1]. LST limitation was less common in low–middle-income countries (LMICs) than in high-income countries (HICs) [17]. The ICU EoL Practice Score (EPS) derived from the ETHICUS-2 study partly explains the substantial variation in treatment limitation decisions; furthermore, ICUs wishing to improve quality of end-of-life care may consider introducing the main weighted components: EoL protocols, palliative-care consultations, and local EoL legislation [18]. This score partly explains worldwide variations in LST limitations [1, 14, 15, 18].
Summary of the evidence
Legislation allowing LST limitations is associated with such limitations being implemented [1, 14, 15, 18]. Legislation fostering patient and family autonomy in EoL situations may contribute to greater patient/family satisfaction with EoL care [15, 18, 19].
| 1.1. Recommendations/expert opinion on clinical application |
|---|
|
Experts suggest that existence of national regulations regarding EoL care allowing withholding or withdrawing LSTs may improve EoL care, optimize patient/family satisfaction, and enhance patient autonomy. Countries without such regulations may consider establishing legal provisions enabling LST limitation. This action should be supported/pursued by intensive care clinicians and their professional societies, lawmakers, and other key leaders. No sufficient level of evidence to allow a formal recommendation. |
|
Experts suggest that such regulations should incorporate patients’ preferences (advance directives including living wills and power of attorney) as part of EoL decision-making. No sufficient level of evidence to allow a formal recommendation. |
Discussion
The EPS and several studies suggest that EoL legislation may promote the documentation of patient preferences in advance directives [14, 19] and good matching of EoL care decisions to patient preferences, notably regarding LST limitations [14, 18, 19]. Establishing advance directives and/or giving power of attorney to a healthcare proxy may facilitate discussions of EoL care preferences [20] and are key components of the recommended shared decision-making process [15, 21]. A lower number of LSTs at the end of life probably reflects greater respect for patient/family autonomy and is associated with greater patient/family satisfaction [22]. Consequently, intensivists, critical-care societies, and other leaders should promote the development of EoL legislation allowing LST limitation.
In critically ill adult patients, does being based in a low/middle-income country (LMIC)/resource-constrained environment compared to high-income countries (HICs) alter approaches to EoL care?
Outcomes
Practice variation in LSTs.
Knowledge and skills of HCPs in the field of EoL care.
Experience of patients and family members.
Healthcare costs.
Background
EoL care in critically ill patients has been assessed in several large studies, most of which were performed in HICs. EoL care practices in the ICU vary widely across the globe, and most patients live in LMICs, where results obtained in HICs may not apply [16, 23, 24]. Looking for differences in ICU EoL care between LMICs and HICs is therefore essential.
Summary of the evidence
Several electronic databases were searched for evidence on ICU EoL care in LMICs, published after 2000. Of the 57 identified publications, a 2022 scoping review and a study comparing LMICs vs. HICs across Asia were of particular interest [25, 26]. Of the 19 studies identified by the scoping review of data from LMICs, all were observational and none obtained information from patients or families [25]. ICU EoL care in LMICs has clearly not received sufficient research attention. The study comparing LMICs and HICs was a questionnaire survey done from May to December 2012 [26]. The respondents were 847 physicians in 255 ICUs in 10 LMICs and 618 physicians in 211 ICUs in six HICs. Major differences were noted between EoL practices between LMICs and HICs, in keeping with previous work by the same group [27]. However, according to GRADE, both studies produced only evidence of very low certainty [26, 27]. Scoping reviews cannot be assessed using GRADE.
| 1.2. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest that in critically ill patients, approaches to EoL care appear to differ between LMICs/resource-constrained environments and HICs across various domains. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Currently available data suggest that LMICs and HICs may differ regarding the use of LST limitations [26, 28, 29], HCP knowledge and skills in the field of EoL care [25, 29, 30], cultural factors influencing EoL care, specific environmental factors [25, 29, 30], patient and family views about EoL care (as shared by HCPs) [26, 29], and cost considerations [25, 26, 31]. ICU EoL care in LMICs is understudied.
Domain 2: Decision-making
In adult critically ill patients with an expected ICU length of stay > 2 days, do interventions aimed at having access to, clarifying and documenting patient preferences and goals of care improve outcome?
Outcomes
Patient-centered care.
Satisfaction with decision-making.
Mental-health symptoms (depression, grieving, and post-traumatic stress disorder [PTSD]).
Background
Each patient should only be offered those ICU treatments whose expected effects are consistent with the patient preferences. The initial ICU management plan may be designed to cure a life-threatening illness, stabilize the patient while a treatment strategy is developed, or alleviate distressing symptoms. After a few days in the ICU, in addition to the treatment response, the match between the treatments used and the patient’s preferences and values must be evaluated. These preferences and values must therefore be known to the ICU team. For patients without legally binding advance directives and/or legally appointed surrogate decision-makers, the relatives or close contacts act as sources of information and may legally act as surrogate decision-makers. However, during family meetings, discussions of patient preferences and values and realistic goals of care may not be straight forward [32]. The optimal time for initiating such discussions may not be obvious. In addition, family members face emotional struggles, notably grief and possibly guilt, when sharing decisions to limit LSTs [33]. A high level of communication and support, including transparent discussions about what is achievable in the context of the patient’s preferences and values, is essential.
Summary of the evidence
In critically ill adults expected to require > 2 days in the ICU, elucidating patient preferences regarding the level of care is crucial for the patient, surrogate decision-maker, and HCPs. Formal family meetings were associated with greater satisfaction with the decision-making process but not with better overall satisfaction with the care provided [34]. In an RCT, a family-support intervention failed to decrease symptoms of anxiety and depression in families but improved families’ ratings of communication and shortened the ICU stay [35].
Meaningful discussions of care goals require that families have a good understanding of LSTs, the level and intensity of support provided, and the patient’s resuscitation status [3, 36]. Additionally, the ICU staff must identify the coping strategies used by each patient and family [9].
| 2.1. Recommendations/expert opinion on clinical application |
|---|
|
Experts suggest that it is a prerequisite that family members have sufficient understanding of the patient’s situation to be able to clarify goals of care. No sufficient level of evidence to allow a formal recommendation. |
|
Experts suggest assessing how patients and family members cope with the ICU situation to identify specific needs for optimal communication and personalized goals of care discussions. No sufficient level of evidence to allow a formal recommendation. |
Discussion
In addition to legislation, religious beliefs and cultural norms may substantially influence EoL care decisions. Regardless of these influences, HCPs should elucidate patient preferences and values, adapt their communication and support strategies to individual patients and family members, negotiate conflicts, and determine appropriate goals of care. Communication skills are of considerable importance, notably for building trust in the pathway of care.
In adult critically ill patients for whom LST is deemed to be non-beneficial does the use of a structured EoL decision-making strategy improve outcomes?
Outcomes
Patient/surrogate satisfaction with decision-making.
Patient/surrogate mental-health symptoms (depression, grieving, and PTSD).
Time to LST withdrawal.
Background
Decision-making for critically ill patients is a complex stepwise process of gathering and interpreting information, weighing different options, and reaching a decision, if possible in collaboration with the patient or surrogate [15]. A structured decision-making strategy may reduce variability and improve patient and surrogate outcomes, while also optimizing healthcare-resource utilization [37]. Depending on family preferences, cultural factors, and local legislation, the decision to limit LSTs is taken by the ICU team alone, by the surrogates, or as the result of a shared decision-making process reflecting individual patient preferences and values.
Summary of the evidence
LSTs can be considered non-beneficial when not expected to achieve survival or not consistent with the treatment goals chosen by the patient, surrogate, and/or HCPs. Good understanding of the situation by any surrogates involved in decision-making is essential [3, 36]. Surrogates differ in their ability and willingness to share decisions and should therefore be asked about their preferred level of involvement [38].
When there is consensus that LSTs are non-beneficial and should be withheld or withdrawn, structured support and communication are important to reduce the risk of complicated grief, anxiety, and PTSD symptoms in the relatives [39].
| 2.2. Recommendations/expert opinion on clinical application |
|---|
|
Experts suggest that in adult critically ill patients for whom LST is deemed to be non-beneficial, implementing structured EoL decision-making strategies may contribute to the understanding of surrogates of the care provided, eliciting the preferred role of surrogates in the decision-making process and clarifying patient-centered goals of care. No sufficient level of evidence to allow a formal recommendations. |
|
Structured support and communication should probably be offered to family members following the decision to forgo ICU treatment in adult critically ill patients, to reduce complicated grief, anxiety, and PTSD symptoms. Low level of evidence. |
Discussion
Standardizing the complex EoL decision-making process is difficult and evaluating its effect on outcomes even more challenging. Neither the optimal decision-making strategy nor the most appropriate outcome measure has been identified to date. Methods for assessing how well the care provided matches the goals are needed. Other patient- and surrogate-related outcome measures (e.g., quality of communication, symptoms of anxiety and PTSD, decisional conflict) may be more strongly influenced by the result of the decisions than by the quality of the decision-making process (e.g., level of comprehension and whether needs for information and support were met). To improve healthcare-resource utilization, criteria that identify patients for whom LSTs are not goal-concordant or merely prolong the dying process would be helpful.
Communication is among the most important aspect of decision-making. Communication should be timely, frequent, and attuned to the needs and preferences of patient or surrogates. Spending more time with the patient or surrogate improves trust, thereby enhancing the shared decision-making process.
In HCP staff who care for adult critically ill patients for whom LST is deemed to be inappropriate by the medical team does the use of a structured EoL decision-making strategy improve staff work satisfaction and decrease mental-health symptoms?
Outcomes
Work satisfaction in ICU HCPs.
Mental-health symptoms in ICU HCPs.
Background
In ICU HCPs, providing LSTs that are not consistent with patients’ goals of care or that merely prolong dying is strongly associated with moral distress and intention to leave the job. The association is stronger in nurses than in physicians [40]. Moral distress may lead to conflicts, loss of trust, and loss of professional respect among team members [41]. Other consequences of moral distress may include depression, PTSD symptoms, burnout, and the loss of highly skilled ICU HCPs [42]. The appropriateness of LSTs and LST limitations therefore deserves close attention. Whether a structured strategy describing the components and timing of the decision-making process improves work satisfaction and/or decreases moral distress in ICU HCPs is unclear.
Summary of the evidence
No evidence on this point has been published. The recommendation below therefore rests solely on expert opinion.
| 2.3. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest the use of a structured EoL decision-making strategy in critically ill patients for whom LST is deemed to be inappropriate. This approach might improve staff satisfaction and decrease mental-health symptoms in HCPs. No sufficient level of evidence to allow a formal recommendations. |
Discussion
Starting or continuing LSTs that are non-beneficial do not meet the patients’ goals of care, or will merely prolong the dying process is strongly associated with moral distress among ICU HCPs [43]. Decision-making strategies should support HCPs, minimize subjectivity, and ensure that patients or surrogates express preferences, values, and desired goals of care. A structured approach is likely to benefit collaboration among HCPs and with the patients and families. The approach should ensure that the opinions, knowledge, and values of each participant are respected. Taking the different viewpoints of the ICU HCPs into consideration can improve the ethical culture in the ICU, thereby benefiting EoL decisions [44].
Domain 3: Palliative and end-of-life care in the ICU
In ICU patients with advanced medical illnesses and deteriorating health in spite of optimal intensive care treatment, does early integration of palliative care reduce symptom distress, improve quality of life, and enhance alignment of care with patient goals?
Outcomes
Patient satisfaction.
Completion of advance care planning.
Transition to do-not-resuscitate/do-not-intubate.
Number of transfers to hospice care.
Patient anxiety, depression, and PTSD experience at three months.
Transition from LSTs to comfort care.
ICU length of stay.
Background
Given the high mortality among critically ill patients, palliative care must be available in ICUs. ICU HCPs as the main providers of palliative care with palliative-care consultants being called in for complex cases is the most common model [45]. For cancer patients, early enrollment in a palliative-care program, before hospital admission, was associated with better patient and family satisfaction, fewer hospital admissions, better quality of life, and achievement of the preferred place of death [46, 47]. Recent studies have sought to determine whether similar benefits are obtained in ICU patients and their families [48–50].
Summary of the evidence
Three single-center low- to very-low-level evidence RCTs from the United States (US) assessed a palliative-care consultation within 3 days after ICU admission of high-risk patients (e.g., with advanced age, lifespan-limiting chronic conditions, or moderate/severe acute conditions) [49–51]. The ICU stay was shorter and patient satisfaction better in one trial [50], while the other demonstrated more transfers to hospice care and fewer ventilator days and tracheostomies, with no difference in ICU stay length [51]. The results of seven observational studies of early palliative-care consultations or early family meetings to discuss patient goals support the findings from the RCTs [52–58].
| 3.1. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest that early palliative care including consultation with palliative care specialists for patients at high risk of morbidity and mortality in ICU might be useful in improving quality of life and enhancing alignment of care with patient goals. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Most studies of early palliative-care integration for ICU patients focused on consultation with palliative-care specialists or on family meetings with ICU staff to discuss goals of care. Other components of palliative care such as symptom management and spirituality were not investigated. Only three RCTs are available and both had a single-center design that may limit general applicability. The seven observational studies also had a single-center design, and five were retrospective.
In patients with advanced medical illnesses and deteriorating health in spite of optimal intensive care treatment, does use of standardized tools for assessment of symptoms, compared to usual care, increase frequency of symptom assessment?
Outcomes
Discomfort, dyspnea, pain.
Delirium.
Thirst.
Sleep and sedation.
Anxiety and depression.
Background
Symptom assessment should be performed routinely, at regular intervals as opposed to only in response to distress, and documented [59]. Thirst, dyspnea, anxiety, fatigue, delirium, sleep, and pain should be evaluated using validated instruments. The presence of each symptom with its severity and any exacerbating and relieving factors should be recorded. Symptom assessment should continue after interventions [60].
Summary of the evidence
Of the 20 identified RCTs, most showed that routine symptom assessment with validated tools and documentation of the results increased the frequency of assessments and treatments [61–63]. Seven of the ten studies [59, 64–69] included in a 2015 systematic review [70] showed that introducing a pain-assessment protocol increased the frequency of pain assessments, improved significantly the documentation of assessment results, and increased the frequency of reports of pain. In a post hoc analysis of prospective observational data, regular pain assessments were associated with higher frequencies of assessments for sedation and procedural pain [71].
Fourteen RCTs assessed interventions aimed at improving sleep such as aromatherapy [72, 73], earplugs and eye masks [74–76], foot reflexology massage [77], and melatonin [78]. Most of these trials had fewer than 100 participants and were therefore graded as supplying only moderate-level evidence.
| 3.2. Recommendations/expert opinion on clinical application | |
|---|---|
|
Validated instruments to assess symptoms should probably be used in ICU patients with advanced illness to improve symptom detection and treatment. Low level of evidence. |
Discussion
Patient’s with advanced medical illness and deteriorating health, despite optimal intensive care, frequently experience symptoms that adversely affect the quality of dying and death, the well-being of relatives, and the mental health of HCPs. Many trials and observational studies of symptom assessment are available, but none provides a high level of evidence. Low-level evidence exists about assessing a wide array of symptoms.
In critically ill patients from whom life-supporting therapies are withheld or withdrawn, does a protocolized approach to withdrawal of life support, compared to usual care without a protocolized approach impact outcomes?
Outcomes
Symptoms.
Opioid and sedative doses.
Time to death.
Background
Practices for foregoing LST withdrawal vary across ICUs and are associated with the number of non-beneficial treatments and duration of the dying process. Several protocols about foregoing LST have been evaluated. The studies did not always quantify the effects of protocols on distressing symptoms, medication use, or time to death but provided some data of interest.
Summary of the evidence
A multicenter observational study comparing terminal weaning to immediate extubation in 402 patients found no differences in PTSD symptoms experienced by relatives [79]. In an observational study of only 14 patients, a nurse-led algorithm for terminal ventilator withdrawal was associated with better respiratory comfort compared to one-step extubation [80]. A multicenter cluster-randomized trial vs. standard care demonstrated a significant decrease in prolonged grief among relatives who had a family conference to prepare for the imminent death, a meeting in the ICU room to provide support, and a meeting after the death [39].
| 3.3. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest that relatives of dying ICU patients may benefit from protocolized support, including family conferences before and after the death of the patient. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Although LST withdrawal is a crucial component of ICU EoL care, robust evidence about the effects of LST-withdrawal protocols on patients and relatives is not available. Rigorous clinical trials of protocols including routine symptom assessments and pharmacologic and/or nonpharmacologic management strategies are urgently needed. Relatives may benefit from protocolized support including family conferences before and after the death of the patient. There is no evidence that terminal weaning reduces PTSD among relatives compared to immediate extubation.
In critically ill patients receiving LSTs, does formal re-evaluation of these therapies in relation to the patient’s evolving condition, prognosis, and achievable goals impact outcomes?
Outcomes
ICU and hospital lengths of stay.
Utilization of intensive-care interventions.
Alignment of care with patient’s goals.
Triggers for palliative care delivery.
Proportionality of ICU treatments.
Clinicians’ perceptions of excessive care.
Background
Few data exist on how intensivists make decisions about continuing or limiting LSTs. When the response to initial treatments is minimal and the prognostic scores intermediate, making the decisions that avoid non-beneficial interventions is particularly difficult [37]. A time-limited trial (TLT) can help [81]. The trial plan and duration should be agreed upon by the intensivists and patients and/or families. At the end of the trial, the appropriateness of continuing or limiting LSTs is assessed [82]. Other methods can be used.
Summary of the evidence
Eight observational descriptive studies [18, 37, 83–88] specifically evaluated TLTs. In addition, one before-after quality-improvement study assessed the impact of an early family conference [54]. An intervention that was designed to improve communication and involved both ICU HCPs and relatives used a TLT for care planning. The intervention improved the quality of family meetings, shortened ICU stays, and decreased treatment intensity and duration in patients less likely to benefit from aggressive management.
| 3.4. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest that regular re-evaluation of the proportionality of ICU LSTs with patients, family members, and multi-disciplinary teams, may reduce unwanted procedures and ICU and hospital lengths of stay. No sufficient level of evidence to allow a formal recommendation. |
Discussion
The available data do not support any specific protocol about foregoing LST. No strong evidence exists that formal LST re-appraisal after a TLT is beneficial. Nonetheless, the experts agree that such a re-appraisal may benefit patients and families. There is some evidence supporting a multi-disciplinary approach, the involvement of patients or relatives in formal discussions with ICU HCPs, and the use of communication aids to enhance comprehension. RCTs are needed to assess whether a formal LST re-appraisal strategy affects patient, family, and HCP outcomes.
Domain 4: Communication
In critically ill patients or their family members does an education program about EoL communication for ICU staff improve outcomes?
Outcomes
Patient and family satisfaction with communication.
Mental-health symptoms.
Better family/staff alignment with EoL decisions.
Effective communication (empathy, active listening, non-verbal communication).
Background
Designing a communication-skills program for ICU HCPs requires time and resources. On the other hand, inconsistent, unclear, or non-empathic communication might decrease satisfaction with, and effectiveness of, information, especially at the EoL [89, 90]. Also, sharing decisions about the level of care between HCPs and families requires specific interpersonal skills.
Summary of the evidence
Studies of communication-skills programs for ICU HCPs have produced variable results. A single-center before-after study of patients who died in the ICU assessed a multifaceted intervention that included clinician education, local champions, academic detailing, feedback to clinicians, and system support [91]. Neither quality of dying as assessed by the family nor family satisfaction was different, but nurse-assessed quality of dying was better and ICU stays were shorter with the intervention. Another multifaceted program improved compliance with specific process measures reflecting communication with family members, although patient-specific outcomes were not significantly different [92]. A prospective, single-center study of weekly communication training (4 h in all) for internal-medicine residents on ICU rotation was associated with better family outcomes [93].
| 4.1. Recommendations/expert opinion on clinical application | |
|---|---|
|
Structured training programs should probably be implemented for ICU HCPs to enhance competencies in EoL communication. Low level of evidence. |
Discussion
Studies have assessed programs to improve EoL communication skills of ICU HCPs with the goal of better supporting families before, during, and after the death of their loved ones. These programs may contribute to reduce anxiety, depression, and PTSD symptoms among relatives. Communication and family satisfaction were consistently improved when communication was more closely centered on patients and families, based on their needs. Prolonged grief, anxiety, and PTSD symptoms were significantly less common [39]. However, family support by the interprofessional ICU team did not significantly decrease mental-health symptoms in relatives, despite better quality of communication and patient- and family-centeredness of care [35]. Importantly, baseline psychological distress of families differed between these two studies.
In family members of critically ill patients, does receiving enhanced communication through brochure/leaflet/website/videos result in improved outcomes?
Outcomes
ICU experience.
Satisfaction with EoL care.
Mental-health symptoms.
Family/staff alignment with EoL decisions.
Background
Comprehension and satisfaction are relevant criteria for evaluating the effectiveness of information communicated to family members of ICU patients [94]. Families unused to medical terminology may struggle to understand the diagnosis, treatment, and prognosis [36]. Brochures, leaflets, websites, and videos designed for individuals without medical training may improve communication.
Summary of the evidence
Printed information tools were effective in several studies [94, 95], including an RCT assessing a family information leaflet [94, 95]. A review of five RCTs not specifically focused on the EoL concluded that printed aids or structured family conferences with the usual ICU team improved comprehension and alleviated family distress while also decreasing the use of invasive treatments [96]. In a review of 19 ICU studies of EoL decision-making, communication aids were associated with better care-goals documentation and shorter mechanical ventilation times and ICU stays [97]. However, the quality of the evidence was low or very low.
| 4.2. Recommendations/expert opinion on clinical application | |
|---|---|
|
Enhanced communication written tools, such as brochures, pamphlets, or leaflets designed for the families of ICU patients, should be implemented in every ICU to complement standard oral communication. High level of evidence. |
Discussion
Printed communication aids within a proactive communication strategy significantly reduced symptoms of PTSD, anxiety, and depression in relatives while also increasing family satisfaction [96, 98, 99]. The content of these aids should be designed to resolve uncertainties about what is occurring and what is possible and to alleviate guilt among relatives.
Two RCTs assessed communication tools in the ICU but did not focus on the EoL. The use by nurses of tablets for communication was associated with increased satisfaction and comprehension in an RCT [100]. Adding daily written summaries of care to usual communication improved mental well-being and satisfaction among relatives starting at the second ICU week [101].
Combining brochures with a website improved comprehension and diminished stress among relatives in a before-after ICU study not focused on the EoL [102]. Inviting families to perform care rituals within 24 h after ICU admission of patients with a 30% predicted ICU mortality risk was associated with a lower prevalence of PTSD and anxiety symptoms after 90 days and with greater family-perceived involvement in decisions [103]. However, handing relatives a list of questions to help elicit their concerns did not improve comprehension [104]. Families at risk for poor comprehension and greater distress, for instance due to language barriers, cultural specificities, or a low level of formal education should receive special attention [104].
In family members of critically ill patients does an intensivist team with training in palliative care skills improve outcomes?
Outcomes
Family satisfaction with communication.
ICU experience.
Mental-health symptoms.
Background
Palliative care is a patient and family-centered strategy to optimize quality of life by anticipating, preventing, and treating suffering related to terminal illness. In the ICU, palliative care includes symptom control, supportive communication with relatives, and clarification of treatment goals. Intensivists may lack the specific knowledge and skills required to provide effective palliative care. Moreover, patient selection, palliative-care implementation models, and triggers for calling in palliative-care consultants remain debated.
Summary of the evidence
Education about ICU EoL care focuses on subordination of technological interventions to care goals, knowledge of prognostic factors and LST processes, trust-building communication with patients and families, skills in honoring cultural factors relevant to EoL decision-making, and emphasizing the importance for both patients and relatives of excellent palliative care [105, 106]. Simulation-based workshops on palliative-care communication skills significantly improved self-assessments of competence in communication [107]. Formal training in ICU EoL care was associated with less discomfort induced by LST limitations among junior intensivists [108]. Palliative-care education for nursing students improved their self-reported ability to deliver physical, psychosocial, and spiritual support to dying patients [109]. A palliative-care e-learning tool for physicians managing dying patients during the COVID-19 pandemic was associated with better self-reported knowledge but had smaller effects on attitudes toward death, including own mortality [110].
| 4.3. Recommendations/expert opinion on clinical application | |
|---|---|
|
An intensivist team with palliative care training should probably manage communication with families of critically ill patients dying in the ICU. Low level of evidence. |
Discussion
A quality-of-communication score [111] including items on EoL communication was significantly better in relatives who received a family-support intervention vs. usual support, although the primary outcome of mental-health-symptom burden was not diminished [35]. A review of RCTs indicated that printed communication aids and structured communication improves emotional outcomes of relatives and shorten ICU stays [96].
In ICU patients or their family members, does having access to palliative/ethical interventions result in improved outcomes?
Outcomes
Patient and family satisfaction with care.
Background
Access to palliative care interventions for patients receiving intensive care and their families has been studied for 2 decades, but the discussion has focused mostly on the effects on length of stay [112] or staff satisfaction with care. A recent review found a predominance of structural and procedural quality indicators for palliative care in intensive care units, and only few outcome indicators [113]. More specifically, information on patient and family satisfaction with palliative care interventions in intensive care units is lacking.
Summary of the evidence
Three studies [91, 114, 115] evaluated a pre–post-comparison on the implementation of a palliative care intervention. No study included a control group. The interventions included training of intensive care staff in palliative care, identification and training of local champions, identification of barriers, academic detailing and feedback to clinicians in two studies [91, 115] and early communication, family meetings, and social support in the third study [114]. All three studies were single site studies and included between 463 and 590 patients. All studies were rated as low evidence in GRADE.
Staff-rated quality of death improved significantly after implementation of a palliative care intervention, even though family-rated quality of death and family satisfaction showed only a trend that did not reach significance [91]. Family members were significantly more satisfied with health care provider communication and competence, accessibility of information, involvement in decision-making, and reported higher overall satisfaction and satisfaction with the death and dying process after implementation of a palliative care intervention [114]. Social workers reported significant increase in the total number of activities for family members after the implementation of a palliative care intervention [113], even though family ratings of social workers were not improved.
In addition, the systematic review of Aslakson et al. [116] in 2014 included 37 papers with 30 palliative care interventions and showed beneficial effects with a decrease in hospital and intensive care length of stay, and no harmful effects, as (with one exception) the interventions decreased or had no significant effect on mortality. However, only 14 interventions reported the effects on family satisfaction, and only one of those studies [114] reported a significant improvement. Other significant findings such as decreases in nonconsensus between families and staff or in between intensive care team members, less family member PTSD and anxiety or an increase in the number of family meetings or the percentage of patient status changes to do-not-resuscitate are indicators of improved patient and family satisfaction in that review.
As few papers were available with only low-grade evidence, no formal recommendation can be formulated.
| 4.4. Recommendation/expert opinion on clinical application | |
|---|---|
|
Experts suggest that palliative care interventions might be useful for patients with poor prognosis in spite of optimal intensive care to improve patient and family member satisfaction with care. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Several studies have demonstrated beneficial effects of palliative care interventions for critically ill patients in intensive care. However, these studies all were rated as low-grade evidence. Two studies focused on palliative care training of intensive care staff, and only one study on palliative care consultations.
Palliative care interventions should include palliative care training for staff, training of local champions for palliative care, regular interdisciplinary and multiprofessional case discussions on treatment goals and treatment and liason with a specialist palliative care service. More research is needed to evaluate the effects of palliative care consultations from a multiprofessional palliative care team on patient and family satisfaction with intensive care.
In critically ill patients at high risk of death, or in their family members, does a structured approach to EoL family meetings result in improved ICU outcomes?
Outcomes
Mental-health symptoms.
Family satisfaction.
Background
EoL meetings with families of patients dying in the ICU aim to protect the psychological and emotional well-being of families. Good comprehension of the medical situation and achievable goals, trust in the ICU team, and perceived empathy are crucial to avoid guilt and other forms of distress. Among structured approaches to EoL meetings, the VALUE method has been found effective [117, 118]. VALUE stands for Value and appreciate the sentiments expressed by the family, Acknowledge emotions, Listen actively, pose questions that foster a deeper Understanding of the patient as an individual, and Elicite questions from the family.
Summary of the evidence
High-evidence studies of structured EoL family meetings have shown variable effects on anxiety, no decrease in depression, and significantly fewer PTSD symptoms [35, 39, 98].
| 4.5. Recommendations/expert opinion on clinical application | |
|---|---|
|
A structured approach for conducting EoL family conferences should probably be used to decrease post-traumatic stress disorder in family members and to improve family satisfaction. Low level of evidence. |
Discussion
Three high-quality RCTs demonstrated that a structured approach to EoL family meetings significantly benefited the mental health of relatives [35, 39, 98]. However, since available high-quality studies were negative on most outcomes and as regard to the high heterogeneity, the level of the recommendation was downgraded.
Of note, a study in four ICUs assessing structured meetings with palliative-care specialists vs. usual meetings with the ICU team found no differences in anxiety or depression and more PTSD symptoms with the intervention [48]. ICU physicians are in frequent contact with families and may therefore be more able to develop a supportive relationship. Structured EoL family meetings led by ICU HCPs may protect relatives from anxiety and complicated grief, improve shared decision-making, and shorten ICU stays.
Domain 5: Family-centered care
Outcomes for the entire domain
Mental-health symptoms.
Family satisfaction with care and quality of dying and death.
Staff satisfaction with care and the dying process.
Quality of communication.
Family satisfaction with decisions (including decisional regret).
Intensity or costs of care (including length of stay).
Palliative-care needs.
Patient-centeredness of care.
In families of patients at high risk of dying in the ICU, do open/flexible visiting hours improve outcomes?
Background
Visiting policies for families vary across ICUs and countries. Many ICUs in northern Europe welcome visits around the clock, whereas restriction to a few hours a day is common in southern Europe. However, flexible visiting hours seem frequently offered to relatives of patients at high risk for dying.
Summary of the evidence
Studies of visiting policies in ICUs have not usually focused on the EoL. No high-quality evidence demonstrating that liberal visiting policies improve outcomes of patients and families have been published. A low-quality cross-over study found that allowing longer visiting hours did not decrease delirium in patients (primary outcome) but lessened anxiety and depression symptoms in relatives [119]. Other studies found greater family satisfaction with flexible visiting hours (defined as adapted to constraints experienced by families) compared to restrictive visiting hours [120–122]. A meta-analysis of observational studies and RCTs showed more ICU staff burnout with unrestricted visiting [121]. In a single-center before-after study, most patients and ICU staff were satisfied with flexible visiting [123]. A comparison of two ICUs with open vs. restricted visiting policies found no major differences in five outcomes of relatives, perhaps because only one of these (access to patients) was likely to be influenced by open visiting hours [123, 124]. Of note, most patients in these studies survived to ICU discharge.
| 5.1. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest the use of flexible visiting to reduce family anxiety and improve satisfaction. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Visiting policies vary widely across ICUs [125]. Only low-quality evidence is available and, importantly, no studies focused specifically on EoL patients [126]. Moreover, no studies assessed patient outcomes.
In patients for whom cardiopulmonary resuscitation is attempted in the ICU, does the option for family to witness the resuscitation effort improve family outcomes?
Background
Cardiac arrest may occur in ICU patients at a time when their relatives are present. Whether relatives can benefit from witnessing resuscitation attempts is beneficial remains unclear.
Summary of the evidence
No high-quality data from ICU studies are available. A 2023 Cochrane review of RCTs in prehospital settings and emergency departments identified only two studies, both at high risk for bias [127]. The results suggest that witnessing resuscitation may decrease the prevalence of mental-health symptoms among relatives, without increasing stress among HCPs.
| 5.2. Recommendations/expert opinion on clinical application | |
|---|---|
| No sufficient level of evidence to allow a formal recommendation or an expert opinion. |
Discussion
No information on witnessing resuscitation attempts in the ICU has been published.
A position statement emphasizes the importance of supporting relatives of patients who experience cardiac arrest [126–128]. Assessing the willingness of relatives to witness resuscitation may be challenging given the time constraint. The relative should be accompanied and offered the opportunity to leave the room at any time. Presence of the relative must not interfere with resuscitation efforts or increase stress in the HCPs. Consequently, allowing relatives to witness resuscitation in the ICU may be best avoided until and if studies demonstrate that this practice is safe and beneficial for relatives, patients, and HCPs.
In families of patients who die in the ICU, does follow-up bereavement support improve outcomes?
Background
Bereavement support for families of patients having died in the ICU varies widely across ICUs and countries. Many ICUs offer anticipatory bereavement support at the time of LST-limitation decisions. Support may include structured family meetings and psychologist sessions during the ICU stay. Printed material providing information about what to expect when a loved one dies in the ICU can be given to relatives. Families can be invited to write diaries about their experience and to collect other memory-making material. Finally, after the death, families may be invited to come back to the ICU to discuss their experience.
Summary of the evidence
We identified 13 studies, all of low or very low quality [129–141]. Several of these studies assessed memory-making items, such as photos, word clouds, electrocardiograms (ECGs), and diaries collected before the death with the goal of easing the bereavement process. In an RCT, condolence letters sent to families did not decrease grief and may have worsened PTSD and depression symptoms [131]. A meeting shortly after the death was a component of a three-step strategy that decreased grief symptoms in another RCT [39]. A third RCT demonstrated that combining a structured EoL meeting with a brochure on bereavement lessened mental-health symptoms in relatives [98].
| 5.3. Recommendations/expert opinion on clinical application |
|---|
|
Bereavement brochures or leaflets combined with structured family conferences prior to death should be proposed to family of patients at the end of life. High level of evidence. |
|
We suggest not routinely sending condolence letters, written by the ICU team, to bereaved family members. Low level of evidence. |
Discussion
The evidence supports combining a structured EoL meeting and a bereavement brochure. The meeting should include nurses, involve active listening, and help relatives express their emotions [98]. A meeting of the intensivist and ICU nurse with the family shortly after the death may be beneficial [39]. Memory- and meaning-making interventions deserve further study. At present, sending routine condolence letters is probably best avoided.
In families of patients at high risk of dying in the ICU, do interventions that support families to be involved in providing or helping with patient care in the ICU improve outcomes?
Background
Families play many active roles in the ICU, notably in EoL situations. However, involving families in EoL care raises practical issues. Moreover, the effect of family involvement on patients, families, and ICU staff must be considered.
Summary of the evidence
One observational [142] and one before-after [143] study were identified. Both provided only very-low- or low-quality evidence and neither was restricted to EoL care. The observational study [142] evaluated the preferences of 127 relatives regarding involvement in care. The most common preferred activities were communicating with the patient (93%), providing music (86%), and reading to the patient (85%). In contrast, oral suctioning, tracheostomy care, and endotracheal tube suctioning were preferred by only 32%, 25%, and 13% of relatives, respectively. Among relatives who stated wanting to provide music, to read to the patient, and to perform artwork with the patient, only 50%, 34%, and 6%, respectively, did so. No outcomes related to providing care were studied. The before-after study [143] was done in three ICUs, two in the US and one in Italy, and assessed rituals performed by relatives of patients with a greater than 50% risk of dying in the ICU. Families were given a booklet and explanation by a clinician about rituals they might want to engage in. The primary outcome of PTSD symptoms in the relatives 90 days after ICU death or discharge was significantly better with the intervention (adjusted odds ratio 0.54; 95% confidence interval [CI], 0.30–0.98).
The nurses reported that the proportion of families providing care increased with the intervention.
| 5.4. Expert opinion on clinical application: | |
|---|---|
|
Experts suggest that in end-of-life situations, encouragement of family-led care would be acceptable to family members and may be associated with better outcomes for caregivers. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Family participation in care may be desirable but raises feasibility issues. Families must be authorized by the ICU team to provide care then receive continuous support during the care they provide. The involvement of families must not adversely affect patient safety or clinician well-being. Also, when offered the opportunity to provide care, families should be made aware that they are free to refuse and to change their mind.
In families of patients at high risk of dying in the ICU and unable to visit, do distance communication protocols (video calls, etc.) improve family outcomes?
Background
During the COVID-19 pandemic, visiting policies were considerably restricted, including in EoL situations. Many ICU teams used remote systems to allow families to communicate with dying patients. Whether this strategy is helpful as part of usual practice deserves evaluation.
Summary of the evidence
We identified two studies, both done during the COVID-19 pandemic and both of very low or low quality. A cross-sectional survey with responses from 182 (54% of ICUs in the United Kingdom) documented use of virtual visiting in 97% of cases [144]. The staff felt that virtual visiting decreased psychological distress in patients and improved staff morale. Virtual visiting was deemed inappropriate for unconscious patients by 23% of ICUs and for dying patients by 7% of ICUs. Of note, restricted in-person visits to dying patients was usually allowed. No family outcomes were collected. A qualitative study done in France assessed themes of lived experiences in 19 relatives of patients who had died of COVID-19 in the ICU [145]. Communication was only via telephone calls. Relatives reported having difficulties establishing a relationship with the ICU team and experiencing feelings of abandonment, unreality, and disbelief.
| 5.5. Recommendation/expert opinion on clinical application | |
|---|---|
| No sufficient level of evidence to allow a formal recommendation or an expert opinion. |
Discussion
Restricted visitation during the COVID-19 pandemic may have adversely impacted family members. Virtual visiting is feasible [144]. No data on family outcomes associated with virtual visiting are available. Virtual visitation at the EoL is an important area for future research.
In families of patients at high risk of dying in the ICU, do interventions that address patients’ and families' cultural needs improve outcomes?
Background
Many countries are multicultural, and culture affects attitudes toward dying and death [146, 147]. Many intensivists lack the knowledge and skills needed to take culture into account as part of patient- and family-centered care [148]. In addition to knowledge about other cultures, self-awareness of one’s own attitudes, experiences, and even biases is required.
Summary of the evidence
Studies suggest the existence of cultural variability in terms of care and outcomes [149]. This applies to race, ethnicity, language, geography, or religion. A survey of 15 ICUs in the US showed that families from minority groups gave lower ratings for the quality of dying in the ICU [150]. In a cluster-randomized trial, also from the US, a mobile application that informed intensivists about family-reported needs induced a larger differential decrease in unmet needs among white families than among black families; the latter of which experienced a similar decrease in needs in both treatment and control groups [151]. In another US study, relatives of minority groups gave higher ratings for communication and care, although this finding seemed mediated by lower socioeconomic status [149, 150].
| 5.6. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest that end-of-life situations should be tailored to the cultural needs of the patient and family where possible. No sufficient level of evidence to allow a formal recommendation. |
Discussion
ICU HCPs should seek to gain knowledge of the specific cultural mores and beliefs held by the population served by their unit. They should be mindful of any biases they may have and strive to develop a high level of respect for cultural differences. Awareness of cultural specificities is crucial when collecting patient and family preferences. Culture may affect reactions to specific care procedures and attitudes toward death.
Domain 6: Interprofessional decision-making
In HCPs providing, does interprofessional decision-sharing improve outcomes?
Outcomes
Moral distress in HCPs.
Conflict among HCP teams.
Background
EoL care in the ICU can be distressing not only to families but also to staff. Lack of effective involvement of HCPs can cause significant moral distress and within-team conflict.
Summary of the evidence
In qualitative interviews, seven nurses and four physicians in a single ICU described EoL decision-making as a balancing act involving teamwork, shared goals, good understanding of the points of view of all those involved, and awareness of one’s own beliefs [152]. A study designed to develop a questionnaire identified seven factors influencing ICU HCP stress and ease of EoL decision-making, including collaboration and role clarity [153]. Psychometric testing found this questionnaire to be reliable and valid. A qualitative, focus-group study of ICU nurse and physician experiences when transitioning to EoL care indicated a need for better interprofessional implementation and acceptance of EoL care plans [154]. In another qualitative study, integrating palliative care within the ICU was perceived by HCPs as improving job satisfaction and collaboration among disciplines [153, 155–157].
| 6.1. Recommendations/expert opinion on clinical application | |
|---|---|
| No sufficient level of evidence to allow a formal recommendation or an expert opinion. |
Discussion
EoL care in the ICU places considerable stress on staff [158, 159]. While we may not have sufficient evidence, involving all members of the ICU team in EoL decisions would seem consistent with acknowledging the value of each. Studies are needed to design interprofessional decision-sharing interventions and to assess their effects on ICU HCP staff outcomes.
Domain 7: Conflict management and burnout
In ICU health care professionals do conflict management strategies prevent conflicts related to the EoL situations?
Outcomes
Moral distress.
PTSD symptoms.
EoL-related ICU conflicts.
Background
Conflicts are common in ICUs, usually occur between nurses and physicians or among nurses, and are particularly frequent in EoL situations [12]. Conflicts are associated with mental ill-being among HCPs. Strategies to prevent and mitigate conflicts among ICU HCPs include staff meetings where all staff members can voice their opinions and feelings without being judged, role clarity, and a safe work environment.
Summary of the evidence
The typology of EoL-related conflicts has been described in several observational studies [12, 160]. Preventing ICU conflicts at the EoL is a key goal. However, no studies have identified interventions that prevent or mitigate EoL conflicts among ICU HCPs.
| 7.1. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest implementing a protocol to prevent and mitigate conflict situations among HCPs or with family members. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Evaluation of multimodal conflict-prevention strategies addressing organization, education, and communication would be welcome. Regular informal staff meetings may help to develop understanding and mutual acceptance of differing viewpoints within the ICU team could be helpful in preventing or resolving intra-team conflict and creating a safe working environment, especially in a multi-ethnic critical-care context [161].
In ICU healthcare professionals facing end-of-life care does implementation of preventive organizational or personal strategies mitigate the prevalence of burnout or mental distress?
Outcomes
Burnout symptoms.
Mental-health symptoms.
Background
Burnout syndromes are common in ICU HCPs [162, 163]. Risk factors include overwork, high stress, poor organizational support, poor teamwork, and limited autonomy [164–166]. Moral distress from perceived inappropriate care given to dying patients interacts with burnout [167]. Burnout is associated with anxiety, depression, substance abuse, and lower quality of care [168]. Job dissatisfaction is common among staff with burnout syndromes, who often leave the profession.
Summary of the evidence
A self-care and mindfulness program was used to promote wellness among ICU nurses [169]. A before-after study showed that an intensive communication strategy about EoL care decreased the risk of burnout by 50% [170]. Both studies provided only very-low- or low-quality evidence.
| 7.2. Recommendations/expert opinion on clinical application | |
|---|---|
|
Experts suggest promoting multi-disciplinary communication in EoL situations and discussing goals of care within all parties involved: patient–family members–professionals, and to implement strategies preventing mental distress, including ethical discussions, in the ICU. No sufficient level of evidence to allow a formal recommendation. |
Discussion
Suggested strategies for preventing burnout include improved EoL care, conflict prevention, and participation in ICU research groups [171]. Research assessing these strategies applied to EoL care is needed.
General considerations
These guidelines aim to help ICU HCPs navigate the considerable challenges raised by EoL care. For many points of interest, few data are available. The considerable variability in practices and outcomes across ICUs and countries reflects this paucity of data and a need for further legislative and research efforts.
The strength of these guidelines is the establishment of a research agenda for the future, summarizing the literature of the last few decades and providing evidence-based recommendations and expert opinions about end-of-life and palliative care for critically ill adults for the benefit of the patients, families and HCP. On the other hand, these guidelines have limitations mainly due to the lack of high-quality studies, especially RCTs, which has prevented to generate bold evidence-based recommendations.
Communication within the ICU team and between the team and the patients and relatives is clearly crucial. Structured programs for ICU HCPs aimed at improving EoL communication have shown promise, although their long-term effects warrant further evaluation, with outcomes of interest including documentation of patient preferences, quality of dying, ICU length of stay, mental-health symptoms in relatives, and mental well-being of HCPs. Obstacles to good communication related to cultural, religious, and racial diversity deserve special attention. How legislation about EoL practices and the rights of patients and families may affect communication and well-being should be studied. ICU HCPs also need specific training in palliative care.
TLTs and other means of avoiding non-beneficial care in a manner that develops a consensus between the ICU team and the patient and family may be valuable for protecting HCPs from moral distress and patients from unnecessary suffering. Visiting policies, the collection of memory- and meaning-making material before the death, and follow-up bereavement support should be evaluated in high-quality studies as possible means of improving outcomes in relatives. Personal-care programs for ICU HCPs and well-being monitoring of staff by ICU heads also deserve investigation.
Conclusions
In conclusion, these guidelines present 8 evidence-based recommendations (6 of low level of evidence and 2 of high level of evidence) and 19 expert opinions (summarized in Table 3). Finally, limited availability of data is stressed and research priorities are identified.
Acknowledgements
The authors gratefully acknowledge Guy François from ESICM, Brussels, Belgium, for his outstanding administrative and organizational support in the development of these guidelines.
Guideline leadership
Co-chairs
Jozef Kesecioglu, Utrecht, The Netherlands.
Katerina Rusinova, Prague, Czechia.
Elie Azoulay, Paris, France.
Methodologist
Michael Darmon, Paris, France.
Domain leads
Domain 1: Charles L, Sprung, Jerusalem, Israel.
Domain 2: Monica Kerckhoffs, Utrecht, The Netherlands.
Domain 3: Judith E Nelson, New York, USA.
Domain 4: Giovanni Mistraletti, Milan, Italy.
Domain 5: Nancy Kentish-Barnes, Paris, France.
Domain 6: Carole Boulanger, Exteter, The United Kingdom.
Domain 7: Margo Van Mol, Rotterdam, The Netherlands.
Abbreviations
- EoL
End of life
- EPS
End-of-life practice score
- HCP
Healthcare professional
- HIC
High-income country
- ICU
Intensive care unit
- LMIC
Low/middle-income country
- LST
Life-sustaining treatment
- PTSD
Post-traumatic stress disorder
- RCT
Randomized-controlled trial
- TLT
Time-limited trial
Declaration
Conflicts of interest
AMi reports travel cost reimbursement for the ESICM 2022 and 2023 annual congresses. CC received honoraria for lectures, and support for attending meetings (NIH grants). He is also member of two DSMBs in the field of pall care and mindfulness. EA declares honoraria for Lectures from GILEAD, PFIZER, SANOFI, ALEXION and receipt of drugs for running a clinical trial (PFIZER). LH is President and CEO of Medical Corporation she has appeared, and her corporation has been paid for expert testimony in legal matters in Canada that pertain to allegations of negligence in critical care medicine in which patients have died. I have also been paid for expert testimony in a criminal case in EOL care in Canada. She received free admission to the ESICM 2023 meeting for all her work for ESICM not solely for this project. JD received payment for expert testimony in a criminal trial in Canada. JM received grants supporting the implementation of palliative care in undergraduate teaching at the Faculty of Medicine in the Czech Republic (Czech Society of Palliative Medicine, Faculty of Medicine, Masaryk University Brno, 1661/2023), for the diagnosis of superinfections in patients with COVID-19 pneumonia on mechanical ventilation (Ministry of Health, Prague[CZ], Grant number: NU22-B-122) and supporting further development of excellence in SP General Medicine Introduction of Objective Structured Clinical Examination (OSCE) and related modifications to the teaching of Intensive Care Medicine (MUNI/ESPRO/0850/2023 and MUNI/IVV/0770/2023). He is member of the Scientific Board BAZE-X1, OxygenBiotech. JK received support for travel and honorarium from Draeger Medical Equipment (Shanghai) Co., Ltd for approximately 2.5 days of academic lectures given in Tianjin during the CSCCM meeting 25-27 May 2023. KP declares a research grant FAME: as a member of the grant’s Scientific Review Committee, she was provided financial support (i.e., travel and accommodations), to attend a meeting in Paris, France in October 2023. She is Chair of the Data Safety Monitoring Committee for the University of Washington “Facilitating Communication Study”, and NIH-sponsored grant (no financial compensation for this work). MSH received honorarium for Grenvik lecture University of Pittsburgh Sept 2023. She received support for travel (ESICM 2023 annual meeting). MV received honoraria for lessons and lectures from CNT (Italian National Transplant Authority), Getinge/Maquet, University of Torino, University of Milano-Bicocca, BSC (Belgian Society of Cardiology). He received travel and accommodation support for lectures and lessons (without honoraria) from SIAARTI (Italian College of Anesthesia and Intensive Care), GiViTI (Gruppo Italiano Valutazione Interventi in Terapia Intensiva), different Universities and healthcare institutions in Italy. He is member of the DSMB for the ENFORCER Study, past Chair and current board member of the Ethics Section of SIAARTI, and member of the Institutional Review Board of EMERGENCY NGO. MD is General secretary and member of the council of the French Society of intensive care medicine (2019-2024). GM is member of the DSMB of the ALBIOSS-BALANCED study and member of the Ethics Committee “Comitato Etico Territoriale n.4 della Lombardia” – IRCCS Istituto Nazionale dei Tumori, Milano, Italy. NK-B received grant from the Agence Nationale de la Recherche, France. NP received grants from the National Institute for Health Research and the RCN Foundation. She is chair of Trustees and Chair of National Outreach Forum (registered UK charity 1181360 – unpaid). JN received grant from the NIH, National Institute of Nursing Research. She received support for attending meeting (University Hospital Research in Health (RHU-5) – October 2023 meeting for “FAME” Project (Agence Nationale de la Recherche-France) Scientific Advisory Board. She is member of the Scientific Advisory Board - FAME” Project (Agence Nationale de la Recherche-France) and NHLBI project. LR is Chair of the Board of Directors of the International Association for Hospice and Palliative Care. RTG received support for travel and accommodation (ESICM LIVES 2023). He is member of the NVIC ethics committee. RE received grant from the National Institute for Health & care Research, UK. She is Director of the National Institute for health & care Research, UK and Trustee/Director, Intensive Care National Audit and Research Centre (ICNARC), UK. SJS received grants from: STIMIT AG, Switzerland; Fresenius Kabi Gmbh, Germany; ASP Gmbh, Germany; Reactive Robotics GmbH, Germany; Innovationsfond of The Federal Joint Committee (G-BA), Germany; ESICM, Switzerland. He received honoraria for lectures from Springer Verlag GmbH, Austria, Advanz Pharma GmbH, Germany and Fresenius Kabi Gmbh, Germany. He received financial support for attending meetings from National (e.g., DGAI) or international (e.g., ESICM) medical societies in the field of anesthesiology and intensive care and their congress organizers and from Charité – Universitätsmedizin Berlin. He is member of the DSMB of the MIDAS Study (PMID: 32885276). He declares fiduciary role in the TiFoNet of the DGAI, Germany. He has stock option from Alphabet Inc., Siemens AG, and Bayer AG. CLS received honoraria from hospitals for lectures on “ICU worldwide end of life practices”. SM declares grant from the EUROPEAN HEALTH AND DIGITAL EXECUTIVE AGENCY (HADEA) - Project 101137221 — EPIC (Enhancing Palliative Care in ICU]. All the other authors have no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sprung CL, Ricou B, Hartog CS et al (2019) Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA 322:1–12. 10.1001/jama.2019.14608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelley AS, Morrison RS (2015) Palliative care for the seriously ill. N Engl J Med 373:747–755. 10.1056/NEJMra1404684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez KL, Barnato AE, Arnold RM (2007) Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med 10:99–110. 10.1089/jpm.2006.0155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azoulay E, Metnitz B, Sprung C et al (2009) End-of-life practices in 282 intensive care units: data from the SAPS 3 database. Intensive Care Med 35:623–630. 10.1007/s00134-008-1310-6 [DOI] [PubMed] [Google Scholar]
- 5.Sprung CL, Cohen SL, Sjokvist P et al (2003) End-of-life practices in European intensive care units: the Ethicus Study. JAMA 290:790–797. 10.1001/jama.290.6.790 [DOI] [PubMed] [Google Scholar]
- 6.Curtis JR, Tonelli MR (2011) Shared decision-making in the ICU: value, challenges, and limitations. Am J Respir Crit Care Med 183:840–841. 10.1164/rccm.201011-1836ED [DOI] [PubMed] [Google Scholar]
- 7.Quill TE, Brody H (1996) Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med 125:763–769. 10.7326/0003-4819-125-9-199611010-00010 [DOI] [PubMed] [Google Scholar]
- 8.Abernethy AP, Currow DC, Fazekas BS et al (2008) Specialized palliative care services are associated with improved short- and long-term caregiver outcomes. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 16:585–597. 10.1007/s00520-007-0342-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson JE, Hanson LC, Keller KL et al (2017) The voice of surrogate decision-makers. family responses to prognostic information in chronic critical illness. Am J Respir Crit Care Med 196:864–872. 10.1164/rccm.201701-0201OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson JE, Puntillo KA, Pronovost PJ et al (2010) In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med 38:808–818. 10.1097/ccm.0b013e3181c5887c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herridge MS, Azoulay É (2023) Outcomes after critical illness. N Engl J Med 388:913–924. 10.1056/NEJMra2104669 [DOI] [PubMed] [Google Scholar]
- 12.Azoulay E, Timsit J-F, Sprung CL et al (2009) Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J Respir Crit Care Med 180:853–860. 10.1164/rccm.200810-1614OC [DOI] [PubMed] [Google Scholar]
- 13.Goold null, Williams null, Arnold null (2000) Handling conflict in end-of-life care. JAMA 283:3199–3200 [PubMed]
- 14.Higel T, Alaoui A, Bouton C, Fournier J-P (2019) Effect of living wills on end-of-life care: a systematic review. J Am Geriatr Soc 67:164–171. 10.1111/jgs.15630 [DOI] [PubMed] [Google Scholar]
- 15.Kon AA, Davidson JE, Morrison W et al (2016) Shared decision-making in intensive care units. Executive summary of the American college of critical care medicine and American thoracic society policy statement. Am J Respir Crit Care Med 193:1334–1336. 10.1164/rccm.201602-0269ED [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Avidan A, Sprung CL, Schefold JC et al (2021) Variations in end-of-life practices in intensive care units worldwide (Ethicus-2): a prospective observational study. Lancet Respir Med 9:1101–1110. 10.1016/S2213-2600(21)00261-7 [DOI] [PubMed] [Google Scholar]
- 17.Lobo SM, De Simoni FHB, Jakob SM et al (2017) Decision-making on withholding or withdrawing life support in the ICU: a worldwide perspective. Chest 152:321–329. 10.1016/j.chest.2017.04.176 [DOI] [PubMed] [Google Scholar]
- 18.Mentzelopoulos SD, Chen S, Nates JL et al (2022) Derivation and performance of an end-of-life practice score aimed at interpreting worldwide treatment-limiting decisions in the critically ill. Crit Care Lond Engl 26:106. 10.1186/s13054-022-03971-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arnfeldt CM, Groenvold M, Johnsen AT et al (2022) Development of an advance directive “communication tool” relevant for patients with advanced cancer in six European countries: experiences from the ACTION trial. PLoS ONE 17:e0271919. 10.1371/journal.pone.0271919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curtis JR, Patrick DL, Caldwell E et al (1999) The quality of patient-doctor communication about end-of-life care: a study of patients with advanced AIDS and their primary care clinicians. AIDS Lond Engl 13:1123–1131 [DOI] [PubMed] [Google Scholar]
- 21.Michalsen A, Long AC, DeKeyser GF et al (2019) Interprofessional shared decision-making in the ICU: a systematic review and recommendations from an expert panel. Crit Care Med 47:1258–1266. 10.1097/CCM.0000000000003870 [DOI] [PubMed] [Google Scholar]
- 22.Chou W-C, Huang C-C, Hu T-H et al (2022) Associations between family satisfaction with end-of-life care and chart-derived, process-based quality indicators in intensive care units. J Palliat Med 25:368–375. 10.1089/jpm.2021.0304 [DOI] [PubMed] [Google Scholar]
- 23.Mark NM, Rayner SG, Lee NJ, Curtis JR (2015) Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Intensive Care Med 41:1572–1585. 10.1007/s00134-015-3810-5 [DOI] [PubMed] [Google Scholar]
- 24.Sprung CL, Rusinova K, Ranzani OT (2015) Variability in forgoing life-sustaining treatments: reasons and recommendations. Intensive Care Med 41:1679–1681. 10.1007/s00134-015-3868-0 [DOI] [PubMed] [Google Scholar]
- 25.Rao SR, Salins N, Joshi U et al (2022) Palliative and end-of-life care in intensive care units in low- and middle-income countries: a systematically constructed scoping review. J Crit Care 71:154115. 10.1016/j.jcrc.2022.154115 [DOI] [PubMed] [Google Scholar]
- 26.Phua J, Joynt GM, Nishimura M et al (2016) Withholding and withdrawal of life-sustaining treatments in low-middle-income versus high-income Asian countries and regions. Intensive Care Med 42:1118–1127. 10.1007/s00134-016-4347-y [DOI] [PubMed] [Google Scholar]
- 27.Phua J, Joynt GM, Nishimura M et al (2015) Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med 175:363–371. 10.1001/jamainternmed.2014.7386 [DOI] [PubMed] [Google Scholar]
- 28.Azab SMS, Abdul-Rahman SA, Esmat IM (2022) Survey of end-of-life care in intensive care units in Ain Shams university hospitals, Cairo, Egypt. HEC Forum Interdiscip J Hosp Ethical Leg Issues 34:25–39. 10.1007/s10730-020-09423-7 [DOI] [PubMed] [Google Scholar]
- 29.Agrawal K, Garg R, Bhatnagar S (2019) Knowledge and awareness of end-of-life care among doctors working in intensive care units at a tertiary care center: a questionnaire-based study. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med 23:568–573. 10.5005/jp-journals-10071-23293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sengupta J, Chatterjee SC (2017) Dying in intensive care units of India: commentaries on policies and position papers on palliative and end-of-life care. J Crit Care 39:11–17. 10.1016/j.jcrc.2016.12.017 [DOI] [PubMed] [Google Scholar]
- 31.Rafiq N, Arthur D, Rahim S et al (2021) Nurses’ perceptions about the dignity of intubated patients. Nurs Ethics 28:980–995. 10.1177/0969733020985268 [DOI] [PubMed] [Google Scholar]
- 32.Scheunemann LP, Ernecoff NC, Buddadhumaruk P et al (2019) Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med 179:676–684. 10.1001/jamainternmed.2019.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schenker Y, Crowley-Matoka M, Dohan D et al (2012) I don’t want to be the one saying “we should just let him die”: intrapersonal tensions experienced by surrogate decision makers in the ICU. J Gen Intern Med 27:1657–1665. 10.1007/s11606-012-2129-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kodali S, Stametz RA, Bengier AC et al (2014) Family experience with intensive care unit care: association of self-reported family conferences and family satisfaction. J Crit Care 29:641–644. 10.1016/j.jcrc.2014.03.012 [DOI] [PubMed] [Google Scholar]
- 35.White DB, Angus DC, Shields A-M et al (2018) A Randomized trial of a family-support intervention in intensive care units. N Engl J Med 378:2365–2375. 10.1056/NEJMoa1802637 [DOI] [PubMed] [Google Scholar]
- 36.Azoulay E, Chevret S, Leleu G et al (2000) Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 28:3044–3049 [DOI] [PubMed] [Google Scholar]
- 37.Kerckhoffs MC, Kant M, van Delden JJM et al (2019) Selecting and evaluating decision-making strategies in the intensive care unit: a systematic review. J Crit Care 51:39–45. 10.1016/j.jcrc.2019.01.029 [DOI] [PubMed] [Google Scholar]
- 38.Frivold G, Dale B, Slettebø Å (2015) Family members’ experiences of being cared for by nurses and physicians in Norwegian intensive care units: a phenomenological hermeneutical study. Intensive Crit Care Nurs 31:232–240. 10.1016/j.iccn.2015.01.006 [DOI] [PubMed] [Google Scholar]
- 39.Kentish-Barnes N, Chevret S, Valade S et al (2022) A three-step support strategy for relatives of patients dying in the intensive care unit: a cluster randomised trial. Lancet 399:656–664. 10.1016/S0140-6736(21)02176-0 [DOI] [PubMed] [Google Scholar]
- 40.Silverman H, Wilson T, Tisherman S et al (2022) Ethical decision-making climate, moral distress, and intention to leave among ICU professionals in a tertiary academic hospital center. BMC Med Ethics 23:45. 10.1186/s12910-022-00775-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamric AB, Blackhall LJ (2007) Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med 35:422–429. 10.1097/01.CCM.0000254722.50608.2D [DOI] [PubMed] [Google Scholar]
- 42.Watts T, Sydor A, Whybrow D et al (2023) Registered Nurses’ and nursing students’ perspectives on moral distress and its effects: a mixed-methods systematic review and thematic synthesis. Nurs Open 10:6014–6032. 10.1002/nop2.1913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Neville TH, Wiley JF, Yamamoto MC et al (2015) Concordance of nurses and physicians on whether critical care patients are receiving futile treatment. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses 24:403–410. 10.4037/ajcc2015476 [DOI] [PubMed] [Google Scholar]
- 44.Van den Bulcke B, Metaxa V, Reyners AK et al (2020) Ethical climate and intention to leave among critical care clinicians: an observational study in 68 intensive care units across Europe and the United States. Intensive Care Med 46:46–56. 10.1007/s00134-019-05829-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Curtis JR, Higginson IJ, White DB (2022) Integrating palliative care into the ICU: a lasting and developing legacy. Intensive Care Med 48:939–942. 10.1007/s00134-022-06729-7 [DOI] [PubMed] [Google Scholar]
- 46.Romano AM, Gade KE, Nielsen G et al (2017) Early Palliative care reduces end-of-life intensive care unit (ICU) use but not ICU course in patients with advanced cancer. Oncologist 22:318–323. 10.1634/theoncologist.2016-0227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haun MW, Estel S, Rücker G et al (2017) Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev 6:CD011129. 10.1002/14651858.CD011129.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carson SS, Cox CE, Wallenstein S et al (2016) Effect of palliative care-led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA 316:51–62. 10.1001/jama.2016.8474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ma J, Chi S, Buettner B et al (2019) Early palliative care consultation in the medical ICU: a cluster randomized crossover trial. Crit Care Med 47:1707–1715. 10.1097/CCM.0000000000004016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Helgeson SA, Burnside RC, Robinson MT et al (2023) Early versus usual palliative care consultation in the intensive care unit. Am J Hosp Palliat Care 40:544–551. 10.1177/10499091221115732 [DOI] [PubMed] [Google Scholar]
- 51.Kamdar BB, Suri R, Suchyta MR et al (2020) Return to work after critical illness: a systematic review and meta-analysis. Thorax 75:17–27. 10.1136/thoraxjnl-2019-213803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Babar A, Eilenfeld K, Alqaisi S et al (2021) Incorporating early palliative medicine consultation into daily morning huddle in the ICU. Crit Care Explor 3:e0459. 10.1097/CCE.0000000000000459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bhangu JK, Young BT, Posillico S et al (2020) Goals of care discussions for the imminently dying trauma patient. J Surg Res 246:269–273. 10.1016/j.jss.2019.07.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chang H-T, Jerng J-S, Chen D-R (2020) Reduction of healthcare costs by implementing palliative family conference with the decision to withdraw life-sustaining treatments. J Formos Med Assoc Taiwan Yi Zhi 119:34–41. 10.1016/j.jfma.2019.02.011 [DOI] [PubMed] [Google Scholar]
- 55.Kupensky DT, Emerick ES, Hileman BM, Chance EA (2020) The association of time to palliative medicine consultation on geriatric trauma outcomes. J Trauma Nurs Off J Soc Trauma Nurses 27:177–184. 10.1097/JTN.0000000000000508 [DOI] [PubMed] [Google Scholar]
- 56.Mehta A, Krishnasamy P, Chai E et al (2023) Lessons learned from an embedded palliative care model in the medical intensive care unit. J Pain Symptom Manage 65:e321–e327. 10.1016/j.jpainsymman.2022.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pottash M, McCamey D, Groninger H et al (2020) Palliative care consultation and effect on length of stay in a tertiary-level neurological intensive care unit. Palliat Med Rep 1:161–165. 10.1089/pmr.2020.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tabibian BE, Salehani AA, Kuhn EN et al (2019) Transitioning the treatment paradigm: how early palliative care service involvement affects the end-of-life course for critically ill patients in the neuro-intensive care unit. J Palliat Med 22:489–492. 10.1089/jpm.2018.0428 [DOI] [PubMed] [Google Scholar]
- 59.Rose L, Haslam L, Dale C et al (2013) Behavioral pain assessment tool for critically ill adults unable to self-report pain. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses 22:246–255. 10.4037/ajcc2013200 [DOI] [PubMed] [Google Scholar]
- 60.Guttormson JL, Khan B, Brodsky MB et al (2023) Symptom assessment for mechanically ventilated patients: principles and priorities: an official american thoracic society workshop Report. Ann Am Thorac Soc 20:491–498. 10.1513/AnnalsATS.202301-023ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Damico V, Cazzaniga F, Murano L et al (2018) Impact of a clinical therapeutic intervention on pain assessment, management, and nursing practices in an intensive care unit: a before-and-after study. Pain Manag Nurs Off J Am Soc Pain Manag Nurses 19:256–266. 10.1016/j.pmn.2018.01.007 [DOI] [PubMed] [Google Scholar]
- 62.Hamdan KM (2019) Nurses’ assessment practices of pain among critically ill patients. Pain Manag Nurs Off J Am Soc Pain Manag Nurses 20:489–496. 10.1016/j.pmn.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 63.Kalfon P, Baumstarck K, Estagnasie P et al (2017) A tailored multicomponent program to reduce discomfort in critically ill patients: a cluster-randomized controlled trial. Intensive Care Med 43:1829–1840. 10.1007/s00134-017-4991-x [DOI] [PubMed] [Google Scholar]
- 64.Radtke FM, Heymann A, Franck M et al (2012) How to implement monitoring tools for sedation, pain and delirium in the intensive care unit: an experimental cohort study. Intensive Care Med 38:1974–1981. 10.1007/s00134-012-2658-1 [DOI] [PubMed] [Google Scholar]
- 65.Gélinas C, Arbour C, Michaud C et al (2013) Patients and ICU nurses’ perspectives of non-pharmacological interventions for pain management. Nurs Crit Care 18:307–318. 10.1111/j.1478-5153.2012.00531.x [DOI] [PubMed] [Google Scholar]
- 66.Gélinas C, Arbour C, Michaud C et al (2011) Implementation of the critical-care pain observation tool on pain assessment/management nursing practices in an intensive care unit with nonverbal critically ill adults: a before and after study. Int J Nurs Stud 48:1495–1504. 10.1016/j.ijnurstu.2011.03.012 [DOI] [PubMed] [Google Scholar]
- 67.Topolovec-Vranic J, Canzian S, Innis J et al (2010) Patient satisfaction and documentation of pain assessments and management after implementing the adult nonverbal pain scale. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses 19:345–354. 10.4037/ajcc2010247 [DOI] [PubMed] [Google Scholar]
- 68.Chanques G, Jaber S, Barbotte E et al (2006) Impact of systematic evaluation of pain and agitation in an intensive care unit. Crit Care Med 34:1691–1699. 10.1097/01.CCM.0000218416.62457.56 [DOI] [PubMed] [Google Scholar]
- 69.Voigt L, Paice JA, Pouliot J (1995) Standardized pain flowsheet: impact on patient-reported pain experiences after cardiovascular surgery. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses 4:308–313 [PubMed] [Google Scholar]
- 70.Georgiou E, Hadjibalassi M, Lambrinou E et al (2015) The impact of pain assessment on critically ill patients’ outcomes: a systematic review. BioMed Res Int 2015:503830. 10.1155/2015/503830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Payen J-F, Bosson J-L, Chanques G et al (2009) Pain assessment is associated with decreased duration of mechanical ventilation in the intensive care unit: a post Hoc analysis of the DOLOREA study. Anesthesiology 111:1308–1316. 10.1097/ALN.0b013e3181c0d4f0 [DOI] [PubMed] [Google Scholar]
- 72.Baumstarck K, Boucekine M, Estagnasie P et al (2019) Assessment of patients’’ self-perceived intensive care unit discomforts: validation of the 18-item version of the IPREA. Health Qual Life Outcomes 17:29. 10.1186/s12955-019-1101-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jodaki K, Abdi K, Mousavi M-S et al (2021) Effect of rosa damascene aromatherapy on anxiety and sleep quality in cardiac patients: a randomized controlled trial. Complement Ther Clin Pract 42:101299. 10.1016/j.ctcp.2020.101299 [DOI] [PubMed] [Google Scholar]
- 74.Leong RW, Davies LJ, Fook-Chong S et al (2021) Effect of the use of earplugs and eye masks on the quality of sleep after major abdominal surgery: a randomised controlled trial. Anaesthesia 76:1482–1491. 10.1111/anae.15468 [DOI] [PubMed] [Google Scholar]
- 75.Altintaş S, Çelik S, Karahan E (2024) The effects of ergonomic sleep mask use on sleep quality and comfort in intensive care patients. J Sleep Res 33:e13966. 10.1111/jsr.13966 [DOI] [PubMed] [Google Scholar]
- 76.Obanor OO, McBroom MM, Elia JM et al (2021) The impact of earplugs and eye masks on sleep quality in surgical ICU patients at risk for frequent awakenings. Crit Care Med 49:e822–e832. 10.1097/CCM.0000000000005031 [DOI] [PubMed] [Google Scholar]
- 77.Alinia-Najjar R, Bagheri-Nesami M, Shorofi SA et al (2020) The effect of foot reflexology massage on burn-specific pain anxiety and sleep quality and quantity of patients hospitalized in the burn intensive care unit (ICU). Burns J Int Soc Burn Inj 46:1942–1951. 10.1016/j.burns.2020.04.035 [DOI] [PubMed] [Google Scholar]
- 78.Gandolfi JV, Di Bernardo APA, Chanes DAV et al (2020) The effects of melatonin supplementation on sleep quality and assessment of the serum melatonin in ICU patients: a randomized controlled trial. Crit Care Med 48:e1286–e1293. 10.1097/CCM.0000000000004690 [DOI] [PubMed] [Google Scholar]
- 79.Robert R, Le Gouge A, Kentish-Barnes N et al (2017) Terminal weaning or immediate extubation for withdrawing mechanical ventilation in critically ill patients (the ARREVE observational study). Intensive Care Med. 10.1007/s00134-017-4891-0 [DOI] [PubMed] [Google Scholar]
- 80.Campbell ML, Yarandi HN, Mendez M (2015) A two-group trial of a terminal ventilator withdrawal algorithm: pilot testing. J Palliat Med 18:781–785. 10.1089/jpm.2015.0111 [DOI] [PubMed] [Google Scholar]
- 81.Vink EE, Azoulay E, Caplan A et al (2018) Time-limited trial of intensive care treatment: an overview of current literature. Intensive Care Med 44:1369–1377. 10.1007/s00134-018-5339-x [DOI] [PubMed] [Google Scholar]
- 82.Quill TE, Holloway R (2011) Time-limited trials near the end of life. JAMA 306:1483–1484. 10.1001/jama.2011.1413 [DOI] [PubMed] [Google Scholar]
- 83.Hill SA, Dawood A, Boland E et al (2022) Palliative medicine in the intensive care unit: needs, delivery, quality. BMJ Support Palliat Care 12:38–41. 10.1136/bmjspcare-2020-002795 [DOI] [PubMed] [Google Scholar]
- 84.Adamski J, Weigl W, Musialowicz T et al (2022) Predictors of treatment limitations in Finnish intensive care units. Acta Anaesthesiol Scand 66:526–538. 10.1111/aas.14035 [DOI] [PubMed] [Google Scholar]
- 85.Chavez G, Richman IB, Kaimal R et al (2018) Reversals and limitations on high-intensity, life-sustaining treatments. PLoS ONE 13:e0190569. 10.1371/journal.pone.0190569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Benoit D, van der Zee E, Darmon M et al (2021) Outcomes of ICU patients with and without perceptions of excessive care: a comparison between cancer and non-cancer patients. Ann Intensive Care 11:120. 10.1186/s13613-021-00895-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Turnbull AE, Ruhl AP, Lau BM et al (2014) Timing of limitations in life support in acute lung injury patients: a multisite study. Crit Care Med 42:296–302. 10.1097/CCM.0b013e3182a272db [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Peñasco Y, González-Castro A, Rodríguez Borregán JC et al (2017) Limitation of life-sustaining treatment in severe trauma in the elderly after admission to an intensive care unit. Med Intensiva 41:394–400. 10.1016/j.medin.2017.03.009 [DOI] [PubMed] [Google Scholar]
- 89.Xu HG, Kynoch K, Tuckett A, Eley R (2020) Effectiveness of interventions to reduce emergency department staff occupational stress and/or burnout: a systematic review. JBI Evid Synth 18:1156–1188. 10.11124/JBISRIR-D-19-00252 [DOI] [PubMed] [Google Scholar]
- 90.Bocci MG, D’Alò C, Barelli R et al (2016) Taking Care of relationships in the intensive care unit: positive impact on family consent for organ donation. Transplant Proc 48:3245–3250. 10.1016/j.transproceed.2016.09.042 [DOI] [PubMed] [Google Scholar]
- 91.Curtis JR, Treece PD, Nielsen EL et al (2008) Integrating palliative and critical care: evaluation of a quality-improvement intervention. Am J Respir Crit Care Med 178:269–275. 10.1164/rccm.200802-272OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Black MD, Vigorito MC, Curtis JR et al (2013) A multifaceted intervention to improve compliance with process measures for ICU clinician communication with ICU patients and families. Crit Care Med 41:2275–2283. 10.1097/CCM.0b013e3182982671 [DOI] [PubMed] [Google Scholar]
- 93.Curtis JR, Back AL, Ford DW et al (2013) Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA 310:2271–2281. 10.1001/jama.2013.282081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Azoulay E, Pochard F, Chevret S et al (2001) Meeting the needs of intensive care unit patient families: a multicenter study. Am J Respir Crit Care Med 163:135–139. 10.1164/ajrccm.163.1.2005117 [DOI] [PubMed] [Google Scholar]
- 95.Azoulay E, Pochard F, Chevret S et al (2002) Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med 165:438–442. 10.1164/ajrccm.165.4.200108-006oc [DOI] [PubMed] [Google Scholar]
- 96.Scheunemann LP, McDevitt M, Carson SS, Hanson LC (2011) Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Chest 139:543–554. 10.1378/chest.10-0595 [DOI] [PubMed] [Google Scholar]
- 97.Oczkowski SJW, Chung H-O, Hanvey L et al (2016) Communication tools for end-of-life decision-making in the intensive care unit: a systematic review and meta-analysis. Crit Care Lond Engl 20:97. 10.1186/s13054-016-1264-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lautrette A, Darmon M, Megarbane B et al (2007) A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 356:469–478. 10.1056/NEJMoa063446 [DOI] [PubMed] [Google Scholar]
- 99.Robin S, Labarriere C, Sechaud G et al (2021) Information pamphlet given to relatives during the end-of-life decision in the ICU: an assessor-blinded, randomized controlled trial. Chest 159:2301–2308. 10.1016/j.chest.2021.01.072 [DOI] [PubMed] [Google Scholar]
- 100.Chiang VCL, Lee RLP, Ho MF et al (2017) Fulfilling the psychological and information need of the family members of critically ill patients using interactive mobile technology: a randomised controlled trial. Intensive Crit Care Nurs 41:77–83. 10.1016/j.iccn.2017.03.006 [DOI] [PubMed] [Google Scholar]
- 101.Greenberg JA, Basapur S, Quinn TV et al (2022) Daily written care summaries for families of critically ill patients: a randomized controlled trial. Crit Care Med 50:1296–1305. 10.1097/CCM.0000000000005583 [DOI] [PubMed] [Google Scholar]
- 102.Mistraletti G, Umbrello M, Mantovani ES et al (2017) A family information brochure and dedicated website to improve the ICU experience for patients’ relatives: an Italian multicenter before-and-after study. Intensive Care Med 43:69–79. 10.1007/s00134-016-4592-0 [DOI] [PubMed] [Google Scholar]
- 103.Amass T, Van Scoy LJ, Hua M et al (2022) Stress-related disorders of family members of patients admitted to the intensive care unit with COVID-19. JAMA Intern Med. 10.1001/jamainternmed.2022.1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Azoulay E, Forel J, Vinatier I et al (2018) Questions to improve family-staff communication in the ICU: a randomized controlled trial. Intensive Care Med 44:1879–1887. 10.1007/s00134-018-5423-2 [DOI] [PubMed] [Google Scholar]
- 105.Danis M, Federman D, Fins JJ et al (1999) Incorporating palliative care into critical care education: principles, challenges, and opportunities. Crit Care Med 27:2005–2013. 10.1097/00003246-199909000-00047 [DOI] [PubMed] [Google Scholar]
- 106.Cohen R, Sprung CL (1999) Critical care education in the medical school curriculum. Crit Care Med 27:2068–2069. 10.1097/00003246-199909000-00080 [DOI] [PubMed] [Google Scholar]
- 107.Brown CE, Back AL, Ford DW et al (2018) Self-assessment scores improve after simulation-based palliative care communication skill workshops. Am J Hosp Palliat Care 35:45–51. 10.1177/1049909116681972 [DOI] [PubMed] [Google Scholar]
- 108.Darmon M, Ducos G, Coquet I et al (2016) Formal academic training on ethics may address junior physicians’’ needs. Chest 150:180–187. 10.1016/j.chest.2016.02.651 [DOI] [PubMed] [Google Scholar]
- 109.Bassah N, Cox K, Seymour J (2016) A qualitative evaluation of the impact of a palliative care course on preregistration nursing students’ practice in cameroon. BMC Palliat Care 15:37. 10.1186/s12904-016-0106-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Schwartz J, Schallenburger M, Tenge T et al (2022) Palliative care e-learning for physicians caring for critically ill and dying patients during the COVID-19 pandemic: an outcome evaluation with self-assessed knowledge and attitude. Int J Environ Res Public Health 19:12377. 10.3390/ijerph191912377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Engelberg R, Downey L, Curtis JR (2006) Psychometric characteristics of a quality of communication questionnaire assessing communication about end-of-life care. J Palliat Med 9:1086–1098. 10.1089/jpm.2006.9.1086 [DOI] [PubMed] [Google Scholar]
- 112.Kyeremanteng K, Gagnon L-P, Thavorn K et al (2018) The impact of palliative care consultation in the ICU on length of stay: a systematic review and cost evaluation. J Intensive Care Med 33:346–353. 10.1177/0885066616664329 [DOI] [PubMed] [Google Scholar]
- 113.Tanaka Y, Masukawa K, Kawashima A et al (2023) Quality indicators for palliative care in intensive care units: a systematic review. Ann Palliat Med 12:584–599. 10.21037/apm-22-1005 [DOI] [PubMed] [Google Scholar]
- 114.Kaufer M, Murphy P, Barker K, Mosenthal A (2008) Family satisfaction following the death of a loved one in an inner city MICU. Am J Hosp Palliat Care 25:318–325. 10.1177/1049909108319262 [DOI] [PubMed] [Google Scholar]
- 115.McCormick AJ, Curtis JR, Stowell-Weiss P et al (2010) Improving social work in intensive care unit palliative care: results of a quality improvement intervention. J Palliat Med 13:297–304. 10.1089/jpm.2009.0204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Aslakson R, Cheng J, Vollenweider D et al (2014) Evidence-based palliative care in the intensive care unit: a systematic review of interventions. J Palliat Med 17:219–235. 10.1089/jpm.2013.0409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Curtis JR, Engelberg RA, Wenrich MD et al (2002) Studying communication about end-of-life care during the ICU family conference: development of a framework. J Crit Care 17:147–160 [DOI] [PubMed] [Google Scholar]
- 118.Lautrette A, Ciroldi M, Ksibi H, Azoulay E (2006) End-of-life family conferences: rooted in the evidence. Crit Care Med 34:S364-372. 10.1097/01.CCM.0000237049.44246.8C [DOI] [PubMed] [Google Scholar]
- 119.Rosa RG, Falavigna M, da Silva DB et al (2019) Effect of flexible family visitation on delirium among patients in the intensive care unit: the ICU visits randomized clinical trial. JAMA 322:216–228. 10.1001/jama.2019.8766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chapman DK, Collingridge DS, Mitchell LA et al (2016) Satisfaction with elimination of all visitation restrictions in a mixed-profile intensive care unit. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses 25:46–50. 10.4037/ajcc2016789 [DOI] [PubMed] [Google Scholar]
- 121.Nassar Junior AP, Besen BAMP, Robinson CC et al (2018) Flexible versus restrictive visiting policies in ICUS: a systematic review and meta-analysis. Crit Care Med 46:1175–1180. 10.1097/CCM.0000000000003155 [DOI] [PubMed] [Google Scholar]
- 122.Schnell D, Abadie S, Toullic P et al (2013) Open visitation policies in the ICU: experience from relatives and clinicians. Intensive Care Med 39:1873–1874. 10.1007/s00134-013-2956-2 [DOI] [PubMed] [Google Scholar]
- 123.Mitchell ML, Aitken LM (2017) Flexible visiting positively impacted on patients, families and staff in an Australian Intensive Care Unit: a before-after mixed method study. Aust Crit Care Off J Confed Aust Crit Care Nurses 30:91–97. 10.1016/j.aucc.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 124.Baharoon S, Al Yafi W, Al Qurashi A et al (2017) Family satisfaction in critical care units: does an open visiting hours policy have an impact? J Patient Saf 13:169–174. 10.1097/PTS.0000000000000140 [DOI] [PubMed] [Google Scholar]
- 125.Giannini A, Garrouste-Orgeas M, Latour JM (2014) What’s new in ICU visiting policies: can we continue to keep the doors closed? Intensive Care Med 40:730–733. 10.1007/s00134-014-3267-y [DOI] [PubMed] [Google Scholar]
- 126.Davidson J, Aslakson R, Long A et al (2017) Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 45:103–128. 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]
- 127.Afzali Rubin M, Svensson TL, Herling SF et al (2023) Family presence during resuscitation. Cochrane Database Syst Rev 5:CD013619. 10.1002/14651858.CD013619.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fulbrook P, Latour J, Albarran J et al (2007) The presence of family members during cardiopulmonary resuscitation: European federation of critical care nursing associations, European society of paediatric and neonatal intensive care and European society of cardiology council on cardiovascular nursing and allied professions joint position statement. Nurs Crit Care 12:250–252. 10.1111/j.1478-5153.2007.00240.x [DOI] [PubMed] [Google Scholar]
- 129.Pattison NA, White C, Lone NI (2021) Bereavement in critical care: a narrative review and practice exploration of current provision of support services and future challenges. J Intensive Care Soc 22:349–356. 10.1177/1751143720928898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kentish-Barnes N, Cohen-Solal Z, Souppart V et al (2017) “It was the only thing i could hold onto, but…”: receiving a letter of condolence after loss of a loved one in the ICU: a qualitative study of bereaved relatives’’ experience. Crit Care Med 45:1965–1971. 10.1097/CCM.0000000000002687 [DOI] [PubMed] [Google Scholar]
- 131.Kentish-Barnes N, Chevret S, Champigneulle B et al (2017) Effect of a condolence letter on grief symptoms among relatives of patients who died in the ICU: a randomized clinical trial. Intensive Care Med 43:473–484. 10.1007/s00134-016-4669-9 [DOI] [PubMed] [Google Scholar]
- 132.Kock M, Berntsson C, Bengtsson A (2014) A follow-up meeting post death is appreciated by family members of deceased patients. Acta Anaesthesiol Scand 58:891–896. 10.1111/aas.12358 [DOI] [PubMed] [Google Scholar]
- 133.Binette E, Elwell J, Parekh de Campos A, Anderson RV (2023) Show and tell: photography and storytelling to better understand the end-of-life experience of families in the intensive care unit. Omega. 10.1177/00302228231190957 [DOI] [PubMed] [Google Scholar]
- 134.Johansson M, Wåhlin I, Magnusson L et al (2018) Family members’ experiences with intensive care unit diaries when the patient does not survive. Scand J Caring Sci 32:233–240. 10.1111/scs.12454 [DOI] [PubMed] [Google Scholar]
- 135.Coventry A, Gerdtz M, McInnes E et al (2023) Supporting families of patients who die in adult intensive care: a scoping review of interventions. Intensive Crit Care Nurs 78:103454. 10.1016/j.iccn.2023.103454 [DOI] [PubMed] [Google Scholar]
- 136.Bazzano G, Buccoliero F, Villa M et al (2023) The role of intensive care unit diaries in the grieving process: a monocentric qualitative study. Nurs Crit Care. 10.1111/nicc.13012 [DOI] [PubMed] [Google Scholar]
- 137.Moss SJ, Wollny K, Poulin TG et al (2021) Bereavement interventions to support informal caregivers in the intensive care unit: a systematic review. BMC Palliat Care 20:66. 10.1186/s12904-021-00763-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Riegel M, Randall S, Buckley T (2019) Memory making in end-of-life care in the adult intensive care unit: a scoping review of the research literature. Aust Crit Care Off J Confed Aust Crit Care Nurses 32:442–447. 10.1016/j.aucc.2018.12.002 [DOI] [PubMed] [Google Scholar]
- 139.Santiago C, Lee C, Piacentino R et al (2017) A pilot study of an interprofessional, multi-component bereavement follow-up program in the intensive care unit. Can J Crit Care Nurs 28:18–24 [Google Scholar]
- 140.Vanstone M, Toledo F, Clarke F et al (2016) Narrative medicine and death in the ICU: word clouds as a visual legacy. BMJ Support Palliat Care. 10.1136/bmjspcare-2016-001179 [DOI] [PubMed] [Google Scholar]
- 141.Efstathiou N, Walker W, Metcalfe A, Vanderspank-Wright B (2019) The state of bereavement support in adult intensive care: a systematic review and narrative synthesis. J Crit Care 50:177–187. 10.1016/j.jcrc.2018.11.026 [DOI] [PubMed] [Google Scholar]
- 142.Hetland BD, McAndrew NS, Kupzyk KA et al (2022) Family caregiver preferences and contributions related to patient care in the ICU. West J Nurs Res 44:214–226. 10.1177/01939459211062954 [DOI] [PubMed] [Google Scholar]
- 143.Amass TH, Villa G, OMahony S et al (2020) Family care rituals in the icu to reduce symptoms of post-traumatic stress disorder in family members-a multicenter, multinational, before-and-after intervention trial. Crit Care Med 48:176–184. 10.1097/CCM.0000000000004113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rose L, Yu L, Casey J et al (2021) Communication and Virtual visiting for families of patients in intensive care during COVID-19: a UK National Survey. Ann Am Thorac Soc. 10.1513/AnnalsATS.202012-1500OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kentish-Barnes N, Cohen-Solal Z, Morin L et al (2021) Lived experiences of family members of patients with severe COVID-19 who died in intensive care units in France. JAMA Netw Open 4:e2113355. 10.1001/jamanetworkopen.2021.13355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Cox C, Olsen O, Parish A et al (2022) Palliative care phenotypes among critically ill patients and family members: intensive care unit prospective cohort study. BMJ Support Palliat Care. 10.1136/spcare-2022-003622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ashana DC, Welsh W, Preiss D et al (2024) Racial differences in shared decision-making about critical illness. JAMA Intern Med 184:424–432. 10.1001/jamainternmed.2023.8433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Brooks LA, Bloomer MJ, Manias E (2019) Culturally sensitive communication at the end-of-life in the intensive care unit: a systematic review. Aust Crit Care Off J Confed Aust Crit Care Nurses 32:516–523. 10.1016/j.aucc.2018.07.003 [DOI] [PubMed] [Google Scholar]
- 149.Long AC, Engelberg RA, Downey L et al (2014) Race, income, and education: associations with patient and family ratings of end-of-life care and communication provided by physicians-in-training. J Palliat Med 17:435–447. 10.1089/jpm.2013.0214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lee JJ, Long AC, Curtis JR, Engelberg RA (2016) The influence of race/ethnicity and education on family ratings of the quality of dying in the ICU. J Pain Symptom Manage 51:9–16. 10.1016/j.jpainsymman.2015.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cox CE, Ashana DC, Riley IL et al (2024) Mobile application-based communication facilitation platform for family members of critically ill patients: a randomized clinical trial. JAMA Netw Open 7:e2349666. 10.1001/jamanetworkopen.2023.49666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.McAndrew NS, Schiffman R, Leske J (2019) Relationships among climate of care, nursing family care and family well-being in ICUs. Nurs Ethics 26:2494–2510. 10.1177/0969733019826396 [DOI] [PubMed] [Google Scholar]
- 153.Schwarzkopf D, Westermann I, Skupin H et al (2015) A novel questionnaire to measure staff perception of end-of-life decision making in the intensive care unit–development and psychometric testing. J Crit Care 30:187–195. 10.1016/j.jcrc.2014.09.015 [DOI] [PubMed] [Google Scholar]
- 154.Brooks LA, Manias E, Nicholson P (2017) Communication and decision-making about end-of-life care in the intensive care unit. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses 26:336–341. 10.4037/ajcc2017774 [DOI] [PubMed] [Google Scholar]
- 155.Poi CH, Khoo HS, Ang S-L et al (2023) Palliative care integration in the intensive care unit: healthcare professionals’ perspectives - a qualitative study. BMJ Support Palliat Care. 10.1136/spcare-2022-003789 [DOI] [PubMed] [Google Scholar]
- 156.Vincent J, Boulanger C, van Mol M et al (2022) Ten areas for ICU clinicians to be aware of to help retain nurses in the ICU. Crit Care 26:310. 10.1186/s13054-022-04182-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Flannery L, Ramjan LM, Peters K (2016) End-of-life decisions in the Intensive Care Unit (ICU) - exploring the experiences of ICU nurses and doctors - a critical literature review. Aust Crit Care Off J Confed Aust Crit Care Nurses 29:97–103. 10.1016/j.aucc.2015.07.004 [DOI] [PubMed] [Google Scholar]
- 158.Moss M, Good VS, Gozal D et al (2016) An official critical care societies collaborative statement-burnout syndrome in critical care health-care professionals: a call for action. Chest 150:17–26. 10.1016/j.chest.2016.02.649 [DOI] [PubMed] [Google Scholar]
- 159.Boulton AJ, Slowther A-M, Yeung J, Bassford C (2023) Moral distress among intensive care unit professions in the UK: a mixed-methods study. BMJ Open 13:e068918. 10.1136/bmjopen-2022-068918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Giabicani M, Arditty L, Mamzer M-F et al (2023) Team-family conflicts over end-of-life decisions in ICU: a survey of French physicians’ beliefs. PLoS ONE 18:e0284756. 10.1371/journal.pone.0284756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Spijkers AS, Akkermans A, Smets EMA et al (2022) How doctors manage conflicts with families of critically ill patients during conversations about end-of-life decisions in neonatal, pediatric, and adult intensive care. Intensive Care Med 48:910–922. 10.1007/s00134-022-06771-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Papazian L, Hraiech S, Loundou A et al (2023) High-level burnout in physicians and nurses working in adult ICUs: a systematic review and meta-analysis. Intensive Care Med. 10.1007/s00134-023-07025-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Azoulay E, Pochard F, Reignier J et al (2021) Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest 160:944–955. 10.1016/j.chest.2021.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Leiter MP, Maslach C (2016) Latent burnout profiles: a new approach to understanding the burnout experience. Burn Res 3:89–100. 10.1016/j.burn.2016.09.001 [Google Scholar]
- 165.Embriaco N, Papazian L, Kentish-Barnes N et al (2007) Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care 13:482–488. 10.1097/MCC.0b013e3282efd28a [DOI] [PubMed] [Google Scholar]
- 166.Azoulay E, De Waele J, Ferrer R et al (2020) Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care 10:110. 10.1186/s13613-020-00722-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kok N, Van Gurp J, van der Hoeven JG et al (2023) Complex interplay between moral distress and other risk factors of burnout in ICU professionals: findings from a cross-sectional survey study. BMJ Qual Saf 32:225–234. 10.1136/bmjqs-2020-012239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Burghi G, Lambert J, Chaize M et al (2014) Prevalence, risk factors and consequences of severe burnout syndrome in ICU. Intensive Care Med 40:1785–1786. 10.1007/s00134-014-3454-x [DOI] [PubMed] [Google Scholar]
- 169.Alvarez C (2020) Replenish at work: an integrative program to decrease stress and promote a culture of wellness in the intensive care unit. Crit Care Nurs Clin North Am 32:369–381. 10.1016/j.cnc.2020.05.001 [DOI] [PubMed] [Google Scholar]
- 170.Quenot JP, Rigaud JP, Prin S et al (2012) Suffering among carers working in critical care can be reduced by an intensive communication strategy on end-of-life practices. Intensive Care Med 38:55–61. 10.1007/s00134-011-2413-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Poncet M, Toullic P, Papazian L et al (2007) Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med 175:698–704. 10.1164/rccm.200606-806OC [DOI] [PubMed] [Google Scholar]